Abstract
Background
Perinatal health disparities including disparities in caesarean births have been observed between migrant and non-migrant women and some literature suggests that non-medical factors may be implicated. A systematic review was conducted to determine if migrants in Western industrialized countries consistently have different rates of caesarean than receiving-country-born women and to identify the reasons that explain these differences.
Methods
Reports were identified by searching 12 literature databases (from inception to January 2012; no language limits) and the web, by bibliographic citation hand-searches and through key informants. Studies that compared caesarean rates between international migrants and non-migrants living in industrialized countries and that did not have a ‘fatal flaw’ according to the US Preventative Services Task Force criteria were included. Studies were summarized, analyzed descriptively and where possible, meta-analyzed.
Results
Seventy-six studies met inclusion criteria. Caesarean rates between migrants and non-migrants differed in 69% of studies. Meta-analyses revealed consistently higher overall caesarean rates for Sub-Saharan African, Somali and South Asian women; higher emergency rates for North African/West Asian and Latin American women; and lower overall rates for Eastern European and Vietnamese women. Evidence to explain the consistently different rates was limited. Frequently postulated risk factors for caesarean included: language/communication barriers, low SES, poor maternal health, GDM/high BMI, feto-pelvic disproportion, and inadequate prenatal care. Suggested protective factors included: a healthy immigrant effect, preference for a vaginal birth, a healthier lifestyle, younger mothers and the use of fewer interventions during childbirth.
Conclusion
Certain groups of international migrants consistently have different caesarean rates than receiving-country-born women. There is insufficient evidence to explain the observed differences.
Keywords: Caesarean, Immigrants, Refugees, Risk factors, Meta-analysis
Background
The use of medical interventions in birth has quickly risen in the last quarter century particularly in industrialized countries where the development of medical technology has advanced rapidly [1]. Most notable has been the dramatic rise in caesarean births with rates in the last 15 years in the US, Canada, Australia and parts of Europe reaching 25% and above (see http://www.oecd.org/els/health-systems/oecdhealthdata2012-frequentlyrequesteddata.htm). While a caesarean birth can be a life-saving procedure it is associated with a significantly increased risk of maternal death from complications of anaesthesia, puerperal infection, and venous thromboembolism [2]. The World Health Organization therefore recommends that caesareans be performed only in medically necessary instances [3].
Migration flows are increasing globally [4] and migrants contribute substantially to the total number of births, exceeding in some Western countries one fifth of births [5,6]. The health of migrants, including perinatal health, has therefore become a research priority [7]. Migrants (immigrants, refugees, asylum-seekers, undocumented and others with temporary or irregular statuses) [8,9] face multiple and intersecting social determinants of health that may compound childbearing health risks, including lower social economic status, lack of support, high levels of stress related to migration and resettlement and barriers in accessing healthcare [10,11]. Refugees and asylum-seekers may also have suffered trauma and abuse [12,13]. Perinatal health disparities [14], including disparities in caesarean births have been observed between migrants and receiving-country-born women and some literature suggests that non-medical factors such as communication barriers, support and/or care practices during labour and delivery, female genital cutting, or cultural preference may also be implicated in caesarean rate differences [15-17]. We conducted a systematic review to address the questions: 1) Do international migrant women in Western industrialized countries have consistently different rates of caesarean birth than receiving-country-born women? And 2) What are the mechanisms (medical and/or non-medical factors) that might explain differences?
Methods
The “Meta-analysis of Observational Studies in Epidemiology (MOOSE)” recommended guidelines for the publication of meta-analyses of observational studies were used to prepare this manuscript [18].
We searched for cross-sectional and cohort studies that provided comparisons of caesarean rates between migrant and non-migrant women. To be included in the review, studies must have examined migrants who crossed international borders and who were living in an industrialized country, defined using the Organization for Economic Cooperation and Development (OECD) member list; studies conducted in refugee camps or with internally displaced persons were excluded. No restrictions were applied based on migrant origin, status or length of time in receiving-country. We searched the following electronic citation databases: Medline, Health Star, Embase, PsycInfo, CINAHL, Sociological Abstracts, Web of Science, Proquest Research Library, Proquest Dissertations and Theses, POPLINE, Global Health and PAIS. The search strategy was developed in conjunction with a McGill University Health Sciences librarian and can be found in Additional file 1. No language limitations were applied. Searches were conducted from inception of each database until January 2012.
We also hand-searched reference lists of identified literature, conducted web searches and contacted migration and health research experts for additional literature. Web sites searched included professional agency [(e.g., International Federation of Gynecology and Obstetrics (FIGO)] and government (Canada, US and Australia) health sites (see Additional file 2). Each site was searched by browsing through relevant indices predefined by each website and by using ‘search boxes’. Terms included: “c(a)esarean, c-section, mode of delivery, (im)migrant, (im)migration, foreign, country of birth”. Requests for literature were made through ROAM (Reproductive Outcomes and Migration), an international research collaboration, involving over 30 researchers from 13 countries, including Canada, Australia and Europe (see http://migrationandreproductivehealth.org/?page_id=76).
We reviewed all abstracts (or full articles if necessary) to determine if inclusion criteria were met. Those included were subsequently fully reviewed and quality-assessed and data were extracted into a database in Excel©. Non-English language reports were reviewed by ROAM collaborators and if no researcher could read the language of the report, we reviewed the English version abstract only.
The US Preventative Services Task Force criteria were used to assess the quality of studies [19]. Studies were evaluated on the 1) comparability of the study groups (assembly and maintenance); 2) degree of participant loss; 3) clarity of their “migrant” and “non-migrant” classifications; 4) validity and reliability of the approaches used to measure the migrant, caesarean birth and other variables; and 5) attention given to potential confounding factors (i.e., age and parity). Studies with a “fatal flaw” (i.e., ≥ 50% of the original sample lost to analysis and/or comparison groups not adequately defined) were removed from further analysis. Studies were scored as either “good” or “fair”- the former if the study met all quality criteria and the latter if it did not meet all criteria but had no fatal flaw. One reviewer assessed all studies and a second reviewer independently assessed 25% of the studies to confirm the assigned quality scores. Discrepancies were resolved through discussion.
A standardized coding form was developed to extract three types of data: 1) publication year and language; 2) study characteristics (e.g., study sample and data sources) and 3) results. The migration indicator (i.e., how migrants were labelled in the study) was recorded verbatim from the report and categorized by type as: “source country/region”, “foreign-born/non-national”, “ethnicity”, “length of time” or “migration status”. Sources of data were classified as: 1) population-based registry; 2) population-based hospital data; 3) population-based survey; or 4) hospital records/research study. Timeframe and geographical coverage (local, regional, or national) of data collection, host country and number of migrants and non-migrants were also recorded. Extracted results included frequencies of caesarean rates (overall, emergency and elective) and indications for caesarean for migrants and non-migrants separately. Explanations for caesarean rate differences between groups postulated in discussion sections were also extracted.
For each study we defined caesarean rates for migrant women as being “higher”, “lower” or “not different” compared to non-migrant women. If a study had results reported for more than one migrant group comparison they were coded as: “higher” if migrant results in all comparison groups were higher or a combination of higher and not different; “lower” if all were lower or lower and not different; “mixed” if some were higher and some lower; and “not different” if all rates between the migrant and non-migrant groups were not statistically different.
We used Review Manager 5.1© to perform meta-analyses to estimate the ‘effect’ of being a migrant on the outcomes of interest: overall caesarean and emergency and elective caesarean rates. The studies were assumed to be heterogeneous due to the range of host countries and migrant groups examined and changes in obstetrical practice over time. We therefore used a random effects model which regards an effect as variable across studies and produces more conservative effect estimates with wider confidence intervals [20]. We combined and analyzed migrant sub-groups defined using UN macro-regions (see Additional file 3) or country of origin, migration status, and length of time in receiving-country. Sub-analyses by parity, receiving- country/region and time period of data collection were also performed. Due to the diversity across studies in variables selected to control for confounding we chose to use unadjusted results in meta-analyses. We calculated each study’s effect size as an odds ratio (OR) using the Mantel-Haenszel model (event/total for migrants and receiving-country women respectively) [20]. Attention was given to ensure duplicate data from different reports were not included twice in analyses and only one comparison from each study was combined for meta-analyses to ensure the results from a comparison group were not counted more than once. A weighted summary effect was calculated for each analysis performed.
To investigate the robustness of results which showed migrant women to consistently have different rates of caesarean compared to receiving-country-born women, sensitivity analyses were performed by limiting the analyses to only population-based data. To assess whether results would differ when covariates were adjusted, we also performed analyses by using adjusted odds ratios and applying the generic inverse variance method to produce summary estimates. Heterogeneity for all meta-analyses was assessed using I2 tests and we considered a value of 50% or more to indicate substantial heterogeneity [20]. We also examined confidence intervals among the studies in each forest plot to assess the degree of overlap; less overlap being interpreted as evidence of heterogeneity [20]. Publication bias was assessed by visual examination of funnel plots of the OR against the standard error of the log of the OR of studies within each migrant subcategory [20].
Results
The database search yielded over eight thousand citations (n=8565). Once duplicates and studies that did not meet the inclusion criteria were excluded, 87 reports remained. Seventeen additional reports were identified: seven through hand searches, nine from ROAM collaborators and one annual report published by the New South Wales (Australia) Department of Health [21] online. Three reports could not be reviewed because of language [22-24]. Twenty studies were removed because the comparison group included migrants, and/or the migrant group included native-born, and/or the assembly of the migrant and non-migrant groups were dissimilar. Seventy-six studies met the inclusion criteria and were assigned a quality score (see Table 1 for a complete description of included studies) [15-17,25-103]. Twenty-two studies were scored as good and 54 were scored as fair (see Table 2). The primary reasons for not meeting all of the quality criteria was a lack of attention to confounding and ambiguity on how study groups (migrants vs. non-migrants) were defined or confirmed.
Table 1.
