Abstract
Although the prevalence of smoking has declined among U.S. adults, an estimated 22.5 percent of the adult population (45.8 million adults) regularly smoked in 2002. Starting from this level, it will not be possible to achieve the Healthy People national health objectives of a reduction in the prevalence of smoking among adults to less than 12 percent by 2010 unless the rate of smoking cessation substantially rises from its current average of about 2.5 percent per year. To achieve that goal it is imperative that we better understand what factors are associated with successful quitting so that policies and resources can be better targeted. We describe the socioeconomic characteristics of smokers who attempt to and successfully quit and show how those characteristics differ across three methods smokers use in their cessation behavior; data are drawn from the 1995–1999 Simmons NAtional Consumer Surveys. These are ‘no-cost’ methods, the use of pharmaceutical products, and the use of conseling programs. The results highlight socioeconomic differences across the methods smoker use and provide evidence that can be used to better target smoking cessation information and resources to smokers most likely to use particular methods. Better targeting is likely to lead to more quitters. While it is unlikely that cessation rates can be raised by enough to achieve the reduction in national smoking prevalence that the Healthy People initiative has set, a better understanding of who chooses which method will move us closer to that goal.
Keywords: Smoking cessation, quit methods, pharmaceutical smoking cessation products, stop smoking programs, USA
Introduction
Cigarette smoking and the use of other forms of tobacco causes approximately 5 million deaths per year globally, making it one of the leading causes of death among adults in the world. According to the World Health Organization (1999, 2006), the current trends in smoking will lead to double the number of deaths (about 10 million) by 2020. Most of this increase stems from tobacco use in low income countries: Murray and Lopez (1996) predict tobacco-related deaths in low income countries will more than quadruple. But the large number of current smokers in the formerly socialist economies and the established market economies mean that tobacco control efforts in these countries remain critical for public health. The European Partnership to Reduce Tobacco Dependence (2001) observes, for example, that: “Unless more is done to help the 200 million European adult smokers stop, the result will be 2 million European deaths a year by 2040.” Recent research indicates that only a limited number of European countries strongly implement initiatives including high taxes on cigarettes, public place smoking bans and advertising bans, large health warning labels on tobacco products, and nationally funded treatments to help smokers stop smoking (Joossens and Raw, 2006). Although NRT products such as nicotine patches and nasal sprays are widely available in both Europe and the US, products approved for sale ‘over-the-counter’ in Europe are typically available only in pharmacies while in the US they are widely available in retail and grocery stores. While the tobacco control initiatives and new quitting technologies have likely contributed to the decline in the prevalence of smoking among U.S. adults, there were still an estimated 22.5 percent of the adult population (45.8 million adults) who regularly smoked in 2002 (CDC 2004).
For practical and policy reasons it is important to better understand characteristics of smokers who try to quit and who successfully quit. From a policy perspective, a better understanding will contribute towards meeting public health goals. For example, the US has set a national health objective (titled Healthy People) to reduce the prevalence of smoking among adults to less than 12 percent by 2010 (CDC 1993; USDHHS 2001). This objective cannot be attained unless the rate of long term smoking cessation substantially rises from its current average of about 2.5 percent per year.1 With a better understanding of the factors associated with successful quitting, policies and resources can be better targeted in the U.S. and other countries.
While a substantial body of research documents socio-economic differences between smokers and non-smokers - smokers are more likely to be poor, less well educated, white or African American, and male - this knowledge is not directly relevant to the goal of increasing the rate of smoking cessation (CDC, 2004; Escobedo & Peddicord, 1996, USDHHS, 1998, USDHHS, 2001). More pertinent are documented differences across socio-economic groups in the type of smokers who successfully quit each year. Although as many women as men attempt to quit smoking, they are less likely to succeed (CDC, 1986; Royce et al., 1997). In general younger smokers attempt to quit more than older smokers (Derby, Lasater and Vass, 1994; U.S. Department of Health and Human Services, 2001). In a time-series study of trends in quit behavior by age, Gilpin and Pierce (2002) show that although middle-aged smokers showed higher quit rates through the 1960s, the 1990 quit rates were higher for younger smokers. Differences in quit behavior by race are most pronounced between whites and African Americans, with whites more likely to quit smoking than African Americans (Gilpin and Pierce, 2002; Hahn et al., 1990; King et al., 2004). It is well established that more highly educated smokers are more likely to quit smoking (CDC, 2004, Gilpin and Pierce, 2002).
To supplement the above knowledge, policy analysts need to understand differences in the socioeconomic characteristics of smokers who use different methods to try to quit or who successfully quit. Such knowledge will aid in the targeting of resources to encourage smokers to quit.
A better understanding of who tries different cessation methods is especially important because new and effective methods have recently been developed. Until 1984, smokers who wanted to quit could choose from among a rather limited and ineffective set of methods to try to quit that included abstinence (cold turkey), hypnosis, psychological counseling, and non pharmaceutical smoking cessation products. Based on a meta-analysis of evidence from clinical trials, the current Public Health Service’s Clinical Practice Guidelines concludes that: “Numerous effective pharmacotherapies for smoking cessation now exist....that reliably increase long-term abstinence rates,’ and identifies buproprion, nicotine gum, nicotine inhaler, nicotine nasal spray, and the nicotine patch as first-line pharmacotherapies (USDHHS 2000). The results of the meta-analysis suggest that compared to the control groups (cold turkey quitting), product use approximately doubles the probability of successful smoking cessation. In 1984 the Federal Drug Administration approved the first clinically effective pharmaceutical smoking cessation product, Nicorette Gum™ for sale in the US. Since then, pharmaceutical firms have discovered and developed several additional pharmaceutical products to help smokers quit. Researchers have demonstrated in clinical trials that pharmaceutical smoking products are effective - smokers using them quit at approximately double the rate of smokers given a placebo (Hughes et al., 1999). Many of these products are available as over the counter medications, including nicotine gum and nicotine patches. Others are still available only by prescription.
While the effectiveness of these new pharmacotherapies has been clinically established, less is known about who is actually using them. Such knowledge is important because of the substantial public health interest in smoking behavior and the efforts being made to convince people to quit smoking. The limited research on this topic suggests that, in recent years, smokers increasingly seek some type of assistance to try to quit, such as counseling or nicotine replacement therapy (NRT) products, and that whites are more likely than African Americans to use pharmaceutical products (Zhu et al., 2000). In this study we will help fill this gap in our understanding by directly investigating the methods smokers choose when they attempt to quit. Our study will shed new light on socio-economic differences in smoking behavior.
This study uses data from two large micro-data sets: the 1995–1999 waves of the Simmons National Consumer Survey (NCS), and the 2000 U.S. National Health Interview Survey (NHIS), to describe and contrast the socio-economic characteristics of smokers who attempt to quit, who succeed in quitting, and who choose one of three methods to try to quit. To analyze the methods smokers choose, we explicitly account for how methods differ with respect to how much smokers have to pay to use them. We first categorize methods by an estimate of what each method will cost to use. We then analyze the probability that a smoker chooses a method in each category as a function of socio-economic characteristics.
