Abstract
Growing evidence links perceptions of neighborhood disorder to adverse health outcomes but little is known about psychological processes that may mediate this association. We tested the hypothesis that two psychological mechanisms—agonistic striving and subordination—mediate the link between perceived neighborhood disorder and hypertension risk in youth. Perceived neighborhood disorder, agonistic striving, subordination experiences, negative affect, obesity, and ambulatory blood pressure during daily activities (48 h) were assessed in a multiethnic sample of 167 low- to middle-income urban adolescents. Path analyses revealed that agonistic striving, subordination, and obesity each independently mediated the association between neighborhood disorder and blood pressure; these variables accounted for 73 % of the shared variance, 42 % of which was explained by agonistic striving. The direct relationship between perceived neighborhood disorder and blood pressure was no longer significant in the presence of these mediators. Negative affect was associated with neighborhood disorder and subordination, but not blood pressure. Agonistic striving proved to be a significant and substantial mediator of the association between perceived neighborhood disorder, blood pressure, and future hypertension risk. New research should seek to clarify the processes by which stressful neighborhoods induce persistent agonistic motives and perceptions of subordination in adolescents.
Keywords: Adolescent health, Perceived neighborhood disorder, Agonistic striving, Social power, Subordination, Implicit motives, Hypertension risk
Introduction
Poor quality or “disordered” neighborhoods may endanger residents’ health by undermining their perceived ability to control important events in their everyday lives (Martin-Storey et al., 2012; Weden et al., 2008; Wen et al., 2006). Neighborhood disorder refers to a lack of social and physical control over one’s neighborhood surroundings (Perkins & Taylor, 1996), a condition reflected in physical indices such as noise pollution, public drunkenness, litter, criminal activity, and harassment by police. Perceptions of neighborhood disorder have been linked to a host of adverse self-reported health outcomes, even after controlling for objective measures of socioeconomic status (Feldman & Steptoe, 2004; Steptoe & Feldman, 2001). Residents’ ratings of perceived neighborhood disorder correlate significantly with observer-rated neighborhood disorder at moderate levels (O’Neil et al., 2001; Perkins et al., 1992); residents and observers alike notice the same manifestations of disorder but the residents’ perceptions encompass an experienced neighborhood that is not readily apparent to the visiting observer. Perceptions of neighborhood disorder have been shown to predict self-reported health outcomes and use of health care services (Martin-Storey et al., 2012). But can individuals’ assessments of their neighborhoods alter their physiologic processes in ways that increase the risk of succumbing to leading public health threats such as cardiovascular illness? If so, what psychological mechanisms might be involved?
Theorists have speculated that adverse appraisals of personal and environmental resources may undermine health by frequently evoking negative emotions such as sadness, anxiety, and anger (Gallo & Matthews, 2003; Suls & Bunde, 2005). Yet a different possibility, suggested by social action theory, attributes certain adverse health effects to stress arousing motives that are induced by difficult interpersonal challenges of living in a disordered neighborhood. Resource-poor and threatening environments undermine social relationships and engender strivings for interpersonal control (Conger & Elder, 1994). Striving to influence or control one’s family members, neighbors, or others can make a challenging neighborhood environment even more stressful by provoking hostile social encounters and continuing power struggles (Ewart, 2011). Declining SES, associated with increased perceptions of neighborhood disorder (Deng et al., 2006; Feldman & Steptoe, 2004), has been linked to higher levels of interpersonal conflict, spouse abuse, harsh parenting, and marital dissolution (Aldarondo & Sugarman, 1996; Sidanius & Pratto, 1999). Social action theory proposes that environmentally-induced striving for interpersonal control can foster hypervigilant mental states and provoke coercive exchanges that raise blood pressure and endanger cardiovascular health (Ewart, 2011; Ewart et al., 1991; Smith et al., 2007).
