Abstract
Rationale: Severe sepsis is common and highly morbid, yet the epidemiology of severe sepsis at the frontier of the health care system—pre-hospital emergency care—is unknown.
Objectives: We examined the epidemiology of pre-hospital severe sepsis among emergency medical services (EMS) encounters, relative to acute myocardial infarction and stroke.
Methods: Retrospective study using a community-based cohort of all nonarrest, nontrauma King County EMS encounters from 2000 to 2009 who were transported to a hospital.
Measurements and Main Results: Overall incidence rate of hospitalization with severe sepsis among EMS encounters, as well as pre-hospital characteristics, admission diagnosis, and outcomes. Among 407,176 EMS encounters, we identified 13,249 hospitalizations for severe sepsis, of whom 2,596 died in the hospital (19.6%). The crude incidence rate of severe sepsis was 3.3 per 100 EMS encounters, greater than for acute myocardial infarction or stroke (2.3 per 100 and 2.2 per 100 EMS encounters, respectively). More than 40% of all severe sepsis hospitalizations arrived at the emergency department after EMS transport, and 80% of cases were diagnosed on admission. Pre-hospital care intervals, on average, exceeded 45 minutes for those hospitalized with severe sepsis. One-half or fewer of patients with severe sepsis were transported by paramedics (n = 7,114; 54%) or received pre-hospital intravenous access (n = 4,842; 37%).
Conclusions: EMS personnel care for a substantial and increasing number of patients with severe sepsis, and spend considerable time on scene and during transport. Given the emphasis on rapid diagnosis and intervention for sepsis, the pre-hospital interval may represent an important opportunity for recognition and care of sepsis.
Keywords: sepsis, emergency medical services, epidemiology
At a Glance Commentary
Scientific Knowledge on the Subject
Severe sepsis is common and highly morbid, yet the epidemiology of severe sepsis at the frontier of the health care system—pre-hospital emergency care—is unknown.
What This Study Adds to the Field
Emergency medical services personnel care for an increasing number of patients hospitalized with severe sepsis, most of whom are diagnosed on admission. These findings, coupled with an average pre-hospital care time of 45 minutes, suggest an important opportunity to recognize severe sepsis before hospital arrival.
Severe sepsis represents a large and increasing burden on the U.S. health care system. The incidence of severe sepsis is greater than 3.0 per 1,000 population, and case fatalities approach 20%, accounting for more than $17 billion annually in medical costs (1–3). Even sepsis survivors often suffer with cognitive impairment and functional disability (4, 5). Advances in severe sepsis therapy, such as time-sensitive antibiotic administration and fluid resuscitation, require prompt diagnosis, and in some cases, transfer to referral centers for definitive therapy (6–11). Until now, such early recognition occurs after patients arrive at hospitals, when a critical window for treatment and referral may already have passed.
An alternative approach may be to diagnose and treat severe sepsis in the pre-hospital period, using emergency medical services (EMS) personnel (12, 13). More than 800,000 EMS personnel provide care to tens of millions of persons as part of an emergency system (14) that transports more than 35 patients every minute of every day (15). EMS systems already play a key role in the management of acute cardiovascular disease, stroke, and trauma, conditions that benefit from care at optimal centers with advanced warning (16–18). Yet, no similar care coordination or pre-hospital management is widely adopted in severe sepsis. The uncertain burden of pre-hospital sepsis, difficulty in rapid diagnosis, and variable pre-hospital care and times are barriers to shifting the paradigm of sepsis care from the emergency department to the ambulance gurney (13, 19).
The goals of this investigation are to describe the incidence, pre-hospital characteristics, and outcomes of EMS encounters hospitalized with severe sepsis in a 10-year cohort study, including those diagnosed on admission. To better understand the burden of severe sepsis on the EMS system, we compared our data with the epidemiology of acute myocardial infarction and stroke, and evaluated trends over the decade. The investigation offers a first step in understanding the opportunities for severe sepsis recognition at the frontier of critical care. Some of the results of these studies have been previously reported in the form of an abstract (20).
Methods
Study Design and Data
We performed a retrospective cohort study of all EMS encounters in King County, Washington excluding the city of Seattle, from 2000 to 2009. Greater King County has 1.2 million residents and is composed of urban, semiurban, and rural areas. The region is served by a mature, two-tier EMS system in existence since 1976. King County EMS is the primary first response for all medical 9-1-1 calls in King County. First-tier response is provided by emergency medical technician–firefighters who provide basic life support (BLS) care. The second tier is provided by paramedics who are trained in advanced life support (ALS), and respond to more severely ill patients on the basis of protocols and assessments by both emergency medical dispatchers and BLS responders. During the decade, no protocols guided the care of sepsis or severe sepsis by EMS personnel, nor did the number of ALS ambulances increase per capita (2.7 per 100,000).
We obtained EMS incident reports from a computerized database containing detailed information on dispatch, demographic, clinical, and transport data for each incident. The data quality, deduplication of records, and database characteristics have been previously described (21). We linked EMS data to Washington State hospital discharge records in the Comprehensive Hospital Abstract Reporting System (CHARS) database, using a hierarchical deterministic matching algorithm with direct identifiers from 2000 to 2010. Our year-specific population estimates were obtained from the U.S. Census Bureau American Community Survey (http://www.census.gov/acs/www/). We did not include the city of Seattle EMS encounters in the primary study, as these reside in a distinct database. The project was approved by the Washington State Department of Health and King County Emergency Medical Services Review Committees.
Case Selection and Definitions
We examined all adult EMS encounters involving nontrauma, non–cardiac arrest patients transported from a scene to a receiving hospital by ground ambulance (Figure 1). We defined trauma and cardiac arrest on the basis of EMS documentation, excluding these patients as they are treated in emergency care systems with mature care pathways (22, 23). We excluded EMS encounters for patients younger than 18 years at the time of the incident, as the epidemiology and etiology of severe sepsis among pediatric encounters are unlikely to be representative of the population as a whole. Repeat EMS encounters for individual patients were included in the cohort. We defined hospitalization with severe sepsis, acute myocardial infarction, and stroke on the basis of clinically validated, administrative definitions based on the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes (24–28). We used the Angus and colleagues implementation of severe sepsis, including explicit diagnoses of severe sepsis (ICD-9-CM 995.92 and 785.52), as it is the most accurate and sensitive algorithm compared with structured manual chart review (29). We defined in-hospital mortality on the basis of hospital discharge disposition fields in the CHARS database (27). Beginning in 2009, CHARS identified conditions that were “present on admission (POA).” For this year, we defined hospitalization with severe sepsis diagnosed on admission if the ICD-9-CM code for both infection and organ dysfunction, or the explicit severe sepsis code, had POA indicator flags. We validated POA indicators for the Angus severe sepsis implementation in a separate cohort and found that the majority agreed with manual chart review (agreement, 91%; κ statistic, 0.78; 95% confidence interval [CI]: 0.67, 0.88). Please see the online supplement for details of the manual validation and agreement for alternative definitions of severe sepsis.
