Abstract
Introduction:
One in 5 young adults in the United States currently smoke, and young adults are less likely than other smokers to make aided quit attempts. Telephone quitlines may be a useful tool for treating this population. This study tested a quitline-based smoking cessation intervention versus mailed self-help materials in smokers 18–24 years old.
Methods:
This was a 2-group randomized clinical trial. The quitline-based counseling intervention (CI) included up to 4 proactive telephone counseling sessions; participants in the self-help (SH) group received only mailed cessation materials. Participants included 410 young adults who had smoked at least 1 cigarette in the past 30 days and who called the Wisconsin Tobacco Quit Line (WTQL) for help with quitting. Primary study outcomes included whether or not a quit date was set, whether or not a serious quit attempt was undertaken, and self-reported 7-day point-prevalence abstinence at 1-, 3-, and 6-month postenrollment.
Results:
The CI and SH groups did not differ in the intent-to-treat abstinence analyses at any of the follow-ups. However, the CI group was significantly more likely to set a quit date at 1-month postenrollment. Follow-up response rates were low (67.8% at 1 month; 53.4% at 3 months; and 48.3% at 6 months) reflecting lower motivation to participate in this kind of research.
Conclusions:
Relative to self-help, quitline counseling motivated young adults to set a quit date but abstinence rates were not improved. Research is needed on how to motivate young adult smokers to seek cessation treatment including quitline services.
INTRODUCTION
In 2010, approximately 20.1% of U.S. young adults 18–24 years old were current smokers (Centers for Disease Control and Prevention, 2011a). However, compared to older smokers, young adults are less likely to receive health professional advice to quit (31.1% vs. >44% for adults 25 years and older) and are less likely to use cessation counseling and/or medication (15.8% vs. >29% for adults 25 years and older) (Centers for Disease Control and Prevention, 2011b; see also Messer, Trinidad, Al-Delaimy, & Pierce, 2008). However, a majority (66.7%) of young adult smokers report being interested in quitting and approximately 62% made an attempt to quit in the past year (Centers for Disease Control and Prevention, 2011b).
In a systematic review of cessation interventions for young adults, Villanti, McKay, Abrams, Holtgrave, and Bowie (2010) found only limited evidence that existing cessation interventions for young adult smokers are efficacious. However, Villanti and colleagues identified three studies with promising interventions characterized by individual tailoring along with extended support via telephone, quitline, web, or E-mail: An et al. (2008), Rabius, McAlister, Geiger, Huang, and Todd (2004), and Zanis et al. (2011). Quit rates at 2–3 months in these three studies varied considerably with the highest rates in college students who received extended support (42.8%; An et al., 2008) and the lowest in young adult smokers who received brief quitline counseling (6.7%; Zanis et al., 2011). In sum, data suggest that young adult smokers are motivated to quit, but they tend to make quit attempts without assistance and little is known about optimal interventions for young adult smokers. Taken together, these findings highlight the importance of developing and identifying effective tobacco prevention and cessation interventions for young adult smokers.
Proactive telephone counseling may be an appropriate cessation strategy for young adult smokers because there is a large evidence base documenting its clinical and cost-effectiveness among adults (Abrams, Graham, Levy, Mabry, & Orleans, 2010; Centers for Disease Control and Prevention, 2007; Fiore et al., 2008; Lichtenstein, Zhu, & Tedeschi, 2010; Stead, Perera, & Lancaster, 2006; Zhu, Melcer, Sun, Rosbrook, & Pierce, 2000; Zhu et al., 2002); the widespread availability of telephones in the United States ensures its potential reach; it can be promoted and disseminated through existing programs with few implementation barriers; and it can be linked to the delivery of smoking cessation interventions provided in health care settings (e.g., Cummins, Hebert, Anderson, Mills, & Zhu, 2007; Kobinsky, Redmond, Smith, Yepassis-Zembrou, & Fiore, 2010).
Although telephone quitlines have been found to be an effective way to reach young adult smokers (Cummins et al., 2007), only two studies have addressed their effectiveness with this population. In one study noted above, Rabius et al. (2004) examined cessation rates in young adults randomized to self-help or quitline counseling, with the counseling group demonstrating a significantly higher abstinence rate at 6 months than did the SH group (9.8% vs. 3.2%, respectively). In contrast, Zanis et al. (2011) found that a brief face-to-face treatment intervention with a health educator yielded a higher 30-day abstinence rate at the 3-month follow-up (19.8%) compared to a brief quitline intervention (10.2%) but the difference was not statistically significant (odds ratio = 2.61; 95% confidence interval: 0.97, 6.98; reported by Villanti et al., 2010). Thus, there is some evidence that quitline counseling enhances cessation rates, even though the results were significant in only one study.
The current study was designed to provide additional data on the effects of proactive telephone quitline counseling in young adult smokers. Specifically, it was designed to determine if such counseling, when paired with mailed self-help materials, is more effective than mailed self-help materials alone in motivating young adult smokers to set a quit date, make a serious quit attempt, and/or quit smoking.
METHODS
Setting
This study was conducted by the Center for Tobacco Research and Intervention (CTRI) at the University of Wisconsin (UW) School of Medicine and Public Health, Madison, WI in collaboration with the State of Wisconsin’s tobacco quitline vendor, Free & Clear, Inc. [now called Alere Wellbeing], Seattle, WA. Institutional Review Board (IRB) approval for the study was granted by the UW Health Sciences IRB.
Participants and Recruitment for Current Study
The original goal of this study was to examine the effectiveness of quitline counseling for adolescent callers only. Due to difficulties in recruiting adolescent smokers via the Wisconsin Tobacco Quit Line (WTQL) in a pilot study, the sample age range in the current study was expanded to include young adult callers, age 18–24 years in addition to adolescent callers 13–17 years of age. In the current study, we were only able to recruit 52 adolescents out of a total of 462 clinical trial participants. Because few adolescents were recruited, and because their counseling intervention differed from that given to young adults, we dropped the adolescents from analyses and present results only for the 410 young adult participants.
