Summary
The case study involves a patient presenting middle cerebral artery thrombosis, related to a severe vasospasm following subarachnoid hemorrhage due to aneurysm rupture. The patient was treated initially by surgical clipping of the left middle cerebral artery aneurysm. After surgery, the neurological status of the patient was normal. Six days later, the patient presented right hemiplegia and aphasia that were related to the proximal left middle cerebral artery thrombosis. Despite recent open-skull surgery, in situ thrombolysis using urokinase and antiplatelet antibodies (abciximab) was performed. The thrombosed artery was reopened and a severe vasospasm was observed. The vasospasm was treated by transluminal angioplasty. No intracranial hemorrhage was noted after thrombolysis and angioplasty, whereas subcutaneous hemorrhage around the scalp incision was observed. The patient recovered from motor and language impairment. The only long-term symptom was a mild dysorthographia. Balance of risk/benefit is discussed for such aggressive thrombolytic therapy. In this particular case, effectiveness and uneventful use of abciximab was demonstrated despite very recent brain surgery that was considered a formal contra-indication for the use of such a powerful thrombolytic drug.
Vessel thrombosis is an exceptional complication of cerebral vasospasm. In the early hours, intra-arterial thrombolysis may be considered, but recent intracranial surgery is usually an exclusion criterion to performing thrombolysis. We report the case of a patient who underwent thrombolysis and angioplasty in the postoperative period to treat this complication of vasospasm.
Key words: abciximab, thrombolysis, vasospasm, subarachnoid hemorrhage
Case Report
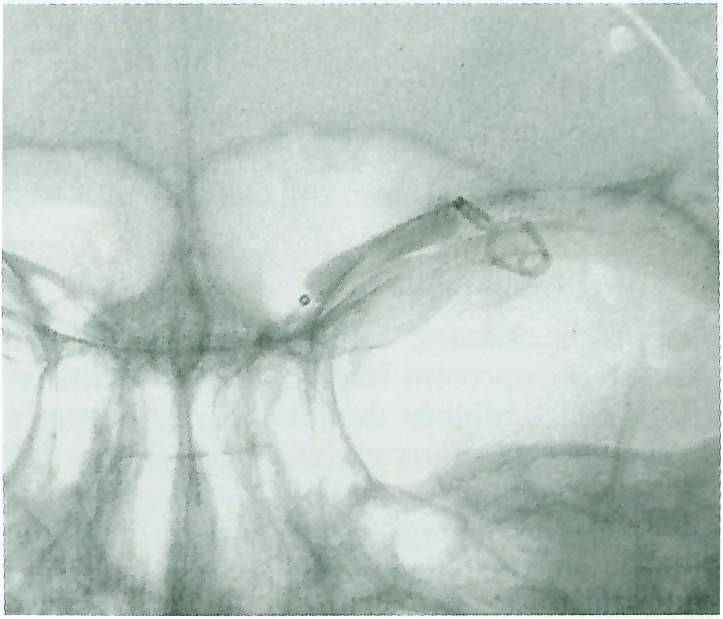
A 36-year-old woman was admitted to the neurosurgical intensive care unit (NICU) for a subarachnoid hemorrhage (SAH). The patient did not have any neurological deficit (grade I in the classification of the World Federation of Neurological Surgeons) and the CT scan showed a diffuse SAH (Fischer grade III). An emergency cerebral angiography disclosed a left middle cerebral artery (MCA) aneurysm located on the MCA bifurcation. The patient underwent a difficult but uneventful operation the same day for clipping of the aneurysm. Three days later, the patient's neurological status was normal. Cerebral blood flow velocities in the middle cerebral arteries (Vmca) measured by transcranial Doppler (TCD) were within normal limits (left side 72 cm.s−1, right side 68 cm.s−1).The patient was discharged from the NICU under treatment with oral nimodip-ine. The CT-scan showed hypodense areas involving mainly the left cortical structures of the temporal pole, the superior temporal gyrus, the insula and the posterior part of the putamen (figure 1). Twenty-four hours later, TCD examination revealed a rise in the left Vmca (Left side 106 cm.s−1, right side 70 cm.s−1) without any clinical deterioration. The patient was again admitted to the NICU to begin intravenous nimodipine and volume expansion. The next day, the left Vmca was 120 cm.s−1 and a “triple H therapy” (hypervolemia, hemodilution and hypertension) was started.
