Abstract
Objectives
To compare classification of pre-pregnancy body mass index (BMI) using self-reported pre-pregnancy weight versus weight measured at the first prenatal visit.
Methods
Retrospective cohort of 307 women receiving prenatal care at the faculty and resident obstetric clinics at a Massachusetts tertiary-care center. Eligible women initiated prenatal care prior to 14 weeks gestation and delivered singleton infants between April 2007 and March 2008.
Results
On average, self-reported weight was 4 pounds lighter than measured weight at the first prenatal visit (SD: 7.2 pounds; range: 19 pounds lighter to 35 pounds heavier). Using self-reported pre-pregnancy weight to calculate pre-pregnancy BMI, 4.2% of women were underweight, 48.9% were normal weight, 25.4% were overweight, and 21.5% were obese. Using weight measured at first prenatal visit, these were 3.6%, 45.3%, 26.4%, and 24.8%, respectively. Classification of pre-pregnancy BMI was concordant for 87% of women (weighted kappa = 0.86; 95% CI: 0.81 – 0.90). Women gained an average of 32.1 pounds (SD: 18.0 pounds) during pregnancy. Of the 13% of the sample with discrepant BMI classification, 74% gained within the same adherence category when comparing weight gain to Institute of Medicine recommendations.
Conclusions
For the vast majority of women, self-reported pre-pregnancy weight and measured weight at first prenatal visit resulted in identical classification of pre-pregnancy BMI. In absence of measured pre-pregnancy weight, we recommend that providers calculate both values and discuss discrepancies with their pregnant patients, as significant weight loss or gain during the first trimester may indicate a need for additional oversight with potential intervention.
Keywords: Gestational weight gain, pre-pregnancy BMI, self-reported weight, prenatal care
Introduction
Numerous studies have identified significant associations between excessive and inadequate gestational weight gain (GWG) and adverse maternal and offspring health outcomes. Women who gain excessively are at increased risk for pre-eclampsia, cesarean delivery, gestational diabetes, and post-partum weight retention[1–6], while their neonates are at increased risk for low 5-minute APGAR scores, seizures, large for gestational age, and childhood obesity[7–9]. Inadequate gain is associated with an increased risk of small for gestational age neonates[4, 7, 10], and preterm birth[11]. An estimated 40–60% of women experience weight gain in pregnancy in excess of Institute of Medicine (IOM) recommendations and 15–20% gain less than recommended[7, 12, 13].
The IOM’s 2009 gestational weight gain recommendations are based on maternal pre-pregnancy body mass index (BMI)[14]. However, fifty percent of pregnancies in the U.S. are unplanned [15] and even women with planned pregnancies do not necessarily seek medical care ahead of time for preconceptional counseling. Thus, pre-pregnancy weight is often unavailable in a patient’s medical record[13, 16]. As a result, self-reported pre-pregnancy weight or measured weight at first prenatal visit, respectively, are often substituted for measured pre-pregnancy weight in calculating pre-pregnancy BMI to guide counseling on gestational weight gain[16]. The purpose of this study is to compare classification of pre-pregnancy BMI using self-reported pre-pregnancy weight versus weight measured at the first prenatal visit.
Patients and Methods
We conducted a secondary analysis of a retrospective cohort established to examine documentation of gestational weight gain counseling [13]. Briefly, eligibility included singleton gestation, initiation of prenatal care before 14 weeks gestation at the obstetric clinics at UMass Memorial Health Care (UMMHC), and delivery at UMMHC in April 2007 through March 2008. This cohort included 239 eligible women receiving prenatal care at the resident obstetric clinic and 238 randomly-selected eligible women receiving prenatal care at the faculty obstetric clinic; this sampling from the two obstetric clinics was based on the objectives of the parent study and the previously-observed differences in sociodemographic characteristics of the patient populations [13]. A more detailed description of selection methods and a flow diagram have been published[13]. Study data were abstracted from women’s American College of Obstetrics and Gynecology (ACOG) prenatal records and electronic labor and delivery records. The study was approved by the University of Massachusetts Medical School’s Institutional Review Board.
