Abstract
Sexual assault history is associated with higher risk of problem drinking and drug use in women, yet little is known about mechanisms linking trauma histories in general to women’s drinking or drug use problems. This study examined how various types of trauma, substance use coping, and PTSD relate to past-year problem drinking and drug use in women who experienced sexual assault. Data from a large, diverse sample of women who had experienced adult sexual assault was analyzed with structural equation modeling to test a theoretical model of the relationship between trauma types, substance use coping, PTSD symptoms, and past-year drinking and drug use (N = 1863). Results show that PTSD symptoms fully mediated the association between non-interpersonal trauma and the use of substances to cope. However, the association between both interpersonal trauma and child sexual abuse severity on substance use to cope were only partially mediated by PTSD symptoms. In turn, use of substances to cope fully mediated the relationship between PTSD and problem drug use as well as partially mediated the effect of PTSD on problem drinking. These results suggest that different trauma types and substance use coping may be important risk factors distinguishing sexually assaulted women who develop PTSD and problematic substance use from those who do not. Identifying women’s histories of different traumas may help to identify those at greater risk for substance use problems.
Keywords: sexual assault, child sexual abuse, PTSD, problem drinking, substance use
1. Introduction
Researchers have identified numerous effects of sexual assault on women, including posttraumatic stress disorder (PTSD) and alcohol and drug problems (Foa & Riggs, 1993; Kilpatrick, Resnick, Ruggiero, Conoscenti, & McCauley, 2007; Wilsnack, Vogeltanz, Klassen, & Harris, 1997). Recent reviews suggest significant comorbidity of PTSD and substance use/drinking problems, particularly in female trauma survivors (Stewart & Israeli, 2001). Theories such as the self-medication hypothesis (Cappell & Greeley, 1987) posit that victims suffering from PTSD may use substances to reduce reexperiencing and intrusive symptoms of PTSD. Although this form of coping may help to dampen trauma symptoms in the short term, it may result in chronic PTSD (Chilcoat and Breslau, 1998; Stewart, Conrod, & Dongier 1998). In support of this theory, a longitudinal study of U.S. women showed that development of PTSD symptoms after childhood rape was followed by twice the number of alcohol abuse symptoms (Epstein, Saunders, Kilpatrick, & Resnick, 1998).
A common response to stressful life events such as rape is engagement in avoidance coping strategies or effortful attempts to avoid or reduce negative affect (Littleton, Horsley, John, & Nelson 2007). Unfortunately, such strategies, although a common protective response to severe stressors, can be ineffective. For example, use of substances (i.e., alcohol, drugs) to cope with negative affect can be seen as a form of avoidance coping. Studies of both general population samples and student samples show that drinking to cope is associated with alcohol consumption and drinking problems (Carpenter & Hasin, 1999; Cooper, Frone, Russell, & Mudar, 1995; Holahan, Moos, Holahan, Cronkite, & Randall, 2001; Park & Levenson, 2002). Studies show women with histories of sexual victimization and other traumas (e.g., child abuse) may be more likely to engage in drinking to cope, possibly in response to PTSD symptoms (Bissonnette et al., 1997; Hussey & Singer, 1993). These PTSD symptoms are related to greater problem drinking (Kaysen et al., 2006; Ullman et al., 2009). Similarly, Bonn-Miller, Vujanovic, Feldner, Bernstein, & Zvolensky (2007) found that PTSD symptoms were related to greater substance use coping in traumatized youth. However, no studies of these variables have examined problem drug use as an outcome in sexual assault victims.
In an earlier study of sexual assault victims, Ullman, Filipas, Townsend, & Starzynski (2005) found that drinking to cope with distress was predicted by child sexual abuse and history of other traumatic events and was associated with greater past-year problem drinking. Further longitudinal analyses revealed that women who were revictimized (i.e., had experienced a new sexual assault or traumatic event within a year from the first survey) had increased problem drinking only if they reported engaging in more drinking to cope with distress (Ullman & Najdowski, 2009). Past research shows comorbidity of trauma exposure and alcohol problems in the general population, and even greater comorbidity in subpopulations of sexual assault victims and substance abusers (Stewart, 1996; Stewart & Israeli, 2001). In addition, some research indicates that the types of trauma experienced (e.g., interpersonal versus non-interpersonal) can have different effects on psychological outcomes (e.g., Ehring & Quack, 2010). Researchers have yet to examine how specific types of trauma exposure may affect problem substance use and possible mediators of these effects. Such work is needed for developing effective intervention and treatment of sexual trauma survivors with comorbid PTSD and substance abuse (Stewart & Israeli, 2001).