Figure 1.
Postoperative CT-scan before arterial thrombolysis.
The next day at 6:30 a.m., the patient presented sudden right-sided hemiplegia and total aphasia. Volume expansion and increase in blood pressure did not improve the neurological status. No signal in the left MCA could be recorded by TCD examination. At 10.30 a.m., cerebral angiography under general anesthesia disclosed complete thrombosis of the proximal left MCA (figures 2-3). After discussion between the neurosurgeon, neuroradiologist, neuroanesthesiologist, and with the family's informed consent, it was decided to perform arterial thrombolysis. A microcatheter (Rapid transit®, Cordis endovascular systems, Miami Lakes, USA) was positioned in the thrombus to infuse 300000 UI urokinase in 20 minutes followed by attempts at mechanical disruption of the clot using the microguide wire.
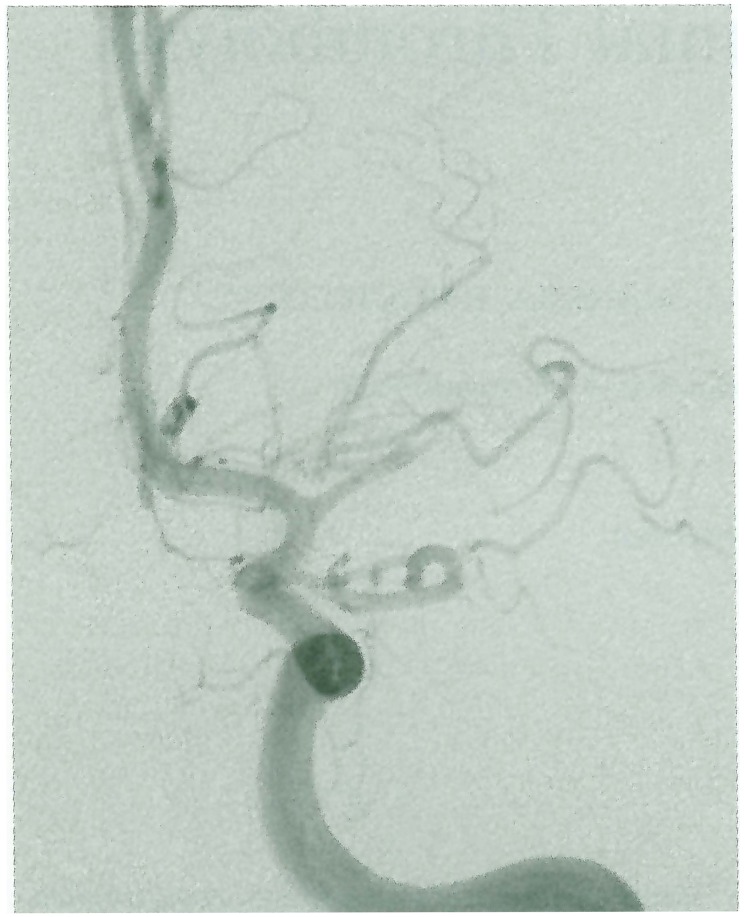
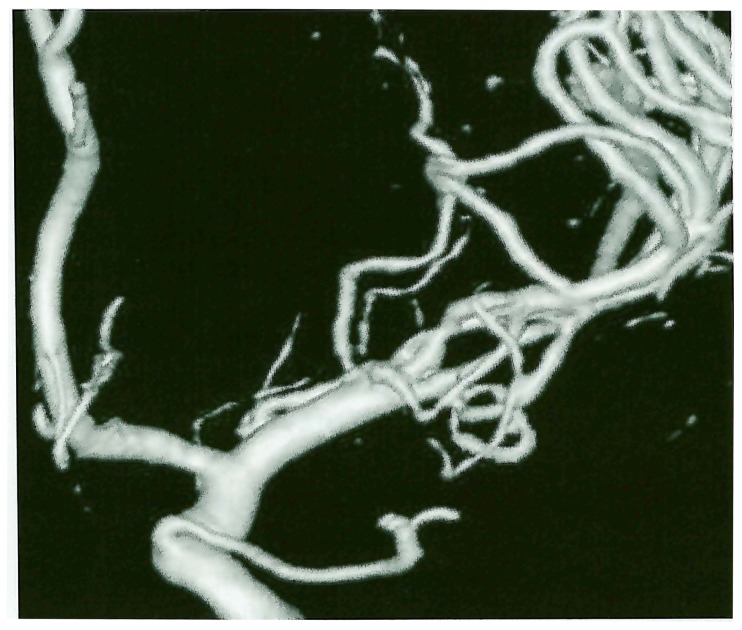
Figure 2.