Data
Survey design
Simmons National Consumer Survey
We use data from the 1995–1999 Simmons National Consumer Surveys (NCS). We combine data from seven waves of NCS surveys (Fall 1995, Spring 1996, Spring 1997, Fall 1997, Spring 1998, Fall 1998, and Fall 1999). Each NCS employs a multi-stage stratified probability sample. The final sample in each wave consists of a representative probability sample of all adults living in households in the U.S. (excluding Hawaii and Alaska) at the time of the survey. In order to minimize respondent fatigue Simmons collects data in several phases. During the Phase 1 face-to-face interviews, interviewers collect respondents’ demographic data, including whether or not respondents smoke and whether or not they have tried to quit smoking in the past year. During the second part of Phase 1 respondents report, by filling out a questionnaire, whether they purchase and use specific products, including smoking cessation products. Survey response rates are generally high (approximately 70 percent) and comparable to response rates on other nationally representative cross-sectional surveys.
2000 National Health Interview Survey
Our second dataset is drawn from the 2000 National Health Interview Survey (NHIS) of the U.S. Department of Health and Human Services. The NHIS uses a multi-stage sample designed to represent the civilian non-institutionalized U.S. population. The survey is administered using computer-assisted personal interviewing (CAPI), and contains socio-demographic information on all members of a surveyed family. Interviewers also collect detailed information on health status, health care services, and behavior on one randomly selected adult and one randomly selected child in each family. While NHIS always asks respondents about whether or not they smoke, the 2000 (Adult) questionnaire collects more detailed information on smoking behavior and the use of specific smoking cessation products.
Our NCS analysis sample includes 31,425 current or former smokers. Of these, 17,341 (55.2%) respondents currently smoke and did not attempt to quit in the past year. The other 14,084 (44.8%) respondents consist of current and former smokers who attempted to quit in the past year. Of those who attempted to quit, 2,999 (9.0%) succeeded and 11,085 (35.3%) failed.
Our smaller NHIS analysis sample includes 8,291 current or former smokers. Of these, 4,203 (50.7%) respondents currently smoke and did not attempt to quit in the past year. All of the remaining 4,088 (49.3%) respondents either attempted to quit or successfully quit in the previous year. Of those who attempted to quit, 870 (10.5%) succeeded and 3,218 (38.8%) failed.
These short-term quit rates are surprisingly consistent with other independently drawn data. Although the rates in these samples are roughly four times higher than the “permanent cessation” rate of 2.5 percent reported by the CDC (1993), they correspond closely with the self-reported one year quit rate of 8.6 percent reported by Liu (2006) who uses data on over 895,000 smokers from pooled Tobacco Use Supplements of the Current Population Surveys. Because smokers quit multiple times before permanent cessation, the short term rate should exceed long term cessation rates by some factor that is not well established in the literature (Prochaska and DiClemente 1983, DiClemente et al., 1991).
Although one might be concerned that smokers are giving socially expected responses to questions about whether they attempt to quit, evidence suggests that smokers fairly accurately report whether they smoke. In a meta-analysis of studies that compared contemporaneous self-reported smoking with biochemical markers of smoking, Patrick et al., (1994) find that smoking status indicators based on self-reported information had an average sensitivity of 87.5 percent and an average specificity of 89.2 percent. Sensitivity and specificity measure respectively the proportion of smokers and nonsmokers correctly assigned their respective labels.
Even though the sample of current and former smokers in the NHIS is much smaller than the NCS, we analyze NHIS data not only to provide an independent check of the patterns we observe in the NCS but also to validate the NCS data. The NHIS is a major ongoing data collection effort of the US National Center for Health Statistics. As a result, many researchers are more familiar with those surveys than they are the NCS data.
Dependent Variables
We investigate three outcomes: whether a smoker attempted to quit in the past year; whether he succeeded or failed; and the method smokers used to successfully quit.
The first two dependent variables are binary response variables. The first dependent variable equals zero for all current smokers who did not try to quit in the past year and equals one for all current and former smokers who tried to quit in the past year. The second dependent variable equals zero for all current smokers who tried but were unable to quit (unsuccessful quitters) and equals one for all former smokers who successfully quit in the past twelve months (successful quitters).
The third dependent variable measures what type of method successful quitters used. We construct this variable using data collected from smokers who attempted to quit in the past year. Both NCS and NHIS interviewers showed a list of commonly used methods to respondents who tried to quit smoking in the past year. Respondents identified all methods on the list that they used in their most recent quit attempt.
Table 1 shows what methods NCS and NHIS smokers used when they tried to quit. The column labeled “Raw” lists the fraction of quit attempters who said they used a particular method, regardless of whether they reported having used more than one method.2 In the second column for each data set, we report the fraction of smokers who tried to quit using a method in one of three mutually exclusive categories (we describe next). In the third column for each data set, we report the fraction of smokers who succeeded in quitting given that they used one of the mutually exclusive methods we describe above.
Table 1.
Methods smokers used to try to quit
| NCS | NHIS | |||||
|---|---|---|---|---|---|---|
| Method | Raw1 | # used # attempt | # success # used method | Raw1 | # used # attempt | # success # used method |
| “Quit smoking programs” | 7.3% | 18.7% | 1.3% | 14.5% | ||
| Stop-smoking program or clinic | 3.8% | 0.7% | ||||
| One-on-one counseling | --- | 0.3% | ||||
| Acupunture | 0.8% | --- | ||||
| Hypnosis | 2.6% | --- | ||||
| “Pharmaceutical cessation aids” | 25.5% | 19.6% | 20.1% | 17.9% | ||
| Nicorette gum | 6.8% | 3.9% | ||||
| Nicotine patch | 21.1% | 12.8% | ||||
| Nicotine nasal spray | --- | 0.1% | ||||
| Nicotine inhaler | --- | 0.6% | ||||
| Zyban/Buproprion/Wellbutrin | --- | 6.5% | ||||
| “No cost” methods | 67.3% | 22.2% | 78.6% | 22.9% | ||
| “Cold turkey” (stopped all at once) | 52.8% | 72.4% | ||||
| Gradually reduction | 16.8% | 9.7% | ||||
| Switch to lower tar/nicotine cigarette | --- | 48.7% | ||||
| Switch to chewing tobacco/snuff | --- | 0.6% | ||||
| Instructions in a pamphlet or book | --- | 0.3% | ||||
| Any other method | 17.8% | 3.0% | ||||
Raw percentages sum to more than 100 percent because respondents can mark more than one category.