Figure 1.
Patient accrual diagram. EMS = emergency medical services.
We abstracted pre-hospital, clinical data from the King County EMS database, including dispatch, demographic, physical examination, procedural, and transport data. We evaluated only initial pre-hospital vital signs, documented by first arriving EMS personnel. We evaluated call urgency as categorized by first responding EMS personnel (e.g., nonurgent, urgent, life-threatening). Additional details on definitional algorithms for ICD-9-CM codes and pre-hospital descriptive data are provided in the online data supplement.
Analysis
We report continuous variables as mean (SD) or median (interquartile range), as appropriate; categorical variables are reported as frequencies or percentages. We analyzed the following: (1) pre-hospital characteristics and outcomes of those EMS encounters hospitalized with severe sepsis, including those with severe sepsis diagnosed on admission; (2) crude incidence and case fatality rates of hospitalizations with severe sepsis, compared with control patients, with acute myocardial infarction (AMI) or stroke; (3) reliability-adjusted rates from mixed logistic regression models including multiple a priori confounders; and (4) temporal trends between 2000 and 2009.
We first describe pre-hospital characteristics and outcomes of all EMS encounters hospitalized with severe sepsis, including pre-hospital vital signs, interventions performed by EMS personnel, and pre-hospital time intervals. Using discharge data, we also report the etiology of severe sepsis, organ failures, and discharge disposition. We compared pre-hospital data for EMS encounters with severe sepsis on admission versus diagnosis later in the hospital stay. To determine whether EMS encounters hospitalized with severe sepsis were different from those arriving by other means, we conducted a sensitivity analysis of 2006 data comparing hospital data for EMS versus no EMS transport to the hospital (further detailed in the online supplement).
We calculated the crude incidence rate of hospitalization for severe sepsis as a proportion of all noncardiac arrest, nontrauma EMS encounters, and compared this with control groups with AMI and stroke. We determined total deaths and crude case fatality rates as the proportion of in-hospital deaths among all cases. To determine adjusted rates, we included age, sex, and receiving hospital in mixed multivariable logistic models. These adjustments account for potential variation over time in demographics among King County residents who access the emergency care and hospital system, hospital coding practices (30), and statistical noise due to differences in sample size (“reliability adjustment”) (31). We considered that trends in case fatality rates may derive from changes in illness severity, and included both the Charlson Comorbidity Index and a pre-hospital clinical risk score for critical illness in our models for case fatality (21, 32). The latter includes important confounders such as initial systolic blood pressure, heart rate, Glasgow Coma Scale score, pulse oximetry, and pre-hospital location (e.g., nursing home).
To analyze trends from 2000 to 2009, we graphed changes in the rates of hospitalization, deaths, and case fatality by year. We evaluated the significance of change over time, using unadjusted Poisson regression, and illustrate year-specific rate estimates from our above-described multivariable mixed models. We hypothesized that differential changes in population could account for trends over the decade, and also graphed hospitalization rates standardized to the age distribution of the King County population in 2001 (census data available from 2001 to 2009). We considered that discharge diagnoses may capture severe sepsis cases only after hospitalization, so we restricted our sample to subjects who expired in-hospital within 72 hours of admission, and repeated our analysis.
We used STATA 11.0 SE (Stata Corp, College Station, TX) for all analyses. All tests were two-tailed, and we considered a P value not greater than 0.05 to be significant per comparison. This work was previously presented in abstract form at the 2012 American Thoracic Society International Conference in San Francisco, California.
Results
Study Population and Incidence of Severe Sepsis
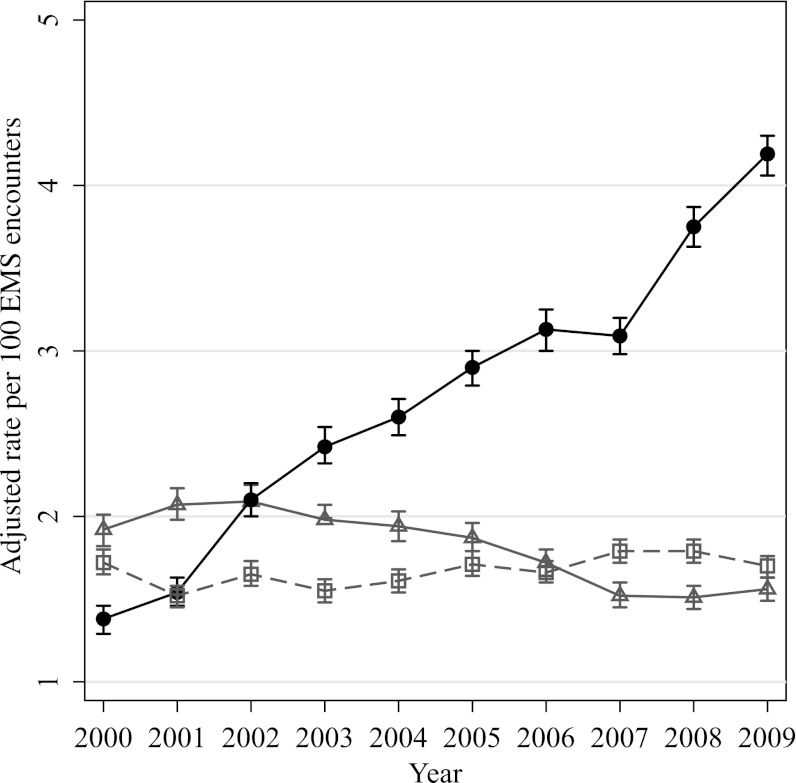
Of all EMS encounters during the study period (n = 883,604), 540,351 (61%) adult encounters were transported to a hospital. Excluding encounters with pre-hospital trauma (n = 128,033; 24%) and cardiac arrest (n = 5,142; 1%) resulted in a study sample of 407,176 records (Figure 1). Of these, the annual number of EMS encounters increased from 34,571 in 2000 to 46,723 by 2009. The percentage admitted to a hospital was 31.7% (n = 128,929), the mean age was 60 years (SD, 21 yr), and 7.3% of encounters (n = 29,602) were transported from nursing homes. We observed that 13,249 EMS encounters were hospitalized with severe sepsis (3.3 per 100 EMS encounters), compared with 9,069 encounters with acute myocardial infarction (2.3 per 100) and 8,981 (2.2 per 100) with stroke. These rates were robust to multivariable adjustment (Figure 2). In a sensitivity analysis, we observed that EMS transported approximately 40% of all hospitalizations for severe sepsis brought to the emergency department during the 2006 calendar year (details provided in the online supplement).