3D DSA arterial phase showing spasm and thrombosis of left MCA.
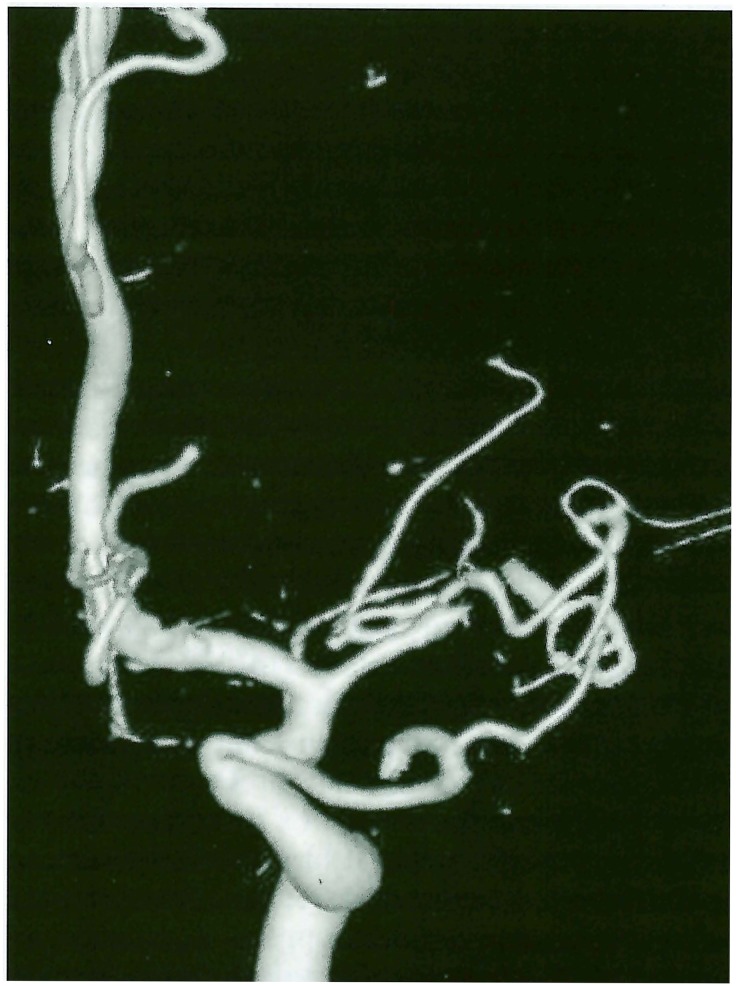
Figure 3.
3D DSA with reconstruction of the surgical clip.
These treatments were unsuccessful and abciximab (ReoPro®, Centocor, Eli Lilly, France) (0.25 mg.kg−1 in 3 minutes) was infused in situ (figure 4).
