Abstract
Objectives:
In a large population-based study among adults in northern Europe the relation between occupational exposure and new-onset asthma was studied.
Methods:
The study comprised 13 284 subjects born between 1945 and 1973, who answered a questionnaire 1989–1992 and again 1999–2001. Asthma was defined as ‘Asthma diagnosed by a physician’ with reported year of diagnose. Hazard ratios (HR), for new-onset adult asthma during 1980–2000, were calculated using a modified job-exposure matrix as well as high-risk occupations in Cox regression models. The analyses were made separately for men and women and were also stratified for atopy.
Results:
During the observation period there were 429 subjects with new-onset asthma with an asthma incidence of 1.3 cases per 1000 person-years for men and 2.4 for women. A significant increase in new-onset asthma was seen for men exposed to plant-associated antigens (HR = 3.6; 95% CI [confidence interval] = 1.4–9.0), epoxy (HR = 2.4; 95% CI = 1.3–4.5), diisocyanates (HR = 2.1; 95% CI = 1.2–3.7) and accidental peak exposures to irritants (HR = 2.4; 95% CI = 1.3–4.7). Both men and women exposed to cleaning agents had an increased asthma risk. When stratifying for atopy an increased asthma risk were seen in non-atopic men exposed to acrylates (HR = 3.3; 95% CI = 1.4–7.5), epoxy compounds (HR = 3.6; 95% CI = 1.6–7.9), diisocyanates and accidental peak exposures to irritants (HR = 3.0; 95% CI = 1.2–7.2). Population attributable risk for occupational asthma was 14% for men and 7% for women.
Conclusions:
This population-based study showed that men exposed to epoxy, diisocyanates and acrylates had an increased risk of new-onset asthma. Non-atopics seemed to be at higher risk than atopics, except for exposure to high molecular weight agents. Increased asthma risks among cleaners, spray painters, plumbers, and hairdressers were confirmed.
Keywords: Atopics and non-atopics, high molecular weight agent, high-risk occupations, irritating agents, job-exposure matrix, low molecualr weight agent, occupational asthma, population attributable risk
INTRODUCTION
In the last decades there has been growing recognition of the importance of adult-onset asthma induced by workplace exposures (Torén and Blanc, 2009). Several systematic reviews have estimated that the population attributable risk (PAR) of adult-onset asthma in relation to different occupational exposures is approximately 15% (Blanc and Torén, 1999; Balmes et al., 2003; Torén and Blanc, 2009). The yielded estimates are, however, quite variable and in a prospective longitudinal study from Europe, the PAR was 6% in northern Europe compared with 23% in southern Europe and 12% in central Europe (Kogevinas et al., 2007). Furthermore, there are only few published papers reporting PAR separately for men and women, indicating a slightly lower PAR for men (9.1%) compared to women (11.5%), (Torén and Blanc, 2009).
More than 360 substances have been identified as potential inducers of asthma. Of these flour, isocyanates, latex, persulphate salts, aldehydes, animals, wood dusts, metals, enzymes account for 50–90% of reported cases (Vandenplas, 2011). Agents causing asthma are often divided into high-molecular weight (HMW), low-molecular weight (LMW) and irritating agents due to different mechanisms (Malo et al., 2009). The knowledge about occupational causes to adult-onset asthma is mainly based on case reports, clinical series and small cross-sectional studies. In the last decade, however, a few large population-based cohort studies and case-control studies have been published showing an increased asthma risk associated with cleaning work, irritants, solvents, pesticides, welding and passive smoking (Kogevinas et al., 2007; Kennedy et al., 2000; Karjalainen et al., 2001; Jaakkola et al., 2003; LeVan et al., 2006). Occupations shown to have high risk of asthma are farmers, painters, plastic workers, cleaners, spray painters and agricultural workers (Kogevinas et al., 1999). In the follow-up of the clinical samples (Stage 2) of the European Community Respiratory Health Survey (ECRHS II) a significant excess of asthma was seen in a group of 14 high-risk occupations including exposure to diisocyanates, reactive chemicals, flour dust, animal derived proteins and rubber latex. Increased risks were also observed for cleaning agents and for nursing (Kogevinas et al., 2007).
The assessment of exposure in general population-based studies regarding asthma is mostly based on either the occupational title per se, occupational title and additional information about intensity, duration, frequency of tasks etc. or job-exposure matrices (JEMs). The latter method has, during the last decade, gained increased support, as it is an un-biased way of assessing exposure. Recall bias is i.e. minimal as occupational titles are regarded as quite valid. An important JEM in this field was developed by Susan Kennedy in late 1990s (Kennedy et al., 2000) and has been frequently used in the ECRHS (Kogevinas et al., 2007; Zock et al., 2004). However, for this study, we have developed a JEM more suitable to exposure conditions in Northern Europe but based on the same principles as the JEM by Kennedy et al (2000).
This study is an analysis of new-onset asthma in relation to job exposure in a large random population from Northern Europe (Denmark, Estonia, Iceland, Norway and Sweden)—the RHINE study (Respiratory Health in Northern Europe). We used the occupational information at follow-up in 1999–2001 to retrospectively estimate the occupational risk factors for new-onset adult asthma in the time period between 1980 and 2000.
METHODS
Study population
The original study population was 21 802 subjects born between 1945 and 1973 participating in Stage 1 of the ECRHS I during 1989–1992. The study population was a randomly selected population from the general population from seven geographic centres (Aarhus, Denmark; Reykjavik, Iceland; Bergen, Norway; Tartu, Estonia; and Gothenburg, Umeå, and Uppsala, Sweden). In 1999–2001 the subjects were mailed a follow-up questionnaire, which was answered by 16 202 subjects (74%), (Torén et al., 2004; Holm et al., 2007; Omenaas et al., 2008).
Questionnaire and definitions
In the baseline study (1989–1992), all subjects completed the ECRHS screening questionnaire comprising items about different asthma-symptoms the last 12 months, current use of asthma medication and allergic rhinitis. At follow-up (1999–2001) all subjects completed a comprehensive questionnaire comprising a full occupational history and questions about self-reported asthma and smoking habits.
New-onset asthma was defined as a positive answer to ‘Do you have or have you ever had asthma after the age of 16?’ and ‘Have you ever had asthma diagnosed by a physician?’ (Torén et al., 1993). Atopy was defined as a positive answer to ‘Do you have hay fever or any other nasal allergy?’ Subjects at follow-up were classified as never-smokers or ever-smokers.
