Abstract
Intimate partner violence (IPV) undermines women's ability to enact safer sex and increases their vulnerability to HIV and other STDs. To better understand the relationship between IPV and sexual risk behavior, we investigated whether the Information – Motivation –Behavioral Skills (IMB) model differentially predicted risk behavior among women who had and had not recently experienced IPV. Data from 717 women who were recruited from a public health clinic showed that 18% reported IPV by a sexual partner in the past 3 months, 28% in the past year, and 57% lifetime. Women who experienced IPV in the last 3 months reported more episodes of unprotected sex and more episodes of unprotected sex with a steady partner in the past 3 months. Multi-group path analyses provided mixed evidence regarding the associations hypothesized by the IMB model; the strength of these associations varied as a function of IPV history. Thus, although information did not predict risk behavior for either group, motivation was associated with condom use only for women with no history of IPV. Behavioral skills were associated with more condom use for both groups. Overall, the IMB model is useful for predicting sexual risk behavior; however, for women with partner violence histories a broader model that includes other contextual factors may be needed. These findings can help to inform the development of more effective sexual risk reduction interventions.
Keywords: Intimate partner violence, women, sexual risk behavior, IMB model, heterosexual transmission, public health
Introduction
HIV and sexually transmitted diseases (STDs) are significant public health problems for women. In 2005, women accounted for 26% of the incident HIV/AIDS cases in the U.S. with 80% of these infections resulting from heterosexual contact (1). Chlamydia and Gonorrhea are the most prevalent STDs among women in the U.S. (2). In the period 2004-2008, the Chlamydia infection rate in women increased 21% (2). STDs have serious health consequences for women. They can cause infertility, ectopic pain, and chronic pelvic pain; pregnant women infected with Chlamydia can pass the infection to their babies during delivery (2).Individuals with STD infections are two to five times more susceptible to HIV infection, and, individuals co-infected with an STD and HIV are more likely to transmit HIV through sexual contact (1).
To reduce rates of STDs and HIV among women, it is important to understand the antecedents of risk behavior. Theories of health behavior have proven useful in this regard. For example, the Information–Motivation–Behavioral Skills (IMB) model (3, 4) posits that sexual risk behavior is predicted by an individual's STD- and HIV-related information, motivation to engage in safer sexual behaviors, and behavioral skills to successfully engage in safer sex (e.g., condom use skills and sexual assertiveness skills) (5). Research indicates that the IMB constructs predict sexual risk behavior in several groups such as substance abusing adults (6), individuals with a mental illness (7), and STD clinic patients (8). Systematic reviews and meta analyses also support the underlying assumptions of the IMB model (9, 10) and sexual risk reduction interventions targeting the constructs in the IMB model reduce sexual risk behavior (11-13).
Although information, motivation, and behavioral skills predict sexual behavior, many studies utilizing the IMB framework find that much of the variance in sexual risk behavior remains unexplained after accounting for the IMB constructs (7, 14), indicating that important constructs may be missing from the model. One limitation of the IMB and other models of risk behavior is the focus on individual-level variables (15-19). Because sexual behavior occurs in a dyad, relationship factors are also likely to influence sexual risk behavior. These relationship factors may be particularly important for women, whose social position and power imbalances in their intimate relationships may influence their ability to engage in safer sexual behaviors (20).
One such relationship factor that is likely to play an important role in women's ability to engage in safer sexual behavior is the threat of intimate partner violence (IPV). In a qualitative study conducted by Epperson, Platais, Valera, Barbieri, Gilbert, El-Bassel (21), women's fear of physical and emotional violence was a central determinant of risky sex. Quantitative studies also indicate that IPV is related to sexual risk behavior and STD/HIV infection (22, 23). The IMB model may not be as useful in predicting sexual risk behavior among women who fear violence from their partner if they try to negotiate for safer sexual behavior. Even if women have the necessary information, are motivated to engage in safer sexual behavior, and have safer sex skills, the threat of or actual partner violence may limit their ability to engage in safer sex. To our knowledge, no previous research has investigated whether IPV moderates the relations among information, motivation, skills, and condom use.
Women with IPV histories attending STD clinics represent a vulnerable group for HIV infection. First, women attending STD clinics are at increased risk for STD and HIV infection (24). Second, women receiving services from STD clinics report high levels of IPV. In an STD clinic sample, 38% women reported lifetime physical assault by an intimate partner and 33% reported verbal threats of violence. Nearly 16% of the women reported at least one episode of physical abuse in the past year (25).
Thus, the purpose of this study was to investigate whether information, motivation, and behavioral skills differentially predict condom use among women from a STD clinic who had and had not recently experienced IPV, using a multi-group path analysis approach. We hypothesized that information, motivation, and behavioral skills would be less strongly associated with condom use for women who were currently experiencing IPV, compared to women who had not experienced recent IPV.
Methods
Participants
This study used baseline data from a randomized controlled trial (RCT) designed to evaluate several sexual risk reduction interventions and conducted at a public STD clinic. Inclusion criteria for the trial were: age 18 or older; willing to participate in a standard clinic visit, including an HIV test; currently HIV negative; and engaged in sexual risk behavior in the past 3 months (i.e., vaginal or anal intercourse without a condom with: (a) more than one sexual partner; or (b) a partner who injected drugs, who had other partners, who was diagnosed with an STD in the last 3 months, or who was HIV positive).
Baseline data were available from 717 women who participated in the RCT. Sixty-five percent of the women were African American (n = 464) and 23% were Caucasian (n = 164); 56% were unemployed (n = 405), 64% had a high school education or less (n = 458), and 66% had an income < $15,000 per year (n = 474). The participants were, on average, 28.2 years old (SD = 9.1); and 79% were in a steady relationship (n = 565).