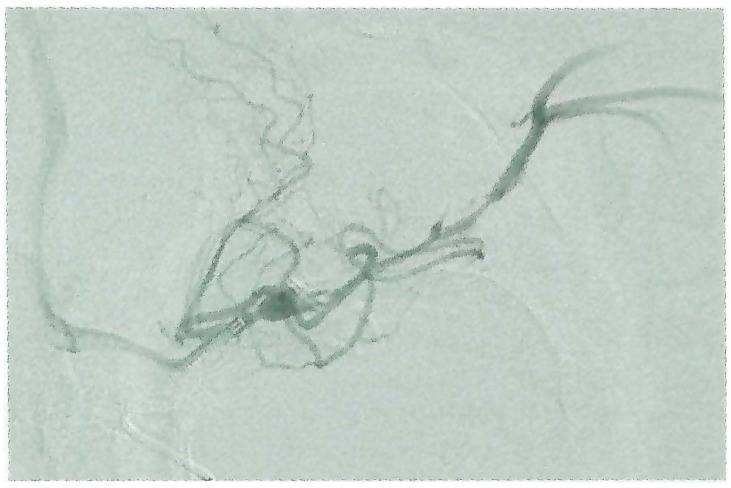
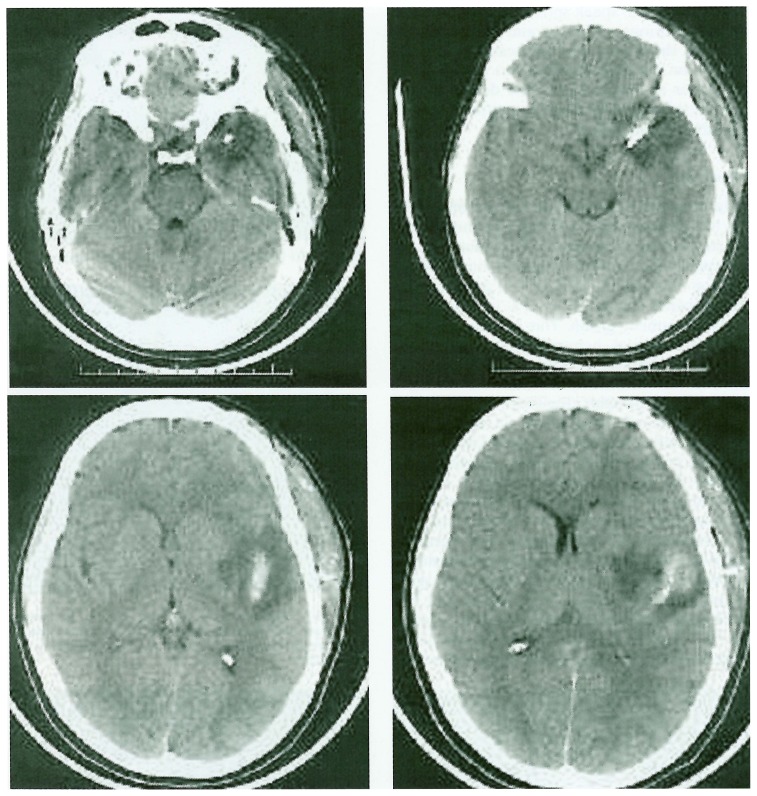
Figure 4.
Hyperselective injection during fibrinolysis (Urokinase and Reopro). Note that the maximum stenosis related to the vasospasm is located 5 mm proximal to the surgical clip.
This permitted complete recanalization of the cerebral artery (figure 5) but revealed a severe proximal MCA vasospasm treated by low pressure (0.5 atmosphere) transluminal angioplasty (figure 6) using a silicon balloon (International Therapeutics Corp., Fremont, Ca, USA). After completion of the procedure (figure 7), the CT scan showed a new left subcutaneous hemorrhage around the scalp incision without any new intracranial hemorrhage (figure 8).