Assessment of occupational exposure
All occupations were classified according to ISCO-88 (International Standard Classification of Occupations), (ILO, 1991). If the national standard of classification differed as compared with ISCO-88, these codes would have been transformed according to the international standard.
We developed a JEM for the countries in northern Europe (N-JEM) based on the same principle used by others (Kogevinas et al., 2007; Kennedy et al., 2000; Kennedy et al., 2011), here named SK-JEM. The study of Kogevinas et al. (2007) showed lower risk of occupational new-onset asthma in northern Europe compared with south and middle Europe. This was a reason to modify the existing JEM to make it more adaptable to working conditions in northern Europe, which might produce higher hazard ratios (HR). All occupations were assessed as being exposed, not exposed or ‘uncertain or low exposed’ by two occupational hygienists (L.L, A.D-H). The assessments were discussed with two specialists in occupational medicine (K.T, E.A) until consensus was reached. An exposed occupation was defined based on the assumption that at least half of the subjects with this specific code should have a high probability of being exposed to the critical agents.
The developed N-JEM includes six main groups: HMW agents, LMW agents, irritating agents, ‘accidental peak exposure to irritants’, an ‘uncertain or low exposed group’, and an unexposed reference group. The HMW, LMW, and irritating agent groups have five, four and seven subgroups, respectively (Table 1). Compared with the SK-JEM, some of the HMW subgroups are merged to increase the number of subjects in the groups. Among LMW agents, acrylates and epoxy compounds are two new groups in the N-JEM, which mainly are included in ‘highly reactive chemicals’ in the SK-JEM. Within the diisocyanate group we have included ‘plumbers and pipe fitters’, motor vehicle mechanics, and ‘welder and flame cutters’ besides those in the SK-JEM. Cleaning agents are moved from the LMW agents to the irritating agents in the N-JEM. Irritating agents include several groups that are separate groups in the SK-JEM. One subgroup in the N-JEM, called ‘inorganic dusts and welding fumes,’ is similar to the main group ‘irritant gases and fumes’ in the SK-JEM, but the latter also include organic dusts and most of the ISCO-codes in ‘cleaning agents’. The most common occupations (ISCO-codes) in each subgroup in the N-JEM are presented in Table 1. A certain occupation can be classified as exposed in more than one exposure category. For instance ‘moulder, core maker’ is an occupation with potential exposure to acrylates, diisocyanates, and ‘inorganic dusts and fumes’. Veterinary assistants are classified as exposed to both HMW animal derived antigens and latex protein. The reference population consisted of subjects working in administrative or clerical jobs, teachers, students as well as those being unemployed or homemakers.
Table 1.
The N-JEM used in the study.
| Main job-exposure groups and subgroups | Example of the most common occupations (4 digit) or groups (not in size order) |
|---|---|
| 1. HMW agents | |
| Animal derived antigens including fish | Animal producers and related workers, animal and crop producers, fishery workers, butchers. |
| Plant-associated antigens including cereal, tobacco and brewery workers | Field crop and vegetable growers, horticulturists, gardeners, bakers, brewers wine and other beverage machine operators. |
| Arthropods, mites, bio-aerosols, enzymes | Grain, milling, spice processing operators, bakers, machinist tool setters and op., agricultural labourers. |
| Latex protein | Dentists, veterinarians, nurses, institution-based and home-based personal care workers. |
| Pharmaceutical product antigens | Pharmacists general, pharmaceutical assistants, nurses, fish farming workers |
| 2. LMW agents | |
| Reactive chemicals (aldehydes, amines etc) | Chemists, hairdressers, construction painters, spray painters (code 7142), printing machine op. |
| Acrylates | Dentists, dental assistants, plumbers and pipe fitters, electrical and electronic equipment mechanics |
| Epoxy chemicals | Floor layers and tile setters, plumbers and pipe fitters, spray painters, motor vehicle mechanics |
| Diisocyanates | Fire fighters, plumbers and pipe fitters, spray painters, welders, motor vehicle mechanics |
| 3. Irritating agents | |
| Cleaning agents | Domestic helpers and cleaners, cleaners in offices, hotels, building caretakers, window cleaners |
| Wood and paper dusts | Builders, carpenters, other building trades, wood process plant op, printing machine op. |
| Inorganic dusts and fumes | Plumbers, building and related electricians, motor vehicle fitters, welders, machinery mechanics |
| Textile dusts | Tailors, upholsters and related workers, sewing op., bleaching, dying and cleaning machine op. |
| Metal working fluids | Machine tool operators, machinist tool setter and op., machinery mechanics, machine tool op. |
| Vehicle/motor exhaust | Postmen, cooks, car repair work (code 7231), motor vehicle drivers, other drivers. |
| ETS | Social work associates, waiters, waitresses, musicians, singers, police officers, prison guards |
| 4. Accidental peak exposure to irritants | Fire fighters, police officers, welders, sheet metal workers, ore and metal furnace operators |
| 5. Uncertain or low exposed | Civil engineering technicians, electrical technicians, electronics and telecommunication technicians, mechanical technicians, child-care workers, mechanical machinery assemblers |
| 6. Reference group | Teaching and business professionals, office clerks, administrative associate professionals |
In addition to the JEM we classified exposure by using a list of occupations associated with high risk of new-onset asthma together with environmental tobacco smoke (ETS). We used the same occupational categories and ISCO-codes as in the ECRHS II study (Kogevinas et al., 2007) with a few changes. ‘Building workers’ and plumbers were extracted from the ‘construction and mining group’ and ‘child and other personal care workers’ formed a separate group from ‘other medical and pharmacy, excluding nurses’.
Based on the N-JEM every year of observation from 1980–2000 (or from the age of 16 years) was classified as exposed, ‘uncertain or low exposed’, unexposed or missing (if occupation or start and/or stop-year were missing) and associated with the specific employment (ISCO-code) each year. Subjects were excluded if they reported onset of asthma before 1980, asthma but not physician-diagnosed, gave no information about jobs during 1980–2000. This resulted in a study population of 13 284 subjects. There were 13 men and 15 women with new-onset asthma, where we had no information about employments at asthma onset. Therefore these cases were excluded and could not be used in the calculations.
Occupational history included all jobs with at least 6 months of employment. Person-years (p-years) were calculated from 1980 or from the age of 16 years if they had not reached that age at 1980 up to year 2000 or until obtaining a diagnosis of asthma. P-years for the reference population also included years from subjects unexposed 1980 or older than 15 years until first exposed job. If asthma developed within 2 years after the end of the employment it is calculated as within the employment, and the exposure period is extended until the year of diagnosis.