Procedures
Patients were called from the waiting room by their registration number and taken to a private room by a trained Research Assistant (RA). The RA shared the purpose of the study and sought their permission to ask a few screening questions to determine their eligibility. The study was explained to all eligible patients and those who agreed to participate provided written consent and contact information. Participants were also asked to complete a calendar of important events over the last 3 months to help them to respond more accurately.
All participants completed an audio computer-assisted self-interview (ACASI) in private. ACASIs allow patients to participate regardless of literacy skills and improve data quality for sensitive topics (26). Participants received $20 for completing the ACASI, which took approximately 45 minutes to complete. All procedures were approved by the IRBs of the participating institutions.
Measures
The ACASI assessed demographic characteristics, sexual health behaviors, psychosocial well-being, intimate partner violence and the hypothesized psychological antecedents of sexual risk behavior (i.e., information, motivation, and behavioral skills).
Demographic characteristics
Participants reported their race, income (re-coded as < $15,000 vs. ≥ $15,000), education (recoded as high school or less vs. more than high school), and employment (re-coded as employed vs. unemployed). Participants were also asked their age and whether they ever traded sex for money or drugs.
Intimate partner violence
Three items assessed recent intimate partner violence (27, 28). Participants were asked (a) if they had ever been hit, kicked, punched, or otherwise hurt by a sexual partner; (b) if they had ever been pressured or forced to have sexual contact; and (c) if their partner had ever threatened to hurt or kill them, prevented them from leaving or entering their home, seeing friends, making phone calls, having or keeping a job, continuing their education, or seeking medical attention. If a participant responded affirmatively to any of the three questions, she was asked when this had happened most recently (past three months, past year, or more than one year ago).
Information
The 18-item Brief HIV Knowledge Questionnaire (HIV-KQ; 29, 30) assessed participants' knowledge of HIV-related information. The number of correct responses was divided by the total number of responses to obtain the percentage of knowledge items correct; thus, greater scores indicate greater HIV knowledge. Previous studies have established the reliability and validity of the Brief HIV-KQ (30).
Motivation
Participants completed five items adapted from existing condom attitudes scales (31, 32). Participants rated each item on a scale from “strongly disagree” = 1 to “strongly agree” = 6. Items were averaged to derive a Condom Attitudes score; a higher score indicated more favorable attitudes towards condom use (α = .70).
Behavioral Skills
Participants completed a subset of seven items from the Condom Influence Strategy Questionnaire (CISQ; 33), a measure of skill in negotiating condom use. Participants indicated how often in the past 3 months they used different condom influence strategies with their sexual partner(s) on a 5-point Likert scale, ranging from “never” = 1 to “almost always” = 5. Items were averaged to form a total CISQ score. A higher score indicated more frequent use of condom influence strategies (α = .89).
Sexual Risk Behavior
Items developed and tested in previous studies (12, 13, 34) were used to assess sexual risk behavior. Participants were asked to report the number of men and number of women with whom they had sex in the past 3 months, and whether they considered any of these partners to be a steady partner. To investigate the frequency of sex, participants were asked to report the number of times they had vaginal and anal sex with and without a condom in the past 3 months with their steady partner and with their other (non-steady) partners. Responses to these items were summed to determine the total number of episodes of unprotected vaginal and/or anal sex in the past 3 months, as well as the number of episodes of unprotected sex with a steady partner (26, 35). Responses to these items were also used to calculate the proportion of unprotected sex episodes in the past 3 months (# unprotected sex episodes ÷ total # of sex episodes) with a steady partner and with all partner(s).
Data Analysis
Data were inspected for outliers [> 3 × the interquartile range (IQR) from the 75th percentile] and trimmed (to 3 × IQR from the 75th percentile + 1). Data that were non-normally distributed were transformed using a log10 transformation.
Chi-square and ANOVA analyses were conducted to determine which demographic and background variables were associated with IPV and with the sexual behavior outcomes; these variables were included as covariates in subsequent analyses. ANCOVAs were conducted to determine whether women who had and had not experienced recent IPV differed on information, motivation, skills, and condom use variables. To determine whether the associations between the IMB variables and sexual risk behavior differed as a function of recent IPV, multi-group path analyses were conducted using Mplus (36). Separate models were conducted for each of the four sexual risk behavior outcomes (i.e., total number of unprotected sex episodes; number of unprotected sex episodes with a steady partner; percentage of total sex episodes that were unprotected; percentage of episodes of sex with a steady partner that were unprotected). The models included direct paths from information, motivation, and skills variables to sexual risk behavior, as well as indirect paths from information and motivation to sexual risk behavior through skills, consistent with the IMB model (3, 5). The models also included paths from the covariates to the outcome and to the mediator (i.e., skills), correlations between the covariates, and a correlation between information and motivation.
We first allowed all path coefficients to vary across the two groups (i.e., IPV and no IPV) and determined which IMB variables were associated with condom use for each of the groups. We then constrained the path coefficients to be equal across the two groups, and determined whether this constraint resulted in an implied worsening of model fit by examining the change in χ2 and degrees of freedom. A significant worsening of model fit with the paths constrained to be equal indicated that the path coefficients differed between the IPV and no IPV groups.
Results
One hundred and twenty nine (18%) of the women reported experiencing partner violence in the last three months, 28% in the past year, and 57% in their lifetime. Participants reported an average of 16.3 episodes of unprotected sex in the past 3 months (SD = 20.2). An average of 68% of episodes of sex in the past 3 months were unprotected (SD = 33%). Participants reported an average of 2.6 sexual partners in the past 3 months (SD = 2.3); 61% of participants (n = 439) reported having more than one sexual partner in the past 3 months.