In order to analyze the method smokers use to quit, we combine responses across multiple quit methods to form three mutually exclusive categories. The categories are generally defined by the out-of-pocket cost of using each method. In the first category we include methods that smokers can try without having to spend any money.3 We label this category as “No-cost.” In the second category we include methods that involve the purchase of a pharmaceutical smoking cessation product. A smoker who used both a “no cost” method and a pharmaceutical product is coded in this category. We label this category as “Product.” In the third category, which we label “Program,” we include hypnosis, acupuncture, or a “quit-smoking” program under the assumption that a smoker who tries to quit using them must spend extra time to attend sessions and possibly pay money out-of-pocket. We assign a smoker to the “Program” category even if he also indicated he used one or both of the other two methods.
Focusing on the three mutually exclusive method categories, Table 1 shows that, when smokers attempt to quit, a large majority of them try to do so using “no-cost” methods. Of smokers that attempted to quit in the past year, more than 67 percent of NCS respondents and more than 78 percent of NHIS respondents tried to quit using methods that involved no direct outlay of cash. A substantial fraction of quit attempters chose methods that involved the outlay of cash, time or both. Table 1 shows that about 25 percent of NCS and about 20 percent of NHIS smokers tried to quit using pharmaceutical smoking cessation products. The fraction who tried to quit using quit smoking programs differed substantially across the NCS (7.3 percent) and NHIS (1.3 percent) surveys.
The NCS data are probably more reliable than the NHIS data because the NCS survey data are widely sold to marketers. Consequently, Simmons Media Markets – the firm that conducts the NCS - invests significant resources to elicit full responses about purchases and participation in quit smoking programs. For example, NCS interviewers meet with survey respondents in face-to-face interviewers to review and individually check responses on self-administered survey booklets that ask questions about product use and consumption behavior (including smoking). Simmons also devotes considerable resources to elicit responses from demographic groups that typically have low response rates. For example, Simmons will assign interviewers with proven success rates in eliciting responses to re-contact people in these groups - often by flying the interviewers to areas with low response rates (Simmons, 1994). Consequently, the NCS survey data are likely to be more representative of consumption patterns.
In the third column of Table 1 we report the rate of success associated with each type of quit method. Among smokers who try “no-cost” methods, about 22 percent of smokers successfully quit. Success rates are only slightly lower (17.5 to 19.6 percent) when smokers attempt to quit with pharmaceutical smoking cessation products. The data suggest that when smokers try “quit smoking programs,” between 14.5 and 18.7 percent succeed.
Although these results seem at odds with the results from clinical trials that show that the rate of smoking abstinence is more than double when smokers use pharmaceutical smoking cessation products than when they use a placebo, they are consistent with the fact that, in these data, we observe smokers who chose to use each method rather than a set of smokers who were randomly assigned to use a particular method. We discuss this point in our conclusion below.
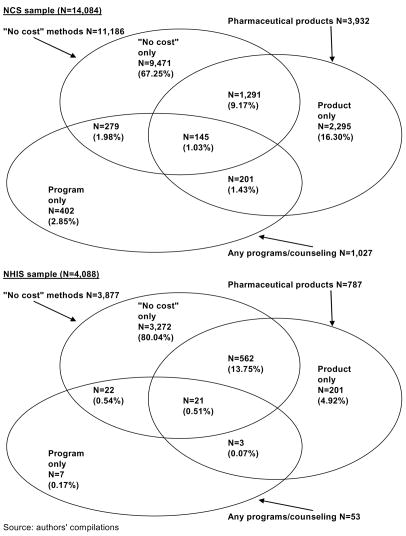
To the extent that our data permit, we adopt a second categorization of quitters that differentiates between smokers who use a single method to quit and smokers who use a combination of two or more methods. Figure 1 shows the number of smokers who tried to quit with each possible combination of available methods. As Figure 1 shows, most smokers use only one method in their quit attempt. For example, of the 14,084 NCS smokers who tried to quit, 86.3 percent used a single method. However, 13.6 percent or 1,916 NCS smokers tried to quit with a combination of products, programs, and no cost methods. Figure 1 shows that far fewer NHIS quit attempters claimed to use programs or any combination of programs with other methods. The small sample size in the NHIS means that we cannot use it to analyze characteristics of smokers across the more detailed quit method categories. However, we can and do use the NCS sample.
Figure 1.
Methods used in most recent attempt to quit smoking
Independent Variables
Both the NCS and NHIS data include information on a wide range of socio-demographic characteristics. Table 2 reports summary statistics for the variables we include in our analysis. We include standard demographic measures -- age and its square, sex, employment status, family income and its square, family size, whether children are present in the household, education, race/ethnicity, and marital status indicators. Family size is slightly higher in the NCS because the variable counts all people living in a household while in the NHIS family size counts only people related by blood or marriage. We also include indicators for whether a smoker is covered by some combination of insurance types. In the NCS the multiple insurance category identifies only those people covered by a combination of Medicare and Medigap supplemental insurance but not private insurance. In the NHIS the variable indicates both people covered by Medicare plus Medigap and people covered by both private insurance and some other type of insurance. Because the NCS sample is pooled from cross-sectional surveys conducted over several years, we also included binary variables to flag the season (Spring vs. Fall) and year (1995, 1996, 1997, or 1998, vs. 1999) the survey was conducted. The descriptive statistics shown in Table 2 establish that samples from each source are quite similar.
Table 2.
Summary Statistics
| Variable | NCS | NHIS |
|---|---|---|
| Former smoker | 9.0% | 10.8% |
| Age of respondent | 40.9 (15.3) | 41.0 (14.7) |
| Female respondent | 51.5% | 47.3% |
| Ethnicity | ||
| Black | 11.9% | 10.9% |
| Hispanic | 8.9% | 8.4% |
| White | 76.2% | 76.5% |
| Other | 2.9% | 4.2% |
| Children present in household | 44.1% | 41.3% |
| Family sizea | 3.1 (1.6) | 2.8 (1.6) |
| Employed | 64.4% | 70.3% |
| Family income | 52,586 (43,694) | 39,571 (23,400) |
| Education | ||
| Less than high school | 23.1% | 22.5% |
| High school graduate | 36.7% | 37.4% |
| Some college | 28.4% | 28.0% |
| College graduate | 11.7% | 12.1% |
| Medical insurance | ||
| Private insurance | 64.4% | 63.2% |
| Medicaid | 5.6% | 8.3% |
| Multiple insurance typesb | 1.5% | 5.7% |
| No insurance | 28.6% | 22.8% |
| Marital Status | ||
| Married | 60.6% | 59.5% |
| Divorced | 13.5% | 19.0% |
| Never married | 25.9% | 21.5% |
|
| ||
| N | ||
| Total sample size | 31,425 | 8,291 |
| Did not attempt to quit | 17,341 | 4,203 |
| Attempted to quit | 14,084 | 4,088 |
| Quit attempt succeeded | 2,999 | 870 |
Notes: Weights are used to compute descriptive statistics.
All people living in a household in the NCS. In the NHIS all people related by blood or marriage.