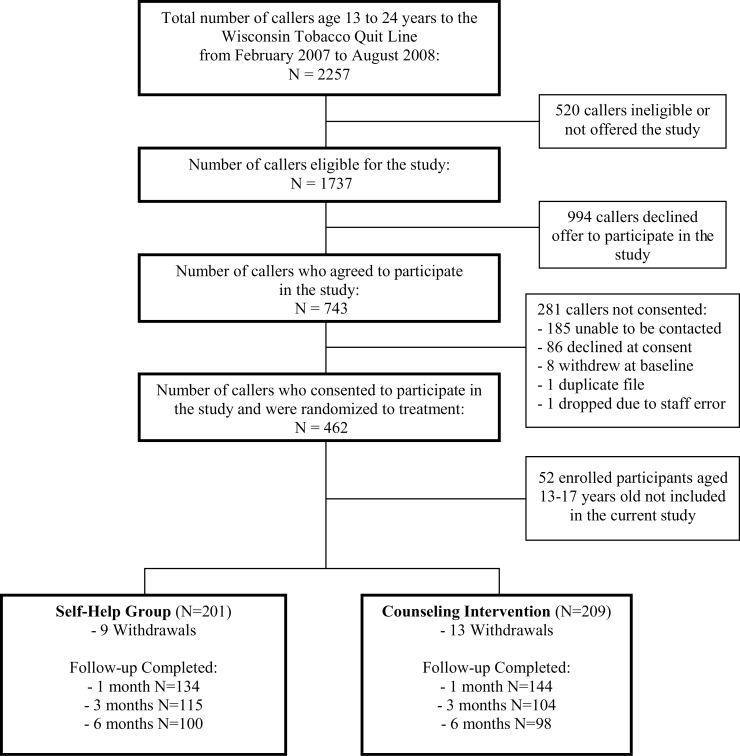
Recruitment for the current study occurred from February 2007 through August 2008; the study was publicized in Wisconsin through flyers at schools, radio spots, and press releases. Most recruitment came from general media advertising urging people of all ages to contact the WTQL. Eligibility criteria included: age 18–24 years; having smoked at least one cigarette within the last 30 days; and being interested in quitting within the next 3 months. Exclusion criteria included: unwilling to be randomized to treatment; use of only noncigarette forms of tobacco (i.e., not a cigarette smoker but other tobacco products were being used); and pregnancy. WTQL intake specialists obtained verbal consent by phone from eligible callers interested in participating; those who consented were randomized to either self-help (SH) or a quitline-based counseling intervention (CI) that included up to four proactive telephone counseling sessions (in which quitline Quit Coaches made calls to study participants). As shown in the Consolidated Standards of Reporting Trials (CONSORT) diagram (Figure 1), 201 young adults smokers were randomized to the SH group and 209 were randomized to the CI group. Participants in the study were not required to set a quit date at the time of study enrollment. Gift cards worth up to $105 were provided for participating in the study; participants received a $10 card for enrolling in the study; a $10 card for completing the 1-month follow-up call; a $15 card for the 3-month follow-up call; two $10 cards for the 6-month follow-up call; and $50 in gift cards for completing an in-person visit for biochemical verification of self-reported abstinence.
Figure 1.
Consolidated Standard for Reporting Clinical Trials (CONSORT) diagram.
Baseline Measures and Randomization to Treatment
After consent was obtained, standard baseline information was collected by WTQL staff during the initial call to the quitline. Baseline information included sociodemographic questions; smoking history and smoking cessation questions; items and scales from the Wisconsin Inventory of Smoking Dependence Motives (Piper et al., 2004); and the Modified Fagerström Tolerance Questionnaire (Prokhorov, Koehly, Pallonen, & Hudmon, 1998; Prokhorov, Pallonen, Fava, Ding, & Niaura, 1996). Quitline staff (in Seattle, WA) randomized callers to either the SH group or the CI group using a list of randomized numbers; university-based follow-up interviewers (in Madison, WI) were unaware of participants’ treatment group assignment.
Interventions
SH Group
Participants randomized to the SH group received no cessation counseling during the initial call to the quitline other than general rapport building during the consent and baseline survey. After randomization, SH group participants were told that they would receive mailed self-help materials. These materials consisted of smoking cessation booklets that the WTQL routinely provided to adult callers to the quitline. No subsequent proactive assistance from the WTQL was offered to SH participants but they could initiate a call to the WTQL during the study for assistance (very few made these calls).
The self-help materials provided to participants in both treatment groups (SH and CI) were a series of quitting guides based on self-reported stage of change (e.g., contemplation, preparation, or action stages; Prochaska & DiClemente, 1983; Prochaska, Velicer, Prochaska, & Johnson, 2004). These quit guides, the Be Free series developed by Free & Clear, were written at a fourth grade reading level, reviewed by a Scientific Advisory Group, and evaluated in focus groups. The first quit guide, provided at enrollment, was designed for smokers in the precontemplation and contemplation stages of quitting; the second quit guide was designed for smokers in the preparation and action stages of quitting; the third booklet was designed for smokers in the maintenance stage of quitting. Both SH and CI participants received the initial mailed materials based on stage of change at enrollment. However, CI participants could receive additional quit guides if they transitioned to a new stage of change (as assessed by WTQL counselors).
Quitline CI Group
Subjects randomized to the CI group received the mailed self-help materials described above and up to four proactive calls from WTQL counselors specially trained to provide cessation counseling to youth and adults. Counseling protocols were based on protocols developed in the seminal National Cancer Institute-funded study by Orleans et al. (1991) (see also Curry, Grothaus, McAfee, & Pabiniak, 1998; Hollis et al., 2007) and recommendations in the 2008 U.S. Public Health Service Clinical Practice Guideline, Treating Tobacco Use and Dependence (Fiore et al., 2008). The counseling protocol consisted of evidence-based counseling that included discussion of smoking history, prior quit attempts, setting a quit date, planning and skill development, problem-solving, and relapse-prevention strategies. Counselors also discussed FDA-approved cessation medications but medications were not provided by the WTQL to study participants; instead, CI participants were advised to discuss medications with their physician. The four proactive calls were scheduled to be completed within a 4–6-week timeframe (approximately every 1–2 weeks); multiple attempts were made to reach participants for each call.
