Abstract
Objective
To examine the long term impact of a communication skills intervention on physicians' communication self-efficacy and the relationship between reported self-efficacy and actual performance.
Methods
62 hospital physicians were exposed to a 20-hour communication skills course according to the Four Habits patient-centered approach in a crossover randomized trial. Encounters with real patients before and after the intervention (mean 154 days) were videotaped, for evaluation of performance using the Four Habits Coding Scheme. Participants completed a questionnaire about communication skills self-efficacy before the course, immediately after the course, and at 3 years follow-up. Change in self-efficacy and the correlations between performance and self-efficacy at baseline and follow-up were assessed.
Results
Communication skills self-efficacy was not correlated to performance at baseline (r=-0.16; p=0.22). The association changed significantly (p=0.01) and was positive at follow-up (r=0.336, p=0.042). The self-efficacy increased significantly (effect size d=0.27). High performance after the course and low self-efficacy before the course were associated with larger increase in communication skills self-efficacy.
Conclusion
A communication skills course led to improved communication skills self-efficacy more than three years later, and introduced a positive association between communication skills self-efficacy and performance not present at baseline.
Practice implications
Communication skills training enhances physicians' insight in own performance.
Keywords: Communication skills training, self-efficacy, performance, longitudinal study
1. Introduction
Patient-centered communication is an integral aspect of medical care [1] and has been promoted for decades [2,3]. However, changing the standard of communication has been slow and difficult [4-8] and the long term impact of communication skills training on physician's assessment of their own communication skills is unknown.
Improving patient-centered care can be difficult because physicians receive very little feedback about their performance. In general, patient satisfaction is highly positively skewed [9,10], and physicians receive few criticisms of their communication behaviour from their patients. This may lead to high confidence in their communication skills [11]. Moreover, today's physicians are in general polite and friendly, masking deficiencies in patient-centered communication [12].
High communication self-efficacy means having confidence in ones' own communication skills. However, this confidence may or may not be appropriate when compared to actual communication performance. Two reviews have concluded that professionals' ability to assess their clinical skills is imprecise, and more so if their skills are poor [13,14]. This has also been shown for physicians' skills in general [15] and communication skills in particular [15,16]. Medical students' self-assessment accuracy is particularly low for communication skills [17-19]. Self-assessment is strongly linked to self-attributions [13], and hard to disentangle from self-efficacy [20] – probably even more so in the absence of feedback. Lack of insight into deficits in one's own performance could potentially explain lack of motivation for improvement, which is troublesome as self-directed learning has been considered a cornerstone of professional development in medicine for several years [21-23]. However, attending a course may be an eye-opener. Physicians whose self-efficacy was reduced after a communication skills course, developed a stronger belief in the effect of such a course on improvement of their skills [24].
Given that physicians receive very little feedback about their communication performance, we hypothesize that communication skills training will not only increase self-efficacy, but also accuracy of the self-efficacy when compared with objectively measured performance. The aims of this study were to explore whether the association between physician communication skills self-efficacy and actual performance changed following a communication skills course, and which variables could predict a change in self-efficacy from baseline to follow-up. To our knowledge, this is the first study to explore long term consequences to self-efficacy and accuracy of that self-assessment after a long follow-up period.
