Abstract
Aims
It is well-established that lipid disorder is an important cardiovascular risk factor, and failure to reach optimal lipid levels significantly contributes to the residual cardiovascular risks. However, limited information is available on the management and the attainment of recommended cholesterol targets in real-world practice in China.
Methods and Results
A nationally representative sample of 12,040 patients with dyslipidemia from 19 provinces and 84 hospitals across China were consecutively enrolled in this survey. Risk stratification and individual cholesterol target was established for all participants. This survey identified a high-risk cohort, with over 50% of patients had hypertension, 37.5% had coronary artery disease, and more than 30% had peripheral artery disease. Thirty-nine percent of all participants received lipid lowering medications. And the majority of them (94.5%) had statins (42.5% with atorvastatin, 29.0% with simvastatin, and 15.2% with rosuvastatin). However, the overall attainment for low-density lipoprotein cholesterol (LDL-C) target is low (25.8%), especially, in female (22.2%), and in patients with increased body mass index (BMI) (38.3% for BMI<18.5, 28.1% for BMI 18.5–24.9, 26.0% for BMI 25.0–29.9, and 17.4% for BMI≥30, P<0.0001). Subgroup analysis also showed the attainment is significantly lower in patients who were stratified into high (19.9%) and very high (21.1%) risk category. In logistic regression analysis, eight factors (BMI, gender, coronary artery disease, systolic and diastolic blood pressure, hypertension, family history of premature coronary artery disease and current smoking) were identified as independent predictors of LDL-C attainment.
Conclusions
Despite the proven benefits of lipid-lowering therapies, current management of dyslipidemia continues to be unsatisfied. A considerable proportion of patients failed to achieve guideline-recommended targets in China, and this apparent treatment gap was more pronounced among patients with increased BMI, higher risk stratification and women.
Introduction
The strong link between dyslipidemia and the risk of future cardiovascular events is well understood. [1]–[7] Previous studies have also demonstrated an important reduction in cardiovascular morbidity and mortality with low-density lipoprotein cholesterol (LDL-C) – lowering therapies. [8]–[12] Furthermore, the benefits of treatment appear more pronounced among patients with established cardiovascular disease or in those at high risk of developing cardiovascular disease. Therefore, the National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) guidelines highlight the importance of the LDL-C as the primary therapeutic target and recommend individualized treatment goals tailored to the estimated cardiovascular risk [1], [2]. And failure to reach recommended lipid goals is associated with increased risk of cardiovascular events [13]–[15]. However, despite the well-established efficacy of lipid-modifying therapy, limited data are available on guideline attainment in ambulatory patients with dyslipidemia in China.
We herein aimed to investigate (1) the current attainment of the recommended LDL-C targets among patients with dyslipidemia in Chinese outpatient clinic, (2) sex differences in attainment of guideline-recommended targets for patients with dyslipidemia, and (3) whether attainment of the recommended LDL-C targets are similar in ambulatory patients stratified by different risk category.
Methods
The Reality China survey is a multi-centre cross-sectional study involving 84 centers in 19 provinces in China. The sampling process was stratified according to geographic region (north, east, south central, northwest, and southwest China), and degree of urbanization (large cities [Beijing, Shanghai, and provincial capitals] and midsize cities) (Supplement S1). The first two stages of sampling, in which provinces were selected from geographic regions and cities were selected from provinces, were not random. In the next stage (the stage in which hospital or centers were selected from cities or townships), the sampling was random. Each center was asked to recruit at least 20 patients. Consecutive patients at an age ≥20 years were screened for a previously or newly diagnosed dyslipidemia when visiting the outpatient clinics. All patients were assessed and treated at the discretion of their physicians in charge according to the usual institutional practice. A standard case record form (CRF) was administered by trained staff to obtain information on demography, conventional risk factors for cardiovascular disease, family history of premature coronary artery disease (CAD), medical history and treatment. All study investigators and staff members completed a training program that they were given detailed instructions concerning the administration of the study CRF. The following data were obtained on enrolment day: weight, height, fasting plasma glucose, systolic and diastolic blood pressure and fasting blood lipids (total-, LDL- and high-density lipoprotein-cholesterol, triglycerides). Estimated glomerular filtration rate (eGFR) was calculated by modified MDRD equation [16] And if eGFR <60 ml/min/1.73 m [2], patients were defined as chronic kidney disease. If patient had more than one clinic visit during the study period, data from the index encounter were used to minimize overrepresentation by patients with multiple visits.
