Summary
The vein of Galen aneurysmal malformation (VGAM) is a high flow arteriovenous shunt at the choroidal level In the neonatal period, it typically presents with cardiac failure. Venous stenoses; occlusions and anomalies are often present. In the absence of adequate venous outflow pathways, severe, irreversible cerebral parenchymal damage may occur due to intracranial venous hypertension, altered hydrodynamics and ischaemia. We present a case of deployment of a stent across a focal superior jugular bulb stenosis in an effort to avert this outcome.
Key words: dural sinus malformation, dural AV shunt, single hole fistula, transarterial embolization, infancy
Introduction
Pediatric dural AV shunt is a rare disease, although it is most often referred to in the literature. Morita et al (1995) reported a poor prognosis with overall mortality of 38%.1 Three different types of dural AV shunt have been described, namely, dural sinus malformation with dural AV shunt, infantile type and adult type which differ in their etiology, presentations, and prognosis.2.
Clinical history
The patient was a 15-month-old boy who presented with progressive macrocrania for several months. Besides, the parents found that there was a pulsatile right retroauricular mass. Physical examination showed a well nourished child with mild macrocrania. There was loco-regional dilation of the vessels with bruit at the retroauricular region. The anterior fontanelle was soft. Clinically, there was no tachycardia and there was no sign of heart failure. Developmentally, he had normal milestones.