Description of included studies
| Reference (language of publication) | Method (geographical coverage, data source, data yr) | Receiving country | Population | Findings Migrants vs. Non-migrants*(Overallcaesarean rates)(Emergency&/orElective caesarean rates) | Quality |
|---|---|---|---|---|---|
| Alonso CP, Maresca MI, Oritz TA, & Serrano MM. (2006) (Spanish) |
Local, hospital records, 2000-2002 |
Spain (Madrid) |
2759 African, American, European, & Oriental "immigrants" vs. 3990 Spanish women. |
L & ND overall (not statistically tested) |
Fair |
| Aurelius G, & Ryde-Blomqvist E. (1978) (English) |
Local, hospital records, 1968-1969 |
Sweden (Stockholm) |
1235 “Immigrants” from Scandinavia, West, South, & East Europe, & “other countries” vs. 412 Swedish women. Only singleton births included. |
H & ND overall (unadjusted) |
Fair |
| Barron SL, & Vessey MP. (1966) (English) |
Local, hospital records, 1958-1960 |
UK (South London) |
1563 West Indian & Irish “immigrants” vs. 3891 British women. Only singleton births. |
H overall (not statistically tested; W Indian: primips H, multips ND; Irish: primips ND, multips H) |
Fair |
| Berger C, Liska G, Gallier J, & Soutoul JH. (1973) (French) |
Local, hospital records, 1970-1972 |
France (Tours) |
800 Portuguese/Spanish, North African, Yugoslavia, “other” “migrants” vs. 2655 French women. |
M overall (not statistically tested) |
Fair |
| Berger C, Laugier J, & Soutoul JH. (1974) (French) | |||||
| Bona G, Zaffaroni M, Cataldo F, Sandri F, & Salvioli GP. (2001) (English) |
National, population-based hospital data, 1996-1997 |
Italy |
3347 “Legal immigrants from developing countries” (Latin America, North Africa, Sub Saharan Africa, Middle East, Indian Sub-continent, Far East, Oceania, Eastern Europe, & Gipsies) vs. 6694 Italians. |
ND overall (all immigrants combined; unadjusted; Variation by groups but not statistically tested) |
Fair |
| Braveman P, Egerter S, Edmonston F, & Verdon M. (1995) (English) |
Regional, population-based registry, 1991 |
US (California) |
81,445 Asian and Latina “foreign born” vs. 93,685 “Whites”. Only singleton primiparous women. |
L & ND overall (adjusted) |
Good |
| Cassell E. (1995) (English) Thesis |
Regional, population-based registry, 1982-1992 |
Australia (Victoria) |
5268 Filipino-born vs. 507,457 Australian-born. |
H overall (stratified by parity and age caesarean rates consistently H) H emerg (unadjusted) H elect (unadjusted) |
Good |
| Chan A, Roder D, & Macharper T. (1988) (English) |
Regional, population-based registry, 1981-1983 |
Australia (South Australia) |
5675 “Non-English speaking countries” (includes Italy, Holland, Germany, Vietnam, Greece, Yugoslavia, Philippines, & “other”) vs. 2894 Australian-born. |
H overall (all immigrants combined; unadjusted; Variation by groups but not statistically tested) H emerg (all immigrants combined; unadjusted) H elect (all immigrants combined; unadjusted) |
Fair |
| Comas M, Català L, Sala M, et al. (2011) (English) |
Local, hospital records, 2006-2007 |
Spain (Barcelona) |
564 Foreign-born (includes women from South America, Asia and North Africa- Morocco, Pakistan and Ecuador most represented) vs. 462 Spanish-born women. Only women who lived in hospital catchment area were included. |
ND overall (all immigrants combined; unadjusted) |
Fair |
| Delvaux T, Buekens P, Thoumsin H, Dramaix M, & Collette J. (2003) (English) |
Local, research study, 1997-1998 |
Belgium (Liege) |
89 North-African nationality vs. 184 Belgian nationality women. Singleton live births, excluded women with gestational diabetes & malformed babies at birth. |
ND overall (unadjusted) |
Fair |
| Diani F, Zanconato G, Foschi F, Turinetto A, & Franchi M. (2003) (English) |
Local, hospital records, 1992-2001 |
Italy (Verona) |
1014 “Non-EU women” (including Central Africa, Northern Africa/Middle East, Eastern Europe, Asia, & Latin America) vs. 12,931 Italians. |
H overall (all immigrants combined; unadjusted) |
Fair |
| Fedeli U, Alba N, Lisiero M, Zambon F, Avossa F, & Spolaore P. (2010) (English) |
Regional, population-based registry, 2006-2007 |
Italy (Veneto region) |
20,332 Regular and Irregular foreign born/migrants vs. 73,098 Italian women. |
L overall (unadjusted; when stratified by age for regular migrants ND across strata except ages 30-34 years H) |
Fair |
| Forna F, Jamieson DJ, Sanders D, & Lindsay MK. (2003) (English) |
Local, hospital records, 1991-2001 |
US (Atlanta) |
13,465 Africa, Asia, Caribbean, Europe, Central & South America, Middle East & “other” foreign-born vs. 36,439 US born (mostly Black women). Excluded women with no prenatal care. |
H & ND overall (unadjusted) |
Fair |
| Gagnon AJ, Dougherty G, Platt RW, et al. (2007) (English) and Gagnon AJ, Van Hulst A, Merry L, et al. (2012) (English) Unpublished when review of literature was conducted, 2007 reference describes original study; 2012 reference is publication of caesarean results (after review of literature was completed) |
Local, research study, 2003-2004 |
Canada (Montreal, Toronto, Vancouver) |
1018 “Recently arrived migrants (≤ 5 years)” and defined by UN Macro Region (Europe, Latin America, Africa, West Asia/North Africa, & South-Central Asia), migration status (refugee, asylum seeker, non-refugee immigrant) and length of time (≤ 2 years vs. > 2 years) vs. 2482 Canadian-born. Only low-risk (≤ 35 years, gestational age ≤ 42 weeks) primiparous women. |
H & ND overall (unadjusted but restricted to low-risk population) ND emerg (unadjusted but restricted to low-risk population) ND elect (not statistically tested) |
Good |
| Gagnon AJ, Wahoush O, Dougherty G, et al. (2006) (English) Unpublished, 2006 reference describes study |
Local, research study, 2006-2009 |
Canada (Montreal, Toronto, Vancouver) |
1025 “Recently arrived migrants” (≤ 5 years) defined by migration status: refugee, asylum seeker, non-refugee immigrant vs. 514 Canadian-born. |
ND overall (unadjusted) ND emerg (unadjusted) ND elect (unadjusted) |
Fair |
| Gann P, Nghiem L, & Warner S. (1989) (English) |
Local, hospital records, 1981-1987 |
US (Lowell) |
310 Cambodian refugees vs. 110 low income Whites. Only singleton births included. Primary caesareans only. |
L overall (unadjusted; ND primips, L multips) |
Fair |
| Gayral-Taminh M, Arnaud C, Parant O, Fournie A, Reme JM, & Grandjean H. (1999) (French) |
Local, hospital records, 1988-1994 (excl 1990) |
France (Toulouse) |
2636 “Black Africa” & Maghreb vs. 3172 French women. Only singleton births included. |
H & ND overall (unadjusted; results consistent when stratified by parity) ND during labour caesarean (unadjusted) ND pre-labour caesarean (unadjusted) |
Fair |
| Giani U, Bruzzese D, Pugliese A, Saporito M, & Triassi M. (2011) (Italian, used English abstract) |
Regional, population-based registry, 2005 |
Italy (Campania) |
1709 Foreign-born women vs. 28,557 Italian women. Excluded repeat caesareans. |
L elect (adjusted) |
Good |
| Harlap S, Kaufman R, Prywes R, Davies AM, Sterk VV, & Weiskopf P. (1971) (English) |
Local, research study, 1964-1967 |
Israel (West Jerusalem) |
13,112 Asian, North African, & Western countries (based on birth place) vs. 7635 Israeli women. Only singleton births. |
H overall (not statistically tested) |
Fair |
| Hazekamp JT. (1982) (English) |
Local, hospital records, 1978 |
Norway (Oslo) |
51 Wives of Pakistani migrant workers vs. 51 Norwegian women matched for age and parity. |
ND overall (not statistically tested) |
Fair |
| Helsel D, Petitti DB, & Kunstadter P. (1992) (English) |
Regional, population-based registry, 1985-1988 |
US (Merced & San Joaquin counties, California) |
1937 Hmong refugees vs. 3776 non-Hispanic Whites. Mixed marriages excluded. Only singleton births included. |
L overall (results consistent across different age and parity strata) |
Good |
| Henry OA, Guaran RL, Petterson CD, & Walstab JE. (1992) (English) |
Local, hospital records, 1979-1988 |
Australia (Melbourne) |
1123 Vietnamese (likely refugees) vs. 35,373 Australian born women. |
ND overall (adjusted) |
Good |
| Holan S, Vangen S, Hanssen K, & Stray-Pedersen B. (2008) (Norwegian) |
Local, research study, 1993-1998 |
Norway (Oslo) |
220 Asian/African women combined (including women from Pakistan, Sri Lanka, India, Vietnam, Morocco, & Somalia) immigrants with diabetes vs. 262 Norwegian women with diabetes. Only singleton births included. |
L overall (unclear if statistically significant; results similar when just primips) ND emerg (not statistically tested) ND elect (not statistically tested) |
Fair |
| Howell R. (1989) (English) |
Local, hospital records, 1980-1984 |
Australia (Brisbane) |
338 Vietnamese refugees and Filipino women (most married to Caucasian men) vs. 14,790 Australian-born women. |
ND overall (unadjusted; ND for primips, L & ND for multips) H emerg (not statistically tested), H (primips) & ND (multips) emerg (unadjusted) L & ND elect (unadjusted but consistent results by parity) |
Fair |
| Ismail KI, Marchocki Z, Brennan DJ, & O’Donoghue K. (2011) (English) |
Local, hospital records, 2009 |
Ireland (Cork) |
867 Eastern European women (refers to women from Belarus, Bulgaria, Czech Republic, Hungary, Moldova, Poland, Romania, Russia, Slovakia, & Ukraine); nationality used to categorize; most would be economic migrants. Multiple, breech and elective or pre-labour caesareans were excluded vs. 5550 Irish women. |
ND caesareans during labour (unadjusted) L (primips, unadjusted but results consistent when stratified by age) & ND (multips, unadjusted) caesareans during labour |
Good |
| Ismail KI, Marchocki Z, Brennan DJ, & O’Donoghue K. (2010) (English) Conference abstract | |||||
| Janevic T.(2011)† (English) Conference abstract |
Local, population-based registry, 1995-2003 |
US (New York) |
511,564 “Foreign-born and ethnicity/region of origin” : North Africa, Sub-Saharan Africa, Africa unspecified, Non-Hispanic Caribbean, Hispanic Caribbean, Mexico, South America, Central America, East Asia, South East Asia/Pacific Islands, & South Central Asian vs. 449,817 US born women. Singleton births only. |
M overall (adjusted) |
Good |
| Johnson EB, Reed SD, Hitti J, & Batra M. (2005) (English) |
Regional, population-based registry, 1993-2001 |
US (Washington) |
579 Somali immigrants vs. 4837 US-born Whites & Blacks. Only singleton births. |
H (compared to US Whites) & ND (compared to US Blacks) (not statistically tested) H (primips) & ND (multips) overall; (adjusted) |
Good |
| Kaminski M. (1975) (French) |
Local, research study, 1963-1969 |
France (Paris) |
1795 Migrants from North Africa, South Europe & the Antilles (only women whose husbands were also born outside of France were considered migrants) vs. 5774 French women. |
H& ND overall (unadjusted) |
Fair |
| Kingston D, Heaman M, Chalmers B, Kaczorowski J, et al. (2011) † (English) |
National, Population-based survey, 2006 |
Canada |
16,040 “Landed immigrants” (residents) (including North America, Central America, Caribbean/Bermuda, South America, West Europe, East Europe, North Europe, South/unspecified Europe, East Africa, North Africa, West/Central Asia/Middle East/Kurdistan, East Asia, South East Asia/Asia/East Timor, South Asia/Asia non-specified) defined as recent (≤ 5 years) and non-recent arrival (> 5 years) vs. 57,800 Canadian-born. Only singleton births. Weighted numbers. |
ND overall (all countries combined & stratified by time since arrival; adjusted; Variation by country but not statistically tested) |
Good |
| Lansakara N, Brown SJ, & Gartland D. (2010) (English) |
Local, research study, 2003-2005 |
Australia (Melbourne) |
212 Mothers born overseas of non-English speaking background- needed to be fluent in English to participate; included women from 53 different countries, largest group were from South Asia, Sri Lanka and India vs. 1074 Australian-born mothers. Primiparous women only. |
ND overall (all countries combined; unadjusted) ND emerg (all countries combined; unadjusted) ND elect (all countries combined; unadjusted) |
Fair |
| LeRay C, Carayol M, Zeitlin J, Breart G, & Goffinet F. (2006) (English) |
National, research study, 2001-2002 |
France |
618 “Origin abroad” (including North Africa, North European, South European, African & Asian) vs. 2797 French. Only low risk primiparous, singleton, cephalic presentation, no induction, Birthweight 2500-4500 g babies, included. |
H caesarean during labour (all migrants combined; adjusted; Variation by groups but not statistically tested) |
Good |
| Loew D, & Schrank P. (1966) (German) |
Local, hospital records, 1956-1965 |
Germany (Russelheim) |
398 “Foreigners” (including Southern Europe, East Europe & “other”) vs. 6602 German women. |
H overall (all foreigners combined; unadjusted) |
Fair |
| Ma J, & Bauman A. (1996) (English) |
Regional, population-based registry, 1990-1992 |
Australia (New South Wales) |
64,922 Immigrant women from Europe, Asia, Africa, New Zealand/Oceania, Middle East, America vs. Australian (non-Aboriginal). |
M overall (unadjusted) |
Fair |
| Malin M, & Gissler M. (2009) (English) |
National, population-based registry, 1999-2001 |
Finland |
6532 Migrants from Latin American/Caribbean, Somali, African, Vietnamese, South East Asian, Iran/Afghan/Iraq, Chinese, South Asian, Middle East, Baltic, Soviet Union, Eastern Europe, Western Europe, & Nordic (only those with resident status) vs. 158,469 Finnish women. Only singleton births. |
M overall (unadjusted but results presented by parity) |
Fair |
| Maslovitz S, Kupferminc MJ, Lessing JB, & Many A. (2005) (English) |
Local, hospital records, 2001-2002 |
Israel (Tel Aviv) |
721 Non-resident foreign labourers [mostly Eastern Europe, also included women from Africa (Kenya, Nigeria, Ghana) and Asia (Thailand, Philippines, China)] vs. 16,012 Israeli residents. |
H overall (all migrants combined; unadjusted) H emerg (all migrants combined; unadjusted) L elect (all migrants combined; unadjusted) |
Fair |
| Merten S, Wyss C, & Ackermann-Liebrich U. (2007) (English) |
National, population-based hospital data, 2000-2002 |
Switzerland |
24,284 Migrants based on nationalities from various regions &/or countries of birth: Africa, Latin America, Asia, Balkan/Turkey, EU/USA; Angola, DR Congo, Morocco, Somalia, Tunisia, Brazil, Dominican Republic, Peru, Philippines, Sri Lanka, Thailand, Vietnam, Albania, Bosnia, Croatia, Kosovo, Macedonia, Serbia, Turkey, Austria, France, Germany, Italy, Netherlands, Poland, Portugal, Russia, Spain, UK, & USA vs. 7500 Swiss women. |
M overall (adjusted) |
Good |
| Moscioni P, Romagnoli C, Pomili G, & Gilardi G. (1995) (Italian) |
Local, hospital records, 1992-1994 |
Italy (Perugia) |
186 “Immigrant/foreign women” vs. 1716 Italian women. |
L overall (unadjusted) |
Fair |
| Mossialos E, Allin S, Karras K, & Davaki K. (2005) (English) |
Local, hospital records, 2002 |
Greece (Athens) |