Measured as those covered by a combination of Medicare and Medigap supplemental insurance but not private insurance in the NCS and those by either Medicare plus Medigap or by both private insurance and some other type of insurance in the NHIS.
Methods
To explore differences in the socio-economic characteristics of smokers who attempted to quit and smokers who successfully quit we use logistic regression analysis. To analyze the methods quit attempters chose, we use multinomial logistic regression analysis. Thus, in the first regression, we model the probability of a quit attempt. In the second regression, we model the probability of a successful quit. In the multinomial logistic regressions, we first model the probability that a smoker attempted to quit using a quit smoking program or smoking cessation product versus a “no-cost” method. We then use the NCS data to run the analysis with more detailed categories of methods smokers used in their quit attempt. In all of our analyses we assume that the latent variable that underlies the probability of each choice is a quadratic function of age and family income.
Results
Probability of a quit attempt
Table 3 reports how socio-economic characteristics are correlated with the probability that a smoker recently attempted to quit. For each sample we report not only the logit coefficient estimates and standard errors but also the implied log odds ratio for a marginal change in the independent variable. The results in Table 3 support and extend the findings of the literature that documents demographic differences between quitters and non quitters. Smokers are less likely to try to quit if they are older, less educated, and unmarried (either divorced or never married). Holding other characteristics constant, women are more likely to try to quit than are men and non white smokers are more likely to try to quit than white smokers. The results in Table 3 also show that whether smokers try to quit is strongly associated with whether smokers have health insurance and the type of insurance they have.4 In the NCS sample, there is some evidence that smokers covered only by Medicaid are more likely to attempt to quit than uninsured smokers. In both samples smokers without any health insurance are less likely to try to quit by between 15 and 17 percent (odds ratio .83 to .85).
Table 3.
Quit attempts
| NCS | NHIS | |||||
|---|---|---|---|---|---|---|
| Independent Variable | Coefficient | Odds | Coefficient | Odds | ||
| Intercept | 0.767 (0.121) | *** | 1.683 (0.227) | *** | ||
| Age of respondent | −0.045 (0.005) | 0.96 | *** | −0.066 (0.009) | 0.94 | *** |
| Age squared | 0.446 (0.053) | 1.56 | *** | 0.531 (0.092) | 1.70 | *** |
| Female respondent | 0.069 (0.023) | 1.07 | *** | 0.101 (0.046) | 1.11 | ** |
| Employed | −0.103 (0.029) | 0.90 | *** | −0.060 (0.059) | 0.94 | |
| Family income*10−4 | 0.003 (0.007) | 1.00 | 0.020 (0.041) | 1.02 | ||
| Family income squared*10−9 | −0.002 (0.003) | 1.00 | −0.004 (0.045) | 1.00 | ||
| Family size | 0.006 (0.011) | 1.01 | −0.063 (0.025) | 0.94 | ** | |
| Presence of children in the household | 0.028 (0.034) | 1.03 | 0.113 (0.072) | 1.12 | ||
| Education (ref. high school graduate) | ||||||
| Less than high school | 0.044 (0.037) | 1.04 | 0.033 (0.063) | 1.03 | ||
| Some college | 0.215 (0.028) | 1.24 | *** | 0.285 (0.057) | 1.33 | *** |
| College graduate | 0.144 (0.034) | 1.16 | *** | 0.283 (0.077) | 1.33 | *** |
| Ethnicity (ref. White) | ||||||
| Black | 0.167 (0.044) | 1.18 | *** | 0.220 (0.066) | 1.25 | *** |
| Hispanic | 0.022 (0.052) | 1.02 | 0.067 (0.071) | 1.07 | ||
| Other | 0.221 (0.064) | 1.25 | *** | −0.045 (0.122) | 0.96 | |
| Marital Status (ref. married) | ||||||
| Divorced | −0.107 (0.033) | 0.90 | *** | −0.122 (0.058) | 0.89 | ** |
| Never married | −0.126 (0.034) | 0.88 | *** | −0.315 (0.072) | 0.73 | *** |
| Medical insurance (ref. private insurance) | ||||||
| Medicaid | 0.107 (0.062) | 1.11 | * | 0.095 (0.080) | 1.10 | |
| Multiple insurance typesa | −0.099 (0.096) | 0.91 | 0.176 (0.087) | 1.19 | ** | |
| No insurance | −0.189 (0.028) | 0.83 | *** | −0.165 (0.062) | 0.85 | *** |
|
| ||||||
| N | 31,425 | 8,291 | ||||
| Attempted to quit | 14,084 | 4,088 | ||||
| Sucessfully quit | 2,999 | 870 | ||||
| Failed to quit | 11,085 | 3,213 | ||||
| −2*Log-likelihood | −21469.7 | −5646.8 | ||||
Source: authors’ calculations from NCS and NHIS. ***, **, and * denote coefficients with p-values of <.01, .05, and .10 respectively.
See note in Table 2.
The results are broadly similar across the two samples. The two anomalies are family size and insurance coverage that is a combination of different types of insurance. The NHIS family size coefficient estimates sugggest that smoker who have bigger families are less likely to attempt to quit while the NCS coefficient estimate on household size suggests there is no association. The lack of an association in the NCS sample may arise because NCS “families” include unrelated persons living in the same household. The second difference in associations across the two samples is across quit attempts among people covered by multiple types of insurance. Again, the difference in the results across the two samples is likely due to differences in how the variable is defined in each sample. In the NCS, the multiple insurance category includes smokers covered by a combination of Medicare and Medigap supplemental insurance. The results suggest that their probability of attempting to quit doesn’t statistically differ from smokers who have private insurance. In the NHIS, the multiple insurance category includes those covered by a combination of Medicare and Medigap supplemental insurance plus those covered by both private insurance and some other type of insurance. The NHIS results in Table 3 suggest that the smokers covered by multiple types of insurance are more likely to attempt to quit than smokers with only private health insurance.
Probability of a successful quit
Table 4 reports differences between smokers who successfully quit in the past year and those who were unsuccessful in their quit attempt. Table 4 both confirms and adds to evidence reported in the literature. For example, similar to literature cited above, we find that women are less likely to successfully quit. We also find that, relative to smokers with twelve years of schooling, smokers with some college are 15 to 23 percent more likely to have succeeded in their quit attempt (odds ratio of 1.15 to 1.23) while smokers with 16 or more years of schooling are 34 to 67 percent more likely to have succeeded in their quit attempt (odds ratio 1.34 to 1.67). Single and divorced smokers are significantly less likely to have successfully quit.
Table 4.
