Abstract
Background
Medication errors are a significant global concern and can cause serious medical consequences for patients. Little is known about medication errors in Middle Eastern countries. The objectives of this systematic review were to review studies of the incidence and types of medication errors in Middle Eastern countries and to identify the main contributory factors involved.
Methods
A systematic review of the literature related to medication errors in Middle Eastern countries was conducted in October 2011 using the following databases: Embase, Medline, Pubmed, the British Nursing Index and the Cumulative Index to Nursing & Allied Health Literature. The search strategy included all ages and languages. Inclusion criteria were that the studies assessed or discussed the incidence of medication errors and contributory factors to medication errors during the medication treatment process in adults or in children.
Results
Forty-five studies from 10 of the 15 Middle Eastern countries met the inclusion criteria. Nine (20 %) studies focused on medication errors in paediatric patients. Twenty-one focused on prescribing errors, 11 measured administration errors, 12 were interventional studies and one assessed transcribing errors. Dispensing and documentation errors were inadequately evaluated. Error rates varied from 7.1 % to 90.5 % for prescribing and from 9.4 % to 80 % for administration. The most common types of prescribing errors reported were incorrect dose (with an incidence rate from 0.15 % to 34.8 % of prescriptions), wrong frequency and wrong strength. Computerised physician rder entry and clinical pharmacist input were the main interventions evaluated. Poor knowledge of medicines was identified as a contributory factor for errors by both doctors (prescribers) and nurses (when administering drugs). Most studies did not assess the clinical severity of the medication errors.
Conclusion
Studies related to medication errors in the Middle Eastern countries were relatively few in number and of poor quality. Educational programmes on drug therapy for doctors and nurses are urgently needed.
Keywords: Medication error, Middle East countries, Prescribing, Administration, Transcribing
Introduction
The Middle Eastern region is strategically, politically and economically important for the whole world. There are fifteen countries between western Asia and northern Africa which make up the Middle Eastern region [1]. Economically, Middle Eastern countries are ranked by the World Bank according to their gross domestic product (GDP) on purchasing power parity (PPP) per capita. The high-income countries (HIC) include Qatar, the United Arab Emirates (U.A.E), Bahrain, Saudi Arabia, Kuwait, Israel and Oman. The upper-middle income countries (UMIC) are Iran, Jordan and Lebanon. The lower-middle iome countries (LMIC) are Egypt, Palestine, Syria, Yemen and Iraq [1]. The population of the Middle Eastern countries is approximately 300 million, with a population growth rate of 1.86 %. Elderly people of 65 years or over represent 3.63 % of the total population of Middle Eastern people [2]. The International Diabetes Foundation estimates that 26.6 million adults (8.6 % of the population) in the Middle East and North Africa currently have diabetes [3]. Obesity rates in the Middle East and North Africa are also among the highest in the world, particularly in the Gulf countries.
Medication errors (MEs) are under-reported in all countries [4], particularly in developing countries. MEs present a universal problem and can cause serious consequences for patients, especially those with acute complex medical conditions [5]. The National Patient Safety Agency revealed that MEs in all care settings in the UK occurred in each stage of the medication treatment process, with 16 % in prescribing, 18 % in dispensing and 50 % in administration of drugs [6].
For paediatric MEs it has been estimated that 3–37 % occur during prescribing, 5–58 % during dispensing, 72–75 % during administration, and 17–21 % are documentation errors [7]. Over an 8-year period in the UK, at least 29 children died due to MEs [8]. Safe drug therapy for children is a major issue in many low-income countries (LIC) and LMIC in the south [9].
Most of the research on MEs has been conducted in HIC in the USA and Europe. Information on the incidence of MEs in LIC and LMIC is limited. In our current research, we have focused on Middle Eastern countries in order to explore and highlight the problem of MEs in this region. There are a variety of reasons why MEs may be different in this region. These include the training of health professionals in clinical pharmacology, differences in relation to the role of clinical pharmacists, and the types of medicines prescribed, alongside cultural issues.
This systematic literature review therefore aimed to identify and review studies of the incidence and types of MEs in Middle Eastern countries, and identify the main contributing factors.
Methods
Search strategy
A systematic review of literature relating to MEs in prescribing, transcribing, dispensing, administration and documentation in adults and children in Middle Eastern countries was conducted in October 2011. The following electronic databases were searched: Embase (1980 – October 2011), Medline (1948 – October 2011), Pubmed (until October 2011), the British Nursing Index (1985 – October 2011) and the Cumulative Index to Nursing & Allied Health Literature (CINAHL) (1982 – October 2011). The search strategy included all ages, all languages, and all types of trials and studies. References from eligible articles were also hand-searched in order to identify additional relevant papers.
Search terms
The following keywords were used as search terms: medication error(s), prescribing error(s), dispensing error(s), administration error(s), documentation error(s), transcribing error(s), medication mistake(s), drug mistake(s), prescribing mistake(s), dispensing mistake(s), administration mistake(s), transcribing mistake (s), wrong medication, wrong drug(s), wrong dose(s), wrong route of administration, wrong calculation(s), physician(s), pharmacist(s) and nurse(s). Each of these key words were combined using “OR” then combined using “AND” with Middle East and also with the names of the appropriate countries (15 countries).
Review procedure
From previous systematic reviews of MEs, studies have been found to be heterogeneous, as they were conducted in different countries used different definitions and different methods to collect data [10, 11]. For this reason we did not try to analyse the data from a statistical viewpoint, but the results are summarised according to the type of MEs.
Inclusion/exclusion criteria
We included all types of studies, i.e., randomised controlled trials, non-randomised controlled trials, longitudinal studies, cohort or case–control studies, and descriptive studies that reported the incidence of medication errors or identified the causes of MEs in the Middle East countries, either in adults or children. We excluded reviews, letters, conference papers, opinions, reports or editorial papers.
Quality assessment
A quality assessment of the identified studies was performed. All relevant studies were reviewed according to 12 criteria adapted from two previous studies [11, 12]. The criteria were adapted to apply to any type of MEs study. Additionally, we evaluated or assessed the documented ethical approval obtained for each study. We therefore evaluated the papers according to the following 13 criteria:
Aims/objectives of the study clearly stated.
Definition of what constitutes a medication error.
Error categories specified.
Error categories defined.
Presence of a clearly defined denominator.
Data collection method described clearly.
Setting in which study conducted described.
Sampling and calculation of sample size described.
Reliability measures.
Measures in place to ensure that results are valid.
Limitations of study listed.
Mention of any assumptions made.
Ethical approval.