Statistical analyses
All statistical analyses were performed with SAS version 9.2. Cox regression analyses were performed with p-years under observation as the dependent variable and asthma as an event. In the analyses men and women were analysed separately and together but in the tables only presented separately. Regression analyses were performed for all individuals, separated in atopics and non-atopics and subjects less than 41 years of age and those 41 and above (Tables not presented). HR and 95% CI were adjusted for age and atopy. In additional analyses HR were also adjusted for smoking but notified in the Tables only if significances were changed. When adjusting for smoking, 313 subjects disappeared because of un-known smoking habits. If there were less than three cases of new-onset asthma in the group, HR were not presented.
PAR for the proportion of new-onset asthma due to exposure to agents at the workplace causing asthma was calculated as PAR = (HR−1/HR)*proportion of exposed asthma cases (Greenland, 2008).
RESULTS
Basic characteristics of the study population are shown in Table 2. The incidences of adult-onset asthma during 1980–2000 were 1.3 asthma cases per 1000 p-years for men and 2.4 cases per 1000 p-years for women, 136 and 293 asthma cases respectively for men and women. Mean age and smoking habits were similar in both sexes.
Table 2.
Characteristics of the study population of 13 284 subjects from northern Europe.
| Men | Women | |
|---|---|---|
| Subjects (%) | 6 253 (47.1) | 7 031 (52.9) |
| Age the year 2000, mean (SD) | 41.1 (7.2) | 40.8 (7.3) |
| Never-smokers (%) | 2 844 (45.5) | 3 194 (45.4) |
| Ever-smokers (%) | 3 263 (52.2) | 3 670 (52.2) |
| Unknown smoking habits (%) | 146 (2.3) | 167 (2.4) |
| Not exposed (%) | 2 241 (35.9) | 3 372 (48.0) |
| Exposed (%) | 3 721 (59.5) | 3 257 (46.3) |
| Uncertain exposure (%) | 291 (4.7)a | 402 (5.7)b |
| Asthma incidence/1000 p-years | 1.3 | 2.4 |
aThere were additional 449 men, who had at least one employment with uncertain exposure.
bThere were additional 337 women, who had at least one employment with uncertain exposure.
Among men the HR of new-onset asthma during exposed time was 1.4 (95% CI = 0.96–1.9) and among women the risk was (HR = 1.2; CI = 0.95–1.6), Table 3, 4. There was an increased risk of new-onset asthma in men exposed to HMW ‘plant associated antigens, cereal, tobacco, etc.’ (HR = 3.6; CI = 1.4–9.0). In subjects exposed to LMW agents, there were increased risks among men exposed to epoxy (HR = 2.4; CI = 1.3–4.5) and diisocyanates (HR = 2.1; CI = 1.2–3.7) (Table 3).
Table 3.
HR and 95% CI of new-onset asthma in job-exposure groups of men according to the JEM for northern Europe adjusted for age and atopy. Atopics and non-atopics are adjusted for age.
| Job-exposure groups (men) | Person-years all | AsthmaAll/atopics/non atopics | All exposed, adjusteda HR (95% CI) | Atopics, adjustedb HR (95% CI) | Non-atopics, adjustedb HR (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| Referents | 51 541 | 59/33/26 | 1 | 1 | 1 | |||
| Any exposure in groups 1–4 | 48 430 | 70/34 /36 | 1.4 | 0.96–1.9 | 1.3 | 0.8–2.1 | 1.5 | 0.9–2.4 |
| 1. HMW agents | 8770 | 15/7/8 | 1.5 | 0.9–2.7 | 1.3 | 0.6–3.0 | 1.8 | 0.8–3.9 |
| Plant-associated antigens, cereal, tobacco, etc. | 1352 | 5/2/3 | 3.6 | 1.4–9.0 | NAc | NAc | 4.1 | 1.2–13.6 |
| Arthropods, mites, bio-aerosols, enzymes | 3948 | 6/3/3 | 1.3 | 0.6–3.1 | 1.2 | 0.4–3.9 | 1.5 | 0.4–4.8 |
| Latex protein | 2618 | 5/3/2 | 1.7 | 0.7–4.2 | 1.8 | 0.6–7.0 | NA | NA |
| 2. LMW agents | 11 249 | 17/5/12 | 1.4 | 0.8–2.3 | 0.8 | 0.3–2.0 | 2.0 | 1.0–4.1 |
| Reactive chemicals | 2764 | 3/1/2 | 1.0 | 0.3–3.1 | NA | NA | NA | NA |
| Acrylates | 4078 | 8/1/7 | 1.8 | 0.8–3.7 | NA | NA | 3.3 | 1.4–7.5 |
| Epoxy chemicals | 4249 | 11/3/8 | 2.4 | 1.3–4.5 | 1.3 | 0.4–4.3 | 3.6 | 1.6–7.9 |
| Diisocyanates | 6158 | 14/5/9 | 2.1 | 1.2–3.7 | 1.5 | 0.6–3.8 | 2.8 | 1.3–6.0 |
| 3. Irritating agents | 35 272 | 53/27/26 | 1.4 | 0.96–2.0d | 1.3 | 0.8–2.3 | 1.5 | 0.9–2.6 |
| Cleaning agents | 1749 | 6/2/4 | 2.6 | 1.1–6.1d | NA | NA | 4.1 | 1.4–12.1 |
| Wood and paper dusts | 5367 | 7/5/2 | 1.2 | 0.5–2.5 | 1.5 | 0.6–3.8 | 0.7 | 0.2–3.1 |
| Inorganic dusts and fumes | 16 517 | 26/12/14 | 1.5 | 0.9–2.3 | 1.3 | 0.7–2.6 | 1.6 | 0.9–3.1 |
| Metal working fluids | 3843 | 4/1/3 | 0.9 | 0.3–2.6 | NA | NA | 1.5 | 0.5–4.9 |
| Vehicle/motor exhaust | 13319 | 15/6/9 | 1.0 | 0.6–1.8 | 0.7 | 0.3–1.8 | 1.3 | 0.6–2.8 |
| ETS | 1974 | 4/3/1 | 1.5 | 0.6–4.3 | 1.8 | 0.5–5.9 | NA | NA |
| 4. Accidental peak exposure to irritants | 3945 | 11/5/6 | 2.4 | 1.3–4.7 | 2.0 | 0.8–5.2 | 3.0 | 1.2–7.2 |
| 5. Uncertain or low exposed | 7565 | 7/2/5 | 0.8 | 0.4–1.8 | NA | NA | 1.4 | 0.5–3.6 |
aadjusted for age and atopy.
badjusted for age.
cNA= not applicable (<3 asthma cases).
dnot significant when adjusted also for smoking.