181 “Immigrants” (majority from Albania, also included other Balkan countries and India/Philippines/Pakistan) vs. 259 Greek women. Only singleton births. |
L overall (all immigrants combined; adjusted) |
Good |
| Oliva GC, Zannella MP, Filidi C, Cavaliere AF, Casarella L, & Mancuso S. (2007) (Italian) |
Local, hospital records, 2000-2004 |
Italy (Rome) |
2628 “Foreign women based on nationality” vs. 11,976 Italian women. |
L overall (unadjusted) H during labour caesarean (unadjusted) L pre-labour caesarean (unadjusted) |
Fair |
| Panagopoulos P, Tsoukalos G, Economou A, et al. (2005) (English) |
Local, hospital records, 2000-2004 |
Greece (Piraeus) |
1990 “Immigrants” (according to nationality) vs. 1081 Greek women. |
ND overall (unadjusted) |
Fair |
| Parsons L, Macfarlane AJ, & Golding J. (1993) (English) |
National, population-based registry, 1982-1985 |
UK |
Mediterranean, African (excluding East Africa), Bangladeshi, & Pakistani vs. UK women. |
M overall (+ variation by parity; unclear if statistically significant) |
Fair |
| Press F, Katz M, Leiberman JR, Shoham I, & Glezerman M. (1993) (English) |
Local, hospital records, 1988-1991 |
Israel (Be’er Sheva) |
431 Ethiopian Jewish immigrants vs. 20,047 Israeli Jewish women. |
ND overall (unadjusted) |
Fair |
| Richman D, & Dixon S. (1985) (English) |
Local, research study, 1980-1981 |
US (San Diego) |
50 Hmong and Cambodian refugees vs. 25 Caucasian (non-Spanish, non-Oriental surnames). |
L overall (unadjusted) |
Fair |
| Rio I, Castelló A, Barona C, et al. (2010) (English) |
Regional, population-based registry, 2005-2006 |
Spain (Catalonia & Valencia) |
34,746 Latin America, Eastern Europe, & Maghreb vs. 180,633 Spanish women. Only singleton births. |
M overall (adjusted for age but not parity) |
Fair |
| Rizzo N, Ciardelli V, Gandolfi-Colleoni G, et al. (2004) (English) |
Local, hospital records, 1997-2001 |
Italy (Bologna) |
510 Immigrant women from non-EU countries vs. 510 Western world (Italy, other EU, Australia, Canada, US). Only singleton births. |
ND overall (unadjusted) ND emerg (unadjusted) L elect (unadjusted) |
Fair |
| Roman H, Blondel B, Bréart G, & Goffinet F. (2008) (English) |
National, population-based survey, 2003 |
France |
585 Africa (excluding North Africa), North Africa, Europe, & “other” nationalities vs. 4658 French women. Only included low risk, singleton births, with no previous caesarean or medical indications for caesarean. |
H & ND overall (not statistically tested) H & ND caesareans during labour (adjusted) H & ND caesareans pre-labour (adjusted) |
Good |
| Rudman A, El-Khouri B, & Waldenström U. (2008) † (English) |
National, population-based survey, 2000 |
Sweden |
236 Swedish-speaking Foreign-born vs. 2472 Swedish women. |
ND overall (unadjusted) ND emerg (unadjusted) ND elect (unadjusted) |
Fair |
| Rumbaut RG. (1996) (English) |
Local, hospital records, 1989-1991 |
US (San Diego) |
1211 “Foreign-born & ethnicity”: defined as White, Asian, Hispanic, & Black; Europe/Canada, Middle East, Indo-Chinese, East Asian, Mexican, Central America & Sub-Saharan Africa vs. 253 US born. |
L & ND overall (unadjusted) |
Fair |
| Saurel-Cubizolles M-J, Saucedo M, Drewniak N, Blondel B, & Bouvier-Colle M-H. (2012) (French) |
National, Population-based survey, 2010 |
France |
1864 Foreign-born (based on nationality) who could complete the survey in French: European (including Turkey), North-African, Sub-Saharan African, & other; 13% arrived in 2009/2010 and 36% between 2005-2008. vs. 12,125 French women. |
H & ND overall (unadjusted) H & ND caesarean during labour (unadjusted) H & ND caesarean pre- labour (unadjusted) |
Fair |
| Saurwein A. (1969) (German) |
Local, hospital records, 1964-1968 |
Germany (Cologne) |
297 “Foreigners” from Southern Europe (including Turks, Greeks, Italian, & Spanish women) vs. 7465 German women. |
H overall (all immigrants combined; unadjusted) |
Fair |
| Schliemann F, & Schliemann G. (1975) (German) |
Local, population-based registry, 1969-1973 |
Germany (Hamburg) |
1217 “Foreigners/Guest workers” from Spain, Italy, Portugal, Yugoslavia, Greece, Turkey & “others” vs. 5112 German women. |
H & ND overall (unadjusted) |
Fair |
| Schultze-Naumburg R, & Scholtes G. (1976) (German, used English abstract) |
Local, hospital records, 1968-1973 |
Germany (Berlin) |
1941 “Foreign women” vs. 9009 German women. |
L overall (not statistically tested) |
Fair |
| Shah D, Tay A, Desai A, Parikh M, Nauta M, & Yoong W. (2011) (English) |
Local, hospital records, 2006-2008 |
UK (North London) |
125 First generation Chinese immigrant women (born in China). Economic migrants most likely and mean length of time in UK =3.2 years. vs. 125 British Caucasian women matched for age and parity. |
L overall (unadjusted but matched by age and parity) |
Good |
| Shah RR, Ray JG, Taback N, Meffe F, & Glazier R. (2011) (English) |
Local, hospital records, 2002-2006 |
Canada (Toronto) |
3672 "Foreign born" based on country and region of birth using World Bank classification: Latin America/Caribbean, Western Europe/USA/Japan/Australia/New Zealand, Eastern Europe/Central Asia, Middle East/North Africa, Sub-Saharan Africa, South Asia, East Asia/Pacific. Asylum seekers examined based on health insurance. < 5years & ≥ 5years also examined. Women with multiple gestation removed. vs. 1435 Canadian-born. |
H & ND overall (adjusted) |
Good |
| Shah RR. (2007) (English) Thesis | |||||
| Sletten K. (2011) (English) Thesis unpublished |
Local, hospital records, 2009-2010 |
Norway (Baerum) |
803 Immigrants from Latin America, Africa, Asia, Eastern Europe, & Western Europe vs. 1634 Norwegian women. Low risk women (35 weeks or greater gestational age, no diabetes, singleton births) only. |
H & ND overall (unadjusted) H & ND emerg (adjusted) L & ND elect (adjusted) |
Good |
| Small R, & Lumley J. (2007) † (English) Conference abstract |
Regional, population-based registry, 1999-2007 |
Australia (Victoria) |
70,417 Women from Non-English-speaking countries (only countries w >1000 births were included): Vietnam, China, Former Yugoslavia, Philippines, Lebanon, India, Sri Lanka, Somalia, Ethiopia, Eritrea, Sudan, Turkey, Malaysia, Iraq, Cambodia, Indonesia, Greece, Germany, Poland and Italy vs. 444,175 Australian-born. |
M overall (+ variation by parity; not statistically tested) |
Fair |
| Small R, Gagnon A, Gissler M, et al. (2008) (English) |
Regional & National, population-based registries, 1997-2004 |
Australia (New South Wales, Victoria), Belgium (Flanders, Brussels), Canada (Ontario, Quebec), Finland, Norway, Sweden |
10,431Somali women vs. 2, 168, 891 receiving-country-born women. |
H overall [Belgium- Flanders (primips & multips) & Belgium -Brussels]; H (primips) & ND (multips) overall (Australia- Victoria, Finland, Norway, & Sweden); ND overall [Australia -New South Wales (primips & multips) & Canada] (unadjusted) |
Fair |
| Stray-Pedersen B, & Austveg B. (1996) (Norwegian) |
Local, hospital records, 1993 |
Norway (Oslo) |
734 "Immigrants" (including Asia/Africa/South America/East Europe and Turkey) vs. 3188 Norwegians. |
H overall (all immigrants combined; unadjusted) |
Fair |
| Teixeira C, Correia S, & Barros H. (2010) (English) Conference abstract |
Geographical coverage not indicated, research study, years not indicated |
Portugal |
743 European/North American, African, & South American (based on country of birth) vs. 6692 Portuguese-born. Singleton births only. |
H & ND overall (adjusted but variables included not indicated) |
Fair |
| Triantafyllidis G, Tziouva K, Papastefanou I, Samolis S, Katsetos C, & Panagopoulos P. (2010) (English) Conference abstract |
Local, hospital records, 2007 |
Greece (Pireaus) |
657 "Immigrants" (based on nationality) (mostly Albanians) vs. 304 Greek women. Only term deliveries (gestational age 37-40 weeks). |
ND overall (unadjusted) |
Fair |
| Van Enk A, Doornbos HP, & Nordbeck HJ. (1990) (English) |
Local, hospital records, 1972-1982 |
Holland (Amsterdam) |
1614 Non-European immigrants defined by ethnic origin: "Blacks" (Surinam & Dutch Antilles), Mediterranean (Turks & Moroccans), Asians [West Indian Asians (Hindustani from Surinam), Chinese & some Indonesians] vs. 6234 Dutch Caucasian. |
H & ND overall (unadjusted; results consistent when stratified by parity) |
Fair |
| Van Enk WJ, Gorissen WH, & Van Enk A. (2000) (English) |
National, population-based registry, 1990-1993 |
Holland |
5841Migrant teenagers (15-19 years old) defined by ethnic and geographical background: Mediterranean [Turkish & North African (mainly Moroccan)], Black (Surinam & Dutch Antilles), Hindustani (West Indian-Asian from Surinam & Dutch Antilles), Asian (Chinese, Malaysian & Malaccan); non-Dutch European (West & East Europe & American), & "others" (mixed, unknown or other ethnicity) vs. 45,570 Dutch (born in Netherlands and West European origin, includes teenagers and 20-24 yr olds). Singleton, primiparous pregnancies. |
M overall (when compared to Dutch teens); L & ND overall (when compared to 20-24 yr old Dutch); (unadjusted but restricted to primips and defined age groups) |
Fair |
| Vangen S, Stoltenberg C, & Schei B. (1996) (English) |
Local, hospital records, 1992 |
Norway (Oslo) |
67 Pakistani vs. 70 Norwegian women. |
ND overall (unadjusted) ND emerg (unadjusted) ND elect (unadjusted) |
Fair |
| Vangen S, Stoltenberg C, Skrondal A, Magnus P, & Stray-Pedersen B. (2000) (English) |
National, population-based registry, 1986-1995 |
Norway |
17,891 Immigrants from Turkey/Morocco, Pakistan, Sri Lanka/India, Vietnam, Philippines, Somalia/Eritrea/Ethiopia, Chile/Brazil vs. 535,600 Norwegians |
M overall (adjusted) H & ND emerg (not statistically tested) M elect (not statistically tested) |
Good |
| Vangen S, Stoltenberg C, Johansen RE, Sundby J, & Stray-Pedersen B. (2002) (English) |
National, population-based registry, 1986-1998 |
Norway |
1733 Somali vs. 702,192 Norwegians. |
H overall (adjusted) H emerg (adjusted) L elect (not statistically tested) |
Good |
| Vangen S, Stray-Pedersen B, Skrondal A, Magnus P, & Stoltenberg C. (2003) (English) |
National, population-based registry,1986-1998 |
Norway |
2408 Filipino mother/Filipino father and mixed= Filipino mother/Norwegian father vs. 615,063 Norwegian women. |
H overall (adjusted) H emerg (not statistically tested) H & ND elect (adjusted) |
Good |
| Vangen S, Stoltenberg C, Holan S, et al. (2003) (English) |
National, population-based registry, 1988-1998 |
Norway |
10,908 "Immigrants" (some had Norwegian citizenship): included countries in North Africa (Morocco, Algeria and Tunisia), South Asia (Pakistan, Sri Lanka, India/Bangladesh) vs. 601,785 Norwegian women. Women with and without diabetes included. |
ND overall (all immigrants combined; not statistically tested) ND emerg (all immigrants combined; not statistically tested) ND elect (all immigrants combined; not statistically tested) |
Fair |
| Versi E, Liu KL, Chia P, & Seddon G. (1995) (English) |
Local, hospital records, 1987-1991 |
UK (East London) |
6460 Bangladeshi vs. 7592 low-income Caucasian women. |
ND overall (unadjusted; results consistent when stratified by parity) ND emerg (not statistically tested) H (multips) & ND (primips) emerg (unadjusted) L (primips & multips) elect (unadjusted) |
Fair |
| Von Katterfeld B, Li J, McNamara B, & Langridge AT. (2011) (English) |
Regional, population-based registry, 1998-2006 |
Australia (West Australia) |
59,245 Foreign-born women as per mother's country of birth as declared in the birth register, ten regional categories as per Standard Australia Classification of countries: Oceania, North/West Europe, South/East Europe, North Africa/Middle East, Sub Saharan Africa, South East Asia, North East Asia, South/Central Asia, Americas vs. 149,737Australian-born (non-indigenous). |
M overall (not statistically tested) H & ND emerg (unadjusted) M elect (unadjusted) |
Fair |
| Walsh J, Robson M, & Foley M. (2009) (English) Conference abstract |
Local, hospital records, 2008 |
Ireland (Dublin) |
931 Eastern Europe, Africa, Britain, India, China vs. 2499 Irish women. Only primiparous women, and delivered singleton, term infants. |
M caesarean during labour (unclear if statistically significant) |
Fair |
| Walsh J, Mahony R, Armstrong F, Ryan G, O’Herlihy C, & Foley M. (2011) (English) |
Local, hospital records, 2008 |
Ireland (Dublin) |
552 Eastern European vs. 2449 Irish women. Primiparous, singleton, term deliveries for women who laboured. |
ND caesarean during labourb (adjusted) ND caesarean pre-labour (excluded group from study) |
Good |
| Ryan G, Armstrong F, Walsh J & Foley M. (2010) (English) Conference abstract | |||||
| Walsh J, Mahony R, McAuliffe F, O'Herlihy C, Robson M, & Foley M. (2009) (English) Conference abstract | |||||
| Yoong W, Wagley A, Fong C, Chukwuma C, & Nauta M. (2004) (English) |
Local, hospital records, 2002 |
UK (North London) |
61 Kosovo-Albanian vs. 61 British Caucasian. |
ND overall (unadjusted) |
Fair |
| Yoong W, Kolhe S, Karoshi M, Ullah M, & Nauta M. (2005) (English) |
Local, research study, 2002 |
UK (North London) |
69 Somali vs. 69 British Caucasian. |
ND overall (unadjusted) |
Fair |
| Zanconato G, Lacovella C, Parazzini F, Bergamini V, & Franchi M. (2011) (English) |
Local, hospital records, 2005-2009 |
Italy (Verona) |
2661 “Immigrants" defined as 5 ethnic minority groups based on geographical location: Sub-Saharan Africa, Central & Eastern Europe, Middle East & North Africa, Central and South America, South and East Asia vs. 6365 Italian women; singleton births only. |
M overall (adjusted for age but not parity) H & ND caesarean during labour (adjusted for age but not parity) M caesarean pre-labour (not statistically tested) |
Fair |
| Zlot AI, Jackson DJ, & Korenbrot C. (2005) (English) |
Local, hospital records, 1994-1998 |
US (San Diego) |
1789 Mexican-born (categorized into acculturation groups by language ability- English, Spanish and bilingual) vs. 313 US born Latina women. Only includes low-risk, low income women. |
H & ND (primips) & L & ND (multips) overall; (adjusted) |
Good |
| Zuppa AA, Orchi C, Calabrese V, et al. (2010) (English) | Local, research study, 2005 | Italy (Rome) | 585 “Immigrants” (includes women from Latin America, East Europe, West Europe, Russia, North America, Asia, Africa) vs. 2334 Italian-born. | L overall (all immigrants combined; unadjusted) | Fair |
* For “overall”, “emerg” and “elect” caesarean rates for different migrant groups (defined by country/region of birth, migration status, ethnicity, length of time in new country &/or language ability) compared to non-migrants: H= Higher rate(s); L= Lower rate(s); ND = No Different rate(s); M= Mixed (Higher & Lower rates or Higher, Lower & No Different rates); ‘adjusted’ if at minimum controlled for parity and age. Presented by parity (primiparous = primips; multiparous= multips) &/or age if ‘unadjusted’ and reported.