Successful quits
| NCS | NHIS | |||||
|---|---|---|---|---|---|---|
| Independent Variable | Coefficient | Odds | Coefficient | Odds | ||
| Intercept | −0.251 (0215) | 0.790 (0.375) | ** | |||
| Age of respondent | −0.053 (0.009) | 0.95 | *** | −0.097 (0.014) | 0.91 | *** |
| Age squared | 0.718 (0.091) | 2.05 | *** | 1.064 (0.153) | 2.90 | *** |
| Female respondent | −0.400 (0.043) | 0.67 | *** | −0.018 (0.080) | 0.93 | |
| Employed | −0.001 (0.053) | 1.00 | −0.171 (0.103) | 0.84 | * | |
| Family income*10−4 | −0.001 (0.012) | 1.00 | 0.039 (0.072) | 1.04 | ||
| Family income squared*10−9 | 0.004 (0.005) | 1.00 | 0.011 (0.078) | 1.01 | ||
| Family size | −0.046 (0.020) | 0.96 | ** | −0.014 (0.047) | 0.99 | |
| Presence of children in the household | 0.113 (0.062) | 1.12 | * | −0.368 (0.129) | 0.69 | *** |
| Education (ref. high school graduate) | ||||||
| Less than high school | −0.117 (0.071) | 0.89 | 0.136 (0.116) | 1.15 | ||
| Some college | 0.136 (0.052) | 1.15 | *** | 0.203 (0.101) | 1.23 | ** |
| College graduate | 0.294 (0.061) | 1 34 | *** | 0.514 (0.127) | 1.67 | *** |
| Ethnicity (ref. White) | ||||||
| Black | −0.007 (0.081) | 0.99 | −0.102 (0.121) | 0.90 | ||
| Hispanic | 0.143 (0.093) | 1.16 | 0.228 (0.123) | 1.26 | * | |
| Other | 0.045 (0.112) | 1.05 | 0.037 (0.215) | 1.04 | ||
| Maritai Status (ref. married) | ||||||
| Divorced | −0.266 (0.066) | 0.77 | *** | −0.186 (0.104) | 0.83 | * |
| Never married | −0.112 (0.064) | 0.89 | * | −0.224 | 0.80 | * |
| Medical insurance (ref. private insurance) | ||||||
| Medicaid | −0.087 (0.113) | 0.92 | −0.334 (0.145) | 0.72 | ** | |
| Multiple insurance typesa | −0.255 (0.164) | 0.77 | −0.124 (0.146) | 0.88 | ||
| No insurance | −0.129 (0.055) | 0.88 | ** | −0.356 (0.115) | 0.70 | *** |
|
| ||||||
| Attempted to quit | 14084 | 4088 | ||||
| Sucessfully quit | 2,999 | 370 | ||||
| Failed to quit | 11,035 | 3218 | ||||
| −2*Log-likelihood | −7117.9 | −2044.9 | ||||
Source: authors’ calculations from NCS and NHIS. ***, **, and * denote coefficients with p-values of <01, .05, and .10 respectively.
See note in Table 2.
As with the quit attempts, the health insurance status of smokers is statistically correlated with whether or not they succeeded in their quit attempts. Smokers poor enough to qualify for Medicaid coverage are much less likely to successfully quit than smokers covered by private insurance (odds ratio of .72 to .92) - though this association is statistically significant only in the NHIS sample. Uninsured smokers are similarly less likely than privately insured smokers to have succeeded in their recent quit attempt (odds ratio of .70 to .88). Results from both samples suggest that smokers are less likely to sucessfully quit as they age up to a certain point. The quadratic term in the model is always signficant and implies that past age 37 (NCS sample) and 45 (NHIS sample) older smokers are increasingly more likely to successfully quit. The measured association between probability of a successful quit and family size also differs between the NCS and NHIS samples. In the NCS, smokers in larger households are marginally less likely to succeed in their quit attempt while the NHIS data suggest that family size is uncorrelated with the probability that a smoker successfully quit.
Methods used to quit – broad categories
Table 5 reports coefficient estimates and log-odds ratios from multinomial logistic regressions that model the method quit attempters chose. For each data set, the first set of results reports coefficient estimates, standard errors, and the log-odds ratio for the choice of a “Program” versus the choice of a “no cost” method. The second set of results reports the same statistics of the choice of a “Product” versus the choice of a “No cost” method.
Table 5.
Quit method used
| NCS | NHIS | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Program | Product | Program | Product | |||||||||
| Independent Variable | Estimate | Odds | Estimate | Odds | Estimate | Odds | Estimate | Odds | ||||
| Intercept | −4.182 (0.358) | *** | −4.509 (0.230) | *** | −8.250 (1.750) | *** | −5.025 (0.489) | *** | ||||
| Age of respondent | 0.040 (0.014) | 1.04 | *** | 0.134 (0.009) | 1.14 | *** | 0.216 (0.068) | 1.24 | *** | 0.180 (0.019) | 1.20 | *** |
| Age squared | −0.247 (0.148) | 0.78 | * | −1.307 (0.100) | 0.27 | *** | −2.210 (0.739) | 0.11 | *** | −1.893 (0.211) | 0.15 | *** |
| Female respondent | 0.201 (0.069) | 1.22 | *** | 0.114 (0.041) | 1.12 | *** | 0.250 (0.290) | 1.28 | 0.150 (0.087) | 1.16 | * | |
| Employed | −0.048 (0.082) | 0.95 | −0.006 (0.051) | 0.99 | −0.762 (0.338) | 0.47 | ** | −0.124 (0.112) | 0.88 | |||
| Family income*10−4 | 0.125 (0.020) | 1.13 | *** | 0.090 (0.012) | 1.09 | *** | 0.173 (0.259) | 1.19 | 0.150 (0.080) | 1.16 | * | |
| Family income squared*10−9 | −0.036 (0.008) | 0.96 | *** | −0.027 (0.005) | 0.97 | *** | −0.085 (0.277) | 0.92 | −0.059 (0.084) | 0.94 | ||
| Family size | 0.004 (0.031) | 1.00 | −0.024 (0.020) | 0.98 | −0.271 (0.194) | 0.76 | −0.183 (0.057) | 0.83 | *** | |||
| Presence of children in the household | 0.002 (0.098) | 1.00 | 0.077 (0.059) | 1.08 | 0.406 (0.461) | 1.50 | 0.143 (0.140) | 1.15 | ||||
| Education (ref. high school graduate) | ||||||||||||
| Less than high school | 0.179 (0.106) | 1.20 | * | 0.200 (0.067) | 1.22 | *** | −0.536 (0.439) | 0.58 | −0.225 (0.133) | 0.80 | * | |
| Some college | 0.011 (0.083) | 1.01 | 0.071 (0.050) | 1.07 | −0.154 (0.345) | 0.86 | 0.112 (0.103) | 1.12 | ||||
| College graduate | −0.038 (0.099) | 0.96 | 0.058 (0.059) | 1.06 | −0.097 (0.437) | 0.91 | −0.105 (0.137) | 0.90 | ||||
| Ethnicity (ref. White) | ||||||||||||
| Black | 0.029 (0.122) | 1.03 | −0.278 (0.079) | 0.76 | *** | 0.232 (0.363) | 1.26 | −0.791 (0.138) | 0.45 | *** | ||
| Hispanic | 0.131 (0.147) | 1.14 | −0.135 (0.097) | 0.87 | −1.115 (0.741) | 0.33 | −1.470 (0.208) | 0.23 | *** | |||
| Other | 0.091 (0.181) | 1.09 | 0.001 (0.109) | 1.00 | 0.784 (0.511) | 2.19 | 0.042 (0.256) | 1.04 | ||||
| Marital Status (ref. married) | ||||||||||||
| Divorced | 0.253 (0.093) | 1.29 | *** | 0.076 (0.058) | 1.08 | −0.563 (0.384) | 0.57 | −0.108 (0.111) | 0.90 | |||
| Never married | −0.019 (0.105) | 0.98 | −0.021 (0.063) | 0.98 | −0.223 (0.467) | 0.80 | −0.332 (0.150) | 0.72 | ** | |||
| Medical insurance (ref. private insurance) | ||||||||||||
| Medicaid | 0.190 (0.167) | 1.21 | −0.081 (0.112) | 0.92 | 0.002 (0.510) | 1.00 | 0.160 (0.156) | 1.17 | ||||
| Multiple insurance typesa | 0.105 (0.247) | 1.11 | 0.271 (0.163) | 1.31 | * | 0.448 (0.466) | 1.57 | 0.373 (0.147) | 1.45 | ** | ||
| No insurance | 0.007 (0.085) | 1.01 | −0.170 (0.053) | 0.84 | *** | 0.262 (0.401) | 1.30 | −0.217 (0.130) | 0.80 | * | ||
|
| ||||||||||||
| Total Sample Size | 14,084 | 4,088 | ||||||||||
| No cost methods | 9,471 | 3,272 | ||||||||||
| Products | 3,586 | 763 | ||||||||||
| Programs | 1,027 | 53 | ||||||||||
Source: authors’ calculations from NCS and NHIS. ***, **, and * denote coefficients with p-values of <.01, .05, and .10 respectively.