Pre-pregnancy weight self-reported at the first prenatal visit and weight measured at this first prenatal visit, occurring in the first trimester, were abstracted from the ACOG antenatal record. Body mass index (BMI; kg/m2) was calculated from height and each of these weights and categorized as underweight (BMI < 18.5 kg/m2), normal weight (18.5 kg/m2 ≤ BMI < 25.0 kg/m2), overweight (25.0 kg/m2 ≤ BMI < 30.0 kg/m2), or obese (30.0 kg/m2 ≤ BMI)[14].
GWG was ascertained by, as available, self-reported weight gain at time of delivery admission or difference between documented weight at last prenatal visit and pre-pregnancy weight. After excluding 34 women missing GWG, we calculated whether GWG was within the 2009 IOM recommendations for pre-pregnancy BMI calculated using self-reported pre-pregnancy weight and weight measured at the first prenatal visit; GWG was categorized as inadequate, appropriate, or excessive [14]. Minimum and maximum appropriate gain at each week of gestational age was determined using recommended gain by end of first trimester and rates of gain during the second and third trimesters, assuming the following ranges of gain by week 40: 25–35 pounds for normal weight, 15–25 pounds for overweight, and 11–20 pounds for obese women[14]. While the 1990 IOM recommendations[17] were contemporary to the pregnancies examined in this study, we compare women’s weight gain to the updated 2009 recommendations[14] to estimate future population burden.
Participant characteristics including age, gestational age at first prenatal visit, race/ethnicity, marital status, primary language, gravidity, and education were abstracted from the ACOG antenatal record. One woman who was separated and four who were divorced were grouped with women whose marital status was single (n=177).
We compared characteristics of women included and excluded in the analytic sample using chi-squared tests for categorical variables and t-tests for continuous variables. We calculated a weighted kappa to measure agreement between pre-pregnancy BMI categories calculated using self-reported pre-pregnancy weight versus weight measured at the first prenatal visit. Statistical significance was set at p < 0.05 for all comparisons. All analyses were performed using SAS (version 9.2, SAS Institute Inc., Cary, NC) statistical analysis software.
Results
Of the 477 women included in the retrospective cohort, 170 (36%) were excluded from the analytic sample because self-reported pre-pregnancy weight (n=133) or height (n=59) was not available in their prenatal care records. A higher proportion of women receiving prenatal care in the faculty obstetric clinic were excluded compared to patients from the resident obstetric clinic (47% versus 24%; p<0.0001). Women excluded due to missing self-reported pre-pregnancy weight and/or height (n=170) were, on average, 2.7 years older (p<0.0001), more likely to be non-Hispanic white or Asian but less likely to be Hispanic/Latina (p=0.0173), more likely to be married (p<0.0001), and more likely to have a college education or educational attainment not recorded in their charts (p<0.0001). These differences correspond with the previously-observed differences in sociodemographic characteristics and documentation practice patterns in these clinics[13].
On average, women in the analytic sample (N=307) were aged 26.8 ± 6.2 years (Table 1). Approximately half the sample was non-Hispanic white (52.0%), 12.6% were non-Hispanic black, and 24.5% Hispanic. Sixty seven percent were multi-gravid. Eighty-one percent spoke English as their primary language, 52.2% were married, and 56.2% had less than a high school education. Mean gestational age at first prenatal visit was 9.7 ± 2.1 weeks.
Table 1.
Characteristics of the sample*, M±SD or N (%)
| Age (y) | 26.8±6.2 |
| Gestational age at first prenatal visit (wk) | 9.7±2.1 |
| Nulligravid | 100 (32.6) |
| Race/ethnicity | |
| Non-Hispanic White | 140 (52.0) |
| Non-Hispanic Black | 34 (12.6) |
| Hispanic | 66 (24.5) |
| Asian | 13 (4.8) |
| Other race/ethnicity | 16 (6.0) |
| Married | 154 (52.2) |
| Primary language is English | 240 (80.8) |
| Education | |
| High school diploma or less | 146 (56.2) |
| Some college | 39 (15.0) |
| 4 years of college or more | 75 (28.8) |
Data missing for race/ethnicity (n=38), marital status (n=12), primary language (n=10), and education (n=47).
