Abstract
HIV serostatus disclosure among people living with HIV/AIDS (PLWHA) is an important component of preventing HIV transmission to sexual partners. Due to barriers like stigma, however, many PLWHA do not disclose their serostatus to all sexual partners. This study explored differences in HIV serostatus disclosure based on sexual behavior subgroup [men who have sex with men (MSM), heterosexual men, and women], characteristics of the sexual relationship (relationship type and HIV serostatus of partner), and perceived stigma. We examined disclosure in a sample of 341 PLWHA: 138 MSM, 87 heterosexual men, and 116 heterosexual women who were enrolled in SafeTalk, a randomized, controlled trial of a safer sex intervention. We found that, overall, 79% of participants disclosed their HIV status to all sexual partners in the past 3 months. However, we found important differences in disclosure by subgroup and relationship characteristics. Heterosexual men and women were more likely to disclose their HIV status than MSM (86%, 85%, and 69%, respectively). Additionally, disclosure was more likely among participants with only primary partners than those with only casual or both casual and primary partners (92%, 54%, and 62%, respectively). Participants with only HIV-positive partners were also more likely to disclose than those with only HIV-negative partners, unknown serostatus partners, or partners of mixed serostatus (96%, 85%, 40%, and 60%, respectively). Finally, people who perceived more HIV-related stigma were less likely to disclose their HIV serostatus to partners, regardless of subgroup or relationship characteristics. These findings suggest that interventions to help PLWHA disclose, particularly to serodiscordant casual partners, are needed and will likely benefit from inclusion of stigma reduction components.
Keywords: HIV serostatus disclosure, stigma, gender differences, sexual partners
HIV serostatus disclosure is an important component of preventing HIV transmission from people living with HIV/AIDS (PLWHA) to their sexual partners, allowing partners to make informed choices before sexual contact. Not only has disclosure been linked to increased condom use and decreased disease transmission (Crepaz & Marks, 2003; Parsons et al., 2005), disclosure also allows serodiscordant couples to take measures to prevent HIV transmission, including the use of pre-exposure prophylaxis and antiretroviral treatment adherence (Brooks et al., 2011; Cohen et al., 2011).
While a substantial body of research has informed our understanding of factors influencing disclosure, at least three gaps remain. First, most research has assessed disclosure within specific subgroups, such as men who have sex with men (MSM) (Klitzman et al., 2007; Marks & Crepaz, 2001; O’Brien et al., 2003), bisexual men (Mutchler et al., 2008), or women (Sowell et al., 2003; Sullivan, Voss, & Li, 2010), but has not directly compared disclosure patterns among subgroups of PLWHA. Second, the extent to which partner-specific variables, such as partner serostatus and relationship type, influence HIV disclosure among different subgroups is unknown. Finally, although previous studies have demonstrated an inverse relationship between HIV stigma and disclosure (Smith, Rossetto, & Peterson, 2008), little research exists regarding the stigma-disclosure association by subgroups. Understanding group differences in disclosure could allow for more targeted prevention programs.
The current study assessed disclosure to sexual partners in a clinically representative, sexually active population of PLWHA. In the full sample and across subgroups of MSM, heterosexual men, and women, our aims were to describe and compare: 1) sexual partner characteristics (relationship type and partner serostatus); 2) the prevalence of disclosure based on partner characteristics; 3) the prevalence of HIV stigma and its association with disclosure; and 4) whether subgroup and sexual partnership characteristics moderated the relationship between HIV stigma and disclosure.
Methods
Participants and Procedures
Data come from the baseline survey of SafeTalk, a randomized, controlled trial of a safer-sex intervention of 490 PLWHA (see Golin et al., 2012 and Widman, Golin, Grodensky, & Suchindran, 2012 for detailed study information). The University of North Carolina at Chapel Hill’s Office for the Protection of Human Research approved all study procedures.
Measures
Subgroups
We determined sexual behavior subgroup (i.e., MSM, heterosexual men, or women) based on participant gender and the gender of their reported sexual partners.