See note in Table 2.
Focusing on patterns that are similar across the two data sets, we find that smokers are more likely to use a costly method when they are female (odds ratios range from 1.12 to 1.22) and when their household income is higher. Even though the coefficient on the quadratic household income variable is statistically significant, the relationship does not turn negative until around 100,000 dollars of income – above the 80th percentile in the 2000 distribution of household income (US Census Bureau 2006). Over most of the income range observed in the data, income raises the probability that a smoker is observed to use a costly method to quit and that association grows weaker at higher income levels.
Interestingly, in the larger NCS sample, smokers with less than twelve years of schooling were more likely to use a program or pharmaceutical product to try to quit smoking (odds ratio 1.20 and 1.22 respectively). This association may capture effects of efforts by tobacco control groups to encourage low educated smokers to quit. Note also that there is weak evidence (p<.10) in the NHIS sample that smokers with less than twelve years of schooling were less likely to use a “product” (odds ratio .80). Given the small sample size available in the NHIS, this association needs to be confirmed in other data sources.
Although the coefficient estimates suggest that Blacks were more likely to use a stop smoking program (odds 1.03 to 1.26) than were whites, the association does not statistically differ from zero. In both the NCS and NHIS samples Blacks and Hispanics were less likely to use a pharmaceutical product to try to quit (odds .45 to .76) though the result for Hispanics is only statistically significant in the NHIS sample.
The method smokers chose is associated with whether they have insurance and the type of insurance they have. Smokers who lack health insurance were less like to choose a product to try to quit (odds ratios range from .80 to .84). In both samples smokers were more likely to use a product in their quit attempt if they had insurance from a combination of Medicare and Medigap (NCS) or a combination of private insurance and some other type of insurance (including a Medicare/Medigap combination) than were smokers with private insurance coverage from a single policy.
Methods used to quit – detailed categories
In Table 6 we report results from a multi-nomial logit model estimates with the more detailed quit methods categories shown in Figure 1. As noted before, for reasons of sample size we estimate the model only with NCS data. While the results from the finer categories are broadly similar to the results in Table 5, some interesting differences also emerge.
Table 6.
Detailed quit method used - NCS sample
| Program only | Product only | No cost+product | Product +program | No cost+program | All three methods | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Independent Variable | Estimate | Odds | Estimate | Odds | Estimate | Odds | Estimate | Odds | Estimate | Odds | Estimate | Odds | ||||||
| Intercept | −5.685 (0.563) | *** | −5.350 (0.285) | *** | −4. 943 (0.335) | *** | −6.376 (0.844) | *** | −4.323 (0.624) | *** | −6.745 (0.955) | *** | ||||||
| Age of respondent | 0.047 (0.022) | 1.049 | ** | 0.154 (0.012) | 1.166 | *** | 0.105 (0.014) | 1.110 | *** | 0.092 (0.033) | 1.096 | *** | 0.008 (0.025) | 1.008 | 0.036 (0.037) | 1.036 | ||
| Age squared | −0.268 (0.230) | 0.765 | −1.509 (0.124) | 0.221 | *** | −0.996 (0.146) | 0.369 | *** | −0.833 (0.341) | 0.435 | ** | −0.034 (0.271) | 0.966 | −0.036 (0.373) | 0.965 | |||
| Female respondent | 0.248 (0.107) | 1.28 | ** | 0.172 (0.049) | 1.19 | *** | 0.011 (0.062) | 1.01 | 0.244 (0.150) | 1.28 | 0.203 (0.127) | 1.22 | −0.001 (0.172) | 1.00 | ||||
| Employed | 0.096 (0.129) | 1.10 | 0.010 (0.061) | 1.01 | −0.032 (0.075) | 0.97 | −0.329 (0.173) | 0.72 | * | −0.288 (0.148) | 0.75 | * | 0.495 (0.225) | 1.64 | ** | |||
| Family income*10−4 | 0.128 (0.030) | 1.14 | *** | 0.102 (0.014) | 1.11 | *** | 0.069 (0.018) | 1.07 | *** | 0.104 (0.044) | 1.11 | ** | 0.114 (0.035) | 1.12 | *** | 0.167 (0.050) | 1.18 | *** |
| Family income squared*10−9 | −0.036 (0.012) | 0.96 | *** | −0.031 (0.006) | 0.97 | *** | −0.019 (0.007) | 0.98 | *** | −0.035 (0.018) | 0.97 | * | −0.031 (0.014) | 0.97 | ** | −0.049 (0.021) | 0.95 | ** |
| Family size | 0.074 (0.045) | 1.08 | * | −0.035 (0.024) | 0.97 | −0.008 (0.028) | 0.99 | −0.025 (0.074) | 0.97 | −0.036 (0.058) | 0.96 | −0.108 (0.088) | 0.90 | |||||
| Presence of children in the household | −0.107 (0.150) | 0.90 | 0.044 (0.071) | 1.04 | 0.139 (0.087) | 1.15 | −0.208 (0.223) | 0.81 | 0.236 (0.177) | 1.27 | 0.199 (0.255) | 1.22 | ||||||
| Education (ref. high school graduate) | ||||||||||||||||||
| Less than high school | 0.216 (0.161) | 1.24 | 0.167(0.080) | 1.18 | ** | 0.259 (0.099) | 1.30 | *** | −0.081 (0.251) | 0.92 | 0.063 (0.203) | 1.06 | 0.561 (0.248) | 1.75 | ** | |||
| Some college | 0.001 (0.126) | 1.00 | −0.041 (0.060) | 0.96 | 0.259 (0.074) | 1.30 | *** | 0.166 (0.176) | 1.18 | −0.057 (0.155) | 0.94 | −0.055 (0.216) | 0.95 | |||||
| College graduate | −0.235 (0.159) | 0.79 | 0.106 (0.068) | 1.11 | −0.044 (0.093) | 0.96 | 0.077 (0.213) | 1.08 | 0.207 (0.174) | 1.23 | −0.155 (0.256) | 0.86 | ||||||
| Ethnicity (ref. White) | ||||||||||||||||||
| Black | 0.358 (0.167) | 1.43 | ** | −0.455 (0.102) | 0.63 | *** | −0.031 (0.109) | 0.97 | −0.636 (0.348) | 0.53 | * | −0.383 (0.266) | 0.68 | 0.310 (0.283) | 1.36 | |||
| Hispanic | −0.128 (0.257) | 0.88 | −0.301 (0.125) | 0.74 | ** | 0.093 (0.132) | 1.10 | −0.013 (0.350) | 0.99 | 0.312 (0.237) | 1.37 | 0.453 (0.339) | 1.57 | |||||
