Abstract
Background:
Chronic rhinosinusitis has a major impact on the quality of life of patients with cystic fibrosis (CF) and may contribute to progression of chronic lung disease. Despite multiple sinus surgeries, maxillary sinus involvement is a recurrent problem. The modified endoscopic medial maxillectomy (MEMM) permits debridement in the clinic, improves mucus clearance with nasal irrigations, and increases access for topical delivery of therapeutics. However, clinical outcomes of aggressive sinus surgery with regimented postoperative medical treatment have not been systematically evaluated.
Methods:
CF patients completed the 22-Item Sinonasal Outcome Test questionnaires before sinus surgery (and bilateral MEMM) and at sequential postoperative visits. Objective measures included Lund-Kennedy endoscopic score and pulmonary function tests (forced expiratory volume at 1 second percent [FEV1%] predicted). Culture-directed antibiotic therapy, prednisone, and topical irrigations were initiated postoperatively.
Results:
Twenty-two patients (mean age, 26.5 years; 4.9 prior sinus operations) underwent MEMM and sinus surgery. Symptom scores were significantly reduced at 60 days (primary outcome, 64.7 ± 18.4 presurgery versus 27.5 ± 15.3 postsurgery; p < 0.0001) and up to a year postoperatively (27.6 ± 12.6; p < 0.0001). Endoscopic scores were also reduced after surgery (10.4 ± 1.1 presurgery versus 5.7 ± 2.4 [30 days], 5.7 ± 1.4 [60 days], 5.8 ± 1.3 [120 days], and 6.0 ± 1.1 [1 year]; p < 0.0001)]. There were no differences in FEV1% predicted up to 1 year postoperatively, but hospital admissions secondary to pulmonary exacerbations significantly decreased (2.0 ± 1.4 versus 3.2 ± 2.4, respectively; p < 0.05).
Conclusion:
Prospective evaluation indicates sinus surgery with MEMM is associated with marked improvement in sinus disease outcomes. Additional studies are necessary to confirm whether this treatment paradigm is associated with improved CF pulmonary disease.
Keywords: Antibiotics, chronic sinusitis, cystic fibrosis, endoscopic medial maxillectomy, mucociliary clearance, sinonasal outcomes, sinus surgery, SNOT-22
Cystic fibrosis (CF) is an autosomal recessive chronic disease that affects the airways (upper and lower) and digestive system of ∼30,000 children and adults in the United States and 70,000 worldwide.1 CF patients have a high prevalence (approaching 100%) of severe chronic rhinosinusitis (CRS), which is often associated with nasal polyposis (6–48%).2–5 The pathophysiology of CRS in CF patients is because of, in large part, impaired mucociliary clearance (MCC)—a critical host defense mechanism for maintaining healthy sinuses in normal individuals.6 Although pulmonary failure leads to the ultimate demise of most CF patients, CRS has a significant impact on their overall quality of life and may contribute to lung disease pathogenesis.7 Treatment strategies vary but usually include a combination of endoscopic sinus surgery, systemic and topical antibiotics/steroids, and nasal irrigations. The indications, timing, and degree of surgical management and postoperative care remain controversial.
Approximately 10–20% of CF patients require surgical management of their disease.8 Of the patients undergoing sinus surgery, failure rates, requiring revision surgery, range from 13 to 89%.3,9 Consequently, many CF patients have had multiple functional endoscopic sinus surgeries (FESSs) by the time they reach adulthood. In essence, surgery does not offer a cure for these patients because the mucosa will never have normal function because of their underlying genetic defect and will always be laden with inflammation and heavy bacterial contamination that has to be controlled with additional medicinal, mechanical, and physical interventions for the desiccated mucus.
Maxillary sinus involvement, in particular, is a recurrent problem because the normal MCC pathway is through the natural ostium and against gravity. In CF, impaired MCC often leads to mucopurulent debris filling the inferior half of the maxillary cavities despite “adequate” maxillary antrostomies, which remains a reservoir for chronic infection and seeding of the airway.10 Ensuring access to the sinuses to enable cleaning could confer benefit in addition to the conventional goal of providing adequate ventilation. The modified endoscopic medial maxillectomy (MEMM) procedure involves removal of the medial maxillary wall, essentially marsupializing the maxillary sinus into the nasal cavity (Fig. 1). This allows clearance of the sinus without the need to oppose gravity or to occur through narrow anatomic ostia. In addition, the procedure permits physical debridement of mucus and polypoid edema in the clinic, improved clearance of mucus with nasal irrigations, and increased access for topical delivery of therapeutics. The effectiveness of aggressive sinus surgery, which includes a supportive care regimen using proactive clinic debridement and aggressive medical treatment, has not been previously reported.
