Abstract
Infants born late preterm (34–36 weeks of gestation) account for 350,000 US births per year, are at risk for developmental delays, and are rarely included in intervention studies.
Purpose
To describe a novel parent delivered movement intervention program for very young infants and outcomes following intervention and to evaluate the feasibility of using a comprehensive set of outcome measures.
Summary of Key Points
Two infants born late preterm received intervention from 0.5 to 2.0 months of adjusted age. Development, postural control, reaching, and object exploration assessments were completed at 3 time points. The intervention was well tolerated by the family. Improvements in developmental outcomes, postural control, and object exploration are presented.
Statement of Conclusion
Very early movement experience provided daily by parents may improve development. In combination, norm-referenced and behavioral measures appear sensitive to changes in infant behaviors.
Keywords: arm/physiology, biomechanics, developmental disabilities, early intervention, family caregivers, female, male, motor skills, physical therapy/methods, postural balance, preterm infants, weight-bearing/physiology
INTRODUCTION
Infants born late preterm (34 – 36 weeks gestation) account for more than 70 percent of preterm births or 350,000 infants per year in the United States.1 Historically, these infants have received little attention as they were not typically admitted to the neonatal intensive care unit (NICU) and have been considered to be at low risk for developmental delays.2 However, recent research suggests that infants BLP are at higher risk of developmental delays and poor school performance compared to infants born full term.3–5 For example, over 30% of children in preschool or kindergarten who were born late preterm have delayed academic performance.4 Infants BLP are 3 times more likely to have cerebral palsy, 1.5 times more likely to have intellectual disabilities and are diagnosed with developmental coordination disorder more than infants born full term.5,6
Although infants born very preterm (BVP), at less than 30 weeks of gestation, frequently receive early intervention services under the Individuals with Disabilities Act (IDEA), infants BLP often do not qualify for these services early in life, delaying potentially beneficial intervention.7–9 For example, infants BVP in Virginia automatically qualify for early intervention, which may include developmental monitoring, parent education, and/or therapy services.9 Infants who do not meet automatic eligibility criteria, including infants BLP, must demonstrate a 25% developmental delay. This level of delay is difficult to document without the use of special assessment tools designed for very young infants, which are not generally used for early intervention eligibility determination.10 Infants BLP who required neonatal intensive care, however, require early intervention at a rate similar to infants BVP by 12 months of age.11 Delayed early intervention means the infants BLP miss a year of intervention during a period of high brain plasticity and when parent education can shape positive parent-infant interaction. Given the prevalence of late preterm birth and the risk of developmental disabilities in this population, developmental monitoring, parent education, and/or direct intervention may be warranted.
Early Movement Experience
The way infants move and interact with objects during early development shapes their understanding of the world. Exploration generates cognition-perception-action cycles, which infants use to expand their movement repertoire, generate learning opportunities, and advance general development.12,13 For example, the ability to maintain a sitting position while reaching and grasping a toy facilitates an infant’s learning about spatial relationships, properties of objects, and effect of interacting with the object.14,15 Infants with delayed motor development, reduced postural control, or atypical movement patterns may not generate the level of daily exploration needed to drive their cognitive, perceptual, and motor development.
In this case series, we provided at-risk infants BLP with an intervention grounded in ‘action perception theory’.16 The purpose of this intervention was to provide each infant experiences to encourage postural control, self-directed movement, and a varied movement repertoire starting at 0.5 months of adjusted age, well before developmental interventions are typically provided to infants BLP who are not admitted to the NICU. Providing very young infants with experiences that are slightly advanced for their age can improve head control, reaching, object exploration, and stepping.12,17–21 For example, infants born full term whose parents provided them with advanced movement experiences for 20 minutes per day for 3 weeks had an accelerated onset of reaching and grasping in the short term as well as advanced problem solving after the intervention ended.17 Separate studies involving similar postural and movement programs started at 1 to 2 months of age advanced a range of behaviors from head control to crawling and walking.19,22 Similar programs have been effective for infants born at less than 33 weeks of gestation to advance reaching and object exploration.21,23 While evidence supports the potential for early experiences to advance motor development in both infant born full term and preterm, there is little evidence on the effectiveness of these programs in infants BLP. This case series starts to address this gap by describing a parent delivered movement program used with 2 infants BLP in the first months of life. As in previous work, the use of a parent delivered intervention maximizes the frequency of intervention, limits the cost to provide the activities, and may enhance translation into early intervention practice.
Measurement Challenges in Early Infancy
The assessment of emerging motor behaviors in the first months of life is equally important and challenging.10 Standardized, norm-referenced assessment tools such as the Test of Infant Motor Performance (TIMP)24 and Bayley Scales of Infant and Toddler Development (Bayley)25 provide general information on the development of the motor system and allow for comparison with a normative sample. However, standardized measures lack detailed information on specific functional behaviors in infancy such as the duration and/or frequency of keeping the head in midline, bringing the hands to the mouth, reaching, manipulating objects, and mouthing objects.10 Therefore, additional measurement tools are needed to describe the development of early functional motor behaviors. Measures of motor behavior including the frequency or duration of head in midline, toy contact, bimanual grasp, hand to mouth, and toy to mouth are sensitive to change and can be used to describe the emergence of behaviors, interactions with the environment, and the effects of intervention.12,17,26,27 Research is needed to evaluate the feasibility of using a combination of standardized, norm-reference developmental measures and measures of functional motor behaviors to evaluate responses to intervention in the first months of life. This case series uses norm referenced and skill specific behavioral measures to describe changes in general developmental and specific functional motor behaviors during the first months of life.
Purpose
The purpose of this case series is to: 1. Describe the use of a parent delivered movement program for infants BLP starting in the first months of life 2. Describe the developmental and motor behavior outcomes following participation in the movement program for the 2 infants in this case series and 3. Determine the feasibility of using a comprehensive set of outcome measures for young infants in future studies.
Description of the Case Series Participants
A set of twins BLP participated in the movement program and are the focus of this case series. The infants were born at 35 weeks and 2 days of gestation, were Caucasian, had 2 older siblings, and both parents had a college education. The female twin (Infant A) was born at 5.02 pounds, was hospitalized for 4 days in the well baby nursery, and had hip dysplasia requiring use of a Pavlik harness until 3 months of age. The male twin (Infant B) was born at 6.02 pounds, was hospitalized for 7 days in the well baby nursery, and had mild reflux requiring medical management in the newborn period according to his parents. All ages throughout the manuscript are adjusted for prematurity (age from the expected date of full term delivery).
Assessment Protocol
A comprehensive battery of assessments was completed to quantify motor development, postural control, reaching, and object exploration using a combination of norm-referenced standardized assessments and sensitive measures of behaviors in the first 6 months of life. Assessment visits were completed at 0.5 months (baseline), 2 months (immediately post intervention), and 4 and 6 months of age (2 and 4 months after termination of intervention) (Table). The mother was encouraged to feed, change diapers, or console as needed so that each infant was in a positive or neutral behavioral state during the assessments. One additional developmental follow-up assessment was completed at 12 months of age. All assessments were videotaped for behavioral coding and scoring.
Table.