Measures Collected by WTQL Counselors
During the initial counseling call with participants, WTQL staff assessed stage of change, prior use of Nicotine replacement therapy (NRT), and reasons for wanting to quit smoking. Data collected during subsequent calls included stage of change, whether a quit attempt had occurred, and, if so, the date of the quit attempt. The total number of calls (range: zero to four) and the total minutes of counseling were recorded and explored in secondary outcome analyses. For purposes of analysis, the number of calls completed was dichotomized: no or one call = 0 (representing minimal utilization) versus two to four calls = 1.
Follow-up Data
Study participants were called by UW-CTRI interviewers at 1, 3, and 6 months following the enrollment date; interviewers were unaware of participant treatment group assignment. Multiple attempts were made to reach each participant as follows: daily calls for 2 weeks at the 1- and 3-month follow-ups, daily calls for 3 weeks at the 6-month follow-up; if no success in the first 2–3 weeks, interviewers called twice weekly for an additional 2 weeks and then once weekly for at least another 2 weeks. Primary outcome measures were whether a quit date was set by a participant since enrolling in the study; whether a serious quit attempt occurred (defined as no smoking for at least 24hr); and smoking status (abstinent vs. smoking) during the 7 days prior to the follow-up call (“Have you smoked a cigarette, even a single puff, in the past 7 days?”). Self-reported abstinence was not biochemically confirmed. Participants were also asked about any use of over-the-counter or prescription cessation medicines; this information was explored in secondary analyses.
Statistical Analyses
All statistical tests were two-tailed; alpha was set at p < .05. χ2 tests and t tests were used for group comparisons. Due to considerable missing data at each of the three follow-ups that increased over time, multiple imputation to account for missing data was deemed inappropriate (Barnes, Larsen, Schroeder, Hanson, & Decker, 2010). For the three primary outcomes, we conducted both intent-to-treat (ITT) and responder-only analyses at each of the three postenrollment study end points (1, 3, and 6 months). For the ITT analysis, missing data were handled as follows: for the outcomes of setting a quit date (yes/no) and making a quit attempt (yes/no), missing was treated as no; for 7-day point-prevalence abstinence, missing was treated as smoking (i.e., that participants who did not complete a follow-up assessment were smoking). ITT and responder-only analyses for testing SH versus CI group differences for the three primary outcomes were computed using logistic regression.
We also conducted a set of secondary analyses examining study participation in relation to participant sociodemographic characteristics (gender, age, race, and education) and smoking history variables (baseline cigarettes per day [CPD], age when daily smoking started, time to first cigarette after waking, and smoking environment). Study participation was indexed by counseling call completion (no or one counseling calls completed vs. two to four calls) and follow-up call completion (no or one follow-up calls completed vs. two or three calls). Race was coded as White versus non-White; smoking environment was coded as no smokers present at home or at work versus smokers present at home or work (or both). χ2 tests and t tests were used for group comparisons. Because these were post hoc analyses involving tests on eight different participant characteristics, we used the Benjamini–Hochberg procedure to control the Type I error rate (Benjamini & Hochberg, 1995; Keselman, Cribbie, & Holland, 2002).
Lastly, we report results of an exploratory analysis of cessation medication use by study participants. This exploratory analysis was motivated, in part, by conflicting findings about the effects of cessation medication in real-world contexts. While such medications have produced evidence of benefit in some studies, such as those examining medication effects in over-the-counter contexts (Fiore et al., 2008; Shiffman and Sweeney, 2008), some survey and longitudinal studies have found little evidence that medication use is associated with greater likelihood of successful cessation (e.g., Messer et al., 2008; Pierce, Cummins, White, Humphrey, & Messer, 2012). Among 278 participants who completed the 1-month follow-up, 72 reported using a cessation medication. In these exploratory analyses, we used χ2 tests to the effect of medication use (yes, no) on the three primary outcomes using the responder-only sample. Because these were post hoc tests on three outcomes, we used a Bonferroni-corrected alpha of .017 to evaluate statistical significance. Also, we used logistic regression to test the interaction of treatment group and medication use.
Sample Size and Power to Detect Predicted Effects
In the original study protocol, the study sample size was set at 460 to have sufficient power (80%; two-tailed test; α = 0.05) to detect a statistically significant group difference in predicted 7-day point-prevalence abstinence rates at 6-month postenrollment of 15% in the SH group versus 25% in the CI group. The achieved sample size of 410 young adults has power of 71% to detect the predicted 6-month effect size.
RESULTS
Treatment Group Comparisons for Baseline Measures
Table 1 provides descriptive statistics for baseline sociodemographic and smoking history variables by treatment group. There were no group differences on any of the baseline measures. Other baseline variables were available only for the CI group participants (data collected by WTQL counselors during the first counseling call). These variables included prior use of NRT, for which 33% of young adults reported such use, and reasons for quitting, with health reasons being the most common (74%) followed by family reasons (37%) and the cost of cigarettes (33%).
Table 1.
