Abstract
Objective
To investigate course and predictors of eating disorders in the postpartum period.
Method
A total of 77,807 women, participating in the Norwegian Mother and Child Cohort Study (MoBa), completed questionnaires during pregnancy including items covering DSM-IV criteria for pre-pregnancy anorexia nervosa (AN), bulimia nervosa (BN), eating disorder not otherwise specified (EDNOS-P), and binge eating disorder (BED). Additional questionnaires were completed at 18 and 36 months postpartum.
Results
Proportions of women remitting at 18 months and 36 months postpartum were 50% and 59% for AN, 39% and 30% for BN, 46% and 57% for EDNOS-P, and 45% and 42% for BED, respectively. However, disordered eating persisted in a substantial proportion of women meeting criteria for either full or subthreshold eating disorders. BN during pregnancy increased the risk for continuation of BN. BMI and psychological distress were significantly associated with course of BED.
Discussion
This is the first large-scale population-based study on course of eating disorders in the postpartum period. The results indicated that disordered eating persists in a substantial proportion of women with pre-pregnancy eating disorders. Health care professionals working with women in this phase of life need to pay specific attention to eating disorder symptoms and behaviors.
Keywords: eating disorder, anorexia nervosa, bulimia nervosa, binge eating disorder, postpartum, pregnancy, weight retention, depression, course, the Norwegian mother and child cohort study, MoBa
Pregnancy and childbirth are major life events accompanied by profound biological, social, and psychological changes. The presence of an eating disorder in this period may negatively affect the pregnancy (e.g., weight gain), delivery (e.g., caesarean section, preterm delivery) or offspring (e.g., birth weight).1–5
Pregnancy may also influence the course of eating disorders. For the majority of women with anorexia nervosa (AN) and bulimia nervosa (BN), pregnancy appears to lead to adaptive changes in eating behaviors.4, 6, 7 However, for some, pregnancy may lead to maladaptive changes in eating behavior. Our research group has found that pregnancy is a risk window for the onset of binge eating disorder (BED) in vulnerable individuals.6, 8
It is unclear if the changes in eating behavior that occur during pregnancy persist into the postpartum period and beyond. Some clinical studies have suggested that the postpartum is a high-risk period for the recurrence of AN and BN.9–11 To the best of our knowledge, no study has explored the postpartum course of pre-pregnancy eating disorders not otherwise specified such as purging disorder (EDNOS-P)12–14 and binge eating disorders (BED).15, 16 In addition, no studies have explored the course of BED that onsets during pregnancy.
Several factors may influence the course of eating disorders in the postpartum period such as weight retention and postpartum depression. The physical and weight changes associated with pregnancy may influence the reemergence of eating disorders symptoms and behaviors postpartum.17–20 Women with AN, BN, EDNOS-P and BED gain more weight during pregnancy,1 express greater concerns about weight gain,21 and have different postpartum weight retention trajectories than women without eating disorders.22 Women with high residual weight post-pregnancy may have a stronger desire to lose weight, and therefore commence rigid eating restrictions, which may result in recurrence of AN, binge eating, and/or other bulimic pathology.23
The risk for depression in the postpartum period is elevated in women with lifetime or current eating disorders compared to women without eating disorders,2, 11, 18, 24, 25 even when controlling for lifetime depression.26 Core eating disorders behaviors may serve an important function in regulating negative mood and emotions,27, 28 and the risk for relapse of eating disorder symptoms postpartum may be increased in vulnerable depressed women.
As only a minority of women with eating disorders are seen in mental health care,29 and the ones who enter treatment are not representative of the total population of women with eating disorders,30, 31 it is important to study the course and predictors of eating disorders in the postpartum period in population based samples. Given the low prevalence of some eating disorders, large sample sizes are essential to be able to study course across eating disorder subtypes.
We explored course of AN, BN, EDNOS-P and BED in the postpartum period using data from the Norwegian Mother and Child Cohort Study (MoBa)32, a large-scale, population-based, prospective pregnancy cohort including more than 100,000 mother-child records of which 77,807 were included in the current research file. The aims were threefold: 1) to study the course of AN, BN, EDNOS-P, and BED at 18 and 36 months postpartum in women with pre-pregnancy eating disorders; 2) to study the course of BED at 18 and 36 months postpartum in women with a pregnancy-onset BED; and 3) to explore predictors of 18 and 36 months postpartum course in women with pre-pregnancy BN and BED.
METHODS
Participants
The data collection was conducted as a part of the Norwegian Mother and Child Cohort study (MoBa) directed by the Norwegian Institute of Public Health (www.fhi.no/morogbarn).32 Participants were recruited from all over Norway from 1999–2008, through a postal invitation in connection with a routine ultrasound examination offered to all pregnant women in Norway at about 17–18 weeks of gestation. Of the invited women, 38.5% consented to participate. The cohort includes 108,593 children, 90,504 mothers (with one or more children) and 71,533 fathers. Blood samples were obtained from both parents at inclusion (17/18 weeks) and from mothers and children (umbilical cord) at birth. Follow up is conducted by questionnaires at regular intervals and by linkage to national health registries, such as the Medical Birth Registry of Norway (MBRN).33 Informed consent was obtained from each participant upon recruitment. The study was approved by The Regional Committee for Medical Research Ethics, the Norwegian Data Inspectorate and the Institutional Review Board of the University of North Carolina at Chapel Hill.
The current study is based on version V of the quality-assured data files released for research on May 2010, and we used information from Questionnaire 1 (17/18 weeks gestation), Questionnaire 4 (6 months postpartum), Questionnaire 5 (18 months postpartum) and Questionnaire 6 (36 months postpartum).
We excluded participants who: a) did not have identification information from both MBRN and Questionnaire 1; b) completed an early pilot version of the Questionnaire 1 (n = 2,605); c) had invalid values for either self-reported age, weight, or height; d) returned Questionnaire 1 after delivery; e) had a multiple pregnancy and f) had a stillbirth. If a woman enrolled in MoBa more than once (due to additional pregnancies), only the first pregnancy was included in these analyses. Based on these criteria, 22,152 mother-child records were excluded. Additionally, we excluded women who did not have valid eating disorder information before pregnancy (n = 3,515). Together this constitutes the baseline sample representing 77,807 women. The baseline dataset was then merged with the postpartum files at 18 and 36 months postpartum, respectively. At 18 months, we excluded participants with insufficient information regarding presence or absence of eating disorder subtypes at 18 months postpartum (n = 4,087), participants who became pregnant since the birth of their index child (n = 6,907) or if information regarding pregnancy status at 18 months postpartum were missing (n = 2,184). At 36 months, we excluded participants with insufficient information regarding presence or absence of eating disorder subtypes at 36 months postpartum (n = 1,180), participants who became pregnant again or had given birth since the delivery of their index child (n = 8,833) or if information regarding new pregnancy/delivery at 36 months postpartum were missing (n = 3,318). Becoming pregnant or having another baby in the study period (at 18 or 36 months) was not significantly associated with having an eating disorder at baseline (x2 = 5.3, df = 4, p = 0.26 and x2 = 2.6, df = 4, p = 0.6, respectively). Based on these criteria 35,648 and 23,773 women were eligible for analyses at 18 months and 36 months postpartum, respectively. The loss of participants between baseline at 18 week of pregnancy (questionnaire 1) and 18 months (questionnaire 5) and 36 months postpartum (questionnaire 6), respectively, was not only due to attrition, but primarily due to the fact that MoBa is a longitudinal study that is still in progress. Many women actively enrolled in the investigation had not yet reached the 18- and 36-month post-partum mark and had therefore not yet qualified for this follow-up. Both the rather low participation rate and the somewhat high attrition rate may represent possible threats to the validity of the present findings. These issues are addressed in the limitations section.
Measures
Eating disorders
The items on eating disorder symptoms and behaviors were designed in accordance with the criteria for eating disorders in the Diagnostic and Statistical Manual of Mental Disorders–IV.34 These criteria have previously been used for studies on eating disorders in the MoBa sample1, 6, 35 and in the Norwegian Institute of Public Health Twin Panel36–38 and yield point prevalence estimates similar to those found in one other Norwegian population-based sample.39 Furthermore, other studies based on these criteria have found similar heritability estimates as interview-based assessment,38, 40 and participants who endorse these criteria41 have been found to also endorse comorbid psychiatric diagnoses in MoBa as well as other samples.8, 42, 43 Diagnostic algorithms were constructed from the questionnaire items to define AN, BN, EDNOS-P, and BED at the following time points: pre-pregnancy (“the 6 months period before pregnancy” measured retrospectively at 18 weeks of gestation), during pregnancy (“now” measured at 18 weeks of gestation), 18 months after delivery (“the last 6 months” measured at 18 months after delivery), and 36 months after delivery (“the last 18 months” measured at 36 months after delivery). AN was not assessed during pregnancy due to difficulties in determining the low weight criterion due to pregnancy related weight gain.