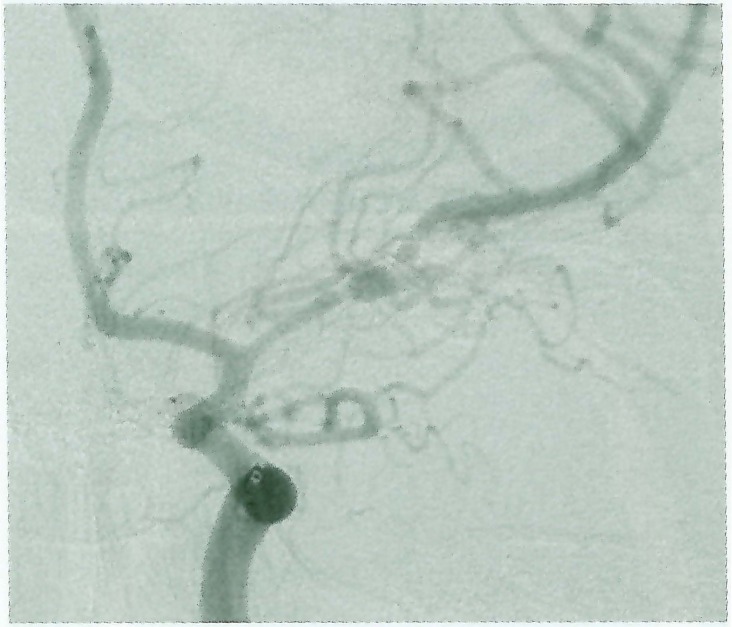
Figure 5.
Result after complete thrombolysis. Severe vasospasm is still located on the proximal MCA.
Figure 6.
Balloon inflation within MCA during angioplasty below the position of the surgical clip.
Figure 7.
Result after angioplasty (3D).
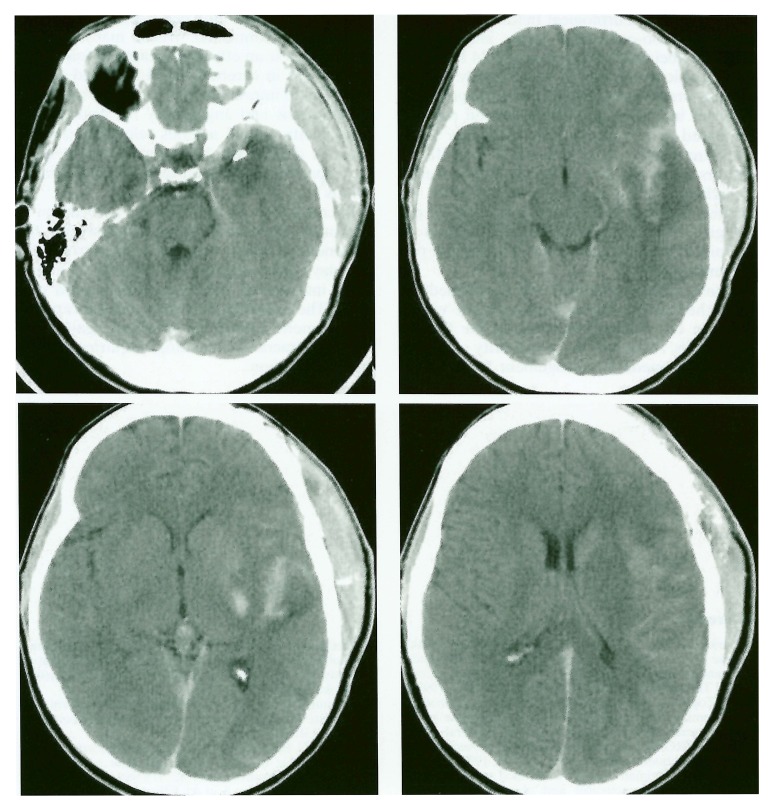
Figure 8.
CT immediatly after thrombolysis and angioplasty. Large subcutaneous hematoma is demonstrated on the side of the craniotomy. No recurrence of intracranial bleeding was noted when compared to onset (initial subarachnoid hemorrhage) and post open surgery CT examination. Temporal pole hypodensity is related to surgery. Cortical-subcortical hypodensity of the insula and peri-insular temporal cortex is related to acute ischemia.