Results
Search results
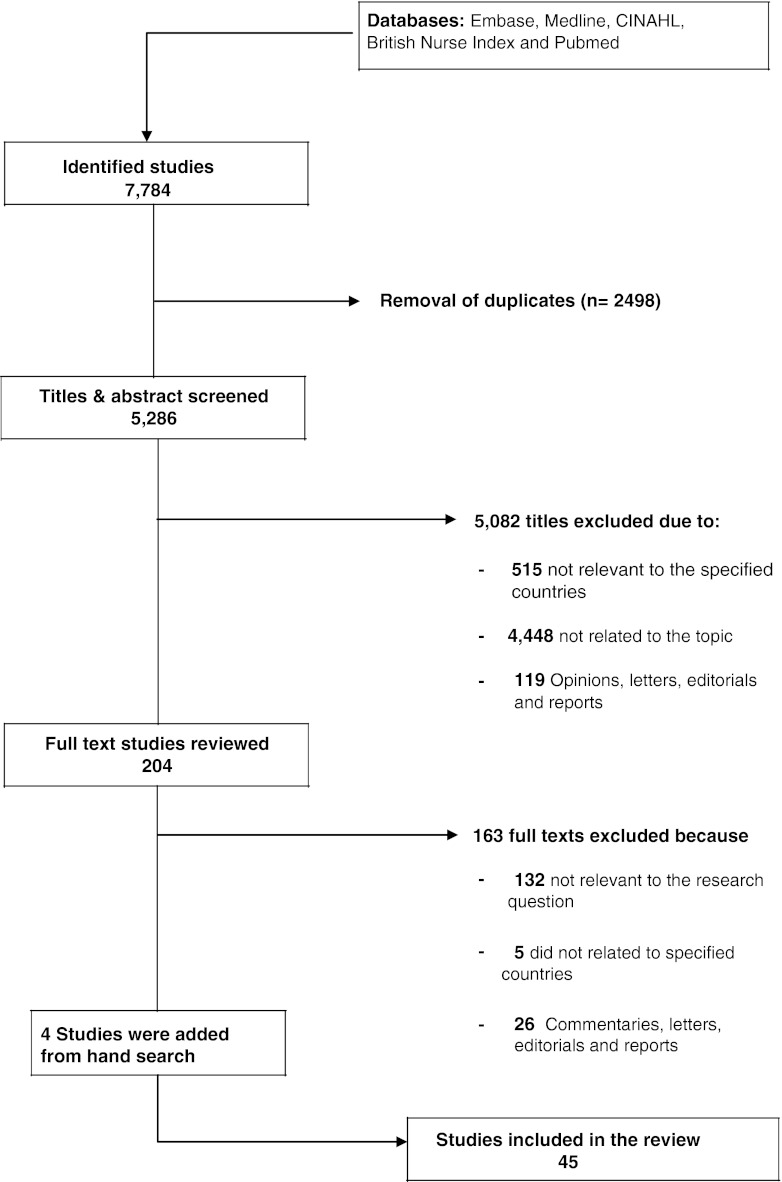
The results of this search strategy can be found in Fig. 1. More than 5,000 articles were excluded, as the papers were either not related to the specified countries or not relevant to MEs. This left 204 articles for full-text review. A further 163 articles were excluded because they were not relevant to the topic, not related to the specified countries or were opinion articles, letters, editorials and reports.
Fig. 1.
Flow chart for search and review process
Forty-one articles were identified as relevant. Four additional relevant studies were identified after hand-searching of the references of these studies. Forty-five articles were therefore finally relevant and are included in this systematic review (Fig. 1). The abstracts of four studies were in English but the full texts were in foreign languages (3 in Persian and 1 in Hebrew), and those papers were translated into the English language.
Countries with data
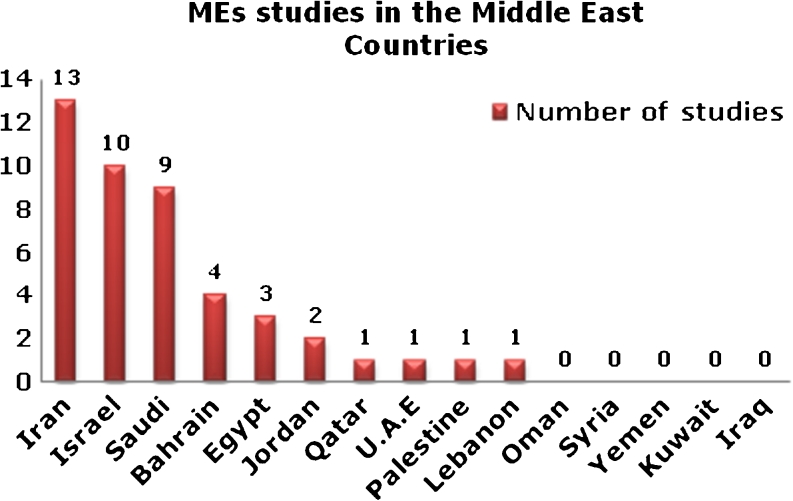
The 45 studies provided data for 10 of the 15 countries of the traditional Middle East (Fig. 2). These included 13 studies in Iran, 10 studies in Israel and 9 studies in Saudi Arabia. There was no available data on MEs in the following countries: Yemen, Kuwait, Iraq, Oman and Syria.
Fig. 2.
Graph illustrating origin of included studies
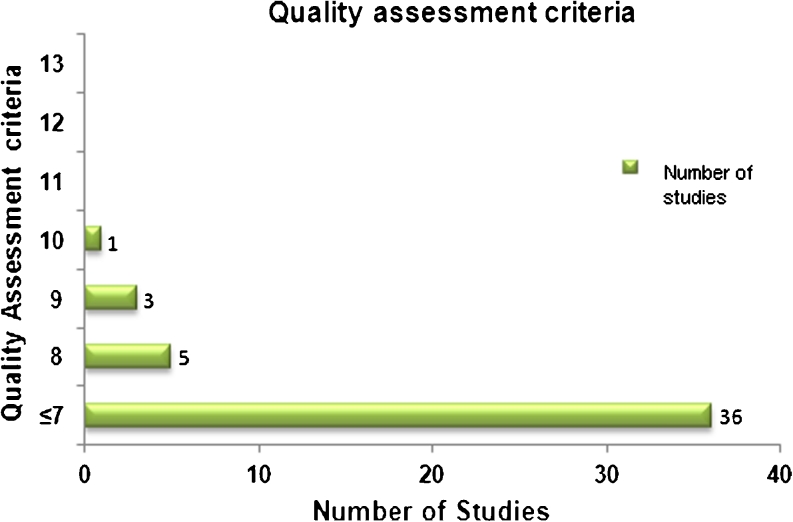
Quality assessment of studies
After the application of the quality assessment criteria which were modified to apply to any type of MEs study, no study met all the 13 criteria. Only one study fulfilled 10 criteria, three studies met 9 criteria, and five met 8 criteria. The remaining studies met less than 7 criteria (Fig. 3). Ten of the 45 studies did not specify the type of MEs and 14 of the 45 studies did not clearly state whether or not ethical approval was obtained.
Fig. 3.
Quality assessment criteria of included studies
Types of medication error studies
Twenty-one of the 45 studies assessed prescribing errors (Table 1). Most (seven) of these studies were conducted in Saudi Arabia and in Israel (five). One study assessed transcribing errors (Table 2). Eleven studies measured medication administration errors (Table 3) and most of these studies were performed in Iran. Tables 4 and 5 contain the 12 intervention studies that have been performed in Middle Eastern countries for adults and paediatric patients. Four of these studies were conducted in Israel. No studies were identified which evaluated dispensing errors and documentation errors in Middle East countries. Nine (20 %) studies out of the 45 studies focused on MEs in paediatric patients.
Table 1.