Figure 1.
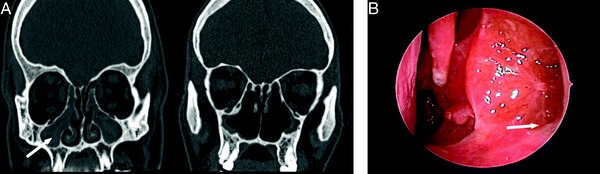
(A) Coronal CT scans showing the preoperative appearance of a patient with cystic fibrosis (CF) after traditional maxillary antrostomies with completely opacified maxillary sinuses (left, white arrow) and postoperative appearance after bilateral modified endoscopic medial maxillectomies and revision sinus surgery (right). (B) Transnasal endoscopic view of a left maxillary sinus after modified endoscopic medial maxillectomy. A 30° endoscope is inserted past the anterior ⅓ of the inferior turbinate revealing a well-healed maxillary cavity with no secretions retained in the floor of the sinus (arrow).
The purpose of the current study was to prospectively evaluate the effectiveness of extensive surgical treatment with regimented postoperative medical care for severe, recalcitrant CF CRS.
METHODS
Subjects
Treatment Protocol.
Treatment of severe CRS was offered to all patients with recalcitrant disease. Prospective evaluation and data collection of subjects were approved by the Institutional Review Board at the University of Alabama at Birmingham. All patients carrying the diagnosis of CF by genotype or sweat chloride and meeting Sinus and Allergy Health Partnership criteria11 for CRS were referred for consultation to a single otolaryngologist (BAW). Patients with persistent symptoms despite aggressive medical treatment (minimum antibiotics for 2 weeks, often including i.v. antibiotics during inpatient admission for pulmonary exacerbations) and panmucosal sinus disease on CT scan, were offered our options per our standard practice including (1) continued medical treatment with saline irrigations and topical steroids/antibiotics, (2) endoscopic sinus surgery, or (3) endoscopic sinus surgery + bilateral MEMMs. The purpose of the surgery is to remove all bony partitions along the skull base and open the sinuses as widely as possible using mucosal sparing technique. Three weeks of postoperative, culture-directed antibiotics and low-dose prednisone at 20 mg (3–8 weeks) were administered postoperatively to reduce postoperative scarring and contracture associated with the presence of extensive infection and inflammation. Saline irrigations were performed twice a day and as needed during the immediate postoperative period. Once spacers and debris were removed postoperatively, topical treatments, including a steroid and antibiotic(s), were prescribed. At the least, patients were on a nasal steroid spray, but the majority of subjects were placed on either budesonide (500 mg) or mometasone (600 mg) combined with their saline irrigations (120 mL). Patients with cultured Staphylococcus aureus used mupirocin (3–4 mg, compounded or ointment form) and nearly all used tobramycin or equivalent for Pseudomonas species. Those receiving pulmonary nebulized tobramycin on alternating months discontinued nasal administration during that time. Once healed, medicinal/mechanical irrigations and debridements in the clinic were continued to reduce severity of exacerbations, help keep mucus cleared, and decrease bacterial burden. The purpose of the culture-directed treatment and steroids was to complete the healing phase without severe infection or inflammation. Endoscopic debridements were performed at each postoperative clinic visit. Patients were scheduled to return to the ear, nose, and throat clinic for inspection and/or debridement of their sinuses every 3 months to coincide with their pulmonary CF clinic appointments.
Surgical Technique
The purpose of the MEMM is to permit wide marsupialization of the maxillary cavity and improve the ability of mechanical irrigations to clear inspissated secretions. MEMM also aids in the ability to perform postoperative debridement and optimizes distribution of topical medications. Using 0° and angled endoscopes, the middle meatal antrostomy is revised first, if necessary, with complete removal of the uncinate process. The inferior turbinate is incised several millimeters posterior to the nasolacrimal opening, leaving the anterior ⅓ of the turbinate to decrease the risk of “empty nose” syndrome or atrophic rhinitis.12 The lateral nasal wall is then perforated anteriorly and a sagittal cut extended posteriorly to the level of the posterior maxillary wall. The medial maxillary wall is then removed following posterior and anterior vertical osteotomies. A mucosal flap pedicled on the nasal floor is elevated from the lateral wall and the ridge is drilled down until level with the palate. The maxillary sinus is now completely contiguous with the nasal cavity, while keeping the anterior ⅓ of the inferior turbinate. The loculated pockets of purulence are suctioned from the maxillary sinus without removing the mucosa. Finally, the pedicled mucosal flap is placed over the exposed maxillary bone and into the maxillary sinus cavity. Meticulous preservation of mucosa is attempted in all cases.