Assessment schedule
| 0.5 mo (Baseline) |
2 mo (immediately post intervention) |
4 mo | 6 mo | 12mo | |
|---|---|---|---|---|---|
| Developmental Assessment | TIMP | TIMP | TIMP | Bayley | |
| Supine Postural Control and Head in midline | X | X | X | ||
| Seated Reaching, Object exploration, Looking | X | X | X | X | |
| Supine Reaching and Head control | X | X | X | X |
Developmental Assessments
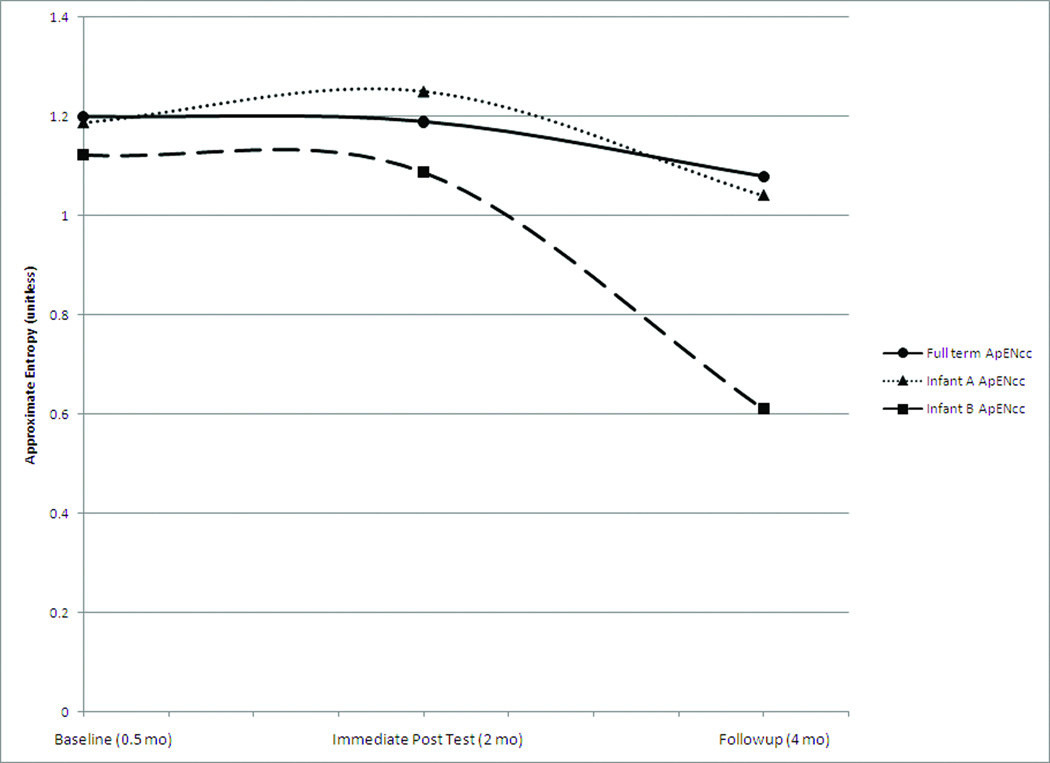
Developmental assessments were included as a general measure of infant development over time and for a comparison with normative data. The Test of Infant Motor Performance (TIMP) was completed at baseline (0.5 mo), immediately post-intervention (2 mo), and at 4 months of age. The TIMP is a reliable and valid norm-references assessment of movement and posture for infants from 34 weeks of gestation to 4 months of age adjusted for prematurity.24,28–30 The TIMP z-scores [TIMP z-score = (TIMP Raw Score - Mean for age group)/SD of the age group] were used to compare infants’ development with the TIMP’s normative data and to evaluate change over time in response to intervention. No developmental assessment was completed at 6 months of age. The Motor Scales of the Bayley Scales of Infant and Toddler Development (Bayley) was completed at 12 months of age.25 The Bayley is a reliable, valid, and norm-referenced standardized assessment of gross and fine motor, cognitive, receptive and expressive language abilities for infants and toddlers.10,25 Scaled scores for the gross and fine motor subtests are presented as a comparison with the Bayley’s normative sample. Both the TIMP and Bayley were scored from videotaped assessment by reliable examiners who were blinded to the infant’s gestational age at birth and to their intervention status.
Postural Control
The magnitude and complexity of center of pressure (COP) displacement at the base of support are measures of postural control that change during the emergence of motor behaviors, differ between infants with and without motor impairments, and change in response to intervention.31–34 Postural sway was assessed while the infant was positioned in supine without a visual stimulus for 5 minutes using a Conformat (Tekscan, South Boston, MA) pressure sensitive mat sampling at 5 Hz.34 Behavioral data were used to identify continuous COP time series of 500 data samples or 100 seconds in length in which the infant was in supine, alert, and no one was touching the infant. As described in detail in our previous work, the magnitude of the variability and complexity of postural control were quantified using the root mean squared (RMS) displacement and approximate entropy (ApEN) in the caudal cephalic (cc) and medial lateral (ml) directions (RMScc, RMSml, ApENcc, and ApENml).34–36 Magnitude of the variability in postural control (RMS) is a reflection of the standard deviation around a central mean value or the amount of variability without regard for the pattern of the variability. Our previous research suggests that the magnitude of the variability in postural control does not change systematically during development of early motor behaviors.33,36 Complexity in the variability of COP movement (ApEN) represents the repeatability of the postural control strategy or the pattern of variability within a time series. Repetitive COP movement or the use of a limited number of postural control patterns is signified by low complexity or ApEN values. Readers who are not familiar with these measures are encouraged to review Dusing and Harbourne35 for an expanded explanation of these terms and clinical examples. In typically developing infants postural control complexity is higher during the initial development of a skill when the infant is utilizing multiple postural control strategies through trial and error. Postural control complexity decreases as an infant learns to consistently perform a skill using the most efficient postural control strategies for that infant.35,36 Infants with CP and those born preterm have reduced postural control complexity during development.34,37 We used these measures of postural control complexity to evaluate changes in postural control following intervention. As described below, we also assessed infants’ ability to maintain the head in midline in supine as an additional measure of postural control.19
Reaching and Object Exploration
Reaching was assessed in supine and sitting at each visit. In supine, infants participated in 5 trials of 60 seconds in length with a toy presented at 80% of arm’s length. The toy was presented directly over the torso at the nipple line. All toys used in the reaching tasks were commercially available small infant rattles. For all sitting tasks, the infant was positioned in an infant high chair with the side removed and a soft strap to stabilize the trunk while allowing for free arm movements. During seated reaching the infant participated in 6 trials of 30 seconds with a toy presented at 80% of arm’s length. In the sitting object exploration condition, infants participated in 6 trials holding onto an object which was placed in the infant’s left or right hand in random order for a maximum of 30 seconds. A total of 3 objects were presented once to each hand. The objects were all commercial available infant toys such as a ring, infant keys, and a soft rattle. If the infant dropped the object it was replaced up to 3 times within the 30 second trial.
Video recordings of the supine COP, supine and seated reaching, and seated object exploration assessments were used to code behaviors including looking, head in midline, toy contact, and toy to mouth. Behavioral coding was completed using the MacShapa v1.1.2a (Department of Mechanical and Industrial Engineering, University of Illinois at Urbana-Champaign, Urbana, IL) coding program and trained coders maintained greater than 85 percent agreement for each variable coded with the formula: Agree/(Agree+Disagree)*100.38 Three pairs of coders were responsible for coding the data included in this case series as well as data from other studies being completed in the same research labs using the same variables. Coding pairs were trained to code specific variables and 20% of the visits were coded twice to ensure a high level of reliability on each variable and between the 2 coders in the pair. The percent of the assessment duration that the infant’s head was in midline was calculated during the supine assessments of COP (No Toy) and during the supine reaching assessment (Toy). Head in midline was coded any time the trained coder observed the infant’s head was within 30 degrees of midline. Reaching was quantified by the percent of time during the reaching assessment each hand was in contact with a toy for each position separately. The sum of the percent of time each hand was in contact with the toy was calculated. Mouthing object exploration in sitting was calculated as the percent of the time holding the object when the object was touching the infant’s lips or mouth. Looking was calculated as the percent of the time the object was presented during the seated reaching trials in which the infant was looking at the object.
Description of Intervention
The movement program used in this case series was designed to encourage parents to provide additional experiences to enhance postural and motor control at an age when most infants BLP receive no intervention. Based on our previous research with infants born full term and preterm as well as action-perception theory, we hypothesized that additional postural control and movement experience would advance motor development, postural control, reaching, and object exploration.17,19,21
The movement program encouraged parents to interact with their infant for a minimum of 20 minutes per day from 0.5 months to 2.0 months of age to “strengthen baby’s neck, shoulders, stomach, legs, and arms using a variety of different activities”. Following the baseline assessment, the mother of the twin infants BLP was provided with an activity booklet, which provided a verbal and pictorial description of activities, including suggested progressions of each activity. The 7 activities included prone play, sitting with upper trunk support, head control practice, midline hand to hand and hand to foot play, assisted kicking, and visualizing / tracking toys (Figure 1). The activities were reviewed with the mother and demonstrated. She was encouraged to support the infant’s attempts with these activities and to provide the least assistance possible to complete the activities. The activity booklet provided a suggestion for the amount of time to spend on each activity ranging from 2 to 4 minutes for a total of 20 minutes per day which could be completed in a single 20 minute session or multiple shorter sessions. The mother completed a daily log documenting how much time she spent on each activity with each infant per day. The twin infants BLP completed at least 20 minutes of the activities on 90 and 80 percent of days during the 1.5 months of the intervention, respectively. The intervention each infant received differed slightly. Infant A did not receive experience in kicking and hand to feet activities because of the Pavlik harness. Infant B completed all 7 items of the movement program for a total of 20 minutes. To make up for these activities, Infant A spent more time on the other 5 items to complete 20 minutes of activity. Although the intervention each infant received differed because of the use of the Pavlik harness worn by Infant A, both infants received additional experiences controlling posture in a variety of positions, practicing self directed movements, and observing toys. These differences in intervention may have influenced each infant’s outcomes. Therefore, each infant’s outcomes are described separately and in detail in this case series.
