Abstract
Background
Research has shown the efficacy of family-based behavioral interventions for overweight children, but a major difficulty is access to effective treatment programs. The objective of this study was to develop and test the initial feasibility and efficacy of a web-based family program for overweight 8- to 12-year-old children.
Methods
A website was created using concepts from effective family-based behavioral programs and input from focus groups with overweight children, parents, and pediatricians. The website provided information about obesity and healthy lifestyles, assessment of dietary and physical activity habits, interactive dietary and physical activity games, and instruction in goal-setting and monitoring of goals. Children selected a dietary and physical activity goal and a daily step goal with pedometers. Feasibility and pilot testing over 4 weeks was conducted with 24 overweight children referred by a physician. Outcomes were z-BMI, healthy eating and physical activity, and intrinsic motivation and self-efficacy for weight control.
Results
Mean number of logins over the study period was 11.4 for the study sample. Eighteen families (75%) returned for the follow-up assessment. Pre–post analyses for these participants showed improvements in intrinsic motivation, (p=0.05), self-efficacy (p=0.025), physical activity (p=0.005), and healthy lifestyle behaviors (p=0.001). Comparisons between high and low users of the program indicated that high users reduced their BMI while low users increased their BMI over time (p=0.02); high users also improved their dietary intake relative to low users (p=0.04). Consumer satisfaction ratings were high.
Conclusion
These pilot findings suggest this is a feasible approach for treatment of overweight children and that children who used the web program frequently improved their BMI and dietary intake.
Introduction
Recent research indicates that the prevalence of overweight and obesity in children is very high, comprising about one-third of children and youth in the United States and increasing in incidence.1 Policy experts consider this epidemic to be a serious public health issue.2 Overweight youth usually remain overweight as adults and are at increased risk for a variety of adverse health conditions3–5; rates are higher in children from lower-income families6,7 and of ethnic minority status.8–10
Studies have shown there is a relationship between child and parental obesity that can be explained by genetic11 and environmental/behavioral factors,12,13 and familial aggregation of physical activity14 and eating habits15 has been observed. Specific behavioral factors involve consumption of high-fat diets16 and physical inactivity,17,18 as well as increased television viewing.19–22 Low levels of physical activity have been associated with glucose intolerance and type 2 diabetes.23,24
The family unit should be targeted in weight control programs for children.25 Research indicates that family involvement is crucial,13,26–34 and that when parents are involved in their own weight loss efforts better results are obtained for children.27 Increased physical activity is also a critical component of weight loss programs for children.35,36
Web-based intervention has been termed the “next transformation in the delivery of health care” and has great potential for dealing with the obesity epidemic.37 Over 75% of Americans are estimated to have internet access, and studies show that about 80% of adult internet users seek health-related information for themselves and their children.38,39 Research has shown that internet health interventions have favorable treatment outcomes.40,41
The internet holds promise for the delivery of weight control interventions, and studies demonstrate the efficacy of several internet behavioral weight loss programs for adults.42–50 Reviews of weight loss programs delivered over the internet conclude that this approach may be an alternative to face-to-face programs.51,52 Several reports suggest the efficacy of web-based weight loss interventions for youth. For example, an internet intervention showed decreased fast food consumption and increased physical activity in adolescent girls.53 Another study showed decreased dietary fat intake and reduced body fat after 6 months of treatment, with increased use of the web site associated with better outcomes54; however, weight loss was not maintained at 2 years, with decreased web use occurring over time.55 Additional studies have found web-based programs to result in increases in physical activity and improved dietary intake in children as young as 8 years of age.56–59
There are many web sites with information related to child obesity, some with interactive games to increase children's nutritional and physical activity knowledge and skills. Most are designed to promote health and prevent obesity, rather than as interactive sites to help children who are already overweight, and few sites contain online tracking components. Little is known about the effects of these programs on changing dietary behavior, physical activity, or weight.
Research has demonstrated the efficacy of family-based behavioral interventions for pediatric weight control.31,32,36,60 However, a major challenge is access to effective treatment programs. The aim of this study was to create and pilot test a web-based family intervention program for overweight children, Families Interacting Together for Health (FIT-4-Health).