Due to slight differences in response alternatives across questionnaires, the frequency criterion for the core eating disorder behaviors were consistent with the DSM-IV criteria (e.g., two times a week) in the postpartum period, but were only required to occur once a week before and during pregnancy (i.e., broadly defined eating disorders). This means that more eating disorder symptomatology was necessary to be categorized as having BN, EDNOS-P, and BED after pregnancy than before. Before pregnancy our categories included: broadly defined AN (amenorrhea not required), broadly defined BN (at least weekly frequency of binge eating and compensatory behaviors such as vomiting, laxatives, excessive exercise, or fasting), broadly defined EDNOS–P (purging at least weekly in the absence of binge eating), and broadly defined BED (at least weekly frequency of binge eating in the absence of compensatory behaviors).
The eating disorder subtypes comprised mutually exclusive categories of AN, BN, EDNOS-P and BED at each time point and “missing”. If an individual had a missing response on one criterion but scored positively on all other criteria for a diagnosis, a classification of missing was assigned. A negative value on at least one criterion for a specific eating disorder indicated no such eating disorder.
Postpartum course
We described the course of continuation, remission, subthreshold, crossover, and incidence at 18 months postpartum. Continuation refers to women who fulfilled the criteria for the same eating disorder both before pregnancy and at 18 months postpartum. Remission described women who fulfilled the criteria for an eating disorder before pregnancy, and reported no eating disorder as well as no core eating disorder behaviors at 18 months postpartum. For BN, for example, this would mean no other eating disorder and no binge eating or compensatory behaviors at 18 months postpartum. Subthreshold refers to those with an eating disorder before pregnancy and still reporting the core eating disorders behaviors of this eating disorder at a reduced frequency of 1 – 4 times a month 18 months postpartum. In this category, the eating disorder continues, but to a lesser extent than captured by the full diagnostic criteria. Crossover refers to women who meet full or subthreshold criteria for a different eating disorder at 18 months postpartum than at pre-pregnancy. Remission, continuation, subthreshold and crossover were defined similarly at 36 months postpartum.
BMI and weight retention
Current self-reported weight was measured in each questionnaire. In addition pre- and post-pregnancy weight was retrospectively reported at 18 weeks of gestation and 6 months postpartum, respectively. Height was assessed during pregnancy and used to calculate body mass index (BMI)(kg/m2) at each time point. The difference in weight between pre-pregnancy and delivery was defined as pregnancy related weight gain. The difference between pre-pregnancy weight and weight at 6, 18, and 36 months (as continuous change score in kg) was used to define post-pregnancy weight retention at 6, 18, and 36 months, respectively.
Psychological distress and depression
An eight-item version of the Hopkins Symptom Checklist- 25 was used to measure psychological distress (i.e., symptoms of anxiety and depression) at 6, 18 and 36 months postpartum.44 This short form is highly correlated (r = .94) with the original scale45 and has good psychometric properties (Cronbach’s alpha of 0.85, 0.85, and 0.86 at 6, 18, and 36 months postpartum, respectively). Items are scored on a scale ranging from 1 (“not at all bothered”) to 4 (“very much bothered”). The sum score was created by adding the scores on all items and dividing by the number of items.
For the assessment of lifetime history of major depression we used an approach designed for self-report purposes.46 Individuals reported the occurrence of five key depressive symptoms for more than two weeks (felt depressed or sad, had problems with appetite or eaten too much, been bothered by lack of energy, blamed yourself and felt worthless, had problems with concentration or had problems making decisions). They were then asked if any of three of these symptoms co-occurred. Individuals who responded positively to this item were considered to have had a lifetime history of major depression.
In Questionnaire 4 (6 months postpartum) women responded to a dichotomous question about postpartum mood (“when you think back to the time just after the birth, did you feel depressed during that period?).
Partner satisfaction
Satisfaction with partner relationship was assessed at 6 and 18 months postpartum using the Relationship Satisfaction Scale, a 10-item scale developed for the MoBa study but partially based on the Marital Satisfaction Scale.47 Preliminary analyses have shown a high correlation with the Quality of Marriage Index.48, 49 The scale has good internal consistency, with Cronbach’s alpha of 0.92 and 0.93 at 6, and 18 months postpartum, respectively. Each item was scored from 1 (“strongly disagree”) to 6 (”strongly agree”). The sum score was created by adding the scores on all items and dividing by the number of items.50 In Questionnaire 6 (36 month postpartum) only a short version with 5 items was used. This short version shows a correlation with the 10 item version of 0.85 (based on data from Questionnaire 1 during pregnancy) and the Cronbach’s alpha is 0.90.
Demographic and other variables
Demographic data were obtained both from Questionnaire 1 (during pregnancy) and MBRN including parity (number of previous live births), maternal age (at child’s birth), years of maternal education (in pregnancy), and partnered status.
Statistical analysis
Means, standards deviations, percentages and counts were calculated for descriptive background characteristics across eating disorder status before pregnancy. A modified Poisson regression model51, 52 was used as a general approach for the three analytical goals. A justification of its usage follows below.
First, we estimated the proportion of continuation, remission, subthreshold and crossover of eating disorders at 18 months postpartum, in women with pre-pregnancy eating disorders. Second, following the same procedure, we estimated the proportion of women with continuation, remission, subthreshold and crossover at 18 months postpartum in women with pregnancy onset of BED. All examined proportions were calculated by including only the respective response in the regression model (i.e., with no predictors) and estimating the intercepts only. Third, we explored predictors of course of BN and BED at 18 months postpartum in women with pre-pregnancy BN and BED, respectively. This was not performed for AN or EDNOS-P due to the low prevalence of these disorders. We included each predictor separately in the continuation, remission, subthreshold and crossover models, and estimated the relative risk (RR) for the postpartum course for BN and BED, respectively. These analyses were conducted with and without adjusting for age and education. Lastly, all the analyses were repeated for each course at 36 months.
Given that Poisson regression provides direct estimates of relative risk this was the preferable choice compared to logistic regression and odds ratio estimates. However, a Poisson regression model applied to binary data (without adjustments) provides conservative results by overestimating the standard error for the estimated relative risk. To remove this bias, we used a robust variance estimator as suggested by Zou51 and Carter52.
In the regression models, most of the predictors were entered as continuous variables. They are scaled differently and the estimated RRs reflect the effect of one unit change in the respective variable and cannot be directly compared. Given the large numbers of tests conducted, we used the Benjamin-Hochberg method to control for the false discovery rate (FDR).53 Together, the covariates in the models for BN and BED at the two postpartum time points (18 and 36 months postpartum) constituted four families of hypothesis and were FDR-adjusted accordingly. For the continuous scale variables, we used SPSS Missing Value Analysis (MVA), Expectation Maximization (EM). Generally, the missing proportion on specific items was low and we imputed missing values when half or more of the items on the respective scale had been reported. All analyses were performed with SPSS for Windows (Version 17.0, SPSS, Chicago).
RESULTS
Sample demographics
The baseline population in this study included 77,807 pregnant women with a mean age of 30.0 years, 53.3% were primiparous, 95.7% were married or cohabiting and 63.6% had attended some form of college. Population characteristics across pre-pregnancy eating disorder status are shown in Table 1.
Table 1.