† Additional data provided.
Table 2.
Summary of study characteristics
| Characteristic | n (number of studies) | % |
|---|---|---|
|
Language of publication |
(n=76) |
|
| English |
62 |
81.6 |
| French |
4 |
5.3 |
| Italian |
3 |
5.3 |
| Spanish |
1 |
2.6 |
| Norwegian |
2 |
3.9 |
| German |
4 |
1.3 |
|
Publication period |
(n=76) |
|
| < 1980 |
9 |
11.8 |
| 1980-1989 |
6 |
7.9 |
| 1990-1999 |
13 |
17.1 |
| 2000-2012 |
45 |
59.2 |
| Unpublished |
3 |
3.9 |
|
Data Sources |
(n=76) |
|
| Population-based data registries |
21 |
27.6 |
| Population-based hospital data |
2 |
2.6 |
| Population-based surveys |
4 |
5.3 |
| Research study/hospital records |
49 |
64.5 |
|
Variables adjusted |
(n=19)* |
|
| Maternal age |
19 |
100 |
| Parity |
17 |
89.5 |
| Education |
7 |
36.8 |
| Gestational age |
8 |
42.1 |
| Marital status |
3 |
15.8 |
| Prenatal care |
3 |
15.8 |
| Social economic status (poverty, income, under-housing, occupation) |
4 |
21.1 |
| Birthweight |
9 |
47.4 |
| Medical complications |
2 |
10.5 |
| Mechanical factors |
1 |
5.3 |
| Previous caesarean |
1 |
5.3 |
| Pregnancy complications (multiple, preterm, fetal stress) |
3 |
15.8 |
| Smoking & substance abuse |
1 |
5.3 |
| Medical indications |
2 |
10.5 |
| Onset of labour |
1 |
5.3 |
| Maternal weight/BMI/diabetes |
5 |
26.3 |
| Assisted reproductive technology |
2 |
10.5 |
| Infant sex |
4 |
21.1 |
| Hospital characteristics (level of care, size of hospital, private facility) |
5 |
26.3 |
| Insurance status |
2 |
10.5 |
| Birth year |
1 |
5.3 |
| Time of day |
1 |
5.3 |
| Location of institution |
2 |
10.5 |
|
Coverage |
(n=75)† |
|
| National |
15 |
19.7 |
| Regional |
12 |
15.8 |
| Local |
49 |
64.5 |
|
Data years |
(n=75)‡ |
|
| < 1980 |
12 |
12.6 |
| 1980–1989 |
17 |
17.9 |
| 1990–1999 |
28 |
29.5 |
| 2000-2010 |
38 |
40.0 |
|
Number of migrants studied |
(n=74)§ |
|
| < 1,000 |
32 |
43.2 |
| 1,000-5,000 |
23 |
31.2 |
| > 5,000-10,000 |
5 |
6.8 |
| >10,000 |
14** |
18.9 |
|
Source regions |
(n=1,029,454)†† |
|
| Sub-Saharan Africa |
66,163 |
6.4 |
| North Africa/West Asia |
65,689 |
6.4 |
| Latin America & Caribbean |
404,729 |
39.3 |
| North America/Australia |
8855 |
0.9 |
| East Asia |
68,084 |
6.6 |
| South-East Asia |
69,589 |
6.8 |
| South Asia |
70,545 |
6.9 |
| Asia (unspecified) |
46,842 |
4.6 |
| Oceania (unspecified) |
18,005 |
1.7 |
| East Europe |
27,922 |
2.7 |
| North/West Europe |
58,065 |
5.6 |
| South Europe |
16,336 |
1.6 |
| Unspecified |
108,630 |
10.6 |
|
Receiving countries |
(n= 76)‡‡ |
|
| Australia |
9 |
11.1 |
| Belgium |
2 |
2.5 |
| Canada |
5 |
6.2 |
| Finland |
2 |
2.5 |
| France |
6 |
7.4 |
| Germany |
4 |
4.9 |
| Greece |
3 |
3.7 |
| Holland |
2 |
2.5 |
| Ireland |
3 |
3.7 |
| Israel |
3 |
3.7 |
| Italy |
9 |
11.1 |
| Norway |
10 |
12.3 |
| Portugal |
1 |
1.2 |
| Spain |
3 |
3.7 |
| Sweden |
3 |
3.7 |
| Switzerland |
1 |
1.2 |
| UK |
6 |
7.4 |
| US |
9 |
11.1 |
|
Quality of reports |
(n=76) |
|
| Good |
22 |
28.9 |
| Fair |
54 |
71.1 |
|
Caesareans |
(n=64)§§ |
|
| Higher |
13 |
20.3 |
| Higher/No different |
12 |
18.8 |
| Lower |
9 |
14.1 |
| Lower/No different |
2 |
3.1 |
| Mixed |
8 |
12.5 |
| No different |
20 |
31.3 |
|
Emergency caesareans |
(n=21)*** |
|
| Higher |
7 |
33.3 |
| Higher/No different |
4 |
19.0 |
| Lower |
0 |
0.0 |
| Lower/No different |
0 |
0.0 |
| Mixed |
0 |
0.0 |
| No different |
10 |
47.6 |
|
Elective caesareans |
(n=19)*** |
|
| Higher |
2 |
10.5 |
| Higher/No different |
3 |
15.8 |
| Lower |
5 |
26.3 |
| Lower/No different |
2 |
10.5 |
| Mixed |
1 |
5.3 |
| No different | 6 | 31.6 |
* Texeira 2010 did not specify variables controlled so excluded; each study may have controlled for more than one variable so total does not equal 19 (or 100%).
† Texeira 2010 did not specify area of coverage; Small 2008 contained regional and national data coverage and so is counted twice.
‡ Texeira 2010 did not specify year(s) of data; total adds to more than 74 since a report may have data from more than one time period.
§ Number of migrants not provided in Giani 2011 and Parsons 1993.
** Kinston 2011 used weighted numbers.
†† Total number of migrants studied across reports (overlap accounted for).
‡‡ Small 2008 studied migrants in 6 receiving countries.
§§ Giani 2011, Ismail 2011, Le Ray 2006, Walsh, Robson & Foley 2009 and Walsh 2011 are excluded due to lack of data for overall caesarean rates; Studies where rates are not statistically compared are also excluded. Small 2008 was counted as 6 studies since results for 6 receiving countries were reported.
*** Studies where rates are not statistically compared are excluded.
Across the 76 studies, data were reported on 1,029,454 migrants (see Table 2). The most common source regions represented were Latin America & Caribbean (39%) followed by ‘origin unspecified’ (11%) and South Asia (7%) (see Table 2). Region and country of origin were the migration indicators most often used to report caesarean rates (57 of 76 studies). “Foreign-born” was used in 16 studies; ethnicity/race/religion/language, length of time and migration status (e.g., “refugees”), were also used in five, three and nine studies respectively.
The receiving countries included Europe (68%), Australia (11%), the US (11%), Canada (6%) and Israel (4%). The primary language of publication was English (82%). Data sources were population-based in 36% of studies, and coverage for the majority (65%) of studies was one city (in most cases one hospital). Data were gathered from 1956 to 2010; 70% from the 1990s or later. More than half of the studies were published from 2000 onward (see Table 2).
Caesarean Birth Rates: Migrants vs. Non-migrants
Comparison of caesarean rates overall between migrants and non-migrants revealed that in 69% of the studies there were differences in caesarean rates between the two groups (see Table 2). For emergency caesareans, more than half of the studies showed migrants to have higher rates or higher and no different compared to receiving-country-born whereas for elective caesareans there was more variation: 26% showed higher rates or higher and no different; 37% showed lower rates or lower and no different and 5% of studies had mixed results (see Table 2).
Meta-analyses
Sub-Saharan Africa (or Africa unspecified)
African migrants had an excess of caesareans compared to receiving-country-born women: France [OR=2.22, (95% CI=1.92, 2.58)] [17,31,94], Australia [OR=1.17 (95% CI=1.11, 1.24)] [34,91]; Canada [OR=1.34 (95% CI=1.08,1.67)] [64,95] and North/West Europe [OR=1.43 (95% CI=1.16, 1.77)] [16,46,82]. US [37,57,81] and Southern European [25,26,88] studies were too heterogeneous to combine, but tended towards higher rates. Analysis by parity showed primiparous African women to be more likely to have a caesarean [OR=2.24 (95% CI=1.63, 3.08)] [31,33,46,64] than non-migrants see Figure 1; multiparous women were also at increased risk [OR=2.02 (95%CI=1.51, 2.71)] [31,46].
Figure 1.
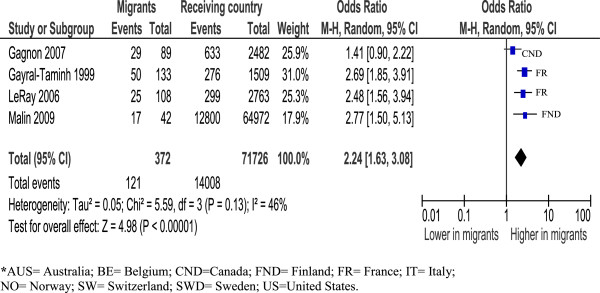
Sub-Saharan Africa primiparous women, overall caesareans.
Analysis by type of caesarean suggests an excess risk of emergency caesareans for Sub-Saharan African women (all estimates above 1), although results were heterogeneous [17,31,33,64,82,88,91,94]. Risks for elective caesareans varied by receiving-country; three studies in France [17,31,94], one in Italy [88] and another in Australia [91] showed higher risks of a planned caesarean, while two other studies, one in Canada [64] and the other in Norway [82], found African women to have the same and lower risk respectively.
Somali women in North America and Australia were found to have higher risks for a caesarean compared to non-migrant women [OR=1.13 (95% CI=1.02, 1.26)] [32,45]. Significant heterogeneity prevented the calculation of a summary estimate for Somali women in Europe, though the tendency appeared similar to North America/Australia results.
Sub-analysis by parity shows primiparous Somali women to have greater risk for caesarean [OR=1.45 (95% CI=1.30, 1.62)] [32,45] (see Figure 2). Multiparous Somali women also appear at increased risk however there was considerable heterogeneity preventing calculation of a summary estimate [32,45]. There were insufficient data for meta-analysis by type of caesarean in Somali women.
Figure 2.
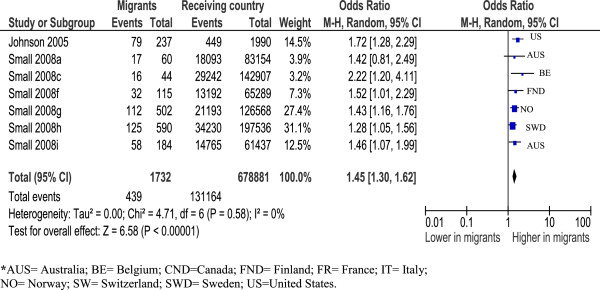
Somali primiparous women, overall caesareans.
North Africa (Maghreb)/West Asia (Middle East) (most studies reported results for North-Africa and West Asia combined)
Sub-group analyses by receiving-country showed lower risk of a caesarean in Canada [OR=0.81 (95% CI=0.74, 0.90)] [64,97] and similar risk in France: [OR=1.09 (95% CI=0.95, 1.26)] [17,31,56,73,94]. Analysis for other countries/regions yielded heterogeneous results. With respect to type of caesarean, North African/West Asian migrant women had an elevated risk if the caesarean was an emergency [OR=1.11 (95% CI=1.03, 1.20)] [15,17,31,33,64,88,91,94].
