Abstract
Study Design
Subgroup analysis of prospective, randomized database.
Objective
The purpose of this study was to compare surgical or patient characteristics, such as fusion, instrumentation, or obesity, to identify whether these factors were associated with increased risk of reoperation for spinal stenosis. This prognostic information would be valuable to patients, healthcare professionals, and society as strategies to reduce reoperation, such as motion preservation, are developed.
Summary of Background Data
Reoperation due to recurrence of index level pathology or adjacent segment disease is a common clinical problem. Despite multiple studies on the incidence of reoperation, there have been few comparative studies establishing risk factors of reoperation after spinal stenosis surgery. The hypothesis of this subgroup analysis was that lumbar fusion or particular patient characteristics, such as obesity, would render patients with lumbar stenosis more susceptible to reoperation at the index or adjacent levels.
Methods
The study population combined the randomized and observational cohorts enrolled in SPORT for treatment of spinal stenosis. The surgically treated patients were stratified according to those who had reoperation (n=54) or no-reoperation (n= 359). Outcome measures were assessed at baseline, 1 year, 2 years, 3 years, and 4 years. The difference in improvement between those who had reoperation and those who did not was determined at each follow-period.
Results
Of the 413 patients who underwent surgical treatment for spinal stenosis, 54 patients had a reoperation within four years. At baseline, there were no significant differences in demographic characteristics or clinical outcome scores between reoperation and non-reoperation groups. Furthermore, between groups there were no differences in the severity of symptoms, obesity, physical examination signs, levels of stenosis, location of stenosis, stenosis severity, levels of fusion, levels of laminectomy, levels decompressed, operation time, intraoperative or postoperative complications. There was an increased percentage of patients with duration of symptoms greater than 12 months in the reoperation group (56% reoperation vs 36% no-reoperation, p<0.008). At final follow-up, there was significantly less improvement in the outcome of the reoperation group in SF36 PF (14.4 vs 22.6, p < 0.05), ODI (−12.4 vs. −21.1, p < 0.01), and Sciatica Bothersomeness Index (−5 vs −8.1, p < 0.006).
Conclusion
Lumbar fusion and instrumentation were not associated with increased rate of reoperation at index or adjacent levels compared to nonfusion techniques. The only specific risk factor for reoperation after treatment of spinal stenosis was duration of pretreatment symptoms > 12 months. The overall incidence of reoperations for spinal stenosis surgery was 13% and reoperations were equally distributed between index and adjacent lumbar levels. Reoperation may be related to the natural history of spinal degenerative disease.
INTRODUCTION
Revision surgery may be required at the index level or adjacent levels after surgical treatment of lumbar stenosis. There are a paucity of studies that identify predictors of lumbar reoperation. Although particular factors, such as obesity, smoking, or fusion, have been demonstrated to affect the outcome of treatment of spinal stenosis, the previous literature has not demonstrated whether these factors influence reoperation. Due to the relatively low incidence of reoperation, there are few prospective cohorts that are large enough to capture a significant number of reoperation cases and attempt to identify predictors of reoperation.
SPORT is a prospective multi-center study of surgical versus non-operative treatment for lumbar stenosis.1 The purpose of this subgroup analysis was to (1) determine the incidence of reoperation after lumbar surgery for spinal stenosis, (2) compare patient demographic characteristics, such as obesity, to identify whether these factors were associated with increased risk of reoperation, and (3) to compare surgical characteristics, such as fusion, to determine whether there was an associated increased risk of reoperation. This prognostic information would be valuable to patients, healthcare professionals, and society as strategies to reduce reoperation, such as motion preservation, are developed.
METHODS
Study Design
SPORT was conducted at 13 multidisciplinary spine practices in eleven states. The human subject committees at each center approved the standardized protocol. SPORT included a randomized cohort and a concurrent observational cohort. The detailed methods have been published previously. 2, 3
Patient Population
Inclusion criteria were neurogenic claudication or radicular leg pain with associated neurological signs, spinal stenosis seen on cross sectional imaging, symptoms that had persisted for at least twelve weeks, and physician confirmation that they were a surgical candidate. Exclusion criteria were spondylolysis and spondylolisthesis. Enrollment began in March 2000 and ended in March 2005. Patients were offered the choice of enrollment into a prospective, randomized arm or an observational arm. For the purposes of this study, the randomized and observational cohorts were combined into a single “as treated” analysis due to extensive crossover in the randomized cohort.