Mean self-reported pre-pregnancy weight was 152.6 ± 40.9 pounds and mean measured weight at first prenatal visit was 156.6 ± 41.7 pounds. BMI calculated from self-reported pre-pregnancy weight was 26.0 ± 6.2 kg/m2 and mean BMI calculated from first prenatal visit was 26.7 ± 6.3 kg/m2. On average, self-reported weight was 4 pounds lighter than measured weight at the first prenatal visit (SD: 7.2 pounds; range: 19 pounds lighter to 35 pounds heavier). For 15.6% of women, self-reported weight was 10+ pounds lighter than measured prenatal weight; self-reported pre-pregnancy weight was 5–10 pounds lighter in 26.4%, 2–5 pounds lighter in 16.6%, ±2 pounds in 25.1%, 2–5 pounds heavier in 9.8%, 5–10 pounds heavier in 4.6%, and 10+ pounds heavier in 2.0%. Half (51.5%) of women had self-reported pre-pregnancy weights within 5 pounds of measured weights at first prenatal visit.
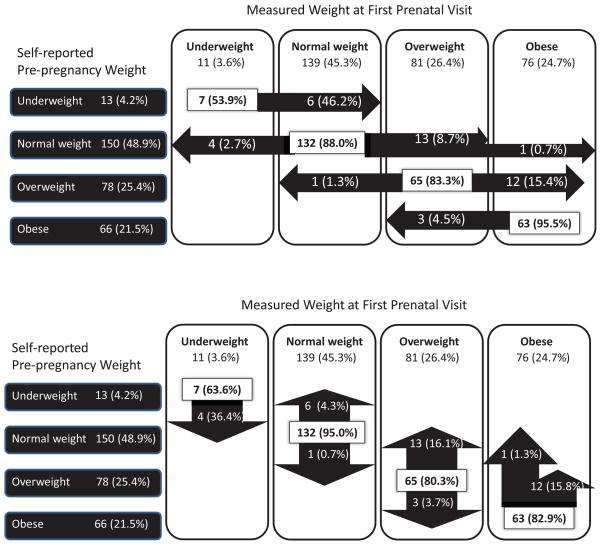
When pre-pregnancy BMI was calculated from self-reported pre-pregnancy weight, 4.2% were underweight, 48.9% were normal weight, 25.4% were overweight, and 21.5% were obese (Figure 1). When calculated from measured weight at first prenatal visit, percentages of underweight, normal weight, overweight, and obese were 3.6%, 45.3%, 26.4%, and 24.8%, respectively. Classification of pre-pregnancy BMI was concordant for 87% of women and discordant for 13% of women (weighted kappa = 0.86; 95% CI: 0.81 – 0.90). Three percent (n=8) women were categorized into a lower BMI category using weight measured at first prenatal visit compared to self-reported pre-pregnancy weight, and 10% (n=32) were classified into a higher BMI category. Discrepant categorizations were into adjacent weight categories except for one woman who was normal weight per self-reported weight and obese per measured weight at first prenatal visit.
Figure 1.
Classification of pre-pregnancy BMI* when calculated using self-reported pre- pregnancy weight versus weight measured at the first prenatal visit
*Underweight (BMI < 18.5 kg/m2), normal weight (18.5 kg/m2 ≤ BMI < 25.0 kg/m2), overweight (25.0 kg/m2 ≤ BMI < 30.0 kg/m2), or obese (30.0 kg/m2 ≤ BMI)[14]. The top panel shows the percentages of women in each category of pre-pregnancy BMI calculated with self-reported pre-pregnancy weight that would be categorized differently based on weight measured at first prenatal visit. The bottom panel shows the proportion of women in each category of pre-pregnancy BMI calculated with weight measured at first prenatal visit that would be categorized differently based on self-reported pre-pregnancy weight.