Maternal characteristics across eating disorders subtypes before pregnancy presented as N (%) or mean (SD)
| AN (n = 72) |
BN (n = 672) |
EDNOS-P (n = 92) |
BED (n = 2,698) |
No-ED (n = 74,273) |
Total sample (n = 77,807) |
|
|---|---|---|---|---|---|---|
| Mean age | 26.3 (5.0) | 29.1 (4.7) | 27.5 (5.6) | 30.0 (4.7) | 30.0 (4.7) | 30.0 (4.7) |
| Partnered status | ||||||
| Married /cohab. | 67 (93.1) | 618 (92.4) | 68 (74.7) | 2,584 (96.1) | 70,758 (95.8) | 74,095 (95.7) |
| other | 5 (6.9) | 51 (7.6) | 23 (25.3) | 106 (3.9) | 3,131 (4.2) | 3,316 (4.3) |
| Education | ||||||
| < 3 years high school | 13 (19.7) | 75 (12.0) | 22 (25.9) | 291 (11.4) | 5,499 (7.8) | 5,900 (8.0) |
| Vocational high school | 14 (21.2) | 99 (15.8) | 14 (16.5) | 456 (17.8) | 9,221 (13.1) | 9,804 (13.3) |
| 3-year high school | 15 (22.7) | 118 (8.8) | 14 (16.5) | 455 (17.8) | 10,525 (15.0) | 11,127 (15.1) |
| Regional technical college/4-year university degree | 12 (18.2) | 221 (35.3) | 27 (31.8) | 948 (37.0) | 28,630 (40.8) | 29,838 (40.6) |
| University or technical college, < 4 years | 12 (18.2) | 113 (18.1) | 8 (9.4) | 409 (16.0) | 16,370 (23.3) | 16,912 (23.0) |
| Parity | ||||||
| 0 | 49 (68.1) | 370 (55.3) | 55 (60.4) | 1,298 (48.3) | 39,677 (53.7) | 41,449 (53.3) |
| 1 | 16 (22.2) | 190 (28.4) | 19 (20.9) | 860 (32.0) | 21,620 (29.3) | 22,705 (29.3) |
| 2 | 4 (5.6) | 88 (13.2) | 11 (12.1) | 399 (14.8) | 9865 (13.4) | 10,367 (13.4) |
| 3 | 2 (2.8) | 15 (2.2) | 5 (5.5) | 98 (3.6) | 2118 (2.9) | 2,238 (2.9) |
| 4+ | 1 (1.4) | 6 (0.9) | 1 (1.1) | 35 (1.3) | 609 (0.8) | 652 (0.8) |
AN, Anorexia Nervosa; BN, Bulimia Nervosa; EDNOS-P, Eating Disorders Not Otherwise Specified- Purging disorder; BED, Binge Eating Disorder; ED, Eating Disorder
Prevalence of eating disorders
Table 2 shows the prevalence of eating disorders before, during and after pregnancy. Before pregnancy, the proportions of women who met criteria for an eating disorder were: 0.1% (n = 72) for AN, 0.9% (n = 672) for BN, 0.1% (n = 92) for EDNOS-P, and 3.5% (n = 2,698) for BED.
Table 2.
Prevalence of eating disorders before and during pregnancy and at 18 and 36 months postpartum
| ANa n (%) | BN n (%) | EDNOS-P n (%) | BED n (%) | No-ED n (%) | |
|---|---|---|---|---|---|
| Before pregnancy1 | 72 (0.1) | 672 (0.9) | 92 (0.1) | 2,698 (3.5) | 74,273 (95.5) |
| During pregnancy1 | - | 183 (0.2) | 20 (<0.1) | 3,180 (4.3) | 70,032 (95.3) |
| 18 months postpartum2 | 72 (0.2) | 245 (0.7) | 18 (0.1) | 962 (2.7) | 31,277 (88.0) |
| 36 months postpartum2 | 58 (0.2) | 222 (0,9) | 22 (0.1) | 740 (3.1) | 19,932 (83.9) |
AN, Anorexia Nervosa; BN, Bulimia Nervosa; EDNOS-P, Eating Disorders Not Otherwise Specified- Purging disorder; BED, Binge Eating Disorder; ED, Eating Disorder
No amenorrhea required
Frequency of core eating disorders behaviors required are minimum once a week
Frequency of core eating disorders behaviors required are minimum twice a week
Postpartum course
18 months postpartum
Table 3 presents course of eating disorders at 18 months postpartum (proportions with 95% confidence interval [CI]) for individual with pre-pregnancy eating disorders and those with BED with onset during pregnancy. The proportions of women remitting at this time point were: 50% for AN (CI: 35% – 72%), 39% for BN (CI: 33% – 45%), 46% for EDNOS-P (CI: 32% – 66%), and 45% for BED (CI: 43% – 48%). For all eating disorders a substantial proportion continued with disordered eating, with either the same eating disorder as before pregnancy (i.e., continuation), continued with partial symptoms (i.e., subthreshold) or migration to another eating disorders than at baseline (i.e., crossover). Among women with onset of BED during pregnancy, 66% reported remission at 18 months postpartum (CI: 63% – 70%).
Table 3.
Course of eating disorders from pre-pregnancy and pregnancy to 18 months postpartum reported in proportions with 95% confidence intervals (CI)
| Pre-pregnancy onset |
Pregnancy onset |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| AN | BN | EDNOS-P | BED | BED | ||||||
| Course | Proportiona | 95% CI | Proportiona | 95% CI | Proportiona | 95% CI | Proportiona | 95% CI | Proportiona | 95% CI |
| Continuation | (11/30) 0.37 | 0.23–0.59 | (36/261) 0.14 | 0.10–0.19 | (5/36) 0.14 | 0.06–0.31 | (255/1210) 0.21 | 0.19–0.24 | (56/621) 0.09 | 0.07–0.12 |
| Remission | (15/30) 0.50 | 0.35–0.72 | (99/255) 0.39 | 0.33–0.45 | (16/35) 0.46 | 0.32–0.66 | (546/1208) 0.45 | 0.43–0.48 | (408/616) 0.66 | 0.63–0.70 |
| Subthreshold | (64/225) 0.25 | 0.20–0.31 | (5/35) 0.14 | 0.06–0.32 | (282/1208) 0.23 | 0.21–0.26 | (90/616) 0.15 | 0.12–0.18 | ||
| Crossover | (4/30) 0.13 | 0.05–0.33 | (56/255) 0.22 | 0.17–0.28 | (9/35) 0.26 | 0.15–0.45 | (125/1208) 0.10 | 0.09–0.12 | (62/616) 0.10 | 0.08–0.13 |
AN, Anorexia Nervosa; BN, Bulimia Nervosa; EDNOS-P, Eating Disorders Not Otherwise Specified- Purging disorder; BED, Binge Eating Disorder.
In the numerator we report the numbers in each course and in the denominator the total number of women with this eating disorder. The sum of the proportions does not equal exactly one due to differences in missing on the items required for each course.
36 months postpartum
Table 4 presents course of eating disorders at 36 months postpartum (proportions with 95% CI). The proportions of women in remission were 59% for AN (CI: 40% – 88%), 30% for BN (CI: 23% – 37%), 57% for EDNOS-P (CI: 40% – 81%), and 42% for BED (CI: 39% – 46%). Nonetheless, also at this time point a substantial proportion continued with disordered eating, either as continuation, subthreshold, or crossover. Among the women with onset of BED during pregnancy, 57% reported remission at 36 months postpartum (CI: 52% – 62%).
Table 4.
Course at eating disorders from pre-pregnancy and pregnancy to at 36 months postpartum reported in proportions with 95% confidence intervals (CI)
| Pre-pregnancy onset |
Pregnancy onset |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| AN | BN | EDNOS-P | BED | BED | ||||||
| Course | Proportiona | 95% CI | Proportiona | 95% CI | Proportiona | 95% CI | Proportiona | 95% CI | Proportiona | 95% CI |
| Continuation | (5/17) 0.29 | 0.14–0.61 | (31/166) 0.19 | 0.14–0.26 | (2/23) 0.09 | 0.02–0.33 | (161/774) 0.21 | 0.18–0.24 | (42/402) 0.10 | 0.08–0.14 |
| Remission | (10/17) 0.59 | 0.40–0.88 | (49/166) 0.30 | 0.23–0.37 | (13/23) 0.57 | 0.40–0.81 | (328/773) 0.42 | 0.39–0.46 | (226/400) 0.57 | 0.52–0.62 |
| Subthreshold | (54/166) 0.33 | 0.26–0.41 | (3/23) 0.13 | 0.05–0.38 | (176/773) 0.23 | 0.20–0.26 | (62/400) 0.16 | 0.12–0.20 | ||
| Crossover | (2/17) 0.12 | 0.03–0.43 | (32/166) 0.19 | 0.14–0.26 | (5/23) 0.22 | 0.10–0.47 | (108/773) 0.14 | 0.12–0.17 | (70/400) 0.18 | 0.14–0.22 |
AN. Anorexia Nervosa; BN. Bulimia Nervosa; EDNOS-P. Eating Disorders Not Otherwise Specified- Purging disorder; BED. Binge Eating Disorder.