The assessment of risk factors was based on the NCEP ATP-III guidelines update [2] and included: age (≥45 years if male or ≥55 years if female), hypertension, low HDL cholesterol (<40 mg/dL), cigarette smoking, family history of premature CAD (first degree relatives before the age of 55 in men and 65 years in women). CAD risk equivalents included: stroke or transient ischemic attack, peripheral arterial disease, aortic abdominal aneurysms, diabetes, multiple risk factors and 10-year Framingham risk >20%. Risk assessment for determining 10-year CAD risk was carried out according to Framingham risk scoring. [1] Diabetes was defined according to medical records or at least two fasting glucose measurements ≥7.0 mmol/L during recruitment. Personal history of CAD and CAD risk equivalents was established according to patients' medical records. Participants were stratified into risk categories according to the cumulative number of risk factors and the Framingham risk score, as reported by the NCEP ATP-III guidelines. The following risk categories that modify LDL-C goals were generated: less than 160 mg/dL (4.14 mmol/L) if low risk (0–1 risk factor), less than 130 mg/dL (3.37 mmol/L) if moderate risk (≥2 risk factors and Framingham risk score 10–20%), less than 100 mg/dL (2.59 mmol/L) if high risk (CAD or CAD risk equivalents) and less than 70 mg/dL (1.81 mmol/L) for very high-risk patients (those who have had a recent heart attack, or have cardiovascular disease combined with diabetes). [2] All participants were investigated on whether they attained individualized LDL-C targets.
The study protocol was approved by the certified central Ethics Committee of An Zhen Hospital, Capital Medical University, Beijing, China. And written informed consent was obtained from all participants in this study.
Statistics
All case record form data were entered into two Epidata 3.02 databases by different people. The two databases were compared, and any necessary corrections were discussed and reassessed. The data were analyzed using SPSS statistical software 13.0. Categorical data are presented as frequencies (percentages), and the differences were compared by the x 2 test; continuous data are presented as mean value +− SD and the differences between groups were compared by the t test. The predictors of LDL-C target attainment failure were investigated by multivariable logistic regression analysis adjusted for baseline characteristics and all potential confounding factors, including demographic factors (age, BMI [categorical variable] and gender), clinical characteristics (diabetes, current smoking, hypertension, CAD, stroke/TIA, peripheral artery disease, chronic kidney disease, aortic abdominal aneurysms and family history of premature CAD), physical examination (systolic and diastolic blood pressure) and treatment status (administration of lipid lowering medication, adverse reaction events related to lipid lowering therapy). All p values were 2-sided, and a p value of <0.05 was considered statistically significant.
Results
Enrollment of patients was initiated in March, 2011 and continued until December, 2011 with starting time varying between centers. Each center collected patients during 2–6 weeks. A total of 12,040 eligible patients with dyslipidemia were enrolled and 1082 subjects were excluded due to protocol violations or missing data. The geographical distribution of participants was relatively well balanced between the north (29%), east (33%), south central (19%), northwest (10%), and southwest (10%) regions of China. Sixty-nine percent of the centers were Tertiary University hospitals.
Risk characteristics of the cohort
The baseline characteristics demonstrated a high risk cohort, with over 50% of patients had concomitant hypertension, 37.5% had coronary artery disease, 17.5% had diabetes and more than 30% had peripheral artery disease (Table 1). In the overall cohort, there were 28.1%, 23.8%, 25.0% and 23.1% of patients had optimal (LDL-C<100 mg/dl), above optimal (130 mg/dl >LDL-C≥100 mg/dl), borderline high (160 mg/dl >LDL-C≥130 mg/dl) and high LDL-C levels (LDL-C≥160 mg/dl) based on the ATP III guidelines. Patients were further divided into different risk categories according to their individual risk factors: 1926 patients (16%) in very high risk category, 5177 patients (43%) in high risk category, 2528 patients (21%) in moderate risk category, and 2408 patients (20%) in low risk category.