The patient returned to the NICU under treatment with nimodipine, dopamine, heparin and sedation. After stopping sedation, the trachea of the patient was extubated. A few hours later, the patient began to recover from her right-sided hemiplegia. Seven days later, there was only a moderate hemiparesis and the patient was able to speak spontaneously but slowly and laboriously. CT-scan and MRI follow up did not show any new intracerebral hemorrhage nor new hypodensity. Two months later, there was no longer any motor deficit and the patient suffered only minor impairment in writing (dysorthographia).
Discussion
Intra-arterial thrombolysis of cerebral arteries has demonstrated a benefit in the first six hours after an ischemic stroke 1. However, intracranial hemorrhage within 24 hours of admission occurred in 35% of the patients after thrombolysis compared to 13% in the conventional treatment group. This increased risk of early intracranial hemorrhage is the reason why recent intracranial surgery is an exclusion criterion in thrombolytic trials for ischemic stroke. We thoroughly discussed the risk versus benefit ratio of thrombolysis in this patient. Aphasia and hemiplegia is a devastating condition in a young woman. The neurosurgeon considered the risk of cerebral bleeding low because surgery had been strictly confined to the subarachnoid space without any cerebral tear. If a subarachnoid hemorrhage had occurred again due to rupture of intracranial hemostasis, it seemed possible to operate the patient again to drain the hematoma. Nevertheless, the risk of bleeding after surgery should not be neglected. The appearance of a new subcutaneous hematoma in the surgical field after the neuro-radiologic procedure showed the precariousness of surgical hemostasis. Treatment with heparin after thrombolysis may be controversial because it increases the risk of intracranial bleeding2. But the attempts at mechanical disruption of the clot and balloon angioplasty certainly induced a trauma to the vessel wall, which increased the thrombotic risk. Abciximab was considered after failure of recanalization of the vessel by urokinase alone. Abciximab is a chimeric antibody to the human platelet glycoprotein Ilb/IIIa (GP Ilb/IIIa) receptor which inhibits the binding of fibrinogen to platelets and thus platelet aggregation. GP Ilb/IIIab inhibitors combined with plasminogen activators increase the potential for initial thrombolysis, the recanalization rate and decrease the risk of reocclusion during coronary thrombolysis or angioplasty 3,4. A successful treatment with abciximab after failure of re-canalization of the basilar artery with urokinase has also been described5. The most serious adverse effect of the drug is bleeding. In a prospective randomized trial on high-risk coronary angioplasty, the rate of major bleeding was twice as high in the abciximab treated group than in the placebo treated group6. The risk was certainly significant in this patient who suffered postoperative cerebral ischemia. There is only limited experience with GP Ilb/IIIa in-hibitors in the neurological field but a doubleblind, placebo-controlled study showed the safety of abciximab infused within 24 hours after ischemic stroke onset7. In that study, asymptomatic brain parenchymal hemorrhages were detected in 7% of abciximab treated patients compared to 5% in the placebo group. These preliminary data suggest that GP Ilb/IIIa inhibitors are probably safe within 24 hours after an ischemic stroke and may improve the recanalization rate after fibrinolysis. But we did not give the patient abciximab or aspirin or ticlopidine after the procedure to limit the risk of hemorrhage8.
Transluminal angioplasty was performed because there was a severe stenosis of the vessel, which in our opinion was responsible for the thrombosis. Although the superiority of angioplasty over medical management for cerebral arterial spasm has not been demonstrated by prospective controlled trials, many reports show that it is an effective treatment leading to an increase in cerebral blood flow and significant clinical improvement9-11. The association of thrombolysis and angioplasty for acute occlusion of intracranial arteries related to atherosclerotic disease has been reported in a study on 13 patients with good technical and clinical results12.