Relationship Type and Partner Serostatus
Based on questions about sexual partners in the last three months, we created a three-category variable for relationship type: 1) only primary partner(s); 2) only casual partner(s); or 3) a combination of primary and casual partner(s). We determined the proportion of partners by serostatus to create a four-category variable: 1) only HIV-positive partner(s); 2) only HIV-negative partner(s); 3) only unknown serostatus partner(s); or 4) a combination of HIV-positive, HIV-negative, and/or unknown serostatus partners.
HIV Stigma
We measured HIV stigma with an abbreviated seven-item disclosure concerns subscale of the HIV Stigma Scale (Berger, Ferrans, & Lashley, 2001; Cronbach’s α = .87).
HIV Serostatus Disclosure
Participants indicated their number of sexual partners and the number of their partners who “knew that you were HIV-positive because you told them that you were positive”. From this, we derived a dichotomous HIV serostatus disclosure variable: 1) “disclosure” (i.e., disclosure to all partners) and 2) “non-disclosure” (i.e., disclosure to less than 100% of partners).
Statistical Analyses
First, we conducted Chi Square analyses with Bonferroni-adjusted post-hoc tests to determine if partnership characteristics differed by subgroup. Next, we examined the percentage of participants who disclosed and used individual logistic regression models to determine if the odds of disclosure varied by subgroup. We used logistic regression to determine if the odds of disclosure varied by relationship type or partner serostatus. Follow-up Chi Square analyses with Bonferroni-adjusted post-hoc tests were used to determine if disclosure differed between subgroups by partnership characteristics. Further, we examined mean differences in HIV stigma within subgroups using a one-way ANOVA, and examined the main effect of stigma on disclosure using logistic regression. Finally, we examined interactions between stigma, subgroups, and sexual partnership characteristics to determine if subgroups moderated the relationship between stigma and disclosure.
Results
Participant and Partnership Characteristics (Tables 1 and 2)
Table 1.
Participant Descriptive Characteristics
| Heterosexual | Heterosexual | |||
|---|---|---|---|---|
| Full Sample N = 341 N (%) |
MSM N = 138 N (%) |
Men N = 87 N (%) |
Women N = 116 N (%) |
|
| Demographics | ||||
| Age [M (SD)] | 42.2 (9.0) | 40.0 (9.5) | 44.9 (7.9) | 42.8 (8.5) |
| Race | ||||
| African-American | 238 (70.0) | 78 (56.9) | 70 (80.5) | 90 (77.6) |
| White | 72 (21.2) | 47 (34.3) | 9 (10.3) | 16 (13.8) |
| Other | 30 (8.8) | 12 (8.8) | 8 (9.2) | 10 (8.6) |
| Education | ||||
| High School or Less | 187 (55.0) | 41 (29.7) | 69 (79.3) | 77 (67.0) |
| Some College or More | 153 (45.0) | 97 (70.3) | 18 (20.7) | 38 (33.0) |
| Employment | ||||
| Not Employed | 212 (62.2) | 75 (54.4) | 60 (69.0) | 77 (66.4) |
| Full or Part-Time | 129 (37.8) | 63 (45.6) | 27 (31.0) | 39 (33.6) |
| Annual income | ||||
| $10,000 or less | 169 (51.7) | 58 (42.7) | 51 (63.8) | 60 (54.1) |
| $10,001 to $20,000 | 83 (25.4) | 39 (28.7) | 19 (23.8) | 25 (22.5) |
| >$20,001 | 75 (22.9) | 39 (28.7) | 10 (12.5) | 26 (23.4) |
| Clinical Characteristics | ||||
| Detectable Viral Load | 128 (37.7) | 57 (41.3) | 28 (32.6) | 43 (37.1) |
| Yrs since Diagnosis [M (SD)] | 9.7 (6.0) | 9.3 (6.5) | 10.8 (5.8) | 9.1 (5.5) |
Note: All participants came from SafeTalk, a safer sex intervention among adults in the southeastern U.S. (Golin et al., 2012). MSM= men who have sex with men. When men indicated they had had sexual contact with both men and women in the previous three months, they were categorized as MSM (n=5).