Doppler examination was performed which disclosed a fistula connecting the retromastoid branch of the right occipital artery and the transverse sinus.
MRI of the brain showed that there was dilated scalp vessel at the right retroauricular region. The right distal sigmoid sinus was absent. There was normal brain parenchyma and no hydrocephalus was found. There was no tonsillar herniation. MRA showed an enlarged right occipital artery. The ipsilateral jugular vein was present.
Clinical Presentation and Management
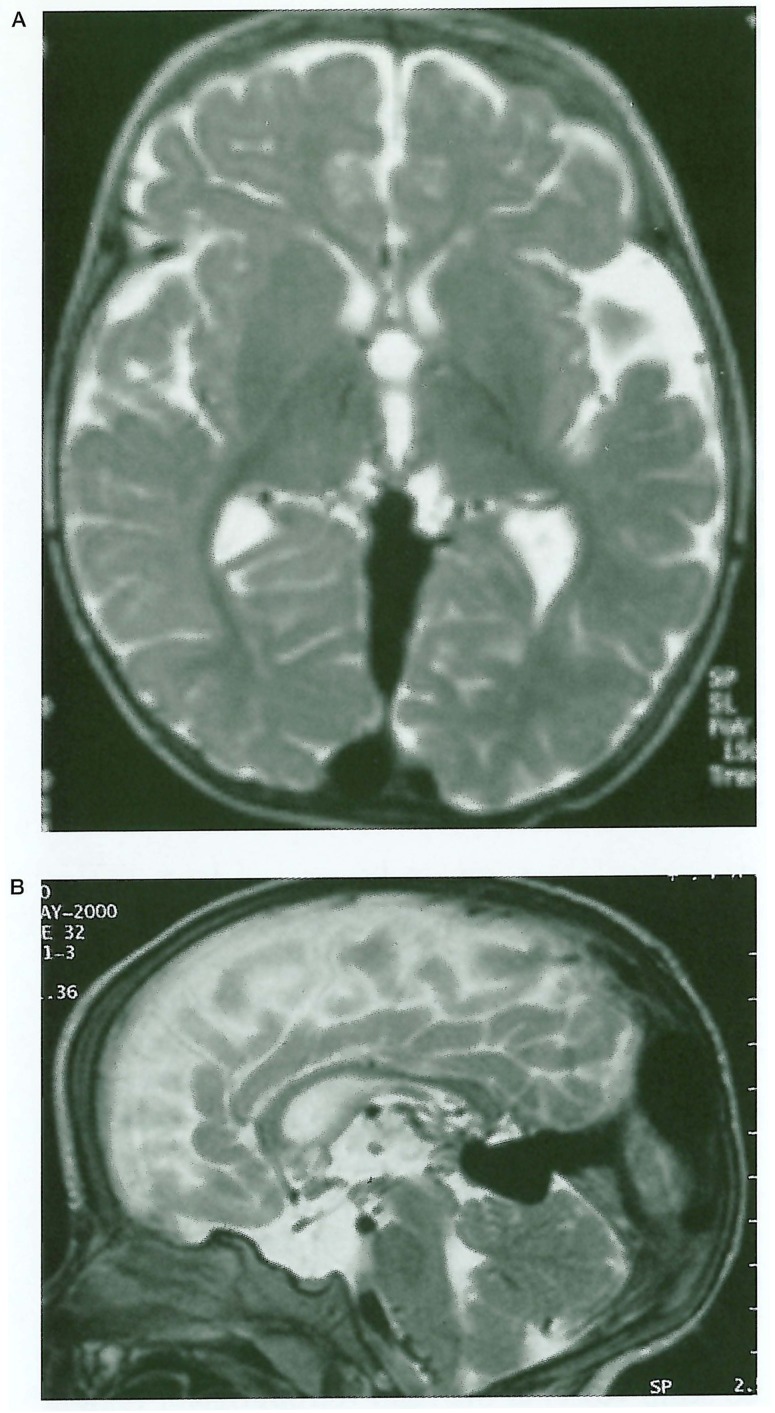
The l5month baby girl was presented to our unit with a history of seizures and macrocephaly. Previous investigations in her country of birth had suggested a vein of Galen aneurysmal malformation (VGAM). This diagnosis was confirmed at angiography. The brain parenchyma appeared normal (figure 1).
Figure 1.
Axial A) and Sagittal B) T2 weighted MRI. Vein of Galen aneurysmal malformation. Persistent falcine sinus. Normal brain parenchyma.
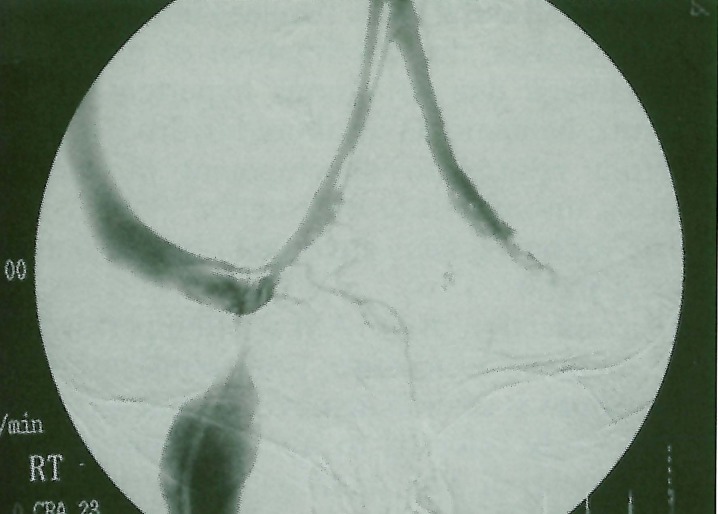
Following partial disconnection of the arteriovenous shunt, the child's neurological status improved, however, on readmission for further treatment it became apparent that restricted venous outflow was a significant problem (figure 2). A CT scan was performed to ensure that the focal stenosis at the level of the superior jugular bulb was not due to bone encroachment and the decision was made to deploy a venous stent across the site of stenosis.
Figure 2.
Digital Subtraction Venogram. Severe right superior jugular bulb stenosis.