2. Methods
2.1 Design
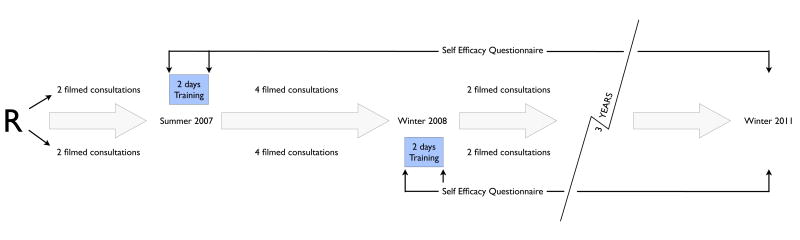
This is an observational study following a crossover randomized controlled trial in 2007-08 [25] with follow-up data collected in 2011. Participating physicians were assessed on videotapes before and up to 12 months (mean 154 days, standard deviation 87 days) after a communication skills course. Data on self-efficacy was collected when the course started, on leaving the course and by a mail survey at follow-up in 2011. Eight encounters were videotaped per physician, of these two before the first course (constituting the baseline assessment). Due to the crossover design, half of the physicians have two observed encounters before the intervention and six after, and the other half vice versa (Figure 1). Because of this, performance scores for physicians after the intervention were based on averages of 2 or 6 videotapes. The course used the Four Habits approach developed in Kaiser Permanente, California, and piloted in Norway [26,27]. The objective was to teach the physicians about important patient-centered communication skills, and inspire them to train systematically after the course. Over two ten-hour days participants were exposed to a half-and-half mix of role-plays in small groups and plenaries with theory and debriefing. In the role-plays, physicians played patients as well as themselves. Physicians were given feedback during role-plays within the course, but no feedback on their behaviour in the videotaped encounters.
Figure 1.
Study design. R marks randomization to two groups.
2.2 Participants
Eligible participants included all physicians less than 60 years of age working in the non-psychiatric clinical departments of a teaching hospital in the capital area of Norway. Physicians were selected for invitation to participate by a random drawing stratified on department and position (fully licensed specialists (seniors)/specialists in training (juniors)). Seventy-one of 103 invited physicians (69%) agreed to participate, eventually 62 (60%) received the intervention. Participating physicians did not significantly differ from the original physician population in terms of gender, age, proportion of senior or junior physicians, or specialty [24]. A sufficient number of videotapes were collected for 56 of the 62 physicians after having received the intervention. Reasons for attrition were mainly maternity leaves (female physicians) or too few available patients (mainly in anaesthesiology) [25].
2.3 Measurements
Communication self-efficacy was measured by the question: “How certain are you that you can successfully perform the following tasks?” in which responses should be given on a scale from 1 (very uncertain) to 10 (very certain) with regard to the nine tasks listed in table 1. Self-efficacy score was the sum of responses across tasks. This measure was developed and validated in the United Kingdom [28] and translated for use in Norway [24]. It has been used in other clinical studies [29,30]. The follow-up survey also contained the question: “Did the course make lasting impact on your clinical practice?” with the answering options “yes”, “no”, and “uncertain”.
Table 1.
The skills included in the measure of self-efficacy. The question was: “How certain are you that you can successfully perform the following tasks?”
| Initiate a conversation with a patient regarding his/her worries |
| Conclude a consultation with a summary of the problems and a treatment plan |
| Assess symptoms of anxiety and depression |
| Communicate bad news to a patient |
| Confront in an appropriate manner a patient who denies his/her illness |
| Cope with a situation in which a patient or a relative expresses disagreement with you as a doctor |
| Encourage a patient to describe his/her feelings |
| Initiate a conversation with a patient regarding his/her worries |
| Conclude a consultation with a summary of the problems and a treatment plan |
The physicians' communication skills performance was evaluated using the Four Habits Coding Scheme (4HCS), developed by Krupat et al to systematically evaluate the quality of physician patient-centered communication [31]. The 4HCS was modeled after the Kaiser Permanente approach used in the communication skills training, and showed acceptable reliability and validity (compared with Roter Interaction Analysis System coding) in the original study [31]. The coding scheme consists of 23 items organized into four habits: investing in the beginning, eliciting of the patient's perspective, demonstrating empathy and investing in the end of the visit. The items are scored on a 5-point scale from 1 = not very effective to 5 = highly effective and the physician's score is a sum across the 23 items. Four experienced psychology students did the rating after three days of training, two of them led by the developer Edward Krupat. Interrater reliability (IRR) was acceptable with an intraclass correlation of >0.70 [32]. When more than one rater assessed a video, the rating given by the most experienced rater was used in the main dataset. Raters were blinded to all information about the physicians and the encounters, including whether the video was made before or after the intervention. The tapes were allocated randomly to the raters.