Revision surgery of the remaining sinuses is then performed. The sphenoid sinus is opened and all bony partitions of the ethmoid cavity are removed sparing the mucosa of the orbit, skull base, and middle turbinate. The frontal recess is dissected using frontal sinus recess instruments and a 70° scope for visualization. The bony partitions and any frontal recess cells are removed sparing all surrounding mucosa. Purulence is removed and the sinuses are irrigated with normal saline on completion of the procedure.
Outcome Measures
Subjects completed the validated 22-Item Sinonasal Outcome Test (SNOT-22) questionnaire13,14 before surgery and at each postoperative visit. Preoperative questionnaires were given after completion of aggressive medical treatment. Questionnaires were also provided before any assessments were performed. Standard demographic data, spirometry, and postoperative follow-up times were collected. Data were collected at 30 ± 7, 120 ± 30, and 365 ± 30 days. The primary outcome measure included SNOT-22 scores at 60 days. Secondary outcomes included Lund-Kennedy endoscopic scores,15 forced expiratory volume at 1 second percent (FEV1%) predicted, number of hospital admissions for pulmonary exacerbations in the year pre- and postsurgery. Lund-Kennedy scores were derived from pre-/intraoperative video and clinic video, but were not blinded because of the presence of the MEMM. Spirometry was performed using American Thoracic Society criteria as part of routine CF clinic visits.16 Spirometry results were collected from outpatient values, but when associated with pulmonary exacerbations, spirometry before discharge was recorded. Outcome measures were tested for significance using paired t-tests or ANOVA as appropriate. A value of p < 0.05 was considered statistically significant.
RESULTS
Between August 2008 and May 2011, a single ear, nose, and throat surgeon had 50 CF patient consultations for the diagnosis of CRS. Only individuals meeting Sinus and Allergy Health Partnership criteria11 for CRS after aggressive medical treatment with panmucosal sinus disease on CT scans were offered surgery. Of 27 patients offered surgery, 23 individuals elected to have bilateral MEMMs and sinus surgery and 22 had sufficient follow-up to be included in the evaluation (Table 1). Three patients elected to have bilateral sinus surgery without MEMM and one patient continues on medical therapy. Average age was 26.5 (range, 19–43 years) years with 14 female patients. The majority of patients (17/22) were F508del homozygotes. Patients had an average of 4.9 FESSs before presentation. Preoperative Lund-McKay17 CT grades were 21.4 ± 1.6, indicating a high degree of disease severity (maximum of 24). Average follow-up was 482 days. Two patients did not return for 60-day follow-up but were seen during subsequent hospitalizations or clinic visits. Few adverse events were reported. Two patients had poor pulmonary function and advanced lung disease at presentation for surgery. They expired from pulmonary failure ∼6 months after surgery, which was considered unrelated to their surgical procedure. Another patient also expired 1 year after her surgery from pulmonary disease. Only two patients required a subsequent operation under general anesthesia; both were for frontal sinus disease. All patients were otherwise routinely debrided successfully on routine clinical follow-up or on inpatient admission for sinus/lung exacerbations.
Table 1.