Materials and Methods
Participants and Setting
Twenty-four overweight children were recruited from two pediatric clinics; inclusion criteria were overweight status, 8–12 years of age, no other serious health problems, families speak and write English, and have high-speed internet connections at their homes. Their mean age was 11.0±1.22 years. The BMI values for these children were all greater than the 85th percentile, with a mean BMI percentile of 98, and mean BMI z-score of 2.19. There were 10 girls and 14 boys; 11 children were Hispanic, 9 were African American, 3 were non-Hispanic white, and 1 was Asian American. Mean years of education for mothers and fathers were 14.7 and 13.8 years. Mean annual family income was $79,368 (range $14,000–$130,000). Most families (75%) had 2 parents living in the home.
FIT-4-Health Web Site
Participants were given the website address for the program and a login user name; they created their own password to enter the FIT-4-Health site. The welcome page contained an orientation to the program, along with six other tabs at the top of the page: What's the Problem?, Let's Get Started, How to Have a Healthy Lifestyle, Setting My Goals, Keeping Track, and What's Next? Clicking on each of these tabs led to another page with text written for the child (with an option to hear the text narrated by a youth voice), along with an icon labeled, “Parent Stuff,” containing more information related to each topic. Children's knowledge and skills were addressed through two interactive games—one focused on discriminating types of physical activities and sedentary behaviors, and the other on healthy and unhealthy food choices and portion sizes. Other modules addressed stimulus control and modification of eating behavior and increasing physical activity and reducing sedentary behavior. The program used a variety of methods including text, graphics, narration, and interactive programming.
The content of the program was informed by the evidence for efficacy in pediatric weight loss.31,32,36,60 A focus group was conducted with 5 pediatricians, who were shown a preliminary version of the program. In a separate focus group with 3 families, overweight children and their parents together were shown the program, and their feedback was obtained about various program features. Because the program was developed to be family-based, we designed the focus groups with both parents and children participating together. After revising the program based on their feedback, pretesting was conducted with 2 more overweight children and their parents, who were observed using the program and then interviewed about program features. On the basis of their feedback, the program was refined further. The focus groups were conducted by 2 of the study investigators (AMD and HS). Transcripts were prepared of each focus group, and the results were content analyzed for common themes.
Children first completed an assessment of their dietary and physical activity habits using items from the Youth Risk Behavior Survey and then selected one dietary and one physical activity behavior to focus on as goals. In addition, all children were given a pedometer and instructed in its use over 3 days to establish their daily step baseline, after which they selected an appropriate daily step goal (e.g., either 10% or 20% above their baseline). The objective was for each child to monitor their performance on a daily basis with each of their three daily goals and record that in the Keeping Track section of the website. Parents were asked to monitor, prompt, and reinforce their child's use of the program, as well as use the parent features of the program to learn more about healthy lifestyles.
Measures
Demographic variables
A demographic interview was conducted with the primary caregiver to obtain demographic data including geographic origins, ethnic status, marital status, and parent education, occupation, and family income.
Anthropometric variables
Children were measured for their height (by stadiometer) and weight (by balance scale), and BMI (weight in kg/height in meters squared) was calculated at baseline and at the 1-month follow-up. BMI was transformed into z-scores based upon national norms for age and sex.
Psychological variables
The Intrinsic Motivation Inventory for Weight Management (IMI-WM) was created for this study because there was no available measure for this construct in children. The Self-Determination Theory web site (www.psych.rochester.edu/SDT/questionnaires.php/) was used to create this measure. The IMI-WM consists of 16 items, each rated on a 7-point scale (not at all true to very true), with 8 comprising a self-efficacy subscale and 8 an importance subscale. A sample item for self-efficacy is: “Overall, I feel confident in being able to manage my diet so that my weight will be healthy.” A sample item for importance is: “I put a lot of effort into managing my weight.” The internal consistencies for the overall scale score and self-efficacy and importance subscales were 0.78, 0.73, and 0.63, respectively.
Behavioral variables
Six items from the Youth Risk Behavior Survey (YRBS; from the CDC's Youth Risk Behavior Surveillance System) were used to measure healthy or unhealthy eating habits. Six other items from the YRBS were used to measure physical activity and sedentary behavior. Examples of questions include: “During the past 7 days, on how many days did you eat breakfast?” and “On how many of the past 7 days did you exercise or participate in physical activity for at least 20 minutes that made you sweat and breathe hard?” An overall composite score for healthy lifestyle was based on these 12 items (alpha=0.56); the internal consistency for the healthy eating scale was 0.47 and for the healthy physical activity scale was 0.50.