Latin America
Differences in caesarean rates between Latin American migrants and non-migrant women depended on receiving-country. Rates were higher in Norway [OR= 2.41 (95%CI=1.79, 3.23)] [15,82], and Canada [OR=1.43(95% CI=1.29, 1.59)] [64,97], whereas in Southern Europe rates were similar [OR=1.03 (95% CI=0.94,1.12)] [26,53,88]. Results in other receiving countries were too few or heterogeneous to combine. Latin American women showed greater risk for an emergency caesarean compared to non-migrant women [OR=1.59(95% CI=1.13, 2.25)] [15,64,82,88]. Results for elective caesareans were too heterogeneous for calculation of a summary estimate.
Caribbean (non-Hispanic)
Three older European studies provided data for migrants from former colonized Caribbean states (Holland, UK, France) and combined showed these women were more likely to have caesarean than non-migrants [OR=1.91 (95% CI=1.37, 2.66)] [72,73,78].
South Asia
Combining studies with similar populations (India, Sri Lanka, unspecified) show these migrant women have an excess of caesareans compared to receiving-country-born women [OR=1.28 (95% CI=1.22, 1.35)] (see Figure 3) [15,16,26,46,58,61,97]. Examined by parity, both primiparous and multiparous women had more caesareans [OR=1.19 (95% CI=1.12, 1.25) and OR=1.39 (95% CI=1.31, 1.47) respectively] [46,61] . Studies for emergency caesareans were too heterogeneous, and there were insufficient data to examine elective caesareans.
Figure 3.
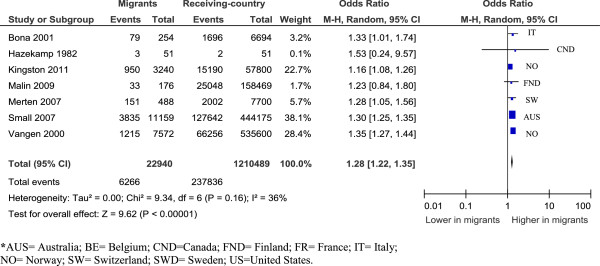
South Asian women, overall caesareans.
East Asia (“Far East”)
East Asian women in Southern Europe and the US are less likely to have a caesarean:[OR=0.59, (95% CI=0.47, 0.73)] [25,26] and [OR=0.73 (95% CI=0.71,0.75)] [37,81] respectively, whereas East Asian women in Australia, the UK, Canada and Finland had similar rates to non-migrant women [OR=0.99 (95%CI= 0.95,1.03)] [46,61,91,93,97].
Sub-analysis of three studies of Chinese women [46,61,93] show no difference between migrant and non-migrant women overall [OR=0.97 (95% CI=0.75, 1.25)], for primiparous women [OR=0.93(95%CI=0.86,1.00)] or for multiparous women [OR=1.02 (95% CI=0.95,1.10)] [46,61].
South-East Asia
Despite significant heterogeneity, migrant women from Vietnam, Thailand, Cambodia, and Laos had lower risks of caesarean compared to non-migrant women in all nine included studies [15,16,37,46,48,49,51,60,61]. Focusing on Vietnamese women, two older studies found Vietnamese to have caesarean rates lower than Australian-born [OR= 0.87 (95% CI=0.75, 1.00] [49,60]. Similarly more recent studies showed Vietnamese women to have lower rates compared to non-migrant women [OR=0.68 (95% CI=0.66, 0.71)] [16,46,61]. Results were consistent for primiparous [OR=0.78 (95% CI=0.64, 0.94)] and multiparous [OR=0.65(95% CI=0.62, 0.68)] women [46,49,61].
Contrary to other South East Asian women, Filipino women tended towards a greater risk for caesarean birth, although heterogeneity prevented calculation of a summary point estimate [15,16,28,39,49,52,61]. Two Australian studies show multiparous Filipino women to have higher rates [OR=1.19 (95% CI=1.10,1.29)] [49,61].
Eastern Europe
Results of studies reporting comparisons of Eastern European women to receiving-country-born are too heterogeneous to calculate a summary point estimate but suggest these women have lower risks for caesarean, with all estimates lower or tending to be lower than one [26,46,53,82,88,97]. Analysis specifically of primiparous women confirmed a reduced risk [OR= 0.52, (95%CI=0.43, 0.63)] [46,87,96]. A sub-analysis of Kosovo women [OR=0.49, (95% CI=0.36, 0.67)] [16,43] and women from Russia/Baltic States living in Europe (Switzerland and Finland) also showed these women to have lower risks [OR=0.75, (95% CI=0.66, 0.85)] [16,46].
Southern Europe
Comparisons of women from Italy, Portugal, Spain, and Greece migrating to other parts of Europe or Australia were heterogeneous although the risks of caesarean were consistently greater than that of receiving-country-born women [16,52,56,61,63,68,73].
Other
Analyses by other migration indicators (migration status and length of time in receiving-country) were possible for migrants in Canada only. These included an analysis of asylum-seekers who showed no difference in rates compared to Canadian-born [OR=0.93 (95% CI=0.74, 1.17)] [64,66,95]; and migrant women in Canada five years or less who showed a greater risk for caesarean [OR=1.14 (95%CI=1.06, 1.23)] [64,66,97].
Sensitivity analyses
Meta-analyses with population-based studies confirmed the findings with consistent results for Sub-Saharan African women in France [OR=2.19 (95% CI=1.80,2.67)] [17,94], and South Asian women [OR=1.25 (95% CI=1.17, 1.33)] [16,26,46,61,97]. Sensitivity analyses also support the findings of higher risk of emergency caesareans for North-African/West Asian women [OR=1.09 (95% CI= 1.00,1.19)] [15,17,91,94] and lower risk of caesareans for Eastern European women (heterogeneous but similar estimate). Sensitivity analyses were not informative for Somali and Vietnamese migrants since all studies initially meta-analyzed were population-based, and for Latin American migrants due to an insufficient number of studies.
Summary estimates of adjusted ORs for overall caesarean rates for Sub-Saharan African [OR=1.41 (95%CI=1.19, 1.66)] [16,65,88,95] and Somali women [OR=1.99 (95% CI=1.44, 2.75)] [16,32,41] were consistent in showing higher rates of caesarean compared to non-migrant women. Inconsistent findings were found however when adjusted meta-analyses were performed for South Asian and Latin American migrants; South Asian women still tended towards higher rates but with a wide, non-significant confidence interval [OR=1.10 (95%CI=0.87, 1.38)] [16,95] and Latin American women showed no difference in emergency caesarean rates compared to non-migrant women [OR=1.01 (95% CI=0.62, 1.63)] [82,88]. Adjusted analyses for emergency caesareans in North-African/West Asian women showed a similar point estimate to the unadjusted analyses but with a wide, non-significant confidence interval [OR=1.16 (95% CI=0.86,1.56)] [17,88]. Adjusted results for Eastern European women were too heterogeneous, but did generate a similar estimate to the unadjusted results.
Assessment for publication bias
Visual inspection of the individual funnel plots for studies reporting overall caesarean rates for Sub Saharan African, Somali, South Asian, Eastern European, Vietnamese, Latin American and North African/West Asian migrants (and emergency caesareans for the two latter) all showed symmetry, suggesting no publication bias, although very small studies were generally lacking.
Mechanisms/indications for caesareans among migrant women
Table 3 summarizes important risk factors/mechanisms for caesareans in migrants cited in included studies and for each factor the number of studies citing this factor/mechanism. Combined the most commonly reported (in order of frequency) were: language/communication barriers, low social economic status (SES), poor maternal health (e.g., anaemia, STIs, TB, parasitic infections), gestational diabetes/high body mass index (BMI), feto-pelvic disproportion, and lack of prenatal care.
Table 3.
Potential mechanisms & risk factors involved in caesareans among migrants
| Mechanism/Risk factor* | Number of studies |
|---|---|
|
Income and social status | |
| Low SES (education, income) |
15 |
| Higher social status |
5 |
| No legal status |
2 |
| Poor nutritional status |
1 |
|
Social support networks | |
| No partner and/or family, friends |
4 |
|
Education and literacy | |
| High education |
3 |
|
Employment and working conditions | |
| Low status job |
1 |
|
Social environment | |
| Poor living conditions |
2 |
|
Physical environment | |
| Violence, trauma or experiences of abuse |
1 |
|
Personal health practices | |
| High BMI &/or Gestational diabetes/diabetes |
12 |
| Smoking, drug or alcohol abuse |
1 |
|
Healthy child development | |
| Fetal distress |
6 |
| Low birthweight |
3 |
| Prematurity |
2 |
|
Biology and genetic endowment | |
| Illness and other pathologies (e.g., anaemia, hepatitis, TB, malaria, HIV/STIs, parasitic or other infections) |
14 |
| Pelvis shape/size (feto-pelvic disproportion) |
13 |
| Older age |
7 |
| Short stature |
4 |
| Pre-eclampsia/hypertension |
4 |
| Prolonged labour/failure to progress |
3 |
| Post-datism |
3 |
|
Health services | |
| Language/communication barriers |
18 |
| Lack of healthcare including prenatal care |
10 |
| Discrimination/racism |
1 |
| Hospital environment |
1 |
|
Gender | |
| Genital cutting |
7 |
|
Culture | |
| Beliefs/preferences about birth |
8 |
| Grand-multiparity |
8 |
| Inter-racial marriage (leading to large birthweight babies) |
4 |
| Acculturation (adoption of unhealthy lifestyles) |
3 |
| Different concepts of health and disease (leading to different health seeking behaviour) |
2 |
| Reduced food intake during pregnancy (to have a smaller fetus) | 1 |
* Mechanisms/Risk Factors are organized under 12 determinants of population health (Public Health Agency of Canada (PHAC). Immigration and Health-Exploring the Determinants of Health. Ottawa: Public Health Agency of Canada; 2011).
Evidence to explain the consistently different rates of caesarean between Sub Saharan African, Somali, South Asian, Vietnamese, Eastern European, Latin American and North African/West Asian (emergency caesareans for the two latter) and non-migrant women, was limited. Variables adjusted (see Table 2) or stratified differed across studies and few studies compared indications for caesarean between migrant and non-migrant groups making it difficult to draw firm conclusions regarding explanatory risk factors or mechanisms.
For Somali [15,16,32,41] and Sub-Saharan African [16,17,82,88,95] migrants, adjusted analyses indicate factors other than maternal age, parity, birthweight, or medical complications [e.g., preterm, feto-pelvic disproportion, hypertension, diabetes, BMI] are involved, although it is difficult to know which factors. Prolonged labour due to pelvic shape [17,31,71], genital cutting [15,32,41,45,46,57,88], language barriers [15-17,32,45], poor maternal health (e.g., infectious diseases, anaemia) [31,46,65], a lack of prenatal care [16,33], and low SES [16,31,32] have all been postulated to be important mechanisms for these women. Gestational diabetes mellitus (GDM) and dystocia were also mentioned as a concern for Sub-Saharan African/Somali women (more than receiving-country-born women) in some studies [32,34,46].
Reports that provided comparisons of medical indications for caesareans between Sub-Saharan African/Somali and non-migrant women show these women to have more caesareans due to fetal distress [31,32] and failed induction [32]. Similarly one study found Sub-Saharan African women who were induced to be more likely to have a caesarean compared to French women who were induced [17], suggesting complications with labour that could be due to any number of different reasons.
Adjusted analyses for South Asian [15] and Latin American (emergency caesareans) [82,88] migrants show age, parity or medical complications (e.g., feto-pelvic disproportion, fetal distress) partially explain excess caesareans in these women, although it is not possible to isolate which of these factors is important. For Latin American women, studies which show consistently higher rates of caesarean irrespective of adjustment of covariates or stratification (e.g., birthweight, hospital type) suggest different contributing factors [15,27,53,65,95]. Seeking social status [55]or cultural preference [15,46,53,95] is one suggested cause; higher rates of pre-eclampsia might also have a role [46]. Stratified analyses by neighbourhood (English-speaking and non-English-speaking) have shown higher rates of caesarean for Latinas compared to US-born when living in non-English-speaking neighbourhoods, leading to the suggestion that communication or cultural barriers might be explanatory mechanisms [27].
For North African/West Asian migrants, hypothesized mechanisms leading to caesarean birth included illness (e.g., hypertension, diabetes) [73], low SES resulting in reduced access to prenatal care [33,73], language barriers [56], and macrosomia [29,70].
Vietnamese [15] and Eastern European [53,87,96] migrants seem to have protective factors that explain their consistently lower rates of caesarean. Proposed protective factors include a preference for a vaginal birth [15,87]; the healthy-immigrant effect (i.e., in which immigrants are healthier than the native population due to immigration selection criteria which excludes individuals with significant health problems) [87,93]; a healthier lifestyle (no smoking, drinking alcohol, or drug abuse; low BMI) [87,96]; young maternal age [87,96]; social support [16] and the use of fewer interventions during labour and birth [87,96]. In Southern Europe (Italy, Spain, Portugal), lower rates among migrants are also thought to be due to a preference for caesareans among non-migrant women [30,50] and because healthcare professionals are more concerned about litigation [25,36,86] from non-migrants.
Filipino migrants were explicitly discussed in a number of studies and hypotheses for their higher caesarean rates included maternal preference [15,39] and feto-pelvic disproportion due to interracial marriage resulting in large birthweight babies [15,28,39,49,52]. More caesareans due to dystocia and feto-pelvic disproportion have been shown, however, this was deemed to not be due to interracial marriage (by comparing Filipino women in mixed marriages to Filipino women in non-mixed marriages) [28,39]. Filipino women who gave birth by caesarean were also found to experience a greater number of medical and obstetric complications (e.g., GDM, anaemia, viral diseases) compared to Australian-born women who delivered by caesarean [28].