Table 1. Characteristics.
| Characteristics | Total (N = 12040) | Male (N = 6860) | Female (N = 5180) |
| Age (years) | 61.7±12.5 | 60.9±13.0 | 62.8±11.9* |
| BMI (kg/m2) | 24.3±3.5 | 24.4±3.4 | 24.1±3.7* |
| Diabetes (%) | 17.5 | 17.4 | 17.6 |
| Hypertension (%) | 51.9 | 52.1 | 51.6 |
| Smoking (%) Never/former/current | 67.9/9.9/22.2 | 46.8/16.5/36.6 | 95.8/1.1/3.1* |
| CAD (%) | 37.5 | 41.0 | 32.9* |
| Stroke/TIA (%) | 12.3 | 12.6 | 12.0 |
| Peripheral artery disease (%) | 31.2 | 30.9 | 31.7 |
| Chronic kidney disease (%) | 3.3 | 3.4 | 3.3 |
| Aortic abdominal aneurysms (%) | 2.3 | 2.9 | 1.6 |
| Family history of premature CAD (%) | 5.7 | 5.7 | 5.6 |
| PCI | 22.3 | 25.3 | 18.3* |
| CABG | 2.1 | 2.4 | 1.7 |
| SBP (mmHg) | 135.1±18.2 | 134.9±18.0 | 135.3±18.4 |
| DBP (mmHg) | 82.7±12.4 | 83.0±12.3 | 82.1±12.4* |
| Total cholesterol (mg/dl) | 199.9±58.7 | 194.7±59.0 | 206.9±57.5* |
| LDL- C (mg/dl) | 128.3±46.3 | 124.7±44.9 | 133.2±47.7* |
| HDL- C (mg/dl) | 49.5±26.9 | 47.7±27.5 | 51.8±25.9* |
| Triglyceride (mg/dl) | 194.6±133.5 | 196.2±140.7 | 192.5±123.2 |
P<0.0001 for comparison between female and male.
BMI: body mass index; TIA: transient ischemic attack; CAD: coronary artery disease; PCI: percutaneous coronary intervention; CABG: coronary artery bypass graft; SBP: systolic blood pressure; DBP: diastolic blood pressure; LDL-C: low-density lipoprotein cholesterol; HDL-C: high-density lipoprotein cholesterol.
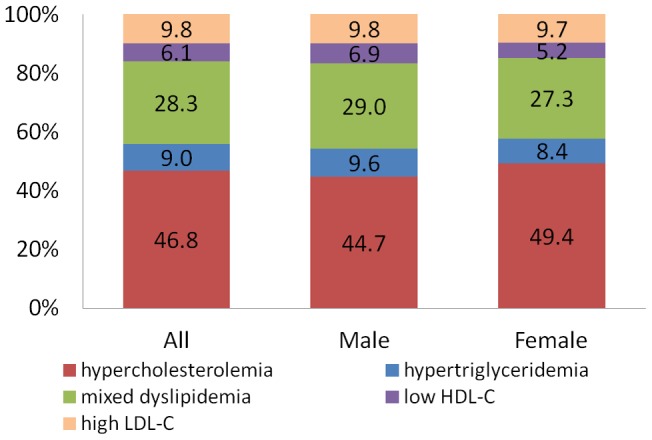
Notably, there were statistically significant differences between men and women in age, body mass index (BMI), smoking status, coronary artery disease and percutaneous coronary intervention proportions. Furthermore, the mean levels of total cholesterol, LDL- C and HDL- C were also significantly higher in female, whereas the diastolic blood pressure was lower in comparison with male (Table 1). The proportion of patients with individual or mixed lipid abnormalities was shown in Figure 1. Female had a higher prevalence of hypercholesterolemia. Conversely, a higher proportion of hypertriglyceridemia, low HDL-cholesterol and mixed lipid disorders were observed in male than in female (Figure 1).
Figure 1. The proportion of patients with individual or mixed lipid disorders.
Lipid modification therapy
In this cohort, 39.3% of all participants received lipid lowering medications before study enrollment. In addition, even for patients in high or very high risk group, the prescription rate was only 42.1% and 46.5%, respectively. And the prescription of lipid lowering medications was strikingly low among patients enrolled from non-tertiary hospitals (31.1%). In patients with lipid lowering medications, the majority of them (94.5%) had statins (42.5% with atorvastatin, 29.0% with simvastatin, and 15.2% with rosuvastatin). The adverse reaction events were rare and did not differ from man and women (Table 2). And there were 41.3% of patients in the overall cohort had received blood lipid tests, and 30.8% of patients had creatine kinase and liver enzyme monitoring within three months before enrollment (Table 2).