No asthma cases were seen in men exposed to HMW agents from pharmaceutical product antigens or irritating agents from textile dust (355 and 187 p-years in the respective sub group).
Less than 3 asthma cases were seen in male exposed to animal derived antigens (2130 p-years).
Table 4.
HR and 95% CI of new-onset asthma in job-exposure groups of women according to the JEM for northern Europe adjusted for age and atopy. Atopics and non-atopics are adjusted for age.
| Job-exposure groups (women) | Person-years all | Asthma All/atopics/ non atopics | All exposed, adjusteda HR (95% CI) | Atopics, adjustedb HR (95% CI) | Non-atopics, adjustedb HR (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| Referents | 75 564 | 174/107/67 | 1 | 1 | 1 | |||
| Any exposure in groups 1–4 | 38 718 | 107/66/41 | 1.2 | 0.95–1.6c | 1.2 | 0.9–1.7 | 1.2 | 0.8–1.7 |
| 1. HMW agents | 23 554 | 63/42/21 | 1.2 | 0.9–1.6 | 1.4 | 0.94–1.9 | 1.0 | 0.6–1.6 |
| Latex protein | 21 258 | 59/40/19 | 1.3 | 0.9–1.7 | 1.4 | 1.0–2.1 | 1.0 | 0.6–1.6 |
| Pharmaceutical product antigens | 4223 | 13/11/2 | 1.3 | 0.8–2.3 | 1.9 | 0.99–3.4 | NAd | NAd |
| 2. LMW agents | 3889 | 10/4/6 | 1.1 | 0.6–2.0 | 0.7 | 0.3–1.8 | 1.7 | 0.8–4.0 |
| Reactive chemicals | 2557 | 10/4/6 | 1.6 | 0.8–3.0 | 1.0 | 0.4–2.6 | 2.7 | 1.2–6.2c |
| 3. Irritating agents | 12 383 | 37/20/17 | 1.3 | 0.9–1.9 | 1.1 | 0.7–1.8 | 1.5 | 0.9–2.6 |
| Cleaning agents | 4752 | 21/10/11 | 2.0 | 1.2–3.0 | 1.5 | 0.8–2.9 | 2.6 | 1.4–5.0 |
| Textile dust | 1088 | 3/1/2 | 1.1 | 0.4–3.5 | NA | NA | NA | NA |
| Vehicle/motor exhaust | 2836 | 7/5/2 | 1.1 | 0.5–2.3 | 1.3 | 0.5–3.2 | NA | NA |
| ETS | 2417 | 9/5/4 | 1.6 | 0.8–3.1 | 1.4 | 0.6–3.5 | 1.9 | 0.7–5.2 |
| 5. Uncertain or low exposed | 6351 | 12/7/5 | 0.8 | 0.5–1.5 | 0.8 | 0.4–1.8 | 0.8 | 0.3–2.1 |
aadjusted for age and atopy
badjusted for age
c not significant if also adjusted for smoking
dNA=not applicable (<3 asthma cases).
No asthma cases were seen in women exposed to HMW agents from ‘Plant assoc. antigens, cereal, tobacco etc., ‘arthropods, mites bio-aerosols and enzymes’, LMW agents from acrylates, epoxy chemicals and diisocyanates, metal working fluids or accidental peak exposure to irritants (313–1176 p-years/group).
Asthma cases (<3) were seen in women exposed to HMW agents from ‘animal derived plants’, irritants from ‘wood and paper dusts’ and inorganic dusts and fumes (532–987 p-years/group).
There was an increased asthma risk among subjects exposed to cleaning agents, and this was true for both men (HR = 2.6; CI = 1.1–6.1) and women (HR = 2.0; CI = 1.2–3.0). An increased asthma risk could also be shown among men exposed to accidental peak exposures to irritants (HR = 2.4; CI = 1.3–4.7) (Tables 3, 4).
When stratifying for atopy the analyses in many cases lost power due to low numbers resulting in wide confidence intervals (CIs). Increased asthma risks were seen in female atopics exposed to pharmaceutical products (HR = 1.9; CI = 0.99–3.4) and latex protein (HR = 1.4; CI = 1.00–2.1), (Table 4). In male atopics we could not show increased asthma risks (Table 3). Significantly increased asthma risks were seen among non-atopic men exposed to acrylates (HR = 3.3; CI = 1.4–7.5), as well as among those exposed to epoxy compounds (HR = 3.6; CI = 1.6–7.9), diisocyanates (HR = 2.8; CI = 1.3–6.0), and also cleaning agents (HR = 4.1; CI = 1.4–12.1), and accidental peak exposures to irritants (HR = 3.0; CI = 1.2–7.2), (Table 3). Among non-atopic women the asthma risks were increased in those exposed to reactive chemicals (HR = 2.7; CI = 1.2–6.2) and cleaning agents (HR = 2.6; CI = 1.4–5.0), (Table 4).
Occupations with the highest risks for new-onset asthma in men were spray-painters, plumbers, cleaners, food and tobacco processing workers, and child and other personal care workers, (Table 5). In male spray-painters, the risk was very high (HR = 7.5; [CI = 2.4–24.1]). The risk was also high in male plumbers (HR = 4.0; CI = 1.6–10.0) and the non-atopic plumbers (HR = 6.0; CI = 2.1–17.2). Among women the occupations with highest risks for new-onset asthma were drivers, cleaners, nurses, and hairdressers. Non atopic ‘female hairdressers’ was also a group with high asthma risk (HR = 4.1; CI = 1.7–10.3), (Table 6).
Table 5.