Figure 1.
Examples of activities in the movement program completed daily by parents.
Description of Outcomes
Developmental Assessments
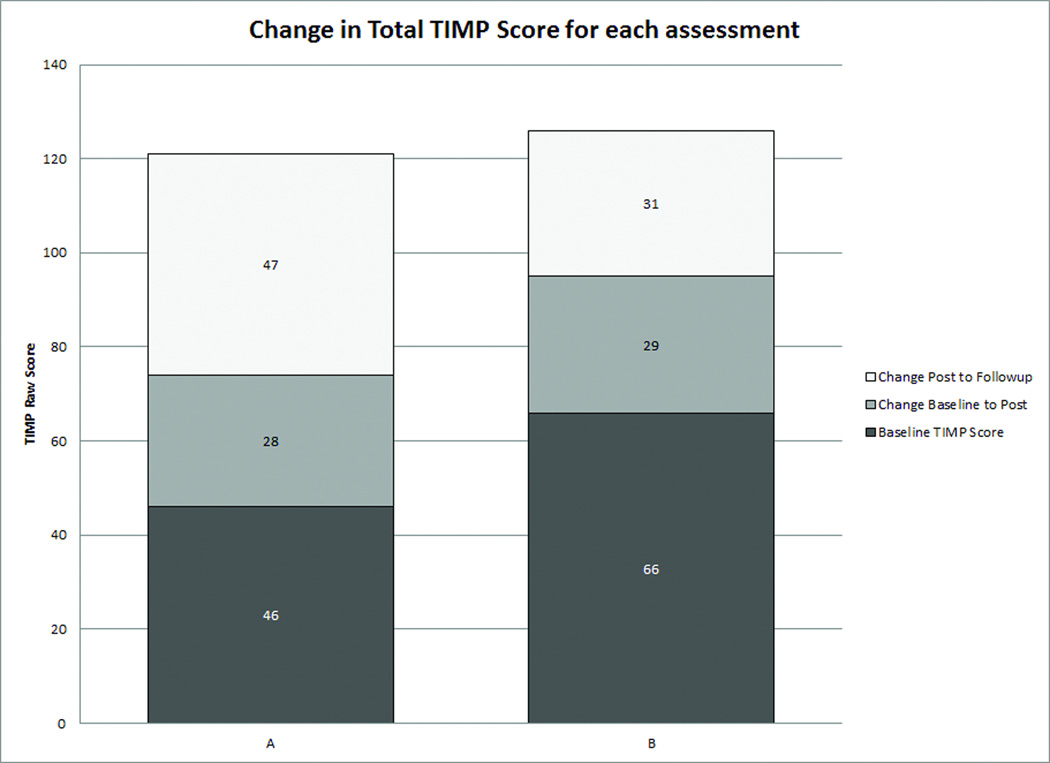
The outcomes of the norm-referenced standardized tests are presented using z-scores or standard scores as a comparison with the normative sample for each assessment. Both of the infants in this case series improved their raw score on the TIMP at each study visit (Figure 2A). Both infants demonstrated an improvement in TIMP z-scores, meaning they were less delayed or closer to the average range at the post intervention visit (Figure 2B). Infant A’s score on the TIMP was more than 1 standard deviation below the mean at the baseline visit, indicating she had delayed movement and postural control compared to the normative sample on the TIMP.29 Her TIMP z-score improved slightly at the immediate post intervention visit and she made a very large improvement, into the average range, between the immediately post intervention visit at 2 months and the follow-up at 4 months of age. Infant B’s TIMP z-score was in the average range at all assessments, but improved over time.
Figure 2.
Test of Infant Motor Performance Scores (TIMP) for each infant. 2A) Baseline TIMP Raw Score and Change in Raw TIMP score at each study visit. 2B) TIMP Z-score at each study visit. A z-score of 0 is equivalent to the mean for the infant’s age. Values above and below 0 are presented in standard deviations from the mean. TIMP scores of −0.5 (dashed line) or below are considered below average.24
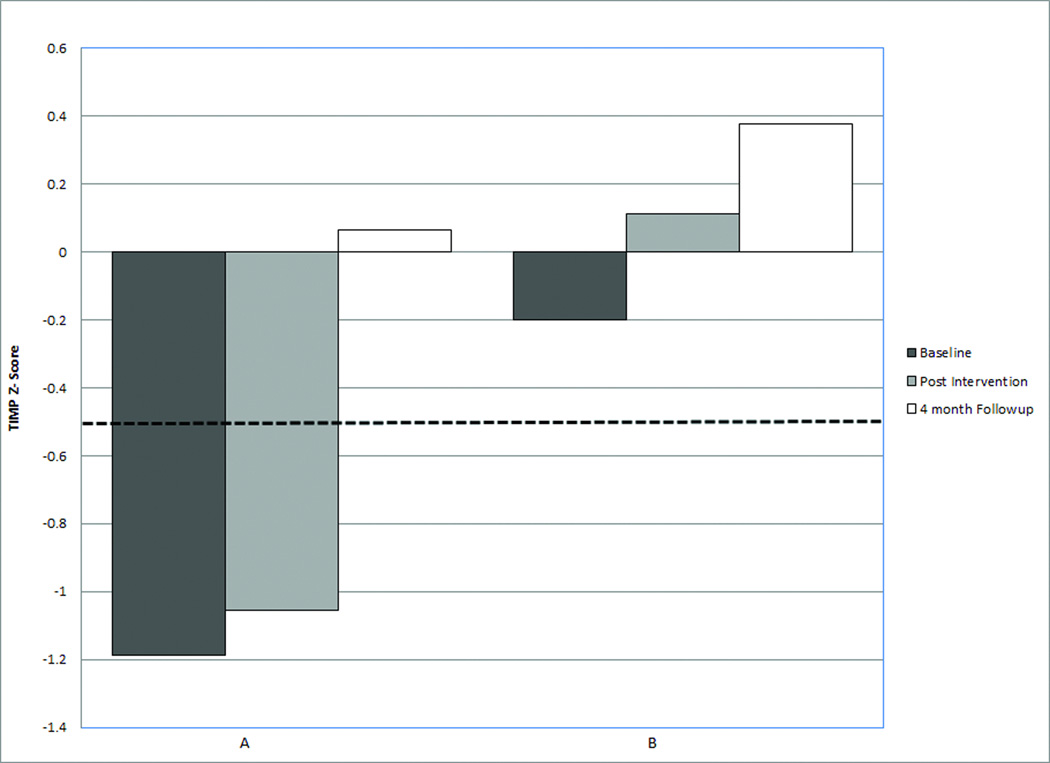
Developmental follow-up assessments with the Bayley25 at 12 months of adjusted age demonstrated that infant A had gross and fine motor skills in the average range. Infant B had average fine motor skills, but his gross motor skills were between 1 and 2 standard deviation below the mean, suggesting a mild gross motor delay (Figure 3).
Figure 3.
Gross and Fine Motor Scaled Scores on the Bayley Scales of Infant and Toddler Development, 3rd Edition at 12 months of adjusted age. Scaled scores have a mean of 10 and a standard deviation of 3. The dashed line represents 1 standard deviation below the mean.