Study interventions
The protocol surgery consisted of standard posterior decompressive laminectomy with or without bilateral single level fusion. The non-operative protocol was “usual recommended care,” to include at least: active physical therapy, education and counseling with instructions regarding home exercise, and nonsteroidal anti-inflammatories if the patient tolerated them.
Study Measures
The primary end points were the SF-36 bodily pain (BP) and physical function (PF) scores and the AAOS MODEMS version of the Oswestry Disability Index (ODI) measured at six weeks, three months, six months and yearly up to 4 years. Secondary outcomes included the Stenosis Bothersomeness Index, the Low Back Pain Bothersomeness scale and the Leg Pain bothersomeness scale. 1 Although this was not an a priori specified subgroup analysis, whether patients underwent additional surgery was prospectively reported by patients and research nurses at each site visit as part of the study protocol. However, additional information on the reoperation including indications, levels, and nature of surgery (decompression or fusion), was not reported in a standard manner.
Statistical analysis
Patients who underwent surgical treatment of spinal stenosis were divided into reoperation and no-reoperation groups. The primary analyses compared baseline demographic and clinical factors, operative details, and change in the clinical outcome measures within each treatment arm (i.e., surgery or non-operative). Change in outcome measures was adjusted for center, age, gender, baseline score, income, treatment preference, duration of symptoms, compensation, smoking status, BMI, baseline Sciatica Bothersomeness, joint, stomach and bowel problems.
Statistical modeling was performed with use of SAS software (version 9.1; SAS Institute, Cary, North Carolina), with the procedures PROC MIXED, and S-PLUS software (version 6.2; Insightful, Seattle, Washington) was used for all other calculations. Significance was defined as a p value of 0.05 on the basis of a two-sided hypothesis test.
Power Analysis
A post-hoc power analysis was performed using chi squared analysis to determine the statistical power given the rate of fusion in the reoperation (7/53=13.2%) and no reoperation groups (40/353 = 11.3%) using SigmaPlot software with alpha = 0.05. The required sample size was also calculated for 80% power given the proportions in group 1 and group 2 and alpha = 0.05 for 80% power to detect a statistically significant difference between groups.
RESULTS
Among the 403 patients who underwent surgery, there were 54 patients who underwent additional surgery (“Reoperation”) and 359 patients who did not undergo additional surgery (“No Reoperation”) within four years of enrollment. Forty-two of 54 patients had complete outcome information (SF36, ODI) at four year final followup. Forty seven of the 54 patients had complete information on the type of reoperation.
There were no statistically significant baseline demographic differences between groups in age, gender, ethnicity, race, education, marital status, work status, compensation, mean BMI, smoking, or comorbidities (Table 1). There was an increased incidence of stomach problems in the Reoperation group (35% vs 19%, p<0.009).
Table 1.
Patient baseline demographic characteristics, comorbidities, and health status measures according to status of revision surgery.
| Had Revision Surgery* (n=54) | No Revision Surgery (n=359) | p-value | |
|---|---|---|---|
| Mean Age (SD) | 62.6 (11.4) | 64 (12.3) | 0.46 |
| Female | 18 (33%) | 141 (39%) | 0.49 |
| Ethnicity: Not Hispanic† | 53 (98%) | 343 (96%) | 0.60 |