Patient evaluations were assessed using three different instruments. The Consumer Assessment of Healthcare Providers and Systems (CAHPS, www.cahps.gov); “Using any number from 0 to 10, where 0 is the worst physician possible and 10 is the best physician possible, what number would you use to rate this physician?” was used to measure global patient satisfaction. The Four Habits Patient Questionnaire (4HPQ) [27] and the Outpatient Experience Questionnaire's (OPEQ) [33] information and communication questions were used for specific patient evaluations of the physicians' communication abilities. The three measures were highly intercorrelated, and all were significantly correlated with the 4HCS [34].
2.4 Analysis
Scores on the individual items in the self-efficacy questionnaire were amalgamated to a sum score before the course, after the course and at follow-up. Four missing item values (out of 369, 1%) in the follow-up survey were imputed using the mean. Changes in self-efficacy were compared using paired t-tests.
The average performance and patient evaluation scores at baseline and after the course were calculated for each physician. For those physicians that was trained first and therefore had their post-intervention scores calculated as an average over six videotapes, we checked that there was no significant difference in performance between the first four and last two post-intervention scores (see figure 1). We calculated the associations between performance and patient evaluations at baseline and self-efficacy before the course using Pearson's r. Likewise, we calculated the association between performance after the course and self-efficacy at follow-up. When comparing these correlated, non-overlapping correlations, we used a Fisher's Z Pearson-Filon statistics developed for such comparisons [35]. We identified physician outliers and ran the analyses without these physicians to inspect whether the conclusions were affected.
We calculated the change in self-efficacy from baseline to follow-up for each physician, and used this as the dependent variable in two backward stepwise regression analyses. Due to the low number of cases, we explored the effects of a limited number of variables; age, gender, self-efficacy before the course, and performance (4HCS) at baseline or after the course.
The study was approved by the Regional Medical Ethics Review Board of South-East Norway.
3. Results
After two reminders, 41 (66%) responded to the follow-up survey (table 2). The characteristics of the responders were not significantly different from those of the non-responders. In particular, variables indicating performance as evaluated by experts or patients, or self-efficacy and motivation of the physicians were not significantly different between responders and non-responders. Of the 41 responders, 24 (59%) said the course had made lasting impact on their practice, 12 were uncertain, and five said they had not changed their practice. There were no significant differences between those who said practice had changed and those that were uncertain or said it had not on any of the independent variables listed in table 2 (data not shown).
Table 2.
Representativeness of responders to follow-up survey 36-42 months after a communication skills course. N (%) if not otherwise specified.
| All (N= 62) | Respondents (N=41) |
Non-respondents (N=21) |
p-value | |
|---|---|---|---|---|
| Gender | .43 | |||
| Females | 28 | 17 (42) | 11 (52) | |
| Males | 34 | 24 (59) | 10 (48) | |
| Age (mean, SD) | 62 | 41 (8.1) | 38 (9.3) | .18 |
| Position | .18 | |||
| Specialists in training | 30 | 17 (42) | 13 (62) | |
| Fully licensed specialists | 32 | 24 (59) | 8 (38) | |
| Type of specialty | .64 | |||
| Internal medicine | 23 | 13 (32) | 10 (47) | |
| Surgical disciplines | 17 | 11 (27) | 8 (29) | |
| Neurology | 8 | 6 (15) | 2 (10) | |
| Pediatrics | 7 | 5 (12) | 2 (10) | |
| Gynaecology | 7 | 6 (15) | 1 (5) | |
| Prior communication training | 1.00 | |||
| Yes | 17 | 11 (27) | 6 (29) | |
| No | 45 | 30 (73) | 15 (71) | |