Unlike past work, this study disaggregates trauma types into non-interpersonal and interpersonal traumas to evaluate their unique effects. This study also adds problem drug use as an outcome, which is important because sexual victimization is linked to higher risk of drug use and abuse in women (Kendler et al., 2000; Kilpatrick, Acierno, Resnick, Saunders, & Best, 1997). Past research has shown that different kinds of trauma can have differential effects; therefore traumas were disaggregated into non-interpersonal trauma, interpersonal trauma and childhood sexual abuse severity. However, we made no hypotheses about how these effects might differ.
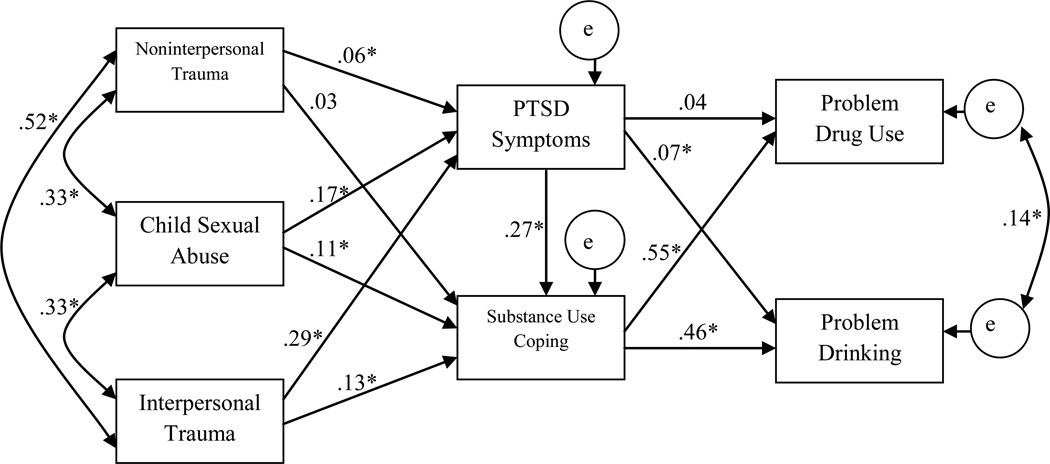
The present study tested a mediation model of trauma exposure and problem substance use (see Figure 1) in a large sample of sexual assault survivors. Several direct effects were hypothesized based on past literature. Traumatic events and child sexual abuse severity were expected to relate to two mediators, (a) use of substances to cope and (b) PTSD (both assessed with respect to sexual assault); both mediators were expected to predict problem drinking and drug use.
Figure 1.
Structural Model of the Relations of Trauma Variables, Substance Use Coping, and PTSD in Predicting Problem Substance Use Outcomes
2. Method
2.1 Participants and Procedure
A volunteer sample of women (N = 1863) from the Chicagoland area, age ranging from 18 to 71 (M = 31.1, SD = 12.2) was recruited for a mail survey. The sample was ethnically diverse (45% African-American, 35% White, 2% Asian, 8.1% other; 14% Hispanic, assessed separately). The sample was well educated with 34.6% having a college degree or higher, 43.5% having some college education, and 21.9% having a high school education or less. Just under half of the sample (46.8%) was currently employed, although income levels were relatively low, with 68% of women having household incomes of less than $30,000. The response rate was 85%.
Recruitment was accomplished via weekly advertisements in local newspapers, on Craigslist, and through university mass mail. In addition, we posted fliers in the community, at other Chicago colleges and universities, as well as at agencies that cater to community members in general and victims of violence against women specifically (e.g., community centers, cultural centers, substance abuse clinics, domestic violence and rape crisis centers). Interested women called the research office and were screened for eligibility using the following criteria: a) had an unwanted sexual experience at the age of 14 or older, b) were 18 or older at the time of participation, and c) had previously told someone about their unwanted sexual experience. We sent eligible participants packets containing the survey, an informed consent sheet, a list of community resources for dealing with victimization, and a stamped return envelope for the completed survey. Participants were paid $25 for their participation. The university’s Institutional Review Board approved all study procedures and documents.