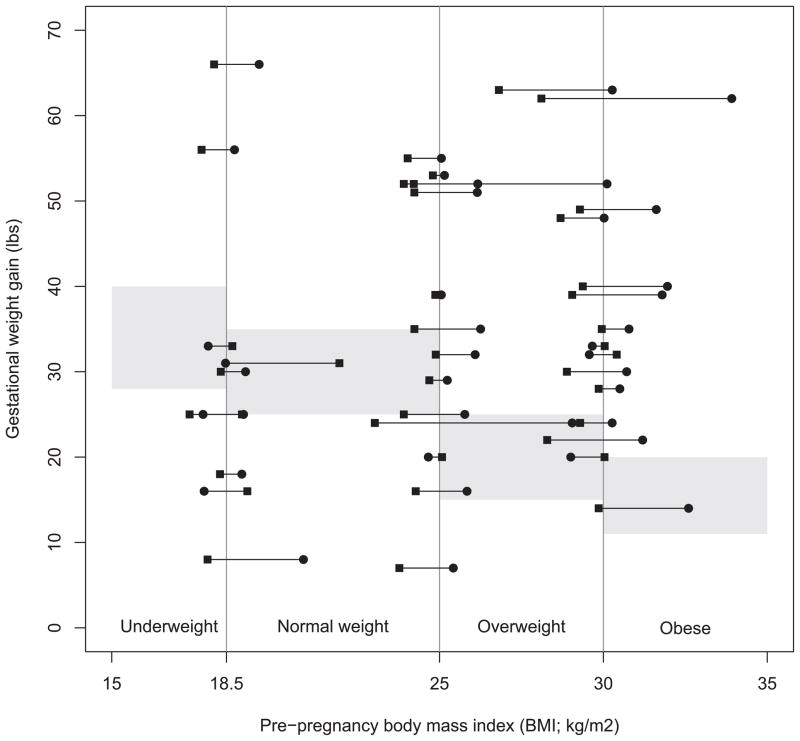
Women gained an average of 32.1 pounds during pregnancy (SD: 18.0 pounds; range: 93-pound loss to 85-pound gain). When compared to IOM recommendations according to pre-pregnancy BMI calculated from self-reported pre-pregnancy weight, 16.8% of women gained less than recommended, 28.6% gained within the recommended range, and 54.6% experienced excessive gain. When BMI-specific weight gain adherence was calculated based on weight measured at first prenatal visit, these numbers were 16.9%, 27.1%, and 56.0%, respectively. Including both the 87% of women with concordant BMI classification and the 13% with discrepant BMI classification (n=273/309 with available GWG), whether gestational weight gain was below, within, or above the range recommended by the IOM was the same for BMI calculated using either self-reported pre-pregnancy weight or weight measured at first prenatal visit. Of the 13% of the sample with discrepant BMI classification (n=39 of 40 whom had available GWG), 74% gained within the same adherence category when comparing weight gain to Institute of Medicine recommendations (Figure 2). Two-thirds (n=4/6) of women who gained less than recommended per their BMI calculated from self-reported pre-pregnancy weight gained less than recommended per their weight measured at first prenatal visit; the remaining two gained within the recommended range. Of the 12 women with adherent gain per their self-reported pre-pregnancy weight, 2 (17%) had inadequate gain per their weight measured at first prenatal visit, 5 (41%) had adherent gain, and 5 (41%) had excessive gain. All but one (n=20/21; 95%) women who overgained according to BMI calculated using self-reported pre-pregnancy weight also overgained if their pre-pregnancy BMI was calculated using weight measured at first prenatal visit.
Figure 2.
Gestational weight gain compared to Institute of Medicine 2009 recommendations according to pre-pregnancy body mass index calculated with self-reported pre-pregnancy weight versus weight measured at first prenatal visit, for the 13% of women with discrepant body mass index category using these two weights (n=39)
Squares are pre-pregnancy BMI calculated with self-reported pre-pregnancy weight and circles are pre-pregnancy BMI calculated with weight measured at first prenatal visit. The shaded (grey) regions are gestational weight gain within pre-pregnancy BMI-specific recommendations[14].