Patient Population
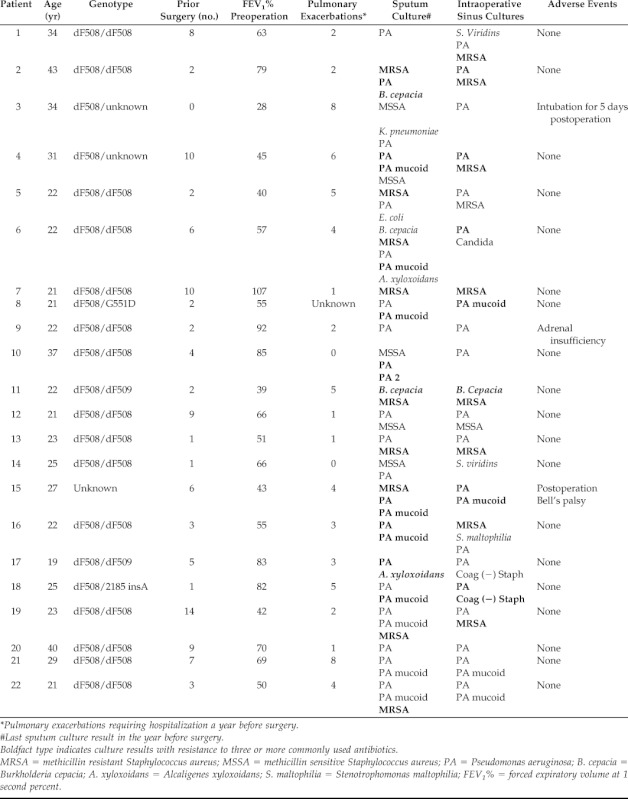
*Pulmonary exacerbations requiring hospitalization a year before surgery.
#Last sputum culture result in the year before surgery.
Boldfact type indicates culture results with resistance to three or more commonly used antibiotics.
MRSA = methicillin resistant Staphylococcus aureus; MSSA = methicillin sensitive Staphylococcus aureus; PA = Pseudomonas aeruginosa; B. cepacia = Burkholderia cepacia; A. xyloxoidans = Alcaligenes xyloxoidans; S. maltophilia = Stenotrophomonas maltophilia; FEV1% = forced expiratory volume at 1 second percent.
Sinus symptom scores by total SNOT-22 were significantly reduced at 60 days (64.7 ± 18.4 presurgery versus 27.5 ± 15.3 postsurgery; p < 0.0001) and remained decreased through 120 days and 1 year postoperatively (27.9 ± 20.4 and 27.6 ± 12.6, respectively; p < 0.0001; Figs. 2 and 3). All subjects experienced a decrease in SNOT-22 (mean change, 37.2; range, 9 - 81), which compared favorably with the minimal clinically important difference of the SNOT-22 score (8.9).13 Robust improvements were also noted in nasal obstruction (4.3 ± 1.1 versus 1.1 ± 1.4; p < 0.0001), postnasal drip (3.9 ± 1.0 versus 1.6 ± 1.3; p < 0.0001), and facial pain/pressure (4.4 ± 0.8 versus 1.1 ± 1.0; p < 0.0001). Lund-Kennedy endoscopic scores (scale of 12) were also significantly reduced at all time points after surgery (10.4 ± 1.1 presurgery versus 5.7 ± 2.4 [30 days], 5.7 ± 1.4 [60 days], 5.8 ± 1.3 [120 days], and 6.0 ± 1.1 [1 year]; all postsurgeries, p < 0.0001; Fig. 4). There were no differences in FEV1% predicted before and after the sinus surgery protocol at 60 days (60.0 ± 18.3 presurgery versus 60.3 ± 19.7 postsurgery; p = 0.48) and 1 year (56.6 ± 21.6; p = 0.61; Fig. 5). The number of hospital admissions secondary to pulmonary exacerbations in the year after surgery was significantly improved compared with the previous year (2.0 ± 1.4 versus 3.2 ± 2.4, respectively; p < 0.05; Fig. 6).
Figure 2.
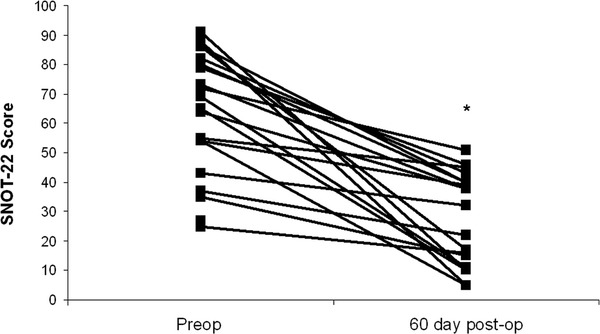
Twenty-two Item Sinonasal Outcomes Test (SNOT-22) scores before and after aggressive sinus surgery with modified endoscopic medial maxillectomies and ordered postoperative medical management. (*p < 0.0001; n = 20).
Figure 3.