Table 2.
Descriptive and Comparative Statistics between Subgroups by Sexual Partnership Characteristics
| Heterosexual | Heterosexual | |||
|---|---|---|---|---|
| Full Sample N = 341 N (%) |
MSM N = 138 N (%) |
Men N = 87 N (%) |
Women N = 116 N (%) |
|
| Relationship Type | ||||
| Primary partners only | 214 (62.9) | 59 (42.8) a | 58 (67.4) b | 97 (83.6) c |
| Casual partners only | 84 (24.7) | 52 (37.7) a | 21 (24.4) a | 11 (9.5) b |
| Mixed relationship type partners | 42 (12.3) | 27 (19.5) a | 7 (8.1) | 8 (6.9) b |
| Partner Serostatus | ||||
| HIV+ partners only | 108 (32.3) | 43 (31.1) | 30 (34.5) | 35 (30.7) |
| HIV− partners only | 141 (42.3) | 37 (26.8) a | 39 (44.8) b | 65 (56.0) b |
| Unknown serostatus partners only | 56 (16.7) | 30 (21.7) | 10 (11.5) | 16 (13.8) |
| Mixed serostatus partners | 36 (10.6) | 28 (20.3) a | 8 (9.2) b | 0 (0) c |
Note: All participants came from SafeTalk, a safer sex intervention among adults in thesoutheastern U.S. (Golin et al., 2012). Mixed relationship type partners = both primary and casual partners. Mixed status partners = any combination of HIV+, HIV−, and unknown status partners. Categories that have different superscript letters within the same row (a,b,c) are significantly different from each other at the p < . 05 level with Bonferroni-adjusted post-hoc tests.
p <10,
p <05,
p <01,
p <001.
We excluded 149 participants from the original 490 in SafeTalk for this analysis: 105 who were sexually abstinent; 32 who had missing data on disclosure; 8 women who reported sexual activity exclusively with women; and 4 transgendered individuals. The final sample included 341 individuals: 138 MSM (40%), 87 heterosexual men (26%), and 116 heterosexual women (34%). See Table 1 for descriptive data and Table 2 for sexual partnership characteristics. Notably, 42% of participants had HIV-negative sexual partners and 17% had partners of unknown serostatus.
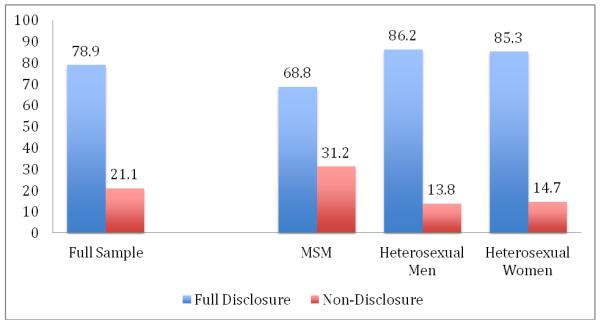
Prevalence of HIV Serostatus Disclosure (Figure 1)
Figure 1.
Percentage of HIV Serostatus Disclosure among PLWHA in the Full Sample and by Subgroup.
Note: MSM = men who have sex with men. Full Disclosure = disclosed HIV serostatus to all sexual partners. Non-Disclosure = did not fully disclose HIV serostatus to all partners.
Across the full sample, 79% of individuals disclosed their HIV status to all sexual partners in the previous three months. Disclosure was more likely among women (85%) and heterosexual men (86%) than MSM (69%) (OR = 2.63, 95% CI [1.40, 4.94], p < .01 and OR = 2.82, 95% CI [1.39, 5.74], p < .01, respectively).