Discussion
The IOM’s most recent guidelines recommend the use of pre-pregnancy BMI for the basis of gestational weight gain counseling. A measured pre-pregnancy weight and height is preferable for calculating pre-pregnancy BMI. However, half of pregnancies in the United States are unplanned[15], and many more are not associated with a medical visit from which measured weight can be obtained. Thus measured pre-pregnancy weight is frequently unavailable in the prenatal care setting[13, 16].
Overall, inaccurate estimates of pre-pregnancy weight could result in erroneous counseling. For example, women classified as obese prior to pregnancy are recommended to gain 11–20 pounds per the 2009 IOM guidelines [14]. If a woman comes to the office 10 weeks into her pregnancy and reports an inaccurate pre-pregnancy weight that yields a BMI in the overweight category, she will be counseled to gain 15–25 pounds. This is a different range than would have been recommended if her actual pre-pregnancy weight were used to guide the recommendation. For 87% of women in the current study, classification of pre-pregnancy BMI was concordant when calculated with self-reported pre-pregnancy versus weight measured at first prenatal visit. Our results agree with another study in which self-reported pre-pregnancy weight was on average 4.4 pounds higher than measured weight at the end of the first trimester and 85% of women were categorized the same into weight categories[18]. The current study adds to this literature by providing contemporary estimates by using a recent sample (2007–2008 versus 1991–1993[18]) and classifying pre-pregnancy weight status per the updated 2009 IOM gestational weight gain recommendations [14].
Several factors may contribute to the significant difference found in this study between self reported pre-pregnancy weight and measured weight at first prenatal visit. Underreporting of weight is common among non-pregnant adults. On average, women of childbearing age underreport their weight by an average of 1.5 kg (or 3.3 pounds)[19]. Women during early pregnancy may underreport their weight, on average, by a similar amount[20]. A recent study found that self-reported and clinically measured pre-pregnancy weights were highly correlated (r = 0.99) and that the mean underreporting of weight by approximately two pounds did not differ by race/ethnicity, gestational age, or pre-pregnancy weight[9]. Women may round their reported pre-pregnancy weights; we found that 31% of self-reported weights ended in zero and 26% in five, more than the 10% expected (data not shown), potentially speaking to digit preference in self-report of pre-pregnancy weight.
Small inconsistencies in measurement have the potential to affect accuracy of weight measured at first prenatal visit. The scale used, clothes a subject is wearing, time of day, voiding status, and sodium intake are all variables that can skew weight data[21]. However, if the differences between pre-pregnancy weight and measured weight at first prenatal visit were attributable to measurement inconsistencies alone, it is likely that the differences would be small. For 42% of our sample, weight measured at first prenatal visit was more than 5 pounds heavier than self-reported pre-pregnancy weight. This indicates that small weight differences due to clothing or voiding status are unlikely to explain the observed discrepancies between self-reported pre-pregnancy weight and weight measured at the first prenatal visit.
Alternatively, first trimester weight gain or weight loss could contribute to observed differences between self-reported pre-pregnancy weight and weight measured at first prenatal visit. The 2009 IOM recommendations assume a 1.1–4.4 pound weight gain for all women through 13 weeks gestation[14]. However, in one study, while average first-trimester gain was approximately 2 kg (roughly 5 pounds), the range of early-pregnancy gain observed ranged from a loss of 3.1 kg (6.8 pounds) to a gain of 7.2 kg (15.9 pounds)[22]. Significant weight loss in the first trimester may be attributable to decreased food consumption [23] such as due to nausea or vomiting, or from hyperemesis gravidarum. Early-pregnancy weight gain may be attributable to decreased physical activity or increased energy intake compared to pre-pregnancy[23]. Weight gain may also be more common among women who quit smoking when learning of their pregnancy, as weight gain often accompanies smoking cessation[24].