| Met in group 3 months after course | .17 | |||
| Yes | 23 | 18 (44) | 5 (24) | |
| No | 39 | 23 (56) | 16 (76) | |
| Communication skills, performance (4HCS) (means, SD) | ||||
| Before course | 62 | 58.8 (9.8) | 61.8 (10.2) | .27 |
| After course | 56 | 62.9 (10.2) | 64.3 (11.6) | .63 |
| Communication skills, patient reports (means, SD) | ||||
| Specific (4HPQ) before course | 62 | 53.7 (4.9) | 54.2 (3.2) | .70 |
| Specific (4HPQ) after | 56 | 55.5 (3.4) | 54.8 (2.9) | .44 |
| General (OPEQ) before | 62 | 25.4 (2.5) | 25.9 (2.3) | .46 |
| General (OPEQ) after | 56 | 25.7 (2.7) | 24.9 (4.2) | .41 |
| Patient global satisfaction (mean, SD) | ||||
| Before (CAHPS) | 62 | 8.6 (1.2) | 8.8 (.77) | .47 |
| After (CAHPS) | 56 | 9.0 (.62) | 8.9 (.87) | .56 |
| Doctor self efficacy (means, SD) | ||||
| Before course | 58 | 57.2 (11.4) | 57.9 (7.4) | .81 |
| After course | 59 | 62.2 (10.7) | 61.8 (8.6) | .88 |
4HCS = Four Habits Coding Scheme, 4HPQ = Four Habits Patient Questionnaire, OPEQ = Outpatient Experiences Questionnaire, CAHPS = Consumer Assessment of Healthcare Providers and Services, SD = standard deviation
The self-efficacy before the course, after the course, and at follow-up were highly correlated (range 0.65 < r < 0.75, p < 0.001 for all paired comparisons). The self-efficacy of the physicians improved during the course, and did not change significantly during the 36-42 months after the course (table 3), leaving an overall effect size (Cohen's d) of 0.27 from baseline to follow-up.
Table 3.
Communication skills self-efficacy immediately before and after communication skills course, and at follow-up (36-42 months later). Means (SD) on a scale from 10 to 90.
| N | Before course | Immediately after course | Follow-up | p-value1 | |
|---|---|---|---|---|---|
| Male doctors | 31 | 56.45 (11.5) | 60.84 (11.8) | .002 | |
| 22 | 61.73 (13.1) | 57.73 (12.6) | .056 | ||
| 22 | 55.36 (12.6) | 58.77 (13.2) | .045 | ||
| Female doctors | 25 | 58.36 (8.4) | 63.84 (7.5) | .001 | |
| 17 | 62.82 (6.4) | 63.47 (11.0) | .802 | ||
| 15 | 60.00 (9.2) | 63.00 (11.7) | .344 | ||
| All | 56 | 57.30 (10.2) | 62.18 (10.1) | <.0005 | |
| (10.7) | (12.1) | ||||
| 37 | 57.24 (11.4) | 60.49 (12.6) | .042 |
Two-tailed paired sample t-tests.
The correlation between the physicians' self-efficacy before the course and performance was not significant at baseline (n=58; r= −0.162; p=0.224). Self-efficacy immediately after the course was not correlated to performance after training (data not shown). However the correlation between performance after training and self-efficacy 3 years later was significantly positive (n=37, r=0.336; p=0.042) (table 4). The difference between correlations was significant for the total group (p=0.011), and separately for female (p=0.027) and male physicians (p=0.047). The difference between correlations was also significant among those physicians who claimed not to have changed practice (p=0.024). We found no correlation between communication skills self-efficacy and patient reports (CAHPS, 4HPQ, OPEQ) at baseline or follow-up.
Table 4.
Correlations between doctor self-efficacy and performance based on video observations.
| Before course | After course –follow-up | P-value1 | |||
|---|---|---|---|---|---|
| N | Pearson's r (p-value) | N | Pearson's r (p-value) | ||
| All | 58 | -.162 (.224) | 37 | .336 (.042) | |
| All with all follow-up data | 33 | -.214 (.233) | 33 | .276 (.120) | .011 |
| Sex | |||||
| Males with all follow-up data | 22 | -.245 (.272) | 22 | .228 (.307) | .047 |
| Females with all follow-up data | 11 | -.233 (.491) | 11 | .576 (.064) | .027 |
| Change of practice | |||||
| Did change practice | 16 | .013 (.961) | 16 | .402 (.122) | .220 |
| Did not change practice | 17 | -.429 (.086) | 17 | .190 (.464) | .024 |
Two-tailed tests for correlated non-overlapping correlations. Comparison of correlation between performance and physician self-efficacy before course versus correlation between performance after course and physician self-efficacy at follow-up.