Descriptive Statistics for Baseline Sociodemographic and Smoking History Variables by Treatment Group
| Baseline characteristics/measures | Self-help group (N = 201) | Counseling intervention group (N = 209) | p value |
|---|---|---|---|
| Female | 57.2% | 61.2% | .41 |
| Race | .68 | ||
| White | 74.9% | 78.8% | |
| African-American | 14.6% | 10.6% | |
| American Indian/Alaska native | 5.5% | 5.3% | |
| Other | 5.0% | 5.3% | |
| Hispanic | 3.5% | 6.2% | .21 |
| Age (years) when first smoked regularlya, mean (SD) | 15.0 (2.8) | 14.7 (2.8) | .20 |
| Number of cigarettes smoked per day, mean (SD) | 15.4 (10.4) | 16.1 (10.6) | .49 |
| Other tobacco use: Cigars | 4.5% | 2.4% | .25 |
| Other tobacco use: smokeless | 4.0% | 5.3% | .54 |
| mFTQb, mean (SD) | 4.8 (1.7) | 4.9 (1.8) | .80 |
| Time to first cigarette after waking | .58 | ||
| Within 5 min | 43.1% | 43.6% | |
| 6–30 min | 31.3% | 30.9% | |
| 31–60 min | 10.3% | 13.7% | |
| Longer than 1 hr | 15.4% | 11.8% | |
| WISDMc subscales, mean (SD) | |||
| Craving | 5.3 (1.6) | 5.2 (1.5) | .92 |
| Cue exposure | 5.5 (1.4) | 5.4 (1.3) | .72 |
| Negative reinforcement | 4.8 (1.5) | 4.5 (1.6) | .09 |
| Environmental goads | 5.2 (1.8) | 5.5 (1.6) | .21 |
| Weight control | 2.7 (1.7) | 2.7 (1.7) | .88 |
| Around other smokers? | .81 | ||
| At home only | 34.5% | 31.7% | |
| At work only | 21.5% | 22.1% | |
| Both home and work | 25.0% | 28.8% | |
| Neither home nor work | 19.0% | 17.3% | |
aRegularly = smoking one or two times per week.
bmFTQ = Modified Fagerström Tolerance Questionnaire (Prokhorov et al., 1996; Prokhorov et al., 1998).
cWISDM = Wisconsin Inventory of Smoking Dependence Motives (Piper et al., 2004); rated on a 1–7 response scale, where 1 = “Not True of Me At All” and 7 = “Extremely True of Me.”
Counseling Intervention Utilization and Follow-up
Nearly 10% of the CI participants (N = 20 out of 209) failed to complete even a single counseling call; these participants enrolled in the study but lacked time during the initial call to the WTQL to be transferred to a counselor and never followed through on any subsequent calls. Twenty-six percent of CI participants completed one call, 29% completed two calls, 22% completed three calls, and only 14% completed all four calls (mean number of calls completed = 2.05, SD = 1.20). The mean total minutes of counseling was 41 (SD = 25). For a participant who did not complete a given counseling call, quitline counselors made, on average, about five calls in an effort to reach the participant.
For the entire sample of 410 participants, 89 (21.7%) failed to complete any follow-up interviews, 83 (20.2%) completed only one follow-up, 102 (24.9%) completed two follow-ups, and 136 (33.1%) completed all three follow-ups. Overall response rates at each of the follow-ups were 67.8% at 1 month; 53.4% at 3 months; and 48.3% at 6 months. There were no treatment group differences in response rates at any of the three follow-ups.
For the participants in the CI group, there was a strong association between the number of counseling sessions completed and the number of follow-up calls completed, χ2(df = 12) = 44.17, p < .001.
Primary Outcomes for Young Adult Participants (N = 410)
As shown in Table 2, the CI group was significantly more likely to set a quit date (59.8%) than the SH group (43.3%; p < .002) at 1-month postenrollment in the ITT analysis as well as in the responder-only analysis (p < .001). This effect was not found at the subsequent study end points except in the responder-only analysis (p = .003) at 6 months. The groups did not differ in the percentage of participants who actually reported making a quit attempt at any of the study end points. Similarly, the groups did not differ in percentage abstinent at any of the study end points for either the ITT or responder-only analysis.
Table 2.
Primary Study Outcomes by Treatment Condition
| Outcome | Self-help group | Counseling intervention group | Odds ratio (95% CI) | p value | ||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| % Setting a quit date | ||||||
| 1-month follow-up | ||||||
| Intent-to-treat | 201 | 43.3% | 209 | 59.8% | 1.95 (1.32–2.89) | <.002 |
| Responder only | 134 | 64.9% | 144 | 86.8% | 3.56 (1.95–6.47) | <.001 |
| 3-Month follow-up | ||||||
| Intent-to-treat | 201 | 42.3% | 209 | 41.6% | 0.97 (0.66–1.44) | .89 |
| Responder only | 115 | 73.9% | 104 | 83.7% | 1.81 (0.93–3.52) | .08 |
| 6-Month follow-up | ||||||
| Intent-to-treat | 201 | 37.3% | 209 | 42.6% | 1.25 (0.84–1.85) | .28 |
| Responder only | 100 | 75.0% | 98 | 90.8% | 3.30 (1.45–7.50) | .003 |
| % Making a quit attempt | ||||||
| 1-Month follow-up | ||||||
| Intent-to-treat | 201 | 38.8% | 209 | 39.7% | 1.04 (0.70–1.54) | .85 |
| Responder only | 134 | 58.2% | 144 | 57.6% | 0.98 (0.61–1.57) | .92 |
| 3-Month follow-up | ||||||
| Intent-to-treat | 201 | 31.3% | 209 | 24.9% | 0.73 (0.47–1.12) | .15 |
| Responder only | 115 | 54.8% | 104 | 50.0% | 0.83 (0.49–1.41) | .48 |
| 6-Month follow-up | ||||||
| Intent-to-treat | 201 | 30.8% | 209 | 31.1% | 1.01 (0.67–1.54) | .96 |
| Responder only | 100 | 62.0% | 98 | 66.3% | 1.21 (0.68–2.16) | .53 |
| % Abstinent at 1 month | ||||||
| 1-Month follow-up | ||||||
| Intent-to-treat | 201 | 8.5% | 209 | 11.0% | 1.34 (0.69–2.59) | .39 |
| Responder only | 134 | 12.7% | 144 | 15.3% | 1.24 (0.63–2.45) | .53 |
| 3-Month follow-up | ||||||
| Intent-to-treat | 201 | 7.5% | 209 | 8.1% | 1.10 (0.53–2.26) | .80 |
| Responder only | 115 | 13.0% | 104 | 16.3% | 1.30 (0.61–2.76) | .49 |
| 6-Month follow-up | ||||||
| Intent-to-treat | 201 | 6.5% | 209 | 6.7% | 1.04 (0.48–2.27) | .93 |
| Responder only | 100 | 13.0% | 98 | 14.3% | 1.12 (0.50–2.51) | .79 |
Primary Outcomes in the CI Group by Counseling Utilization
Participants who had two or more counseling sessions were somewhat more likely to report making a quit attempt (44.4%) compared to participants who had zero or one session (31.1%; p = .06). Similarly, the group of participants who had more counseling sessions had a marginally significant higher abstinence rate (14.1%) compared to participants with fewer counseling sessions (5.4%; p = .06).