Bivariate Analyses
Relative to participants who did not report recent IPV, participants who reported IPV in the past 3 months were more likely to be unemployed, χ2 = 14.08, p < .001 and to have traded sex for money or drugs, χ2 = 16.12, p < .0001. Therefore, employment status and trading sex were included as covariates in all models.
Participants with a high school or less education reported more episodes of unprotected sex in the past 3 months than participants who had attended some college, t(712) = -2.43, p < .05. Education was included as a covariate in the analyses with the number of episodes of unprotected sex (total) as the outcome. Older age was associated with a greater percentage of episodes of unprotected sex total, t(712) = 17.40, p < .0001, and with a steady partner, t(560) = 11.35, p < .001. Older age was included as a covariate in the analyses with the percentage of episodes of unprotected sex (total and with a steady partner) as the outcomes.
Multivariate Analyses
After controlling for relevant covariates, women who experienced IPV reported more episodes of unprotected sex in the past 3 months, F(1, 695) = 13.64, p < .001, and more episodes of unprotected sex with a steady partner, F(1, 546) = 10.80, p < .01 (see Table 1), compared to women who had not experienced recent IPV. Women who had and had not experienced recent IPV did not differ in scores on information, motivation, or skills measures, or in the percentage of episodes of unprotected sex (total and with a steady partner) after controlling for relevant covariates (ps > .05).
Table 1.
IMB constructs and sexual risk behavior by recent intimate partner violence (IPV)
| No recent IPV (n = 588) |
Recent IPV (n = 129) |
|||
|---|---|---|---|---|
| M | SD | M | SD | |
| IMB Constructs | ||||
| Information (HIV Knowledge Questionnaire) | 76% | 19% | 72% | 21% |
| Motivation (attitude towards condoms) | 4.66 | 0.92 | 4.43 | 0.92 |
| Behavioral skills (Condom Influence Strategy Questionnaire) | 2.43 | 1.14 | 2.38 | 1.11 |
| Sexual Risk Behavior | ||||
| Unprotected sex (number of episodes, past 3 months) ** | 14.8 | 18.9 | 22.9 | 24.2 |
| Unprotected sex (percentage of episodes, past 3 months) | 67% | 33% | 73% | 32% |
| Unprotected sex with steady partner (number of episodes, past 3 months) * | 16.0 | 19.3 | 23.8 | 23.6 |
| Unprotected sex with steady partner (percentage of episodes, past 3 months) | 73% | 35% | 78% | 33% |
Note: Analyses controlled for relevant demographic covariates.
p < .01
p < .001
Moderated Mediational Analyses
Number of Episodes of Unprotected Sex (all partners)
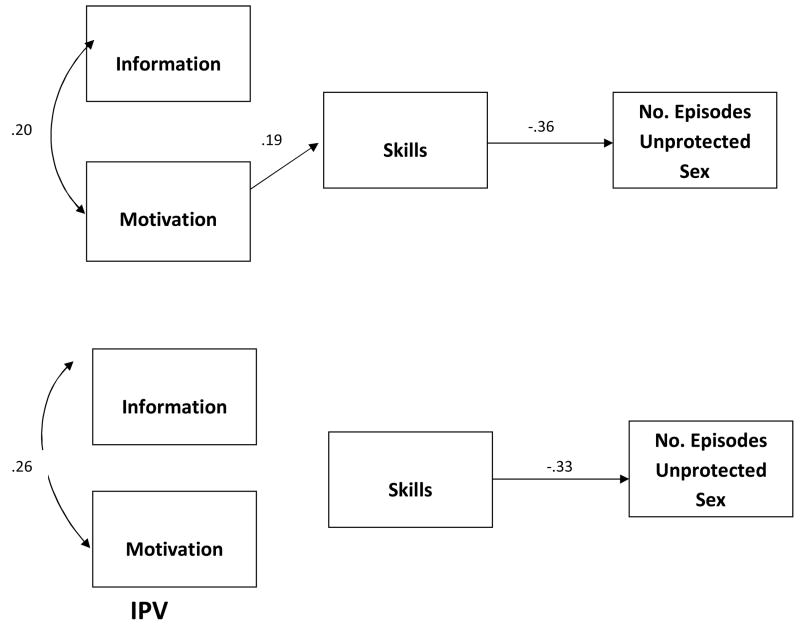
To control for covariates in the moderated mediation models, paths were included from the relevant covariates to: (a) the mediator (i.e., skills) and (b) the outcome variable. In analyses predicting the total number of episodes of unprotected sex in the past 3 months, information was unrelated to the number of episodes of unprotected sex for both groups. There was a significant indirect effect from motivation to the number of episodes of unprotected sex through skills (estimate = -0.07, SE = 0.02, p < .01) for women who had not experienced recent IPV. Greater motivation was associated with greater skills that were, in turn, associated with fewer episodes of unprotected sex. For the women who experienced recent IPV, there was no indirect effect of motivation on sexual risk behavior. When the path from motivation to skills was constrained to be equal across the two groups, there was a marginally significant worsening of model fit, χ2Δ = 3.57, dfΔ = 1, p < .06, indicating that the strength of the path coefficient differed marginally between the two groups. Skills was negatively related to the number of episodes of unprotected sex for both women who had and had not experienced recent IPV (see Figure 1); for both groups, greater skills were associated with fewer episodes of unprotected sex.
Figure 1.