Procedures
Participants were recruited during their regularly scheduled clinic appointments. The physician recruited the family and gave potential participants the study phone number to call to learn more about the study. Research assistants screened and scheduled families for an initial baseline appointment where they completed informed consent/assent procedures and baseline assessments of anthropometric, behavioral, and psychological variables. The research assistant then conducted an orientation to the web program, with the parent and child using a laptop computer. Participants were asked to use the web site for the following 4 weeks, after which they would be scheduled to return to the clinic to complete the 1-month postbaseline assessment, including the same measures taken at baseline plus a brief consumer satisfaction measure developed for this study. Participants were encouraged to visit the web site as often as possible, if not daily, at least several times per week. Parents were instructed to visit the site with the child, praise the child for visiting the site, and practice implementing strategies from the web site at home. At the completion of the orientation, a pedometer was given to the child to track the number of steps taken each day. Families received gift coupons after completing baseline ($25) and 1-month postenrollment assessments ($75).
Statistical Analyses
Paired t-tests were used to evaluate changes in anthropometric status, behavior, and psychological functioning. For a within-subjects analysis, assuming a correlation between pretest and posttest greater than r=0.70, 24 participants provided 80% power assuming a medium effect size at p=0.05 (one-tailed). Given the small sample size and hypothesis of improvement, one-tailed tests were used. Repeated measures analysis of variance (ANOVA) was also used in tests comparing children who were high versus low utilizers of the website.
Results
Program Usage
Mean number of logins over the 4-week study period was 11.42 for the entire sample, with a range of 1–34. Eighteen of 24 families (75%) returned for the follow-up assessment. The mean number of logins for the 6 children who did not return for follow-up in the study time frame was only 2.83; mean logins value for the remaining 18 children was 14.30. These 18 participants were divided into 2 groups based on the median of logins (12) to form low and high program utilization groups. Mean±standard deviation (SD) logins for the low group was 5.88 (±2.98) and for the high group was 22.67 (±9.19) (t(16)=−5.21, p=0.001).
Pre–Post Results for Sample that Completed Follow-Up Assessment
Pre–post differences were first examined by paired t-tests for the 18 children who returned for follow-up. The results of these analyses showed significant effects for the IMI total score (t(17)=−1.82, p=0.05), IMI self-efficacy (t(17)=−2.09, p=0.025), healthy physical activity (t(17)=−2.84, p=0.005), and healthy lifestyle composite (t(17)=−4.15, p=0.001), all of which improved over time. There were no significant changes in z-BMI.
Comparison of High and Low Program Users
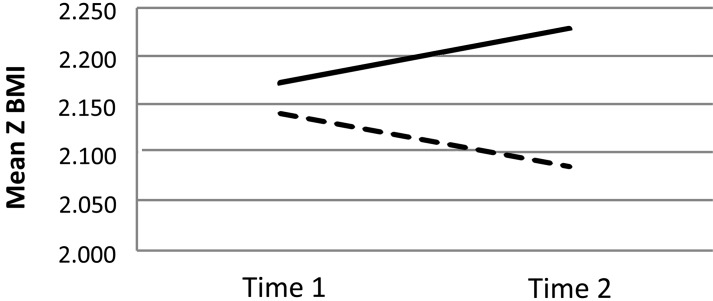
Due to differences in usage across participants, analyses were conducted to assess whether high (n=9) vs. low (n=9) users differed over time, using a repeated-measures, mixed analysis design. There was a significant interaction effect for z-BMI (F(1,16)=6.36, p=0.02). As shown in Figure 1, high users reduced their z-BMI while low users increased their z-BMI over time.
Figure 1.
Changes in child z-BMI as a function of type of user and time. (Solid line) Low utilizer; (dashed line) high ultilizer.