Studies describing prescribing errors
| Country (Setting) | Type of study | Duration | Sample | Outcome | Reference |
|---|---|---|---|---|---|
| Israel (General hospital) | Prospective, prescriptions were reviewed in pharmacy. | 6 months | 14,385 prescriptions | 160 MEs were detected; 97 (60.6 %) were prescribing errors; Incorrect dosage (44) was the most common type. | [14] |
| Bahrain (Primary care) | Prospective, prescriptions were collected by pharmacists. | 2 weeks | 77,511 prescriptions | 7.7 % of prescriptions contained errors; Omission errors (93.6 %), Commission errors (6.3 %). | [15] |
| Iran (Teaching hospital) | Prospective, prescriptions from elderly patients were collected. | 4 months | 3000 prescriptions | 829 (27 %) patients received at least one inappropriate prescription; 746 (24 %) patients had at least one medicine prescribed in duplicate. | [22] |
| Bahrain (Primary care) | Prospective, prescriptions for infants were collected by pharmacists. | 2 weeks | 2282 prescriptions | 90.5 % of prescriptions contained errors; 74.5 % of medications contained drug errors; Dosing frequency was incorrectly written in 20.8 % and dose strength was incorrectly in 17.7 %. | [16] |
| Palestine (General hospital) | Prospective, all patients with creatinine clearance ≤59 ml/min were included, data were collected from patients’ files. | 4 months | 78 patients | 63 (80 %) patients were having at least one inappropriate medication; 1.5—fold greater than the recommended dose, poor knowledge of pharmacokinetics of prescribed drug. | [23] |
| Egypt (Teaching hospital, ICU) | Prospective, direct observation by pharmacist was conducted to record medication-related problems. | 1 year | 220 patients | 619 medication-related problems were detected in 213 patients; Incorrect dosing (22 %) was the most common errors in ICU. | [24] |
| Bahrain (Primary care) | Prospective, iron prescriptions for infants were collected and reviewed by pharmacist. | 2 weeks | 2,282 prescriptions | 159 prescriptions included iron preparation; 56 out of 159 were issued without dosage forms and duration of therapy. | [17] |
| Iran (Teaching hospital) | Prospective, drug order sheets in nephrology ward were reviewed by clinical pharmacist. | 4 months | 76 patients (818 medications) | 86 (10.5 %) prescribing errors were detected in 46 of the admissions; wrong frequency (37.2 %), wrong dose (19.8 %) and overdose(12.8 %) were the most common types of errors. | [18] |
| Saudi (Primary care) | Prospective, prescriptions were reviewed in public and private centres | NR | 600 prescriptions | 64 (72 %) physicians were classified as writing low-quality prescriptions | [25] |
| Saudi (Teaching hospital) | Prospective, medication charts and orders data collected by pharmacists | 1 month | 1582 medication order | 113 (7.1 %) prescribing errors were detected; Wrong strength 39 (35 %) followed by wrong dose frequency 26 (23 %). | [26] |
| Saudi (Primary care) | Prospective, all medication prescriptions were analysed. | 1 working day | 5299 prescriptions | 990 (18.7 %) prescribing errors identified; 8 (0.15 %) prescribing errors had serious effect on the patients. | [27] |
| Bahrain (Primary care) | Prospective, prescriptions issued by the residents were collected by pharmacists | 1 year | 2692 prescriptions | 2372 (88 %) prescriptions had errors; total number of errors was 7139; Incorrect dose and wrong dose frequency (24.7 %) of errors. | [19] |
| Israel (Teaching hospital) | Prospective, case–control study | 18 months | 274 patients | 137 MEs were identified; 63 (46 %) errors were prescribing. | [20] |
| Saudi (Teaching hospital) | Retrospective, all prescriptions obtained from pharmacy were analysed by physicians and pharmacists. | 1 year | 3796 prescriptions | 94 % of prescriptions had no quantity indicated; 90.7 % of prescriptions had incomplete instructions for patients. | [28] |
| Iran (Paediatric hospital) | Retrospective, hospital information-based study. | 6 months | 898 medical charts | Incomplete information in 74 % of medication orders; Time of drug administration not reported in 47.8 % of medical charts. | [29] |
| Israel (Teaching hospital, ED) | Retrospective, charts review was performed by two physicians for adult patients transferred by ambulance. | 1 year | 471 patient charts | 24 (12.7 %) of 188 patients receiving drugs in vehicle were subject to MEs; In ED 120 (36 %) of 332 patients were subject to MEs. | [30] |
| Saudi (Tertiary hospital, PICU & paediatric wards) | Retrospective of paediatric physicians medication orders. | 5 weeks | 2,380 medication orders | 1,333 MEs were reported; 1,051 (78.8 %) errors were potentially harmful; Incidence rate was 56 per 100 medication order; Dose errors were the highest incidence (22 %). | [21] |
| Saudi (General Hospital) | Medical records were reviewed for adult patients. | 2 years | 2627 patient files | 3963 MEs were identified; 60 % of patient files contained one error; 30 % of patient files contained two errors, and 3 errors or more found in 10 % of patient files. Wrong strength was reported in 914 patients (35 %). | [31] |
| Israel (Not applicable) | Questionnaire | NR | N/A | 18 % of doctor orders were written according to the hospital standard; 3 % of doctors and 25 % of nurses were the rate of compliance in ED. | [32] |
| Israel (Not applicable) | Structured questionnaire sent to active physicians to evaluate the rates and types MEs that they had encountered. | NR | 627 physicians | 470 (79 %) physician made an error in prescribing; 376 (63 %) physicians made more than one error; 94 (16 %) physicians made one error. | [33] |
| Saudi (Primary care) | Self—administered questionnaire designed to explore factors influencing prescribing. | NR | 87 physicians | 47 (54 %) physicians believed that limited knowledge of pharmacology is a main cause of prescribing errors; 65 % of physicians had not received training in drug prescribing; 34 % of physicians had consulted a pharmacist before drug prescribing. | [34] |
MEs: Medication Errors; NR: Not Reported, N/A: Not Available.
Table 2.
Study describing transcribing errors
| Country (setting) | Type of study | Duration | Sample | Outcome | Reference |
|---|---|---|---|---|---|
| Iran (Teaching hospital) | Prospective, direct observational study to detect transcribing MEs. | 5 months | 287 medication charts | 289 errors were identified with average one error per chart; Omission error was rated as the highest (52 %) transcription error found in this study | [35] |
MEs: Medication Errors
Table 3.
Studies describing administration errors
| Country (setting) | Type of study | Duration | Sample | Outcome | Reference |
|---|---|---|---|---|---|
| Iran (Teaching hospital, ICU) | Prospective, random observational study by pharmacists for preparation and administration of IV drugs by nurses | 2 weeks | 524 preparation & administration process | 380 (9.4 %) errors were identified out of 4040 opportunities for errors; 33.6 % were related to the preparation process; 66.4 % were administration errors; Injection of bolus doses faster than recommended was 43 % of errors. | [38] |
| Israel (Three hospitals; 32 wards) | Multi-method (observations, interviews, administrative data) were conducted to test the learning mechanisms to limit MAEs. | NR | 173 nurses | One patient in 3 was exposed to MAEs each time they received medication. | [39] |
| Lebanon (10 community pharmacies) | Retrospective, each patient profile was reviewed and to confirm patient record information in-person interviews by qualified pharmacists. | 7 months | 277 patients | 60 % of patients were taking at least 1 inappropriate medication; Missing doses represented 19 % of patients with inappropriate medication . | [41] |
| Saudi (Teaching hospital) | Retrospective, incident reports documented by physicians and nurses were collected. | 2 years | 23,957 admissions | 38 MEs were reported; Incidence rate of MEs was 1.58 per 1000 admission; Missed medication was the most common error in 15 (39.5 %) patients; 50 % of the errors occurred at night. | [42] |
| Jordan (24 hospitals) | Descriptive (questionnaire) study of nurses’ perceptions about rate, causes and reporting of MEs. | NR | 799 nurses | Average number of MEs per nurse was 2.2; 42.1 % of MEs were reported to nurse managers; 60 % of nurses failed to report MEs. | [43] |
| Iran (Cardiac care unit) | Questionnaire study to investigate the frequency, type and causes of MEs in cardiac care unit. | NR | 60 nursing students | 10 % of nursing students had made MAEs; Incorrect drug dose calculation, poor drug knowledge were the most common type of errors. | [44] |
| Iran (Teaching hospital) | Survey study to investigate the frequency, type and causes of MEs of nursing students | NR | 76 nursing students | 17 % of nursing students reported MAEs; Wrong drug dose was the common cause of error. | [45] |
| Iran (Three nursing schools) | Descriptive self—report questionnaires | (Winter 2008) | 240 nursing students | 124 MAEs were made by student nurses; 0.5 average number of MAEs per nurse. | [46] |
| Iran (Different hospitals) | Questionnaire study was conducted to identify nursing errors and the related factors | (in 2010) | 239 nurses & head nurse | Lack of compiling and reviewing of the drug allergies and medical history of the patient were 34.7 % and 31.7 %, respectively; Lack of considering the proper time of giving the medicines were 27.5 % and 31.7 %, respectively. | [47] |
| Jordan (Teaching hospital) | Descriptive questionnaire study to determine the types, stages and factors contributing to MEs. | Not reported | 126 nurses | Rate of MEs of nurses, physicians and pharmacists were 48 %, 31.7 % and 11.1 %, respectively; Wrong dosage and wrong patient were the highest type of MEs reported. | [40] |
| Iran (Teaching & non teaching hospitals) | Questionnaire study performed to evaluate the relationship between the incidence and reporting of MEs by nurses and work conditions. | 7 months | 286 nurses | 19.5 ME cases were recalled by each nurse; Relationship between error incidence and nursing work load was statistically significant. | [48] |
ICU: Intensive Care Unit; MAEs: Medication Administration Errors; MEs: Medication Errors; NR: Not Reported
Table 4.