Table 2. Lipid lowering therapy.
| Total (N = 12040) | Male (N = 6860) | Female (N = 5180) | |
| Prior lipid lowering therapy (%) | 39.3 | 39.5 | 39.0 |
| Statins (%) | 37.1 | 37.5 | 36.5 |
| Niacin (%) | 1.5 | 1.4 | 1.7 |
| Fibrates (%) | 6.0 | 6.2 | 5.8 |
| Monitoring of blood lipid 3 months prior to enrollment (%) | 41.3 | 40.7 | 42.2 |
| Monitoring of creatine kinase and Liver enzyme 3 months prior to enrollment (%) | 30.8 | 30.9 | 30.6 |
| Adverse effect (%) | 1.5 | 1.5 | 1.5 |
| Myalgia (%) | 0.3 | 0.3 | 0.3 |
| Elevation of Liver enzyme (%) | 0.4 | 0.4 | 0.4 |
| Elevation of creatine kinase (%) | 0.04 | 0.06 | 0.02 |
Attainment of recommended cholesterol targets
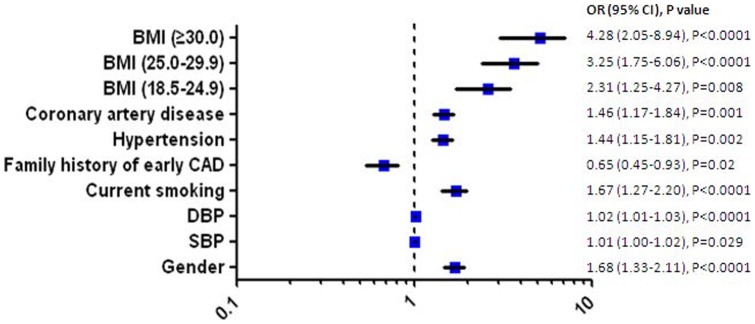
After establishing individualized LDL-C target, the overall attainment for LDL-C target was low in this survey (25.8%), especially, in female, and in patients with increased BMI as well. The attainment was significantly lower for patients in high (19.9%) and very high (21.1%) risk category (Table 3). And among patients with lipid lowering therapy, a significantly increased LDL-C attainment rate was observed in patients taking rosuvastatin (Table 3). In multivariate logistic regression analysis, eight factors (BMI, gender, coronary artery disease, systolic and diastolic blood pressure, hypertension, family history of premature CAD and current smoking) were identified as independent predictors for failure to reach recommended LDL-Cholesterol targets (Figure 2).
Table 3. Attainment of recommended cholesterol targets in each subgroup.
| Number of patients in each subgroup | LDL-C attainment rate (%) | P value for difference among subgroup | |
| Gender | P<0.0001 | ||
| Male | 6860 | 28.5 | |
| Female | 5180 | 22.2 | |
| BMI (Kg/m2) | P<0.0001 | ||
| <18.5 | 300 | 38.3 | |
| 18.5–24.9 | 6252 | 28.1 | |
| 25.0–29.9 | 3676 | 26.0 | |
| ≥30.0 | 533 | 17.4 | |
| Age group (years) | P<0.0001 | ||
| 20–29 | 69 | 30.4 | |
| 30–39 | 431 | 24.6 | |
| 40–49 | 1505 | 23.8 | |
| 50–59 | 3176 | 23.3 | |
| 60–69 | 3386 | 24.3 | |
| 70–79 | 2518 | 29.7 | |
| ≥80 | 955 | 32.5 | |
| Risk stratification | P<0.0001 | ||
| Low | 2408 | 38.1 | |
| Moderate | 2528 | 29.7 | |
| High | 5177 | 19.9 | |
| Very high | 1926 | 21.1 | |
| Centers | P<0.0001 | ||
| Tertiary | 8668 | 28.0 | |
| Non-tertiary | 3372 | 20.1 | |
| Statin treatment group | P<0.0001 | ||
| Simvastatin | 1376 | 36.2 | |
| Atorvastatin | 2011 | 34.9 | |
| Rosuvastatin | 717 | 51.1 | |
| Others | 628 | 40.0 |
BMI: body mass index.
Figure 2. Independent predictors of failure to reach recommended LDL-Cholesterol targets.
Discussion
In this large, multi-centre, cross-sectional cohort study of 12040 high-risk ambulatory patients with lipid disorders, we demonstrated that less than 40% of patients received lipid lowering medications and only about a quarter achieved the target LDL-C levels. In particular, patients in high risk category, with increased BMI and female were less likely to meet the recommended LDL-C targets.