| Race - White | 44 (81%) | 305 (85%) | 0.65 |
| Education - At least some college | 33 (61%) | 226 (63%) | 0.91 |
| Marital Status - Married | 42 (78%) | 258 (72%) | 0.46 |
| Work Status | 0.80 | ||
| Full or part time | 16 (30%) | 131 (36%) | |
| Disabled | 6 (11%) | 34 ( 9%) | |
| Retired | 26 (48%) | 156 (43%) | |
| Other | 6 (11%) | 38 (11%) | |
| Compensation - Any‡ | 4 (7%) | 26 (7%) | 0.81 |
| Mean Body Mass Index (BMI), (SD)§ | 29 (4.7) | 29.4 (5.4) | 0.60 |
| Smoker | 6 (11%) | 31 (9%) | 0.74 |
| Comorbidities | |||
| Hypertension | 23 (43%) | 152 (42%) | 0.91 |
| Diabetes | 6 (11%) | 51 (14%) | 0.69 |
| Osteoporosis | 3 (6%) | 29 (8%) | 0.71 |
| Heart Problem | 15 (28%) | 87 (24%) | 0.69 |
| Stomach Problem | 19 (35%) | 67 (19%) | 0.009 |
| Bowel or Intestinal Problem | 5 (9%) | 45 (13%) | 0.64 |
| Depression | 6 (11%) | 40 (11%) | 0.82 |
| Joint Problem | 30 (56%) | 192 (53%) | 0.89 |
| Other¶ | 19 (35%) | 124 (35%) | 0.95 |
| Time since most recent episode > 1 year | 30 (56%) | 128 (36%) | 0.008 |
| Pseudoclaudication - Any | 44 (81%) | 290 (81%) | 0.95 |
| SLR or Femoral Tension | 13 (24%) | 76 (21%) | 0.76 |
| Pain radiation - any | 41 (76%) | 281 (78%) | 0.83 |
| SF-36 scores, mean(SD)|| | |||
| Bodily Pain (BP) | 29.5 (15.4) | 28.8 (16.3) | 0.77 |
| Physical Functioning (PF) | 31 (21.4) | 31.9 (21.9) | 0.79 |
| Physical Component Summary (PCS) | 28 (7.2) | 28.8 (7.8) | 0.49 |
| Mental Component Summary (MCS) | 49.2 (12.1) | 48.5 (12) | 0.70 |
| Oswestry (ODI)** | 45.9 (18.1) | 45.6 (17.9) | 0.89 |
| Stenosis Frequency Index (0–24)†† | 15.4 (4.7) | 14.9 (5.7) | 0.59 |
| Stenosis Bothersome Index (0–24)‡‡ | 15.5 (4.8) | 15.4 (5.5) | 0.92 |
| Back Pain Bothersomeness§§ | 4.6 (1.6) | 4.2 (1.8) | 0.09 |
| Leg Pain Bothersomeness¶¶ | 4.5 (1.4) | 4.6 (1.6) | 0.71 |
| Satisfaction with symptoms - very dissatisfied | 46 (85%) | 274 (76%) | 0.20 |
| Problem getting better or worse | 0.17 | ||
| Getting better | 0 ( 0%) | 14 ( 4%) | |
| Staying about the same | 12 (22%) | 103 (29%) | |
| Getting worse | 41 (76%) | 236 (66%) | |
| Treatment preference | 0.41 | ||
| Preference for non-surg | 7 (13%) | 74 (21%) | |
| Not sure | 10 (19%) | 57 (16%) | |
| Preference for surgery | 37 (69%) | 228 (64%) | |
| Procedure | 0.43 | ||
| Decompression only | 41 (85%) | 309 (89%) | |
| Non-instrumented fusion | 2 ( 4%) | 20 ( 6%) | |
| Instrumented fusion | 5 (10%) | 20 ( 6%) | |
| Multi-level fusion | 1 (2%) | 15 (4%) | 0.66 |
| Decompression level | |||
| L2–L3 | 24 (47%) | 121 (35%) | 0.13 |
| L3–L4 | 39 (76%) | 239 (69%) | 0.35 |
| L4–L5 | 47 (92%) | 321 (93%) | 0.84 |
| L5-S1 | 20 (39%) | 132 (38%) | 0.99 |
| Number of Levels decompresssed | 0.35 | ||
| 0 | 2 ( 4%) | 6 ( 2%) | |
| 1 | 9 (17%) | 83 (24%) | |
| 2 | 14 (26%) | 112 (32%) | |
| 3+ | 28 (53%) | 152 (43%) | |
| Operation time | 127.8 (65.8) | 129.4 (66.1) | 0.87 |
| Blood loss | 277.8 (289.2) | 317.4 (419.8) | 0.52 |
| Blood Replacement | |||
| Intraoperative replacement | 5 (10%) | 34 (10%) | 0.81 |
| Post-operative transfusion | 3 (6%) | 17 (5%) | 0.98 |
| Length of stay | 2.8 (2.1) | 3.3 (2.4) | 0.24 |
| Intraoperative complications | |||
| Dural tear/ spinal fluid leak | 3 (6%) | 34 (10%) | 0.52 |
| Other | 0 (0%) | 3 (1%) | 0.84 |
| None | 49 (94%) | 315 (89%) | 0.41 |
| Postoperative complications/events¶¶ | |||
| Wound hematoma | 1 (2%) | 3 (1%) | 0.99 |
| Wound infection | 3 (6%) | 6 (2%) | 0.17 |
| Other | 0 (0%) | 23 (7%) | 0.12 |
| None | 45 (88%) | 305 (87%) | 1 |
Patients who underwent reoperation for lumbar spine stenosis within four years of index surgery. The index surgery is within four years of enrollment.