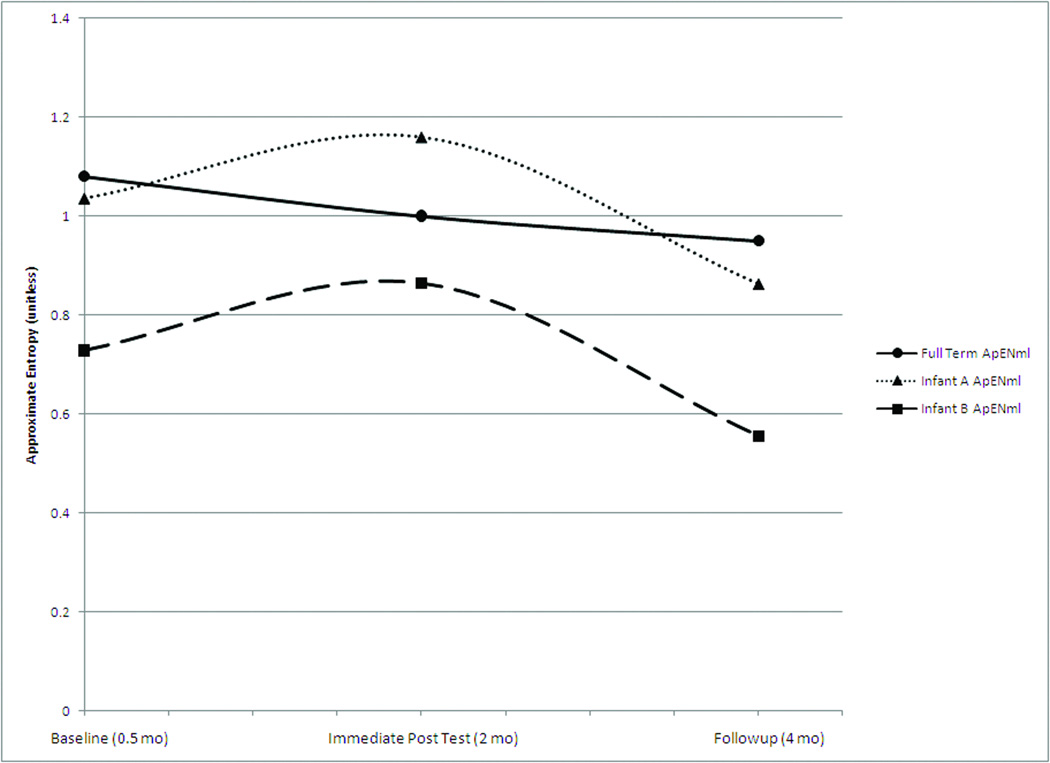
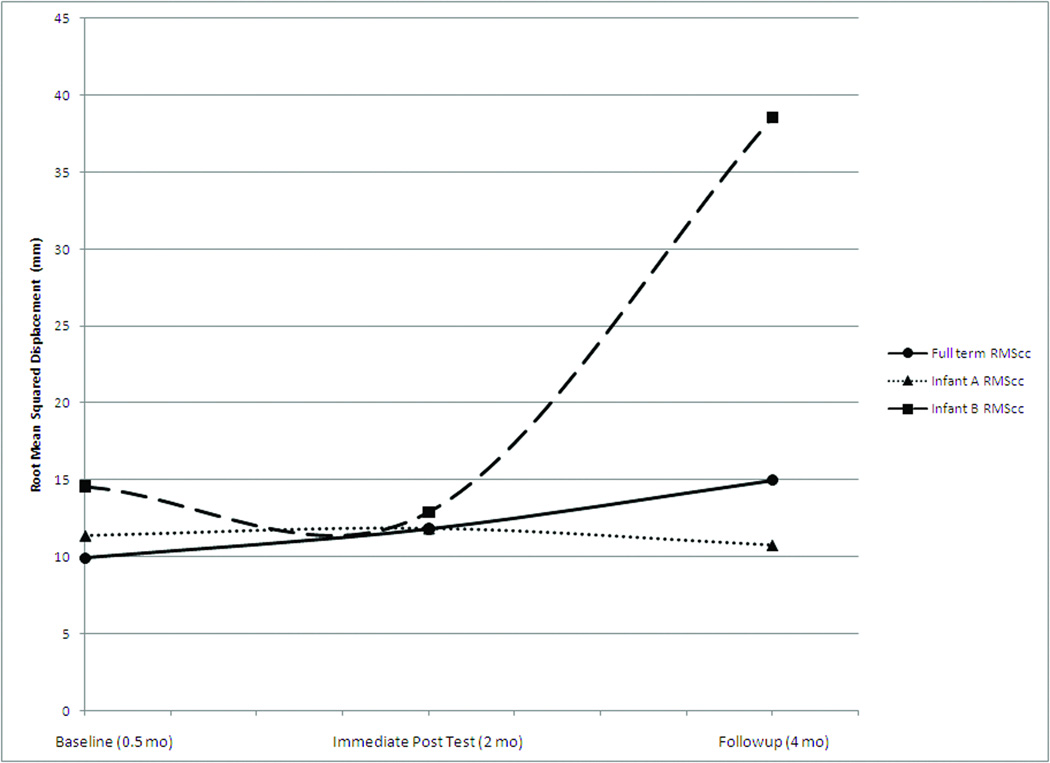
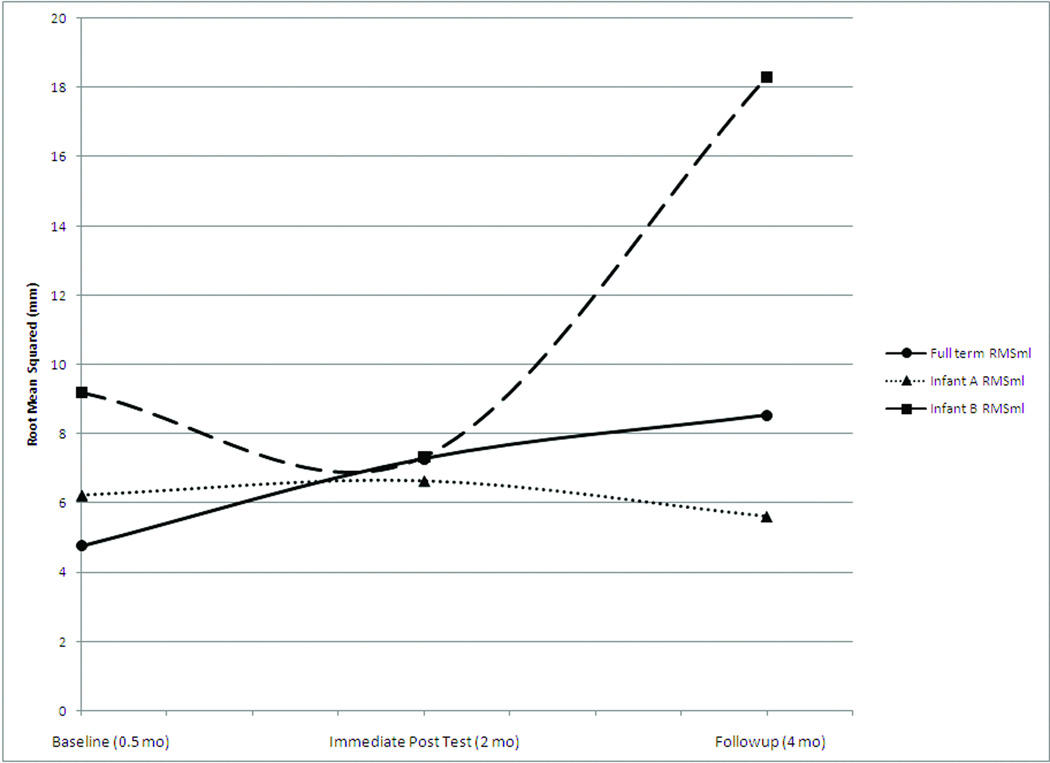
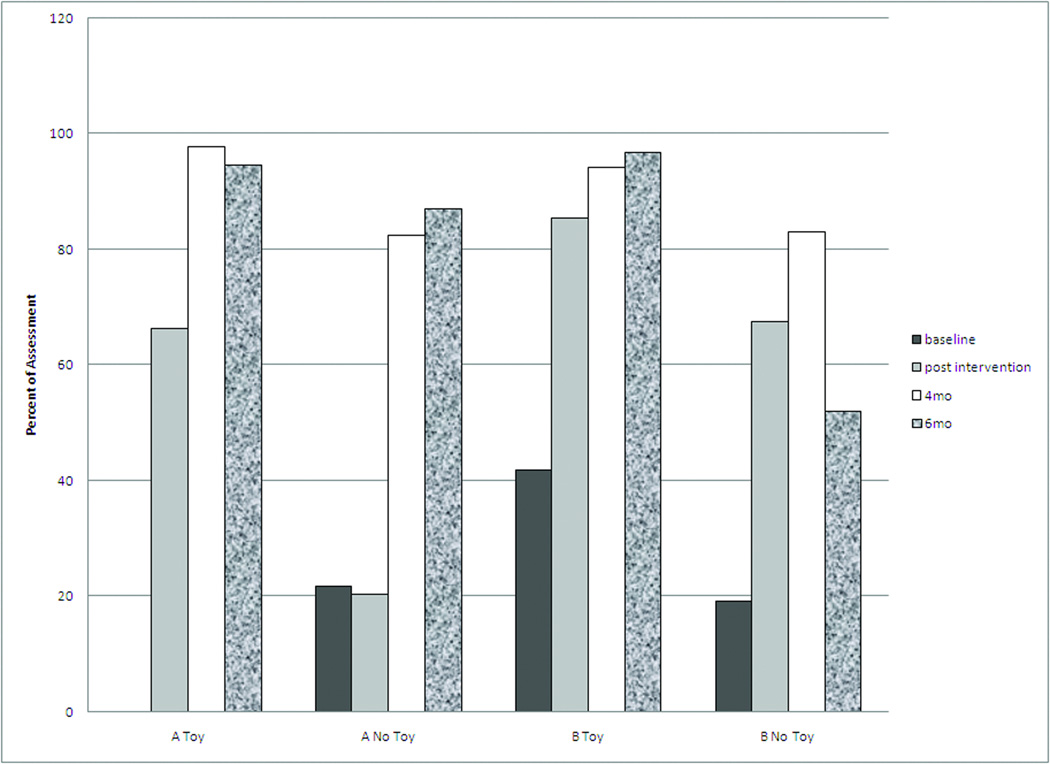
Postural Control
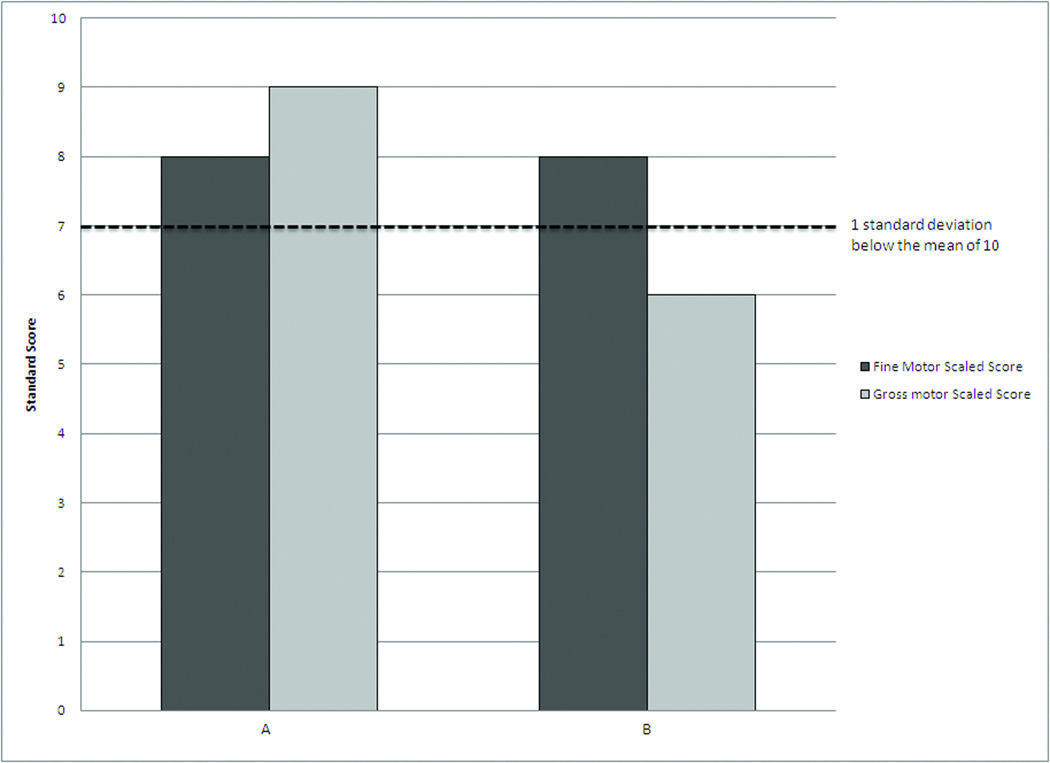
The development of postural control in the infants BLP in this case series differed from each other with Infant A being similar to infants born full term, based on data derived from previous research on infants born full term using the same COP protocol (Figure 4 A-C).36 Infant A demonstrated baseline complexity values and a trajectory similar to the data of infants born full-term. Infant B had a similar developmental trajectory, with a more repetitive or less complex postural control at all time points. During the intervention his postural control complexity remained stable, however, the decrease in complexity following the end of the intervention was quite large compared to infant A and the full term comparison data.36 Midline head control in supine improved for both infants BLP over time with each maintaining his/her head in midline most of the time by 4 months of age. By 2 months of age each infant maintained his/her head in midline while in a supine position, for a longer duration when a toy was presented than without a visual stimulus (Figure 5).
Figure 4.