HR and 95% CI of new-onset asthma in men working in high-risk occupational groups together with ETS adjusted for age and atopy. Atopics and non-atopics are adjusted for age.
| Occupational group (men) | Person-years all | Asthma All/atopics/non atopics | All exposed, adjusteda HR (95% CI) | Atopics, adjustedb HR (95% CI) | Non-atopics, adjustedb HR (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| Referents | 57 668 | 67/38/29 | 1 | 1 | 1 | |||
| Cleaners, building caretakers | 1749 | 6/2/4 | 2.6 | 1.1–5.9c | NAd | NAd | 3.9 | 1.4–11.4 |
| Child and other personal care work | 1640 | 5/3/2 | 2.5 | 1.0–6.3 | 2.7 | 0.8–8.7 | NA | NA |
| Building workers not carpenters | 6456 | 9/7/2 | 1.3 | 0.6–2.5 | 1.9 | 0.8–4.2 | NA | NA |
| Plumbers and pipe fitters | 1209 | 5/1/4 | 4.0 | 1.6–10.0 | NA | NA | 6.0 | 2.1–17.2 |
| Agriculture and forestry | 2862 | 3/1/2 | 0.9 | 0.3–2.8 | NA | NA | NA | NA |
| Food and tobacco processing | 1365 | 4/3/1 | 2.7 | 0.97–7.3 | 3.8 | 1.2–12.3 | NA | NA |
| Welders and flame cutters | 1262 | 3/1/2 | 2.2 | 0.7–6.9 | NA | NA | NA | NA |
| Metal making and treating | 1604 | 4/3/1 | 2.1 | 0.8–5.8 | 2.9 | 0.9–9.4e | NA | NA |
| Other metal workers | 7506 | 8/4/4 | 1.0 | 0.5–2.0 | 1.0 | 0.3–2.7 | 1.0 | 0.4–2.8 |
| Electrical processors | 3891 | 6/1/5 | 1.4 | 0.6–3.1 | NA | NA | 2.5 | 0.96–6.4 |
| Spray painters | 363 | 3/1/2 | 7.5 | 2.4–24.1 | NA | NA | NA | NA |
| Remainder transportation, storage | 2074 | 5/3/2 | 2.2 | 0.9–5.5 | 2.8 | 0.9–9.3e | NA | NA |
| Remainder blue collar worker | 2596 | 4/1/3 | 1.3 | 0.5–3.5 | NA | NA | 2.1 | 0.6–6.8 |
| Drivers | 6189 | 6/2/4 | 0.9 | 0.4–2.0 | NA | NA | 1.2 | 0.4–3.5 |
| ETS | 1442 | 3/2/1 | 1.8 | 0.6–5.7 | NA | NA | NA | NA |
aadjusted for age and atopy.
badjusted for age.
cnot significant if also adjusted for smoking.
dNA=not applicable (<3 asthma cases).
esignificant if also adjusted for smoking.
Table 6.
HR and 95% CI of new-onset asthma in women working in high-risk occupational groups together with ETS adjusted for age and atopy. Atopics and non-atopics are adjusted for age.
| Occupational group (women) | Person-years all | Asthma All/atopics/non atopics | All exposed adjusteda HR (95% CI) | Atopics, adjustedb HR (95% CI) | Non-atopics, adjustedb HR (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| Referents | 77 432 | 180/116/64 | 1 | 1 | 1 | |||
| Cleaners, building caretakers | 4752 | 21/10/11 | 1.9 | 1.2–3.0 | 1.4 | 0.7–2.7 | 2.8 | 1.5–5.3 |
| Nurses | 7251 | 24/18/6 | 1.5 | 0.95–2.1c | 1.8 | 1.1–2.9 | 0.9 | 0.4–2.2 |
| Child and other personal care worker | 15480 | 42/28/14 | 1.2 | 0.9–1.7 | 1.4 | 0.9–2.1 | 1.0 | 0.6–1.8 |
| Hairdresser, beautician | 1579 | 8/3/5 | 1.9 | 0.95–3.9c | 1.0 | 0.3–3.3 | 4.1 | 1.7–10.3 |
| Food and tobacco processing | 1580 | 3/2/1 | 0.8 | 0.3–2.6 | NAd | NAd | NA | NA |
| Textile and leather workers | 1201 | 3/1/2 | 1.0 | 0.3–3.1 | NA | NA | NA | NA |
| Drivers | 393 | 3/2/1 | 3.7 | 1.2–11.6 | NA | NA | NA | NA |
| Remainder blue collar worker | 1292 | 3/3/0 | 0.9 | 0.3–2.8 | 1.3 | 0.4–4.0 | NA | NA |
| Not classified workers | 2273 | 5/2/3 | 0.9 | 0.4–2.2 | NA | NA | 1.6 | 0.5–5.1 |
| ETS | 1324 | 5/3/2 | 1.6 | 0.7–3.9 | 1.5 | 0.5–4.6 | NA | NA |
aadjusted for age and atopy, badjusted for age, cnot significant when also adjusted for smoking, dNA=not applicable (<3 asthma cases).
Men of age 40 years or younger seemed to be at highest risk of new-onset asthma if exposed to diisocyanates, cleaning agents or accidental peak exposures, while men older than 40 years seemed to be at higher risk if exposed to plant-associated antigens. For women, age did not seem to have an effect of new-onset asthma if exposed to cleaning agents, but younger women seemed to be at higher risk if exposed to reactive chemicals (figures not shown).
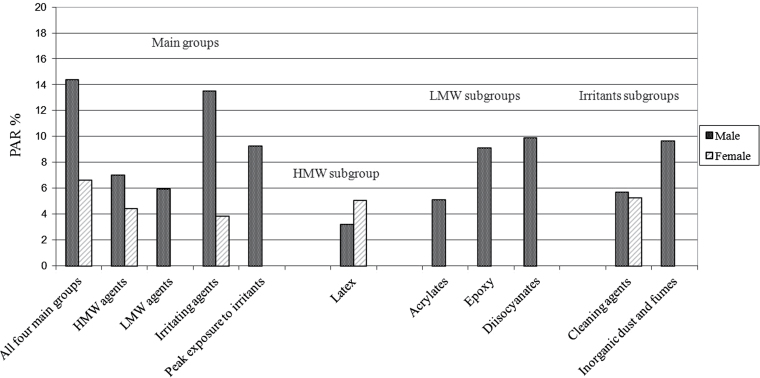
PAR for new-onset asthma was 14% among men and 7% among women for any exposure in the four main groups defined in the N-JEM. PAR for specific exposure groups varied from 3 to 14% (Figure 1).
Fig 1.
PAR for new-onset asthma in male and female job-exposure groups according to the N-JEM for northern Europe.
DISCUSSION
A key finding from the present general population-based study was that men exposed to highly reactive chemicals, such as epoxy, diisocyanates, and acrylates, had a marked increased risk of new-onset asthma. It was especially intriguing that exposure to epoxy increased the risk for new-onset asthma, particularly pronounced for non-atopic subjects. Another interesting result was that men exposed to accidental peak exposure to irritants had a high risk of new-onset asthma. We confirmed earlier observations regarding increased asthma risks among cleaners, male spray painters and plumbers, and female hairdressers. In the N-JEM we have considered more occupations to be exposed to epoxy compounds, acrylates, and diisocyanates compared with the SK-JEM.