2.2 Measures
2.2.1. Sexual victimization
Sexual victimization in both childhood (prior to age 14) and adulthood (at age 14 or older) was assessed using a modified version of the Sexual Experiences Survey (SES, Koss, Gidycz, & Wisniewski 1987). The revised measure (Testa, VanZile-Tamsen, Livingston, & Koss, 2004) assesses various forms of sexual assault including: unwanted sexual contact, verbally coerced intercourse, attempted rape, and rape resulting from force or incapacitation (e.g., from alcohol or drugs). The revised 11-item SES measure had good reliability (α = .73); similar reliability was found in our sample (α = .78). Both child sexual abuse and adult sexual assault were assessed with the SES measure in the survey, but no measure of adult sexual assault was included in the model, because all women had a sexual assault in adulthood.
2.2.2. Child sexual abuse severity
In this study responses to the SES prior to age 14 were used to code a 5-level ordinal variable indicating child sexual abuse severity ranging from fondling/kissing through completed rape (M = 1.88, SD = 1.72, α = .89). Child sexual abuse was assessed separately from other traumatic events, with the SES, because this trauma requires multiple specific behavioral questions. This trauma has unique effects on both women’s PTSD and substance use/abuse outcomes (Sartor et al., 2012; Wilsnack et al., 1997) compared to other traumas (Molnar, Buka, & Kessler, 2001).
2.2.3. Traumatic life events
Traumatic event history was assessed with a revised version of the Stressful Life Events Screening Questionnaire (Goodman, Corcoran, Turner, Yuan, & Green, 1998), the SLESQ-Revised, developed as a brief self-report measure of various traumatic events (Green, Chung, Daroowalla, Kaltman, & DeBenedictis 1998). Green and colleagues’ revised version includes child abuse and adult violence experiences, stalking (Logan, 2007) and a question we added on neighborhood/community violence, “Have you ever lived in a neighborhood or community where you felt threatened or your life was in danger?” This measure is scored as the sum of events experienced by each respondent (excluding child and adult sexual assault both assessed by the Revised SES). The measure had good test-retest reliability (median Kappa = .73), and adequate convergent validity (with a lengthier interview) with a median Kappa of .64. Past research suggests that interpersonal and non-interpersonal traumas are unique and may have different effects (Ehring & Quack, 2010; Green et al., 2000). Thus, based on a principal components analysis with promax rotation, we disaggregated traumas into interpersonal trauma (e.g., stalking, child abuse, abuse by a romantic partner, abuse by someone else, emotional abuse), and non-interpersonal trauma (e.g., military war zone, dangerous neighborhood, threatened with a weapon, in other frightening situations, force used against you in robbery, close friends died from homicide, witnessed death).
2.2.4. Posttraumatic stress symptoms associated with sexual assault
PTSD symptoms were assessed with the Posttraumatic Stress Diagnostic Scale (PDS; Foa, 1995), a standardized 17-item instrument based on DSM-IV criteria. On a scale ranging from 0 (not at all) to 3 (almost always), women rated how often each symptom (i.e., reexperiencing/intrusion, avoidance/numbing, hyperarousal) bothered them in relation to the sexual assault during the past 12 months. If women had more than one assault, PTSD symptoms were assessed with respect to the most serious assault. The PDS has acceptable test–retest reliability for a PTSD diagnosis in assault survivors over two weeks (κ=.74; Foa, Cashman, Jaycox, & Perry 1997). The 17 items were summed to assess the extent of posttraumatic symptomatology (M = 21.13, SD = 12.93, α =.93 in this sample).
2.2.5. Substance use to cope
Substance use to cope was assessed with two items from the Brief COPE, a 28-item self-report scale of coping strategies (Carver, 1997). We assessed substance use coping by summing two Brief COPE items on the use of alcohol and/or drugs in the past 12 months to cope with the sexual assault (“I used alcohol or other drugs to make myself better”, “I used alcohol or other drugs to help me through it”). These 2 coping items are highly correlated, r (1820) = .89, p < .001. The response scale ranges from 1 (I didn't do this at all) to 4 (I did this a lot) for each item (M = 4.23, SD = 2.36, α = .94 in this sample).