In the regression model, higher performance at baseline predicted an increase in self-efficacy from baseline to follow-up (table 5). Gender, age or self-efficacy at baseline did not predict change in self-efficacy in this model. When we added performance after the course to the model, performance at baseline was eliminated as these two variables were highly correlated and performance after the course was associated more strongly with change in self-efficacy. In this new model, baseline self-efficacy was also significant. Higher post-course performance and lower baseline self-efficacy predicted increased self-efficacy from baseline to follow-up (table 5).
Table 5.
Predictors of change in physician communication skills self-efficacy from baseline to follow-up. N=33.
| β (not adjusted) | p | R2 | β (adjusted) | p | R2 | |
|---|---|---|---|---|---|---|
| 1st model | ||||||
| Gender | -.177 | .324 | .031 | .203 | ||
| Age | -.244 | .171 | .059 | |||
| Baseline skills confidence | -.297 | .094 | .088 | |||
| Baseline performance | .450 | .009 | .203 | .450 | .009 | |
| 2nd model | ||||||
| Gender | -.177 | .324 | .031 | .369 | ||
| Age | -.244 | .171 | .059 | -.262 | .092 | |
| Baseline skills confidence | -.297 | .094 | .088 | -.306 | .052 | |
| Performance after course | .487 | .004 | .237 | .440 | .006 |
4. Discussion and Conclusion
4.1 Discussion
An exposure to 20 hours of communication skills training according to the Four Habits model introduced a lasting increase in the communication skills self-efficacy of the participating physicians. The increase was most prominent in those individuals with better performance after the course who also had low baseline self-efficacy. By introducing 20 hours of theory and rehearsal in role plays with feedback, even a stable construct like self-efficacy can be modified. Previously, an effect of the Four Habits approach on clinician confidence in end of life conversations has been observed to last for at least three months [36].Our findings suggest that a change in general communication skills self-efficacy may last for at least three years.
The association between self-efficacy and objectively rated performance also changed as a result of the course. While self-efficacy was not associated with performance at baseline, performance evaluated at a median of 5 months after the course was significantly correlated with self-efficacy at follow-up more than three years later. The induced change was significant also in subgroups, even among physicians that claimed not to have changed practice following the course. We are not aware of previous studies of such long-term effects of communication skills training on self-efficacy and accuracy of self-efficacy compared with performance.
The increase in self-efficacy and increased association between self-efficacy and performance are potentially due to a mixture of experiences in the course and in practice afterwards. Previous analyses demonstrated that the Four Habits approach improved performance of the participants [25]. The performance after the course is an indicator of how well the participants were able to apply their newly acquired knowledge in practice. As this indicator is correlated with self-efficacy more than three years later, physicians may have continued to relate their experiences in practice to what they learned in the course, thereby becoming more realistic about their skills. Good baseline performance indicated a larger increase in self-efficacy regardless of baseline self-efficacy. These physicians may have recognized that their pre-course communication skills were supported by what was taught in the course, leading to increased self-efficacy. The strong association between post-course performance and self-efficacy at follow-up supports the notion that these physicians recognize their increased mastery of communication after the course, particularly for those whose baseline self-efficacy was low. We are not aware of any other activity in the hospital that could explain these lasting changes. There were no systematic behavioral interventions, no systematic supervision of clinical communication, and no incentive for the physicians to attend other external courses in clinical communication.