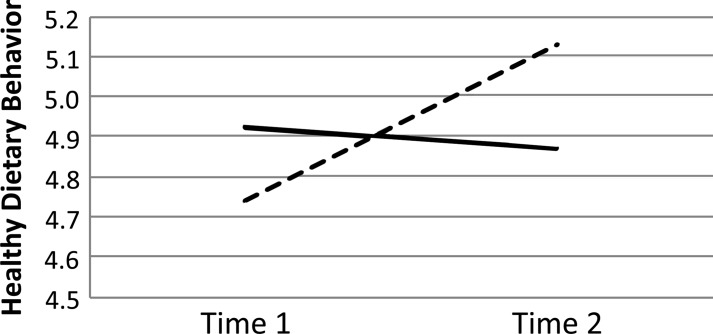
There was a significant group by time interaction effect for healthy eating behavior (based on the YRBS). As shown in Figure 2, high users improved over time relative to low users (F(1,16)=3.37, p=0.04). There was also a marginal interaction effect for IMI-Self Efficacy (F(1,16)=2.86, p=0.06), with high users increasing more over time than low users.
Figure 2.
Healthy dietary behavior as a function of type of user and time. (Solid line) Low utilizer; (dashed line) high ultilizer.
Significant effects of time were observed for physical activity (from the YRBS) (F(1,16)=7.58, p=0.005), healthy lifestyle composite score (from the YRBS) (F(1,16)=16.61, p=0.001), and for the IMI total score (F(1,16)=3.16, p=0.05), all of which improved over time. There were no differences between the high and low user groups on demographics or initial levels of intrinsic motivation or behavioral functioning.
Behavioral Goals
The most frequently chosen dietary goal was to increase consumption of fruit (n=10); other goals included increasing vegetables (n=6), decreasing unhealthy snacking (n=5), and decreasing sweetened beverages (n=2). The most frequently chosen physical activity goals were to reduce screen time (n=8) and to increase either moderate or vigorous activity (n=8). Pedometer goals were set for each child depending on their baseline values.
Tracking of Behavioral Goals
The mean number of days in which children in each utilization group tracked their dietary, physical activity, and pedometer step goals were examined. In the low use group, children tracked their dietary goals on average for 11.1 days, their physical activity goals on 8.0 days, and their step goals on 8.78 days. In the high use group, on average children tracked their dietary goals on 20.2 days, their physical activity goals on 16.3 days, and their step goals on 22.5 days.
Consumer Satisfaction Ratings
At the postassessment, parents completed a brief questionnaire regarding their satisfaction with the web program, and children were interviewed using the same questionnaire. Overall, the program was highly rated. Most families reported that the program was engaging, with 94% of children and 66.7% of parents reporting it was either very or somewhat engaging; 39% of children reported that the information was presented fairly clearly, and 61% reported it was presented very clearly. Information was relatively easy to find for 39% and very easy to find for 61%. Ninety-four percent of parents and 67% of children reported that they would strongly recommend the program to other children and families.
Discussion
This pilot study was an initial evaluation of the FIT-4-Health web program. The program was evidence-based in that it used approaches such as goal setting, self-monitoring, and involvement of parents in supporting children's healthy lifestyle behaviors.31,32,36,60 Program development also considered the perspective of children, their parents, and pediatricians through focus groups. In this pre–post pilot study with 24 overweight children, 18 (75%) completed the follow-up assessment, revealing significant improvements over the 1-month trial in intrinsic motivation and healthy lifestyle behaviors; the 6 families who did not return for follow-up did not use the web program very much. High program users reduced their z-BMI, whereas low users increased their z-BMI over time; high users also reported increases in healthy eating relative to low users, and there was a similar trend for self-efficacy for weight control of children in the high user group. In the overall study sample, 9 of the 24 children (37.5%) used the web program a mean 22.7 times over the course of 1 month, and also had high frequency of tracking their goals over time. Consumer satisfaction with the program was high, with 94.4% of parents and 66.7% of children reporting that they would strongly recommend the program to other children and families. These results are consistent with previous web-based health promotion studies with children53,54,56,59 and provide support for the initial efficacy of the FIT-4-Health web program for overweight children.
The clinical significance of the changes in z-BMI for the high users compared to the low users is noteworthy. Even though a change of 0.05 in a z-score may not appear clinically significant, this change occurred only after a 30-day time period, during which the low user group actually increased their z-BMI by 0.06; therefore, the effective z-score change for the 1-month period was 0.11. Because the pilot study was limited to a 1-month trial, it is not clear whether children who continue to use this program would be able to maintain this rate of weight loss or if at some point they would revert to previous habits.