| Other | 0.276 (0.265) | 1.32 | 0.012 (0.129) | 1.01 | −0.015 (0.165) | 0.99 | 0.319 (0.351) | 1.38 | −0.129 (0.347) | 0.88 | −0.717 (0.718) | 0.49 | ||||||
| Marital Status (ref. married) | ||||||||||||||||||
| Divorced | 0.227 (0.145) | 1.25 | −0.002 (0.069) | 1.00 | 0.211 (0.085) | 1.23 | ** | 0.174 (0.194) | 1.19 | 0.283 (0.176) | 1.33 | 0.330 (0.227) | 1.39 | |||||
| Never married | 0.035 (0.164) | 1.04 | −0.132 (0.078) | 0.88 | * | 0.147 (0.092) | 1.16 | −0.476 (0.259) | 0.62 | * | 0.160 (0.182) | 1.17 | −0.039 (0.280) | 0.96 | ||||
| Medical insurance (ref. private insurance) | ||||||||||||||||||
| Medicaid | 0.194 (0.255) | 1.21 | −0.193 (0.143) | 0.82 | 0.063 (0.154) | 1.07 | 0.528 (0.325) | 1.70 | −0.051 (0.328) | 0.95 | 0.026 (0.478) | 1.03 | ||||||
| Multiple insurance typesa | 0.088 (0.382) | 1.09 | 0.355 (0.187) | 1.43 | * | 0.114 (0.257) | 1.12 | 0.865 (0.381) | 2.37 | ** | −0.427 (0.602) | 0.65 | −1.070 (1.021) | 0.34 | ||||
| No insurance | −0.088 (0.134) | 0.92 | −0.199 (0.064) | 0.82 | *** | −0.125 (0.078) | 0.88 | 0.083 (0.186) | 1.09 | 0.001 (0.153) | 1.00 | 0.149 (0.209) | 1.16 | |||||
|
| ||||||||||||||||||
| Total Sample Size | 14084 | |||||||||||||||||
| No cost methods | 9,471 | |||||||||||||||||
| Pharmaceutical cessation products only | 2,295 | |||||||||||||||||
| Quit smoking programs only | 402 | |||||||||||||||||
| No cost+pharmaceutical product | 1,291 | |||||||||||||||||
| Pharmaceutical product +program | 201 | |||||||||||||||||
| No cost+program | 279 | |||||||||||||||||
| All three methods | 145 | |||||||||||||||||
Source: authors’ calculations from NCS. ***, **, and * denote coefficients with p-values of <.01, .05, and .10 respectively.
See note in Table 2.
First, while female smokers are more likely to quit with all methods (except combinations of no-cost, product, and program) relative to no-cost only, the strongest association is for methods that include a program of some type. Another interesting result revealed by the more detailed analysis is that smokers with less than high school education are much more likely to quit with methods or combinations of methods that include the use of a product (relative to no-cost methods only). This result is consistent with the finding in Mathios et al. (2006) that less educated consumers are exposed to more pharmaceutical product advertising than are more highly educated consumers. The more detailed analysis also suggests that smokers with some education past high school are more likely to attempt to quit with no cost methods and products (odds ratio 1.30) or perhaps with products combined with programs (though the association is not statistically different from zero). The more detailed categories also reveal that Blacks and Hispanics are much less likely to try to quit using only a smoking cessation product (odds ratio of .63 and .74 respectively) and that Blacks are more likely to try with a program only (odds ratio 1.4). Finally, for the insurance variables, the more detailed analysis suggests that NCS smokers covered by both Medicare and Medigap supplemental insurance are more likely to attempto quit with either a product only or a combination of a product and program (odds ratio 1.4 and 2.4 respectively). Because the association between Medicare/Medigap coverage and the use of the combination of products and programs is so strong – it leaves us with the question of whether this association results from increasing coverage of smoking cessation program by those insurance plans. If this association is in fact due to increased coverage of smoking cessation programs, it would provide strong evidence for policy makers. The more involved study of this question is left for future research.
Conclusions and Implications
The results in Table 5 and Table 6 show that the set of smokers who attempt to quit using methods that involve out-of-pocket time and money costs are not a random sample of all smokers. , Pharmaceutical products have been shown to double smoking abstinence rates in clinical trials over smokers administered placebos. However, the findings of this study suggest that, because of self-selection, the success rate of smokers using those products in actual practice is likely to be different than in clinical trials. More importantly, the results show that the probability that smokers choose a particular smoking cessation method varies systematically with socioeconomic characteristics. Our results provide evidence that can be used to better target smoking cessation information and resources to smokers most likely to use particular methods. In particular, there is intriguing and suggestive evidence that Black smokers are more likely to use stop smoking programs and that non white smokers are less likely to use clinically effective pharmaceutical products. Our results also hint that an avenue for getting smokers to use those products may be through Medicaid and Medicare reimbursement policies. We present evidence that suggests that Medicare recipients are more likely to use pharmaceutical products. In any event, better targeting of information about various methods to quit smoking is likely to lead to more quits and therefore make it more likely that we will raise cessation rates by enough to achieve the reduction in national smoking prevalence that the Healthy People initiative has set. More broadly, our results point to promising avenues of policy making and research for the substantial effort that is underway worldwide to develop tobacco control initiatives and policies to encourage smokers to quit.