Interventional studies in adults
| Country (Setting) | Intervention | Duration | Sample | Outcome | Reference |
|---|---|---|---|---|---|
| Israel (Teaching hospital) | Comparison between prescription orders using CDOE and Handwritten order | NR | 4600 hospitalization days | Prescribing errors occurred in handwritten orders (11.3 %) higher than in CDOE (3.2 %); The use of CDOE was associated with a significant reduction in mean hospital stay. | [49] |
| Israel (Teaching hospital) | Comparison between CDOE and handwritten order in similar department | NR | 1350 adult patients (641 handwritten,709 CDOE) | Incidence of prescribing errors by handwritten orders (7.2 %) was higher than in CDOE (3 %); CDOE has a large impact on the prevention of prescribing errors. | [50] |
| U.A.E (Teaching hospital) | Clinical pharmacists established training and educational materials for inpatient nurses about MEs. | 4 months | 370 nurses | The clinical pharmacist’s program has improved knowledge of the inpatient nursing staff in terms of raising their awareness about medication errors. | [51] |
| Qatar (4 Primary care) | Pharmacists in four clinics within the service used online, integrated health care software to document all clinical interventions made. | 3 months | 82,800 patients | 589 (0.7 %) patients prescriptions were intercepted for suspected errors; 51 % of the interventions were related to dosing errors. | [52] |
| Egypt (Teaching hospital, cancer centre) | Clinical pharmacy interventions (detecting MEs, correcting those errors, sending recommendations to medical staff). | 1 year | 89 adults, 11 paediatrics | MEs reduced from 1548 to 444 errors after clinical pharmacy intervention implemented; 76 % of the errors recorded occurred in the prescribing stage. | [53] |
| Iran (Teaching hospital, infectious disease ward) | Assessment of the clinical pharmacists role in detecting and preventing of MEs. | 1 year | 861 patients | 112 MEs were detected by clinical pharmacists; physicians were responsible for MEs more than nurses and patients 55 (49 %), 54 (48 %), 3 (2.7 %) respectively. Drug dosing, drug choice were the most common error types. | [54] |
| Saudi (Three Goverement Centres) | Three types of interventions were evaluated: pre/post improve the quality of physicians prescriptions | NR | 61 physicians | In pre: 8 % of prescribed drugs were with major errors. In post: 2 % of prescribed drugs were with errors. | [55] |
CDOE (Computerized Drug Order Entry); MEs: Medication Errors; NR: Not Reported; U.A.E: United Arab Emirates.
Table 5.
Interventional studies in paediatric and neonatal patients
| Country(Setting) | Intervention | Duration | Sample | Outcome | Reference |
|---|---|---|---|---|---|
| Israel (Children Hospital, PCCD) | Pre/post implementation of CPOE and CDSS | 3 years | 13124 drug orders in first part 46970 orders in second part | 3 errors were identified in the first part of the study (all were overdoses); No errors were identified in the second part. | [56] |
| Israel (Children hospital, PICU) | CPOE implementation in four different periods | 3 years | 5000 PICU medication orders | 273 (5.5 %) medication orders contained prescription errors; 83 % of prescription errors were reduced after CDSS implemented. | [57] |
| Iran (Teaching hospital, Neonatal ward) | Comparison between physician order entry (POE) and nurse order entry (NOE) methods effect on reducing dosing MEs. | 4 months | 158 neonates | 80 % of non-intercepted medication errors in POE (period 1) occurred in the prescribing stage compared to 60 % during NOE (period 2); Prescribing errors were decreased from 10.3 % with POE to 4.6 % with NOE period, respectively. | [58] |
| Iran (Teaching hospital, Neonatal ward) | Comparison of CPOE effect without and with CDSS in three periods. | 7.5 months | 248 patients | MEs rates before intervention implemented (period 1) was 53 %; Implementation of CPOE without CDSS the MEs rate was 51 %; After CDSS was added the MEs rate was 34 %; Overdose was the most frequent type of errors. | [59] |
| Egypt (Teaching hospital, PICU) | Pre/post (physician education; new medication chart; physician feedback) study of prescribing errors in PICU. | 10 months | Pre :1417 medication orders, Post: 1096 medication orders | 1107 (78 %) orders had at least one prescribing error; Significant reduction in prescribing error rate to 35 % post-intervention (P < 0.001); Severe errors reduced from 29.7 % to 7 % after intervention. | [60] |
PCCD: Paediatric Clinical Care Department; CPOE: Computerized Physician Order Entry; CDSS: Clinical Decision Support System; PICU: Paediatric Intensive Care Unit.
Incidence of medication errors
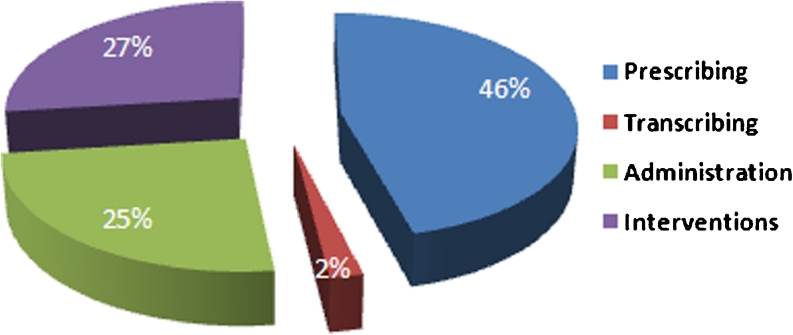
The incidence of MEs in this review is difficult to compare between studies because different methodologies and different definitions were used. We classified our results according to where they occurred during the medication treatment process, i.e., prescribing, transcribing and administration (Fig. 4).
Fig. 4.
Study classification by stage of medication process
Prescribing errors
Prescribing errors have been defined as MEs initiated during the prescribing process. These include the incorrect selection of medication, wrong dose, wrong strength, wrong frequency, incorrect route of administration, inadequate instruction for use of a medication and wrong dosage form [13]. Twenty-one (46 %) of the studies reported MEs that occurred during the prescribing stage of the medication process (Table 1). Eight studies identified in this review used the above definition [14–21], while the remaining studies did not clearly state a definition of prescribing errors. Thirteen were prospective studies and were conducted in six countries [14–20, 22–27]. Five were retrospective studies [21, 28–31], and the remaining three studies were questionnaires [32–34]. Four studies assessed prescribing errors in children [16, 17, 21, 29].
Estimates of the results were difficult to compare between studies because rates of error were expressed differently. Al-Khaja et al. reported the highest error rate, which was 90.5 % of prescriptions in a primary health care centre [16], while the lowest rate, reported by Al-Dhawailie, was 7.1 % of prescriptions in a teaching hospital [26]. The most common types of prescribing errors reported among the Middle Eastern countries were incorrect dose, wrong frequency and wrong strength. This systematic review revealed that the percentage of dosing errors that were reported during medication prescribing ranged from 0.15 % to 34.8 % of the prescriptions (Table 6).
Table 6.
prescriptions with dosing errors
| Country (setting) | No. of Prescriptions or medication orders | Dosing errors (number) | Dosing errors (%) | References |
|---|---|---|---|---|
| Israel (General hospital) | 14,385 prescriptions | 44 prescriptions | 0.3 | [14] |
| Bahrain (Primary care) | 77,511 prescriptions | 1,413 prescriptions | 1.8 | [15] |
| Bahrain (Primary care) | 2,282 prescriptions | 795 prescriptions | 34.8 | [16] |
| Egypt (Teaching hospital) | 2,286 medication prescribed | 503 medication prescribed | 22 | [24] |
| Bahrain (Primary care) | 2,282 prescriptions | 60 prescriptions | 2.6 | [17] |
| Iran (Teaching hospital) | 86 prescriptions | 11 prescriptions | 12.8 | [18] |
| Saudi (Primary care) | 1,582 medication orders | 14 medication orders | 0.89 | [26] |
| Saudi (Primary care) | 5,299 prescriptions | 8 prescriptions | 0.15 | [27] |
| Bahrain (Primary care) | 5880 medication orders | 397 medication orders | 6.7 | [19] |
| Israel (Teaching hospital) | 4736 prescriptions | 31 prescriptions | 0.65 | [20] |
| Israel (Teaching hospital) | 471 medication orders | 12 medication orders | 2.5 | [30] |
| Saudi (Tertiary hospital) | 2,380 medication orders | 526 medication orders | 22.1 | [21] |
Transcribing errors
One prospective study of transcription errors using a direct observational method was performed in Iran (Table 2) [35]. Transcribing errors were defined as any deviation in transcribing a medication order from the previous step. This study used a direct observation method of the transcribing process. The transcribing process involved prescriptions being either transferred to the hospital pharmacy or dispensed from ward-based stocks. When prescriptions were sent to the pharmacy, all the information was transcribed into the pharmacy information system. The pharmacy staff then filled, checked and dispatched the drugs to the ward. The observation process included review of each medication order on the order sheet, its transcription, administration nursing note and documentation of its prescriptions to the pharmacy database. The study result revealed that over 50 % of omission errors occurred at transcription stage.