For this type of intervention to be successful in helping children lose weight, the program must be used on a regular basis over a longer period of time. The data indicate differences in effects for those who frequented the web site often versus those who did not, and the consumer satisfaction assessment indicated that there is room for improvement with regard to the visual interface and activities to encourage engagement. Although the development of the web program was informed by focus groups that included parents, children, and physicians, more effort is needed to create an appealing and engaging web program. This is a critical need because previous research indicates overweight children decrease their use of a web program over time.55 Other health-oriented web programs for youth have successfully included a social networking component or “chat room” as part of the intervention, which may help with engagement over time.61 Once engagement is established, it is essential to maintain program interest through frequently updating materials and creating fun interactive game-like activities.
Study Limitations
Although initial results are promising, they must be interpreted with caution because this was a small sample. The study design did not include a control group. Other than anthropometrics, measurement relied on self-report of children, and statistical analyses did not control for type I error. During program development, only 5 families participated in focus groups to provide feedback on the program features. The internal consistencies of the IMI-WM total score and subscales were relatively low but acceptable for research purposes in the current study; however, future studies should more fully examine its reliability and validity, as well as the YRBS items for dietary and physical activity behaviors in larger study samples. The age range for recruitment was intentionally narrow, but future studies will need to determine whether this type of program could be effective for younger and older children. Moreover, because participants in this study were recruited from two university-based medical practices, it will be important to evaluate this type of program in community-based practices to improve generalizability.
Implications
These pilot study results suggest that this type of web-based family intervention program is feasible and can achieve some success for pediatric weight control, particularly for those children and parents who use the program more frequently. A key issue is program engagement. The next phase of this project will employ video models and more interactive game-like activities to increase program appeal and usage. The program will also be expanded to include more issues, such as intrinsic motivation for weight control, eating out, dealing with emotional eating, and parental and child responsibilities for lifestyle behaviors. Once the FIT-4-Health web program is fully developed, it will be important to test its effectiveness in a larger randomized controlled trial in community-based settings.
Conclusion
These pilot findings suggest that this type of family-based web program is a feasible approach for the treatment of overweight children and that children who use the web program more frequently improve their BMI and dietary intake. Further development of this program and its examination in a randomized trial with a larger number of children over a longer period of time is needed to determine its clinical effectiveness.
Acknowledgments
This research was supported by two grants from the National Institutes of Health (NIH) (R41 HD051244 and T32 HD07510). Appreciation is extended to Milagra Tyler of Deschutes Research, Inc. and Tim Woolley and Widya Mak of InterVision Media.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Ogden CL. Carroll MD. Curtin LR, et al. Prevalence of overweight and obesity in the United States 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine, Committee on the Prevention of Obesity in Children and Youth. Preventing Childhood Obesity: Health in the Balance. Institute of Medicine, National Academies; Washington DC: 2005. [Google Scholar]