This work has implications for prenatal counseling. Half of women were overweight or obese when BMI was calculated from either self-reported pre-pregnancy weight, or weight at first prenatal visit, and excessive gain is common. Therefore, it is reasonable to gear overall recommendations to those at risk of gaining more than recommended, and to use weight at first prenatal visit as a default value from which to calculate BMI and make GWG recommendations. However, it is equally important to apply clinical judgment and to override this default when clinically appropriate. For example, it may be appropriate to recommend GWG of 28–40 pounds for women who are underweight either by self-reported pre-pregnancy weight or weight measured at their first prenatal visit. Adherence to IOM recommendations in consecutive pregnancies is concordant; women who undergain in one pregnancy are at increased risk of inadequate gain in subsequent pregnancies, and excessive gain puts women at higher risk for subsequent excessive gain[25]. Therefore, if a woman was an inadequate gainer in a previous pregnancy, it may make sense to calculate her BMI from a lower self-reported pre-pregnancy weight, than a higher measured weight at first prenatal visit. Conversely, if a woman is overweight and nulliparous, she is at risk of gaining excessively[26], so for women whose self-reported pre-pregnancy weights and measured weights at first prenatal visit span the normal weight and overweight ranges, it may be prudent to advise them based on recommendations for overweight women. If self-reported pre-pregnancy weight and weight measured at first prenatal visit differ by more than five pounds, providers may want to inquire about weight gain or loss during the first trimester, and factors attributing to this weight change, as either significant weight gain or loss during early pregnancy may indicate a need for additional oversight with potential intervention.
The importance of use of self-report pre-pregnancy weight versus measured first prenatal weight, from first trimester visits, for calculation of BMI is predicated on assumptions that BMIs are being calculated and that counseling is based on these calculations, which may not always be the case[13]. Studies have found that providers often offer incorrect or no gestational weight gain counseling to their patients. In one study, 27% of women reported receiving no advice regarding gestational weight gain, and among those who received advice, 36% were advised to gain more or less than recommended[27]. In another study, 29% of women report receiving provider advice about gestational weight gain, with only 12% advised to gain in accordance with the 2009 IOM guidelines[28]. Other authors report comparable findings, [29, 30] indicating a possible need to help prenatal care providers routinely provide advice regarding gestational weight gain, or to make this advice more memorable for pregnant women. Given the high concordance of BMI calculation regardless of weight used, counseling of all women using either method has the potential to significantly positively impact the number of women offered accurate counseling.
Our study has additional strengths and limitations. Thirty-six percent of participants were excluded from the analytic sample due to unavailability of self-reported pre-pregnancy weight or height, likely reflecting low rates of counseling about gestational weight gain[13]. Our sample came from obstetric clinics in a tertiary care setting and did not include subjects from private obstetric practice or family medicine settings. However, the diversity of our study population offers greater likelihood that our findings are generalizable to obstetric populations at other academic sites across the U.S.. As is often in the case in the prenatal care setting[13, 16], measured pre-pregnancy weight was not available; thus, we compared classification of pre-pregnancy weight status using self-reported pre-pregnancy weight versus weight measured at first prenatal visit. Future research could illuminate determinants of discrepancies between these two approximations of pre-pregnancy weight by comparing them to objectively measured weight obtained prior to conception. By including only women who initiated prenatal care before 14 weeks gestation, we insured that weight measured at first prenatal visit was during the first trimester, during which minimal weight gain is recommended. However, weight change during the first weeks of pregnancy can vary significantly[22], and we did not collect information about factors that might affect first-trimester weight gain or loss, such as significant changes in food consumption or physical activity from pre-pregnancy or pregnancy symptoms affecting diet or activity such as nausea, vomiting, or change in appetite.
For the vast majority of women, self-reported pre-pregnancy weight and measured weight at first prenatal visit resulted in identical classification of pre-pregnancy BMI status. This is fortuitous given the number of pregnancies that are unplanned and/or not preceded by medical care or preconception counseling. Given the link between gestational weight gain outside of the ranges recommended by the IOM and maternal and fetal outcomes[1–9, 11], this study serves to highlight the importance of calculating BMI in pregnancy and providing accurate counseling based on these calculations.