The strength of the present study is the general population-based frame, which is important for the external validity of the results. The population emanates from five countries in northern Europe, but we believe that the results are valid also for other industrialized regions worldwide. Another advantage is the use of a rather unbiased assessment of the exposure—a JEM based on occupational titles. Furthermore, we are taking into account both the timing of the exposure by calculating person-years of exposures in each specific job and the time of onset of asthma, which associate new-onset asthma with the exposure at onset. If asthma develops within 2 years after changing job, the asthma and extended time period is included in that specific job.
The study design has also some limitations. The most obvious is the retrospective estimate of the outcome and that it is based on self-reported physician-diagnosed asthma. Torén et al (1993) have previously shown that the definitions ‘do you have or have you ever had asthma’ or ‘have you ever had asthma diagnosed by a doctor’ together with a reported year of onset of asthma have high specificity and low sensitivity, eventually leading to an under detection of subjects with asthma. If there are subjects with undiagnosed asthma this might lead to a bias in hazard risks, which would lead to underestimation of incidence risks if the asthma case is diagnosed during an unexposed job and to overestimation if the asthma case is diagnosed during an exposed job. The reported year of onset of asthma is sensitive to misclassification, meaning that a subject may report an incorrect year. There are studies validating the self-reported year of diagnosis or disease onset among subjects with asthma, showing that almost all subjects with asthma reported precise years-of-onset ±2 years (Torén et al., 2006; Pattaro et al., 2007).
The study period was 1980–2000 and it might be more difficult to recall some short-time jobs during the first decade together with start- and stop-year leading to some bias. At the same time these people were quite young (born 1945–1973).
Self-reported job titles linked to a JEM might give potential misclassification. An imprecise job title like metal work will in most cases not give an ISCO code, and the job will not be included in the calculations. Uncertainties in job titles might give wrong ISCO-codes and thus a misclassification. If, in a group with few asthma cases like ‘plant associated antigens’ with significant risk of new-onset asthma, one of the asthma cases is wrongly classified to that group it might lead to insignificance and wider CIs.
In this study the average response rate was 74%. In an analysis of non-responders in a recent general population-based study from Sweden there were no differences regarding the prevalence of asthma, cough or wheeze between responders and non-responders (Rönmark et al., 2009). Even if smokers and unemployed were overrepresented among the non-responders, the asthma risk in relation to occupational exposures was similar among responders and non-responders (Rönmark et al., 2009). Hence, we conclude that the obtained relative risks were likely not to be biased by non-response selection.
Despite the relatively large size of the study, one important limitation is the lack of power. There are a number of job-exposure groups and occupational groups with limited number of subjects resulting in wide CIs. In order to increase the number of subjects in some job-exposure groups we merged subjects with similar exposures compared with the SK-JEM. For example ‘plant associated antigens, cereal, tobacco etc.’ includes flour-associated antigens, other plant-associated antigens (tobacco, fruit, tea, coffee, brewery, and wine work), and mixed agents from agricultural work (not animal).
The present N-JEM is in its structure rather similar to the SK-JEM. With the N-JEM we could show an increase in new-onset asthma for men exposed to epoxy compounds and acrylates, while most of these occupations were included in a bigger group called highly reactive chemicals in the SK-JEM. Merging of similar groups in the N-JEM, like ‘plant associated antigens’, resulted in an increased asthma risk for men, which could not be shown for the individual groups. In the N-JEM we have chosen not to include the verification steps and there are several reasons for that. Due to the study size a verification step should be quite time consuming. In the postal questionnaire used in the study, subjects were asked about all employments 6 months or longer specifying trade and tasks/occupation. We did not ask what the firm, company or organisation did or what services they provided. In many of the answers the trade was also missing, why the exposure after the verification step still should remain unclear for most of the subjects checked. In a publication, where the verification steps have been used, the outcome barely changed (Zock et al., 2004). In another investigation the verification step was checked among workers in animal health technology, pastry making, and dental hygiene, where the exposure situations were quite well investigated and compared with self-reported and investigator-scored exposure (Suarthana et al., 2009). The study showed that 366 job titles from 227 participants needed exposure verification and good knowledge about the exposure at the workplaces. In two out of nine groups the HR changed considerably after the verification step, but for the other seven groups the changes were limited with small changes in the 95% CI. This shows that the verification step can somewhat improve the results, but it will demand much more detailed questions about job titles and exposure situations.
We showed an increased risk of new-onset asthma in relation to several occupational exposure groups, but the most novel finding was the increased risk for asthma among workers exposed to epoxy agents. However, these findings will have to be judged with some caution as the majority of the exposed cases originate from two occupations—plumbers and pipe fitters (5 asthma cases) and car and varnisher painters (3 asthma cases), where the workers might be exposed to both epoxy compounds and diisocyanates. From clinical experiences we have noticed that plumbers and pipe fitters in the Nordic countries often use epoxy and acrylate glues to join plastic tubes and diisocyanates (1-component) for isolation in long distance pipes. Together with motor vehicle mechanics, these three groups constitute about 90% of the asthma cases in the epoxy group and 30% of the diisocyanate group. At the same time these groups make up 90% of the employments (a subject can have more than one employment in a specific occupation) in the epoxy group and 64% in the diisocyanate group. There is, however, one cross-sectional study from Finland on construction painters, where asthma was related to both epoxy and polyurethane compounds, reflecting the methodological problem of concomitant use of products containing more than one asthma-inducing agent (Kaukiainen et al., 2008).
Men and women exposed to cleaning agents showed increased risk for asthma, which is in line with previous publications (Kogevinas et al., 2007). High accidental peak exposure of irritants have been associated with airway inflammation and increased risk for asthma among pulp and paper mill workers with recurring gassing events (Olin et al., 2004; Henneberger et al., 2005; Andersson et al., 2006). In the present study we showed a high asthma risk among men in occupations associated with accidental peak exposure to irritants, which was also shown in ECRHS II (Kogevinas et al., 2007). We used the same ISCO-codes as in the SK-JEM, and in our study, welders and flame cutters, sheet metal workers, police officers, and fire fighters were the most common occupations. The estimated risk was quite high (2.4) and even higher among non-atopics (3.0). These results emphasize that accidental peak exposures to irritants may induce airway inflammation and subsequent development of asthma.