In the numerator we report the numbers in each course and in the denominator the total number of women with this eating disorder. The sum of the proportions does not equal exactly one due to differences in missing on the items required for each course
Predictors of postpartum course
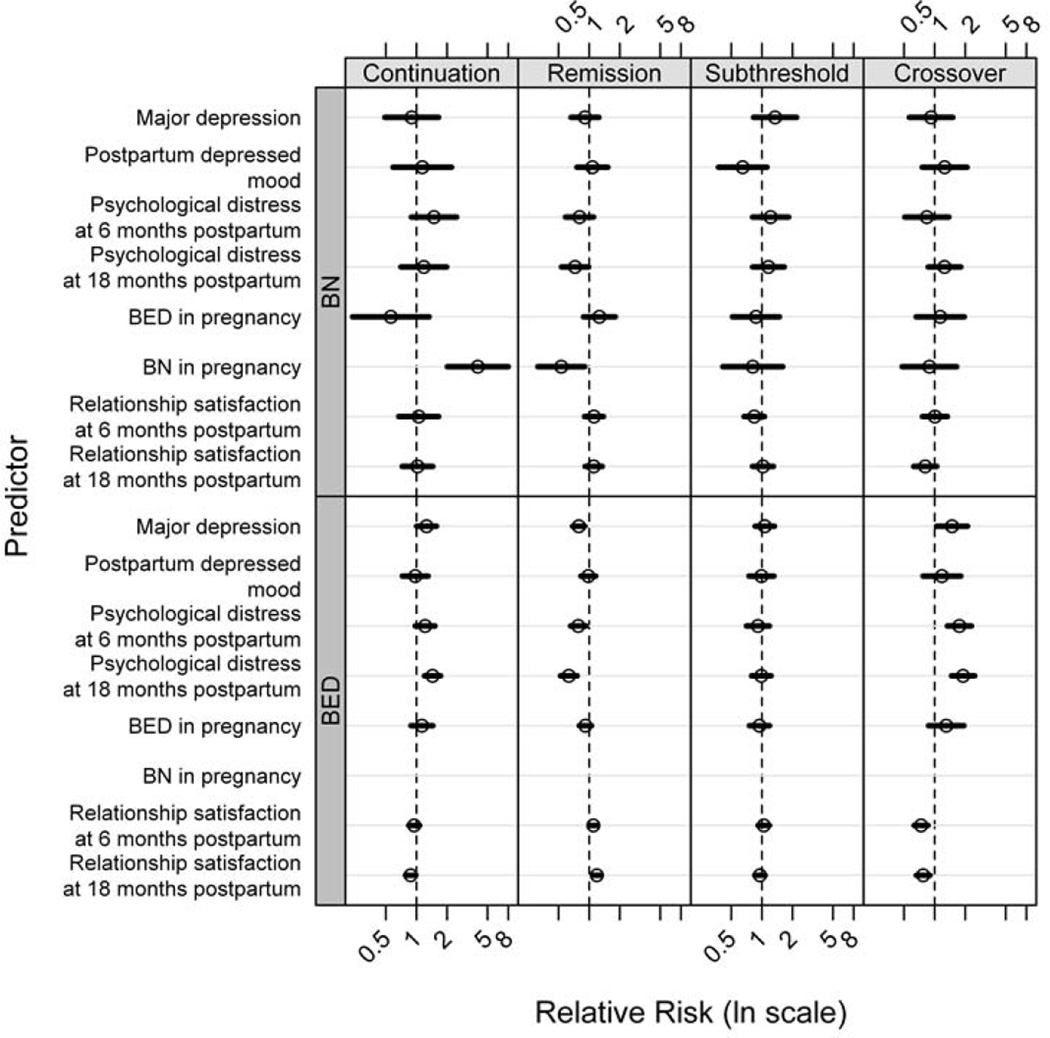
We tested whether BMI (before pregnancy, 6, 18, and 36 months postpartum) and weight retention (at birth, 6, 18, and 36 months postpartum) psychological distress (6, 18, and 36 months postpartum), relationship satisfaction (6, 18, and 36 months postpartum), postpartum depressed mood, presence of BED in pregnancy, and presence of BN in pregnancy (for BN only) were associated with course of BN and BED at 18 and 36 months postpartum. The results from all the factors tested are presented in Figure 1–4. Figures 1 and 3 present weight-related factors associated with course (i.e., continuation, remission, subthreshold, and crossover) of BN and BED at 18 and 36 months postpartum, respectively. Figure 2 and 4 present psychosocial factors associated with each specific course of BN and BED at 18 and 36 months postpartum, respectively. In the text below, we report all of the relative risks estimates, adjusted for age and education, that remained significant after FDR adjustment (FDR p < 0.05).
Figure 1.
The association between weight-related factors and course (continuation, remission, subthreshold and crossover) of BN and BED at 18 months postpartum, respectively, presented as relative risk (dots) with confidence intervals (lines) in ln scale.
Figure 2.
The association between psychosocial factors and course (continuation, remission, subthreshold and crossover) of BN and BED at 18 months postpartum, respectively, presented as relative risk (dots) with confidence intervals (lines) in ln scale.
Figure 3.
The association between weight-related factors and course (continuation, remission, subthreshold and crossover) of BN and BED at 36 months postpartum, respectively, presented as relative risk (dots) with confidence intervals (lines) in ln scale.
Figure 4.
The association between psychosocial factors and course (continuation, remission, subthreshold and crossover) of BN and BED at 36 months postpartum, respectively, presented as relative risk (dots) with confidence intervals (lines) in ln scale.
The presence of BN in pregnancy, increased the risk for continuation of BN at 18 and 36 months postpartum (adjusted RR = 4.3, FDR p < 0.006 and adjusted RR = 3.3, FDR p < 0.024, respectively) (Figure 2 and 4). Psychological distress at 6 and 36 months postpartum were positively associated with continuation of BN at 36 months postpartum (adjusted RR = 1.99, FDR p < 0,024 and adjusted RR = 2.07, FDR p < 0.001, respectively) (Figure 4).
BMI (before pregnancy, 6, 18 and 36 months after delivery) were associated with course of BED at 18 and 36 months postpartum (Figure 1 and 3). Specifically, BMI (at all time points) was positively associated with continuation of BED (adjusted RRs between 1.04 – 1.07, FDR p<0.004) and negatively associated with remission of BED (adjusted RR between 0.96–0.97, FDR p < 0.028) at 18 and 36 months postpartum.
Pregnancy related weight gain was positively associated with crossover of BED at 18 months postpartum (adjusted RR = 1.03, FDR p <0.044) and negatively associated with continuation of BED at 36 months postpartum (adjusted RR = 0.97, FDR p < 0.025) (Figure 1 and 3). Weight retention at 6 months postpartum was positively associated with BED crossover at 18 months postpartum (adjusted RR = 1.03, FDR p <0.028). Weight retention at 18 months postpartum was positively associated with continuation of BED at 18 months postpartum (adjusted RR = 1.02, FDR p <0.035) (Figure 1). Weight retention at 36 months postpartum was positively associated with continuation of BED and negatively associated with remission of BED at 36 months postpartum (adjusted RR = 1.02, FDR p <0.009 and adjusted RR = 0.99, FDR p <0.025, respectively) (Figure 3).
Psychological distress at 6 months postpartum was negatively associated with remission of BED and positively associated with BED crossover at 18 months postpartum (adjusted RR = 0.78, FDR p < 0.02 and adjusted RR = 1.8, FDR p < 0.004, respectively). Psychological distress at 18 months was positively associated with continuation and crossover of BED (adjusted RR = 1.45, FDR p < 0.004 and adjusted RR = 1.90, FDR p < 0.004, respectively), and negatively associated with remission of BED at 18 months postpartum (adjusted RR = 0.63, FDR p < 0.004) (Figure 2). Psychological distress at 36 months was positively associated with BED crossover at 36 months postpartum (adjusted RR = 1.54, FDR p < 0.015) (Figure 4). Lifetime depression was negatively associated with remission of BED at 18 months postpartum (adjusted RR = 0.79, FDR p < 0.004) (Figure 2).
Partner relationship satisfaction at 6 months postpartum was negatively associated with BED crossover at 18 months postpartum (adjusted RR = 0.74, FDR p < 0.004). Relationship satisfaction at 18 months postpartum was positively associated with remission of BED at 18 months postpartum (adjusted RR = 1.19, FDR p < 0.004) and negatively associated with BED crossover BED (adjusted RR =0.77, FDR p < 0.004) (Figure 2). Further, relationship satisfaction at 36 months postpartum was negatively associated with continuation of BED at 36 months postpartum (RR = 0.81, FDR p < 0.009) (Figure 4).