Changes in the magnitude and complexity of center of pressure (COP) variability in the case infants compared to infants born full term. The average data from 22 infants born full term, previously published, is included for reference.36 4A: Complexity of COP variability in the caudal cephalic direction. 4B: Complexity of COP variability in the medial lateral direction. 4C: Magnitude of the COP variability in the caudal cephalic direction. 4D: Magnitude of the COP variability in the medial lateral direction.
Figure 5.
Development of midline head control in supine, during and after the movement program.
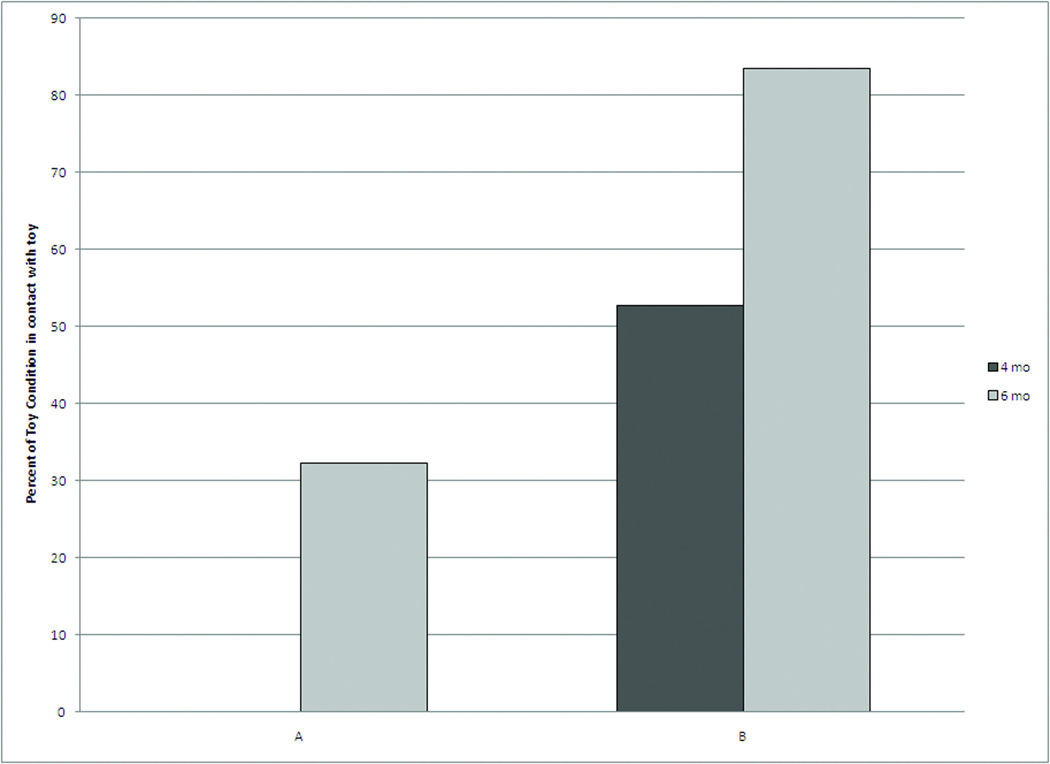
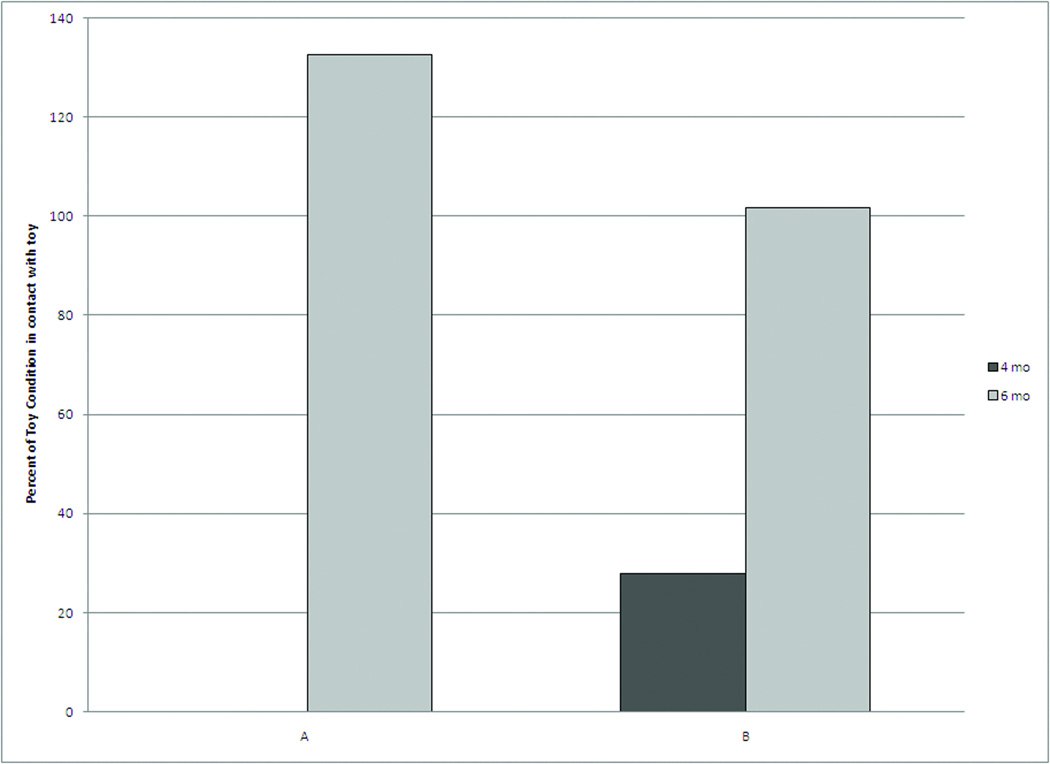
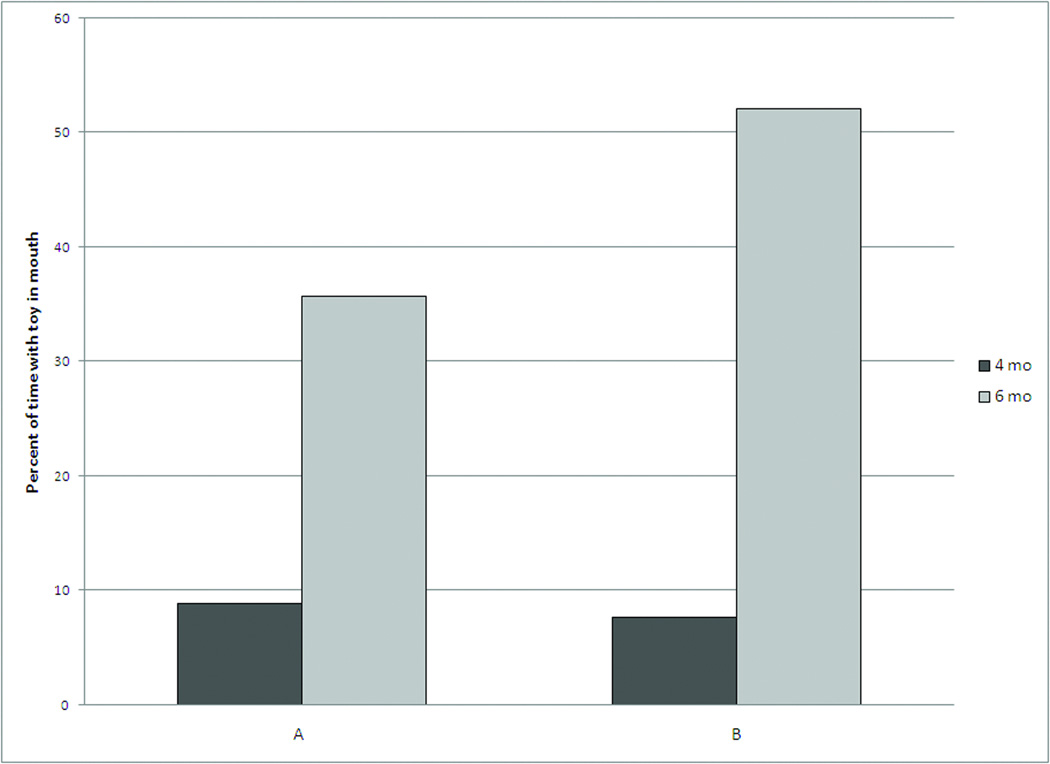
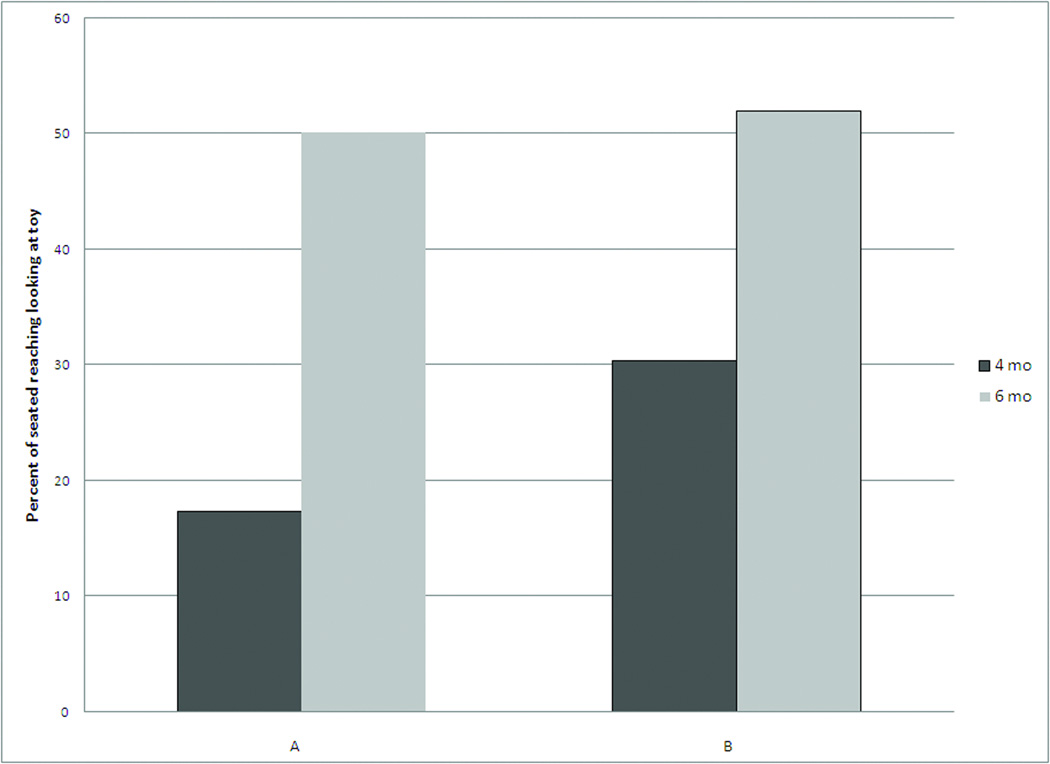
Reaching and Object Exploration
The Infants BLP both demonstrated improving reaching and object exploration which may have been affected by the movement program. The infants did not demonstrate reaching in either sitting or supine or object exploration in sitting on a regular basis before 4 months of age. Both infants made contact with the toy by 6 months of age from both supine and sitting (Figure 6A and 6B). Both Infants BLP were in contact with the toy for a greater percentage of the assessment period when in sitting, compared to supine. Infant B contacted the toy more in supine than Infant A at 4 and 6 months of age (Figure 6A). By 6 months of age both infants BLP had a hand in contact with the toy during most of the sitting assessment (Figure 6B). Both infants BLP started to explore objects while sitting in a chair with trunk support by bringing the toy to his or her mouth at 4 months with an increase in this behavior by 6 months of age (Figures 6C). Both infants increased the percent of the time they looked at a toy suspended in front of them while sitting in a chair from 4 to 6 months of age (Figures 6D).
Figure 6.
Reaching in supine and sitting and object exploration in sitting. For each part of the figure the black represents the 4 month visit and the gray represents the 6 month visit. Infants made little to no contact with the toys during the baseline and post intervention visits so they are not included. 6A) Reaching in Supine: Sum of the Percent of the assessment time each hand was in contact with the toy in supine. Value ranges from 0 to 200 if the infant was in contact with the toy for 100 percent of the time with both hands. 6B) Reaching in Sitting: Sum of the Percent of the assessment time each hand was in contact with the toy in sitting. Value ranges from 0 to 200 if the infant was in contact with the toy for 100 percent of the time with both hands. 6C) Object to mouth in Sitting: Percent of the time holding the object in which the object is touching the infant’s mouth or lips. 6D) Looking in Sitting: Percent of the seated reaching that the infant was looking at the object.