Figure 2.
Temporal changes in the rates of hospitalizations with severe sepsis among emergency medical services (EMS) encounters, adjusted for age, sex, and receiving hospital. A comparison with acute myocardial infarction (AMI) and stroke is provided for context. Error bars represent 95% confidence intervals. Solid circles, severe sepsis; gray triangles, AMI; gray squares, stroke.
Pre-Hospital Characteristics and Care of Severe Sepsis Hospitalizations
Among EMS encounters hospitalized with severe sepsis (Table 1), we observed that only one-half were transported by paramedics (54%), and one in five was thought to have life-threatening conditions by EMS personnel (19%). As recently as 2009, more than half of encounters met systemic inflammatory response syndrome (SIRS) criteria for heart rate (58%) and respiratory rate (50%) at the time EMS personnel arrived on scene. Pre-hospital hypotension was uncommon, present in only 21% of encounters (Table 1). On average, EMS personnel provided on-scene care for 35 (±18) minutes, including a mean 43 (±19) minutes when paramedics responded (see Table E1 in the online supplement). Many encounters were notable for scene times greater than 50 minutes (n = 1,856; 15% of those with complete data). The average transport time from scene to hospital was 12.6 (±10) minutes. EMS personnel commonly placed supplemental oxygen (72%), but placed peripheral intravenous access in fewer than one-half of patients (37%). Endotracheal intubation and bag valve mask ventilation were similarly uncommon.
TABLE 1.
PRE-HOSPITAL CHARACTERISTICS OF SEVERE SEPSIS HOSPITALIZATIONS COMPARED WITH THOSE HOSPITALIZED WITH ACUTE MYOCARDIAL INFARCTION OR STROKE
| Variable | Hospitalizations with Severe Sepsis (n = 13,249) | Hospitalizations with AMI (n = 9,069) | Hospitalizations with Stroke (n = 8,981) |
| Age, yr: mean (SD) | 71 (16) | 71 (14) | 75 (14) |
| Female sex, no. (%) | 6,149 (48) | 3,863 (44) | 4,826 (55) |
| Level of EMS care, no. (%) | |||
| ALS + BLS | 7,114 (54) | 6,562 (72) | 2,625 (29) |
| BLS only | 6,135 (46) | 2,507 (28) | 6,356 (71) |
| EMS severity, no (%)* | |||
| Life-threatening | 1,822 (19) | 1,566 (21) | 656 (9) |
| Urgent | 4,990 (51) | 4,552 (61) | 4,298 (60) |
| Nonurgent | 2,876 (30) | 1,378 (18) | 2,231 (31) |
| Pre-hospital time interval, min: mean (SD) | |||
| Responding to scene time | 4.7 (3.6) | 4.3 (3.3) | 4.6 (3.4) |
| Total scene time | 34.8 (18.3) | 34.4 (17) | 26.9 (14) |
| Scene-to-hospital time | 12.6 (10.5) | 12 (9.3) | 13.1 (10.2) |
| Abnormal pre-hospital vital signs, no. (%) | |||
| Systolic blood pressure ≤ 90 mm Hg | 2,485 (21) | 938 (12) | 285 (4) |
| Respiratory rate > 36 breaths/min | 1,790 (16) | 681 (9) | 152 (2) |
| Glasgow Coma Scale score ≤ 11 | 1,699 (14) | 381 (4) | 1,048 (12) |
| SaO2 < 88% | 1,369 (10.3) | 378 (3) | 139 (2) |
| Heart rate ≥ 120 beats/min | 2,771 (24) | 1,089 (14) | 527 (7) |
| Pre-hospital critical illness risk score, mean (SD)† | 2.3 (1.4) | 1.71 (1.09) | 1.49 (0.92) |
| Pre-hospital procedures, no. (%) | |||
| Supplemental oxygen | 9,520 (72) | 7,670 (85) | 5,888 (66) |
| Bag valve mask ventilation | 1,538 (11.6) | 405 (4) | 415 (5) |
| Endotracheal intubation | 1,968 (15) | 467 (5) | 511 (6) |
| ECG monitoring | 6,872 (52) | 6,468 (71) | 2,543 (28) |
| Peripheral intravenous access‡ | 4,842 (37) | 5,311 (59) | 1,438 (16) |
Definition of abbreviations: ALS = advanced life support; AMI = acute myocardial infarction; BLS = basic life support; EMS = emergency medical services; SaO2 = arterial oxygen saturation.
Determined by first arriving EMS personnel.
Calculated as an integer score ranging from 0 to 8, using a previously published risk model (21).
Peripheral intravenous access does not include placement of central or intraosseous catheters.
Severe Sepsis Diagnosed on Admission
Using validated present-on-admission indicators in 2009, we observed that the vast majority of severe sepsis among EMS encounters was diagnosed on admission (80%; 1,844 of 2,305). Using only admission diagnoses, the rate of severe sepsis hospitalization (3.94 per 100 encounters) was greater than that for acute myocardial infarction (1.75 per 100 encounters) and stroke (2.11 per 100 encounters) combined. Notably, more hypotension, depressed mental status, and hypoxemia were present during pre-hospital care of severe sepsis cases diagnosed on admission, compared with severe sepsis diagnosed later in the hospital stay (Table 2; P < 0.05).
TABLE 2.