Episodes of Unprotected Sex, Past 3 Months
Note: only significant paths shown; no. = number; IPV = intimate partner violence
Number of Episodes of Unprotected Sex (steady partners only)
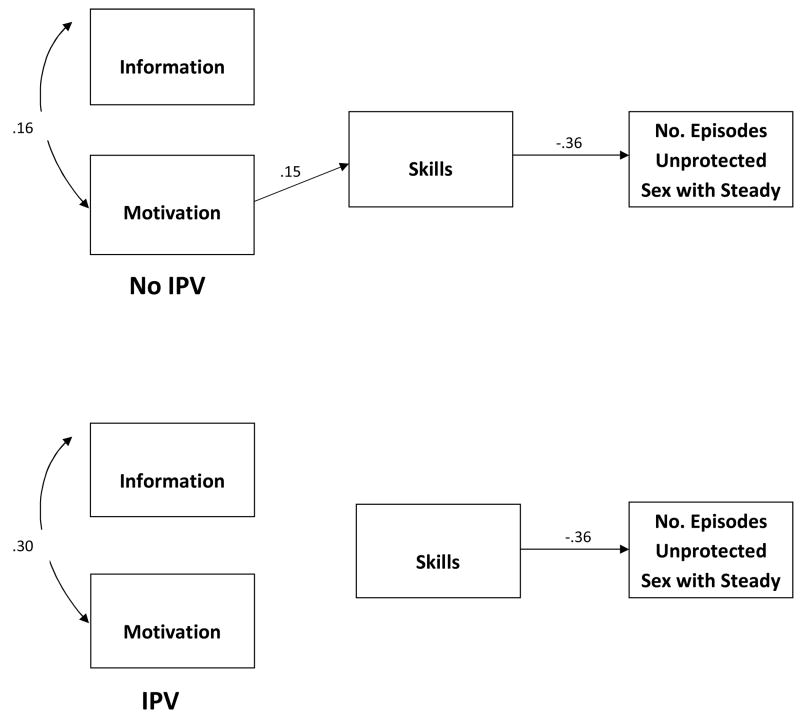
Additional analyses were conducted with the 565 women who reported a steady partner in the past 3 months; the outcome was the number of episodes of unprotected sex in the past 3 months with a steady partner (see Figure 2). Findings were similar to analyses with the full sample of women, with information unrelated to episodes of unprotected sex for either group, an indirect effect of motivation on episodes of unprotected sex (through skills) only for women who had not experienced recent IPV (estimate = -0.05, SE = 0.02, p < .01), and skills negatively associated with the number of episodes of unprotected sex for both groups. None of the path coefficients significantly differed between the two groups.
Figure 2.
Episodes of Unprotected Sex with a Steady Partner, Past 3 Months
Note: only significant paths shown; no. = number; IPV = intimate partner violence
Percentage of episodes of unprotected sex (all partners)
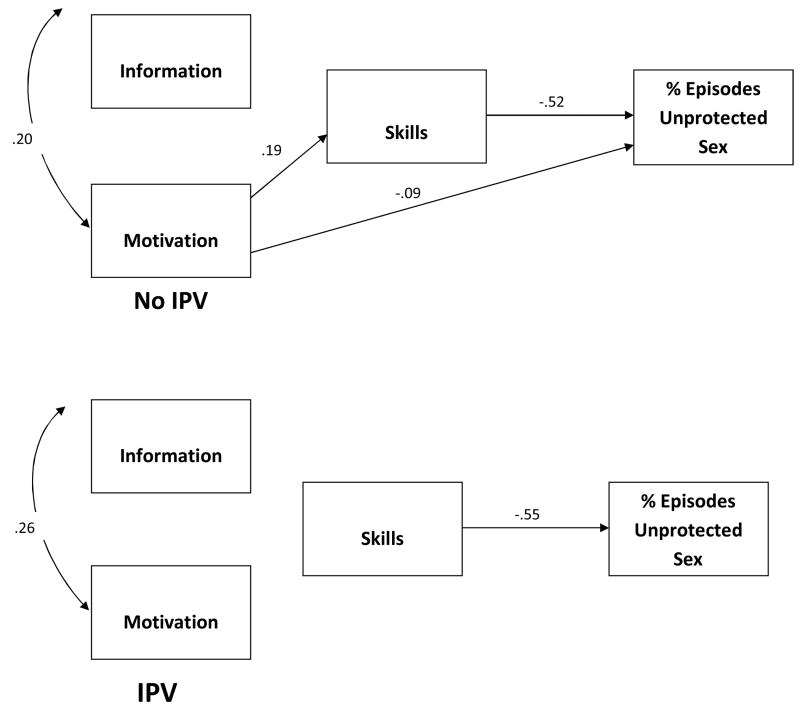
Information was unrelated to the percentage of episodes of unprotected sex for either group. For women who did not experience recent IPV, there was an indirect effect from motivation to percentage of episodes of unprotected sex through skills (estimate = -.10, SE = .02, p < .001). Greater motivation was associated with greater skills that were, in turn, associated with a smaller percentage of episodes of unprotected sex. There was also a direct effect of motivation on the percentage of episodes of unprotected sex only for women who did not experience recent IPV; women who were more motivated reported a smaller percentage of episodes of unprotected sex. Constraining the path coefficient from motivation to skills to be equal across the two groups resulted in a marginally significant worsening of model fit, χ2Δ = 3.71, dfΔ = 1, p < .06, indicating that the strength of this path coefficient differed marginally between women who had and had not experienced recent IPV. Constraining the path coefficient from motivation to the percentage of episodes of unprotected sex to be equal across groups did not result in a worse model fit. For both women who did and did not experience recent IPV, skills were negatively related to the percentage of episodes of unprotected sex total in the past 3 months, indicating that women with greater condom skills had a smaller percentage of episodes of unprotected sex (see Figure 3).
Figure 3.