One achievement of this study is that communication skills self-efficacy of a sample of physicians representing several specialties was compared to expert judgment of performance in real encounters. Having follow-up data more than three years after the intervention is another important strength of this analysis. However, no direct observations of performance at the extended follow-up were available and follow-up performance was accessed at an earlier time point. It would be interesting to know if communication performance remained improved after three years. As with any long term follow up, another weakness is that one third of the physicians was lost or did not respond. However, these physicians did not differ from those included in the analyses on any variables including baseline communication skills performance and self-efficacy. Also, although self-efficacy and self-assessment are related concepts, we cannot infer that findings would have been similar had the physicians been asked to assess their own performance in the observed encounters. Finally, we have provided an expert judgment and considered it a criterion measure of communication performance. To imply that expert judgment is a gold standard has been criticized by Ward et al [22] and others. However, we used four blinded raters, randomly allocated videotapes, and demonstrated high interrater reliability. The Four Habits Coding scheme has been externally validated and used in several studies for the objective evaluation of communication skills performance [31,37]. Therefore, it is unlikely that biases in expert judgements have distorted the conclusions.
4.2 Conclusion
We have provided evidence that a 20-hour communication skills training course based on the Four Habits approach was associated with long-term increases in self-efficacy and a significantly positive association between self-efficacy at follow-up up to three and a half years later and performance the first year after intervention. This suggests that communication skills training may not only cause lasting improvements in physicians' self-confidence in their communication skills ability, but that the increased confidence is accurately associated with improvements in performance.
4.3 Practice implications
A postgraduate basic communication skills course for physicians may function as a source of insight in own performance. This insight is an important source for (further) improvement.
Acknowledgments
Declaration of interest
Funding/support: This work was partially funded by the Regional Health Enterprise for South-East Norway.
Helpful statistical advice was given by Jurate Saltyte Benth, and Haldor Husby administered the follow-up mail survey.
Footnotes
Other disclosures: The authors declare no conflicts of interest.
References
- 1.Kurtz S, Silverman J, Benson J, Draper J. Marrying content and process in clinical method teaching: enhancing the Calgary-Cambridge guides. Acad Med. 2003;78:802–9. doi: 10.1097/00001888-200308000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Pendleton D, Schofield T, Tate P, Havelock P. The consultation: an approach to learning and teaching. Oxford: Oxford University Press; 1984. [Google Scholar]
- 3.Stewart M, Belle Brown J, Wayne Weston W, McWhinney IR, McWilliam C, Freeman TR. Patient-centered medicine: transforming the clinical method. Thousand Oaks: Sage Publications; 1995. [Google Scholar]
- 4.Barth J, Lannen P. Efficacy of communication skills training in oncology: a systematic review and meta-analysis. Ann Oncol. 2011;22:1030–40. doi: 10.1093/annonc/mdq441. [DOI] [PubMed] [Google Scholar]
- 5.Fellowes D, Wilkinson S, Moore P. Communication skills training for health care professionals working with cancer patients, their families and/or carers (Review) Cochrane Database Syst Rev. 2004;2:CD003751. doi: 10.1002/14651858.CD003751.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Hulsman RL, Ros WJ, Winnubst JA, Bensing JM. Teaching clinically experienced physicians communication skills. A review of evaluation studies. Med Educ. 1999;33:655–68. doi: 10.1046/j.1365-2923.1999.00519.x. [DOI] [PubMed] [Google Scholar]