Race or ethnic group was self-assessed. Whites and blacks could be either Hispanic or non-Hispanic.
This category includes patients who were receiving or had applications pending for workers compensation, Social Security compensation, or other compensation.
The body-mass index is the weight in kilograms divided by the square of the height in meters.
Other = problems related to stroke, cancer, fibromyalgia, CFS, PTSD, alcohol, drug dependency, lung, liver, kidney, blood vessel, nervous system, migraine or anxiety.
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms.
The Stenosis Frequency Index ranges from 0 to 24, with lower scores indicating less severe symptoms.
The Stenosis Bothersomeness Index ranges from 0 to 24, with lower scores indicating less severe symptoms.
The Low Back Pain Bothersomness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms
Any reported complications up to 8 weeks post operation. None of the following were reported: bone graft complication, CSF leak, nerve root injury, paralysis, cauda equina injury, wound dehiscence, pseudarthrosis.
At baseline, there were no statistically significant differences between groups in primary outcome measures (SF36 BP, PF, PCS, MCS, ODI). There were no statistically significant differences between groups in the secondary outcome measures: Stenosis Frequency Index, Stenosis Bothersomeness Index, Back Pain Bothersomeness, Leg Pain Bothersomeness, percent satisfied with symptoms, percentage of problems improving or worsening, or treatment preference at baseline (Table 1). There were no statistically significant baseline differences between groups in clinical findings between groups (pseudoclaudication, SLR, pain radiation, neurological deficit, reflexes, sensory deficit, motor weakness, stenosis levels, stenosis locations, or stenosis severity). There was an increased percentage of patients with duration of symptoms greater than 12 months in the reoperation group (56% Reoperation vs 36% No-Reoperation, p<0.008).
There were no statistically significant differences in procedure details for the index procedure (decompression vs. noninstrumented fusion vs instrumented fusion, multilevel fusion, laminectomy level, or number of levels decompressed) between groups. There were no statistically significant differences in operative time, blood loss, blood replacement, intraoperative replacement, post operative transfusion, length of stay, intraoperative complications (including dural tear), or postoperative complications (hematoma, infection, or other) between groups (Table 1). However, the post-hoc power based on the numbers of patients in both groups who revealed inadequate power to detect a statistically significant difference in the rate of fusion between reoperation and no-reoperation groups. The required sample size to detect a difference is 4233 patients given the percentages of fusion in the reoperation and no reoperation groups.
In total, 13% (54/413) of patients underwent reoperation within 4 years. There were 47 patients in whom the details of the reoperation are available. Indications for reoperation are reported in Table 2. Of the 47 reoperations, the majority of reoperations (24/47 = 45%) were performed for recurrent spinal stenosis or development of spondylolisthesis. A new condition accounted for (8/47 = 15% of all reoperations. Nine (5/47) percent of reoperations were performed for complications of the index operation. Levels of reoperation are reported in Table 3. Of 35 patients in whom location of reoperation was available, 17 (17/413 = 4.2% of the overall population) had reoperation at the index level only and 18 (18/413 = 4.4% of entire population) had surgery at least one level other than the index level. Twelve patients (2.9%) had unknown level of reoperation surgery. Therefore the actual incidence of reoperation at the index level is between 4.2 and 7.2% and adjacent level reoperation is between 4.4 and 7.4%.
Table 2.
Indications for Reoperation Surgery
| Recurrent stenosis/progressive spondylolisthesis | 24 (6%), |
| Pseudoarthrosis/fusion exploration | 0 |
| Complication | 5 (1.2%) |
| New condition | 8 (2%) |
| Other | 14 (3.4%) |
Table 3.
Levels of Reoperation
| Percent of Reoperations | Percent of Total Patient Population | ||
|---|---|---|---|
| Index Level | 17 | 36% (Range 36% - 61%) | 4.2% (Range 4.2% - 7.2%) |
| Adjacent Level | 18 | 38% (Range 38% - 63%) | 4.4% (Range 4.4% - 7.4%) |
Twelve patients had unknown (unreported) levels of reoperation. Therefore, a range of incidence of reoperation was calculated assuming that all of the reoperations occurred at either the index or adjacent levels.