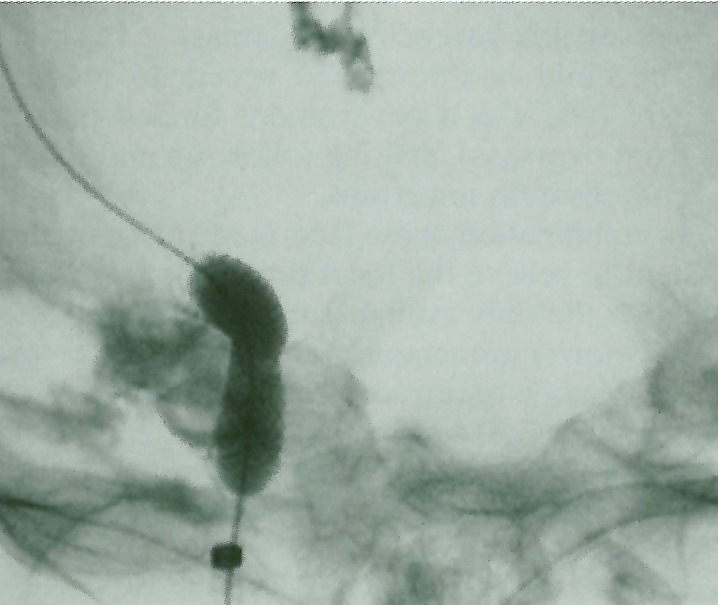
A right femoral venous approach was utilised. The venous pressure was measured proximal and distal to the superior jugular bulb stenosis. Following initial angioplasty, a stent was placed across the stenosis and post deployment angioplasty (figure 3-4) was performed to maximise the diameter of the stent. Venous pressure measurements were repeated. The baby was anticoagulated, initially with heparin and subsequently with warfarin, for a period of three months.
Figure 3.
Angioplasty balloon within almost fully deployed stent. Glue from previous embolisation.
Figure 4.
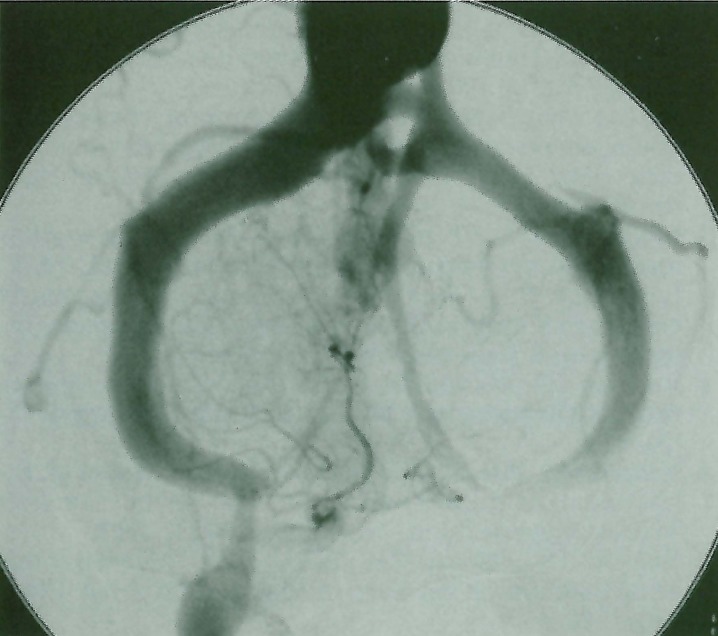
Deployed stent with some residual stenosis. Less filling of collateral pathways.
Results
The initial venous pressure measurements were 40 cm of water above and 15 cm of water below the stenosis, a gradient of 25 cm of water. The stent deployed with a residual stenosis. Post deployment angioplasty produced some improvement in the configuration of the stent though some residual stenosis persisted (figure 5). Repeat pressure measurements were 25 cm of water above and 15 cm of water below the stenosis, a gradient of 10 cm of water. There were no evident complications. The patient's clinical status improved; the rate of head growth normalised, she is currently seizure-free, neurologically and developmentally normal.
Discussion
VGAM is characterised by arteriovenous shunts at the choroidal level, within the subarachnoid space, in the region of the vein of Galen. There is associated aneurysmal dilatation and abnormal persistence of the median vein of the prosencephalon, an embryological midline venous structure and precursor of the vein of Galen. The normal vein of Galen is not present. The dilated persistent median vein of the prosencephalon does not drain normal brain parenchyma; the brain drains by alternative pathways. The malformation often drains into a persistent falcine sinus and there may be agenesis of the straight sinus and anomalies of other dural venous sinuses3,10,11,12.