Acknowledgments
Partial salary support for Dr. Moore Simas is provided by the National Institutes of Health contract HHSN267200700024C. Partial salary support for Dr. Waring is provided by the National Institutes of Health grant 1U01HL105268.
References
- 1.Kiel DW, et al. Gestational weight gain and pregnancy outcomes in obese women: how much is enough? Obstet Gynecol. 2007;110(4):752–8. doi: 10.1097/01.AOG.0000278819.17190.87. [DOI] [PubMed] [Google Scholar]
- 2.Gunderson EP, Abrams B, Selvin S. The relative importance of gestational gain and maternal characteristics associated with the risk of becoming overweight after pregnancy. Int J Obes Relat Metab Disord. 2000;24(12):1660–8. doi: 10.1038/sj.ijo.0801456. [DOI] [PubMed] [Google Scholar]
- 3.Siega-Riz AM, et al. A systematic review of outcomes of maternal weight gain according to the Institute of Medicine recommendations: birthweight, fetal growth, and postpartum weight retention. Am J Obstet Gynecol. 2009;201(4):339 e1–14. doi: 10.1016/j.ajog.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 4.DeVader SR, et al. Evaluation of gestational weight gain guidelines for women with normal prepregnancy body mass index. Obstet Gynecol. 2007;110(4):745–51. doi: 10.1097/01.AOG.0000284451.37882.85. [DOI] [PubMed] [Google Scholar]
- 5.Kabiru W, Raynor BD. Obstetric outcomes associated with increase in BMI category during pregnancy. Am J Obstet Gynecol. 2004;191(3):928–32. doi: 10.1016/j.ajog.2004.06.051. [DOI] [PubMed] [Google Scholar]
- 6.Stotland NE, Hopkins LM, Caughey AB. Gestational weight gain, macrosomia, and risk of cesarean birth in nondiabetic nulliparas. Obstet Gynecol. 2004;104(4):671–7. doi: 10.1097/01.AOG.0000139515.97799.f6. [DOI] [PubMed] [Google Scholar]
- 7.Stotland NE, et al. Gestational weight gain and adverse neonatal outcome among term infants. Obstet Gynecol. 2006;108(3 Pt 1):635–43. doi: 10.1097/01.AOG.0000228960.16678.bd. [DOI] [PubMed] [Google Scholar]
- 8.Wrotniak BH, et al. Gestational weight gain and risk of overweight in the offspring at age 7 y in a multicenter, multiethnic cohort study. Am J Clin Nutr. 2008;87(6):1818–24. doi: 10.1093/ajcn/87.6.1818. [DOI] [PubMed] [Google Scholar]
- 9.Oken E, et al. Gestational weight gain and child adiposity at age 3 years. Am J Obstet Gynecol. 2007;196(4):322 e1–8. doi: 10.1016/j.ajog.2006.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vesco KK, et al. Newborn size among obese women with weight gain outside the 2009 Institute of Medicine recommendation. Obstet Gynecol. 2011;117(4):812–8. doi: 10.1097/AOG.0b013e3182113ae4. [DOI] [PubMed] [Google Scholar]
- 11.Nohr EA, et al. Obesity, gestational weight gain and preterm birth: a study within the Danish National Birth Cohort. Paediatr Perinat Epidemiol. 2007;21(1):5–14. doi: 10.1111/j.1365-3016.2007.00762.x. [DOI] [PubMed] [Google Scholar]
- 12.Gould Rothberg BE, et al. Gestational weight gain and subsequent postpartum weight loss among young, low-income, ethnic minority women. Am J Obstet Gynecol. 2011;204(1):52 e1–11. doi: 10.1016/j.ajog.2010.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moore Simas TA, et al. Efforts needed to provide Institute of Medicine-recommended guidelines for gestational weight gain. Obstet Gynecol. 2010;115(4):777–83. doi: 10.1097/AOG.0b013e3181d56e12. [DOI] [PubMed] [Google Scholar]
- 14.IOM. Weight gain during pregnancy: reexamining the guidelines. National Academy Press; Washington DC: 2009. [PubMed] [Google Scholar]