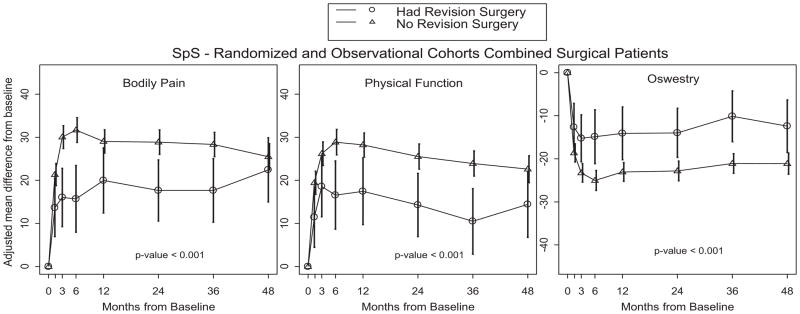
Adjusted changes in outcome measures between reoperation and no-reoperation groups are displayed in Table 4. Averaged over four years, there was significantly less improvement in the reoperation group compared to the no-reoperation group in the primary outcome measures SF36 BP (18 vs 27.9, p<0.001), SF36 PF (14 vs 24.9 p<0.001), ODI (−12.7 vs −21.9, p<0.001), There was also significantly less improvement in a secondary outcome measure, the sciatica bothersomeness index averaged over four years (−4.8 vs −8.2, p<0.001) (Table 4, Figure 1). Outcome scores at one, two, three, and four years are indicated in Table 4. At one year after the reoperation, there was significantly less improvement in SF36 BP (20 vs 29, p=0.03), SF36 PF (17.4 vs 28.2, p=0.01), SF36 PCS (7.1 vs 10.9, p=0.03), ODI (−14.1 vs −23.1, p=0.007), Sciatica Bothersomeness Index (−6 vs −8.9, p=0.01), Low Back Pain Bothersomeness (−1.5 vs −2.2, p=0.04), Leg Pain Bothersomeness (−1.9 vs −2.8, p=0.01). At four years after the index operation, there was no difference between reoperation and no reoperation patients in SF36 BP (22.4 vs 25.5, p=0.46), SF36 PCS (6.5 vs 9, p=0.18), Low Back Pain Bothersomeness (−1.6 vs −1.8, p=0.4), and Patient Satisfaction (59.8% vs 58.1%, p=0.79). There was less improvement in reoperation patients in SF36 PF (14.4 vs 22.6, p=0.05), ODI (−14.4 vs −21.1, p=0.01), Sciatica Bothersomeness Index (−5 vs −8.1, p=0.006).
Table 4.
Levels of Reoperation Surgery
| Total (n = 47) | Match (n=17) | No match (n=18) | No level (n=12) | |
|---|---|---|---|---|
| Recurrent stenosis | 23 | 9 | 12 | 2* |
| Pseudoarthrosis/fusion exploration | 0 | 0 | 0 | 0 |
| Complication | 3 | 0 | 0 | 3 |
| Other | 13 | 4 | 2 | 7 |
| New condition | 8 | 4 | 4 | 0 |
HSS732 and NEBR159 have type of revision of recurrent stenosis, but no levels were recorded.
Figure 1.
Primary outcomes over time by status of revision surgery with area under curve p-value that compares revision surgery group to no revision surgery group.
DISCUSSION—NOT HIGHLIGHTED BECAUSE SIGNIFICANTLY CHANGED
The cumulative rate of reoperation was 13% of patients over the study period and averaged 3.3% of patients per year. The only specific patient demographic risk factor associated with reoperation was duration of symptoms greater than 12 months. Despite the study hypothesis, surgical factors, such as fusion or instrumentation, were not different between the reoperation and no reoperation groups. These results demonstrate that patients who underwent reoperation had significantly less improvement in outcome immediately after the index operation, but outcomes improved over the study period.