DISCUSSION
To the best of our knowledge, this is the first, large-scale, population-based study exploring course and predictors of eating disorders in the postpartum period. There are three main findings that will be discussed consecutively.
Course of eating disorders in the postpartum period
The point prevalence of pre-pregnancy eating disorders in our sample is commensurate with reports for BN, but somewhat lower than reports for AN, and somewhat higher than for BED in epidemiological studies on non-pregnant samples in Norway.39
Generally, many patterns were observed at both postpartum time points. However, due to small numbers, the confidence intervals were wide for AN and EDNOS-P, with proportions of women in remission not significantly different from the proportions in continuation.
For BN, the proportions of women remitted were approximately 40% and 30% at 18 and 36 months postpartum, respectively. These results are in accordance with what has been reported from the few clinical studies on postpartum course of BN. In one retrospective study of 94 women with BN at conception, Morgan et al11 reported that one third of women no longer met criteria for bulimia in the postpartum period and 4% had improved clinically. In another retrospective study of 20 women with BN, one third remitted in pregnancy, although nearly half reported more disturbed eating after delivery than before conception.9
The remission proportions for BED were 45% and 42% for 18 and 36 months, respectively, i.e., slightly higher than the comparative remission rates for BN. There are no studies on course of BED in the postpartum period with which we can compare these results. However they appear to differ from findings reported in the few studies investigating course of BED in non-pregnant community based samples. Fairburn et al.54 reported a higher remission rate in a community sample of 48 women with BED over a 5-year period. In contrast, Cachelin et al55 reported greater stability (i.e., lower remission rate) in a small community sample of 31 women with BED followed for 6 months.
Most of the studies, with a few exceptions,10 investigating eating disorder attitudes and behaviors dimensionally in population-based18, 20, 56 or clinical samples 7, 9, 11 have reported decreased symptomatology during pregnancy, followed by an increase to pre-pregnancy levels in the postpartum period. However, a direct comparison of these finding with ours is not meaningful, given that we also explored migration across diagnostic categories. In the population-based studies mentioned above, normal variations in disordered eating and attitudes were explored, and they include few,56 or no18, 20 women who meet the diagnostic criteria for AN or BN. However, compared with the clinical studies mentioned above7, 9, 11 we report lower rates of women who continue with eating disorders in the postpartum period. This observation could indicate that the postpartum course of eating disorders is more favorable in the general population than in clinical samples and reflect the fact that individuals who seek therapy often have more serious disorders and a higher rate of comorbidity.57
Overall, when the proportions of the different postpartum outcomes are being compared, with the exception of BN at 36 months, remission was the most typical postpartum course for women with pre-pregnancy eating disorders across subtypes. This may indicate that pregnancy can have a persistent positive effect for some women with eating disorders. Although speculative, this would be in line with previous studies that have proposed a general positive effect of becoming a mother on eating disorder symptoms.18, 20, 58, 59 In one population based study on young women, a greater reduction in eating disorder symptoms was found in women who became mothers compared to the ones who remained childless.58 Similarly, childbirth was not associated with increased symptomatology following treatment for BN.59
A substantial proportion of women continued to fulfil criteria for an eating disorder in the postpartum period. On-going eating disorders may interfere with maternal adjustment60 increasing the risk for postpartum depression2, 26 and interfering with breastfeeding61 and feeding behaviors62 such as using food for non-nutritive purposes63 having detached and non-interactive mealtimes64 and being more concerned about their daughter’s weight.63 These variables are important to acknowledge and underscore the importance of detection and intervention for mothers with eating disorders in order to provide them with treatment and tools for both general parenting and parenting around eating-related themes.
Course of pregnancy onset of BED
For women with the first onset of BED during pregnancy, the proportion remitting was significantly higher and the proportion continuing was significantly lower, than women with BED onset before pregnancy. Previously we have found that correlates and risk factors for BED that onsets during pregnancy are similar to BED with a non-pregnancy onset.8 However, the more transient symptom presentation of BED that emerges during pregnancy supports the hypothesis that particular changes related to pregnancy are operative in increasing risk for BED in this period. Several social, psychological and biological changes, such as the myriad neuroendocrine changes that affect bodily functions influencing metabolism, appetite, and mood,65, 66 may be important in understanding this elevated risk for BED onset in pregnancy.
BED in pregnancy is associated with dietary patterns of increased fat and sugar intake,35 higher gestational weight gain,1, 67 and risk for large for gestational age babies.1 As a first step to ensure a healthy diet throughout pregnancy, enhancing dietary counselling during pregnancy is a worthwhile consideration.
Predictors of postpartum course
We found that the presence of BN in pregnancy increased the risk for continuation of BN in the postpartum period approximately fourfold. Previously, our research group has shown that only a minority of women with pre-pregnancy BN continue to meet criteria for BN when they enter pregnancy.6 Women, who continue both binge eating and compensatory behaviors despite being pregnant, may have a more severe form of BN characterized by a long-lasting course with symptoms that persist into the postpartum period.
Although postpartum weight retention has been suggested to play an important role in explaining relapse of eating disorders in the postpartum period,17–20 this was not supported for BN in the present study. Weight retention was not significantly associated with postpartum course of BN. However, it is possible that concern about weight retention postpartum is more relevant to the course of eating disorders postpartum than the actual weight retention itself. Unfortunately, this was not measured in the present study.
Higher BMI was positively associated with continuation of BED and negatively associated with remission of BED at 18 and 36 months postpartum. Although BED in general is associated with high weight and BMI,42, 68–70 BED also occurs in individuals of normal weight.71 We were not able to disentangle the causal relationship between BMI and BED in the present study, and do not know if high BMI is a consequence or antecedent of BED. Continuation of BED may, due to increased energy intake over time, result in high BMI. However, we cannot rule out the possibility that high BMI also influences the probability of BED continuation. Women with higher BMI may be more likely to engage in extreme dieting and rigid food restrictions, behaviors that may result in an increased risk for continuation of binge eating.23
Psychological distress measured at different time points was associated with continuation, remission, and crossover of BED in the postpartum. Psychological distress at 36 months postpartum was associated with continuation of BN at 36 months postpartum. Psychological distress is a known characteristic associated with BED and BN in clinical and population-based samples.42, 69, 72, 73, 74, 75 The strongest association was found between psychological distress and crossover from BED to BN through starting additional compensatory behaviors in the postpartum period. We observed a cross-sectional association between psychological distress and continuation of BED and cannot determine whether psychological distress and BED are causally related or to what extent they are both influenced by other underlying factors. Still, the possibility that binge eating in the postpartum period may serve to regulate negative affect cannot be ruled out.23, 27
Partner relationship satisfaction was associated with BED course in the postpartum period. Previous research has found marital functioning to be associated with BED76 and interpersonal problems have been found to be a predictor of poor outcome in BED.77
Limitations
Although the present study has several strengths there are also limitations. First, the majority of data were collected from self-reported measures. Although the items used to determine the diagnosis of eating disorders have been used in other epidemiologic studies in Norway,36, 38, 42 structured interviews may have provided more accurate diagnostic information on eating disorders.78 However, this procedure is complex, time consuming and prohibitively expensive rendering it impractical in samples as large as MoBa. Additional support for self-report of stigmatized behaviors comes from recent research indicating that when measuring unwanted behaviours including purging in population based settings, some women will deny previously self-reported behaviours in subsequent interviews.79 This indicates that self-report may actually have advantages over clinical interviews in the case of sensitive information. The accuracy of self-reported weight has also been discussed,80–83 and an objective measure would have been optimal but impractical in samples as large as MoBa. Second, the frequency criterion used to assess the core eating disorder behaviors (i.e., binge eating and compensatory behaviors) was once a week before pregnancy and twice a week or more in the postpartum period. Due to these differences, direct comparisons of the prevalence estimates are not meaningful. However, since we used “no core eating disorders behaviors present” as a definition of remission at 18 and 36 months postpartum, this will not affect our remission estimates. To ensure that all women who continued with some form of pathological eating postpartum were included, we used subthreshold eating disorder as a separate postpartum course. Third, eating disorder status prior to pregnancy was retrospectively reported, but given the limited time delay until assessment, the impact of retrospective recall bias should be minimal. For participants with AN, we cannot rule out the possibility that some of their responses may be inaccurate due to the cognitive distortions associated with the illness that result in an underestimation or denial of existing problems. Fourth, of the invited women, 38.5% agreed to participate in MoBa. Although somewhat low, this is not unusual for epidemiological studies and does not necessarily imply a biased sample.32, 84 Initial comparisons of the MoBa cohort to the Norwegian population indicate lower rates of preterm births (7.2 vs 7.7%) and low birth weights (4.6% vs 5.1%) among participants.32 Participants are more educated, with approximately 61% attending some form of college compared with 49% in the general female population between 25 and 29 years of age and 46% between 30 and 39 years of age reported to have attained a tertiary level of education (i.e., college or university) by Statistics Norway in 2007 (http://www.ssb.no/utniv_en/). This reflects a social gradient associated with participation. The low participation rate may have biased the prevalence estimates, most likely downwards. It is important to bear in mind that selection bias does not necessarily influence the results regarding courses and the associations between variables.32, 85 Fifth, the follow up participation rate was 72.4% at 18 months and 58.5% at 36 months for the complete MoBa cohort (in Sept 2011). We cannot rule out the possibility that women who dropped out of the study continued with eating disordered behaviors to a greater extent than the women who continued to participate. Hypothetically, this could result in an overestimation of the remission rates and underestimation of the continuation rates. Unfortunately, detailed information from the women lost to follow up was not available.