Percentage of Episodes of Unprotected Sex, Past 3 Months
Note: only significant paths shown; IPV = intimate partner violence
Percentage of episodes of unprotected sex (steady partners only)
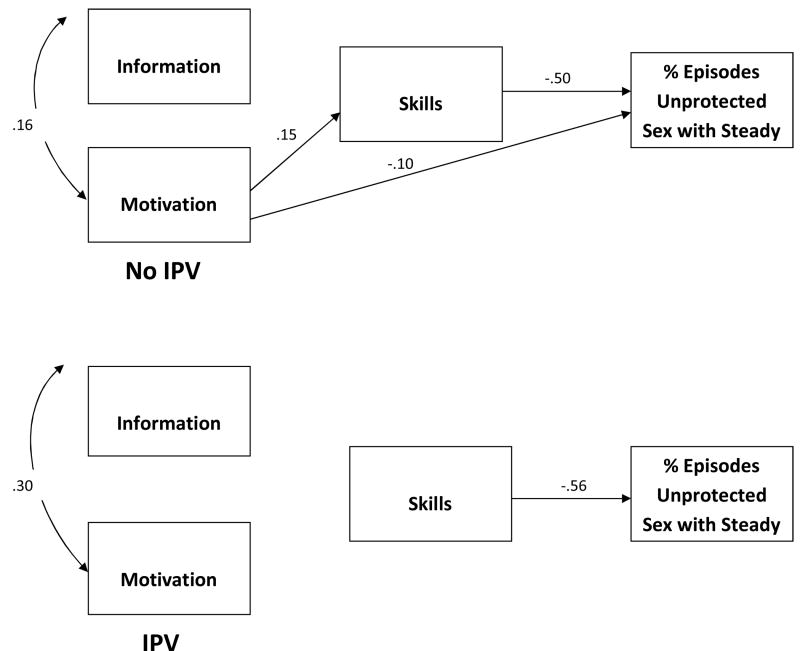
Additional analyses were conducted with the subset of women (n = 565) who reported having a steady partner in the past 3 months, with the percentage of episodes of unprotected sex with a steady partner as the outcome (see Figure 4). In these analyses, information was unrelated to the percentage of episodes of unprotected sex. Motivation was directly and negatively associated with the percentage of episodes of unprotected sex for women who had not experienced recent IPV; in addition, for these women, motivation was indirectly associated with the percentage of episodes of unprotected sex through skills (estimate = -.07, SE = .02, p < .01). Constraining the path from motivation to the percentage of episodes of unprotected sex resulted in a marginally significant worsening of model fit, χ2Δ = 2.89, dfΔ = 1, p < .09, indicating that this path differed marginally between the two groups of women. Constraining the path from motivation to skills to be equal across groups did not result in a worse model fit. Skills were negatively related to the percentage of episodes of unprotected sex for both women who had and had not experienced recent IPV.
Figure 4.
Percentage of Episodes of Unprotected Sex with a Steady Partner, Past 3 Months
Note: only significant paths shown; IPV = intimate partner violence
Discussion
The IMB model has been used to successfully predict sexual risk behavior with a variety of populations (6, 8, 37, 38). However, to our knowledge this is the first study to compare the utility of the determinants of condom use as specified by the IMB model among women who have and have not experienced recent IPV. Women in this study reported high rates of physical IPV: 18% reported IPV in the past 3 months, 28% in the past year, and 57% in their lifetime. These rates are similar in magnitude to those reported previously among women attending STD clinics (39) and are higher than those reported by national samples of women (40). This study further highlights the need for HIV risk reduction interventions targeting abused women at STD clinics.
Results from the multi-group path analyses reported herein provide partial support for the associations hypothesized by the IMB model among women with and without histories of recent IPV. Contrary to the IMB model, however, information did not predict the number and percentage of episodes of unprotected sex for either of the two groups. This finding is consistent with other studies that have found little to no relationship between the construct of information and sexual risk behavior (5, 41). Others have suggested that information may only be important in populations with low levels of HIV-related information (5).
As predicted by the IMB model, and consistent with previous research findings (42, 43), our study found a direct association between greater behavioral skills and more condom use for both the groups. Results suggest that women attending STD clinics who have the skills necessary to engage in HIV-preventive behavior use condoms more frequently regardless of whether or not they experienced recent IPV. It is important to note that we did not assess IPV severity in this study. Even women who have good condom negotiation skills may not be able to successfully use those skills if they are experiencing severe IPV. An important area of future research will be to determine whether IPV severity affects the relation between behavioral skills and condom use.
An important finding of this research was the differential impact of motivation on condom use among women with and without histories of recent partner violence. Consistent with our hypotheses, condom-related motivation was associated directly and indirectly with condom use among women with no experience of partner violence, but not for women with histories of recent partner violence. Although multi-group analyses comparing the strength of the paths associated with motivation between the IPV and no IPV groups did not reach traditional levels of statistical significance, the finding that paths associated with motivation were significant for women not experiencing IPV but were not significant for women who had experienced recent IPV are worthy of further study. The importance of motivation for women without a history of IPV supports previous research (11). However, contrary to previous research, motivation did not predict condom use among women who had experienced recent partner violence. This suggests that partner violence is a unique barrier to behavior change that may reduce the importance of condom-related motivation in promoting safer sex.
Though the IMB model has been useful in understanding sexual risk behavior and in developing sexual risk reduction interventions, this model focuses on individual-level determinants of sexual behavior, with less consideration of relationship factors that may influence sexual behavior. An implicit assumption of this model is that individuals control their own sexual behavior; for women in violent relationships, this assumption is likely to be inaccurate (44). A more powerful explanatory model might include a combination of cognitive, behavioral, relational, social, and contextual factors specifically related to women and their risk for HIV infection (15, 18, 19). For example, IPV-related post-traumatic stress disorder (PTSD) might impact women's sexual risk behavior. A recent study demonstrated that women with IPV-related PTSD were four times more likely to engage in recent sexual risk behavior than women without IPV-related PTSD (45). Further, in violent relationships, partner dynamics such as relationship power might play an important role in determining women's sexual risk. Studies have shown that higher relational power is associated with greater influence on issues related to sex and safer sexual practices (46). Another potentially important relational variable is a partner's motivation to use condoms (47). For women in violent relationships, a partner's motivation for condom use may be a stronger predictor of condom use than the women's motivation. Research should investigate whether these and other relational variables predict condom use among women, especially women in violent relationships.