PRE-HOSPITAL CHARACTERISTICS OF SEVERE SEPSIS HOSPITALIZATIONS IN 2009, COMPARING BY DIAGNOSIS ON ADMISSION
| Variable | All Hospitalizations with Severe Sepsis (n = 2,305) | Severe Sepsis Diagnosed on Admission (n = 1,844) | Severe Sepsis Not Diagnosed on Admission (n = 461) | P Value* |
| Age, yr: mean (SD) | 72 (15) | 73 (15) | 69 (17) | <0.01 |
| Female sex, no. (%) | 1,184 (52) | 951 (52) | 233 (51) | 0.72 |
| Level of EMS care, no. (%) | ||||
| ALS + BLS | 1,118 (48) | 908 (49) | 210 (46) | 0.16 |
| BLS only | 1,187 (52) | 936 (51) | 251 (54) | |
| EMS severity, no (%)† | ||||
| Life-threatening | 67 (17) | 56 (18) | 11 (18) | 0.54 |
| Urgent | 197 (52) | 160 (51) | 37 (58) | |
| Nonurgent | 115 (30) | 99 (31) | 16 (25) | |
| Pre-hospital time interval, min: mean (SD) | ||||
| Responding to scene time | 6.2 (3.7) | 6.1 (3.4) | 6.6 (4.8) | <0.01 |
| Total scene time | 32.8 (17.1) | 33.2 (17.2) | 31.1 (16.5) | 0.02 |
| Scene-to-hospital time | 12.7 (10.5) | 12.4 (10.1) | 14.4 (12.0) | 0.01 |
| Abnormal pre-hospital vital signs, no. (%) | ||||
| Systolic blood pressure ≤ 90 mm Hg | 477 (22) | 408 (23) | 69 (17) | <0.01 |
| Respiratory rate > 36 breaths/min | 227 (11) | 192 (11) | 35 (8) | 0.07 |
| Glasgow Coma Scale score ≤ 11 | 382 (12) | 248 (13) | 34 (7) | <0.01 |
| SaO2 < 88% | 344 (15) | 294 (16) | 50 (11) | <0.01 |
| Heart rate ≥ 120 beats/min | 448 (20) | 374 (21) | 74 (17) | 0.04 |
| Pre-hospital critical illness risk score, mean (SD) ‡ | 2.28 (1.34) | 2.36 (1.38) | 1.95 (1.11) | <0.01 |
| Pre-hospital procedures, no. (%) | ||||
| Supplemental oxygen | 1,518 (66) | 1,235 (67) | 283 (61) | 0.03 |
| Bag valve mask ventilation | 191 (8) | 167 (9) | 24 (5) | <0.01 |
| ECG monitoring | 1,047 (45) | 856 (46) | 191 (41) | 0.05 |
| Endotracheal intubation | 252 (11) | 224 (12) | 28 (6) | <0.01 |
| Peripheral intravenous access§ | 720 (31) | 596 (32) | 124 (27) | 0.03 |
Definition of abbreviations: ALS = advanced life support; BLS = basic life support; EMS = emergency medical services; SaO2 = arterial oxygen saturation.
Comparing diagnosed on admission versus not diagnosed on admission; parametric or nonparametric test, as appropriate.
Determined by first arriving EMS personnel.
Calculated as an integer score ranging from 0 to 8, using a previously published risk model (20).
Peripheral intravenous access does not include placement of central or intraosseous catheters.
Outcomes of Pre-Hospital Encounters
We observed that respiratory diagnoses were the most common etiology of severe sepsis among EMS encounters, whereas organ failures were more likely to be renal or pulmonary (Table 3). Nearly one in four severe sepsis cases had two or more organ failures (n = 3,294; 25%) One-half were admitted to an intensive care unit (n = 6,224; 52%), and less than one-third were eventually discharged to home (29%). The total number of severe sepsis deaths was 2,596 (19.6%), nearly double the deaths among EMS encounters hospitalized with AMI (n = 932; 10.2%) or stroke (n = 1,076; 12%). In mixed logistic models adjusted for demographics, pre-hospital illness severity, comorbidity, and receiving hospital, we estimated EMS encounters with severe sepsis were more likely to die in the hospital (10.6 per 100) than those with AMI (2.5 per 100) or stroke (8.0 per 100). In a sensitivity analysis of 2006 data, the hospitalization characteristics and outcomes of severe sepsis were similar when comparing those who were and were not transported by EMS (Table E2).
TABLE 3.
COMPARISON OF OUTCOMES OF EMERGENCY MEDICAL SERVICES ENCOUNTERS HOSPITALIZED WITH SEVERE SEPSIS, ACUTE MYOCARDIAL INFARCTION, AND STROKE
| Variable | Hospitalizations with Severe Sepsis (n = 13,249) | Hospitalizations with Acute MI (n = 9,069) | Hospitalizations with Stroke (n = 8,981) |
| Possible etiology of sepsis, no. (%)* | |||
| Respiratory | 8,154 (62) | — | — |
| Urological | 5,043 (38) | — | — |
| Gastrointestinal | 3,808 (29) | — | — |
| Skin, soft tissue, joint | 1,579 (12) | — | — |
| Central nervous system | 75 (1) | — | — |
| Cardiovascular | 105 (1) | — | — |
| Organ failures, no. (%) | |||
| Renal | 7,232 (55) | 1,148 (13) | 494 (6) |
| Pulmonary | 5,242 (40) | 978 (11) | 949 (11) |
| Cardiac | 2,279 (17) | 663 (7) | 85 (1) |
| Hematologic | 1,928 (15) | 223 (2) | 178 (2) |
| Neurological | 708 (5) | 112 (1) | 129 (1) |
| Hepatic | 277 (2) | 67 (1) | 13 (<1) |
| Total organ failures, mean (SD) | 1.41 (0.75) | 0.35 (0.7) | 0.21 (0.49) |
| Charlson Comorbidity Index, mean (SD) | 1.8 (1.7) | 2.17 (1.32) | 2.36 (1.48) |
| Admission to intensive care, no. (%) | 6,224 (52) | 4,460 (61) | 2,613 (35) |
| Hospital length of stay, d: median (IQR) | 6 (3–11) | 3 (2–5) | 3 (2–6) |
| Discharge disposition, no. (%)† | |||
| Expired | 2,596 (19.6) | 932 (10) | 1,076 (12) |
| Home | 3,812 (29) | 4,957 (55) | 2,778 (31) |
| Skilled nursing facility | 3,839 (29) | 1,308 (14) | 2,525 (28) |
| Long-term acute care | 150 (1) | 18 (<1) | 32 (<1) |
Definition of abbreviations: IQR = interquartile range; MI = myocardial infarction.
Possible etiologies of severe sepsis and the types of organ failures are not mutually exclusive categories.
Excludes categories such as home with health aid, transfer to acute care hospital, and unknown.