Participant Characteristics and Study Participation
As shown in Table 3, the only participant characteristic that was associated with counseling call completion was education (after applying the Benjamini–Hochberg procedure to control the Type I error rate). More specifically, participants with less education (i.e., not completing a high school degree) were less likely to complete more than one counseling call. In contrast, several participant characteristics were associated with follow-up call completion after applying the Benjamini–Hochberg correction for multiple tests. Sociodemographic characteristics associated with completing no or only one follow-up calls included less education, race other than White, a higher baseline smoking rate, younger age when daily smoking started, smoking a cigarette in the first 30min after waking, and having smokers in the home or at work. Table 3 also shows that participants completing no or only one follow-up call engaged in significantly fewer minutes of quitline counseling (32.5 vs. 47.4min for participants who completed 2 or 3 follow-up calls).
Table 3.
Participant Characteristics by Counseling Call Completion and Follow-up Call Completion Only
| Participant characteristic | 0 or 1 counseling calls completeda | 2–4 counseling calls completeda | Test value | Unadjusted p value | ||
|---|---|---|---|---|---|---|
| N | % or mean (SD) | N | % or mean (SD) | |||
| Age, years | 74 | 21.2 (1.7) | 135 | 21.4 (1.9) | t(df = 207) = −0.40 | .691 |
| Gender, % female | 74 | 62.2% | 135 | 60.7% | χ2(df = 1) = 0.04 | .840 |
| Race, % White | 74 | 73.0% | 134 | 82.1% | χ2(df = 1) = 2.38 | .123 |
| Education, % completing less than 12th grade | 73 | 34.2% | 135 | 14.8% | χ2(df = 1) = 7.64 (linear by linear) | .006* |
| Baseline cigarettes per day | 74 | 17.0 (11.2) | 135 | 15.7 (10.2) | t(df = 207) = 0.86 | .389 |
| Age started smoking daily | 73 | 14.1 (2.5) | 131 | 15.0 (2.9) | t(df = 207) = −2.13 | .034 |
| Time to first cigarette after waking, % ≤30 min | 71 | 78.9% | 133 | 72.2% | χ2(df = 1) = 1.09 | .296 |
| Smokers at home or work, % saying no | 73 | 19.2% | 135 | 16.3% | χ2(df = 1) = 0.28 | .600 |
| Participant characteristic | 0 or 1 follow-up calls competed | 2 or 3 follow-up calls competed | χ2 value or t test value | Unadjusted p value | ||
| N | % or mean (SD) | N | % or mean (SD) | |||
| Age, years | 172 | 21.3 (1.9) | 238 | 21.3 (2.0) | t(df = 207) = −.02 | .983 |
| Gender, % female | 172 | 57.6% | 238 | 60.5% | χ2(df = 1) = 0.36 | .549 |
| Race, % White | 170 | 71.8% | 237 | 80.6% | χ2(df = 1) = 4.34 | .037* |
| Education, % completing less than 12th grade | 171 | 26.9% | 237 | 16.0% | χ2(df = 1) = 13.15 (linear by linear) | .0003* |
| Baseline cigarettes per day | 172 | 17.1 (11.7) | 238 | 14.8 (9.4) | t(df = 207) = 2.22 | .027* |
| Age started smoking daily | 169 | 14.4 (2.7) | 233 | 15.1 (2.8) | t(df = 207) = −2.41 | .017* |
| Time to first cigarette after waking, % ≤30 min | 168 | 81.0% | 231 | 69.7% | χ2(df = 1) = 6.48 | .011* |
| Smokers at home or work, % saying no | 170 | 12.9% | 238 | 21.8% | χ2(df = 1) = 5.30 | .021* |
| Total minutes of quitline counselinga | 92 | 32.5 (22.6) | 117 | 47.4 (25.1) | t(df = 207) = −4.46 | <.0001* |
aCounseling intervention participants only.
*Statistically significant after Benjamini–Hochberg procedure to control the Type I error rate (Benjamini & Hochberg, 1995; Keselman, Cribbie, & Holland, 2002).
Exploratory Analysis of Cessation Medication Use
Study treatment did not include provision of cessation medication. However, at the 1-month follow-up, 72 participants (17.5% of the total sample; 25.9% of the responder-only sample) reported using cessation medications: 22 used nicotine gum, 32 used nicotine patch, 8 used nicotine lozenge, 3 used the nicotine inhaler, 5 used bupropion SR, and 18 used varenicline (some individuals used more than one medication). We conducted exploratory analyses of medication use in relation to the 3 primary outcomes in the 278 participants (67.8% response rate for the total sample) who completed the 1-month follow-up call (responder-only analysis). Bonferroni-corrected results of initial exploratory analyses showed that medication users, relative to nonusers, were more likely to set a quit date (87.5% vs. 72.3%, respectively; χ2(df = 1) = 6.78, p = .009) and to report being abstinent (31.9% vs. 7.7%, respectively; χ2(df = 1) = 25.86, p < .0001). A higher percentage of medication users reported making a serious quit attempt compared to nonusers (69.4% vs. 53.9% %, respectively; χ2(df = 1) = 5.30, p = .021) but the difference was not statistically significant with Bonferroni correction. We also tested whether or not the effect of medication use on the primary outcomes varied by treatment group; more specifically, we tested logistic regression models that included the interaction of treatment group with medication use. These analyses yielded no significant interactions.
DISCUSSION
Analyses of primary outcomes for young adults showed that, relative to self-help, quitline counseling significantly increased the likelihood of setting a quit date at 1-month postenrollment not at the 3- or 6-month end points. Contrary to prediction, quitline counseling did not affect the likelihood of making a serious quit attempt or successfully quitting at any of the study end points.