- 7.Kramer AW, Düsman H, Tan LH, Jansen JJ, Grol RP, van der Vleuten CP. Acquisition of communication skills in postgraduate training for general practice. Med Educ. 2004;38:158–67. doi: 10.1111/j.1365-2923.2004.01747.x. [DOI] [PubMed] [Google Scholar]
- 8.Butalid L, Verhaak PFM, Tromp F, Bensing JM. Changes in the quality of doctor-patient communication between 1982 and 2001: an observational study on hypertension care as perceived by patients and general practitioners. BMJ Open. 2011;1:e000203. doi: 10.1136/bmjopen-2011-000203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sitzia J, Wood N. Patient satisfaction: a review of issues and concepts. Soc Sci Med. 1997;45:1829–43. doi: 10.1016/s0277-9536(97)00128-7. [DOI] [PubMed] [Google Scholar]
- 10.Makoul G, Krupat E, Chang CH. Measuring patient views of physician communication skills: Development and testing of the Communication Assessment Tool. Patient Educ Couns. 2007;67:333–42. doi: 10.1016/j.pec.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Nørgaard B. Communication with patients and colleagues. Dan Med Bull. 2011;58:B4359. [PubMed] [Google Scholar]
- 12.Agledahl K, Wifstad Å, Førde R, Gulbrandsen P. Courteous but not curious: How doctors' politeness masks their existential neglect. A qualitative study of video-recorded patient consultations. J Med Ethics. 2011;37:650–4. doi: 10.1136/jme.2010.041988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gordon MJ. A review of the validity and accuracy of self-assessments in health professions training. Acad Med. 1991;66:762–9. doi: 10.1097/00001888-199112000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Colthart I, Bagnall G, Evans A, Allbutt H, Haig A, Illing J, McKinstry B. The effectiveness of self-assessment on the identification of learner needs, learner activity, and impact on clinical practice: BEME Guide No.10. Med Teach. 2008;30:124–45. doi: 10.1080/01421590701881699. [DOI] [PubMed] [Google Scholar]
- 15.Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy of physician self-assessment compared with observed measures of competence. A systematic review. JAMA. 2006;296:1094–102. doi: 10.1001/jama.296.9.1094. [DOI] [PubMed] [Google Scholar]
- 16.Lipsett PA, Harris I, Downing S. Resident self-other assessor agreement. Influence of assessor, competency, and performance level. Arch Surg. 2011;146:901–6. doi: 10.1001/archsurg.2011.172. [DOI] [PubMed] [Google Scholar]
- 17.Blanch-Hartigan D. Medical students' self-assessment of performance: results from three meta-analyses. Patient Educ Couns. 2011;84:3–9. doi: 10.1016/j.pec.2010.06.037. [DOI] [PubMed] [Google Scholar]
- 18.Lanning SK, Brickhouse TH, Gunsolley JC, Ranson SL, Willett RM. Communication skills instruction: An analysis of self, peer-group, student instructors and faculty assessment. Patient Educ Couns. 2011;83:145–51. doi: 10.1016/j.pec.2010.06.024. [DOI] [PubMed] [Google Scholar]
- 19.Haffling AC, Beckman A, Edgren G. Structured feedback to undergraduate medical students: 3 years' experience of an assessment tool. Med Teach. 2011;33:e349–e357. doi: 10.3109/0142159X.2011.577466. [DOI] [PubMed] [Google Scholar]
- 20.Eva KW, Regehr G. Self-assessment in the health professions: A reformulation and research agenda. Acad Med. 2005;80(10):S46–S54. doi: 10.1097/00001888-200510001-00015. [DOI] [PubMed] [Google Scholar]
- 21.Nothnagle M, Anandarajah G, Goldman RE, Reis S. Struggling to be self-directed: residents' paradoxical beliefs about learning. Acad Med. 2011;86:1539–44. doi: 10.1097/ACM.0b013e3182359476. [DOI] [PubMed] [Google Scholar]
- 22.Ward M, Gruppen L, Regehr G. Measuring self-assessment: Current state of the art. Adv Health Sci Educ. 2002;7:63–80. doi: 10.1023/a:1014585522084. [DOI] [PubMed] [Google Scholar]