Feasibility
The movement program and the comprehensive assessment paradigm used in this case series were feasible and well tolerated by the infants and family in the first months of life. The infants BLP included in this case series completed the intervention at least 80 percent of the recommended frequency, despite the fact that both were receiving the intervention and other children were in the home. Initiating the intervention at 0.5 months of adjusted age was feasible and helped this mother establish a routine for developmental play early in the infants’ lives. Infants completed each assessment visit in 1 to 3 sessions. In combination, the 10 minutes of supine (COP assessment and supine reaching) and 10 minutes of sitting (reaching and object exploration) plus the TIMP were tolerated well. Equipment set up time in the family home, transition time between activities, and care giving breaks resulted in most sessions lasting about one hour per infant. In general, the visits at 2 months of age or less required multiple sessions as parents had more difficulty estimating when their infants would be awake and playful and infants fatigued faster than at older ages. Scoring the assessments by video enabled the research team to save time during the assessment visit and allowed for scoring by individuals blind to infants’ medical and intervention history.
DISCUSSION
Infants BLP, between 34 and 36 weeks of gestation, can participate in a parent delivered movement program as early as 0.5 months of age (adjusted for prematurity) when parents are establishing care giving routines. The movement program presented in this 2 infant case series is novel as it engaged the parent in activities to support posture and movement experiences starting weeks or months before these infants typically would receive early intervention services under IDEA. The mother who completed the movement program activities with her twins was eager to support the twin’s development and performed the activities on an almost daily basis during the 1.5 months of intervention. She reported that the activities became a part of her routine play with the twins and that it was feasible to include them in care giving. Previous research suggests that parent can modify their interaction with their infants following education in the first months after hospital discharge.39 We speculate that parents who participate in this or similar movement programs will change their interactions with their infants to include components of the movement program in their daily activities during and after the intervention periods, increasing the ability for these programs to enhance infant development.40
A Movement Program May Improve Development
Both infants in this case series demonstrated improved motor development and postural control during the study period. Both demonstrated increasing TIMP z-scores during and after the movement program suggesting the infants’ motor development improved at a faster rate than the normative sample of the TIMP. Similar to infants born full term, the infants’ postural control complexity remained fairly constant during the movement program. Infant A’s experience for over 3 months in a Pavlik harness may have altered her development of postural control as well as her postural control assessment, as she wore the Pavlik Harness for these assessments. However, both infants demonstrated a slight decrease in postural control complexity over time, which signifies the infants’ abilities to select efficient postural control strategies.33,35,36 The very rapid decline in postural control complexity observed in infant B after the completion of the movement program suggests his postural control may have become excessively repetitive. This type of repetitive postural control may be an early indicator of developmental delay or motor impairments, which were identified in this infant at 12 months of age.35 In combination, the postural control findings from this case series are generally consistent with research documenting differences in postural control complexity between infants at risk of developmental disabilities and the ability to change postural control complexity through intervention.31,32,34
Improvement in postural control supports the development of reaching and object exploration.41 While the movement program did not directly provide the infants with additional reaching or object exploration experiences, the 2 infants in this case series improved their reaching, especially in sitting. Postural control and reaching in supine are linked to coordination and motor impairments at 6 years of age.41,42 Although our measures of postural control and reaching differ from this research, the evidence suggests that reduced variability of postural control at 4 months (“still” posture42) and limited reaching at 6 months are associated with future motor dysfunction. Both infants in this case series demonstrated increased successful reaching for objects in supine and sitting by 6 months of age. We speculate that the improvements observed in reaching in the case series infants may be, in part, related to improved postural control.
Both of the infants who participated in the movement program in this case series demonstrated increasing exploration of toys by looking at suspended toys and bringing a toy to the mouth. While typically developing infants bring hands and toys to mouth in early infancy, additional experience with objects has been shown to advance mouthing behaviors.18 While our intervention did not specifically focus on object experience, we speculate that increased reaching and postural control facilitated more opportunities to interact with objects.
Early Intervention May be Warranted for Infants BLP
Intervention programs have been shown to improve development for infants born full term and preterm, yet, aside from the intervention received as a result of this study, these infants BLP did not receive any early intervention services and their mother was not educated by anyone in the medical community on play activities in the first 12 months of life. While neither infant was cared for in the NICU, the infants were still at risk for developmental delays based on their late preterm birth status. While further research is needed, this case series, in combination with other literature, provides preliminary evidence that parents may be taught to provide experiences that help their infants “catch up” from mild motor delays.17,21,23,38 While this case series cannot confirm that the movement program improved development in these infants BLP, it does support the need and feasibility for infants born late preterm to participate in developmental monitoring and parent education in the first year of life. If the benefit of very early intervention is documented through larger studies, it could have significant policy implications for timing and eligibility for early intervention services and to support parents in providing early movement experiences for infants BLP.
A Comprehensive Assessment Plan Is Needed to Document Changes
The comprehensive assessment included in this study was feasible to complete for infants as young as 0.5 months of adjusted age. It required a significant commitment from the families and researchers to complete all portions of the assessment, using multiple sessions if necessary. While the TIMP and Bayley provide a view of an infant’s motor development, they are not sensitive to changes in postural control, spontaneous movement, reaching, or object exploration. Likewise, the measures of postural control, reaching, and object exploration do not provide information on the infant’s broader motor development. However, the combination of the measures in this case series provided a sensitive measure of change. The TIMP, head control, and postural sway measures changed from 0.5 to 2 months of age when the infants were participating in an intervention to advance postural control and were provided movement experience. The TIMP, reaching, and object manipulation measures all demonstrated change in the months following intervention suggesting that any one of these measures alone would be insufficient to show the broad scope of changes during the first 6 months of life. To evaluate the efficacy of interventions on development, researchers must quantify an infant’s ability to generate movement, reach, and interact with objects all of which supports motor, cognitive, and language development.17,43 This case series supports the feasibility of this protocol to evaluate developmental change in young infants. Additional measures of parent-infant play may be warranted to document how the intervention influences parent/infant play routines during and beyond the intervention period.
Conclusion
The findings from this 2 infant case series, while preliminary in nature, support the feasibility of providing a parent delivered movement program to infants BLP starting at 0.5 months of adjusted age. The positive changes in motor development, postural control, reaching and object exploration seen in the twins born late preterm suggest the need for a larger study to evaluate the efficacy of a movement program to enhance development. Future studies should include a combination of measures to ensure sensitivity to change and to document the relationships between the intervention and parent child interaction, postural control, skill acquisition, object exploration, motor and cognitive development.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the families who generously allowed us to share in the development of their infants. We also thank the research staff in the Infant Motor Behavior Lab at the University of Delaware and the Motor Development Lab at Virginia Commonwealth University for their support in this study.
Grant Support: This project was funded in part by the National Institutes of Health (1K12HD055931-01 & NIH NICHD R01 HD051748-01A1).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare no conflict of interest.