In conclusion, we describe the association of urokinase, abciximab and angioplasty for the treatment of middle cerebral artery thrombosis five days after surgery for clipping of a ruptured intracranial aneurysm with a good outcome. The potential benefit of this therapeutic management should be weighted against the risk of intracranial bleeding, requiring careful patient selection.
References
- 1.Furlan A, Higashida R, et al. Intra-arterial prourokinase for acute ischemic stroke. The PRO ACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA. 1999;282:2003–2011. doi: 10.1001/jama.282.21.2003. [DOI] [PubMed] [Google Scholar]
- 2.del Zoppo G, Higashida R, et al. PRO ACT: a phase II randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. PRO ACT Investigators. Prolyse in Acute Cerebral Thromboembolism. Stroke. 1998;29:4–11. doi: 10.1161/01.str.29.1.4. [DOI] [PubMed] [Google Scholar]
- 3.Ohman E, Kleiman N, et al. Combined accelerated tissue-plasminogen activator and platelet glycoprotein Ilb/IIIa integrin receptor blockade with Integrilin in acute myocardial infarction. Results of a randomized, placebo-controlled, dose-ranging trial. IMPACT-AMI Investigators (see comments) Circulation. 1997;95:846–854. doi: 10.1161/01.cir.95.4.846. [DOI] [PubMed] [Google Scholar]
- 4.Antman E, Giugliano R, et al. Abciximab facilitates the rate and extent of thrombolysis: results of the thrombolysis in myocardial infarction (TIMI) 14 trial. The TIMI 14 Investigators. Circulation. 1999;99:2720–2732. doi: 10.1161/01.cir.99.21.2720. [DOI] [PubMed] [Google Scholar]
- 5.Wallace R, Furlan A, et al. Basilar artery rethrombosis: successful treatment with platelet glycoprotein IIB/IIIA receptor inhibitor. Am J Neuroradiol. 1997;18:1257–1260. [PMC free article] [PubMed] [Google Scholar]
- 6.EPIC investigators Use of a monoclonal antibody directed against the platelet glycoprotein Ilb/IIIa receptor in high-risk coronary angioplasty. The EPIC Investigation. N Engl J Med. 1994;330:956–961. doi: 10.1056/NEJM199404073301402. [DOI] [PubMed] [Google Scholar]
- 7.Abciximab in acute ischemic stroke. a randomized, double-blind, placebo-controlled, dose-escalation study. The Abciximab in Ischemic Stroke Investigators. Stroke. 2000;31:601–609. doi: 10.1161/01.str.31.3.601. [DOI] [PubMed] [Google Scholar]
- 8.Cheung RT, Ho DS. Fatal hemorrhagic transformation of acute cerebral infarction after the use of abciximab. Stroke. 2000;31:2517–2527. doi: 10.1161/01.str.31.10.2517-a. [DOI] [PubMed] [Google Scholar]
- 9.Bejjani G, Bank W, et al. The efficacy and safety of angioplasty for cerebral vasospasm after subarachnoid hemorrhage. Neurosurgery. 1998;42:979–986. doi: 10.1097/00006123-199805000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Firlik A, Kaufmann A, et al. Effect of transluminal angioplasty on cerebral blood flow in the management of symptomatic vasospasm following aneurysmal subarachnoid hemorrhage. J Neurosurg. 1997;86:830–839. doi: 10.3171/jns.1997.86.5.0830. [DOI] [PubMed] [Google Scholar]
- 11.Polin R, Coenen V, et al. Efficacy of transluminal angioplasty for the management of symptomatic cerebral vasospasm following aneurysmal subarachnoid hemorrhage. J Neurosurg. 2000;92:284–290. doi: 10.3171/jns.2000.92.2.0284. [DOI] [PubMed] [Google Scholar]
- 12.Ueda T, Sakaki S, et al. Angioplasty after intra-arterial thrombolysis for acute occlusion of intracranial arteries. Stroke. 1998;29:2568–2574. doi: 10.1161/01.str.29.12.2568. [DOI] [PubMed] [Google Scholar]