Footnotes
The paper has benefitted from the thoughtful comments of two anonymous referees. We thank Eamon Molloy for expert research assistance.
Even assuming that no new smokers start, 37.4 million people (18.4 percent of the 2000 population) will be smokers in 2010 if the cessation rate remains steady. The cessation rate has to rise to 8 percent to achieve the Healthy People objective.
Although Zyban was approved for sale in 1997, it is not included as a separate NCS response category.
If a smoker only indicated he used some “other” method he is included in this category.
In the NCS private insurance includes medical, hospital, and health care insurance.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Dean R. Lillard, Cornell University Ithaca, NY, UNITED STATES, drl3@cornell.edu
Vandana Plassmann, Cornell University, vp25@cornell.edu.
Donald Kenkel, Cornell University and NBER, dsk10@cornell.edu.
Alan Mathios, Cornell University, adm5@cornell.edu.
References
- CDC. Current trends smoking prevalence and cessation in selected states, 1981–1983 and 1985 – The Behavioral Risk Factor Surveys. Morbidity and Mortality Weekly Report. 1986;35(47):740–743. [PubMed] [Google Scholar]
- CDC. Smoking cessation during previous year among adults – United States, 1990 and 1991. Morbidity and Mortality Weekly Report. 1993;42(26):504–507. [PubMed] [Google Scholar]
- CDC. Cigarette smoking among adults – United States, 2002. Morbidity and Mortality Weekly Report. 2004;53(20):427–431. [PubMed] [Google Scholar]
- Derby CA, Lasater TM, Vass K. Characteristics of smokers who attempt to quit and of those who recently succeeded. American Journal of Preventive Medicine. 1994;10(6):327–334. [PubMed] [Google Scholar]
- DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Valesquez MM, Rossi JS. The Process of Smoking Cessation: An Analysis of Precontemplation, Contemplation, and Preparation Stages of Change. Journal of Consulting and Clinical Psychology. 1991;59 (2):295–304. doi: 10.1037//0022-006x.59.2.295. [DOI] [PubMed] [Google Scholar]
- Escobedo LG, Peddicord JP. Smoking prevalence in U.S. birth cohorts: The influence of gender and education. American Journal of Public Health. 1996;86(2):231–236. doi: 10.2105/ajph.86.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Partnership to Reduce Tobacco Dependence. WHO evidence based recommendations on the treatment of tobacco dependence. Geneva: World Health Organization; 2001. [Google Scholar]
- Gilpin EA, Pierce JP. Demographic differences in patterns in the incidence of smoking cessation: United States 1950–1990. Annals of Epidemiology. 2002;12(3):141–50. doi: 10.1016/s1047-2797(01)00266-6. [DOI] [PubMed] [Google Scholar]
- Hahn LP, Folsom AR, Sprafka JM, Norsted SW. Cigarette smoking and cessation behaviors among urban blacks and whites. Public Health Reports. 1990;105(3):290–295. [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Goldstein MG, Hurt RD, Shiffman S. Recent advances in the pharmacotherapy of smoking. Journal of the American Medical Association. 1999;281(1):72–76. doi: 10.1001/jama.281.1.72. [DOI] [PubMed] [Google Scholar]
- Joossens L, Raw M. The tobacco control scale: a new scale to measure country activity. Tobacco Control. 2006;(15):247–253. doi: 10.1136/tc.2005.015347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King G, Poldenak A, Bendel RB, Vilsaint MC, Nahata SB. Disparities in smoking cessation between African Americans and whites: 1990–2000. American Journal of Public Health. 2004;91(11):1965–1971. doi: 10.2105/ajph.94.11.1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Feng. Manuscript. Department of Policy Analysis and Management; Cornell University: 2006. Cutting through the Smoke: Separating the Effect of Price on Smoking Initiation vs. Cessation. [Google Scholar]
- Machlin SR, Kleinman JC, Madans JH. Validity of mortality analysis based on retrospective smoking information. Statistics in Medicine. 1989;8(8):997–1009. doi: 10.1002/sim.4780080810. [DOI] [PubMed] [Google Scholar]
- Mathios Alan, Donald Kenkel, Dean Lillard, Rosemary Avery. Manuscript. Department of Policy Analysis and Management; Cornell University: 2006. Exposure to Smoking Cessation Product Advertising: Who Sees What and Where? [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual Causes of Death in the United States: 2000. Journal of the American Medical Association. 2004;291 (10):123801245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Murray Christopher JL, Lopez Alan D. Evidence-Based Health Policy – Lessons from the Global Burden of Disease Study. Science. 1996;274 (5288):740–743. doi: 10.1126/science.274.5288.740. [DOI] [PubMed] [Google Scholar]
- Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The Validity of Self-Reported Smoking: A Review and Meta-Analysis. American Journal of Public Health. 1994 Jul;:1086–1093. doi: 10.2105/ajph.84.7.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and Process of Self-change of Smoking: Toward an Integrative Model of Change. Journal of Consulting and Clinical Psychology. 1983;51 (3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Royce JM, Corbett K, Sorensen G, Okene J. Gender, social pressure, and smoking cessations: The Community Intervention Trial for Smoking Cessation (COMMIT) at baseline. Social Science and Medicine. 1997;44(3):359–370. doi: 10.1016/s0277-9536(96)00149-9. [DOI] [PubMed] [Google Scholar]
- Simmons Market Research Bureau. Study of Media and Markets: Technical Guide. 1994. [Google Scholar]
- U.S. Department of Health and Human Services. Tobacco Use Among US Racial/Ethnic Minority Groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: A Report of the Surgeon General. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1998. [Google Scholar]
- U.S. Department of Health and Human Services [USDHHS] Clinical Practice Guideline: Treating Tobacco Use and Dependence 2000 [Google Scholar]
- U.S. Department of Health and Human Services. Women and smoking: A Report of the Surgeon General. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2001. [Google Scholar]
- U.S. Census Bureau. Historical Income Tables – Households. 2006. [accessed 12/15/2006]. http://www.census.gov/hhes/income/histinc/inchhtoc.html#3.
- Warner K. Possible Increases in the Underreporting of Cigarette Consumption. Journal of the American Statistical Association. 1978 Jun;:314–318. [Google Scholar]
- World Health Organization. The World Health Report 1999: Making a Difference. Geneva: World Health Organization; 1999. [Google Scholar]
- World Health Organization. Tobacco Free Initiative (TFI) 2006. Available online at http://www.who.int/tobacco/en/
- Zhu SH, Melcer T, Sun J, Rosbrook B, Pierce JP. Smoking cessation with and without assistance. American Journal of Preventive Medicine. 2000;18(4):305–311. doi: 10.1016/s0749-3797(00)00124-0. [DOI] [PubMed] [Google Scholar]