Differences in Disclosure Based on Partnership Characteristics
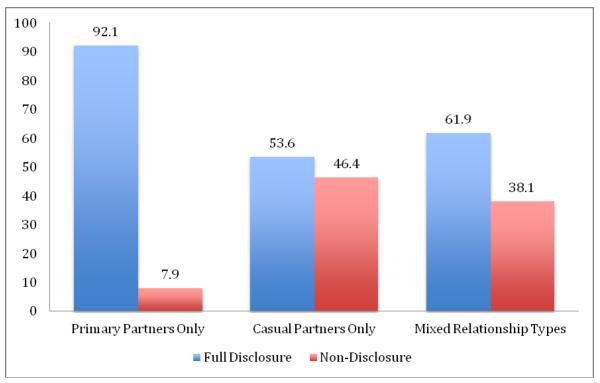
Relationship Type (Figure 2)
Figure 2.
Percentage of HIV Serostatus Disclosure among PLWHA based on Sexual Partner Relationship Types.
Note: Mixed Partner Types: combination of primary and casual partners. Full Disclosure = disclosed HIV serostatus to all sexual partners. Non-Disclosure = did not fully disclose HIV serostatus to all partners.
Disclosure was less likely among participants with only casual partners (54%) and mixed relationship types (62%) relative to those with only primary partners (92%) (OR = 0.10, 95% CI [0.05, 0.19], p < .001 and OR = 0.14, 95% CI [0.06, 0.31], p < .001, respectively). The proportion of participants who disclosed did not differ significantly among subgroups (Table 3).
Table 3.
Percentage of Participants with HIV Disclosure: Comparisons between Subgroups by Sexual Partnership Characteristics
| MSM (N = 138) |
Heterosexual Men (N = 87) |
Heterosexual Women (N = 116) |
|||||
|---|---|---|---|---|---|---|---|
| #Disclose/ #In Group |
Disclosure (%) |
#Disclose/ #In Group |
Disclosure (%) |
#Disclose/ #In Group |
Disclosure (%) |
Chi Square Test Between Groups |
|
| Relationship Type | |||||||
| Primary partners only | 50/59 | 84.8 | 55/58 | 94.8 | 92/97 | 94.8 | χ(2) = 5.95+ |
| Casual partners only | 26/52 | 50.0 | 14/21 | 66.7 | 5/11 | 45.5 | χ(2) = 2.01 |
| Mixed relationship type | 19/27 | 70.4 | 5/7 | 71.4 | 2/8 | 25.0 | χ(2) = 5.71+ |
| Partner Serostatus | |||||||
| HIV+ partners only | 40/43 | 93.0 | 30/30 | 100 | 34/35 | 97.1 | χ(2) = 2.52 |
| HIV− partners only | 33/37 | 89.2 | 34/39 | 87.2 | 54/65 | 83.1 | χ(2) = 0.81 |
| Unknown serostatus only | 7/30 | 23.3 a | 5/10 | 50.0 | 11/16 | 68.8 b | χ(2) = 9.29* |
| Mixed serostatus | 15/28 | 53.6 | 6/8 | 75.0 | 0/0 | 0 | χ(2) = 1.18 |
Note: All participants came from SafeTalk, a safer sex intervention among adults in the southeastern U.S. (Golin et al., 2012) #Disclose = Number of people who disclosed to all partners. #In Group = number of people in part cular group. Disclosure = full HIV serostatus disclosure. Mixed relationship type = both primary and casual partners. Mixed serostatus = any combination of HIV+, HIV−, and unknown serostatus partners. Categories that have different superscript letters within the same row (a,b) are significantly different from each other at the p < 05 level with Bonferroni-adjusted post-hoc tests.
p <10,
p <05
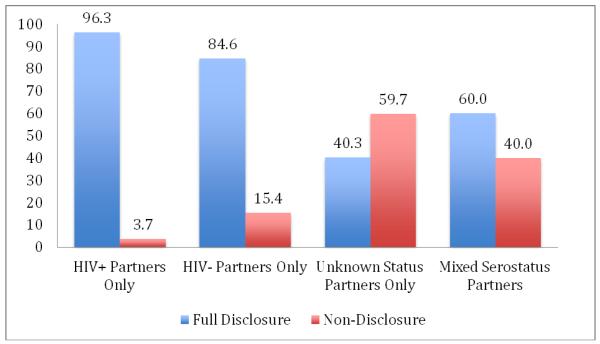
Partner Serostatus (Figure 3)
Figure 3.