2.2.6. Problem drinking
Past-year problem drinking was assessed with the Michigan Alcoholism Screening Test (MAST, Selzer, 1971), a widely used 25-item standardized self-report screening instrument for alcohol abuse and dependence. The number of alcohol-related problems during the past year was coded as a continuous measure (M = 2.90, SD = 4.22, α =.80 in this sample) and indicates a low level of alcohol problems, with only 20% problem drinkers, compared to 38% in another similar study of sexual assault victims (Ullman et al., 2008).
2.2.7. Drug use problems
Problem drug use symptoms were assessed using a modified, shortened version of the Drug Abuse Screening Test, the DAST-10 (DAST-10, McCabe et al., 2006). The DAST-10 has good internal consistency (α = .86), temporal stability (test–retest intraclass correlation coefficient = .71), and can identify individuals needing more intensive assessment for substance abuse problems (Cocco & Carey, 1998). The scale was also reliable for our sample, α =.86. We found a loe level of problems related to drug abuse according to Skinner’s (1982) DAST screening guidelines (M = 2.02, SD = 2.68), with 29% meeting the criteria for problem drug use, yet a greater level of problem symptoms in comparison to other samples of women (McCabe, Boyd, Cranford, Morales, & Slayden 2006).
3. Results
To test our hypotheses, we used AMOS 19 (Arbuckle, 2010) to construct an observed variables model of the effects of trauma histories, substance use coping, and PTSD on both problem drinking and drug use outcomes using maximum likelihood estimation. Most measures were univariate normal with skew less than 3 and kurtosis less than 4 (Kline, 1998). However the past-year MAST score had a slightly high kurtosis (k = 6.04). We used the untransformed variables, given that with larger samples effects of violations of normality assumptions regarding kurtosis are minimal (Tabachnick & Fidell, 2001). Correlations of all variables in the models were positive and significant (r’s .14–.56, p’s < .001).
We tested an initial model with child sexual abuse and the summed number of traumatic events as exogenous variables (not shown). The model fit was acceptable with CFI of .98 and RSMEA of .073; χ2 (4, N=1863) = 43.46, p < .001. We then disaggregated the traumatic events variable into non-interpersonal and interpersonal traumas. We allowed the exogenous variables to be correlated and had a direct path from PTSD to substance use coping, as we expected a self-medication effect. Both mediators predicted problem drinking and drug use as outcome variables. The final model with standardized regression weights is shown in Figure 1, and had a good fit with CFI of .99, TLI of .93, IFI of .99, and RSMEA of .059; χ2 (6, N=1863) = 45.23, p = .000. Although the model chi-square was significant, it was relatively low considering the very high power of this large sample. Fit indices exceed the recommendation of 0.95, except the TLI, and the RMSEA is lower than 0.06, indicating good fit (Hu & Bentler, 1999).
Although the theorized model had good fit, is possible that drug and alcohol use exacerbate PTSD symptoms. Therefore, we ran an alternative model in which substance abuse coping as well as alcohol and drug problems predicted PTSD (paths from trauma variables to PTSD and substance abuse coping remained). This model fit was slightly worse, CFI of .98, RMSEA of .064 with the upper limit of RMSEA exceeding .08. Most importantly, PTSD was not predicted by either drug abuse (β = −.01, ns) or alcohol use (β = .04, ns). Therefore, it appears the directionality of the theorized model may be more accurate, however we cannot be sure given the cross-sectional nature of these data. In our suggestions of causality we rely primarily on theoretical considerations (i.e., self-medication hypothesis) and prior research.
With no mediators in the model, non-interpersonal trauma, interpersonal trauma, and child sexual abuse had direct effects on all outcome variables, except that non-interpersonal traumas did not relate to problem drinking. All traumas were also positively associated with PTSD symptoms that in turn partially mediated the effects of traumas on substance use coping. Lastly, PTSD and substance use coping fully mediated the effect of traumas on problem drinking and partially mediated the effect on problem drug use. Significant mediation was verified by bootstrapping techniques recommended by Preacher and Hayes (2004).