Administration errors
Administration errors have been defined as a discrepancy between the drug therapy received by the patient and that intended by the prescriber or according to standard hospital policies and procedures [36, 37]. Three studies used this definition [38–40], while the remaining eight studies mainly used general definitions of MEs rather than a medication administration error definition. Two were prospective studies (Table 3) [38, 39]. One was an observational study in Iran which assessed the administration of intravenous drugs [38]. The other study, in Israel, used a variety of methods (observations, interviews and administrative data) [39]. The variation between the studies in definitions and methods used for data collection made comparisons difficult. The study that defined errors in preparation and administration, found that the error rates were higher in the administration process compared to the preparation process for intravenous medications, and within the administration process the technique of administration of bolus injection was the most common error (43.4 %) [38].
Two were retrospective studies [41, 42]. Seven were questionnaire studies of nurses’ perceptions of administration errors [40, 43–48]. The reported administration error rates ranged from 9.4 % to 80 % [38, 41]. Saab et al. reviewed patient records and confirmed their results through interviews with patients [41]. They found that the use of an inappropriate drug was higher when patients used both over-the-counter (OTC) and prescription medicines [41]. Sadat-Ali and colleagues assessed the prevalence and characteristics of MEs in patients admitted to a teaching hospital [42]. The authors found that the prevalence of MEs was low (1.58 per 1000 admission). This is likely due to the method used in the study, which was a retrospective review of incident reports—notorious for underestimation of error rates [42]. In addition, the authors revealed that most of the MEs (50 %) occurred during the night shift [42]. Seven questionnaire studies were conducted (5 in Iran and 2 in Jordan). All these studies evaluated nurses and student nurses opinion about the drug administration errors in their area of work [40, 43–48] (Table 3).
Interventional studies
Twelve (27 %) studies were identified describing interventions used to reduce MEs [49–60]. Of these, seven interventions were implemented in adult patients (Table 4) [49–55], and five interventions in paediatric and neonatal patients (Table 5) [56–60]. The interventions had been evaluated in studies from 3 months to 3 years, and most studies involved a comparison of computerised drug order entry systems, with or without clinical decision support systems (CDSS), and/or with handwritten prescriptions. The outcomes for all interventions were positive and led to the prevention and reduction of MEs.
Four interventional studies examined the role of the clinical pharmacist in reducing MEs [51–54]. All these studies were in adult patients only. These interventions led to a significant reduction in the number of MEs. Most of the errors detected were in the prescribing stage. Incorrect drug dosing, incorrect drug choice and drug interactions were the most common errors detected by clinical pharmacists. One of the intervention studies used a self-reported questionnaire designed to collect data after the clinical pharmacists established training and educational materials for inpatient nurses about MEs. No ME data was actually observed or collected [51].
In paediatric and neonatal patients, computerised physician order entry interventions, with and without CDSS, was the most commonly used intervention. All interventions that were implemented in paediatric patients found that medication error rates decreased after the CDSS was added to the computerised physician order entry system [56, 57, 59].
In addition, one study among the interventional studies in paediatric patients was conducted to compare two medication order entry methods: the physician order entry (POE) and nurse order entry [58]. The authors found that the error rates decreased within the NOE period compared to the errors within the POE period [58].
Types of errors
Incorrect dose was the most common type of error reported in 12 studies [14–21, 24, 26, 27, 30]. The dose error rates were reported from 0.15 % to 34.8 % of prescriptions errors (Table 6). Other studies included wrong frequency errors [16, 17], wrong strength [15, 16, 20, 25, 31], wrong or without dosage form [15, 16, 24, 27] and wrong duration of therapy [15, 16, 24, 27].
Medications involved
Differences in the reporting of medications between studies were apparent; some studies involved the medication names, and others listed only the therapeutic class. Most of the errors were related to antihistamine drugs [16, 22, 27], antibiotic medications [14, 23, 38, 60] and anticoagulant drugs [45, 54, 60]. In addition, medications reported in studies conducted on paediatric patients found that antihistamines, paracetamol, electrolytes and bronchodilator drugs were the most common drugs associated with errors [16, 30].
Severity of reported medication errors
The majority of studies did not assess the clinical consequences of reported MEs. Six (13 %, 6/45) attempted to classify the severity of the MEs [14, 21, 26, 30, 31, 38] (Table 7). Only one study reported the severity of the MEs in detail, but was a retrospective study [21]. Two other studies were retrospective [30, 31], while the other three were prospective studies [14, 26, 38]. One study reported 26 deaths and felt that MEs were a contributory factor [31].
Table 7.
Clinical consequences and medicines of reported medication errors
| Country | Type of error | Medicines | Clinical consequences | Reference |
|---|---|---|---|---|
| Israel | Prescribing | Anti-infectives, TPN, cytotoxics | Errors divided into potentially serious, clinically significant and clinically non-significant. MEs most frequent in haemato-oncology and these were the errors that were of greatest clinical significance | [14] |
| Saudi Arabia | Prescribing | Not stated | Examples of potentially serious errors were given including tenfold errors of amphotericin and captopril | [26] |
| Israel | Prescribing | Cardiovascular drugs | 14 MEs (8 %) were clinically significant. There were also 3 (2 %) severe MEs | [30] |
| Saudi Arabia | Prescribing | IV fluids, antibiotics, bronchodilators, opioid analgesics, cardiovascular drugs, sedatives | Majority of MEs were potentially harmful (1051, 79 %) | [21] |
| Saudi Arabia | Prescribing | Antibiotics, cardiovascular drugs | MEs were a contributory factor to 26 deaths | [31] |
| Iran | Administration | Antibiotics, antacids, corticosteroids | No clinically significant errors detected | [38] |
Factors contributing to medication errors
The determination of factors contributing to MEs is an important aspect of this review because preventing MEs from reaching the patient depends on a sound knowledge of the causes or contributing factors. The factors contributing to MEs were reported in 12 studies [15, 16, 19, 21, 26, 27, 31, 40, 42, 45–47]. The most common factors reported in this review were as follows:
Lack of knowledge of prescribing skills.
Lack of pharmacological knowledge of physicians and nurses.
Poor compliance with drug prescribing and administration guidelines.
Lack of reporting of MEs.
Heavy workload and new staff.
Miscommunications between health care professionals.
In general, poor knowledge of medicine prescribing and administration was the most common reported contributory factor of MEs in Middle Eastern countries [15, 16, 26, 31, 45, 47].
Discussion
The aim of this systematic review was to review studies of the incidence and types of MEs in Middle Eastern countries and to identify the main contributory factors involved. MEs are an important variable in determining patient safety. This review showed that there have been relatively few studies of MEs in the Middle East compared to the number from the US and Europe [61]. To our knowledge, no previous systematic review has evaluated MEs in Middle Eastern countries. Additionally, the quality of the studies in the Middle East was poor. Poor knowledge of clinical pharmacology was a major factor in many of the papers. This systematic literature review has shown that the scientific literature on MEs published in Middle Eastern countries is limited. No information was available on five of the countries included in the review. Many studies focused mainly on adult patients.