The rate of reoperation reported is similar to that of other studies in the literature. 4,5 The reported rate of reoperation after laminectomy for treatment of spinal stenosis without spondylolisthesis varies from 2.7% to 36% at five to ten years after surgery; 6,7 however the mean rate appears to be 10–15%. 4,5
The prevalence of other clinical factors suspected to affect outcome, such as obesity, 8 smoking, or older age, was not significantly different between reoperation and non-reoperation groups. The clinical finding of increased duration of symptoms associated with reoperation was not surprising. Previous SPORT studies have established that duration of spinal stenosis symptoms greater than 12 months is associated with less improvement in outcome. 9 We suspect that patients with poor outcome may have been predisposed to undergo revision surgery due to refractory pain.
The most commonly advanced hypothesis of adjacent segment disease is that fusion leads to premature degeneration at other nonfused segments. 5,10,11–13 Our results demonstrate similar rates of fusion in patients who underwent reoperation (7/53 = 13.2%) and versus no reoperation (40/353= 11.2%, p =0.43), although the power analysis reveals underpowering to detect a statistically significant difference in the rate of fusion between groups given the current proportions. Some previous studies have attributed increased rates of adjacent segment disease to fusion 5,11–13 Compared to these previous reports, our study is the largest in the literature and includes a pure, relatively homogenous study population of spinal stenosis patients instead of a mixed group of patients with spinal stenosis and spondylolisthesis. 5
Patients who underwent reoperation demonstrated significantly less improvement than patients who did not undergo reoperation immediately after the index operation. However, by four years after the index surgery, the outcomes of the reoperation and no reoperation patients became more similar in several measures. These results conflict with some of the previous studies describing a high incidence of “Failed Back Surgery Syndrome” after reoperation. 15 We suspect that the poor outcome of reoperation reflects a poor outcome of the index operation since the clinical factor of duration of symptoms greater than 12 months has been demonstrated to be a predictor of poor outcome of index surgery in other SPORT subgroup analyses. 9 Additionally, there was no difference in clinical signs and symptoms, such as depressed reflexes or claudication symptoms, between groups to suggest misdiagnosis as the etiology of the poor results of reoperation in some patients.
Limitations of this study include the retrospective nature of the analysis and the small numbers of patients who underwent reoperation. As discussed earlier, there is a possibility of type II error which may have prevented us from identifying true differences between the reoperation and no reoperation groups. This is due to the relatively rare incidence of reoperation. Additionally, there is the inherently subjective nature of surgeons and patients choosing reoperation and the possibility that there may have been other patients who experienced a poor outcome who chose not to undergo reoperation. However, other studies specifically focused on adjacent segment disease have used reoperation as an endpoint. 5 There is also the possibility of an unknown confounder influencing the incidence of reoperation, such as litigation or facet degeneration, which may predispose patients toward premature degeneration at the index or adjacent segments. Another limitation of this study is that the authors were unable to identify whether the preoperative symptoms resolved after the initial operation prior to the reoperation. Poor results of the index operation may confound the results of the reoperation and lead to the impression that the reoperation was a clinical failure.
In conclusion, reoperation was a relatively uncommon event occurring in 13% of patients and approximately 50% of the reoperations were performed for symptoms at adjacent spinal levels. The only specific patient demographic risk factor associated with reoperation was duration of symptoms greater than 12 months. These results demonstrate that patients who underwent reoperation had significantly less improvement in outcome immediately after the index operation, but outcomes improved over the study period. These results suggest reconsideration of the classical hypothesis of elevated rates of adjacent segment disease occurring due to lumbar fusion, since reoperations occurred after both decompressions and lumbar fusions.
KEY POINTS.
This subgroup analysis compared patients who underwent reoperation to patients who did not undergo reoperation to establish risk factors for reoperation after treatment of spinal stenosis.
Reoperation after treatment of spinal stenosis was only related to duration of pretreatment symptoms greater than 12 months.
In contrast to the study hypothesis, there was no increase in the rate of reoperation associated with lumbar fusion or instrumentation.
There was no increased rate of reoperation associated with obesity, smoking, severity of stenosis, or number of levels of laminectomy.
The overall incidence of reoperations for spinal stenosis surgery was 13% at four years and reoperations were equally distributed between index and adjacent lumbar levels.
Acknowledgments
Funding Sources:
The authors would like to acknowledge funding from the following sources: The National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444) and the Office of Research on Women’s Health, the National Institutes of Health, and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention.
The Manuscript submitted does not contain information about medical device(s)/drug(s). National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444); Office of Research on Women’s Health, the National Institutes of Health; and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention funds were received to support this work. Relevant financial activities outside the submitted work: consultancy, board membership, royalties, and stock/stock options.