When analysing the risk of asthma in certain a priori defined high-risk occupations the expectation was to find increased risks. Among men the highest risk was found among spray painters, where the risk estimate of 7.5 indicates that almost all cases of asthma among spray-painters is due to the occupational exposure. Other male high-risk occupations were plumbers, cleaners, and food and tobacco processing workers. Child and other personal care workers also showed significantly increased new-onset asthma (HR = 2.5; CI = 1.0–6.3). This is in line with an article by Mirabelli et al. (2007), which showed that ‘other health care workers’ (not nurses) experienced risk of new-onset asthma. They also showed that, in Sweden, quite few in this job category used latex gloves, why the asthma might be more due to cleaning agents and disinfectants. This is a job category that should be investigated more. Female atopic nurses showed a significant asthma risk (HR = 1.8; CI = 1.1–2.9), which might indicate that latex gloves could be a risk factor. Female cleaners, hairdressers, and drivers showed increased asthma risks, which confirm earlier results.
In this study we decided to stratify by sex and atopy even if this might increase the CIs. We have shown differences in outcome for men and women as well as for atopics and non-atopics for several exposure groups and occupations. If the analyses were not stratified by sex but adjusted for sex, atopy and age, we got significant asthma risk all exposed (HR = 1.3; CI = 1.0-1.5) and borderline risk for all atopics. Increased asthma risk was seen for exposure to epoxy, diisocyanates, cleaning agents and accidental peak exposure with somewhat lower HRs compared with men but with both higher and lower CIs. There was also an increased asthma risk for all exposed to irritating agents (HR = 1.3; CI = 1.0-1.7) as well as the non-atopics in this group. There was no significant increase in asthma risk for exposure to plant-associated antigens and acrylates. There was a borderline significant increase in asthma risk for HMW agents (HR = 1.3; CI = 0.98–1.7) and also for the atopics (HR = 1.4; CI = 0.98–1.9). In groups where one sex dominated the number of p-years (latex, epoxy, diisocyanates, spray painters, plumbers) the HR and CIs did not change very much. In exposure groups with increased risk of new-onset asthma we calculated p for interaction between men and women and atopics and non-atopics. P for interaction showed significant differences for sex for ‘all exposed’, HMW agents, latex, irritating agents, cleaning agents, child and other personal care workers and borderline significance for food and tobacco processing and nurses. There were significant differences between atopics and non-atopics for ‘all exposed’, LMW agents, cleaning agents and borderline significance for HMW agents, reactive chemicals, acrylates, epoxy, and hairdressers. For those groups with no asthma cases among women (acrylates, epoxy, diisocyanates, accidental peak exposure to irritants, spray painters, plumbers) it is not relevant to calculate a P-value for interaction.
Atopy is considered as an important risk factor for new-onset asthma in occupations classified as exposed to HMW proteins (Vandenplas, 2011, Kogevinas et al., 2007). In our study this was only shown for female atopics exposed to latex protein and pharmaceutical products. If not stratifying for sex there was a borderline significant asthma risk for subjects exposed to latex protein (HR = 1.3; CI = 0.98–1.7) and significant risk for the atopics (HR = 1.5; CI = 1.0–2.1). Among male, the only occupational group where atopics had an increased asthma risk was food and tobacco processing workers. An explanation might be that the group includes several occupations, where workers might be exposed to HMW agents. For LMW agents and irritants, our analyses indicate that non-atopics were at highest asthma risks. This was also true if not stratifying for sex. Wang et al. (2010) have shown that non-atopic asthma was significantly associated with exposure to LMW asthmagens including industrial cleaning agents.
In the analyses we have adjusted for age and atopy (first column in the tables), but we also did the analyses unadjusted for those not stratified by age or atopy. There were very small differences in HRs and CIs with and without adjusting for atopy and the significant asthma risks were not changed, why we do not consider atopy as a potential confounder.
The PAR of adult asthma was 14.4% for men and 6.6% for women for the study period 1980–2000. This is quite similar to a recent published general population-based study from west Sweden, which found a higher PAR among men, 17.3%, compared with women, 5.1% (Torén et al., 2011). There are few studies with gender-specific estimates of PAR. In the review by Torén and Blanc (2009), five papers were, and in those papers there was a slightly higher PAR for women compared with men. In our study there were 149 men and 308 women, who got new-onset asthma during the follow-up period. This should give an estimate of 1.2 asthma cases/1000 p-years among men and 2.2 asthma cases/1000 p-years among women. Application of these figures on the PAR would give 136 men and 293 women with new-onset of occupational asthma per million people per year.
In the present general population-based study with an N-JEM, based on the same principles as the SK-JEM, we could verify some well-known asthma risks and identify some new risks. Men exposed to epoxy compounds, diisocyanates and acrylates had an increased risk of new-onset asthma. Furthermore, men exposed to accidental high peaks of irritants had a high asthma risk. We confirmed earlier findings of increased asthma risks in men and women exposed to cleaning agents. Regarding exposure to LMW agents and irritants, non-atopic subjects seemed to be at highest risk of new-onset asthma. We have shown that it is important to stratify for sex and atopy even if the CIs might increase. The proportion of adult asthma attributable to workplace factors was 14% for men and 7% for women.
FUNDING
Icelandic Research Council, the Swedish Heart and Lung Foundation, the Vårdal Foundation for Health Care and Allergic Research, the Swedish Association Against Asthma and Allergy, the Swedish Council for Working Life and Social Research, the Bror Hjerpstedt Foundation, the Norwegian Research Council project (135773/330), the Norwegian Asthma and Allergy Association, the Danish Lung Association and the Estonian Science Foundation (4350).
Acknowledgments
Acknowledgements—There are no conflicts of interest for any of the authors.