Percentage of HIV Serostatus Disclosure among PLWHA based on Serostatus of their Sexual Partners.
Note: Mixed serostatus = any combination of HIV+, HIV−, and unknown serostatus partners. Full Disclosure = disclosed HIV serostatus to all sexual partners. Non-Disclosure = did not fully disclose HIV serostatus to all partners.
Relative to disclosure to HIV-positive partners (96.3%), disclosure was less likely to HIV-negative partners (84.6%), unknown serostatus partners (40.3%), and mixed serostatus partners (60.0%) (OR = 0.23, 95% CI [0.08, 0.70], p = .01; OR = 0.03, 95% CI [0.01, 0.09], p < .001; and OR = 0.07, 95% CI [0.02, 0.25], p < .001, respectively). The association between disclosure and partner serostatus varied by subgroup when partner serostatus was unknown [χ2 (2) = 9.29, p < .01] (Table 3). Specifically, MSM had less disclosure to unknown serostatus partners (22.6%) than did women (69%), χ2 (1) = 9.04, p < .01.
HIV Stigma and Disclosure
HIV stigma (full sample M = 21.57, SD = 5.67) did not differ between subgroups: MSM (M = 22.14, SD = 5.47), heterosexual men (M = 20.65, SD = 5.76) and women (M = 21.58, SD = 5.79), F(2, 330) = 1.82, p = .16. Importantly, HIV stigma was inversely associated with disclosure, where greater stigma was associated with lower odds of being in the disclosure group (OR = 0.89, 95% CI [0.81, 0.93], p < .001). The relationship between stigma and disclosure was not moderated by subgroup or sexual partner characteristics.
Discussion
This study analyzed HIV disclosure among sexually active PLWHA that included three subgroups – MSM, heterosexual men, and women – and explored whether disclosure differed among these groups by sexual partner serostatus or relationship status. Overall, 21% of participants failed to disclose to all sexual partners, with MSM being least likely to disclose (Weinhardt et al., 2004). Participants with casual or mixed relationships disclosed less than those in exclusively primary relationships (Duru et al., 2006, Vu et al., 2012) and less to HIV-negative, unknown, and mixed serostatus partners than to HIV-positive partners (Klitzman et al., 2007; McKay & Mutchler, 2010; Niccolai, Dorst, Myers, & Kissinger, 2006). MSM were particularly unlikely to disclose to unknown status partners. This study is unique in directly comparing disclosure among the three subgroups across sexual partnership types. Our findings suggest future disclosure research should focus as much on relationship characteristics as on gender and sexual orientation of PLWHA.
Most PLWHA reported experiencing HIV-related stigma, and individuals who experienced more stigma were less likely to disclose their HIV status (Simbayi et al., 2007; Smith et al., 2008). This study went beyond previous work in showing that the association between stigma and disclosure did not differ between subgroups or across relationship types, suggesting this association is extremely robust. Effective methods of reducing HIV-related stigma and enhancing PLWHA’s efficacy to disclose in the face of stigma are urgently needed (Chaudoir, Fisher, & Simoni, 2011).
Limitations
While we stressed participant confidentiality and used an ACASI to help minimize the recall and social desirability biases to which self-reported data may be subject (Des Jarlais et al., 1999), participants may have still over-reported disclosure. Second, because we did not collect data from participants’ sexual partners, we were unable to conduct analyses at the dyad level. Finally, our findings may not generalize to PLWHA who are not in care.