Contributor Information
Kris Radcliff, Rothman Institute, Thomas Jefferson University, 925 Chestnut Street, Philadelphia, PA 19107.
Patrick Curry, Thomas Jefferson University, Philadelphia, PA.
Alan Hilibrand, Rothman Institute, Thomas Jefferson University, 925 Chestnut Street, Philadelphia, PA 19107.
Chris Kepler, Rothman Institute, Thomas Jefferson University, 925 Chestnut Street, Philadelphia, PA 19107.
Jon Lurie, Dartmouth Medical Center, Dartmouth, NH.
Wenyan Zhao, Dartmouth Medical Center, Dartmouth, NH.
Todd Albert, Richard H. Rothman Professor and Chairman, Rothman Institute, Thomas Jefferson University, 925 Chestnut Street, Philadelphia, PA 19107.
James Weinstein, Dartmouth Medical Center, Dartmouth, NH.
References
- 1.Birkmeyer NJ, et al. Design of the Spine Patient outcomes Research Trial (SPORT) Spine (Phila Pa 1976) 2002;27(12):1361–72. doi: 10.1097/00007632-200206150-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weinstein JN, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 2008;358(8):794–810. doi: 10.1056/NEJMoa0707136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weinstein JN, et al. Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the Spine Patient Outcomes Research Trial. Spine (Phila Pa 1976) 2010;35(14):1329–38. doi: 10.1097/BRS.0b013e3181e0f04d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jansson K-Å, et al. Spinal stenosis re-operation rate in Sweden is 11% at 10 years—A national analysis of 9,664 operations. European Spine Journal. 2005;14(7):659–663. doi: 10.1007/s00586-004-0851-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghiselli G, et al. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am. 2004;86-A(7):1497–503. doi: 10.2106/00004623-200407000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Yamashita K, Ohzono K, Hiroshima K. Five-year outcomes of surgical treatment for degenerative lumbar spinal stenosis: a prospective observational study of symptom severity at standard intervals after surgery. Spine (Phila Pa 1976) 2006;31(13):1484–90. doi: 10.1097/01.brs.0000219940.26390.26. [DOI] [PubMed] [Google Scholar]
- 7.Yasar B, et al. Functional and clinical evaluation for the surgical treatment of degenerative stenosis of the lumbar spinal canal. J Neurosurg Spine. 2009;11(3):347–52. doi: 10.3171/2009.3.SPINE08692. [DOI] [PubMed] [Google Scholar]
- 8.Rihn J. Does Obesity Affect Outcomes in the Lumbar Spine Patient? A subgroup analysis of SPORT. North American Spine Society Annual Meeting; 2010; Orlando, Florida. [Google Scholar]
- 9.Radcliff KE, et al. Does the duration of symptoms in patients with spinal stenosis and degenerative spondylolisthesis affect outcomes?: analysis of the Spine Outcomes Research Trial. Spine. 2011;36(25):2197–210. doi: 10.1097/BRS.0b013e3182341edf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hilibrand AS, et al. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81(4):519–28. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Ekman P, et al. A prospective randomised study on the long-term effect of lumbar fusion on adjacent disc degeneration. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2009;18(8):1175–86. doi: 10.1007/s00586-009-0947-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Katz JN, et al. Predictors of surgical outcome in degenerative lumbar spinal stenosis. Spine (Phila Pa 1976) 1999;24(21):2229–33. doi: 10.1097/00007632-199911010-00010. [DOI] [PubMed] [Google Scholar]
- 13.Katz JN, et al. Lumbar laminectomy alone or with instrumented or noninstrumented arthrodesis in degenerative lumbar spinal stenosis. Patient selection, costs, and surgical outcomes. Spine (Phila Pa 1976) 1997;22(10):1123–31. doi: 10.1097/00007632-199705150-00012. [DOI] [PubMed] [Google Scholar]
- 14.Kornblum MB, et al. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudarthrosis. Spine. 2004;29(7):726–33. doi: 10.1097/01.brs.0000119398.22620.92. discussion 733–4. [DOI] [PubMed] [Google Scholar]
- 15.North RB, et al. Failed back surgery syndrome: 5-year follow-up in 102 patients undergoing repeated operation. Neurosurgery. 1991;28(5):685–90. discussion 690–1. [PubMed] [Google Scholar]