- 3.Whitaker R. Wright J. Pepe M, et al. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 4.Manson JE. Willett WC. Stampfer MJ, et al. Body weight and mortality among women. N Engl J Med. 1995;333:677–685. doi: 10.1056/NEJM199509143331101. [DOI] [PubMed] [Google Scholar]
- 5.Must A. Jacques P. Dallal G, et al. Long-term morbidity and mortality of overweight adolescents: A follow-up of the Harvard Growth Study. N Engl J Med. 1992;327:1350–1355. doi: 10.1056/NEJM199211053271904. [DOI] [PubMed] [Google Scholar]
- 6.Sherwood NE. Wall M. Neumark-Sztainer D, et al. Effect of socioeconomic status on weight change patterns in adolescents. Prev Chronic Dis. 2009;6:A19. [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma AJ. Grummer-Strawn LM. Dalenius K, et al. Obesity prevalence among low-income preschool aged children—United States, 1998–2008. MMWR. 2009;58:769–773. [PubMed] [Google Scholar]
- 8.Berenson GS. Srinivasan SR. Hunter SM, et al. Risk factors in early life as predictors of adult heart disease: The Bogalusa Heart Study. Am J Med Sci. 1989;298:141–151. doi: 10.1097/00000441-198909000-00001. [DOI] [PubMed] [Google Scholar]
- 9.US Department of Health and Human Services. Nutrition, Report of the Secretary's Task Force on Black and Minority Health—Volume II Cross Cutting Issues in Minority Health. US Department of Health and Human Services; Washington, DC: 1985. [Google Scholar]
- 10.Malina RM. Katzmarzyk PT. Validity of the body mass index as an indicator of the risk and presence of overweight in adolescents. Am J Clin Nutr. 1999;70:131S–136S. doi: 10.1093/ajcn/70.1.131s. [DOI] [PubMed] [Google Scholar]
- 11.Stunkard A. Foch T. Hrubec Z. A twin study of human obesity. JAMA. 1986;256:51–54. [PubMed] [Google Scholar]
- 12.Epstein LH. Valoski A. Wing RR, et al. Ten-year outcomes of behavioral family-based treatment for childhood obesity. Health Psychol. 1994;13:373–383. doi: 10.1037//0278-6133.13.5.373. [DOI] [PubMed] [Google Scholar]
- 13.Epstein LH. Wing RR. Koeske R, et al. Long-term effects of family-based treatment of childhood obesity. J Consult Clin Psychol. 1987;55:91–95. doi: 10.1037//0022-006x.55.1.91. [DOI] [PubMed] [Google Scholar]
- 14.Sallis JF. Patterson TL. Buono MJ, et al. Aggregation of physical activity habits in Mexican-American and Anglo families. J Behav Med. 1988;11:31–40. doi: 10.1007/BF00846167. [DOI] [PubMed] [Google Scholar]
- 15.Patterson TL. Rupp JW. Sallis JF, et al. Aggregation of dietary calories, fats, and sodium in Mexican American and Anglo families. Am J Prev Med. 1982;4:75–82. [PubMed] [Google Scholar]
- 16.Hill J. Melanson M. Wyatt H. Dietary fat and regulation of energy balance: Implications for obesity. J Nutr. 2000;130:284S–288S. [PubMed] [Google Scholar]
- 17.Berkowitz RI. Agras JA. Korner AF, et al. Physical activity and adioposity: A longitudinal study from birth to childhood. J Pediatr. 1985;106:734–738. doi: 10.1016/s0022-3476(85)80345-0. [DOI] [PubMed] [Google Scholar]
- 18.Gortmaker SL. Dietz WH. Cheung LW. Inactivity, diet, and the fattening of America. J Am Diet Assoc. 1990;90:1247–1255. [PubMed] [Google Scholar]
- 19.Dietz WH. Gortmaker SL. Do we fatten our children at the television set? Obesity and television viewing in children and adolescents. Pediatrics. 1985;75:807–12. [PubMed] [Google Scholar]
- 20.Gortmaker SL. Must A. Sovol AM, et al. Television viewing as a cause of increasing obesity among children in the United States, 1986–1990. Arch Pediatr Adolesc Med. 1996;150:356–362. doi: 10.1001/archpedi.1996.02170290022003. [DOI] [PubMed] [Google Scholar]
- 21.Kimm S. Obarzanek E. Barton BA, et al. Race, socioeconomic status, and obesity in 9 to 10 year-old girls: The NHLBI Growth and Health Study. Ann Epidemiol. 1996;6:266–275. doi: 10.1016/s1047-2797(96)00056-7. [DOI] [PubMed] [Google Scholar]
- 22.Taras HL. Sallis JF. Patterson TL, et al. Television's influence on children's diet and physical activity. J Dev Behav Pediatr. 1989;10:176–180. [PubMed] [Google Scholar]