Several study limitations should be noted. First, we did not assess whether all of the sexual behavior reported by participants occurred in the context of a violent relationship. Some women (61%) reported more than one sexual partner in the past 3 months. To address this limitation, researchers might collect event-level data (48) to determine whether violence at a sexual event is associated with sexual risk behavior at that event. Second, the sample was restricted to women who attended an urban STD clinic, most of whom were low-income, African American women; findings may not generalize to other women. Third, each IMB construct was assessed with only one measure, providing imperfect assessments of these constructs. Future research might obtain more detailed assessments. Fourth, the analyses may have been underpowered to detect effects in the multi-group comparisons. For example, despite large difference between the no IPV and IPV groups in the size of the path coefficients from motivation to skills (ranging from .15 to .19 for the no IPV group and from -.003 to .05 for the IPV group), these differences only approached significance in the multi-group comparisons.
Our study findings have important implications for developing HIV risk-reduction interventions for women with recent histories of IPV. Information and motivation were largely unrelated to sexual risk behavior for women who experienced recent IPV; therefore, traditional IMB-based interventions may not be optimal for these women. Women may be motivated to prevent HIV and STDs, but may not have the relational power to practice safer sex. Sexual risk reduction interventions that address dynamics of healthy relationships, mental and emotional health as a consequence of IPV, instill gender pride, and discuss gender-based power as well as intimate partner violence should be developed and evaluated. Recently, a group of researchers successfully conducted a feasibility study on an intervention aimed at reducing HIV risk behaviors among women seeking services for IPV from a community-based organization in South Africa (49). Women in both the intervention groups reported fewer HIV misperceptions and trauma symptoms as well as greater HIV knowledge, risk reduction intentions, and self-efficacy. More intervention trials are needed in this area. Although couple-focused interventions would be worthwhile, recruitment of couples and men provide significant challenges to health providers. Researchers will also have to be mindful of the nature and type of abuse and ensure the safety of women while developing, implementing, and evaluating such interventions.
Clearly, the key target for risk reduction interventions is behavioral skills. Whereas typical sexual risk reduction interventions may focus on teaching assertiveness skills, interventions with women who are in violent relationships may need skills specific to requesting safer sex while maintaining personal safety. A study by Neighbors and O'Leary (50) found that message framing affected how men responded to condom requests; in addition, men who perpetrated IPV were more likely to refuse condom use and react with violence if they identified the request as threatening to self or the relationship. Thus, an important skill might be to teach women with violent partners safer ways of asking their partner to practice safer sex and to use messages that do not inadvertently irritate the partner and increase their risk for IPV. Although this recommendation maybe interpreted as victim blaming, given the number of women who remain in abusive relationships(51), it is important to acknowledge the sociocultural disadvantage that many women continue to experience. Although it is essential to work to reduce this disadvantage through structural, social, and interpersonal empowerment, there is the immediate need to address the acute vulnerability that women often find difficult to avoid. Furthermore, it is essential that research be continued and programs be developed to help men reduce IPV against women. Qualitative research is also needed with women who experience IPV to understand the skills and techniques they have used to reduce their sexual risk. By furthering our understanding about gender, power, and relational dynamics that impact intimate relationships, researchers can develop effective sexual risk reductions for women who experience IPV.
Acknowledgments
This research was supported by NIH grant # R01-MH068171 to Michael P. Carey. We thank all those who participated in the research, and the Health Improvement Project team members.
Contributor Information
Mona Mittal, Department of Community and Preventive Medicine, University of Rochester, Rochester, NY, USA.