Trends over Time
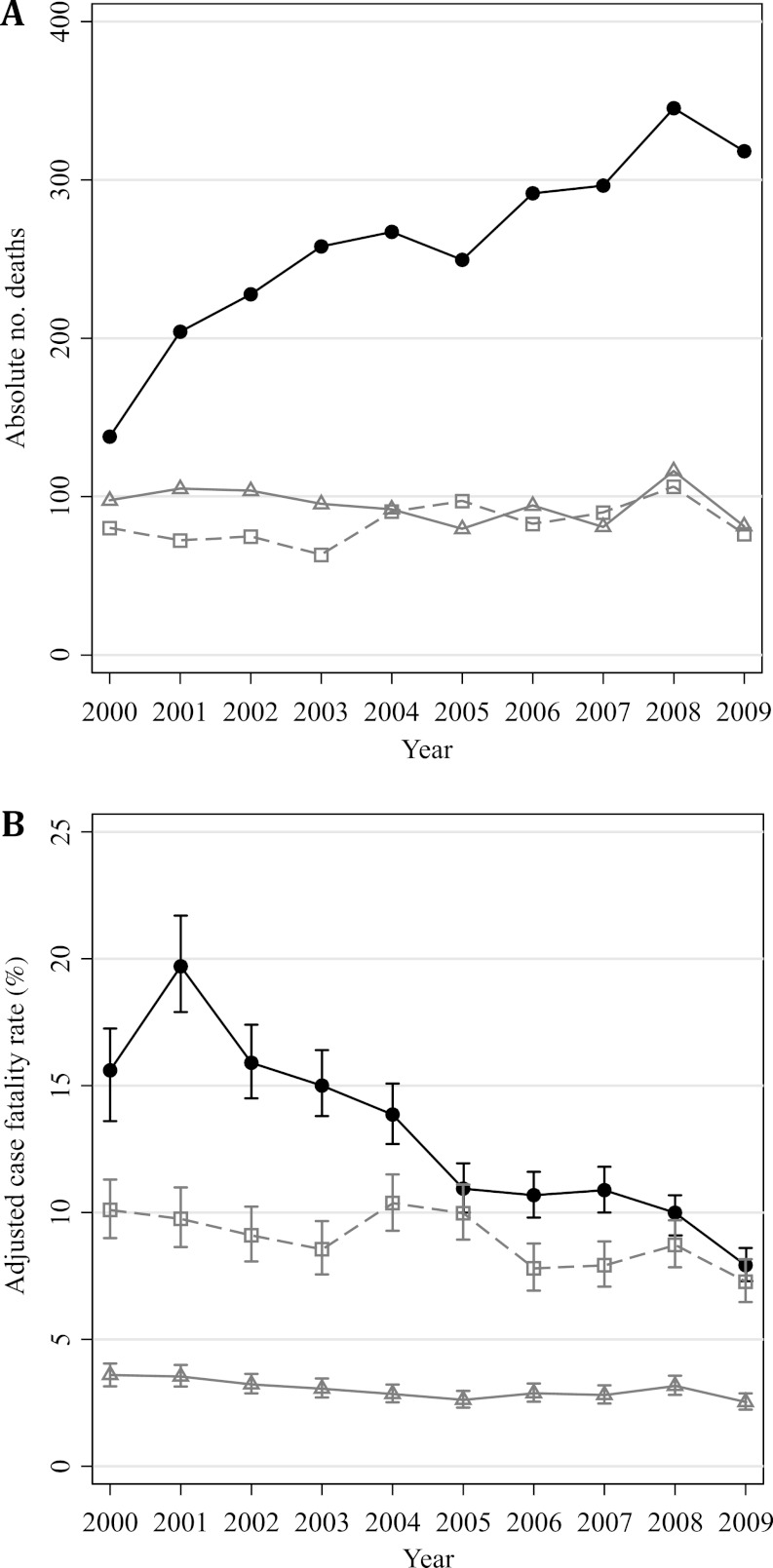
The crude rate of severe sepsis hospitalization increased by 11.8% per year (95% CI: 10, 13.7%; P < 0.01), relative to a 2.7% (95% CI: 1.3, 4.1%; P < 0.01) decrease per year for AMI and 2.9% (95% CI: 1.7, 4.1%; P < 0.01) increase per year for stroke. By 2009, for every 4 patients hospitalized with acute myocardial infarction, EMS personnel cared for 10 patients hospitalized with severe sepsis, including 8 of whom were diagnosed on admission. This trend was robust to adjustment for age, sex, and receiving hospital in mixed logistic models (Figure 2). The results were similar when we age-standardized rates to the King County population (Figure E1) or when we restricted our sample to only patients who died within 72 hours of admission (Figure E2). The absolute number of deaths among EMS encounters hospitalized with severe sepsis also increased over the decade, whereas adjusted case fatality rates improved (Figure 3). We found, however, that pre-hospital severity of illness increased during the study (Figure E3).
Figure 3.
(A) Absolute number of deaths and (B) adjusted case fatality rate among emergency medical services (EMS) encounters hospitalized with severe sepsis. Adjusted models include age, sex, Charlson Comorbidity Index, receiving hospital, and a pre-hospital clinical risk score for critical illness. A comparison with acute myocardial infarction and stroke is provided for context. Solid circles, severe sepsis; gray triangles, AMI; gray squares, stroke.
Discussion
In a large, community-based cohort over 10 years, we demonstrate that EMS personnel frequently encounter patients hospitalized with severe sepsis. The EMS system, as a whole, transports up to 40% of all severe sepsis hospitalizations in emergency departments, administering pre-hospital care for almost 1 hour in the sickest patients. Even though most severe sepsis cases were diagnosed on hospital admission, pre-hospital interventions, including intravenous access, were uncommon. These findings, coupled with the considerable time window for pre-hospital care, suggest an important and increasing opportunity to recognize and potentially treat severe sepsis before hospital arrival.