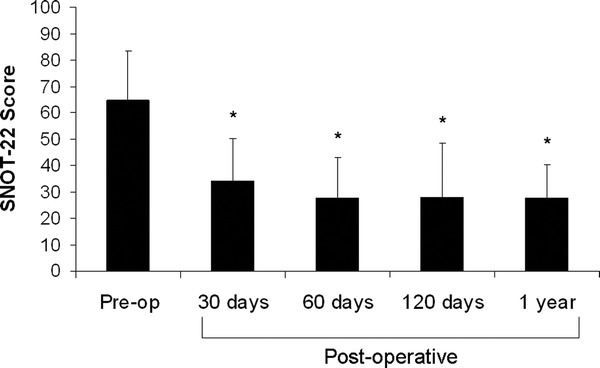
Total Twenty-two Item Sinonasal Outcomes Test (SNOT-22) score preoperatively and at each postoperative visit (*p < 0.0001). No significant difference in total SNOT-22 scores were observed among postoperativie visits (p = 0.89).
Figure 4.
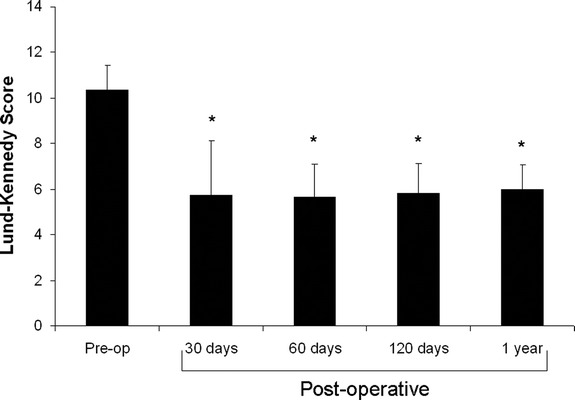
Lund-Kennedy endoscopic score preoperatively and at each postoperative visit (*p < 0.0001).
Figure 5.
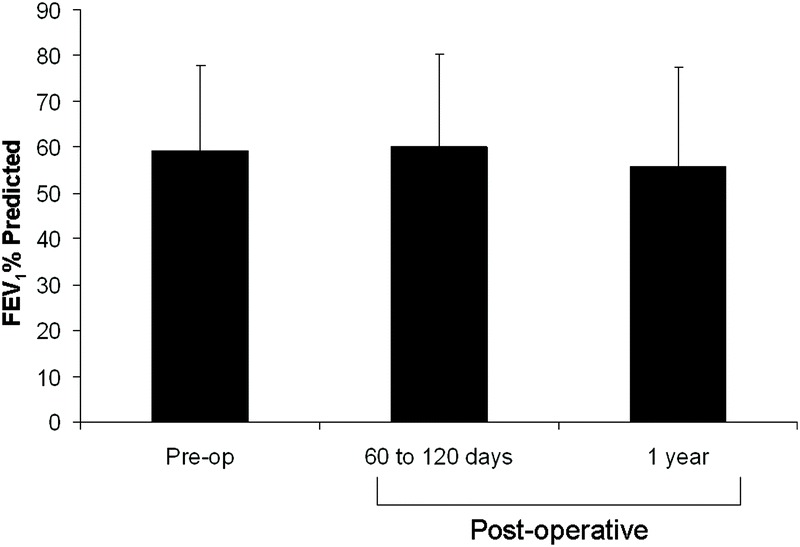
Forced expiratory volume at 1 second percent (FEV1%) predicted preoperative and at each postoperative visit. FEV1]% at 60 and 120 days were combined (p = 0.48).
Figure 6.
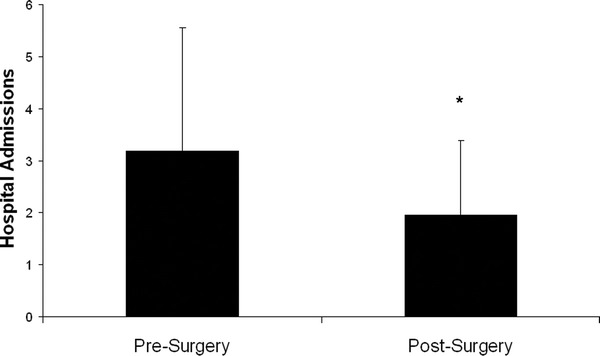
The number of hospital admissions per year before and after sinus surgery (*p < 0.05).