Conclusion
This study highlights both differences and similarities among MSM, heterosexual men, and women living with HIV. As the HIV prevention toolkit expands with the success of recent PrEP and “treatment as prevention” studies (Brooks et al., 2011; Cohen et al., 2011), HIV serostatus disclosure is increasingly important and beneficial for serodiscordant partners. While future studies could explore further the meaning and process of disclosure, our findings suggests that interventions to improve effective disclosure may need to be tailored on sexual partnership characteristics, particularly for MSM.
Acknowledgments
We would like to first thank the many patients whose participation made this project possible. We would like to thank Kemi Amola Hill, Niasha Brown, Zulfia Chariyeva, Rebecca Davis, Jennifer Groves, Tyndall Harris, Meheret Mamo, Shilpa Patel, Jessica Kadis Pepper, Kathy Ramsey, Katherine Tiller, and Latoya White for their assistance in data collection, cleaning, and management. We would also like to acknowledge Ross Oglesbee for her administrative assistance and the staff in the clinics in which the study was conducted for their enthusiastic support. This work was supported by National Institutes of Health (NIH) grants #: R01 MH069989-01A2, DK56350-01, T32 AI 07001-31, T32 AI 07001-34, and UNC CFAR grant #: P30-AI50410. The content is solely the responsibility of the authors and does not represent the official views of the NIH.
References
- Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Research in Nursing and Health. 2001;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Brooks RA, Kaplan RL, Lieber E, Landovitz RJ, Lee SJ, Leibowitz AA. Motivators, concerns, and barriers to adoption of preexposure prophylaxis for HIV prevention among gay and bisexual men in HIV-serodiscordant male relationships. AIDS Care. 2011;23(9):1136–45. doi: 10.1080/09540121.2011.554528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudoir SR, Fisher JD, Simoni JM. Understanding HIV disclosure: a review and application of the Disclosure Processes Model. Social Science & Medicine. 2011;72(10):1618–1629. doi: 10.1016/j.socscimed.2011.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone DH, Kanouse DE, Collins RL, Miu A, Chen JL, Morton SC, Stall R. Sex without disclosure of positive HIV serostatus in a US probability sample of persons receiving medical care for HIV infection. American Journal of Public Health. 2003;93(6):949–54. doi: 10.2105/ajph.93.6.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, HPTN 052 Study Team Prevention of HIV-1 infection with early antiretroviral therapy. New England Journal of Medicine. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crepaz N, Marks G. Serostatus disclosure, sexual communication and safer sex in HIV-positive men. AIDS Care. 2003;15(3):379–387. doi: 10.1080/0954012031000105432. [DOI] [PubMed] [Google Scholar]
- Des Jarlais D, Paone D, Milliken J, Turner CF, Miller H, Gribble J, Friedman SR. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomised trial. Lancet. 1999;353:1657–1661. doi: 10.1016/s0140-6736(98)07026-3. [DOI] [PubMed] [Google Scholar]
- Duru OK, Collins RL, Ciccarone DH, Morton SC, Stall R, Beckman R, Kanouse DE. Correlates of sex without serostatus disclosure among a national probability sample of HIV patients. AIDS and Behavior. 2006;10(5):495–507. doi: 10.1007/s10461-006-9089-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golin CE, Earp JA, Grodensky CA, Patel SN, Suchindran C, Parikh M, Groves J. Longitudinal effects of SafeTalk, a motivational interviewing-based program to improve safer sex practices among people living with HIV/AIDS. AIDS and Behavior. 2012;16(5):1182–91. doi: 10.1007/s10461-011-0025-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klitzman R, Exner T, Correale J, Kirshenbaum SB, Remien R, Ehrhardt AA, Charlebois E. It’s not just what you say: Relationships of HIV disclosure and risk reduction among MSM in the post-HAART era. AIDS Care. 2007;19(6):749–756. doi: 10.1080/09540120600983971. [DOI] [PubMed] [Google Scholar]