These data have implications for the practice of pre-hospital medicine and the development of a coordinated, regionalized system of critical care as recommended by the Institute of Medicine (33). No consensus exists on which emergency care conditions should be prioritized in such a centralized system (34). The changing burden, high case fatality rates, and frequent involvement of EMS in severe sepsis suggest it may deserve consideration along with acute cardiovascular disease and trauma in critical care system–level planning. For practicing EMS personnel, the ample pre-hospital care interval and large sepsis case volume highlight an understudied opportunity to optimize care (19). Few data or consensus exists to guide pre-hospital treatment or advanced notification of severe sepsis to hospitals (13, 35, 36), and the National EMS Research Agenda does not yet include topics related to infection or severe sepsis (37, 38). Paramedics could facilitate hospital-based triage and care, or affect pre-hospital care by delivery of fluid resuscitation or vasopressors (35), placement of venous access (39), or even administration of antibiotics for suspected sepsis (40). Yet, it is unknown whether the potential time-savings of these interventions would outweigh adverse events, inadvertent treatment, or mistriage. These steps deserve testing in rigorous observational and interventional studies, should accurate, reliable, and practical diagnostic tools for sepsis become available to first responders.
Despite spending almost 1 hour with the sickest patients, EMS personnel may be unaware they are transporting a patient with severe sepsis, a major barrier to testing patient or system interventions in pre-hospital sepsis (19). We observed that many EMS encounters hospitalized with severe sepsis were transported by basic life support providers, classified as “nonurgent,” and did not receive pre-hospital intravenous access—even though the vast majority were diagnosed on hospital admission. This occurred on a backdrop of thousands of low-risk EMS encounters, among whom 40% were not transported to hospitals and 70% brought to hospitals were discharged from the emergency department. The large low-risk call volume, coupled with modest EMS personnel knowledge of sepsis (12, 19), highlights an urgent need for accurate recognition tools for severe sepsis. Although no “12-lead ECG” is available, biological platforms that include traditional biomarkers or molecular expression profiles may complement existing clinical tools to assist in sepsis case finding. Such biological tools could build on physiological criteria (e.g., SIRS), and are increasingly available as point-of-care tests and biomarker panels in emergency care settings (41–43).
When we extrapolate our data to the U.S. health care system, EMS personnel may care for greater than 60,000 more patients per year hospitalized with severe sepsis than are hospitalized with acute myocardial infarction and stroke combined. Consistent with prior reports of hospital data, we found that the EMS system is caring for more patients hospitalized with severe sepsis. Multiple mechanisms may underlie this changing epidemiology (44, 45). First, population aging and more chronic disease in the community may increase the at-risk population for severe sepsis (46). These same risk factors may contribute to a relatively greater use of the EMS system in severe sepsis—as many elders have no transport to hospitals and are disproportionate users of 9-1-1 (47, 48). Alternatively, new ICD-9-CM codes for severe sepsis since 2003 may identify patients not previously captured, increasing the apparent burden on both EMS and hospitals. Such a trend is also hypothesized for organ failure coding, specifically acute kidney injury (49). These changes in ICD-9-CM coding practice may represent meaningful misclassification if the current approach overidentifies patients without true severe sepsis. However, administrative ICD9-CM algorithms for severe sepsis, including the Angus implementation, continue to be less sensitive compared with structured, manual chart review (29).
We also observed a temporal increase in severe sepsis deaths among EMS encounters, whereas case fatality rates are decreasing. No sepsis protocols were implemented at King County EMS during the decade, and differential pre-hospital care is unlikely to account for changes in outcomes. Yet, similar findings are reported by others in hospital cohorts (49, 50). This trend may reflect improvements in hospital care, including implementation of early resuscitation strategies in the emergency department (9, 11, 51), prompt and appropriate antibiotics (7), or improved care in the intensive care unit (52). Alternatively, less sick patients may fulfill the severe sepsis case definition (44). We assessed measures of pre-hospital illness severity, which increased during the decade and were greatest among patients with severe sepsis. This finding suggests that lower acuity is unlikely to be the only driver of the decrease in case fatality. In fact, other mechanisms, such as variable transfer patterns to long-term acute care facilities, termed “discharge bias,” may impact in-hospital mortality statistics (46, 53, 54).
We recognize the limitations of this investigation. First, we used administrative definitions of severe sepsis, acute myocardial infarction, and stroke that rely on ICD-9-CM codes. Although we used definitional algorithms that are clinically validated in prior studies (26–29), we expect that some misclassification is present among cases identified with acute illness and those without. Notably, a small minority of patients developed severe sepsis later in the hospital stay, and we were unable to define POA cases before 2009. Our single-center manual validation of severe sepsis POA indicators revealed high accuracy—although POA flags may be differentially used across hospitals (55). Future studies are needed to understand the importance of pre-hospital care for the minority of patients who may develop severe sepsis later in the hospital stay. Second, we used a cohort of primarily ground transport and urban/suburban EMS encounters in King County, and our data may be less generalizable to longer distance or aeromedical transports in rural areas. In fact, we observed longer scene and transport times than previously described in trauma patients (56)—and are unable to determine whether this results from the performance of pre-hospital procedures or vice versa. Last, we acknowledge that unmeasured changes in population epidemiology may impact relative trends of severe sepsis. For these reasons, we used a population in which virtually all EMS responses are met by the King County EMS system, and report rates among EMS encounters age-standardized to U.S. Census data in a sensitivity analysis. Our study region has broad diversity with respect to age, sex, and race/ethnicity, and has been previously used for national estimates of the incidence of critical illness (57). Sensitivity analyses were unchanged from our primary analysis, and support the generalizability of the findings to the U.S. emergency care system.
Emergency medical services personnel care for a substantial and increasing number of patients with severe sepsis. Given the emphasis on rapid diagnosis and intervention for severe sepsis and septic shock, the pre-hospital interval represents an important opportunity for recognition and care of sepsis.
Supplementary Material
Acknowledgments
The authors acknowledge the assistance of Mr. William O’Brien for linking data between EMS records and hospital discharge data. The authors also acknowledge the assistance of Brandon Cicero in obtaining King County census data.
Footnotes
Supported in part by a grant from the American Heart Association (11CRP5050017; C.W.S.). T.D.R. is supported by grants from the National Institutes of Health (R01 HL088576-01A1, R01 HL074098-01A1). D.M.Y. is supported in part by grants from the National Institutes of Health (1P50GM076659, 1R01HL085565-01A2, 1K12HL109068-01). D.C.A. is supported in part by a grant from the National Institutes of Health (P50GM076659). These funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Author Contributions: C.W.S., involved in design of the study, acquisition of data, analysis of data, and drafting and revision of the manuscript; T.D.R., involved in conception, acquisition of data, hypothesis delineation, and substantial revision of the manuscript; J.M.K., involved in conception, design of the study, and substantial revision of the manuscript; A.J.W., involved in acquisition of data, analysis of the data, and substantial revision of the manuscript; D.M.Y., involved in conception, design of the study, and substantial revision of the manuscript; D.C.A., involved in conception, design of the study, and substantial revision of manuscript.