- 23.Dowse GK. Zimmet PZ. Gareeboo H, et al. Abdominal obesity and physical inactivity are risk factors for NIDDM and impaired glucose tolerance in Indian, Creole, and Chinese Mauritians. Diabetes Care. 1991;14:271–282. doi: 10.2337/diacare.14.4.271. [DOI] [PubMed] [Google Scholar]
- 24.King H. Taylor R. Zimmet P, et al. Risk factors for diabetes in three Pacific populations. Am J Epidemiol. 1984;119:396–409. doi: 10.1093/oxfordjournals.aje.a113758. [DOI] [PubMed] [Google Scholar]
- 25.Sallis JF. Nader PR. Family determinants of health behaviors. In: Gochman DS, editor. Health Behavior: Emerging Research Perspectives. Plenum; New York: 1988. pp. 107–124. [Google Scholar]
- 26.Brownell KD. Kaye FS. A school-based behavior modification, nutrition education and physical activity program for obese children. Am J Clin Nutr. 1982;35:277–283. doi: 10.1093/ajcn/35.2.277. [DOI] [PubMed] [Google Scholar]
- 27.Epstein LH. Valoski A. Wing R, et al. Ten-year follow-up of behavioral family based treatment for obese children. JAMA. 1990;264:2519–2523. [PubMed] [Google Scholar]
- 28.Epstein LH. Myers M. Raynor H, et al. Treatment of pediatric obesity. Pediatrics. 1998;101:554–570. [PubMed] [Google Scholar]
- 29.Golan M. Weizman A. Apter A, et al. Parents as the exclusive agents of change in the treatment of childhood obesity. Am J Clin Nutr. 1998;67:1130–1135. doi: 10.1093/ajcn/67.6.1130. [DOI] [PubMed] [Google Scholar]
- 30.Golan M. Weizman A. Fainaru M. Impact of treatment for childhood obesity on parental risk factors for cardiovascular disease. Prev Med. 1999;29:519–526. doi: 10.1006/pmed.1999.0584. [DOI] [PubMed] [Google Scholar]
- 31.Jelalian E. Hart C. Pediatric obesity. In: Roberts M, editor; Steele R, editor. Handbook of Pediatric Psychology. 4th. Guilford Press; New York: 2009. pp. 446–463. [Google Scholar]
- 32.Jelalian E. Saelens B. Empirically supported treatments in pediatric psychology: Pediatric obesity. J Pediatr Psychol. 1999;24:223–248. doi: 10.1093/jpepsy/24.3.223. [DOI] [PubMed] [Google Scholar]
- 33.Israel AC. Guile CA. Baker JE, et al. An evaluation of enhanced self-regulation training in the treatment of childhood obesity. J Pediatr Psychol. 1994;19:737–749. doi: 10.1093/jpepsy/19.6.737. [DOI] [PubMed] [Google Scholar]
- 34.Epstein LH. Wing RR. Koeske R, et al. A comparison of lifestyle change and programmed aerobic exercise on weight and fitness changes in obese children. Behav Ther. 1982;13:651–665. [Google Scholar]
- 35.Epstein LH. Goldfield G. Physical activity in the treatment of childhood overweight and obesity: Current evidence and research issues. Med Sci Sports Exerc. 1999;31:S553–S559. doi: 10.1097/00005768-199911001-00011. [DOI] [PubMed] [Google Scholar]
- 36.Goldfield GS. Raynor H. Epstein LH. Treatment of pediatric obesity. In: Wadden T, editor; Stunkard A, editor. Handbook of Obesity Treatment. Guilford Press; New York: 2002. pp. 532–555. [Google Scholar]
- 37.Kassirer JP. The next transformation in the delivery of health care. N Engl J Med. 1995;332:52–54. doi: 10.1056/NEJM199501053320110. [DOI] [PubMed] [Google Scholar]
- 38.Fox S. Washington DC: Pew Research Center's Internet & American Life Project; 2011. [Dec 8;2012 ]. Health Topics. [Google Scholar]
- 39.Tuffrey C. Finlay F. Use of the internet by parents of paediatric outpatients. Arch Dis Child. 2002;87:534–536. doi: 10.1136/adc.87.6.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Murray E. Burns J. See TS, et al. Interactive health communication applications for people with chronic disease. Cochrane Database Syst Rev. 2005:CD004274. doi: 10.1002/14651858.CD004274.pub4. [DOI] [PubMed] [Google Scholar]
- 41.Barak A. Klein B. Proudfoot J. Defining internet-supported therapeutic interventions. Ann Behav Med. 2009;38:4–17. doi: 10.1007/s12160-009-9130-7. [DOI] [PubMed] [Google Scholar]
- 42.Fontaine KR. Allison DB. Obesity and the internet. In: Fairburn C, editor; Brownell K, editor. Eating Disorders and Obesity. 2nd. Guilford Press; New York: 2002. pp. 609–612. [Google Scholar]
- 43.McCoy MR. Couch D. Duncan ND, et al. Evaluating an internet weight loss program for diabetes prevention. Health Promot Int. 2005;20:221–228. doi: 10.1093/heapro/dai006. [DOI] [PubMed] [Google Scholar]