Implications
Although, some women experienced remission of their initial eating disorder postpartum, there were a substantial proportion of new mothers who continued with an eating disorder in the postpartum period, despite pregnancy, childbirth and the new life circumstances involving taking care of a newborn. Many women do not disclose their eating disorder during pregnancy and postpartum86 and it is important for health-care professionals working with pregnant women and new mothers to be trained in how to recognize eating disorder symptoms and behaviors. Detection is a critical first step in implementing adequate interventions. This is important in itself and could also possibly interrupt the trans-generational “cycle of risk” hypothesized to be associated with eating disorders87, 88.
Acknowledgements
Supported by National Institutes of Health grants HD047186, NO-ES-75558, and 1 U01 NS 047537-01, the Norwegian Ministry of Health and Ministry of Education and Research, and the Norwegian Research Council/FUGE grant 151918/S10. We are grateful to all the participating families in Norway who take part in this ongoing cohort study.
Footnotes
Conflict of interest
All authors declare that they have no conflicts of interest.
References
- 1.Bulik CM, Von HA, Siega-Riz AM, Torgersen L, Lie KK, Hamer RM, et al. Birth outcomes in women with eating disorders in the Norwegian Mother and Child cohort study (MoBa) Int J Eat Disord. 2009;42:9–18. doi: 10.1002/eat.20578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Franko DL, Blais MA, Becker AE, Delinsky SS, Greenwood DN, Flores AT, et al. Pregnancy complications and neonatal outcomes in women with eating disorders. Am J Psychiatry. 2001;158:1461–1466. doi: 10.1176/appi.ajp.158.9.1461. [DOI] [PubMed] [Google Scholar]
- 3.Koubaa S, Hallstrom T, Lindholm C, Hirschberg AL. Pregnancy and neonatal outcomes in women with eating disorders. Obstet Gynecol. 2005;105:255–260. doi: 10.1097/01.AOG.0000148265.90984.c3. [DOI] [PubMed] [Google Scholar]
- 4.Micali N, Simonoff E, Treasure J. Risk of major adverse perinatal outcomes in women with eating disorders. Br J Psychiatry. 2007;190:255–259. doi: 10.1192/bjp.bp.106.020768. [DOI] [PubMed] [Google Scholar]
- 5.Sollid CP, Wisborg K, Hjort J, Secher NJ. Eating disorder that was diagnosed before pregnancy and pregnancy outcome. Am J Obstet Gynecol. 2004;190:206–210. doi: 10.1016/s0002-9378(03)00900-1. [DOI] [PubMed] [Google Scholar]
- 6.Bulik CM, Von Holle A, Hamer R, Knoph Berg C, Torgersen L, Magnus P, et al. Patterns of remission, continuation and incidence of broadly defined eating disorders during early pregnancy in the Norwegian Mother and Child Cohort Study (MoBa) Psychol Med. 2007;37:1109–1118. doi: 10.1017/S0033291707000724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crow SJ, Agras WS, Crosby R, Halmi K, Mitchell JE. Eating disorder symptoms in pregnancy: a prospective study. Int J Eat Disord. 2008;41:277–279. doi: 10.1002/eat.20496. [DOI] [PubMed] [Google Scholar]
- 8.Knoph Berg C, Torgersen L, Von Holle A, Hamer RM, Bulik CM, Reichborn-Kjennerud T. Factors associated with binge eating disorder in pregnancy. Int J Eat Disord. 2011;44:124–133. doi: 10.1002/eat.20797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lacey JH, Smith G. Bulimia nervosa. The impact of pregnancy on mother and baby. Br J Psychiatry. 1987;150:777–781. doi: 10.1192/bjp.150.6.777. [DOI] [PubMed] [Google Scholar]
- 10.Blais MA, Becker AE, Burwell RA, Flores AT, Nussbaum KM, Greenwood DN, et al. Pregnancy: Outcome and impact on symptomatology in a cohort of eating- disordered women. Int J Eat Disord. 2000;27:140–149. doi: 10.1002/(sici)1098-108x(200003)27:2<140::aid-eat2>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 11.Morgan JF, Lacey JH, Sedgwick PM. Impact of pregnancy on bulimia nervosa. Br J Psychiatry. 1999;174:135–140. doi: 10.1192/bjp.174.2.135. [DOI] [PubMed] [Google Scholar]
- 12.Keel PK, Haedt A, Edler C. Purging disorder: An ominous variant of bulimia nervosa? Int J Eat Disord. 2005;38:191–199. doi: 10.1002/eat.20179. [DOI] [PubMed] [Google Scholar]
- 13.Keel PK, Striegel-Moore RH. The validity and clinical utility of purging disorder. Int J Eat Disord. 2009;42:706–719. doi: 10.1002/eat.20718. [DOI] [PubMed] [Google Scholar]
- 14.Keel PK. Purging disorder: Subthreshold variant or full-threshold eating disorder? Int J Eat Disord. 2007;40:89–94. doi: 10.1002/eat.20453. [DOI] [PubMed] [Google Scholar]
- 15.Fichter MM, Quadflieg N, Hedlund S. Long-term course of binge eating disorder and bulimia nervosa: relevance for nosology and diagnostic criteria. Int J Eat Disord. 2008;41:577–586. doi: 10.1002/eat.20539. [DOI] [PubMed] [Google Scholar]
- 16.Wilfley DE, Wilson GT, Agras WS. The clinical significance of binge eating disorder. Int J Eat Disord. 2003;34:96–106. doi: 10.1002/eat.10209. [DOI] [PubMed] [Google Scholar]
- 17.Franko DL. Eating Disoders in Pregnancy and the Postpartum. In: Hendrick V, editor. Psychiatric Disorders in Pregnancy and the Postpartum: Principles and Treatment. Totowa, NJ: Humana Press; 2006. [Google Scholar]
- 18.Lai BP-Y, Tang CS-K, Tse WK-L. A Longitudinal Study Investigating Disordered Eating during the Transition to Motherhood among Chinese Women in Hong Kong. Int J Eat Disord. 2006;39:303–311. doi: 10.1002/eat.20266. [DOI] [PubMed] [Google Scholar]
- 19.Micali N, Treasure J, Simonoff E. Eating disorders symptoms in pregnancy: a longitudinal study of women with recent and past eating disorders and obesity. J Psychosom Res. 2007;63:297–303. doi: 10.1016/j.jpsychores.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 20.Stein A, Fairburn CG. Eating habits and attitudes in the postpartum period. Psychosom Med. 1996;58:321–325. doi: 10.1097/00006842-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Swann RA, Von Holle A, Torgersen L, Gendall K, Reichbom-Kjennerud T, Bulik CM. Attitudes toward weight gain during pregnancy: Results from the Norwegian mother and child cohort study (MoBa) Int J Eat Disord. 2009;42:394–401. doi: 10.1002/eat.20632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zerwas SC, Von Holle A, Perrin EM, Skinner AC, Reba-Harrelson L, Hamer R, Stoltenberg C, et al. Gestational and postpartum weight change patterns in mothers with eating disorders. 2012 doi: 10.1002/erv.2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Polivy J, Herman CP. Dieting and binging. A causal analysis. Am Psychol. 1985;40:193–201. doi: 10.1037//0003-066x.40.2.193. [DOI] [PubMed] [Google Scholar]
- 24.Micali N, Treasure J. Biological effects of a maternal ED on pregnancy and foetal development: a review. Eur Eat Disord Rev. 2009;17:448–454. doi: 10.1002/erv.963. [DOI] [PubMed] [Google Scholar]
- 25.Morgan JF, Lacey JH, Chung E. Risk of postnatal depression, miscarriage, and preterm birth in bulimia nervosa: retrospective controlled study. Psychosom Med. 2006;68:487–492. doi: 10.1097/01.psy.0000221265.43407.89. [DOI] [PubMed] [Google Scholar]