Prescribing errors
Many differences were found with regard to how the studies obtained and reported data. Most of the studies in Middle Eastern countries evaluated MEs during the prescribing stage. The reported incidence of prescribing errors in this review ranged from 7.1 % to 90.5 % of medication orders. A high rate of prescribing errors is known to be an international problem [61, 62]. In a previous systematic review conducted in the UK to identify the prevalence, incidence and nature of prescribing errors in hospital inpatients, prescribing errors were found to be a common occurrence [61], and this is consistent with our findings. The incidence of prescribing errors in that review were 2–14 % of medication orders [61], which was lower than that found in our review of MEs in Middle Eastern countries. However, another study in the UK found that prescribing error rates vary widely, ranging from 0.3 % to 39.1 % of medication orders [63]. It is possible that the incidence rate of prescribing errors in the Middle Eastern countries is higher than that reported in other countries in the world, for example in the UK, but it could also be due to methodological differences.
Transcribing errors
Although some studies classified the transcribing stage as the third most important area in the medication treatment process, Lisby et al. identified the transcribing stage as the area in which most errors occur [64]. In our review only one study assessed transcribing errors, and found that over 50 % of omission errors occurred at transcription stage; this is consistent with other studies [64, 65]. The shortage of studies in this stage of medication treatment may distort the reality of the incidence rate of errors.
Administration errors
Our review showed that administration errors occurred in 9.4 % to 80 % of drug administrations. This is higher than that reported in studies in HIC. Two observational studies found that medication administration error rates in the acute care setting varied between 14.9 % and 32.4 % in France and Switzerland, respectively [66, 67].
In our review only one observational study determined the frequency of MEs that occurred during the preparation and administration of intravenous drugs in an intensive care unit. It found that the rate of errors in drug administration (66.4 %) was higher than in preparation (33.6 %) [38]. Another study found that the medication administration error rate for intravenous medication is significantly higher than other types of medication, the researchers observing the preparation error rate as 26 % and the administration error rate as 34 % [68]. Our findings therefore are also consistent with the previous studies’ results highlighting that intravenous MEs occur more frequently than preparation errors [68]. In addition, Armitage and Knapman found that the frequency of administration errors ranges from 2.4 % to 47.5 %, depending on the drug distribution system in place [69]. The difference between the results of these studies may be affected by the different definitions and different methods used, and may also be due to the place of research and settings. However, in the UK a recent report by National Patient Safety Agency (NPSA) specified that 56 % of reported errors associated with severe harm occurred at the administration step [70].
Our results indicate that the most common types of errors reported were incorrect drug dose, wrong frequency and wrong strength during the prescribing stage. This is consistent with previous studies’ results. In comparison, studies of MEs in US and UK hospitals found that incorrect doses were the most common type of error [71]. The UK National Patient Safety Agency (2009) reported that the most common type of medication errors that occurred in the NHS was a wrong dose or wrong frequency of medications [6], also consistent with our findings.
Based on our review results, the main factor contributing to MEs in Middle Eastern countries is poor knowledge of medicines in both doctors (prescribers) and nurses (administering drugs), as was also the case with other studies’ [72]. Educational programmes for drug prescribers and nurses concerning drug therapy are urgently needed to avoid drug errors and to improve patient safety by clinical pharmacists and clinical pharmacologists. Different studies have found that clinical pharmacists play a significant role in delivering training and competency assessment [73].
Limitation of this review
Some limitations of this review should be considered in interpreting the results. The search strategy and search terms were designed in order to be as comprehensive as possible, but the databases used were directly biased to English-language research and studies. We therefore may have missed some studies because the original languages of the included countries of the Middle East is not English; all of the included countries speak Arabic except Iran (Persian) and Israel (Hebrew).
Conclusion
As the first systematic review to describe MEs in Middle Eastern countries, this review aimed to find out which scientific literature has reported on or evaluated MEs in Middle East countries. Although the studies related to MEs in the Middle Eastern countries were relatively few in number, there was a wide variation between studies in the error rates reported, and this may due to the variations in their definitions of medication errors, settings, the denominators and methodologies used. However, the quality of MEs studies that were identified in this review was poor. Most of the studies were conducted on adult patients, while very few MEs studies have been performed in paediatric hospitals. Many studies focused on prescribing errors and factors contributing to MEs. Our findings highlighted that poor knowledge of medicines was a contributory factor in both prescribers and nurses administering drugs. Middle Eastern countries urgently need to introduce educational programmes to improve prescribing skills and knowledge of prescribers, and to encourage nurses to improve their quality of drug administration.
Suggested recommendations
According to the review results, the following recommendations are suggested to allow decision-makers to improve medication safety and reduce MEs in Middle Eastern countries:
Increase the awareness of MEs of health care professionals.
Prescribers need to pay more attention to drug dosing.
Improve medication error reporting systems and policy among the Middle Eastern countries by removing barriers, clarifying the importance of reporting and encouraging health care professionals to report medication errors.
Clinical consequences of MEs should be assessed and evaluated in future studies
Carry out regular intensive educational and training programmes in pharmacotherapy for undergraduate medical and paramedical students.
Educational programmes by clinical pharmacists and clinical pharmacologists on drug therapy are urgently needed for doctors and nurses.
Acknowledgments
Zayed Alsulami is a postgraduate research student and sponsored by the Saudi Arabian government. The authors acknowledge these sponsors. The authors also thank Vafadar-Isfahani Natasha and Peter J Vas for their help in translating four reviewed papers into the English language.
Competing interest
The authors declare that they have no competing interests.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Footnotes
Contributor statement
All authors contributed to the manuscript during planning, data analysis, interpretation and revision. All authors approve of this final submitted version after their revision of the manuscript. Also, all authors agree to allow the corresponding author, Zayed Alsulami, to serve as the primary correspondent with the editorial office and to review and sign off on the final proofs prior to publication.
References
- 1.World Bank, World Development Indicators (2007) Washington, DC
- 2.Nations U. World population prospects: The 2010 Revision. New York: United Nations; 2010. [Google Scholar]