Discussion
Our review of 76 studies comparing the rates of caesarean births between migrant and non-migrant women living in OECD countries, show that women from Sub-Saharan Africa, Somalia and South Asia consistently have an excess of caesareans compared to receiving-country-born women while Eastern European and Vietnamese women have lower overall caesarean rates. North African/West Asian and Latin American women have higher emergency caesarean rates.
The literature provides inadequate empirical evidence to explain differences in caesarean rates observed. Overall it appears that a combination of factors and mechanisms are likely to be involved. The most frequently postulated risk factors for caesarean risk in migrant populations include: language/communication barriers, low SES, poor maternal health, gestational diabetes/high BMI, feto-pelvic disproportion, and lack of prenatal care. There were no studies identified examining determinants of caesareans in migrants specifically. However, gestational diabetes mellitus (GDM) and feto-pelvic disproportion are known to complicate delivery and increase the risk of caesarean [104,105] and these are more common in some migrant women [28,39,106]. Reasons for increased risk of GDM in migrants are unknown but might be associated with a genetic pre-disposition, or physiological response to dietary changes; the involvement of a stress response has also been proposed. Feto-pelvic disproportion might be the result of short stature, a large birthweight baby or childhood malnutrition [107].
A BMI above normal is associated with a number of adverse reproductive outcomes, including GDM, macrosomia, prolonged labour, pre-eclampsia and caesarean [108,109], although the exact mechanisms have not been identified. Excessive weight among childbearing women also varies by ethno-cultural background, with African women representing one of the groups with the highest rates of obesity [94,110].
Inadequate prenatal care is more common among migrants [111]. Language and no health insurance are often cited barriers to healthcare [11,112]. Women who do not receive prenatal care, or who cannot communicate their medical history, may have undiagnosed and untreated medical conditions and they do not benefit from other preventative interventions (e.g., advice about prenatal nutrition) [113]. Medical issues that may not be identified include parasitic infections, anaemia and TB which are known to affect some childbearing migrant women [114-116], although their association with caesarean birth is unclear.
Poverty, unemployment and low social status are significant concerns for migrants [117,118]. Low SES may indirectly be protective against caesarean since women of low SES are less likely to receive care in a private facility and there may be less concern of litigation among healthcare professionals caring for these women. However, low SES may be a barrier to accessing prenatal care, and is known to be independently associated with poorer health. Qualitative studies suggest that a lack of information and/or support during pregnancy and birth due to marginalization, communication barriers, and/or cultural insensitivity (e.g., genital cutting), may result in anxiety, fear and disempowerment [119,120] and lead to unnecessary caesareans.
Confirmation and further understanding of social support as a protective mechanism could have positive implications for reducing caesarean rates among migrants. Additional support (in addition to routine care) including emotional support as well as practical assistance provided during pregnancy has been shown to reduce the risk of caesarean birth for women in socially disadvantaged situations [121]. Continuous support during labour is also associated with a reduced risk of caesarean [122]. This strategy may be particularly beneficial for reducing emergency caesareans, which overall appear to be more common among migrants.
Our findings also suggest that receiving-country is an important variable to consider, particularly for certain groups (e.g., North African, Latin American, East Asian). The degree to which variation in caesarean outcomes across countries represents effects of policies and/or healthcare delivery [123] or other particularities of receiving countries (e.g., cultural factors) versus differences in the migrant populations resettling in each country, remains unknown. More precise definitions of migrants and more complete individual level migration-related data, including source country, length of time in host country, receiving-country language ability (at the time of pregnancy and birth), and migration status (e.g., refugee or economic immigrant) [124] would allow for better interpretation of results particularly since results from Canadian studies have shown that length of residence post-migration (< 5 years) was a significant predictor of more caesarean births. Confirmation of these findings in other OECD countries would be informative.
Research to establish evidence for risk factors associated with caesarean birth in migrants and to deconstruct the pathways (e.g., genetic or physiological, psychological stress, delivery of maternity care) by which they lead to disparities in mode of birth outcomes, is needed. Pathways are likely multi-factorial and complex. Future work using a combination of quantitative and qualitative approaches may be valuable in more fully expounding the processes. Moreover, greater b on differences in caesarean indications/mechanisms would be more informative than simply comparing caesarean rates between migrant and non-migrant women since rates may not be higher, but there may still be disparities in risk factors for caesarean births.
Strengths and limitations
There are limitations to this review. The web searches, although extensive, did not include all of the government and professional agency websites from all OECD countries. The majority of included studies were rated as ‘fair’ quality for not controlling for confounding or due to some ambiguity in their definitions of the study groups. The heterogeneity due to variation in the migrant populations studied or how source countries were grouped to represent regions, made it challenging to combine data for meta-analysis. US studies were largely missing from meta-analyses due to heterogeneity (for Sub-Saharan African women) or lack of data for the source regions analyzed (for Eastern European, Vietnamese, South Asian, Latin American and North-African/West Asian women). This might be problematic since other systematic reviews comparing the perinatal health of migrants to non-migrants [125,126] had varied outcomes between US and European regions. Nonetheless, a broad range of studies was included and analyzed; the database searches were exhaustive with no time or language limitations and only three reports could not be reviewed due to language. Rigorous methods for reviewing, extracting and analyzing data were applied, optimizing the quality of the results generated. The consistency of the results with population-based data offers confidence in the robustness of the findings.
A major strength of this review is that it is the first of which we are aware to systematically examine hypotheses put forward to explain differences in caesarean rates between migrant and non-migrant women and to assess these in light of the available empirical evidence.
Conclusion
Sub-Saharan African, Somali, and South Asian migrants consistently have higher caesarean rates while Eastern-European and Vietnamese migrants have lower overall caesarean rates compared to receiving-country-born women. North-African/West Asian and Latin American migrant women have higher emergency caesarean rates. To date there is inadequate empirical evidence to explain observed differences in caesarean rates; more focused research is urgently needed.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
LM reviewed the literature, extracted data, performed analyses and wrote the first draft of the paper. AG conceived the study, reviewed literature, and critically revised the manuscript for important intellectual content. RS and BB contributed to the design of the study and critically revised the manuscript for important intellectual content. All authors approved of the final version of the paper to be published.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Supplementary Material
Database search strategy.
Websites searched.
UN Macro Regions.
Contributor Information
Lisa Merry, Email: lisa.merry@mail.mcgill.ca.
Rhonda Small, Email: r.small@latrobe.edu.au.
Béatrice Blondel, Email: beatrice.blondel@inserm.fr.
Anita J Gagnon, Email: anita.gagnon@mcgill.ca.
Acknowledgements
The ROAM (Reproductive Outcomes and Migration) collaboration for locating relevant literature and providing assistance to review non-English reports. Luisa Ciofani (McGill University Health Centre & Canadian Association of Perinatal and Women’s Health Nurses (CAPWHN)); Vyta Senikas (Society of Obstetricians and Gynaecologists of Canada (SOGC)); and Emmanuelle Hébert (Canadian Association of Midwives (CAM) for their professional input to the manuscript.
Funding
Canadian Institutes of Health Research (CIHR) provided funds to support the research (FRN: 103265). The McGill University Health Centre- Research Institute provided research space and administrative support. Lisa Merry holds a FRSQ (Fonds de Recherche Santé Québec) Doctoral training award and a FRESIQ (Fondation de recherche en sciences infirmières du Québec) doctoral bursary through their MELS Universities’ program and is also funded by the Strategic Training Program in Global Health Research, a partnership of the Canadian Institutes of Health Research and the Québec Population Health Research Network.
References
- Betrán AP, Merialdi M, Lauer JA, Bing Shun W, Thomas J, Van Look P, Wagner M. Rates of caesarean section: analysis of global, regional and national estimates. Paediatr Perinat Epidemiol. 2007;21:98–113. doi: 10.1111/j.1365-3016.2007.00786.x. [DOI] [PubMed] [Google Scholar]
- Deneux-Tharaux C, Carmona E, Bouvier-Colle MH, Bréart G. Postpartum maternal mortality and cesarean delivery. Obstet Gynecol. 2006;108:541–548. doi: 10.1097/01.AOG.0000233154.62729.24. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Appropriate technology for birth. Lancet. 1985;2:436–437. [PubMed] [Google Scholar]
- United Nations, Department of Economic and Social Affairs, Population Division. Trends in International Migrant Stock: The 2008 Revision (United Nations database, POP/DB/MIG/Stock/Rev.2008) New York: United Nations; 2009. Available at: http://www.un.org/esa/population/publications/2009Migration_Chart/ittmig_wallchart09.pdf. [Google Scholar]
- Statistics Canada. Canada's demographic situation: Fertility of immigrant women. The Daily. 2003. Monday, December 22. Available at: http://www.statcan.gc.ca/daily-quotidien/031222/dq031222c-eng.htm.
- Sobotka T. Overview Chapter 7: the rising importance of migrants for childbearing in Europe. Demographic Research. 2008;19:225–248. [Google Scholar]
- World Health Organization. Health of Migrants -The Way Forward: report of a global consultation, Madrid, Spain, 3-5 March 2010. Geneva: World Health Organization Press; 2010. Available at: http://www.who.int/hac/events/consultation_report_health_migrants_colour_web.pdf. [Google Scholar]
- International Organization for Migration (IOM) International Migration Law - Glossary on Migration. 2. Geneva: IOM; 2011. [Google Scholar]
- United Nations High Commissioner for Refugees (UNHCR) Refugee Status Determination, Identifying who is a refugee. Geneva: UNHCR; 2005. [Google Scholar]
- Fuentes-Afflick E, Hessol NA. Immigration status and use of health services among Latina women in the San Francisco Bay Area. J Womens Health. 2009;18:1275–1280. doi: 10.1089/jwh.2008.1241. [DOI] [PubMed] [Google Scholar]
- terKuile S, Rousseau C, Munoz M, Nadeau L, Ouimet MJ. The universality of the Canadian health care system in question: Barriers to services for immigrants and refugees. Int J Migr Health Soc Care. 2007;3:15–26. doi: 10.1108/17479894200700003. [DOI] [Google Scholar]
- Eisenman DP, Keller AS, Kim G. Survivors of torture in a general medical setting: how often have patients been tortured, and how often is it missed? West J Med. 2000;172:301–304. doi: 10.1136/ewjm.172.5.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carballo M, Nerukar A. Migration, refugees, and health risks. Emerg Infect Dis. 2001;7(3 Suppl):556–560. doi: 10.3201/eid0707.017733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagnon AJ, Zimbeck M, Zeitlin J. Migration to western industrialized countries and perinatal Health: A systematic review. Soc Sci Med. 2009;69:934–946. doi: 10.1016/j.socscimed.2009.06.027. [DOI] [PubMed] [Google Scholar]