4. Discussion
The present study builds on and extends past research by testing a theoretical model of the predictors of problem drinking and drug use in a large, diverse sample of adult sexual assault victims. We used structural equation modeling to examine the relationship between trauma exposure variables, substance use to cope, past-year PTSD, and past-year problem drinking and drug use. Consistent with a previously found association between trauma and drinking problems (Ouimette & Brown, 2003), we found that a higher degree of lifetime trauma exposure and sexual abuse severity in childhood were each associated with a greater use of substances to cope. This relationship was mediated by PTSD and supports the self-medication model, which posits that those who drink to cope with distress or because they believe it will reduce stress have more PTSD symptoms (Cappell & Greeley, 1987).
Non-interpersonal traumas and interpersonal traumas both predicted PTSD but only interpersonal traumas predicted substance use to cope. Child sexual abuse severity was also associated with both PTSD symptoms and substance use to cope. These findings suggest that trauma type is important, as suggested by Green and colleagues (2000) and Ehring and Quack (2010) in understanding how such histories impact mechanisms leading to drinking and substance use problems. Perhaps interpersonal traumas are more likely to affect women’s trust in others, and their ability to rely on their social network to cope, which in turn increases their reliance on maladaptive coping strategies such as drinking. In fact, histories of interpersonal trauma are more likely to elicit feelings of betrayal and reduced trust in others (Gobin, 2012). Thus, when people do not share their interpersonal trauma experiences because they are less likely to trust others, this could reduce the opportunity to get effective support, leaving them alone to deal with increased distress and psychological symptoms, which in turn might lead to increased drinking to cope. These findings also fit with other research showing greater effects of intimate partner violence versus non-intimate partner violence traumas on binge drinking and depression in adolescents (Cisler et al., 2012).
Our results revealed that PTSD and substance use coping fully mediated the effects of traumatic events on problem drinking and partially mediated the effects of traumatic effects on problem drug use. However, it should be noted that the direct effects were small (βs = .02 – .15). All trauma types also predicted PTSD. Yet, only child sexual abuse and interpersonal trauma predicted substance use coping after controlling for the mediating effect of PTSD. Lastly, substance use coping mediated the relationship of PTSD to problem drug use.
This model suggests that disaggregating trauma types may be important for understanding the pathways through which trauma histories are associated with problem drinking and drug use. Substance use coping strongly predicted problem drinking and drug use in the past year, whereas PTSD predicted problem drinking, but not problem drug use. This model fit the data better than a preliminary model summing all trauma types together, suggesting that using overall summed measures of traumatic events may obscure unique effects of specific trauma types. Future models should examine how both past histories of trauma and exposure to new traumatic events affect women’s substance use coping and PTSD symptoms, given that these two factors influence problem substance use outcomes. Better understanding of the role of trauma histories in substance abuse may help develop targeted treatments for distinct subgroups of sexual assault survivors. Although the sample size was suitably large for the demands of structural equation modeling, the generalizability of our findings is limited by the cross-sectional design and nonrepresentative sample of the study. The sample was comprised of all adult sexual assault victims to better understand how trauma histories and post-assault coping and PTSD predict substance use problems in this high-risk group. As a result, the sample is not representative of the general population and our findings should not be generalized to all trauma survivors. We were primarily interested in the added risk trauma histories can present for developing problems commonly associated with sexual assault, in an effort to understand why some victims develop such problems while others are more resilient. Child sexual abuse was assessed with a multi-item scale, whereas other traumas had only single item measures. Therefore, the study does not allow for a full assessment of the effects of all childhood and adult traumas. Also, given that all women were assaulted in adulthood, we cannot examine risk factors for revictimization. However, with future waves of data we will be able to further explore risk for future revictimization.
Finally, like all structural equation modeling, these analyses are limited by the fact that a model with good fit does not mean that the model is proven. Although a model with good fit can result when the model accurately reflects reality, good fit can also result when the model is equivalent to an alternative model that reflects reality, the model fits data from a nonrepresentative sample but does not fit the population, or the number of parameters is so great that it cannot have poor fit (Kline, 1998). We are currently collecting longitudinal data from this sample, which may help clarify the direction of effects.