Theresa E. Senn, Center for Health and Behavior, Syracuse University, Syracuse, NY
Michael P. Carey, Center for Health and Behavior, Syracuse University, Syracuse, NY
References
- 1.Centers for Disease Control and Prevention. HIV/AIDS surveillance report 2009. Atlanta: US Department of Health and Human Services Centers for Disease Control and Prevention; 2007. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance report 2009. Atlanta: US Department of Health and Human Services; 2010. [Google Scholar]
- 3.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111:455–74. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 4.Fisher WA, Fisher JD. A general social psychological model for changing AIDS risk behavior. In: Pryor L, Reeder G, editors. The social psychology of HIV infection. Hillsdale: Erlbaum; 1993. pp. 127–53. [Google Scholar]
- 5.Fisher JD, Fisher WA, Shuper PA. The Information-Motivation-Behavioral Skills Model of HIV Preventive Behavior. In: DiClemente RJ, Crosby RA, Kegler MC, editors. Emerging Theories in Health Promotion Practice and Research. San Francisco: Jossey-Bass; 2009. pp. 22–55. [Google Scholar]
- 6.Bryan AD, Fisher JD, Fisher WA, Murray DM. Understanding condom use among heroin addicts in methadone maintenance using the information, motivation, behavioral skills model. Subst Use Misuse. 2000;35:451–71. doi: 10.3109/10826080009147468. [DOI] [PubMed] [Google Scholar]
- 7.Kalichman SC, Malow R, Devieux J, Stein JA, Piedman F. HIV risk reduction for substance using seriously mentally ill adults: Test of the information-motivation-behavioral skills (IMB) model. Community Ment Health J. 2005;41:277–90. doi: 10.1007/s10597-005-5002-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalichman SC, Simbayi LC, Cain D, Jooste S, Skinner D, Cherry C. Generalizing a model of health behavior change and AIDS stigma for use with sexually transmitted infection clinic patients in Cape Town, South Africa. AIDS Care. 2006;18:178–82. doi: 10.1080/09540120500456292. [DOI] [PubMed] [Google Scholar]
- 9.Herbst JH, Kay LS, Passin WF, Lyles CM, Crepaz N, Marin BV. A systematic review and meta-analysis of behavioral interventions to reduce HIV risk behaviors of Hispanics in the United States and Puerto Rico. AIDS Behav. 2007;11:25–47. doi: 10.1007/s10461-006-9151-1. [DOI] [PubMed] [Google Scholar]
- 10.Noar SM. Behavioral interventions to reduce HIV-related sexual risk behavior: Review and synthesis of meta-analytic evidence. AIDS Behav. 2008;12(3):335–53. doi: 10.1007/s10461-007-9313-9. [DOI] [PubMed] [Google Scholar]
- 11.Anderson ES, Wagstaff DA, Heckman TG, Winett RA, Roffman RA, Solomon LJ. Information-motivation-behavioral skills (IMB) model: Testing direct and mediated treatment effects on condom use among women in low-income housing. Ann Behav Med. 2006;31:70–9. doi: 10.1207/s15324796abm3101_11. [DOI] [PubMed] [Google Scholar]
- 12.Carey MP, Maisto SA, Kalichman SC, Forsyth AD, Wright EM, Johnson BT. Enhancing motivation to reduce the risk of HIV infection for economicaly disadvantaged urban women. J Consult Clin Psychol. 1997;4:531–41. doi: 10.1037//0022-006x.65.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carey MP, Braaten LS, Maisto SA, Gleason JR, Forsyth AD, Durant LE. Using information, motivational enhancement, and skills training to reduce the risk of HIV infection for low-income urban women: A second randomized clinical trial. Health Psychol. 2000;19:3–11. doi: 10.1037//0278-6133.19.1.3. [DOI] [PubMed] [Google Scholar]
- 14.Scott-Sheldon LAJ, Carey MP, Vanable PA, Senn TE, Coury-Doniger P, Urban MA. Predicting Condom Use among STD Clinic Patients Using the Information-Motivation-Behavioral Kills (IMB) Model. J Health Psychol. 2010;20(10):1–10. doi: 10.1177/1359105310364174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amaro H, Raj A. On the margin: Power and women's HIV risk reduction strategies. Sex Roles. 2000;42:723–49. [Google Scholar]
- 16.Harman JJ, Amico KR. The relationship-oriented Information-Motivation-Behavioral Skills model: A multilevel structural equation model among dyads. AIDS Behav. 2008;13:173–84. doi: 10.1007/s10461-007-9350-4. [DOI] [PubMed] [Google Scholar]
- 17.Johnson BT, Redding CA, DiClemente RJ, Mustanski BS, Dodge BM, Sheeran P, et al. A Network-Individual-Resource Model for HIV Prevention. AIDS Behav. 2010 doi: 10.1007/s10461-010-9803-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O' Leary A. Women at risk for HIV from a primary partner: Balancing risk and intimacy. Annu Rev Sex Res. 2000;11:191–234. [PubMed] [Google Scholar]
- 19.Wingood GM, DiClemente RJ. Understanding the role of gender relations in HIV prevention research for women. American Journal of Public Health. 1995;85(4):592. doi: 10.2105/ajph.85.4.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Edu Behav. 2000;27:539–65. doi: 10.1177/109019810002700502. [DOI] [PubMed] [Google Scholar]
- 21.Epperson MW, Platais I, Valera P, Barbieri R, Gilbert L, El-Bassel N. Fear, Trust, and Negotiating Safety: HIV Risks for Black Female Defendants. J Women Social Work. 2009;24(3):257–71. doi: 10.1177/0886109909337377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garcia-Moreno C, Watts C. Violence against women: its importance for HIV/AIDS. AIDS. 2000;14:253–65. [PubMed] [Google Scholar]
- 23.Wingood GM, DiClemente RJ. Rape among African American women: Sexual, psychological, and social correlates predisposing survivors to risk of STD/HIV. J Womens Health. 1998;7(1):77–84. doi: 10.1089/jwh.1998.7.77. [DOI] [PubMed] [Google Scholar]
- 24.Weinstock H, Dale M, Linley L, Gwinn M. Unrecognized HIV infection among patients attending sexually transmitted disease clinics. Am J Pub Health. 2002;92(2):280–3. doi: 10.2105/ajph.92.2.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Augenbraun M, Wilson TE, Allister L. Domestic violence reported by women attending a sexually transmitted disease clinic. Sex Transm Dis. 2001;28:143–7. doi: 10.1097/00007435-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Schroder KEE, Carey MP, Vanable PA. Methodological issues in the assessment and analysis of sexual risk behavior: I. Item, content, scaling, and analytical options. Ann Behav Med. 2003;26(2):76–103. doi: 10.1207/s15324796abm2602_02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DiIorio C, Hartwell T, Hansen N. Childhood sexual abuse and risk behaviors among men at high risk for HIV infection. Am J Pub Health. 2002;92:214–9. doi: 10.2105/ajph.92.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feldhaus KM, Koziol-McLain J, Amsburg HL, Norton IM, Lowenstein SR, Abbott JT. Accuracy of 3 brief screening questions for detecting partner violence in the emergency department. J Am Med Assoc. 1997;277(17):1351–61. [PubMed] [Google Scholar]