- 23.Gordon MJ. Self-assessment programs and their implications for health professions training. Acad Med. 1992;67:672–9. doi: 10.1097/00001888-199210000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Gulbrandsen P, Fossli Jensen B, Finset A. Changes in self-efficacy among hospital doctors after a training course in clinical communication skills. Tidsskr Nor Legeforen. 2009;129:2343–6. doi: 10.4045/tidsskr.09.0261. [English version available ( http://tidsskriftet.no/lts-pdf/pdf2009/2343-6eng.pdf)] [DOI] [PubMed] [Google Scholar]
- 25.Fossli Jensen B, Gulbrandsen P, Dahl FA, Krupat E, Frankel RM, Finset A. Effectiveness of a short course in clinical communication skills for hospital physicians: results of a crossover randomized controlled trial (ISRCTN22153332) Patient Educ Couns. 2011;84:163–9. doi: 10.1016/j.pec.2010.08.028. [DOI] [PubMed] [Google Scholar]
- 26.Stein T, Frankel RM, Krupat E. Enhancing clinician communication skills in a large healthcare organization: A longitudinal case study. Patient Educ Couns. 2005;58:4–12. doi: 10.1016/j.pec.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 27.Gulbrandsen P, Krupat E, Benth JS, Garratt A, Safran DG, Finset A, Frankel R. ”Four habits” goes abroad – report from a pilot study in Norway. Patient Educ Couns. 2008;72:388–93. doi: 10.1016/j.pec.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 28.Parle M, Maguire P, Heaven C. The development of a training model to improve health professionals' skills, self-efficacy and outcome expectancies when communicating with cancer patients. Soc Sci Med. 1997;44:231–40. doi: 10.1016/s0277-9536(96)00148-7. [DOI] [PubMed] [Google Scholar]
- 29.Ammentorp J, Sabroe S, Kofoed PE, Mainz J. The effect of training in communication skills on medical doctors' and nurses' self-efficacy. A randomized controlled trial. Patient Educ Couns. 2007;66:270–7. doi: 10.1016/j.pec.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 30.Doyle D, Copeland HL, Bush D, Stein L, Thompson S. A course for nurses to handle difficult communication situations. A randomized controlled trial of impact on self-efficacy and performance. Med Educ. 2011;82:100–9. doi: 10.1016/j.pec.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 31.Krupat E, Frankel R, Stein T, Irish J. The Four Habits Coding Scheme: Validation of an instrument to assess clinicians' communication behavior. Patient Educ Couns. 2006;62:38–45. doi: 10.1016/j.pec.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 32.Fossli Jensen B, Gulbrandsen P, Dahl FA, Saltyte-Benth J, Krupat E, Finset A. The interrater reliability of the Four Habits Coding Scheme as part of a randomized controlled trial. Patient Educ Couns. 2010;80:405–9. doi: 10.1016/j.pec.2010.06.032. [DOI] [PubMed] [Google Scholar]
- 33.Garratt AM, Bjaertnes ØA, Krogstad U, Gulbrandsen P. The OutPatient Experiences Questionnaire (OPEQ): data quality, reliability, and validity in patients attending 52 Norwegian hospitals. Qual Saf Health Care. 2006;6:181–94. doi: 10.1136/qshc.2005.014423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fossli Jensen B, Dahl FA, Safran DG, Garratt AM, Krupat E, Finset A, Gulbrandsen P. The ability of a behaviour specific questionnaire to identify poorly performing doctors. BMJ Qual Saf. 2011;20:885–93. doi: 10.1136/bmjqs-2011-000021. [DOI] [PubMed] [Google Scholar]
- 35.Raghunathan TE, Rosenthal R, Rubin DB. Comparing correlated but nonoverlapping correlations. Psychological Methods. 1996;1:178–83. [Google Scholar]
- 36.Runkle C, Wu E, Wang EC, Gordon GH, Frankel R. Clinician confidence about conversations at the end of life is strengthened using the four habits approach. J Psychosoc Oncol. 2008;26:81–95. doi: 10.1080/07347330802118040. [DOI] [PubMed] [Google Scholar]
- 37.Blanch-Hartigan D, Hall JA, Roter DL, Frankel RM. Gender bias in patients' preceptions of patient-centered behaviors. Patient Educ Couns. 2010;80:315–20. doi: 10.1016/j.pec.2010.06.014. [DOI] [PubMed] [Google Scholar]