Although sufficient clinical studies have shown the definitive benefits of lipid-lowering therapy and LDL-C attainment in prevention of cardiovascular disease, [8]–[12] there is limited data on the contemporary treatment and LDL-C attainment in patients with dyslipidemia in China. Our study provides new information regarding the “real world” management in these high-risk patients across China. The finding that only about a quarter of the patients in our study attained the recommended lipid targets is significant and emphasizes important treatment gaps in China. Especially, nearly 60% of patients in this cohort were identified as high or very high risk category, which need stringent control on serum cholesterol. Early studies have indicated the LDL-C goal attainment was 38% among 4888 outpatients enrolled in the Lipid Treatment Assessment Project in the United States [17]. And more recently, Vascular Protection (VP) and Guidelines Oriented Approach to Lipid Lowering (GOALL) Registries showed their LDL attainment rate reached to 51% among 8056 outpatients with diabetes or established cardiovascular disease in Canada. [18] To our knowledge, the only existing data focused on Chinese population is REALITY-Asia study, [19] which was conducted in China, Korea, Malaysia, Singapore, Taiwan, and Thailand, retrospectively recruited 2622 patients with hypercholesterolemia newly initiated on statin monotherapy. This study documented that 48% of patients attained LDL-C targets, and the attainment rate was also significantly lower as the risk-category escalated, including 38% of those in high risk group, 62% of those in moderate risk group, and 81% of those in low risk group. Our study was conducted in a large Chinese population and we also observed the same trend. However, in our study the overall attainment was surprisingly low, only 25%, this phenomenon might be mainly explained by the low proportion of lipid lowering therapy (less than 40%) in our population. Besides, nearly 30% of participants were enrolled from community hospitals and they had even lower proportion of lipid lowering therapy (31.1%). It also contributes to the low attainment rate. And yet, we believe this result did reflect the “real world” practice and the huge gap between guidelines and daily clinical practice in China.
Another important finding of our study is that we identified several factors which would strongly affect the LDL-C attainment. First and foremost, gender is a strong predictor for attainment failure, with 22% attainment in female. This finding was consistent to VP and GOALL registry. [18], [20] In addition, our study indicated the different pattern of lipid disorder between man and woman. Specifically, female had a higher prevalence of hypercholesterolemia and a lower proportion of hypertriglyceridemia, which is similar to the study conducted by M. Pirro, et al. [21] Second important predictor for attainment failure is obesity. Patients with increased BMI had significantly lower attainment, this result concurs with V. Bhan, et al. (pos-hoc analysis of the VP and GOALL registry). [20] It reflects the difficulty in managing obese patients, who are often resistant to therapy and might require combined drug therapy, as well as lifestyle interventions. And previous observational studies also suggest patients with increased BMI had higher incidence of adverse cardiac events after percutaneous coronary intervention [22]–[24], the disparity of LDL-C attainment may be one of the reasons contributing to the worse outcome in patients with obesity. In addition, the mean BMI was lower in the China REALITY Survey population (24.3 kg/m2) than the VP and GOALL registry (29.3 kg/m2). [18] And there is growing evidence that metabolic and cardiovascular risk profiles are different in Asian and Caucasian individuals and the thresholds for diagnosing obesity are lower in Asian individuals. [25], [26] Therefore, we believe the result from our study would be more persuasive for Chinese population.
Finally, recent studies also suggest that statin could provide cardiovascular benefits beyond LDL-cholesterol lowering effect. [27] Therefore risk reduction could be achieved by statin treatment without achieving the targets due to pleiotropic effects. However, our survey also indicated that statin was only prescribed to less than 40% of overall participants. Even for high or very high risk category, the prescription rate was merely 42.1% and 46.5%, respectively. And it poses imperative demands for developing national program to raise public awareness.
Limitations
The present study had several limitations. First, lipid measurements were not performed in a central core laboratory. However, this also reflects “real world” practice where physicians initiate or titrate therapy based on available test results. Second, we did not collect data on the duration of lipid lowering therapy or adherence to medications. Third, life-style modifications or non-pharmacological therapies were not assessed in our study. Finally, this survey is a cross-sectional study. A prospective follow-up study is required to assess the medical treatment, attainment in relation to mortality in patients with dyslipidemia.