References
- 1.Martin J, Hamilton B, Ventura S, et al. Births: Final Data for 2009. National Vital Statistics Reports. 2011:60. [PubMed] [Google Scholar]
- 2.Ishiguro A, Namai Y, Ito YM. Managing"healthy" late preterm infants. Pediatr Int. 2009;51:720–725. doi: 10.1111/j.1442-200X.2009.02837.x. [DOI] [PubMed] [Google Scholar]
- 3.Morse SB, Zheng H, Tang Y, Roth J. Early school-age outcomes of late preterm infants. Pediatrics. 2009;123:e622–e629. doi: 10.1542/peds.2008-1405. [DOI] [PubMed] [Google Scholar]
- 4.McGowan JE, Alderdice FA, Holmes VA, Johnston L. Early childhood development of late-preterm infants: a systematic review. Pediatrics. 2011;127:1111–1124. doi: 10.1542/peds.2010-2257. [DOI] [PubMed] [Google Scholar]
- 5.Petrini JR, Dias T, McCormick MC, Massolo ML, Green NS, Escobar GJ. Increased risk of adverse neurological development for late preterm infants. J Pediatr. 2009;154:169–176. doi: 10.1016/j.jpeds.2008.08.020. [DOI] [PubMed] [Google Scholar]
- 6.Moster D, Lie RT, Markestad T. Long-term medical and social consequences of preterm birth. N Engl J Med. 2008;359:262–273. doi: 10.1056/NEJMoa0706475. [DOI] [PubMed] [Google Scholar]
- 7.McCormick MC, Litt JS, Smith VC, Zupancic JAF. Prematurity: An Overview and Public Health Implications. Annual Review of Public Health. 2011;32:367–379. doi: 10.1146/annurev-publhealth-090810-182459. [DOI] [PubMed] [Google Scholar]
- 8.Individuals with Disabilities Education Improvement Act of 2004
- 9.Infant & Toddler Connection of Virginia. Practice Manual, Chapter 5 Infants and Toddler Connection Web site http://www.infantva.org/documents/PracManCh5.pdf. [Accessed 2/23/12]. Updated 8/7/11. [Google Scholar]
- 10.Spittle AJ, Doyle LW, Boyd RN. A systematic review of the clinimetric properties of neuromotor assessments for preterm infants during the first year of life. Dev Med Child Neurol. 2008;50:254–266. doi: 10.1111/j.1469-8749.2008.02025.x. [DOI] [PubMed] [Google Scholar]
- 11.Kalia JL, Visintainer P, Brumberg HL, Pici M, Kase J. Comparison of enrollment in interventional therapies between late-preterm and very preterm infants at 12 months' corrected age. Pediatrics. 2009;123:804–809. doi: 10.1542/peds.2008-0928. [DOI] [PubMed] [Google Scholar]
- 12.Libertus K, Needham A. Teach to reach: The effects of active vs. passive reaching experiences on action and perception. Vision Research. 2010;50:2750–2757. doi: 10.1016/j.visres.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanakogi Y, Itakura S. Developmental correspondence between action prediction and motor ability in early infancy. Nat Commun. 2011;2:341. doi: 10.1038/ncomms1342. [DOI] [PubMed] [Google Scholar]
- 14.Soska KC, Adolph KE, Johnson SP. Systems in Development: Motor Skill Acquisition Facilitates Three-Dimensional Object Completion. Developmental Psychology. 2010;46:129–138. doi: 10.1037/a0014618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adolph KE, Tamis-LeMonda CS, Ishak S, Karasik LB, Lobo SA. Locomotor experience and use of social information are posture specific. Dev Psychol. 2008;44:1705–1714. doi: 10.1037/a0013852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bertenthal BI, Longo MR. Motor knowledge and action understanding: A developmental perspective. In: Klatzky RL, MacWhinney B, Behrman M, editors. Embodiment, ego-space, and action. New York, NY US: 2008. [Psychology Press]. pp. 323–368. [Google Scholar]
- 17.Lobo MG JC. Postural and Object-oriented Experiences Advance Early Reaching, Object Exploration, and Means-end Behavior. Child Dev. 2008;79:1869–1890. doi: 10.1111/j.1467-8624.2008.01231.x. [DOI] [PubMed] [Google Scholar]
- 18.Needham A, Barrett T, Peterman K. A pick-me-up for infants' exploratory skills: Early simulated experiences reaching for objects using 'sticky mittens' enhances young infants' object exploration skills. Infant Behav Dev. 2002;25:279–295. [Google Scholar]
- 19.Lee HM, Galloway JC. Early Intensive Postural and Movement Training Advances Head Control in Very Young Infants. Physical Therapy. 2012;83:1290–1302. doi: 10.2522/ptj.20110196. [DOI] [PubMed] [Google Scholar]
- 20.Zelazo N, Zelazo P, Cohen K, Zelazo P. Specificity of Practice Effects on Elementary Neuromotor Patterns. Developmental Psychology. 1993;29:686–691. [Google Scholar]
- 21.Heathcock JC, Lobo M, Galloway JC. Movement training advances the emergence of reaching in infants born at less than 33 weeks of gestational age: a randomized clinical trial. Phys Ther. 2008;88:310–322. doi: 10.2522/ptj.20070145. [DOI] [PubMed] [Google Scholar]
- 22.Lobo MA, Galloway JC. Enhanced handling and positioning in early infancy advances development throughout the first year. Child Development. 2012 Jul-Aug;83(4):1290–1302. doi: 10.1111/j.1467-8624.2012.01772.x. [DOI] [PubMed] [Google Scholar]
- 23.Heathcock JC, Galloway JC. Exploring objects with feet advances movement in infants born preterm: a randomized controlled trial. Phys Ther. 2009;89:1027–1038. doi: 10.2522/ptj.20080278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Campbell S. The Test of Infant Motor Performance: Test User's Manual Version 2.0. Chicago, IL: Infant Motor Performance Sclares, LLC; 2005. [Google Scholar]
- 25.Bayley N. Balyey Scales of Infant and Toddler Development. 3rd ed. San Antonio, TX: PsychCorp; 2006. [Google Scholar]
- 26.Corbetta D, Snapp-Childs W. Seeing and touching: The role of sensory-motor experience on the development of infant reaching. Infant Behavior & Development. 2009;32:44–58. doi: 10.1016/j.infbeh.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 27.Rochat P. Self-perception and action in infancy. Exp Brain Res. 1998;123:102–109. doi: 10.1007/s002210050550. [DOI] [PubMed] [Google Scholar]
- 28.Campbell SK. Test-retest reliability of the Test of Infant Motor Performance. Pediatric Physical Therapy. 1999;11:60–66. [Google Scholar]
- 29.Campbell SK, Kolobe TH, Wright BD, Linacre JM. Validity of the Test of Infant Motor Performance for prediction of 6-, 9- and 12-month scores on the Alberta Infant Motor Scale. Dev Med Child Neurol. 2002;44:263–272. doi: 10.1017/s0012162201002043. [DOI] [PubMed] [Google Scholar]
- 30.Campbell SK, Levy P, Zawacki L, Liao PJ. Population-based age standards for interpreting results on the test of motor infant performance. Pediatr Phys Ther. 2006;18:119–125. doi: 10.1097/01.pep.0000223108.03305.5d. [DOI] [PubMed] [Google Scholar]
- 31.Harbourne R, Willett S, Kyvelidou A. A comparison of interventions for children with cerebral palsy to improve sitting postural control. Physical Therapy. 2010;90:XX. doi: 10.2522/ptj.2010132. [DOI] [PubMed] [Google Scholar]
- 32.Deffeyes JE, Harbourne RT, Kyvelidou A, Stuberg WA, Stergiou N. Nonlinear analysis of sitting postural sway indicates developmental delay in infants. Clin Biomech (Bristol, Avon) 2009;24:564–570. doi: 10.1016/j.clinbiomech.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 33.Harbourne RT, Stergiou N. Nonlinear analysis of the development of sitting postural control. Dev Psychobiol. 2003;42:368–377. doi: 10.1002/dev.10110. [DOI] [PubMed] [Google Scholar]
- 34.Dusing S, Kyvelidou A, Mercer VS, Stergiou N. Infants Born Preterm Exhibit Different Patterns of Center of Pressure Movement Than Infants Born at Term. Physical Therapy. 2009;89:1354–1362. doi: 10.2522/ptj.20080361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dusing SC, Harbourne RT. Variability in postural control during infancy: implications for development, assessment, and intervention. Phys Ther. 2010;90:1838–1849. doi: 10.2522/ptj.2010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dusing SC, Thacker LR, Stergiou N, Galloway JC. Early complexity supports development of motor behaviors in the first months of life. Dev Psychobiol. 2012 doi: 10.1002/dev.21045. epub May 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harbourne R, Deffeyes JE, DeJong SL, Stuberg WA, Kyvelidou A. Nonlinear variables can assist in identifying postural control deficits in infants. Journal of Sport & Exercise Psychology (Supplement) 2007;29:S9. [Google Scholar]
- 38.Lobo MA, Galloway JC, Savelsbergh GJ. General and task-related experiences affect early object interaction. Child Dev. 2004;75:1268–1281. doi: 10.1111/j.1467-8624.2004.00738.x. [DOI] [PubMed] [Google Scholar]
- 39.Kang R, Barnard K, Hammond M, et al. Preterm infant follow-up project: a multi-site field experiment of hospital and home intervention programs for mothers and preterm infants. Public Health Nurs. 1995;12:171–180. doi: 10.1111/j.1525-1446.1995.tb00006.x. [DOI] [PubMed] [Google Scholar]
- 40.Bakewell-Sachs S, Gennaro S. Parenting the post-NICU premature infant. MCN Am J Matern Child Nurs. 2004;29:398–403. doi: 10.1097/00005721-200411000-00011. [DOI] [PubMed] [Google Scholar]
- 41.Fallang B, Saugstad OD, Hadders-Algra M. Postural adjustments in preterm infants at 4 and 6 months post-term during voluntary reaching in supine position. Pediatr Res. 2003;54:826–833. doi: 10.1203/01.PDR.0000088072.64794.F3. [DOI] [PubMed] [Google Scholar]
- 42.Fallang B, Oien I, Hellem E, Saugstad OD, Hadders-Algra M. Quality of reaching and postural control in young preterm infants is related to neuromotor outcome at 6 years. Pediatr Res. 2005;58:347–353. doi: 10.1203/01.PDR.0000170898.60160.09. [DOI] [PubMed] [Google Scholar]
- 43.Lobo MA, Harbourne RT, Dusing SC, McCoy SW. Grounding Early Intervention: Physical Therapy Cannot Just Be About Motor Skills Anymore. Phys Ther. 2012 doi: 10.2522/ptj.20120158. epub Sept 20. [DOI] [PMC free article] [PubMed] [Google Scholar]