- 29.Carey MP, Morrison-Beedy D, Johnson BT. The HIV-Knowledge Questionnaire: Development and evaluation of a reliable, valid, and practical self-administered questionnaire. AIDS Behav. 1997;1:61–74. [Google Scholar]
- 30.Carey MP, Schroder KEE. Development and psychometric evaluation of the brief HIV knowledge questionnaire (HIV-KQ-18) AIDS Educ Prev. 2002;14:174–84. doi: 10.1521/aeap.14.2.172.23902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brown IS. Development of a scale to measure attitude towar the comdom as a method of birth control. J Sex Res. 1984;20:255–63. [Google Scholar]
- 32.Sacco WP, Levine B, Reed DL, Thompson K. Attitudes abotu condom use as an AIDS-relevant behavior: Their factor structure and relation to condom use. Psychol Asess. 1991:265–72. [Google Scholar]
- 33.Noar SM, Morokoff PJ, Harlow LL. Condom negotiation in hetersexually active men and women: Development and validation of a condom influence strategy questionnaire. Psychol Health. 2002;17(6):711–35. [Google Scholar]
- 34.Carey MP, Carey KB, Maisto SA, Gordon CM, Schroder KEE, Vanable PA. Reducing HIV risk among psychiatric outpatients: Results from a randomized controlled trail. J Consult Clin Psychol. 2004;72(2):252–68. doi: 10.1037/0022-006X.72.2.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weinhardt LS, Forsyth AD, Carey MP, Jaworski BC, Durant LE. Reliability and validity of self-reported HIV-risk behavior: Progress since 1990 and recommendations for research and practice. Arch Sex Behav. 1998;27:155–80. doi: 10.1023/a:1018682530519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Muthen LK, Muthen BO. Mplus User's Guide. 5th edition. Los Angeles, CA: Muthen & Muthen; 1998-2007. [Google Scholar]
- 37.Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of an information-motivation-behavioral skills model of AIDS preventitive behavior in gay me and heterosexual university students. Health Psychol. 1994;13(3):238–50. doi: 10.1037//0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- 38.Fisher WA, Williams SS, Fisher JD, Malloy TE. Understanding AIDS risk behavior among sexually active urban adolescents. An empirical test of the Information-Motivation-Behavioral Skills model. AIDS Behav. 1999;3:13–23. [Google Scholar]
- 39.Augenbraun M, Wilson TE, Allister L. Domestic violence reported by women attending a sexually transmitted disease clinic. Sex Transm Dis. 2001;28(3):143–7. doi: 10.1097/00007435-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 40.Tjaden P, Thoennes N. Extent, nature, and consequences of intimate partner violence: Findings from the National Violence Against Women Survey. Washington, DC: National Institute of Justice and the Centers for Disease Control and Prevention; 2000. [Google Scholar]
- 41.Fisher JD, Fisher WA. Theoretical approaches to individual-level change in HIV risk behavior. In: Peterson JL, DiClemente RJ, editors. Handbook of HIV prevention. New York: Kluwer Academic/ Plenum Press; 2000. pp. 3–55. [Google Scholar]
- 42.Donenberg GR, Schwartz RM, Emerson E, Wilson HW, Bryant FB, Coleman G. Applying a Cognitive-Behavioral Model of HIV Risk to Youths in Psychiatric Care. AIDS Educ Prev. 2005;17(3):200–16. doi: 10.1521/aeap.17.4.200.66532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kalichman S, Stein JA, Malow R, Averhart C, Devieux J, Jennings T, et al. Predicting protected sexual behavior using Information-Motivation-Behavioral skills model among adolescent substance abusers in court-ordered setting. Psychol Health Med. 2002;7(3):327–38. doi: 10.1080/13548500220139368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kalichman SC, Williams EA, Cherry C, Belcher L, Nachimson D. Sexual coercion, domestic violence, and negotiating condom use among low-income African American women. J Womens Health. 1998;7:371–8. doi: 10.1089/jwh.1998.7.371. [DOI] [PubMed] [Google Scholar]
- 45.Cavanaugh CE, Hansen NB, Sullivan TP. HIV sexual risk behavior among low-income women experiecing intimate partner violence: The role of posttraumatic stress disorder. AIDS Behav. 2010;14(2):318–27. doi: 10.1007/s10461-009-9623-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Karney BR, Hops HH, Redding CA, Reis HT, Rothman AJ, Simpson JA. A Framework for Incorporating Dyads in Models of HIV-Prevention. AIDS Behav. 2010;2010 doi: 10.1007/s10461-010-9802-0. In-print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Crosby RA, Salazar LF, YW L, Sanders SA, Graham CA, Arno JN. Theory-based approach to understanding condom errors and problems reported by men attending an STI clinic. AIDS Behav. 2008;12(3):412–8. doi: 10.1007/s10461-007-9264-1. [DOI] [PubMed] [Google Scholar]
- 48.Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? Findings from event-level research. Annu Rev Sex Res. 2000;11:125–57. [PMC free article] [PubMed] [Google Scholar]
- 49.Sikkema KJ, Nufield SA, Hansen NB, Mohlahlane R, Rensburg MJV, Watt MH, et al. Integrating HIV prevention into services for abused women in South Africa. AIDS Behav. 2010;14(2):431–9. doi: 10.1007/s10461-009-9620-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Neighbors AJ, O' Leary A. Responses of male inmates to primary partner requests for condom use: Effects of message content and domestic violence history. AIDS Educ Prev. 2003;15(1):93–108. doi: 10.1521/aeap.15.1.93.23841. [DOI] [PubMed] [Google Scholar]
- 51.Griffing S, Ragan DF, Sage RE, L M, Bingham LE, Primm BJ. Domestic violence survivors' self-identified reasons for returning to abusive relationships. J Interpers Violence. 2002;17(3):306–19. [Google Scholar]