In conclusion, despite the proven benefits of lipid-lowering therapies, current management of dyslipidemia is still suboptimal in China. A considerable proportion of patients failed to achieve guideline-recommended targets, and the treatment gap was more pronounced among patients with increased BMI, higher risk stratification and women. Our study also suggests more aggressive treatment strategies and national improvement projects should be implemented to narrow the existing gap.
Disclosures
This study was supported by the Chinese Society of Cardiology (a federally incorporated none-profit academic research organization) and AstraZeneca. The industry sponsors had no involvement in the study conception or design; collection, analysis, and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication. The authors had full access to the data and take full responsibility for its integrity. All the authors have read and agreed to the article as written.
Supporting Information
(PPT)
Acknowledgments
The involvement of the REALITY-CHINA Study Investigators and their hospitals is acknowledged as follows: An Zhen Hospital, Capital Medical University; The People's Hospital of Beijing University; Beijing Hospital; Peking Union Medical College Hospital; Xuan Wu Hospital, Capital Medical University; China–Japan Friendship Hospital; Shanghai First People's Hospital; Xinhua Hospital of Shanghai Second Medical University; Renji Hospital of Shanghai Second Medical University; Shanghai Jiaotong University Affiliated Sixth People's Hospital; Shanghai Tenth People's Hospital.
Funding Statement
This study was supported by the Chinese Society of Cardiology (a federally incorporated none-profit academic research organization) and AstraZeneca. The industry sponsors had no involvement in the study conception or design; collection, analysis, and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication. The authors had full access to the data and take full responsibility for its integrity. All the authors have read and agreed to the article as written.
References
- 1. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Final report. Circulation 106: 3143–3421. [PubMed] [Google Scholar]
- 2. Grundy SM, Cleeman JI, Merz CN, Brewer HB, Clark LT, et al. (2004) Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. J Am Coll Cardiol 44: 720–32. [DOI] [PubMed] [Google Scholar]
- 3. Fodor JG, Frohlich JJ, Genest JJ, McPherson PR (2000) Recommendations for the management and treatment of dyslipidemia: Report of the Working Group on Hypercholesterolemia and Other Dyslipidemias. Can Med Assoc J 162: 1441–1447. [PMC free article] [PubMed] [Google Scholar]
- 4. De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, et al. (2003) European guidelines on cardiovascular disease prevention in clinical practice: third joint task force of European and other societies on cardiovascular disease prevention in clinical practice. Eur Heart J 24: 1601–1610. [DOI] [PubMed] [Google Scholar]
- 5. Stamler J, Wentworth D, Neaton JD (1986) Prevalence and prognostic significance of hypercholesterolemia in men with hypertension. Prospective data on the primary screenees of the Multiple Risk Factor Intervention Trial. Am J Med 80: 33–9. [DOI] [PubMed] [Google Scholar]
- 6. Assmann G, Schulte H (1988) The Prospective Cardiovascular Münster (PROCAM) study: prevalence of hyperlipidemia in persons with hypertension and/or diabetes mellitus and the relationship to coronary heart disease. Am Heart J 116: 1713–24. [DOI] [PubMed] [Google Scholar]
- 7. Wilson PWF, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB (1998) Prediction of coronary heart disease using risk factor categories. Circulation 97: 1837–47. [DOI] [PubMed] [Google Scholar]
- 8. Murphy SA, Cannon CP, Wiviott SD, de Lemos JA, Blazing MA, et al. (2007) Effect of intensive lipid-lowering therapy on mortality after acute coronary syndrome (a patient-level analysis of the Aggrastat to Zocor and Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis in Myocardial Infarction 22 trials). Am J Cardiol 100: 1047–1051. [DOI] [PubMed] [Google Scholar]
- 9. Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, et al. (2004) Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med 350: 1495–1504. [DOI] [PubMed] [Google Scholar]