DISCUSSION
CRS in the CF population is a source of significant morbidity and may contribute to the progression of CF lung disease by seeding the lower airway with pathogenic bacteria.18 As more CF patients have reached adulthood, a more aggressive treatment algorithm for CRS has emerged. Many adult CF patients have had multiple sinus surgeries—a fact highlighted by the patient group in the current study (average, 4.9). In a retrospective review in 2006 we reported the first use of MEMM in patients with chronic maxillary sinusitis.19 All patients in this cohort had failed traditional maxillary antrostomies and the majority had prior Caldwell-Luc procedures that had stripped the mucosa from the maxillary sinuses. Results showed that MEMM was a successful treatment in this patient population (which included CF patients) and was associated with a low risk of complications, although prospective evaluation was not performed. In another retrospective case series, Schatz20 reported on a very aggressive surgical approach for the maxillary sinuses of children with CF who had prior endoscopic sinus surgery. After bilateral Caldwell-Luc approaches and endoscopic medial maxillectomies, there was a reduction in symptoms as well as a significant decrease in hospital admissions and improvement in FEV1% in this patient population. However, with angled endoscopes and curved suction instruments, a Caldwell-Luc is not necessary if an MEMM is performed because the entire sinus can be accessed through this approach. Subsequently, Cho et al. in 2008 reported on the endoscopic maxillary mega-antrostomy (a modification of the MEMM) as a safe and effective treatment for recalcitrant maxillary sinusitis.21 The present study extends these observations and for the first time shows that MEMM, combined with revision sinus surgery and aggressive postoperative medical management, is associated with a decrease in symptoms (improved SNOT-22 scores) and objective findings (improved Lund-Kennedy scores) after 60 days of clinical follow-up in patients with recalcitrant CF CRS. In addition, improvement was persistent at 1 year of follow-up, suggesting sustained improvements in symptoms and that nasal examination can be obtained with this approach.
Optimal management of CRS in CF patients consists of systemic anti-inflammatory medications and antimicrobials, topical treatments, and, frequently, FESS. Topical nasal steroids have been shown to reduce polyp size and associated symptoms.22,23 In a recent systematic literature review, Lim et al.24 concluded that the use of topical antimicrobials in the management of CRS is efficacious. However, this therapeutic approach may be limited by poor penetration of treatment agents. Other topical treatments in CF sinus disease include hypertonic saline and dornase alfa, which have shown benefit, but may also be limited by ineffective delivery.25–27 The surgical approach suggested here includes aggressive sinus surgery, including bilateral MEMMs, which maximized patency of all sinuses. This approach not only facilitates intraoffice debridement, but also allows for more effective delivery of topical therapeutics in a manner not achieved with regular maxillary antrostomies. This may explain the robust response observed in our study.
There has long been an observed link between upper and lower respiratory tract disease. In a review from 2001, Passalacqua et al.28 compiled evidence that supports the theory of a united airway. A clear link between allergic rhinitis/CRS and asthma has been established. In this patient population control of sinus disease has been shown to reduce the frequency of asthma exacerbations.29,30 The link between CRS and pulmonary function in the CF population is less defined. In 1997, Madonna et al.31 failed to reveal any improvement in FEV1% in 15 pediatric CF patients after undergoing aggressive medical and surgical management of their sinus disease. However, in 2006 Shatz did show improvement in FEV1% and decrease in hospital admissions after aggressive surgical management of 15 pediatric patients.20 Additionally, in a series of 37 CF patients who underwent lung transplantation, aggressive sinus management led to a lower incidence of tracheobronchitis and pneumonia.18 This suggests that aggressive management of sinus disease in the CF patient population could have a long-term benefit on the degree of bacterial transmission to the lower airway. In our series, although we did not see a change in FEV1%, we did observe a reduced number of hospital admissions for pulmonary exacerbations in the year after surgery. The mean rate of acute pulmonary exacerbations in our study population before surgery was 3.2/year (range, 0–8), reflecting a relatively ill CF population at baseline. This decreased to 2.0/year (range, 0–5). These data suggest a significant benefit is associated with aggressive surgical management. Because FEV1% decline is associated with pulmonary exacerbations,32 ongoing prospective follow-up, including spirometry data, will allow us to further delineate whether aggressive sinus surgery with regimented postoperative care can confer improved pulmonary function decline.
The data presented here exhibit a robust treatment effect for impact in sinus disease and confirms the safety and tolerability of this therapeutic approach in CF subjects with difficult CRS. Although other studies have noted significant improvement in quality-of-life measures after routine FESS operations using other validated questionnaires, the SNOT-22 has not been used as an outcome measure for the CF population and, thus, no direct comparisons are available.33 These results warrant further evaluation of the protocol, including direct comparison with a control group with a larger sample size.