This article has an online supplement, which is available from this issue’s table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.201204-0713OC on October 18, 2012
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Dombrovskiy VY, Martin AA, Sunderram J, Paz HL. Rapid increase in hospitalization and mortality rates for severe sepsis in the united states: a trend analysis from 1993 to 2003. Crit Care Med 2007;35:1244–1250 [DOI] [PubMed] [Google Scholar]
- 2.Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada-Vera B. Deaths: final data for 2006. Natl Vital Stat Rep 2009;57:1–134 [PubMed] [Google Scholar]
- 3.Kumar G, Kumar N, Taneja A, Kaleekal T, Tarima S, McGinley E, Jimenez E, Mohan A, Khan RA, Whittle J, et al. Nationwide trends of severe sepsis in the 21st century (2000–2007). Chest 2011;140:1223–1231 [DOI] [PubMed] [Google Scholar]
- 4.Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 2010;304:1787–1794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perl TM, Dvorak L, Hwang T, Wenzel RP. Long-term survival and function after suspected gram-negative sepsis. JAMA 1995;274:338–345 [PubMed] [Google Scholar]
- 6.Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 2006;34:1589–1596 [DOI] [PubMed] [Google Scholar]
- 7.Gaieski DF, Mikkelsen ME, Band RA, Pines JM, Massone R, Furia FF, Shofer FS, Goyal M. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med 2010;38:1045–1053 [DOI] [PubMed] [Google Scholar]
- 8.Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 2008;36:296–327 [DOI] [PubMed] [Google Scholar]
- 9.Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001;345:1368–1377 [DOI] [PubMed] [Google Scholar]
- 10.Ferrer R, Artigas A, Levy MM, Blanco J, Gonzalez-Diaz G, Garnacho-Montero J, Ibanez J, Palencia E, Quintana M, de la Torre-Prados MV. Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA 2008;299:2294–2303 [DOI] [PubMed] [Google Scholar]
- 11.Jones AE, Shapiro NI, Trzeciak S, Arnold RC, Claremont HA, Kline JA. Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA 2010;303:739–746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seymour CW, Carlbom D, Engelberg RA, Larsen J, Bulger EM, Copass MK, Rea TD. Understanding of sepsis among emergency medical services: a survey study. J Emerg Md 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang HE, Weaver MD, Shapiro NI, Yealy DM. Opportunities for emergency medical services care of sepsis. Resuscitation 2010;81:193–197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bailey JC, editor. EMS workforce for the 21st century: a national assessment [public health in the 21st century]. Hauppauge, NY: Nova Biomedical; 2008
- 15.Pitts SR, Niska RW, Xu J, Burt CW. National hospital ambulatory medical care survey: 2006 emergency department summary. Natl Health Stat Report 2008;6:1–38 [PubMed] [Google Scholar]
- 16.Jollis JG, Roettig ML, Aluko AO, Anstrom KJ, Applegate RJ, Babb JD, Berger PB, Bohle DJ, Fletcher SM, Garvey JL, et al. Implementation of a statewide system for coronary reperfusion for ST-segment elevation myocardial infarction. JAMA 2007;298:2371–2380 [DOI] [PubMed] [Google Scholar]
- 17.Nathens AB, Jurkovich GJ, Cummings P, Rivara FP, Maier RV. The effect of organized systems of trauma care on motor vehicle crash mortality. JAMA 2000;283:1990–1994 [DOI] [PubMed] [Google Scholar]
- 18.Rea TD, Fahrenbruch C, Culley L, Donohoe RT, Hambly C, Innes J, Bloomingdale M, Subido C, Romines S, Eisenberg MS. CPR with chest compression alone or with rescue breathing. N Engl J Med 2010;363:423–433 [DOI] [PubMed] [Google Scholar]
- 19.Suffoletto B, Frisch A, Prabhu A, Kristan J, Guyette FX, Callaway CW. Prediction of serious infection during prehospital emergency care. Prehosp Emerg Care 2011;15:325–330 [DOI] [PubMed] [Google Scholar]
- 20.Seymour CW, Rea TD, Kahn JM, Yealy DM, Angus DC. Severe sepsis in prehospital emergency care: analysis of incidence, care, and outcome. Am J Respir Crit Care Med 2012;185:A1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seymour CW, Kahn JM, Cooke CR, Watkins TR, Heckbert SR, Rea TD. Prediction of critical illness during out-of-hospital emergency care. JAMA 2010;304:747–754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosenblatt RA, Macfarlane A, Dawson AJ, Cartlidge PH, Larson EH, Hart LG. The regionalization of perinatal care in Wales and Washington State. Am J Public Health 1996;86:1011–1015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med 2006;354:366–378 [DOI] [PubMed] [Google Scholar]
- 24.Joynt KE, Harris Y, Orav EJ, Jha AK. Quality of care and patient outcomes in critical access rural hospitals. JAMA 2011;306:45–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rosamond WD, Chambless LE, Sorlie PD, Bell EM, Weitzman S, Smith JC, Folsom AR. Trends in the sensitivity, positive predictive value, false-positive rate, and comparability ratio of hospital discharge diagnosis codes for acute myocardial infarction in four us communities, 1987–2000. Am J Epidemiol 2004;160:1137–1146 [DOI] [PubMed] [Google Scholar]
- 26.Hammar N, Alfredsson L, Rosen M, Spetz CL, Kahan T, Ysberg AS. A national record linkage to study acute myocardial infarction incidence and case fatality in Sweden. Int J Epidemiol 2001;30:S30–S34 [DOI] [PubMed] [Google Scholar]
- 27.Tirschwell DL, Longstreth WT., Jr Validating administrative data in stroke research. Stroke 2002;33:2465–2470 [DOI] [PubMed] [Google Scholar]
- 28.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001;29:1303–1310 [DOI] [PubMed] [Google Scholar]
- 29.Iwashyna TJ, Odden A, Rohde J, Bonham C, Kuhn L, Malani P, Chen L, Flanders S. Identifying patients with severe sepsis using administrative claims: patient-level validation of the Angus implementation of the international consensus conference definition of severe sepsis. Med Care (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Romano PS, Schembri ME, Rainwater JA. Can administrative data be used to ascertain clinically significant postoperative complications? Am J Med Qual 2002;17:145–154 [DOI] [PubMed] [Google Scholar]
- 31.Dimick JB, Staiger DO, Birkmeyer JD. Ranking hospitals on surgical mortality: the importance of reliability adjustment. Health Serv Res 2010;45:1614–1629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130–1139 [DOI] [PubMed] [Google Scholar]
- 33. Committee on the Future of Emergency Care in the United States Health System, Institute of Medicine. Hospital based emergency care: at the breaking point. Washington, DC: National Academies Press; 2007.