- 10. de Lemos JA, Blazing MA, Wiviott SD, Lewis EF, Fox KA, et al. (2004) Early intensive vs a delayed conservative simvastatin strategy in patients with acute coronary syndromes: phase Z of the A to Z trial. JAMA 292: 1307–1316. [DOI] [PubMed] [Google Scholar]
- 11. LaRosa JC, Grundy SM, Waters DD, Shear C, Barter P, et al. (2005) Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med 352: 1425–1435. [DOI] [PubMed] [Google Scholar]
- 12. Pedersen TR, Faergeman O, Kastelein JJ, Olsson AG, Tikkanen MJ, et al. (2005) High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA 294: 2437–2445. [DOI] [PubMed] [Google Scholar]
- 13. Baessler A, Fischer M, Huf V, Mell S, Hengstenberg C, et al. (2005) Failure to achieve recommended LDL cholesterol levels by suboptimal statin therapy relates to elevated cardiac event rates. Int J Cardiol 101: 293–8. [DOI] [PubMed] [Google Scholar]
- 14. Miller M, Cannon CP, Murphy SA, Qin J, Ray KK PROVE IT-TIMI 22 investigators (2008) Impact of triglyceride levels beyond low-density lipoprotein cholesterol after acute coronary syndrome in the PROVE IT-TIMI 22 trial. J AmColl Cardiol 51: 724–30. [DOI] [PubMed] [Google Scholar]
- 15. Kastelein JJ, van der Steeg WA, Holme I, Gaffney M, Cater NB, et al. (2008) Lipids, apolipoproteins, and their ratios in relation to cardiovascular events with statin treatment. Circulation 117: 3002–9. [DOI] [PubMed] [Google Scholar]
- 16. Ma YC, Zuo L, Chen JH, Luo Q, Yu XQ, et al. (2006) Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol 17: 2937–2944. [DOI] [PubMed] [Google Scholar]
- 17. Pearson TA, Laurora I, Chu H, Kafonek S (2000) The lipid treatment assessment project (L-TAP): a multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med 160: 459–467. [DOI] [PubMed] [Google Scholar]
- 18. Yan AT, Yan RT, Tan M, Hackam DG, Leblanc KL, et al. (2006) Contemporary management of dyslipidemia in high-risk patients: targets still not met. Am J Med 119: 676–683. [DOI] [PubMed] [Google Scholar]
- 19. Kim HS, Wu Y, Lin SJ, Deerochanawong C, Zambahari R, et al. (2008) Current status of cholesterol goal attainment after statin therapy among patients with hypercholesterolemia in Asian countries and region: the Return on Expenditure Achieved for Lipid Therapy in Asia (REALITY-Asia) study. Curr Med Res Opin 24(7): 1951–63. [DOI] [PubMed] [Google Scholar]
- 20. Bhan V, Yan RT, Leiter LA, Fitchett DH, Langer A, et al. (2010) Guidelines Oriented Approach in Lipid Lowering (GOALL) Registry and Vascular Protection (VP) Registry Investigators. Relation Between Obesity and the Attainment of Optimal Blood Pressure and Lipid Targets in High Vascular Risk Outpatients. Am J Cardiol 106(9): 1270–6. [DOI] [PubMed] [Google Scholar]
- 21. Pirro M, Del Giorno R, Lupattelli G, Mannarino MR, Roscini AR, et al. (2010) Cardiovascular risk factors and recommended lipid goals attainment among patients referred in a tertiary care lipid clinic. Eur J Intern Med 22(4): 412–7. [DOI] [PubMed] [Google Scholar]
- 22. Wang ZJ, Zhou YJ, Liu YY, Yu M, Shi DM, et al. (2009) Obesity and cardiovascular thrombotic events in patients undergoing percutaneous coronary intervention with drug-eluting stents. Heart 95(19): 1587–92. [DOI] [PubMed] [Google Scholar]
- 23. Wang ZJ, Zhou YJ, Zhao YX, Liu YY, Shi DM, et al. (2012) Effect of obesity on repeat revascularization in patients undergoing percutaneous coronary intervention with drug-eluting stents. Obesity 20(1): 141–6. [DOI] [PubMed] [Google Scholar]
- 24. Sarno G, Räber L, Onuma Y, Garg S, Brugaletta S, et al. (2011) Impact of body mass index on the five-year outcome of patients having percutaneous coronary interventions with drug-eluting stents. Am J Cardiol 108(2): 195–201. [DOI] [PubMed] [Google Scholar]
- 25.International Diabetes Federation. The IDF consensus worldwide definition of the metabolic syndrome. Available: http://www.idf.org/webdata/docs/IDF_Metasyndrome_definition.pdf.
- 26. Hu DY, Pan CY (2006) Yu JM; China Heart Survey Group (2006) The relationship between coronary artery disease and abnormal glucose regulation in China: the China Heart Survey. Eur Heart J 27(21): 2573–9. [DOI] [PubMed] [Google Scholar]
- 27. Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM, et al. (2008) JUPITER Study Group. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 359: 2195–207. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PPT)