VGAM and dural sinus malformations are the only intracranial arteriovenous malformations demonstrated to have been present in the foetal period4. They are more common in males. Most present in either the neonatal period or in infancy. Almost all cerebral arteriovenous shunts detected antenatally or in the neonatal period are VGAM. In general, the high flow arteriovenous shunt of VGAM is initially well tolerated from a neurological point of view and the presentation is with cardiac failure or altered CSF dynamics and macrocephaly3,5,7,10,12.
If possible, treatment of the shunt in VGAM is deferred to allow for growth of the child, as intervention in neonates is technically difficult and hazardous5,10,12. Criteria for intervention in infancy include macrocephaly, developmental delay, seizures and reversible neurological deficit. Cardiac failure unresponsive to medical management is an indication for urgent embolisation in the neonatal period3,10,12.
Macrocephaly is seldom, if ever, due to obstructive hydrocephalus. Ventricular drainage may result in worsening of the patient's condition5,12. Macrocephaly has been postulated to reflect altered cerebrospinal fluid (CSF) resorption. In neonates CSF resorption occurs by cerebral venous pathways prior to development of mature arachnoid granulations in the dural venous sinuses. Embolisation of the VAGM often results in resolution of the dilatation of the ventricles and macrocephaly3,10,12.
In this patient, a combination of unfavourable venous anatomy (paucity of alternative venous pathways) and superior jugular bulb stenosis lead to venous hypertension, macrocephaly and neurological dysfunction. These features could be expected to progress in the event of worsening venous outflow restriction and would result in irrevocable brain damage unless treated.
In the study by Yamada et al6, in an animal model utilising surgically created high flow arteriovenous shunts to the superior sagittal sinus, venous pressure did not rise significantly in the absence of outflow obstruction. On the other hand, even in the absence of an arteriovenous shunt, occlusion of a dural venous sinus produced a significant increase in superior sagittal sinus pressure. These authors concluded that venous outflow obstruction was necessary for cerebral venous hypertension to occur both in the presence and absence of an arteriovenous shunt6. We have had previous experience of a patient with a VAGM that was successfully treated with complete embolisation of the arteriovenous shunts but nonetheless died one year later following total occlusion of the superior jugular bulbs in the absence of alternative venous pathways.
These data concur with the clinical experience in VGAM and other conditions in which there is arteriovenous shunting (pial arteriovenous malformations or fistulae, dural sinus malformations, childhood dural arteriovenous fistu-lae and adult dural sinus fistulae) into the dural venous sinuses; the development of parenchymal damage due to venous hypertension, ischaemia, haematoma or altered hydrodynamics is often related to development of venous stenosis, thrombosis or obstruction1,2,3,8,10,11,12.
The following facts governed our decision to place a stent:
-
1
Disconnection of VGAM is often performed as a staged procedure; total obliteration of the shunt is seldom achieved in one sitting.
-
2
The study referred to above6 suggests that treatment of the underlying arteriovenous communication may not relieve venous hypertension in the presence of established outflow obstruction.
-
3
Persistent venous hypertension may lead to irreversible parenchymal damage.
-
4
The child had restricted access to medical care (she was a government funded patient from overseas), making follow-up and repeat embolisation uncertain.
In combination, these facts made placement of a stent to relieve the focal superior jugular bulb stenosis the only available mechanism to immediately lower intracranial venous pressure before brain damage occurred. The overall prognosis of untreated VGAM may depend on patency of the superior jugular bulbs12. The successful reduction of the pressure gradient and improvement in the patient's clinical status suggest that the haemodynamic effect of the superior jugular bulb stenosis was reversed by stent placement. We hope that damage to the brain has been averted.
The pathogenesis of venous stenosis and occlusion in VGAM and other intracranial arteriovenous shunts is uncertain. While macrocephaly and altered skull base growth and maturation may contribute to venous outflow restriction12,13, in this case, there was no evidence of this on bone algorithm CT. Nor was there evidence of venous sinus thrombosis. It is worth noting that venous stenoses are common in the high flow fistulae created for renal dialysis patients. High flow vasculopathy may underlie the venous stenoses of VGAM and other intracranial high flow shunts. Angioplasty and stenting have both been utilised in the setting of venous stenoses in peripheral arteriovenous shunts, with variable success, but some promising results including long-term patency rates up to 75%9.