- 34.Carr BG, Conway PH, Meisel ZF, Steiner CA, Clancy C. Defining the emergency care sensitive condition: a health policy research agenda in emergency medicine. Ann Emerg Med 2010;56:49–51 [DOI] [PubMed] [Google Scholar]
- 35.Seymour CW, Cooke CR, Mikkelsen ME, Hylton J, Rea TD, Goss CH, Gaieski DF, Band RA. Out-of-hospital fluid in severe sepsis: effect on early resuscitation in the emergency department. Prehosp Emerg Care 2010;14:145–152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Seymour CW, Band RA, Cooke CR, Mikkelsen ME, Hylton J, Rea TD, Goss CH, Gaieski DF. Out-of-hospital characteristics and care of patients with severe sepsis: a cohort study. J Crit Care 2010;25:553–562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sayre MR, White LJ, Brown LH, McHenry SD. The national EMS research strategic plan. Prehosp Emerg Care 2005;9:255–266 [DOI] [PubMed] [Google Scholar]
- 38.Sayre MR, White LJ, Brown LH, McHenry SD. The national EMS research agenda executive summary: emergency medical services. Ann Emerg Med 2002;40:636–643 [DOI] [PubMed] [Google Scholar]
- 39.Davis DP, Ramanujam P. Central venous access by air medical personnel. Prehosp Emerg Care 2007;11:204–206 [DOI] [PubMed] [Google Scholar]
- 40.Cooke ME. Prehospital administration of benzyl penicillin by paramedics in the UK. J Emerg Prim Health Care 2005;3:1–2 [Google Scholar]
- 41.Guyette F, Suffoletto B, Castillo JL, Quintero J, Callaway C, Puyana JC. Prehospital serum lactate as a predictor of outcomes in trauma patients: a retrospective observational study. J Trauma 2011;70:782–786 [DOI] [PubMed] [Google Scholar]
- 42.Goyal M, Pines JM, Drumheller BC, Gaieski DF. Point-of-care testing at triage decreases time to lactate level in septic patients. J Emerg Med 2008;38:578–581 [DOI] [PubMed] [Google Scholar]
- 43.Jansen TC, van Bommel J, Mulder PG, Rommes JH, Schieveld SJ, Bakker J. The prognostic value of blood lactate levels relative to that of vital signs in the pre-hospital setting: a pilot study. Crit Care 2008;12:R160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lagu T, Rothberg MB, Shieh MS, Pekow PS, Steingrub JS, Lindenauer PK. Hospitalizations, costs, and outcomes of severe sepsis in the United States 2003 to 2007. Crit Care Med 2012;40:754–761 [DOI] [PubMed] [Google Scholar]
- 45.Lindenauer PK, Lagu T, Shieh MS, Pekow PS, Rothberg MB. Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009. JAMA 2012;307:1405–1413 [DOI] [PubMed] [Google Scholar]
- 46.Kahn JM, Benson NM, Appleby D, Carson SS, Iwashyna TJ. Long-term acute care hospital utilization after critical illness. JAMA 2010;303:2253–2259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tangherlini N, Pletcher MJ, Covec MA, Brown JF. Frequent use of emergency medical services by the elderly: a case–control study using paramedic records. Prehosp Disaster Med 2010;25:258–264 [DOI] [PubMed] [Google Scholar]
- 48.Platts-Mills TF, Leacock B, Cabanas JG, Shofer FS, McLean SA. Emergency medical services use by the elderly: analysis of a statewide database. Prehosp Emerg Care 2010;14:329–333 [DOI] [PubMed] [Google Scholar]
- 49.Kumar G, Kumar N, Taneja A, Kaleekal T, Tarima S, McGinley E, Jimenez E, Mohan A, Khan RA, Whittle J, et al. Nationwide trends of severe sepsis in the twenty-first century (2000–2007). Chest 2011;140:1223–1231 [DOI] [PubMed] [Google Scholar]
- 50.Dombrovskiy VY, Martin AA, Sunderram J, Paz HL. Facing the challenge: decreasing case fatality rates in severe sepsis despite increasing hospitalizations. Crit Care Med 2005;33:2555–2562 [DOI] [PubMed] [Google Scholar]
- 51.Otero RM, Nguyen HB, Huang DT, Gaieski DF, Goyal M, Gunnerson KJ, Trzeciak S, Sherwin R, Holthaus CV, Osborn T, et al. Early goal-directed therapy in severe sepsis and septic shock revisited: concepts, controversies, and contemporary findings. Chest 2006;130:1579–1595 [DOI] [PubMed] [Google Scholar]
- 52.Scales DC, Dainty K, Hales B, Pinto R, Fowler RA, Adhikari NK, Zwarenstein M. A multifaceted intervention for quality improvement in a network of intensive care units: a cluster randomized trial. JAMA 2011;305:363–372 [DOI] [PubMed] [Google Scholar]
- 53.Kahn JM, Kramer AA, Rubenfeld GD. Transferring critically ill patients out of hospital improves the standardized mortality ratio: a simulation study. Chest 2007;131:68–75 [DOI] [PubMed] [Google Scholar]
- 54.Vasilevskis EE, Kuzniewicz MW, Dean ML, Clay T, Vittinghoff E, Rennie DJ, Dudley RA. Relationship between discharge practices and intensive care unit in-hospital mortality performance: evidence of a discharge bias. Med Care 2009;47:803–812 [DOI] [PubMed] [Google Scholar]
- 55.Goldman LE, Chu PW, Osmond D, Bindman A. The accuracy of present-on-admission reporting in administrative data. Health Serv Res 2011;46:1946–1962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Carr BG, Brachet T, David G, Duseja R, Branas CC. The time cost of prehospital intubation and intravenous access in trauma patients. Prehosp Emerg Care 2008;12:327–332 [DOI] [PubMed] [Google Scholar]
- 57.Rubenfeld GD, Herridge MS. Epidemiology and outcomes of acute lung injury. Chest 2007;131:554–562 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.