- Vangen S, Stoltenberg C, Skrondal A, Magnus P, Stray-Pedersen B. Cesarean section among immigrants in Norway. Acta Obstet Gyn Scan. 2000;79:553–558. doi: 10.1080/j.1600-0412.2000.079007553.x. [DOI] [PubMed] [Google Scholar]
- Merten S, Wyss C, Ackermann-Liebrich U. Caesarean sections and breastfeeding initiation among migrants in Switzerland. Int J Public Health. 2007;52:210–222. doi: 10.1007/s00038-007-6035-8. [DOI] [PubMed] [Google Scholar]
- Roman H, Blondel B, Bréart G, Goffinet F. Do risk factors for elective cesarean section differ from those of cesarean section during labor in low risk pregnancies? J Perinat Med. 2008;36:297–305. doi: 10.1515/JPM.2008.044. [DOI] [PubMed] [Google Scholar]
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, Atkins D. Methods Work Group, Third US Preventive Services. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20(3 Suppl):21–35. doi: 10.1016/s0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Green S, editor. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011] 2011. (The Cochrane Collaboration). Available at: http://handbook.cochrane.org/ [Google Scholar]
- Centre for Epidemiology and Research NSW Department of Health. New south wales mothers and babies 2008. NSW Public Health Bull. 2010;21 [Google Scholar]
- van Enk W, Gorissen W, van Enk A. Tienerzwangerschappen naar etniciteit in Nederland, 1990-1993. Ned Tijdschr Geneeskd. 1999;143:465–471. [PubMed] [Google Scholar]
- Herpola O. Indications for caesarean section. Duodecim. 1947;63:25–30. [Google Scholar]
- Wittlinger H, Beck HO, Brandner U. Geburtshilfe Frauenheilkd. 1971. pp. 1174–1183. [PubMed]
- Alonso CP, Maresca MI, Alonso OT, Moro SM. Perinatology of newborns of immigrant parents at Hospital Clinico 'San Carlos' in Madrid, Spain. Acta Pediatr Esp. 2006;64:61–67. [Google Scholar]
- Bona G, Zaffaroni M, Cataldo F, Sandri F, Salvioli GP. Infants of immigrant parents in Italy. A national multicentre case control study. Panminerva Med. 2001;43:155–159. [PubMed] [Google Scholar]
- Braveman P, Egerter S, Edmonston F, Verdon M. Racial/ethnic differences in the likelihood of cesarean delivery, California. Am J Public Health. 1995;85:625–630. doi: 10.2105/AJPH.85.5.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassell E. Thesis. Monash University: Department of Social and Preventive Medicine; 1995. An Investigation of the Adverse Obstetric Profile and Pregnancy Outcomes Among Philippines-Born Women in Victoria, 1982-92. [Google Scholar]
- Delvaux T, Buekens P, Thoumsin H, Dramaix M, Collette J. Cord C-peptide and insulin-like growth factor-I, birth weight, and placenta weight among North African and Belgian neonates. Am J Obstet Gynecol. 2003;189:1779–1784. doi: 10.1016/S0002-9378(03)00808-1. [DOI] [PubMed] [Google Scholar]
- Diani F, Zanconato G, Foschi F, Turinetto A, Franchi M. Management of the pregnant immigrant woman in the decade 1992-2001. J Obstet Gynaecol. 2003;23:615–617. doi: 10.1080/01443610310001604367. [DOI] [PubMed] [Google Scholar]
- Gayral-Taminh M, Arnaud C, Parant O, Fournie A, Reme JM, Grandjean H. Pregnancy and labor of women born in Maghreb and Black Africa followed to delivery at the Maternity Hospital of Toulouse. J Gynecol Obstet Biol Reprod. 1999;28:462–471. [PubMed] [Google Scholar]
- Johnson EB, Reed SD, Hitti J, Batra M. Increased risk of adverse pregnancy outcome among Somali immigrants in Washington state. Am J Obstet Gynecol. 2005;193:475–482. doi: 10.1016/j.ajog.2004.12.003. [DOI] [PubMed] [Google Scholar]
- LeRay C, Carayol M, Zeitlin J, Breart G, Goffinet F. PREMODA Study Group. Level of perinatal care of the maternity unit and rate of cesarean in low-risk nulliparas. Obstet Gynecol. 2006;107:1269–1277. doi: 10.1097/01.AOG.0000218098.70942.a2. [DOI] [PubMed] [Google Scholar]
- Ma J, Bauman A. Obstetric profiles and pregnancy outcomes of immigrant women in New South Wales, 1990-1992. Aust N Z J Obstet Gynaecol. 1996;36:119–125. doi: 10.1111/j.1479-828X.1996.tb03265.x. [DOI] [PubMed] [Google Scholar]
- Panagopoulos P, Tsoukalos G, Economou A, Zikopoulos M, Koutras I, Petrakos G, Pachakis M. Delivery and immigration: the experience of a Greek Hospital. Clin Exp Obstet Gynecol. 2005;32:55–57. doi: 10.1016/j.ogc.2004.10.002. [DOI] [PubMed] [Google Scholar]
- Rizzo N, Ciardelli V, Gandolfi-Colleoni G, Bonavita B, Parisio C, Farina A, Bovicelli L. Delivery and immigration: the experience of an Italian hospital. Eur J Obstet Gynecol Reprod Biol. 2004;116:170–172. doi: 10.1016/j.ejogrb.2004.02.018. [DOI] [PubMed] [Google Scholar]
- Rumbaut R. Unraveling a public health enigma: Why do immigrants experience superior perinatal health outcomes. Res Sociol Health Care. 1996;13B:337–391. [Google Scholar]
- Vangen S, Stoltenberg C, Schei B. Ethnicity and use of obstetrical analgesia: do Pakistani women receive inadequate pain relief in labour? Ethn Health. 1996;1:161–167. doi: 10.1080/13557858.1996.9961783. [DOI] [PubMed] [Google Scholar]
- Vangen S, Stray-Pedersen B, Skrondal A, Magnus P, Stoltenberg C. High risk of cesarean section among ethnic Filipinos: an effect of the paternal contribution to birthweight? Acta Obstet Gynecol Scand. 2003;82:192–193. doi: 10.1034/j.1600-0412.2003.00075.x. [DOI] [PubMed] [Google Scholar]
- Vangen S, Stoltenberg C, Holan S, Moe N, Magnus P, Harris JR, Stray-Pedersen B. Outcome of pregnancy among immigrant women with diabetes. Diabetes Care. 2003;26:327–332. doi: 10.2337/diacare.26.2.327. [DOI] [PubMed] [Google Scholar]
- Vangen S, Stoltenberg C, Johansen RE, Sundby J, Stray-Pedersen B. Perinatal complications among ethnic Somalis in Norway. Acta Obstet Gynecol Scand. 2002;81:317–322. doi: 10.1034/j.1600-0412.2002.810407.x. [DOI] [PubMed] [Google Scholar]
- Versi E, Liu KL, Chia P, Seddon G. Obstetric outcome of Bangladeshi women in east London. Br J Obstet Gynaecol. 1995;102:630–637. doi: 10.1111/j.1471-0528.1995.tb11401.x. [DOI] [PubMed] [Google Scholar]
- Yoong W, Wagley A, Fong C, Chukwuma C, Nauta M. Obstetric performance of ethnic Kosovo Albanian asylum seekers in London: a case–control study. J Obstet Gynaecol. 2004;24:510–512. doi: 10.1080/01443610410001722527. [DOI] [PubMed] [Google Scholar]
- Yoong W, Kolhe S, Karoshi M, Ullah M, Nauta M. The obstetric performance of United Kingdom asylum seekers from Somalia: a case–control study and literature review. Int J Fertility & Womens Med. 2005;50:175–179. [PubMed] [Google Scholar]
- Small R, Gagnon A, Gissler M, Zeitlin J, Bennis M, Glazier RH, Haelterman E, Martens G, McDermott S, Urquia M. et al. Somali women and their pregnancy outcomes post-migration: data from six receiving countries. Br J Obstet Gynaecol. 2008;115:1630–1640. doi: 10.1111/j.1471-0528.2008.01942.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malin M, Gissler M. Maternal care and birth outcomes among ethnic minority women in Finland. BMC Public Health. 2009;9:84. doi: 10.1186/1471-2458-9-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fedeli U, Alba N, Lisiero M, Zambon F, Avossa F, Spolaore P. Obstetric hospitalizations among Italian women, regular and irregular immigrants in North Eastern Italy. Acta Obstet Gynecol Scand. 2010;89:1432–1437. doi: 10.3109/00016349.2010.512065. [DOI] [PubMed] [Google Scholar]
- Gann P, Nghiem L, Warner S. Pregnancy characteristics and outcomes of Cambodian refugees. Am J Public Health. 1989;79:1251–1257. doi: 10.2105/AJPH.79.9.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell R. Philippino and Vietnamese Women - A Study of Intrapartum Differences. Aust N Z J Public Health. 1989;29:399–402. doi: 10.1111/j.1479-828x.1989.tb01777.x. [DOI] [PubMed] [Google Scholar]
- Mossialos E, Allin S, Karras K, Davaki K. An investigation of Caesarean sections in three Greek hospitals. Eur J Public Health. 2005;15:288–295. doi: 10.1093/eurpub/cki002. [DOI] [PubMed] [Google Scholar]
- Helsel D, Petitti DB, Kunstadter P. Pregnancy among the Hmong: birthweight, age, and parity. Am J Public Health. 1992;82:1361–1364. doi: 10.2105/AJPH.82.10.1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan A, Roder D, Macharper T. Obstetric Profiles of Immigrant Women from Non-English Speaking Countries in South Australia, 1981-1983. Aust N Z J Obstet Gynaecol. 1988;28:90–95. doi: 10.1111/j.1479-828X.1988.tb01630.x. [DOI] [PubMed] [Google Scholar]
- Rio I, Castelló A, Barona C, Jané M, Más R, Rebagliato M, Bosch S, Martínez E, Bolúmar F. Caesarean section rates in immigrant and native women in Spain: the importance of geographical origin and type of hospital for delivery. Eur J Public Health. 2010;20:524–529. doi: 10.1093/eurpub/ckq067. [DOI] [PubMed] [Google Scholar]
- Triantafyllidis G, Tziouva K, Papastefanou I, Samolis S, Katsetos C, Panagopoulos P. Frequency of Cesarean Section (CS) and Infectious Diseases Among Greek and Immigrant Women in a Greek Public Nursery [abstract]. Abstracts of the XXII European Congress of Perinatal Medicine, 2010. J Matern Fetal Neonatal Med. 2010;23:289. [Google Scholar]
- Zlot AI, Jackson DJ, Korenbrot C. Association of acculturation with cesarean section among Latinas. Matern Child Health J. 2005;9:11–20. doi: 10.1007/s10995-005-2447-3. [DOI] [PubMed] [Google Scholar]
- Berger C, Liska G, Gallier J, Soutoul JH. Comportement obstetrical des migrantes. Revue de Medecine de Tours. 1973;7:607–611. [Google Scholar]
- Forna F, Jamieson DJ, Sanders D, Lindsay MK. Pregnancy outcomes in foreign-born and US-born women. Int J Gynaecol Obstet. 2003;83:257–265. doi: 10.1016/S0020-7292(03)00307-2. [DOI] [PubMed] [Google Scholar]
- Hazekamp JT. Care and control in immigrant Pakistani pregnancy. Experience from Ullevaal Hospital in Oslo. Tidsskrift for den Norske laegeforening: tidsskrift for praktisk medicin, ny raekke. 1982;102:237–239. [PubMed] [Google Scholar]
- Richman D, Dixon S. Comparative study of Cambodian, Hmong, and Caucasian infant and maternal perinatal profiles. J Nurse Midwifery. 1985;30:313–319. doi: 10.1016/0091-2182(85)90168-5. [DOI] [PubMed] [Google Scholar]
- Henry OA, Guaran RL, Petterson CD, Walstab JE. Obstetric and birthweight differences between Vietnam-born and Australian-born women. Med J Australia. 1992;156:321–324. doi: 10.5694/j.1326-5377.1992.tb139788.x. [DOI] [PubMed] [Google Scholar]
- Small R, Lumley J. Variations in Caesarean Section by Maternal Country of Birth, Victoria 1999-2003[abstract] J Paediatr Child Health. 2007;43:A53. [Google Scholar]
- Zuppa AA, Orchi C, Calabrese V, Verrillo G, Perrone S, Pasqualini P, Cota F, Ranno O, Valentini P, Giannantonio C. Maternal and neonatal characteristics of an immigrant population in an Italian hospital. J Matern Fetal Neonatal Med. 2010;23:627–632. doi: 10.3109/14767050903258761. [DOI] [PubMed] [Google Scholar]
- Aurelius G, Ryde-Blomqvist E. Pregnancy and Delivery among Immigrants. Scand J Public Health. 1978;6:43–48. doi: 10.1177/140349487800600109. [DOI] [PubMed] [Google Scholar]
- Gagnon AJ, Dougherty G, Platt RW, Wahoush O, George A, Stanger E, Oxman-Martinez J, Saucier JF, Merry L, Stewart DE. Refugee and refugee-claimant women and infants post-birth: migration histories as a predictor of Canadian health system response to needs. Can J Public Health. 2007;98:287–291. doi: 10.1007/BF03405405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teixeira C, Correia S, Barros H. Abstract Book of the 3rd Conference on Migrant and Ethnic Minority Health in Europe. Hungary: Pécs; 2010. Geographic origin and risk of cesarean section in Portugal [abstract] p. 78. 27-29 May 2010. [Google Scholar]
- Gagnon AJ, Wahoush O, Dougherty G, Saucier JF, Dennis CL, Merry L, Stanger E, Stewart DE. The Childbearing Health and Related Service Needs of Newcomers (CHARSNN) study protocol. BMC Pregnancy Childbirth. 2006;6 doi: 10.1186/1471-2393-6-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loew D, Schrank P. Bericht uber 7000 Geburten in einem mittleren Krankenhaus unter Berucksichtigung der Geburtsverlaufe bei Auslanderinnen. Zentralbl Gynakol. 1966;1:23–31. [PubMed] [Google Scholar]
- Schliemann F, Schliemann G. Deliveries in foreign women. Geburtshilfe Frauenheilkd. 1975;35:210–217. [PubMed] [Google Scholar]
- Saurwein A. Delivery in foreign women: frequency and indication of cesarean section. Geburtshilfe Frauenheilkd. 1969;29:728–734. [PubMed] [Google Scholar]
- Harlap S, Kaufman R, Prywes R, Davies AM, Sterk VV, Weiskopf P. Patterns of obstetric intervention in a total population. A report from the Jerusalem perinatal study. Israel J Med Sci. 1971;7:1115–1127. [PubMed] [Google Scholar]
- Maslovitz S, Kupferminc MJ, Lessing JB, Many A. Perinatal outcome among non-residents in Israel. Israel Med Assoc J: Imaj. 2005;7:315–319. [PubMed] [Google Scholar]