REFERENCES
- Andersson E, Knutsson A, Hagberg S, et al. (2006). Incidence of asthma among workers exposed to sulphur dioxide and other irritant gases. Eur Respir J; 27: 720–5 [DOI] [PubMed] [Google Scholar]
- Balmes J, Becklake M, Blanc P, et al. ; Environmental and Occupational Health Assembly, American Thoracic Society (2003). American Thoracic Society Statement: Occupational contribution to the burden of airway disease. Am J Respir Crit Care Med; 167: 787–97 [DOI] [PubMed] [Google Scholar]
- Blanc PD, Torén K. (1999). How much adult asthma can be attributed to occupational factors? Am J Med; 107: 580–7 [DOI] [PubMed] [Google Scholar]
- Greenland S. (2008). Attributable fraction estimation. In Rothman KJ, Greenland S, Lash TL, editors. Modern Epidemiology; 3rd edn Philadelphia, PA: Wolters Kluwer and Lippincott Williams & Wilkins; p. 295–9 ISBN-13: 978-0-7817-5564-1 [Google Scholar]
- Henneberger PK, Olin AC, Andersson E, et al. (2005). The incidence of respiratory symptoms and diseases among pulp mill workers with peak exposures to ozone and other irritant gases. Chest; 128: 3028–37 [DOI] [PubMed] [Google Scholar]
- Holm M, Omenaas E, Gíslason T, et al. RHINE Study Group (2007). Remission of asthma: a prospective longitudinal study from northern Europe (RHINE study). Eur Respir J; 30: 62–5 [DOI] [PubMed] [Google Scholar]
- ILO (1991). International Standard Classification of Occupations ISCO 88; Geneva, Switzerland: ILO; ISBN 92-2-106438-7 [Google Scholar]
- Jaakkola JJ, Piipari R, Jaakkola MS. (2003). Occupation and asthma: a population-based incident case-control study. Am J Epidemiol; 158: 981–7 [DOI] [PubMed] [Google Scholar]
- Karjalainen A, Kurppa K, Martikainen R, et al. (2001). Work is related to a substantial portion of adult-onset asthma incidence in the Finnish population. Am J Respir Crit Care Med; 164: 565–8 [DOI] [PubMed] [Google Scholar]
- Kaukiainen A, Martikainen R, Riala R, et al. (2008). Work tasks, chemical exposure and respiratory health in construction painting. Am J Ind Med; 51: 1–8 [DOI] [PubMed] [Google Scholar]
- Kennedy SM, Le Moual N, Choudat D, et al. (2000). Development of an asthma specific job exposure matrix and its application in the epidemiological study of genetics and environment in asthma (EGEA). Occup Environ Med; 57: 635–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy SM, Le Moual N, Choudat D, et al. (2011). Asthma- specific Job Exposure Matrix, Estimating occupational risks for asthma in epidemiology Available at http://cesp.vjf.inserm.fr/asthmajem/ Accessed 13 December 2011
- Kogevinas M, Antó JM, Sunyer J, et al. (1999). Occupational asthma in Europe and other industrialised areas: a population-based study. European Community Respiratory Health Survey Study Group. Lancet; 353: 1750–4 [DOI] [PubMed] [Google Scholar]
- Kogevinas M, Zock JP, Jarvis D, et al. (2007). Exposure to substances in the workplace and new-onset asthma: an international prospective population-based study (ECRHS-II). Lancet; 370: 336–41 [DOI] [PubMed] [Google Scholar]
- LeVan TD, Koh WP, Lee HP, et al. (2006). Vapor, dust, and smoke exposure in relation to adult-onset asthma and chronic respiratory symptoms: the Singapore Chinese Health Study. Am J Epidemiol; 163: 1118–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malo JL, Chan-Yeung M. (2009). Agents causing occupational asthma. J Allergy Clin Immunol; 123: 545–50 [DOI] [PubMed] [Google Scholar]
- Mirabelli MC, Zock JP, Plana E, et al. (2007). Occupational risk factors for asthma among nurses and related healthcare professionals in an international study. Occup Environ Med; 64: 474–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olin AC, Andersson E, Andersson M, et al. (2004). Prevalence of asthma and exhaled nitric oxide are increased in bleachery workers exposed to ozone. Eur Respir J; 23: 87–92 [DOI] [PubMed] [Google Scholar]
- Omenaas E, Svanes C, Janson C, et al. (2008). What can we learn about asthma and allergy from the follow-up of the RHINE and the ECRHS studies? Clin Respir J; 2 Suppl 1: 45–52 [DOI] [PubMed] [Google Scholar]
- Pattaro C, Locatelli F, Sunyer J, et al. (2007). Using the age at onset may increase the reliability of longitudinal asthma assessment. J Clin Epidemiol; 60: 704–11 [DOI] [PubMed] [Google Scholar]
- Rönmark EP, Ekerljung L, Lötvall J, et al. (2009). Large scale questionnaire survey on respiratory health in Sweden: effects of late- and non-response. Respir Med; 103: 1807–15 [DOI] [PubMed] [Google Scholar]
- Suarthana E, Heederik D, Ghezzo H, et al. (2009). Risks for the development of outcomes related to occupational allergies: an application of the asthma-specific job exposure matrix compared with self-reports and investigator scores on job-training-related exposure. Occup Environ Med; 66: 256–63 [DOI] [PubMed] [Google Scholar]
- Torén K, Blanc PD. (2009). Asthma caused by occupational exposures is common - a systematic analysis of estimates of the population-attributable fraction. BMC Pulm Med; 9: 7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torén K, Brisman J, Järvholm B. (1993). Asthma and asthma-like symptoms in adults assessed by questionnaires. A literature review. Chest; 104: 600–8 [DOI] [PubMed] [Google Scholar]
- Torén K, Ekerljung L, Kim JL, et al. (2011). Adult-onset asthma in west Sweden–incidence, sex differences and impact of occupational exposures. Respir Med; 105: 1622–8 [DOI] [PubMed] [Google Scholar]
- Torén K, Gislason T, Omenaas E, et al. ; RHINE Group (2004). A prospective study of asthma incidence and its predictors: the RHINE study. Eur Respir J; 24: 942–6 [DOI] [PubMed] [Google Scholar]
- Torén K, Palmqvist M, Löwhagen O, et al. (2006). Self-reported asthma was biased in relation to disease severity while reported year of asthma onset was accurate. . J Clin Epidemiol; 59: 90–3 [DOI] [PubMed] [Google Scholar]
- Vandenplas O. (2011). Occupational asthma: etiologies and risk factors. Allergy Asthma Immunol Res; 3: 157–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang TN, Lin MC, Wu CC, et al. (2010). Risks of exposure to occupational asthmogens in atopic and nonatopic asthma: a case-control study in Taiwan. Am J Respir Crit Care Med; 182: 1369–76 [DOI] [PubMed] [Google Scholar]
- Zock JP, Cavallé N, Kromhout H, et al. (2004). Evaluation of specific occupational asthma risks in a community-based study with special reference to single and multiple exposures. J Expo Anal Environ Epidemiol; 14: 397–403 [DOI] [PubMed] [Google Scholar]