- 3.International Diabetes Federation . IDF diabetes atlas. 4. Brussels: International Diabetes Federation; 2009. [PubMed] [Google Scholar]
- 4.Osborne J, Blais K, Hayes J. Nurses’ perceptions: When is it a medication error? J Nurs Admin. 1999;29:33–38. doi: 10.1097/00005110-199904000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Kozer E. Medication errors in children. Paediatr Drugs. 2009;11:52–54. doi: 10.2165/0148581-200911010-00017. [DOI] [PubMed] [Google Scholar]
- 6.National Patient Safety Agency (2009) The report from the patient safety observatory. Safety in Doses: Improving the use of medicines in the NHS. London: NPSA. Available at http://www.nrls.npsa.nhs.uk/resources/?entryid45=61625 (last accessed 11 January 2012)
- 7.Miller M, Robinson K, Lubomski L, Rinke M, Pronovost P. Medication errors in paediatric care: a systematic review of epidemiology and an evaluation of evidence supporting reduction strategy recommendations. Qual Saf Health Care. 2007;16:116–126. doi: 10.1136/qshc.2006.019950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cousins D, Clarkson A, Conroy S, Choonara I. Medication errors in children - An eight year review using press reports. Paediatr Perinat Drug Ther. 2002;5:52–58. doi: 10.1185/146300902322125893. [DOI] [Google Scholar]
- 9.Choonara I. Children’s medicines–a global problem. Arch Dis Child. 2009;94:467. doi: 10.1136/adc.2009.160101. [DOI] [PubMed] [Google Scholar]
- 10.Conroy S, Sweis D, Planner C, Yeung V, Collier J, Haines L, et al. Interventions to reduce dosing errors in children: A systematic review of the literature. Drug Saf. 2007;30:1111–1125. doi: 10.2165/00002018-200730120-00004. [DOI] [PubMed] [Google Scholar]
- 11.Ghaleb M, Barber N, Franklin B, Yeung V, Khaki Z, Wong I. Systematic review of medication errors in pediatric patients. Ann Pharmacother. 2006;40:1766–1776. doi: 10.1345/aph.1G717. [DOI] [PubMed] [Google Scholar]
- 12.Allan E, Barker K. Fundamentals of medication errors research. Am J Health Syst Pharm. 1990;47:555–571. [PubMed] [Google Scholar]
- 13.Lesar T, Briceland L, Stein D. Factors related to errors in medication prescribing. JAMA. 1997;277:312–317. doi: 10.1001/jama.1997.03540280050033. [DOI] [PubMed] [Google Scholar]
- 14.Lustig A. Medication error prevention by pharmacists—an Israeli solution. Pharm World Sci. 2000;22:21–25. doi: 10.1023/A:1008774206261. [DOI] [PubMed] [Google Scholar]
- 15.Alkhaja K, Alansari T, Sequeira R. An evaluation of prescribing errors in primary care in Bahrain. Int J Clin Pharmacol Ther. 2005;43:294–301. doi: 10.5414/cpp43294. [DOI] [PubMed] [Google Scholar]
- 16.Alkhaja K, Alansari T, Damanhori A, Sequeira R. Evaluation of drug utilization and prescribing errors in infants: A primary care prescription-based study. Health Policy. 2007;81:350–357. doi: 10.1016/j.healthpol.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 17.Alkhaja K, Sequeira R, Alansari T, Damanhori A, James H, Handu S. Pediatric iron preparation for infants in Bahrain: some therapeutic concerns. Int J Clin Pharmacol Ther. 2010;48:200–205. doi: 10.5414/cpp48200. [DOI] [PubMed] [Google Scholar]
- 18.Vessal G. Detection of prescription errors by a unit-based clinical pharmacist in a nephrology ward. Pharm World Sci. 2010;32:59–65. doi: 10.1007/s11096-009-9341-9. [DOI] [PubMed] [Google Scholar]
- 19.Khaja K, Sequeira R, Alansari T, Damanhori A. Prescription writing skills of residents in a family practice residency programme in Bahrain. Postgrad Med J. 2008;84:198–204. doi: 10.1136/pgmj.2007.062547. [DOI] [PubMed] [Google Scholar]
- 20.Ben-Yehuda A, Bitton Y, Sharon P, Rotfeld E, Armon T, Muszkat M. Risk factors for prescribing and transcribing medication errors among elderly patients during acute hospitalization: a cohort, case–control study. Drugs Againg. 2011;28:491–500. doi: 10.2165/11590610-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 21.Aljeraisy M, Alanazi M, Abolfotouh M. Medication prescribing errors in a pediatric inpatient tertiary care setting in Saudi Arabia. BMC Res Notes. 2011;4:294. doi: 10.1186/1756-0500-4-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Azoulay L, Zargarzadeh A, Salahshouri Z, Oraichi D, Bérard A. Inappropriate medication prescribing in community-dwelling elderly people living in Iran. Eur J Clin Pharmacol. 2005;61:913–919. doi: 10.1007/s00228-005-0036-4. [DOI] [PubMed] [Google Scholar]
- 23.Sweileh W, Janem S, Sawalha A, Abu-Taha A, Zyoud S, Sabri I, et al. Pharmacoepidem Drug Saf. 2007;16:908–912. doi: 10.1002/pds.1412. [DOI] [PubMed] [Google Scholar]
- 24.Sabry N, Farid S, Aziz E. Role of the pharmacists in identification of medication related problems in the ICU: A preliminary screening study in an Egyptian Teaching Hospital. Aust J Basic Appl Sci. 2009;3:995–1003. [Google Scholar]
- 25.Neyaz Y, Khoja T, Qureshi N, Magzoub M, Haycox A, Walley T. Predictors of quality of medication prescribing in primary care in Riyadh city, Saudi Arabai. East Mediterr Health J. 2011;17:167–171. [PubMed] [Google Scholar]
- 26.Aldhawailie A. Inpatient prescribing errors and pharmacist intervention at a teaching hospital in Saudi Arabia. Saudi Pharm J. 2011;19:193–196. doi: 10.1016/j.jsps.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khoja T, Neyaz Y, Qureshi N, Magzoub M, Haycox A, Walley T. Medication errors in primary care in Riyadh city, Saudi Arabia. East Mediterr Health J. 2011;17:156–159. [PubMed] [Google Scholar]
- 28.Irshaid Y, Alhomrani M, Hamdi A, Adjepon-Yamorah K, Mahfouz A. Compliance with good practice in prescription writing at outpatient clinics in Saudi Arabia. East Mediterr Health J. 2005;11:922–928. [PubMed] [Google Scholar]
- 29.Valizadeh F, Ghasemi S, Nagafi S, Delfan B, Mohsenzadeh A. Errors in medication orders and the nursing staff’s reports in medical notes of children. Iran J Pediatr. 2008;18:33–40. [Google Scholar]
- 30.Lifshitz A, Goldstein L, Sharist M, Strugo R, Asulin E, Haim S, et al. Medication prescribing errors in the prehospital setting and in the ED. Am J Emerg Med. 2012;30(5):726–731. doi: 10.1016/j.ajem.2011.04.023. [DOI] [PubMed] [Google Scholar]
- 31.Dibbi H, Alabrashy H, Hussain W, Fatani M, Karima T. Causes and outcome of medication errors in hospitalized patients. Saudi Med J. 2006;27:1489–1492. [PubMed] [Google Scholar]
- 32.Vaknin O, Wingart-Emerel E, Stern Z. The quality of medication orders: can it be improved? Harefuah. 2003;42:490–494. [PubMed] [Google Scholar]
- 33.Bar-Oz B, Goldman M, Lahat E, Greenberg R, Avgil M, Blay A, et al. Medication errors and response bias: the tip of the iceberg. Isr Med Assoc J. 2008;10:771–774. [PubMed] [Google Scholar]
- 34.Magzoub M, Neyaz Y, Khoja T, Qureshi N, Haycox A, Walley T. Determinants of physicians’ medication prescribing behaviour in primary care in Riyadh city, Saudi Arabia. East Meditter Health J. 2011;17:160–166. [PubMed] [Google Scholar]
- 35.Fahimi F, Mohammed A, Abrishami R, Sistanizad M, Mazidi T, Faghihi T, et al. Transcription errors observed in a teaching hospital. Arch Iranian Med. 2009;12:173–175. [PubMed] [Google Scholar]
- 36.Greengold N, Shane R, Schneider P, Flynn E, Elashoff J, Hoying C, et al. The impact of dedicated medication nurses on the medication administration error rate: A randomized controlled trial. Arch Intern Med. 2003;163:2359–2367. doi: 10.1001/archinte.163.19.2359. [DOI] [PubMed] [Google Scholar]
- 37.Dean B. Errors in medication administration. Intens Care Med. 1999;25:341–342. doi: 10.1007/s001340050852. [DOI] [PubMed] [Google Scholar]
- 38.Fahimi F, Ariapanah P, Faizi M, Shafaghi B, Namdar R, Ardakani M. Errors in preparation and administration of intravenous medications in the intensive care unit of a teaching hospital: an observational study. Aust Crit Care. 2008;21:110–116. doi: 10.1016/j.aucc.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 39.Drach-Zahavy A, Pud D. Learning mechanisms to limit medication administration errors. J Adv Nurs. 2010;66:794–805. doi: 10.1111/j.1365-2648.2010.05294.x. [DOI] [PubMed] [Google Scholar]