Our study had a number of strengths. Unlike past studies examining these mediators of the sexual assault -- drinking relationship (e.g., Miranda, Meyerson, Long, Marx, & Simpson, 2002; Ullman et al., 2005), this study had a larger, ethnically and socioeconomically diverse sample, and examined multiple trauma types as well as problem drug use, known sequelae of trauma exposure (Ouimette & Brown, 2003). These findings suggest that trauma history, substance use to cope, and PTSD help to explain alcohol and drug problems in sexual assault victims and may be used to enhance treatment of victimized women with PTSD and substance use problems. Specific trauma types should be assessed in both research and treatment, because they may have distinct effects on PTSD and substance use coping, both of which impact substance use problems in sexually assaulted women.
Table 1.
Bivariate correlations between trauma variables, coping, and symptoms (ns = 1551–1760)
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | |
|---|---|---|---|---|---|---|---|
| 1. Child sexual abuse severity | — | .34* | .34* | .24* | .29* | .15* | .19* |
| 2. Non-Interpersonal trauma | — | .52* | .21* | .27* | .14* | .24* | |
| 3. Interpersonal trauma | — | .28* | .38* | .22* | .24* | ||
| 4. Substance use coping | — | .36* | .47* | .56* | |||
| 5. PTSD | — | .22* | .23* | ||||
| 6. Problem drinking | — | .37* | |||||
| 7. Problem drug use | — | ||||||
Note.
p ≤ .001.
Highlights.
Child sexual abuse and interpersonal trauma predicted substance use coping.
PTSD mediated effects of contextual trauma and substance use coping.
Interpersonal trauma had stronger effects on PTSD and substance use coping than contextual trauma.
PTSD and substance use coping mediated relations of traumatic events with substance use outcomes.
Acknowledgements
We thank Cynthia Najdowski, Saloni Shah, Susan Zimmerman, Rene Bayley, Farnaz Mohammad-Ali, & Gabriela Lopez for assistance with data collection.
Role of Funding Sources
Funding for this study was provided by NIAAA Grant R01-AA17429. NIAAA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Sarah Ullman designed the study and wrote the protocol, conducted literature searches and provided summaries of previous research studies. Mark Relyea conducted the statistical analysis. Sarah Ullman wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
References
- Arbuckle JL. AMOS (Version 19) Chicago: Small Waters; 2010. [Computer software]. [Google Scholar]
- Bissonnette M, Wall A-M, Wekerle C, McKee SA, Hinson RE, Tsianis D. Is a post-traumatic stress disorder (PTSD) mediational model a valid framework for understanding undergraduate drinking behavior? Alcoholism: Clinical and Experimental Research. 1997;21:54A. [Summary]. [Google Scholar]
- Bonn-Miller M, Vujanovic A, Feldner M, Bernstein A, Zvolensky M. Posttraumatic stress symptom severity predicts marijuana use coping motives among traumatic event-exposed marijuana users. Journal of Traumatic Stress. 2007;20:577–586. doi: 10.1002/jts.20243. [DOI] [PubMed] [Google Scholar]
- Cappell H, Greeley J. Alcohol and tension reduction: An update on research and theory. In: Blane HT, Leonard KE, editors. Psychological theories of drinking and alcoholism. New York: Guilford; 1987. pp. 15–54. [Google Scholar]
- Carpenter KM, Hasin DS. Drinking to cope with negative affect and DSM-IV alcohol use disorders: A test of three alternative explanations. Journal of Studies on Alcohol and Drugs. 1999;60:694–704. doi: 10.15288/jsa.1999.60.694. [DOI] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Chilcoat HD, Breslau NL. Investigation of the causal pathways between PTSD and drug use. Addictive Behaviors. 1998;23:827–840. doi: 10.1016/s0306-4603(98)00069-0. [DOI] [PubMed] [Google Scholar]
- Cisler JM, Begle AM, Amstadter AB, Resnick HS, Danielson CK, Saunders BE, Kilpatrick DG. Exposure to interpersonal violence and risk for PTSD, depression, delinquency, and binge drinking among adolescents: Data from the NSA-R. Journal of Traumatic Stress. 2012;25:33–40. doi: 10.1002/jts.21672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cocco KM, Carey KB. Psychometric properties of the Drug Abuse Screening Test in psychiatric outpatients. Psychological Assessment. 1998;10:408–414. [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Ehring T, Quack D. Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy. 2010;41:587–598. doi: 10.1016/j.beth.2010.04.004. [DOI] [PubMed] [Google Scholar]