- Barron SL, Vessey MP. Immigration a new social factor in obstetrics. Br Med J. 1966;1:1189–1194. doi: 10.1136/bmj.1.5497.1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminski M. La grossesse des femmes migrantes à Paris. Rev Fr Gynecol Obstet. 1975;70:483–491. [Google Scholar]
- Rudman A, El-Khouri B, Waldenström U. Evaluating multi-dimensional aspects of postnatal hospital care. Midwifery. 2008;24:425–441. doi: 10.1016/j.midw.2007.03.004. [DOI] [PubMed] [Google Scholar]
- Press F, Katz M, Leiberman JR, Shoham I, Glezerman M. Obstetric performance in Ethiopian immigrants compared with Israeli parturients. Israel J Med Sci. 1993;29:403–407. [PubMed] [Google Scholar]
- Moscioni P, Romagnoli C, Pomili G, Gilardi G. Immigrant women and health services. Experience with hospital obstetric-gynecologic department (1992–94) Minerva Ginecol. 1995;47:373–379. [PubMed] [Google Scholar]
- Walsh J, Robson M, Foley M. The influence of ethnicity on caesarean section rates in the home of active management of labour[abstract] Int J Gynecology & Obsterics. 2009;107S2:373–374. [Google Scholar]
- van Enk A, Doornbos HP, Nordbeck HJ. Some characteristics of labor in ethnic minorities in Amsterdam. Int J Gynaecol Obstet. 1990;33:307–311. doi: 10.1016/0020-7292(90)90515-M. [DOI] [PubMed] [Google Scholar]
- van Enk WJ, Gorissen WH, van Enk A. Teenage pregnancy and ethnicity in The Netherlands: frequency and obstetric outcome. Eur J Contracept Reprod Health Care. 2000;5:77–84. doi: 10.1080/13625180008500379. [DOI] [PubMed] [Google Scholar]
- Schultze-Naumburg R, Scholtes G. Entbindungen bei Ausländerinnen. In Medizinische Klinik. 1976;2:63–67. [PubMed] [Google Scholar]
- Janevic T. Final Program for the Society for Pediatric and Perinatal Epidemiologic Research (SPER) 24th annual meeting: June 20 – 21, 2011. Montreal; 2011. Differences in cesarean delivery in New York City by race, ethnicity, and nativity, 1995-2003 [abstract] p. 74. [Google Scholar]
- Sletten K. Thesis. Institute of Health and Society, Health Sciences; Perinatal outcomes of immigrants giving birth at a low risk central hospital in Norway: A comparison study at Bærum hospital of different ethnic groups and Norwegian women. Unpublished (completed 2011). Abstract available at: https://www.duo.uio.no/handle/123456789/28440. [Google Scholar]
- Stray-Pedersen B, Austveg B, In: Mid-life Norwegian Gynaecological Association 50 years festschrift. Bordahl P, editor. Tapir Trondheim; 1996. Our new country men: challenges and opportunities. [Google Scholar]
- Parsons L, Macfarlane AJ, Golding J. In: Race and health in contemporary Britain. Ahmad WIU, editor. Buckingham: Open University Press; 1993. Pregnancy, birth and maternity care. [Google Scholar]
- Holan S, Vangen S, Hanssen K, Stray-Pedersen B. Diabetes hos gravide født i Asia, Afrika og Norge. Tidsskr Nor Legeforen. 2008;128:1289–1292. [PubMed] [Google Scholar]
- Oliva GC, Zannella MP, Filidi C, Cavaliere AF, Casarella L, Mancuso S. Characteristics of the puerperium and complications in the vaginal delivery and the caesarean section. Comparison between the Italian and foreign population in casuistry 2000–2004 of the Policlinico "A. Gemelli". Giornale Italiano di Ostetricia e Ginecologia. 2007;29:75–81. [Google Scholar]
- Ismail KI, Marchocki Z, Brennan DJ, O'Donoghue K. Intrapartum caesarean rates differ significantly between ethnic groups–Relationship to induction. Eur J Obstet Gynecol Reprod Biol. 2011;158:214–219. doi: 10.1016/j.ejogrb.2011.06.009. [DOI] [PubMed] [Google Scholar]
- Zanconato G, Iacovella C, Parazzini F, Bergamini V, Franchi M. Pregnancy outcome of migrant women delivering in a public institution in northern Italy. Gynecol Obstet Invest. 2011;72:157–162. doi: 10.1159/000328318. [DOI] [PubMed] [Google Scholar]
- Comas M, Català L, Sala M, Payà A, Sala A, Del Amo E, Castells X, Cots F. Descriptive analysis of childbirth healthcare costs in an area with high levels of immigration in Spain. BMC Health Serv Res. 2011;11:77. doi: 10.1186/1472-6963-11-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giani U, Bruzzese D, Pugliese A, Saporito M, Triassi M. Risk factors analysis for Elective Caesarean Section in Campania region (Italy) Epidemiol Prev. pp. 101–110. [PubMed]
- Von Katterfeld B, Li J, McNamara B, Langridge AT. Obstetric profiles of foreign-born women in Western Australia using data linkage, 1998–2006. Aust N Z J Obstet Gynaecol. 2011;51:225–232. doi: 10.1111/j.1479-828X.2010.01282.x. [DOI] [PubMed] [Google Scholar]
- Lansakara N, Brown SJ, Gartland D. Birth outcomes, postpartum health and primary care contacts of immigrant mothers in an Australian nulliparous pregnancy cohort study. Matern Child Health J. 2010;14:807–816. doi: 10.1007/s10995-009-0514-x. [DOI] [PubMed] [Google Scholar]
- Shah D, Tay A, Desai A, Parikh M, Nauta M, Yoong W. The obstetric performance of Chinese immigrants residing in the UK. J Obstet Gynaecol. 2011;31:480–482. doi: 10.3109/01443615.2011.580396. [DOI] [PubMed] [Google Scholar]
- Saurel-Cubizolles M-J, Saucedo M, Drewniak N, Blondel B, Bouvier-Colle M-H. Santé périnatale des femmes étrangères en France. Bulletin épidémiologique hebdomadaire. 2012;2-3-4:30–34. [Google Scholar]
- Shah RR, Ray JG, Taback N. Adverse Pregnancy Outcomes Among Foreign-Born Canadians. J Obstet Gynaecol Can. 2011;33:207–215. doi: 10.1016/s1701-2163(16)34821-6. [DOI] [PubMed] [Google Scholar]
- Walsh J, Mahony R, Armstrong F, Ryan G, O’Herlihy C, Foley M. Ethnic variation between white European women in labour outcomes in a setting in which the management of labour is standardised—a healthy migrant effect? BJOG. 2011;118:713–718. doi: 10.1111/j.1471-0528.2010.02878.x. [DOI] [PubMed] [Google Scholar]
- Kingston D, Heaman M, Chalmers B, Kaczorowski J, O’Brien B, Lee L, Dzakpasu S, O’Campo P. Comparison of Maternity Experiences of Canadian-Born and Recent and Non-Recent Immigrant Women: Findings From the Canadian Maternity Experiences Survey. J Obstet Gynaecol Can. 2011;33:1105–1115. doi: 10.1016/S1701-2163(16)35078-2. [DOI] [PubMed] [Google Scholar]
- Berger C, Laugier J, Soutoul JH. Caracteristiques de l'accouchement et du nouveau-ne de migrante: fitude de 800 dossiers. Journal de Gynicologie Obstetrique et Biologie de la Reproduction. 1974;3:1227–1234. [PubMed] [Google Scholar]
- Shah RR. Thesis. University of Toronto, Graduate Department of Health Policy, Management and Evaluation; 2007. Adverse Obstetrical and Perinatal Outcomes Among Foreign-Born Women Living in Canada. [Google Scholar]
- Ryan G, Armstrong F, Walsh J, Foley M. Ethnic variation in the mode of onset nulliparous term labour and resultant caesarean section rates with consideration of birth weight [abstract] Ir J Med Sci. 2010;179(supplement 2):S84. [Google Scholar]
- Walsh J, Mahony R, McAuliffe F, O'Herlihy C, Robson M, Foley M. Ethnic variation in the onset of spontaneous nulliparous term labor and cesarean delivery rates may be explained by differences in maternal ageand BMI (319) [abstract] Am J Obstet Gynecol. 2009;201:S127. [Google Scholar]
- Ismail K, Marchocki Z, Brennan D, O'Donoghue K. Comparing labour outcomes between different racial groups [abstract] Arch Dis Child Fetal Neonatal Ed. 2010;95(Suppl 1):Fa77. [Google Scholar]
- Gagnon AJ, Van Hulst A, Merry L, George A, Saucier JF, Stanger E, Wahoush O, Stewart DE. Cesarean section rate differences by migration indicators. Archives of Gynecology and Obstetrics. 2012. published online November 2012. [DOI] [PubMed]
- The HAPO Study Cooperative Research Group. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358:1991–2002. doi: 10.1056/NEJMoa0707943. [DOI] [PubMed] [Google Scholar]
- Benjamin SJ, Daniel AB, Kamath A, Ramkumar V. Anthropometric measurements as predictors of cephalopelvic disproportion. Acta Obstet Gynecol Scand. 2012;91:122–127. doi: 10.1111/j.1600-0412.2011.01267.x. [DOI] [PubMed] [Google Scholar]
- Gagnon AJ, McDermott S, Rigol-Chachamovich J, Bandyopadhyay M, Stray-Pedersen B, Stewart D. for the ROAM Collaboration. International migration and gestational diabetes mellitus: a systematic review of the literature and meta-analysis. Paediatr Perinat Epidemiol. 2011;25:575–592. doi: 10.1111/j.1365-3016.2011.01230.x. [DOI] [PubMed] [Google Scholar]
- Konje JC, Ladipo OA. Nutrition and obstructed labor. Am J Clin Nutr. 2000;72:291S–297S. doi: 10.1093/ajcn/72.1.291S. [DOI] [PubMed] [Google Scholar]
- Siega-Riz AM, Laraia B. The implications of maternal overweight and obesity on the course of pregnancy and birth outcomes. Matern Child Health J. 2006;10:153–156. doi: 10.1007/s10995-006-0115-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg TJ, Garbers S, Chavkin W, Chiasson MA. Prepregnancy weight and adverse perinatal outcomes in an ethnically diverse population. Obstet Gynecol. 2003;102:1022–1027. doi: 10.1016/j.obstetgynecol.2003.07.005. [DOI] [PubMed] [Google Scholar]
- Loetscher KCQ, Selvin S, Zimmermann R, Abrams B. Ethnic-cultural background, maternal body size and pregnancy outcomes in a diverse Swiss cohort. Women Health. 2007;45:25–40. doi: 10.1300/J013v45n02_02. [DOI] [PubMed] [Google Scholar]
- Heaman M, Bayrampour H, Kingston D, Blondel B, Gissler M, Roth C, Alexander S, Gagnon A. Migrant women’s utilization of prenatal care: a systematic review. Matern Child Health J. 2012. published online June 2012. [DOI] [PubMed]
- Bischoff A, Bovier PA, Isah R, Francoise G, Ariel E, Louis L. Language Barriers Between Nurses and Asylum Seekers: Their Impact on Symptom Reporting and Referral. Soc Sci Med. 2003;57:503–512. doi: 10.1016/S0277-9536(02)00376-3. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services. Healthy people, Tracking. Washington D.C.: US Government Printing Office; 2010. p. 2000. [Google Scholar]
- Carballo M, Grocutt M, Hadzihasanovic A. Women and migration: a public health issue. World Health Stat Q. 1996;49:158–164. [PubMed] [Google Scholar]
- Kahler LR, Sobota CM, Hines CK, Griswold K. Pregnant women at risk: An evaluation of the health status of refugee women in Buffalo, New York. Health Care Women Int. 1996;17:15–23. doi: 10.1080/07399339609516216. [DOI] [PubMed] [Google Scholar]
- McGinn T. Reproductive health of war-affected populations: what do we know? Int Fam Plan Perspect. 2000;26:174–180. doi: 10.2307/2648255. [DOI] [Google Scholar]
- Liu J, Kerr D. Family change and economic well-being in canada: the case of recent immigrant families with children. Int Migr. 2003;41:113–140. doi: 10.1111/1468-2435.00254. [DOI] [Google Scholar]
- Blume K, Gustafsson B, Pedersen PPJ, Verner M. At the lower end of the table: determinants of poverty among immigrants to Denmark and Sweden. J Ethnic Migr Stud. 2007;33:373–396. doi: 10.1080/13691830701234517. [DOI] [Google Scholar]
- Liamputtong P, Watson LF. The meanings and experiences of cesarean birth among Cambodian, Lao and Vietnamese immigrant women in Australia. Women Health. 2006;43:63–82. doi: 10.1300/J013v43n03_04. [DOI] [PubMed] [Google Scholar]
- Vangen S, Johansen RE, Sundby J, Traeen B, Stray-Pedersen B. Qualitative study of perinatal care experiences among Somali women and local health care professionals in Norway. Eur J Obstet Gynecol Reprod Biol. 2004;112:29–35. doi: 10.1016/S0301-2115(03)00313-0. [DOI] [PubMed] [Google Scholar]
- Hodnett ED, Fredericks S, Weston J. Support during pregnancy for women at increased risk of low birthweight babies. Cochrane Database Syst Rev. 2010;6 doi: 10.1002/14651858.CD000198.pub2. [DOI] [PubMed] [Google Scholar]
- Hodnett ED, Gates S, Hofmeyr GJ, Sakala C, Weston J. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2011;2 doi: 10.1002/14651858.CD003766.pub3. [DOI] [PubMed] [Google Scholar]
- Bollini P, Pampallona S, Wanner P, Kupelnick B. Pregnancy Outcome of Migrant Women and Integration Policy: A Systematic Review of the International Literature. Soc Sci Med. 2009;68:452–461. doi: 10.1016/j.socscimed.2008.10.018. [DOI] [PubMed] [Google Scholar]
- Gagnon AJ, Zimbeck M, Zeitlin J. Migration and perinatal health surveillance: an international Delphi survey. Eur J Obstet Gynaecol Reprod Biol. 2010;149:37–43. doi: 10.1016/j.ejogrb.2009.12.002. [DOI] [PubMed] [Google Scholar]
- Gissler M, Alexander S, MacFarlane A, Small R, Stray-Pedersen B, Zeitlin J, Zimbeck M, Gagnon AJ. Stillbirths and infant deaths among migrants in industrialised countries. Acta Obstet Gynecol Scand. 2009;88:134–148. doi: 10.1080/00016340802603805. [DOI] [PubMed] [Google Scholar]
- Urquia M, Glazier R, Blondel B, Zeitlin J, Gissler M, McFarlane A, Ng E, Heaman M, Stray-Pedersen B, Gagnon AJ. International migration and adverse birth outcomes: role of ethnicity, region of origin and destination. J Epidemiol Community Health. 2010;64:243–251. doi: 10.1136/jech.2008.083535. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Database search strategy.
Websites searched.
UN Macro Regions.