- 44.Rothert K. Strecher VJ. Doyle LA, et al. Web-based weight management programs in an integrated health care setting: A randomized, controlled trial. Obesity. 2006;14:266–272. doi: 10.1038/oby.2006.34. [DOI] [PubMed] [Google Scholar]
- 45.Tate DF. Jackvony EH. Wing RR. Effects of internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: A randomized trial. JAMA. 2003;289:1833–1836. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- 46.Tate DF. Wing RR. Winett RA. Using internet technology to deliver a behavioral weight loss program. JAMA. 2001;285:1172–1177. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- 47.Bond GE. Burr R. Wolf FM, et al. The effects of a web-based intervention on the physical outcomes associated with diabetes among adults age 60 and older: A randomized trial. Diabetes Technol Ther. 2007;9:52–59. doi: 10.1089/dia.2006.0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Winett RA. Tate DF. Anderson ES, et al. Long-term weight gain prevention: A theoretically based Internet approach. Prev Med. 2005;41:629–641. doi: 10.1016/j.ypmed.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 49.Womble LG. Wadden TA. McGuckin BG, et al. A randomized controlled trial of a commercial internet weight loss program. Obes Res. 2004;12:1011–1018. doi: 10.1038/oby.2004.124. [DOI] [PubMed] [Google Scholar]
- 50.Micco M. Gold EC. Buzzell P, et al. Internet weight loss: Stand-alone intervention or adjunct to traditional behavioral treatment? Ann Behav Med. 2007;33:49–56. doi: 10.1207/s15324796abm3301_6. [DOI] [PubMed] [Google Scholar]
- 51.Saperstein SL. Atkinson NL. Gold RS. The impact of Internet use for weight loss. Obes Res. 2007;8:459–465. doi: 10.1111/j.1467-789X.2007.00374.x. [DOI] [PubMed] [Google Scholar]
- 52.Weinstein PK. A review of weight loss programs delivered via the Internet. J Cardiovasc Nurs. 2006;21:251–258. doi: 10.1097/00005082-200607000-00003. [DOI] [PubMed] [Google Scholar]
- 53.Winett RA. Roodman AA. Winett SG, et al. The effects of Eat4Life internet-based health behavior program on the nutrition and activity practices of high school girls. J Gender Culture Health. 1999;4:239–254. [Google Scholar]
- 54.Williamson DA. Martin PD. White MA, et al. Efficacy of an internet-based behavioral weight loss program for overweight adolescent African-American girls. Eat Weight Disord. 2005;10:193–203. doi: 10.1007/BF03327547. [DOI] [PubMed] [Google Scholar]
- 55.Williamson D. Walden H. White M, et al. Two-year Internet-based randomized controlled trial for weight loss in African-American girls. Obesity. 2006;14:1231–1243. doi: 10.1038/oby.2006.140. [DOI] [PubMed] [Google Scholar]
- 56.Long JD. Armstrong MI. Amos E, et al. Pilot using World Wide Web to prevent diabetes in adolescents. Clin Nurs Res. 2006;15:67–79. doi: 10.1177/1054773805282446. [DOI] [PubMed] [Google Scholar]
- 57.Frenn M. Malin S. Brown RL, et al. Changing the tide: An Internet/video exercise and low-fat intervention with middle-school students. Appl Nurs Res. 2005;18:13–21. doi: 10.1016/j.apnr.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 58.Jago R. Baranowski T. Baranowski J, et al. Fit for life Boy Scout badge: Outcome evaluation of a troop and internet intervention. Prev Med. 2006;42:181–187. doi: 10.1016/j.ypmed.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 59.Thompson D. Baranowski J. Cullen K, et al. Development of a theory-based internet program promoting maintenance of diet and physical activity change to 8-year-old African American girls. Computers Educ. 2007;48:446–459. [Google Scholar]
- 60.Delamater AM. Jent J. Moine CT, et al. Empirically supported treatment of overweight adolescents. In: Jelalian E, editor; Steele R, editor. Handbook of Child and Adolescent Obesity. Springer; New York: 2008. pp. 221–239. [Google Scholar]
- 61.Woodruff SI. Edwards CC. Conway TL, et al. Pilot test of an internet virtual world chat room for rural teen smokers. J Adolesc Health. 2001;29:239–243. doi: 10.1016/s1054-139x(01)00262-2. [DOI] [PubMed] [Google Scholar]