- 15.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38(2):90–6. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 16.Harris HE, Ellison GT. Practical approaches for estimating prepregnant body weight. J Nurse Midwifery. 1998;43(2):97–101. doi: 10.1016/s0091-2182(97)00159-6. [DOI] [PubMed] [Google Scholar]
- 17.IOM. Nutrition during pregnancy: report of the committee on nutritional status during pregnancy and lactation, food and nutrition board. National Academy Press; Washington DC: 1990. [Google Scholar]
- 18.Lederman SA, Paxton A. Maternal reporting of prepregnancy weight and birth outcome: consistency and completeness compared with the clinical record. Matern Child Health J. 1998;2(2):123–6. doi: 10.1023/a:1022996924094. [DOI] [PubMed] [Google Scholar]
- 19.Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Diet Assoc. 2001;101(1):28–34. doi: 10.1016/S0002-8223(01)00008-6. quiz 35–6. [DOI] [PubMed] [Google Scholar]
- 20.Fattah C, et al. Body Mass Index (BMI) in women booking for antenatal care: comparison between selfreported and digital measurements. Eur J Obstet Gynecol Reprod Biol. 2009;144(1):32–4. doi: 10.1016/j.ejogrb.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 21.Harris HE, et al. How accurate are antenatal weight measurements? A survey of hospital and community clinics in a South Thames Region NHS Trust. Paediatr Perinat Epidemiol. 1998;12(2):163–75. doi: 10.1046/j.1365-3016.1998.00100.x. [DOI] [PubMed] [Google Scholar]
- 22.Carmichael S, Abrams B, Selvin S. The pattern of maternal weight gain in women with good pregnancy outcomes. Am J Public Health. 1997;87(12):1984–8. doi: 10.2105/ajph.87.12.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Olson CM, Strawderman MS. Modifiable behavioral factors in a biopsychosocial model predict inadequate and excessive gestational weight gain. J Am Diet Assoc. 2003;103(1):48–54. doi: 10.1053/jada.2003.50001. [DOI] [PubMed] [Google Scholar]
- 24.Klesges RC, et al. The prospective relationships between smoking and weight in a young, biracial cohort: the Coronary Artery Risk Development in Young Adults Study. J Consult Clin Psychol. 1998;66(6):987–93. [PubMed] [Google Scholar]
- 25.Waring ME, Moore Simas TA, Liao X. Gestational weight gain within recommended ranges in consecutive pregnancies: A retrospective cohort study. Midwifery. 2012 Oct 23; doi: 10.1016/j.midw.2012.04.014. doi:pii:S0266-6138(12)00068-X10.1016.j.midw.2012.04.014. [epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chu SY, et al. Gestational weight gain by body mass index among US women delivering live births, 2004–2005: fueling future obesity. Am J Obstet Gynecol. 2009;200(3):271 e1–7. doi: 10.1016/j.ajog.2008.09.879. [DOI] [PubMed] [Google Scholar]
- 27.Cogswell ME, et al. Medically advised, mother’s personal target, and actual weight gain during pregnancy. Obstet Gynecol. 1999;94(4):616–22. doi: 10.1016/s0029-7844(99)00375-0. [DOI] [PubMed] [Google Scholar]
- 28.McDonald SD, et al. Despite 2009 guidelines, few women report being counseled correctly about weight gain during pregnancy. Am J Obstet Gynecol. 2011;205(4):333 e1–6. doi: 10.1016/j.ajog.2011.05.039. [DOI] [PubMed] [Google Scholar]
- 29.Phelan S, et al. Practitioner advice and gestational weight gain. J Womens Health (Larchmt) 2011;20(4):585–91. doi: 10.1089/jwh.2010.2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stotland NE, et al. Body mass index, provider advice, and target gestational weight gain. Obstet Gynecol. 2005;105(3):633–8. doi: 10.1097/01.AOG.0000152349.84025.35. [DOI] [PubMed] [Google Scholar]