- Epstein JN, Saunders BE, Kilpatrick DG, Resnick HS. PTSD as a mediator between childhood rape and alcohol use in adult women. Child Abuse and Neglect. 1998;22:223–234. doi: 10.1016/s0145-2134(97)00133-6. [DOI] [PubMed] [Google Scholar]
- Foa EB. Posttraumatic Stress Diagnostic Scale manual. Minneapolis: National Computer Systems; 1995. [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of PTSD: The Posttraumatic Stress Diagnostic Scale. Psychological Assessment. 1997;9:445–451. [Google Scholar]
- Foa EB, Riggs DS. Posttraumatic stress disorder and rape. In: Oldham JM, Tasman A, editors. Review of psychiatry. Washington, DC: American Psychiatric Press; 1993. pp. 273–303. [Google Scholar]
- Gobin R. Unpublished doctoral dissertation. University of Oregon; 2012. Trauma, trust, and betrayal awareness. [Google Scholar]
- Goodman LA, Corcoran C, Turner K, Yuan N, Green BL. Assessing traumatic event exposure: General issues and preliminary findings for the Stressful Life Events Screening Questionnaire. Journal of Traumatic Stress. 1998;11:521–542. doi: 10.1023/A:1024456713321. [DOI] [PubMed] [Google Scholar]
- Green BL, Chung JY, Daroowalla A, Kaltman S, DeBenedictis C. Evaluating the cultural validity of the Stressful Life Events Screening Questionnaire. Violence Against Women. 2006;12:1191–1213. doi: 10.1177/1077801206294534. [DOI] [PubMed] [Google Scholar]
- Green BL, Goodman LA, Krupnick JL, Corcoran CB, Petty RM, Stockton P, Stern N. Outcomes of single versus multiple trauma exposure in a screening sample. Journal of Traumatic Stress. 2000;13:271–286. doi: 10.1023/A:1007758711939. [DOI] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Cronkite RC, Randall PK. Drinking to cope, emotional distress and alcohol use and abuse: A 10-year model. Journal of Studies on Alcohol and Drugs. 2001;62:190–198. doi: 10.15288/jsa.2001.62.190. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Hussey DL, Singer M. Psychological distress, problem behaviors, and family functioning of sexually abused adolescent inpatients. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:954–961. doi: 10.1097/00004583-199309000-00010. [DOI] [PubMed] [Google Scholar]
- Kaysen D, Simpson T, Dillworth T, Larimer M, Gutner C, Resick P. Alcohol problems and posttraumatic stress disorder in female crime victims. Journal of Traumatic Stress. 2006;19:399–403. doi: 10.1002/jts.20122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler K, Bulik C, Silberg J, Hettema J, Myers J, Prescott C. Child sexual abuse and adult psychiatric and substance use disorders in women: An epidemiological and cotwin control analysis. Archives of General Psychiatry. 2000;57:953–959. doi: 10.1001/archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- Kilpatrick D, Acierno R, Resnick H, Saunders B, Best C. A 2-year longitudinal analysis of the relationships between violent assault and substance use in women. Journal of Consulting and Clinical Psychology. 1997;65:834–847. doi: 10.1037//0022-006x.65.5.834. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Ruggiero KJ, Conoscenti LM, McCauley J. Drug facilitated, incapacitated, and forcible rape: A national study. Final Report. NCJRS Document # 219181. U.S. Department of Justice; 2007. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York: Guilford Press; 1998. [Google Scholar]
- Koss MP, Gidycz CA, Wisniewski N. The scope of rape: Incidence and prevalence of sexual aggression and victimization in a national sample of students in higher education. Journal of Consulting and Clinical Psychology. 1987;55:162–170. doi: 10.1037//0022-006x.55.2.162. [DOI] [PubMed] [Google Scholar]
- Littleton H, Horsley S, John S, Nelson D. Trauma coping strategies and psychological distress: A meta-analysis. Journal of Traumatic Stress. 2007;20:977–988. doi: 10.1002/jts.20276. [DOI] [PubMed] [Google Scholar]