In this view, perceptions of neighborhood disorder can damage health by arousing stressful motives. Entailed by this hypothesis is its corollary, namely, the implication that neighborhood environments also can increase stress levels by blocking the ability to satisfy motives that the environment arouses. The many challenges of living in a disadvantaged and dangerous neighborhood can increase one’s need to exercise social control yet also make it difficult to satisfy such striving by exerting social influence or power (Guinote & Vescio, 2010; Keltner et al., 2003). Unfavorable living conditions may increase one’s exposure to denigration, subordination, marginalization, and isolation, and foster negative self-appraisals and feelings of powerlessness (Bullock & Lott, 2010; Sidanius & Pratto, 1999). Social action theory proposes that such appraisals promote states of heightened cardiovascular arousal against potential threats (Ewart et al., 2004; Tomaka et al., 1993). If frequent or sustained, such states may have damaging physiological consequences (Miller et al., 2009; Sapolsky, 2005). Research is needed to determine how social motives and power appraisals may operate—both together and independently—to mediate relationships between human living environments and cardiovascular disease risk. We here report data from a recent community-based study of urban adolescents testing the hypothesis that perceptions of neighborhood disorder foster social control motives and appraisals of denigration and low social power that elevate youths’ prevailing blood pressure levels, thereby increasing their risk of future hypertension and related cardiovascular diseases (Perloff et al., 1983; White et al., 1989).
Psychologists have begun to examine the adverse health effects of unfair treatment and rejection, both of which are increased by social disadvantage (Beatty et al., 2011; Beatty & Matthews, 2009; Dickerson et al., 2009; Eisenberger et al., 2003). But the potentially damaging consequences of persistent stress-inducing motives have received little attention (Ewart et al., 2012). Developing a social-motivational analysis of stress mechanisms involves undertaking the challenging task of identifying and measuring personal motives or self-goals that shape behavior in stressful social encounters. These goals often are “implicit;” that is, the goal is experienced so often in threatening circumstances that it becomes embedded in routine actions that are performed automatically and unthinkingly (Custers & Aarts, 2010; McClelland et al., 1989). Implicit motives thus are difficult to self-monitor and report on questionnaires. An alternative measurement approach uses a situationally grounded narrative assessment protocol, the Social Competence Interview (SCI; Ewart et al., 2002), which is designed to measure implicit self-goals that generate chronic stress. The procedure involves, first, re-living a problem situation that often causes stress; then imagining that this situation is a movie about a person similar to oneself; and finally, inventing a desired ending and narrative for the film and applying it to one’s personal circumstances. Motives that repeatedly evoke stress responses are inferred from the film narrative and emotion indices (see below). The participant’s level of emotional expressiveness during the interview indexes the likelihood that the implicit motive will cause recurring stress.
Social-motivational assessment with the SCI in two studies of more than 500 Black and White urban youth in different cities has disclosed that the recurring life difficulties that cause a person to experience chronic emotional stress tend to generate persistent motivational dispositions or “strivings.” These either take the form of a continuing struggle to overcome a personal defect, control a problem behavior, or improve performance (“transcendence striving”), or else take the form of a continuing struggle to change other people by getting them to be more friendly, more compliant, or less hostile (“agonistic striving;” Ewart, 1994; Ewart et al., 2011; Ewart & Jorgensen, 2004). Although the SCI assessment procedure allows for the possibility that, in a particular situation, an individual may have both self-focused and other-focused motives simultaneously, research has shown repeatedly that this is less true of the persistent life difficulties that generate recurring stress. Findings in different populations show that people tend to frame their ongoing, chronic difficulties either as perpetual agonistic struggles to control other people, or as perpetual transcendence struggles to control the self. Further, as we have described in previous reports, agonistic and transcendent strivings combine with differing levels of emotional expressiveness to form three qualitatively different motivational profiles, each of which characterized a distinctive cluster containing from 26 to 39 % of the participants in each sample (Ewart et al., 2011; Ewart & Jorgensen, 2004). One subgroup is emotionally invested in a continuing struggle to change or control other people but shows little or no desire to change or control the self. A second subgroup is emotionally invested in a continuing struggle to change or control the self but shows little or no desire to change or control other people. And a third distressed subgroup exhibits a lack of goal focus, and wishes instead that the persistent difficulties would just go away. In our social-motivational theory, these three subgroups are seen to be characterized, respectively, by agonistic striving, transcendence striving, and dissipated striving. During the SCI assessment protocol, each group displays a distinctive behavioral signature: The agonistic striving profile is marked by a high level of emotional expressiveness, high agonistic goal focus, and low transcendence goal focus; the transcendence striving profile is marked by a high level of emotional expressiveness, low agonistic goal focus, and high transcendence goal focus; and the dissipated striving profile is marked by a low level of expressed emotion and a lack of goal focus. Having replicated these profiles in different adolescent populations, we now can ask if they are related to perceptions of neighborhood disorder, and if they mediate associations between perceived neighborhood disorder and poor health outcomes.