- Marks G, Crepaz N. HIV-positive men’s sexual practices in the context of self-disclosure of HIV status. Journal of Acquired Immune Deficiency Syndromes. 2001;27(1):79–85. doi: 10.1097/00126334-200105010-00013. [DOI] [PubMed] [Google Scholar]
- McKay T, Mutchler MG. The effect of partner sex: Nondisclosure of HIV status to male and female partners among men who have sex with men and women (MSMW) AIDS and Behavior. 2010;15(6):1140–52. doi: 10.1007/s10461-010-9851-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutchler MG, Bogart LM, Elliott MN, McKay T, Suttorp MJ, Schuster MA. Psychosocial correlates of unprotected sex without disclosure of HIV-positivity among African-American, Latino, and White men who have sex with men and women. Archives of Sexual Behavior. 2008;37(5):736–747. doi: 10.1007/s10508-008-9363-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niccolai LM, King E, D’Entremont D, Pritchett EN. Disclosure of HIV serostatus to sex partners: A new approach to measurement. Sexually Transmitted Disease. 2006;33(2):102–105. doi: 10.1097/01.olq.0000194591.97159.66. [DOI] [PubMed] [Google Scholar]
- O’Brien ME, Richardson-Alston G, Ayoub M, Magnus M, Peterman TA, Kissinger P. Prevalence and correlates of HIV serostatus disclosure. Sexually Transmitted Diseases. 2003;30(9):731–735. doi: 10.1097/01.OLQ.0000079049.73800.C2. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Schrimshaw EW, Bimbi DS, Wolitski RJ, Gómez CA, Halkitis PN. Consistent, inconsistent, and non-disclosure to casual sexual partners among HIV-seropositive gay and bisexual men. AIDS. 2005;19(Suppl 1):S87–97. doi: 10.1097/01.aids.0000167355.87041.63. [DOI] [PubMed] [Google Scholar]
- Simbayi LC, Kalichman SC, Strebel A, Cloete A, Henda N, Mqeketo A. Disclosure of HIV status to sex partners and sexual risk behaviours among HIV-positive men and women, Cape Town, South Africa. Sexually Transmitted Infections. 2007;83(1):29–34. doi: 10.1136/sti.2006.019893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith R, Rossetto K, Peterson BL. A meta-analysis of disclosure of one’s HIV-positive status, stigma and social support. AIDS Care. 2008;20(10):1266–1275. doi: 10.1080/09540120801926977. [DOI] [PubMed] [Google Scholar]
- Sowell RL, Seals BF, Phillips KD, Julious CH. Disclosure of HIV infection: How do women decide to tell? Health Education Research. 2003;18(1):32–44. doi: 10.1093/her/18.1.32. [DOI] [PubMed] [Google Scholar]
- Sullivan K, Voss J, Li D. Female disclosure of HIV-positive serostatus to sex partners: A two-city study. Women & Health. 2010;50(6):506–526. doi: 10.1080/03630242.2010.516697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vu L, Andrinopoulos K, Mathews C, Chopra M, Kendall C, Eisele TP. Disclosure of HIV status to sex partners among HIV-infected men and women in Cape Town, South Africa. AIDS and Behavior. 2012;16(1):132–8. doi: 10.1007/s10461-010-9873-y. [DOI] [PubMed] [Google Scholar]
- Weinhardt LS, Kelly JA, Brondino MJ, Rotheram-Borus MJ, Kirshenbaum SB, Chesney MA, National Institute of Mental Health Healthy Living Project Team HIV transmission risk behavior among men and women living with HIV in 4 cities in the United States. Journal of Acquired Immune Deficiency Syndromes. 2004;36(5):1057–1066. doi: 10.1097/00126334-200408150-00009. [DOI] [PubMed] [Google Scholar]
- Widman L, Golin CE, Grodensky CA, Suchindran C. Do safer sex self-efficacy, attitudes toward condoms, and HIV transmission risk beliefs differ among men who have sex with men, heterosexual men, and women living with HIV? AIDS and Behavior. 2012 doi: 10.1007/s10461-011-0108-7. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]