- 26.Mazzeo SE, Slof-Op't Landt MC, Jones I, Mitchell K, Kendler KS, Neale MC, et al. Associations among postpartum depression, eating disorders, and perfectionism in a population-based sample of adult women. Int J Eat Disord. 2006;39:202–211. doi: 10.1002/eat.20243. [DOI] [PubMed] [Google Scholar]
- 27.McCarthy M. The thin ideal, depression and eating disorders in women. Behav Res Ther. 1990;28:205–215. doi: 10.1016/0005-7967(90)90003-2. [DOI] [PubMed] [Google Scholar]
- 28.Hilbert A, Tuschen-Caffier B. Maintenance of binge eating through negative mood: a naturalistic comparison of binge eating disorder and bulimia nervosa. Int J Eat Disord. 2007;40:521–530. doi: 10.1002/eat.20401. [DOI] [PubMed] [Google Scholar]
- 29.Hoek HW, van HD. Review of the prevalence and incidence of eating disorders. Int J Eat Disord. 2003;34:383–396. doi: 10.1002/eat.10222. [DOI] [PubMed] [Google Scholar]
- 30.Fairburn CG, Welch SL, Norman PA, O'Connor ME, Doll HA. Bias and bulimia nervosa: how typical are clinic cases? Am J Psychiatry. 1996;153:386–391. doi: 10.1176/ajp.153.3.386. [DOI] [PubMed] [Google Scholar]
- 31.Wilfley DE, Pike KM, Dohm FA, Striegel-Moore RH, Fairburn CG. Bias in binge eating disorder: how representative are recruited clinic samples? J Consult Clin Psychol. 2001;69:383–388. doi: 10.1037//0022-006x.69.3.383. [DOI] [PubMed] [Google Scholar]
- 32.Magnus P, Irgens LM, Haug K, Nystad W, Skjaerven R, Stoltenberg C, et al. Cohort profile: The Norwegian Mother and Child Cohort Study (MoBa) Int J Epidemiol. 2006;35:1146–1150. doi: 10.1093/ije/dyl170. [DOI] [PubMed] [Google Scholar]
- 33.Irgens LM. The Medical Birth Registry of Norway. Epidemiological research and surveillance throughout 30 years. Acta Obstet Gynecol Scand. 2000;76:435–439. [PubMed] [Google Scholar]
- 34.APA. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC, US: American Psychiatric Publishing; 1994. [Google Scholar]
- 35.Siega-Riz AM, Haugen M, Meltzer HM, Von HA, Hamer R, Torgersen L, et al. Nutrient and food group intakes of women with and without bulimia nervosa and binge eating disorder during pregnancy. Am J Clin Nutr. 2008;87:1346–1355. doi: 10.1093/ajcn/87.5.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reichborn-Kjennerud T, Bulik CM, Kendler KS, Roysamb E, Maes H, Tambs K, et al. Gender differences in binge-eating: a population-based twin study. Acta Psychiatr Scand. 2003;108:196–202. doi: 10.1034/j.1600-0447.2003.00106.x. [DOI] [PubMed] [Google Scholar]
- 37.Reichborn-Kjennerud T, Bulik CM, Kendler KS, Roysamb E, Tambs K, Torgersen S, et al. Undue Influence of Weight on Self-Evaluation: A Population-Based Twin Study of Gender Differences. Int J Eat Disord. 2004;35:123–132. doi: 10.1002/eat.10252. [DOI] [PubMed] [Google Scholar]
- 38.Reichborn-Kjennerud T, Bulik CM, Tambs K, Harris JR. Genetic and Environmental Influences on Binge Eating in the Absence of Compensatory Behaviors: A Population-Based Twin Study. Int J Eat Disord. 2004;36:307–314. doi: 10.1002/eat.20047. [DOI] [PubMed] [Google Scholar]
- 39.Gotestam KG, Agras WS. General population-based epidemiological study of eating disorders in Norway. Int J Eat Disord. 1995:119–126. doi: 10.1002/1098-108x(199509)18:2<119::aid-eat2260180203>3.0.co;2-u. 1995. [DOI] [PubMed] [Google Scholar]
- 40.Javaras KN, Laird NM, Reichborn-Kjennerud T, Bulik CM, Pope HG, Jr, Hudson JI. Familiality and heritability of binge eating disorder: results of a case-control family study and a twin study. Int J Eat Disord. 2008;41:174–179. doi: 10.1002/eat.20484. [DOI] [PubMed] [Google Scholar]
- 41.Kendler KS. Toward a scientific psychiatric nosology. Strengths and limitations. Arch Gen Psychiatry. 1990;47:969–973. doi: 10.1001/archpsyc.1990.01810220085011. [DOI] [PubMed] [Google Scholar]
- 42.Reichborn-Kjennerud T, Bulik CM, Sullivan PF, Tambs K, Harris JR. Psychiatric and medical symptoms in binge eating in the absence of compensatory behaviors. Obes Res. 2004;12:1445–1454. doi: 10.1038/oby.2004.181. [DOI] [PubMed] [Google Scholar]
- 43.Knopg Berg C, Bulik CM, Holle AV, Torgersen L, Hamer R, Sullivan P, et al. Psychosocial factors associated with broadly defined bulimia nervosa during early pregnancy: Findings from the Norwegian mother and child cohort study. Aust N Z J Psychiatry. 2008;42:396–404. doi: 10.1080/00048670801961149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tambs K, Moum T. How well can a few questionnaire items indicate anxiety and depression? Acta Psychiatr Scand. 1993;87:364–367. doi: 10.1111/j.1600-0447.1993.tb03388.x. [DOI] [PubMed] [Google Scholar]
- 45.Tambs K. Valg av spørsmål til kortversjoner av etablerte instrumenter. Forslag til fremgangsmåte og noen eksempler. In: Sandanger I, Sørensen T, editors. Ubevisst sjeleliv og bevisst samfunnsliv: psykisk helse i en sammenheng: festskrift til Tom Sørensen på hans 60-årsdag. Nittedal: Universitetet i Oslo Nordkyst psykiatri; 2004. [Google Scholar]
- 46.Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. The lifetime history of major depression in women. Reliability of diagnosis and heritability. Arch Gen Psychiatry. 1993;50:863–870. doi: 10.1001/archpsyc.1993.01820230054003. [DOI] [PubMed] [Google Scholar]
- 47.Blum JS, Mehrabian A. Personality and temperament correlates of marital satisfaction. J Pers. 1999;67:93–125. [Google Scholar]
- 48.Roysamb E, Vitterso J, Tambs K. The relationship satisfaction scale. Reliability, validity and goodness of fit. 2012 [Google Scholar]
- 49.Norton R. Measuring marital quality: A critical look at the dependent variable. J Marriage Fam. 1983;45:141–151. [Google Scholar]
- 50.Rosand GM, Slinning K, Eberhard-Gran M, Roysamb E, Tambs K. Partner relationship satisfaction and maternal emotional distress in early pregnancy. BMC Public Health. 2011;11:161. doi: 10.1186/1471-2458-11-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 52.Carter RE, Lipsitz SR, Tilley BC. Quasi-likelihood estimation for relative risk regression models. Biostatistics. 2005;6:39–44. doi: 10.1093/biostatistics/kxh016. [DOI] [PubMed] [Google Scholar]
- 53.Benjamini Y, Hochberg Y. Controlling the False Discovery Rate - A Practical and Powerful Approach to Multiple Testing. J R Stat Soc Ser B. 1995;57:289–300. [Google Scholar]
- 54.Fairburn CG, Cooper Z, Doll HA, Norman P, O'Connor M. The Natural Course of Bulimia Nervosa and Binge Eating Disorder in Young Women. Arch Gen Psychiatry. 2000;57:659–665. doi: 10.1001/archpsyc.57.7.659. [DOI] [PubMed] [Google Scholar]
- 55.Cachelin FM, Striegel-Moore RH, Elder KA, Pike KM, Wilfley DE, Fairburn CG. Natural course of a community sample of women with binge eating disorder. Int J Eat Disord. 1999;25(1):45–54. doi: 10.1002/(sici)1098-108x(199901)25:1<45::aid-eat6>3.0.co;2-3. 1999. [DOI] [PubMed] [Google Scholar]