CONCLUSION
Prospective evaluation indicates significant improvement in symptoms with aggressive sinus surgery that includes MEMM combined with a comprehensive postoperative approach and was associated with reduced frequency of pulmonary exacerbation requiring hospitilization. Additional studies are necessary to determine whether this treatment paradigm will provide long-term symptom improvement and confer advantages in CF pulmonary outcomes.
Footnotes
Presented at the 23rd conference of the North American Cystic Fibrosis, Minneapolis, Minnesota, October 23, 2009, and the meeting of the American Rhinologic Society, Las Vegas Nevada, April 30, 2010
SM Rowe and BA Woodworth are inventors on a patent submitted regarding the possible activity of chloride secretagogues for therapy of sinus disease (Provisional Patent Application Under 35 U.S.C. §111[b] and 37 C.F.R. §1.53[c] in the United States Patent and Trademark Office). BA Woodworth is a consultant for Gyrus ENT and ArthroCare ENT. SM Rowe served as a consultant for Vertex Pharmaceuticals. The remaining authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Rowe SM, Miller S, Sorscher EJ. Cystic fibrosis. N Engl J Med 352:1992–2001, 2005. [DOI] [PubMed] [Google Scholar]
- 2. Brihaye P, Clement PA, Dab I, et al. Pathological changes of the lateral nasal wall in patients with cystic fibrosis (mucoviscidosis). Int J Pediatr Otorhinolaryngol 28:141–147, 1994. [DOI] [PubMed] [Google Scholar]
- 3. Cepero R, Smith RJ, Catlin FI, et al. Cystic fibrosis—An otolaryngologic perspective. Otolaryngol Head Neck Surg 97:356–360, 1987. [DOI] [PubMed] [Google Scholar]
- 4. Gentile VG, Isaacson G. Patterns of sinusitis in cystic fibrosis. Laryngoscope 106:1005–1009, 1996. [DOI] [PubMed] [Google Scholar]
- 5. Rosbe KW, Jones DT, Rahbar R, et al. Endoscopic sinus surgery in cystic fibrosis: Do patients benefit from surgery? Int J Pediatr Otorhinolaryngol 61:113–119, 2001. [DOI] [PubMed] [Google Scholar]
- 6. Regnis JA, Robinson M, Bailey DL, et al. Mucociliary clearance in patients with cystic fibrosis and in normal subjects. Am J Respir Crit Care Med 150:66–71, 1994. [DOI] [PubMed] [Google Scholar]
- 7. Kingdom TT, Lee KC, FitzSimmons SC, et al. Clinical characteristics and genotype analysis of patients with cystic fibrosis and nasal polyposis requiring surgery. Arch Otolaryngol Head Neck Surg 122:1209–1213, 1996. [DOI] [PubMed] [Google Scholar]
- 8. Ramsey B, Richardson MA. Impact of sinusitis in cystic fibrosis. J Allergy Clin Immunol 90:547–552, 1992. [DOI] [PubMed] [Google Scholar]
- 9. Jaffe BF, Strome M, Khaw KT, et al. Nasal polypectomy and sinus surgery for cystic fibrosis—A 10 year review. Otolaryngol Clin North Am 10:81–90, 1977. [PubMed] [Google Scholar]
- 10. Woodworth BA, Ahn C, Flume PA, et al. The delta F508 mutation in cystic fibrosis and impact on sinus development. Am J Rhinol 21:122–127, 2007. [DOI] [PubMed] [Google Scholar]
- 11. Benninger MS, Ferguson BJ, Hadley JA, et al. Adult chronic rhinosinusitis: Definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol Head Neck Surg 129:S1–S32, 2003. [DOI] [PubMed] [Google Scholar]
- 12. Payne SC. Empty nose syndrome: What are we really talking about? Otolaryngol Clin North Am 42:331–337, ix-x, 2009. [DOI] [PubMed] [Google Scholar]
- 13. Hopkins C, Gillett S, Slack R, et al. Psychometric validity of the 22-item Sinonasal Outcome Test. Clin Otolaryngol 34:447–454, 2009. [DOI] [PubMed] [Google Scholar]
- 14. Piccirillo JF, Thawley SE, Haiduk A, et al. Indications for sinus surgery: How appropriate are the guidelines? Laryngoscope 108:332–338, 1998. [DOI] [PubMed] [Google Scholar]