- 40.Alshara M. Factors contributing to medication errors in Jordan: a nursing perspective. Iran J Nurs Midwifery Res. 2011;16:1–4. [PMC free article] [PubMed] [Google Scholar]
- 41.Saab Y, Hachem A, Sinno S, El-Moalem H. Inappropriate medication use in elderly Lebanese outpatients: Prevalence and risk factors. Drug Aging. 2006;23:743–752. doi: 10.2165/00002512-200623090-00004. [DOI] [PubMed] [Google Scholar]
- 42.Sadat-Ali M, Alshafei B, Alturki R, Ahmed S, Alabbas S, Alomran A. Medication administration errors in Eastern Saudi Arabia. Saudi Med J. 2010;31:1257–1259. [PubMed] [Google Scholar]
- 43.Mrayyan M, Shishani K, Alfaouri I. Rate, causes and reporting of medication errors in Jordan: nurses’ perspectives. J Nurs Manag. 2007;15:659–670. doi: 10.1111/j.1365-2834.2007.00724.x. [DOI] [PubMed] [Google Scholar]
- 44.Koohestani H, Baghcheghi N. Investigation medication errors of nursing students in cardiac care unit. Sci J Forensic Med. 2008;13:249–255. [Google Scholar]
- 45.Koohestani H, Baghcheghi N, Khosravi S. Frequency, type and causes of medication errors in student nurses. Iran J Nurs Res. 2008;21:17–27. [Google Scholar]
- 46.Koohestani H, Baghcheghi N. Barriers to the reporting of medication administration errors among nursing students. Aust J Adv Nurs. 2009;27:66–74. [Google Scholar]
- 47.Islamian J, Taheri F, Bahrami M, Mojdeh S. Assessing the nursing error rate and related factors from the view of nursing staff. Iran J Nurs Midwifery Res. 2010;15:272–277. [PMC free article] [PubMed] [Google Scholar]
- 48.Joolaee S, Hajibabaee F, Peyrovi H, Haghani H, Bahrani N. The relationship between incidence and report of medication errors and working conditions. Int Nurs Rev. 2011;58:37–44. doi: 10.1111/j.1466-7657.2010.00872.x. [DOI] [PubMed] [Google Scholar]
- 49.Oliven A, Zalman D, Shilankov Y, Yeshurun D, Odeh M. Prevention of prescription errors by computerized, on-line, individual patient related surveillance of drug order entry. Stud Health Technol Inform. 2002;90:632–634. [PubMed] [Google Scholar]
- 50.Oliven A, Michalake I, Zalman D, Dorman E, Yeshurun D, Odeh M. Prevention of prescription errors by computerized, on-line surveillance of drug order entry. Int J Med Inform. 2005;74:377–386. doi: 10.1016/j.ijmedinf.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 51.Elnour A, Ellahham N, Alqassas H. Raising the awareness of inpatient nursing staff about medication errors. Pharm World Sci. 2008;30:182–190. doi: 10.1007/s11096-007-9163-6. [DOI] [PubMed] [Google Scholar]
- 52.Hooper R, Adam A, Kheir N. Pharmacist-documented interventions during the dispensing process in a primary health care facility in Qatar. Drug Health Care Patient Saf. 2009;1:73–80. doi: 10.2147/dhps.s5534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Abou alsoud N, Elhamamsy M, Alzawahry H. Effects of clinical pharmacist interventions on clinical outcomes in oncology patients. Res J Medicine & Med Sci. 2010;5:133–141. [Google Scholar]
- 54.Khalili H, Farsaei S, Rezaee H, Dashti-Khavidaki S. Role of clinical pharmacists’ interventions in detection and prevention of medication errors in a medical ward. Int J Clin Pharm. 2011;33:281–284. doi: 10.1007/s11096-011-9494-1. [DOI] [PubMed] [Google Scholar]
- 55.Qureshi N, Neyaz Y, Khoja T, Magzoub M, Haycox A, Walley T. Effectiveness of three interventions on primary care physicians’ medication prescribing in Riyadh city, Saudi Arabia. East Meditter Health J. 2011;17:172–179. [PubMed] [Google Scholar]
- 56.Vardi A, Efrati O, Levin I, Matok I, Rubinstein M, Paret G, et al. Prevention of potential errors in resuscitation medications orders by means of a computerised physician order entry in paediatric critical care. Resuscitation. 2007;73:400–406. doi: 10.1016/j.resuscitation.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 57.Kadmon G, Bron-Harley E, Nahum E, Schiller O, Haski G, Shonfeld T. Computerized order entry with limited decision support to prevent prescription errors in a PICU. Pediatr. 2009;124:935–940. doi: 10.1542/peds.2008-2737. [DOI] [PubMed] [Google Scholar]
- 58.Kazemi A, Fors U, Tofighi S, Tessma M, Ellenius J. Physician order entry or nurse order entry? Comparison of two implementation strategies for a computerized order entry system aimed at reducing dising medication errors. J Med Internet Res. 2010;12:e5. doi: 10.2196/jmir.1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kazemi A, Ellenius J, Pourasghar F, Tofighi S, Salehi A, Amanati A, et al. The effect of computerized physician order entry and decision support system on medication errors in the neonatal ward: Experiences from an Iranian Teaching hospital. J Med Syst. 2011;35:25–37. doi: 10.1007/s10916-009-9338-x. [DOI] [PubMed] [Google Scholar]
- 60.Alagha H, Badary O, Ibrahim H, Sabri N. Reducing prescribing errors in the paediatric intensive care unit: an experiance from Egypt. Acta Paediatr. 2011;100:e169–e174. doi: 10.1111/j.1651-2227.2011.02270.x. [DOI] [PubMed] [Google Scholar]
- 61.Lewis P, Dornan T, Taylor D, Tully M, Wass V, Ashcroft D. Prevalence, incidence and nature of prescribing errors in hospital inpatients: A systematic review. Drug Saf. 2009;32:379–389. doi: 10.2165/00002018-200932050-00002. [DOI] [PubMed] [Google Scholar]
- 62.Dean B, Schachter M, Vincent C, Barber N. Prescribing errors in hospital inpatients: Their incidence and clinical significance. Qual Saf Health Care. 2002;11:340–344. doi: 10.1136/qhc.11.4.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Franklin B, Vincent C, Schachter M, Barber N. The inciedence of prescribing errors in hospital inpatients: An overview of the research methods. Drug Saf. 2005;28:891–900. doi: 10.2165/00002018-200528100-00005. [DOI] [PubMed] [Google Scholar]
- 64.Lisby M, Nielsen P, Mainz J. Errors in the medication process: frequency, type, and potential clinical consequences. Int J Qual Health Care. 2005;17:15–22. doi: 10.1093/intqhc/mzi015. [DOI] [PubMed] [Google Scholar]
- 65.Jiménez Muñioz A, Miguez A, Pérez M, Escribano M, Garcia M, Saez M. Medication error prevalence. Int J Health Care Qual Assur. 2010;23:328–338. doi: 10.1108/09526861011029389. [DOI] [PubMed] [Google Scholar]
- 66.Tissot E, Cornette C, Limat S, Mourand J, Becker M, Etievent J, et al. Observational study of potential risk factors of medication administration errors. Pharm World Sci. 2003;25:264–268. doi: 10.1023/B:PHAR.0000006519.44483.a0. [DOI] [PubMed] [Google Scholar]
- 67.Schneider M, Cotting J, Pannatier A. Evaluation of nurses’ errors associated in the preparation and administration of medication in a pediatric intensive care unit. Pharm World Sci. 1998;20:178–182. doi: 10.1023/A:1012087727393. [DOI] [PubMed] [Google Scholar]
- 68.Wirtz V, Barber N, Taxis K. An observational study of intravenous medication errors in the United Kingdom and in Germany. Pharm World Sci. 2003;25:104–111. doi: 10.1023/A:1024009000113. [DOI] [PubMed] [Google Scholar]
- 69.Armitage G, Knapman H. Adverse events in drug administration: A literature review. J Nurs Manag. 2003;11:130–140. doi: 10.1046/j.1365-2834.2003.00359.x. [DOI] [PubMed] [Google Scholar]
- 70.National Patient Safety Agency . The fourth report from the patient safety observatory. Safety in doses: medication safety incidents in the NHS. Patient safety observational report. London: NPSA; 2007. [Google Scholar]
- 71.Dean B, Allan E, Barber N, Barker K. Comparison of medication errors in an American and a British hospitals. Am J Health-Syst Pharm. 1995;52:2543–2549. doi: 10.1093/ajhp/52.22.2543. [DOI] [PubMed] [Google Scholar]
- 72.O’Shea E. Factors contributing to medication errors: a literature review. Clin Nurs. 1999;8:496–504. doi: 10.1046/j.1365-2702.1999.00284.x. [DOI] [PubMed] [Google Scholar]
- 73.Conroy S, North C, Fox T, Haines L, Planner C, Erskine P, et al. Educational interventions to reduce prescribing errors. Arch Dis Child. 2008;93:313–315. doi: 10.1136/adc.2007.127761. [DOI] [PubMed] [Google Scholar]