- 56.Rocco PL, Orbitello B, Perini L, Pera V, Ciano RP, Balestrieri M. Effects of pregnancy on eating attitudes and disorders: a prospective study. J Psychosom Res. 2005;59:175–179. doi: 10.1016/j.jpsychores.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 57.Bushnell JA, Wells JE, McKenzie JM, Hornblow AR, Oakley-Browne MA, Joyce PR. Bulimia comorbidity in the general population and in the clinic. Psychol Med. 1994;24:1994-611. doi: 10.1017/s0033291700027756. [DOI] [PubMed] [Google Scholar]
- 58.von ST, Wichstrom L. The impact of becoming a mother on eating problems. Int J Eat Disord. 2008;41:215–223. doi: 10.1002/eat.20493. [DOI] [PubMed] [Google Scholar]
- 59.Carter FA, McIntosh VV, Joyce PR, Frampton CM, Bulik CM. Bulimia nervosa, childbirth, and psychopathology. J Psychosom Res. 2003;55:357–361. doi: 10.1016/s0022-3999(02)00641-4. [DOI] [PubMed] [Google Scholar]
- 60.Koubaa S, Hallstrom T, Hirschberg AL. Early maternal adjustment in women with eating disorders. Int J Eat Disord. 2008;41:405–410. doi: 10.1002/eat.20521. [DOI] [PubMed] [Google Scholar]
- 61.Torgersen L, Ystrom E, Haugen M, Meltzer HM, Von HA, Berg CK, et al. Breastfeeding practice in mothers with eating disorders. Maternal & Child Nutrition. 2010;6:243–252. doi: 10.1111/j.1740-8709.2009.00208.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Reba-Harrelson L, Von HA, Hamer RM, Torgersen L, Reichborn-Kjennerud T, Bulik CM. Patterns of maternal feeding and child eating associated with eating disorders in the Norwegian Mother and Child Cohort Study (MoBa) Eat Behav. 2010;11:54–61. doi: 10.1016/j.eatbeh.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Agras S, Hammer L, McNicholas F. A prospective study of the influence of eating-disordered mothers on their children. Int J Eat Disord. 1999;25:253–262. doi: 10.1002/(sici)1098-108x(199904)25:3<253::aid-eat2>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 64.Waugh E, Bulik CM. Offspring of women with eating disorders. Int J Eat Disord. 1999;25:123–133. doi: 10.1002/(sici)1098-108x(199903)25:2<123::aid-eat1>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 65.Brunton PJ, Russell JA. The expectant brain: adapting for motherhood. Nat Rev Neurosci. 2008;9:11–25. doi: 10.1038/nrn2280. [DOI] [PubMed] [Google Scholar]
- 66.Russell JA, Douglas AJ, Ingram CD. Brain preparations for maternity--adaptive changes in behavioral and neuroendocrine systems during pregnancy and lactation. An overview. Prog Brain Res. 2001;133:1–38. doi: 10.1016/s0079-6123(01)33002-9. [DOI] [PubMed] [Google Scholar]
- 67.Siega-Riz AM, Von Holle A, Haugen M, Meltzer HM, Hamer R, Torgersen L, et al. Gestational weight gain of women with eating disorders in the Norwegian pregnancy cohort. Int J Eat Disord. 2011;44:428–434. doi: 10.1002/eat.20835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Grucza RA, Przybeck TR, Cloninger CR. Prevalence and correlates of binge eating disorder in a community sample. Comp Psychiatry. 2007;48:124–131. doi: 10.1016/j.comppsych.2006.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.de ZM. Binge eating disorder and obesity. Int J Obes Relat Metab Disord. 2001;25:51–55. doi: 10.1038/sj.ijo.0801699. [DOI] [PubMed] [Google Scholar]
- 71.Dingemans AE, Van Furth EF. Binge eating disorder psychopathology in normal weight and obese individuals. Int J Eat Disord. 2012;45:135–138. doi: 10.1002/eat.20905. [DOI] [PubMed] [Google Scholar]
- 72.Telch CF, Stice E. Psychiatric comorbidity in women with binge eating disorder: prevalence rates from a non-treatment-seeking sample. J Consult Clin Psychol. 1998;66:768–776. doi: 10.1037//0022-006x.66.5.768. [DOI] [PubMed] [Google Scholar]
- 73.Dunkley DM, Grilo CM. Self-criticism, low self-esteem, depressive symptoms, and over-evaluation of shape and weight in binge eating disorder patients. Behav Res Ther. 2007;45:139–149. doi: 10.1016/j.brat.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 74.Stein D, Meged S, Bar-Hanin T, Blank S, Elizur A, Weizman A. Partial eating disorders in a community sample of female adolescents. J Am Acad Child Adolesc Psychiatry. 1997;36:1116–1123. doi: 10.1097/00004583-199708000-00019. [DOI] [PubMed] [Google Scholar]
- 75.Braun DL, Sunday SR, Halmi KA. Psychiatric comorbidity in patients with eating disorders. Psychol Med. 1994;24:859–867. doi: 10.1017/s0033291700028956. [DOI] [PubMed] [Google Scholar]
- 76.Whisman MAP, Dementyeva AB, Baucom DHP, Bulik CMP. Marital Functioning and Binge Eating Disorder in Married Women. Int J Eat Disord. 2012;45:385–389. doi: 10.1002/eat.20935. [DOI] [PubMed] [Google Scholar]
- 77.Hilbert A, Saelens BE, Stein RI, Mockus DS, Welch RR, Matt GE, et al. Pretreatment and Process Predictors of Outcome in Interpersonal and Cognitive Behavioral Psychotherapy for Binge Eating Disorder. J Consult Clin Psychol. 2007;75:645–651. doi: 10.1037/0022-006X.75.4.645. [DOI] [PubMed] [Google Scholar]
- 78.Goldfein JA, Devlin MJ, Kamenetz C. Eating disorder examination-questionnaire with and without instruction to assess binge eating in patients with binge eating disorder. Int J Eat Disord. 2005;37:107–111. doi: 10.1002/eat.20075. [DOI] [PubMed] [Google Scholar]
- 79.Mond JM, Hay PJ, Rodgers B, Owen C. Self-report versus interview assessment of purging in a community sample of women. Eur Eat Disord Rev. 2007;15:403–409. doi: 10.1002/erv.792. [DOI] [PubMed] [Google Scholar]
- 80.Villanueva EV. The validity of self-reported weight in US adults: a population based cross-sectional study. BMC Public Health. 2001;1:11. doi: 10.1186/1471-2458-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Brunner Huber LR. Validity of self-reported height and weight in women of reproductive age. Matern Child Health J. 2007;11:137–144. doi: 10.1007/s10995-006-0157-0. [DOI] [PubMed] [Google Scholar]
- 82.White MA, Masheb RM, Grilo CM. Accuracy of self-reported weight and height in binge eating disorder: misreport is not related to psychological factors. Obesity. 2010;18:1266–1269. doi: 10.1038/oby.2009.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Meyer C, McPartlan L, Sines J, Waller G. Accuracy of self-reported weight and height: relationship with eating psychopathology among young women. Int J Eat Disord. 2009;42:379–381. doi: 10.1002/eat.20618. [DOI] [PubMed] [Google Scholar]
- 84.Hartge P. Participation in Population Studies. Epidemiology. 2006;17:252–254. doi: 10.1097/01.ede.0000209441.24307.92. [DOI] [PubMed] [Google Scholar]
- 85.Nohr EA, Frydenberg M, Henriksen TB, Olsen J. Does low participation in cohort studies induce bias? Epidemiology. 2006;17:413–418. doi: 10.1097/01.ede.0000220549.14177.60. [DOI] [PubMed] [Google Scholar]
- 86.Lemberg R, Phillips J. The impact of pregnancy on anorexia nervosa and bulimia. Int J Eat Disord. 1989;8:285–295. [Google Scholar]
- 87.Cnattingius S, Hultman CM, Dahl M, Sparen P. Very preterm birth, birth trauma, and the risk of anorexia nervosa among girls. Arch Gen Psychiatry. 1999;56:634–638. doi: 10.1001/archpsyc.56.7.634. [DOI] [PubMed] [Google Scholar]
- 88.Bulik CM, Reba L, Siega-Riz AM, Reichborn-Kjennerud T. Anorexia nervosa: definition, epidemiology, and cycle of risk. Int J Eat Disord. 2005;37:2–9. doi: 10.1002/eat.20107. [DOI] [PubMed] [Google Scholar]