- 15. Lund VJ, Kennedy DW. Quantification for staging sinusitis. The Staging and Therapy Group. Ann Otol Rhinol Laryngol Suppl 167:17–21, 1995. [PubMed] [Google Scholar]
- 16. Lin SH, Kuo PH, Kuo SH, et al. Severity staging of chronic obstructive pulmonary disease: Differences in pre- and post-bronchodilator spirometry. Yonsei Med J 50:672–676, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lund VJ, Mackay IS. Staging in rhinosinusitus. Rhinology 31:183–184, 1993. [PubMed] [Google Scholar]
- 18. Holzmann D, Speich R, Kaufmann T, et al. Effects of sinus surgery in patients with cystic fibrosis after lung transplantation: A 10-year experience. Transplantation 77:134–136, 2004. [DOI] [PubMed] [Google Scholar]
- 19. Woodworth BA, Parker RO, Schlosser RJ. Modified endoscopic medial maxillectomy for chronic maxillary sinusitis. Am J Rhinol 20:317–319, 2006. [DOI] [PubMed] [Google Scholar]
- 20. Shatz A. Management of recurrent sinus disease in children with cystic fibrosis: A combined approach. Otolaryngol Head Neck Surg 135:248–252, 2006. [DOI] [PubMed] [Google Scholar]
- 21. Cho DY, Hwang PH. Results of endoscopic maxillary mega-antrostomy in recalcitrant maxillary sinusitis. Am J Rhinol 22:658–662, 2008. [DOI] [PubMed] [Google Scholar]
- 22. Henriksson G, Westrin KM, Karpati F, et al. Nasal polyps in cystic fibrosis: Clinical endoscopic study with nasal lavage fluid analysis. Chest 121:40–47, 2002. [DOI] [PubMed] [Google Scholar]
- 23. Hadfield PJ, Rowe-Jones JM, Mackay IS. A prospective treatment trial of nasal polyps in adults with cystic fibrosis. Rhinology 38:63–65, 2000. [PubMed] [Google Scholar]
- 24. Lim M, Citardi MJ, Leong JL. Topical antimicrobials in the management of chronic rhinosinusitis: A systematic review. Am J Rhinol 22:381–389, 2008. [DOI] [PubMed] [Google Scholar]
- 25. Cimmino M, Nardone M, Cavaliere M, et al. Dornase alfa as postoperative therapy in cystic fibrosis sinonasal disease. Arch Otolaryngol Head Neck Surg 131:1097–1101, 2005. [DOI] [PubMed] [Google Scholar]
- 26. Raynor EM, Butler A, Guill M, et al. Nasally inhaled dornase alfa in the postoperative management of chronic sinusitis due to cystic fibrosis. Arch Otolaryngol Head Neck Surg 126:581–583, 2000. [DOI] [PubMed] [Google Scholar]
- 27. Tomooka LT, Murphy C, Davidson TM. Clinical study and literature review of nasal irrigation. Laryngoscope 110:1189–1193, 2000. [DOI] [PubMed] [Google Scholar]
- 28. Passalacqua G, Ciprandi G, Canonica GW. The nose-lung interaction in allergic rhinitis and asthma: United airways disease. Curr Opin Allergy Clin Immunol 1:7–13, 2001. [DOI] [PubMed] [Google Scholar]
- 29. Senior BA, Kennedy DW. Management of sinusitis in the asthmatic patient. Ann Allergy Asthma Immunol 77:6–15, 1996. [DOI] [PubMed] [Google Scholar]
- 30. Senior BA, Kennedy DW, Tanabodee J, et al. Long-term results of functional endoscopic sinus surgery. Laryngoscope 108:151–157, 1998. [DOI] [PubMed] [Google Scholar]
- 31. Madonna D, Isaacson G, Rosenfeld RM, et al. Effect of sinus surgery on pulmonary function in patients with cystic fibrosis. Laryngoscope 107:328–331, 1997. [DOI] [PubMed] [Google Scholar]
- 32. Zemanick ET, Harris JK, Conway S, et al. Measuring and improving respiratory outcomes in cystic fibrosis lung disease: Opportunities and challenges to therapy. J Cyst Fibros 9:1–16, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Khalid AN, Mace J, Smith TL. Outcomes of sinus surgery in adults with cystic fibrosis. Otolaryngol Head Neck Surg 141:358–363, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]