Conclusion
The long-term efficacy of this procedure is unknown. Even if the superior jugular bulb venous stent only remains patent for a short time, it may have averted damage to the brain parenchyma and allowed time for further intervention to be considered.
References
- 1.Davies MA, Saleh J, et al. The Natural History and Management of Intracranial Dural Arteriovenous Fistulae. Interventional Neuroradiology. 1997;3(nº 4 (Part 1: Benign Lesions)) doi: 10.1177/159101999700300404. [DOI] [PubMed] [Google Scholar]
- 2.Davies MA, Saleh J, et al. The Natural History and Management of Intracranial Dural Arteriovenous Fistulae. Interventional Neuroradiology. 1997;3(nº 4 (Part 2: Aggressive Lesions)) doi: 10.1177/159101999700300405. [DOI] [PubMed] [Google Scholar]
- 3.Lasjaunias P, Hui F, et al. Cerebral Arteriovenous Malformations in Children. Child’s Nervous Syst. 1995;11 doi: 10.1007/BF00303807. [DOI] [PubMed] [Google Scholar]
- 4.Lasjaunias P. A Revised Concept of the Congenital Nature of Cerebral Arteriovenous Malformations. Interventional Neuroradiology. 1997;3(nº 4) doi: 10.1177/159101999700300401. [DOI] [PubMed] [Google Scholar]
- 5.Johnson IH, Whittle IR, et al. Vein of Galen Malformation: Diagnosis and Management. Neurosurgery. 1987;20(5) doi: 10.1227/00006123-198705000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Yamada M, Miyasaka Y, et al. A Canine Model of Intracranial Arteriovenous Shunt with Acute Cerebral Venous Hypertension. Neurol Res. 1998;20(1) doi: 10.1080/01616412.1998.11740487. [DOI] [PubMed] [Google Scholar]
- 7.Watson DG, Smith RR, Brann AW. Arteriovenous Malformation of the Vein of Galen. Am J Dis Child. 1976;130 doi: 10.1001/archpedi.1976.02120060066013. [DOI] [PubMed] [Google Scholar]
- 8.Massoud TF, Hademenos GJ. Risk of intracranial arteriovenous malformation rupture due to venous drainage impairment. A theoretical analysis. Stroke. 1996;27(6) doi: 10.1161/01.str.27.6.1072. [DOI] [PubMed] [Google Scholar]
- 9.Nazarian GK, Bjarnason H, et al. Iliofemoral venous stenoses: effectiveness of treatment with metallic endovascular stents. Radiology. 1996;200(1) doi: 10.1148/radiology.200.1.8657909. [DOI] [PubMed] [Google Scholar]
- 10.Garcia-Monaco R, Lasjaunias P, Berenstein A. Therapeutic Management of Vein of Galen Aneurysmal Malformations. In: Vinuela , et al., editors. Interventional Neuroradiology: Endovascular Therapy of the Central Nervous System. Raven; 1992. [Google Scholar]
- 11.Lylyk P, March AD, et al. Alternative Therapeutic Approaches in Intravascular Embolisation of Vein of Galen Vascular Malformations. In: Vinuela , et al., editors. In Interventional Neuroradiology: Endovascular Therapy of the Central Nervous System. Raven; 1992. [Google Scholar]
- 12.Lasjaunias P. Vascular Diseases in Neonates, Infants and Children. Springer-Verlag; 1997. [Google Scholar]
- 13.Taylor WJ, Hayward RD, et al. Enigma of raised intracranial pressure in patients with complex craniosynostosis: the role of abnormal intracranial venous drainage. J Neurosurg. 2001;94(3) doi: 10.3171/jns.2001.94.3.0377. [DOI] [PubMed] [Google Scholar]