Utilization of quitline counseling was fairly low. Only 35% of young adult callers completed three or four calls and nearly 10% of young adult participants completed no counseling calls at all. It should be noted that, although this study offered a monetary incentive for participation, it did not require participants to set a quit date. This is in keeping with routine practice at the tested quitline in which individuals can receive counseling despite not committing to making a quit attempt. However, this means that this study may have recruited participants low in quitting motivation, which could account for the relatively low counseling utilization as well as the lack of treatment differences in the overall ITT abstinence analyses. These findings suggest a need for improved triage and counseling of young adult smokers calling quitlines for assistance such that those lower in motivation to quit would receive more potent motivational treatment and those ready to quit would receive evidence-based cessation counseling and, if appropriate, pharmacotherapy (Baker et al., 2011; Fiore et al., 2008).
Analyses of counseling utilization showed that more intense quitline counseling (two or more sessions) was associated with better outcomes including greater quitting success in the young adult sample. It is possible that participants who engaged in more counseling were more motivated to quit and this may explain their higher abstinence rates. The current correlational findings argue for conducting additional research on counseling intensity in young smokers.
Given the lower-than-expected rates of study engagement (i.e., in counseling and follow-up), we explored participant characteristics in relation to counseling call completion as well as follow-up call completion. Due to the number and post hoc nature of these analyses, we controlled for potential inflation of the Type I error rate using the Benjamini–Hochberg procedure (Benjamini & Hochberg, 1995). Participants with less than a high school education were less likely to complete more than one counseling call than other participants but no other participant characteristic appeared to be associated with counseling engagement. In contrast, several participant characteristics were associated with follow-up call completion. More specifically, participants with a higher baseline smoking rate, earlier age of starting to smoke regularly, higher levels of nicotine dependence (indexed by time to first cigarette after waking), and having smokers at home or work were significantly less likely to complete more than one follow-up call. Also, lower education and non-White race were associated with lower follow-up participation. Since all these factors tend to be associated with cessation failure (e.g., Bolt et al., 2009), these findings suggest that participants’ inability to quit was, in part, responsible for their failure to engage in follow-up assessments. These findings may be informative for future studies of young adult smokers in terms of increasing study engagement and in drawing inferences regarding missingness. Given that lower treatment and follow-up participation rates were associated with certain sociodemographic characteristics (e.g., lower educational attainment, non-White) and heavier smoking, new tailored interventions are needed that address the special challenges of young adult smokers with these and other relapse risk factors (Audrain-McGovern et al., 2009; Cengalli, O’Loughlin, Lauzon, & Cornuz, 2011).
Although not originally a focus of the study, secondary analyses examined the relations of medication use with outcome because of conflicting findings about the effects of cessation medication in real-world contexts (e.g., Pierce and Gilpin, 2002; Reed, Anderson, Vaughn, & Burns, 2005). In our study, participants were not offered cessation medication but 72 of the 278 participants completing the 1-month follow-up reported using cessation medication. Analyses (with Bonferroni correction to account for the post hoc nature of these comparisons) showed that users of medication were significantly more likely to set a quit date (87.5% of cessation medication users vs. 72.3% of nonusers) and to report abstinence at 1 month (31.9% of medication users vs. 7.8% for nonusers). No differences in the effect of medication use on primary outcomes were found by treatment group. Thus, the current effectiveness trial shows that medication use is strongly related to cessation outcomes. These findings might be due to more motivated smokers choosing to use medication, or due to the beneficial effects of medication, or both. Moreover, interpretation of this finding must be highly tentative given the small sample size and rate of missingness in this dataset.
Limitations of the study include a somewhat modest sample size and relatively low response rates for the 3- and 6-month follow-ups that reduced confidence in results at the later study end points. Although the low response rate at 6 months makes it difficult to reliably estimate true group differences in abstinence, it is likely that the true effect size is smaller than what we predicted (15% in the SH group vs. 25% in the CI group) and, as such, the study was probably underpowered to detect a group difference in abstinence. Lower-than-expected response rates at all follow-up end points combined with modest counseling utilization likely contributed to the lower abstinence rates in the CI group and the lack of a significant overall difference in abstinence between the SH and CI interventions. Another limitation is that there was no evaluation of the use or helpfulness of the self-help materials. Also, the dose of intervention in the CI group was limited, with only a few counseling sessions and no study-related medication. Lastly, analyses of medication use were post hoc rather than planned analyses.
There are very few studies of quitline interventions for young adult smokers. The current study shows that quitline-based counseling may benefit young adults in spurring them to set a quit date. A meaningful portion of young adult participants (18% of the total sample; 26% of the responder-only sample) were motivated to obtain cessation medication independent of the study and we found that medication users were significantly more likely to set a quit date and to be more successful in quitting than were other participants not using cessation medications. However, analyses of cessation medications were post hoc reflecting the fact that there was no random assignment to medication conditions; therefore, no firm conclusions can be drawn regarding medication effects.
In summary, the results of this study suggest that the tested quitline intervention was relatively little used by these young adult smokers, and that the intervention had relatively little effect on abstinence rates. Further, the results point to the need for innovative treatment approaches for engaging young adults in a serious, aided, quit attempts. The results also suggest that the effects of cessation medication, as it is used in real-world contexts by the population, merit additional study. In addition, young adults with more severe nicotine dependence likely need additional treatment and support in order to achieve abstinence. Likewise, smokers with socioeconomic, educational, or other risk factors may benefit from more intensive or specialized interventions to increase engagement in treatment and to decrease relapse. Lastly, intervention efforts should be augmented by policy and prevention strategies including indoor smoke-free laws, higher tobacco product prices, and strong counter-advertising mass-media campaigns in order to reduce the initiation and prevalence of smoking in youth and young adults.