- Logan TK. Personal communication. 2007 [Google Scholar]
- McCabe S, Boyd C, Cranford J, Morales M, Slayden J. A modified version of the Drug Abuse Screening Test among undergraduate students. Journal of Substance Treatment. 2006;31:297–303. doi: 10.1016/j.jsat.2006.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda R, Meyerson LA, Long PJ, Marx BP, Simpson SM. Sexual assault and alcohol use: Exploring the self-medication hypothesis. Violence and Victims. 2002;17:205–217. doi: 10.1891/vivi.17.2.205.33650. [DOI] [PubMed] [Google Scholar]
- Molnar B, Buka S, Kessler R. Child sexual abuse and subsequent psychopathology: Results from the National Comorbidity Survey. American Journal of Public Health. 2001;91:753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouimette P, Brown PJ. Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders. Washington, DC: American Psychological Association; 2003. [Google Scholar]
- Park CL, Levenson MR. Drinking to cope among college students: Prevalence, problems, and coping processes. Journal of Studies on Alcohol and Drugs. 2002;63:486–497. doi: 10.15288/jsa.2002.63.486. [DOI] [PubMed] [Google Scholar]
- Preacher K, Hayes A. SPSS and SAS procedures for estimating indirect effects in Simple mediation models. Behavior, Research, Methods, Instrumentation, and Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Sartor C, McCutcheon V, Nelson E, Duncan A, Bucholz K, Heath A. Investigating the association between childhood sexual abuse and alcohol use disorders in women: Does it matter how we ask about sexual abuse? Journal of Studies on Alcohol and Drugs. 2012;763:740–748. doi: 10.15288/jsad.2012.73.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selzer ML. The Michigan Alcoholism Screening Test: The quest for a new diagnostic instrument. American Journal of Psychiatry. 1971;127:1653–1658. doi: 10.1176/ajp.127.12.1653. [DOI] [PubMed] [Google Scholar]
- Skinner HA. The Drug Abuse Screening Test. Addictive Behavior. 1982;7(4):363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Stewart SH. Alcohol abuse in individuals exposed to trauma: A critical review. Psychological Bulletin. 1996;120:83–112. doi: 10.1037/0033-2909.120.1.83. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Israeli AL. Substance abuse and co-occurring psychiatric disorders in victims of intimate violence. In: Wekerle C, Hall A, editors. The violence and addiction equation: Theoretical and clinical issues in substance abuse and relationship violence. New York: Hogrefe & Huber; 2001. pp. 98–122. [Google Scholar]
- Stewart SH, Pihl R, Conrod P, Dongier M. Functional associations among trauma, PTSD, and substance-related disorders. Addictive Behaviors. 1988;23:797–812. doi: 10.1016/s0306-4603(98)00070-7. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 4th ed. New York: Harper Collins; 2001. [Google Scholar]
- Testa M, VanZile-Tamsen C, Livingston JA, Koss MP. Assessing women’s experiences of sexual aggression using the Sexual Experiences Survey: Evidence for validity and implications for research. Psychology of Women Quarterly. 2004;28:256–265. [Google Scholar]
- Ullman SE, Filipas HH, Townsend SM, Starzynski L. Trauma exposure, PTSD, and problem drinking among sexual assault survivors. Journal Studies on Alcohol & Drugs. 2005;66:610–619. doi: 10.15288/jsa.2005.66.610. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Najdowski CJ. Revictimization as a moderator of psychosocial risk factors for problem drinking in female sexual assault survivors. Journal of Studies on Alcohol and Drugs. 2009;70:41–49. doi: 10.15288/jsad.2009.70.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman SE, Starzynski LL, Long S, Mason G, Long LM. Sexual assault disclosure, social reactions, and problem drinking in women. Journal of Interpersonal Violence. 2008;23:1235–1257. doi: 10.1177/0886260508314298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilsnack SC, Vogeltanz ND, Klassen AD, Harris TR. Childhood sexual abuse and women’s substance abuse: National survey findings. Journal of Studies on Alcohol and Drugs. 1997;58:264–27. doi: 10.15288/jsa.1997.58.264. [DOI] [PubMed] [Google Scholar]