FUNDING
THS was supported by National Institute on Drug Abuse Grant 5K23DA017801, a grant from the Wisconsin Partnership Program at the University of Wisconsin School of Medicine and Public Health (UWSMPH), and a Clinical Research Scholar Award from the Clinical Investigator Preparatory Program at the UWSMPH. SSS, TBB, and MCF were supported by National Cancer Institute (NCI) Grant 9P50CA143188 and National Institute on Drug Abuse (NIDA) Grant 5P50DA019706. TBB was also supported by NCI Grant 5K05CA139871. TM was supported during the study by a research subcontract from the University of Wisconsin to Free & Clear (the quitline vendor for the WTQL; Free & Clear is now called Alere Wellbeing). The study was also supported by funding from the American Legacy Foundation (ALF). The findings of the study do not necessarily represent the views of ALF, ALF staff, or its Board of Directors. This study was completed prior to clinical registration mandates. University of Wisconsin Health Sciences IRB approval was granted, May 31, 2005.
DECLARATION OF INTERESTS
THS, DLF, TBB, MCF, and SSS have no financial disclosures to declare. TM, was employed by and owned stock in Free & Clear (now called Alere Wellbeing), the quitline vendor for the Wisconsin Tobacco Quitline, during the study. TM no longer owns stock in Free & Clear or Alere Wellbeing.
ACKNOWLEDGMENTS
The authors wish to acknowledge the following individuals from Alere Wellbeing (Seattle, WA) who contributed substantially to this project: Anne Perez-Cromwell for survey programming, Jennifer Pech Cinnamon for her general assistance with myriad essential tasks throughout the study, Mona Deprey for managing the study, and Susan Zbikowski for her preliminary review of the manuscript. Lastly, we thank the service delivery staff who provided services to the study participants.
REFERENCES
- Abrams D. B., Graham A. L., Levy D. T., Mabry P. L., Orleans C. T. (2010). Boosting population quits through evidence-based cessation treatment and policy. American Journal of Preventive Medicine, 38, S351–S363 doi:10.1016/j.amepre.2009.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- An L. C., Klatt C., Perry C. L., et al. (2008). The RealU online cessation intervention for college smokers: A randomized controlled trial. American Journal of Preventive Medicine, 47(2), 194–199 doi:10.1016/j.ypmed.2008.04.011 [DOI] [PubMed] [Google Scholar]
- Audrain-McGovern J., Rodriguez D., Epstein L. H., Rodgers K., Cuevas J., Wileyto E. P. (2009). Young adult smoking: What factors differentiate ex-smokers, smoking cessation treatment seekers and nontreatment seekers? Addictive Behaviors, 34, 1036–1041 doi:10.1016/j.addbeh.2009.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker T. B., Mermelstein R., Collins L. M., Piper M. E., Jorenby D. E., Smith S. S., et al., et al. (2011). New methods for tobacco dependence treatment research. Annals of Behavioral Medicine, 41(2), 192–207 doi:10.1007/s12160-010-9252-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes S. A., Larsen M. D., Schroeder D. R., Hanson A., Decker P. A. (2010). Missing data assumptions and methods in a smoking cessation study. Addiction, 105, 431–437 doi:10.1111/j.1360-0443.2009.02809.x [DOI] [PubMed] [Google Scholar]
- Benjamini Y., Hochberg Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society B, 57, 289–300 doi:10.2307/2346101 [Google Scholar]
- Bolt D. M., Piper M. E., McCarthy D. E., Japuntich S. J., Fiore M. C., Smith S. S., et al. (2009). The Wisconsin Predicting Patients’ Relapse questionnaire. Nicotine & Tobacco Research, 11, 481–492 doi:10.1093/ntr/ntp030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cengalli S., O’Loughlin J., Lauzon B., Cornuz J. (2011). A systematic review of longitudinal population-based studies on the predictors of smoking cessation in adolescent and young adult smokers. Tobacco Control, 21, 355–362 doi:10.1136/tc.2011.044149 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2007). Best Practices for Comprehensive Tobacco Control Programs—2007. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Retrieved from http://www.cdc.gov/tobacco/stateandcommunity/best_practices/pdfs/2007/bestpractices_complete.pdf [Google Scholar]
- Centers for Disease Control and Prevention (2011a). Vital signs: Current cigarette smoking among adults aged ≥ 18 years—United States, 2005–2010. Morbidity and Mortality Weekly Report, 60, 1207–1212 Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6035a5.htm?s_cid=mm6035a5_w [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2011b). Quitting smoking among adults—United States, 2001–2010. Morbidity and Mortality Weekly Report, 60, 1513–1519 Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6044a2.htm?s_cid=mm6044a2_w [PubMed] [Google Scholar]
- Cummins S. E., Hebert K. K., Anderson C. M., Mills J. A., Zhu S. H. (2007). Reaching young adult smokers through quitlines. American Journal of Public Health, 97, 1402–1405 doi:10.2105/AJPH.2006.101741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry S. J., Grothaus L. C., McAfee T., Pabiniak C. (1998). Use and cost effectiveness of smoking-cessation services under four insurance plans in a health maintenance organization. The New England Journal of Medicine, 339, 673–679 doi:10.1056/NEJM199809033391006 [DOI] [PubMed] [Google Scholar]
- Fiore M. C., Jaen C. R., Baker T. B., Bailey W. C., Benowitz N. L., Curry S. J., et al. (2008). Treating tobacco use and dependence: 2008 update. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; Retrieved from http://www.surgeongeneral.gov/tobacco/treating_tobacco_use08.pdf [Google Scholar]
- Hollis J. F., McAfee T. A., Fellows J. L., Zbikowski S. M., Stark M., Riedlinger K. (2007). The effectiveness and cost effectiveness of telephone counselling and the nicotine patch in a state tobacco quitline. Tobacco Control, 16, i53–i59 doi:10.1136/tc.2006.019794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keselman H. J., Cribbie R., Holland B. (2002). Controlling the rate of Type I error over a large set of statistical tests. British Journal of Mathematical and Statistical Psychology, 55, 27–40 doi:10.1348/000711002159680 [DOI] [PubMed] [Google Scholar]
- Kobinsky K. H., Redmond L. A., Smith S. S., Yepassis-Zembrou P. L., Fiore M. C. (2010). The Wisconsin Tobacco Quit Line’s Fax to Quit program: Participant satisfaction and effectiveness. Wisconsin Medical Journal, 109, 79–84 Retrieved from http://www.wisconsinmedicalsociety.org/_WMS/publications/wmj/pdf/109/2/79.pdf [PubMed] [Google Scholar]
- Lichtenstein E., Zhu S. H., Tedeschi G. J. (2010). Smoking cessation quitlines: An underrecognized intervention success story. American Psychologist, 65, 252–261 doi:10.1037/a0018598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer K., Trinidad D. R., Al-Delaimy W. K., Pierce J. P. (2008). Smoking cessation rates in the United States: A comparison of young adult and older smokers. American Journal of Public Health, 98, 317–322 doi:10.2105/AJPH.2007.112060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orleans C. T., Schoenbach V. J., Wagner E. H., Quade, D., Salmon, M. A., Pearson, D. C., et al., et al. (1991). Self-help quit smoking interventions: Effects of self-help materials, social support instructions, and telephone counseling. Journal of Consulting and Clinical Psychology, 59, 439–448 doi:10.1037/0022-006X.59.3.439 [DOI] [PubMed] [Google Scholar]
- Pierce J. P., Cummins S. E., White M. M., Humphrey A., Messer K. (2012). Quitlines and nicotine replacement for smoking cessation: Do we need to change policy? Annual Review of Public Health, 33, 341–356 doi:10.1146/annurev-publhealth-031811-124624 [DOI] [PubMed] [Google Scholar]
- Pierce J. P., Gilpin E. A. (2002). Impact of over-the-counter sales on effectiveness of pharmaceutical aids for smoking cessation. JAMA, 288, 1260–1264 doi:10.1001/jama.288.10.1260 [DOI] [PubMed] [Google Scholar]
- Piper M. E., Piasecki T. M., Federman E. B., Bolt D. M., Smith S. S., Fiore M. C., Baker T. B. (2004). A multiple motives approach to tobacco dependence: the Wisconsin Inventory of Smoking Dependence Motives (WISDM-68). Journal of Consulting and Clinical Psychology, 72, 139–154 doi:10.1037/0022-006X.72.2.139 [DOI] [PubMed] [Google Scholar]
- Prochaska J. O., DiClemente C. C. (1983). Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51, 390–395 doi:10.1037/0022-006X.51.3.390 [DOI] [PubMed] [Google Scholar]
- Prochaska J. O., Velicer W. F., Prochaska J. M., Johnson J. L. (2004). Size, consistency, and stability of stage effects for smoking cessation. Addictive Behaviors, 29, 207–213 doi:10.1016/S0306-4603(03)00086-8 [DOI] [PubMed] [Google Scholar]
- Prokhorov A. V., Koehly L. M., Pallonen U. E., Hudmon K. S. (1998). Adolescent nicotine dependence measured by the modified Fagerstrom Tolerance Questionnaire at two time points. Journal of Child & Adolescent Substance Abuse, 7, 35–47 doi:10.1300/J029v07n04_03 [Google Scholar]
- Prokhorov A. V., Pallonen U. E., Fava J. L., Ding L., Niaura R. (1996). Measuring nicotine dependence among high-risk adolescent smokers. Addictive Behaviors, 21, 117–127 [DOI] [PubMed] [Google Scholar]
- Rabius V., McAlister A. L., Geiger A., Huang P., Todd R. (2004). Telephone counseling increases cessation rates among young adult smokers. Health Psychology, 23, 539–541 doi:10.1037/0278-6133.23.5.539 [DOI] [PubMed] [Google Scholar]
- Reed M. B., Anderson C. M., Vaughn J. W., Burns D. M. (2005). The effect of over-the-counter sales of the nicotine patch and nicotine gum on smoking cessation in California. Cancer Epidemiology, Biomarkers & Prevention, 14, 2131–2136 doi:10.1158/1055–9965.EPI-04-0919 [DOI] [PubMed] [Google Scholar]
- Shiffman S., Sweeney C. T. (2008). Ten years after the Rx-to-OTC switch of nicotine replacement therapy: What have we learned about the benefits and risks of non-prescription availability? Health Policy, 86, 17–26 doi:10.1016/j.healthpol.2007.08.006 [DOI] [PubMed] [Google Scholar]
- Stead L., Perera R., Lancaster T. (2006). Telephone counselling for smoking cessation. Cochrane Database of Systematic Reviews, 3, CD002850 doi:10.1002/14651858.CD002850.pub2 [DOI] [PubMed] [Google Scholar]
- Villanti A. C., McKay H. S., Abrams D. B., Holtgrave D. R., Bowie J. V. (2010). Smoking-cessation interventions for U.S. young adults: A systematic review. American Journal of Preventive Medicine, 39, 564–574 doi:10.1016/j.amepre.2010.08.009 [DOI] [PubMed] [Google Scholar]
- Zanis D. A., Hollm R. F., Derr D., Ibrahim J. K., Collins B. N., et al. (2011). Comparing intervention strategies among rural, low SES, young adult tobacco users. American Journal of Health Behavior, 35, 240–247 doi/pii:10.5555/ajhb.2011.35.2.240 [DOI] [PubMed] [Google Scholar]
- Zhu S-H., Anderson C. M., Tedeschi G. J., Rosbrook B., Johnson C. E., Byrd M., Gutiérrez-Terrell E. (2002). Evidence of real-world effectiveness of a telephone quitline for smokers. New England Journal of Medicine, 347, 1087–1093 doi:10.1056/NEJMsa020660 [DOI] [PubMed] [Google Scholar]
- Zhu S-H., Melcer T., Sun J., Rosbrook B., Pierce J. P. (2000). Smoking cessation with and without assistance: A population-based analysis. American Journal of Preventive Medicine, 18, 305–311 doi/pii:S0749379700001240 [DOI] [PubMed] [Google Scholar]