Whereas most research on perceived neighborhood disorder and health has examined self-reported outcomes (Martin-Storey et al., 2012), we here investigate a physiologic outcome—ambulatory blood pressure. Social action theory predicts that the three motive profiles have different implications for future hypertension risk in adulthood, indexed in adolescence by relatively higher mean levels of ambulatory blood pressure during daily activities. Blood pressure in normotensive youth has been shown to predict risk of hypertension in early adulthood (Bao et al., 1995; Beckett et al., 1992; Nelson et al., 1992). Ambulatory pressure levels index risk more reliably than do clinic assessments (Kamarck & Lovallo, 2003; Pickering et al., 1985), correlate more strongly with indices of cardiovascular dysfunction, and are of greater prognostic value than casual readings made in the clinic (Perloff et al., 1983; White et al., 1989). The predicted associations between the three motive profiles and ambulatory blood pressure levels have been observed in two separate adolescent samples. Profile comparisons controlling for gender, race, and body mass disclosed that, although the blood pressures of the three profile groups did not differ when measured in the laboratory during quiet rest, youths with the agonistic profile exhibited significantly higher prevailing ambulatory blood pressure throughout the day, especially during social interactions that characterized most daily activities (Ewart et al., 2011; Ewart & Jorgensen, 2004). For example, the sizes of the mean difference between the diastolic pressure of the agonistic striving group during social interactions, and that of the other two profile groups, have ranged from one-half to two-thirds of an SD of resting blood pressure. These findings, replicated in two geographically distant urban populations, indicate that young people with the agonistic striving profile may be at significantly greater risk of developing hypertension in adulthood.
The second of the two studies (Ewart et al., 2011) revealed that the large blood pressure elevations during daily activities that mark the agonistic striving profile are not predicted by increased cardiovascular reactivity during the SCI, or during an anger recall task. Nor are they predicted by anger responses to these tasks, or by anger recorded on an electronic diary during normal activities. Implicit agonistic and transcendent motives assessed with the SCI thus predict large differences in risk that are not predicted by resting blood pressure levels, cardiovascular reactivity, or diverse indices of anger intensity or frequency. Implicit agonistic motives therefore represent a psychological mechanism through which perception of neighborhood disorder could increase risk independently of any effects that the stressful environment might be observed to exert on clinic blood pressure levels, cardiovascular reactivity, or anger. These findings suggest that the analysis of implicit motives may afford new insights into psychosocial factors that link neighborhood environments to illness outcomes.
The analysis of agonistic and transcendent motives also may facilitate more precise causal understanding of mediating psychological mechanisms. Most research on psychosocial factors that contribute to stress-related illness has focused on identifying “stress-prone” personality traits or affective dispositions, such as Type A behavior, hostility, anxiety, and depression. Yet these constructs and the scales used to measure them contain diverse mixtures of attitudinal, emotional, and behavioral components and often overlap with other constructs (Suls & Bunde, 2005). As a result, constructs and measures that predict health outcomes in one study may not do so in another. This has yielded a mixed and occasionally confusing picture of relationships between psychosocial factors and illness (Suls & Bunde, 2005). Even when significant associations are detected, the psychological factors usually are defined as personality traits, that is, as behavioral trends or averages. But averages are not causal mechanisms. Trait data can help predict who is at risk without disclosing the causal processes that account for the personality trait and the related illness vulnerability. By relating health outcomes to environmentally induced motives and power appraisals, social action theory offers a testable model of causal mechanisms that may explain the connection between perception of neighborhood disorder and increased cardiovascular risk.
How might the two proposed mechanisms—agonistic striving and self-appraisals of social subordination or powerlessness—operate in everyday settings? Are they experienced together or independently? A desire to control others can be related or unrelated to a self-appraisal of one’s social standing. For example, a self-appraised loss of status can trigger agonistic striving to assert one’s social worth (Keltner et al., 2003), but frequent experiences of social denigration may generate stable appraisals of low social power that induce passive withdrawal, foster chronic loneliness and undermine health (Hawkley & Cacioppo, 2007). A substantial body of evidence from research on social organization in humans and related primates suggests that ongoing interactions among group members tend to generate stable differences in social power (Boehm & Flack, 2010). Some individuals or subgroups regularly dominate (or are dominated by) other individuals or subgroups. The pervasiveness of stratified power differences among humans and other primates implies that perceptions of neighborhood disorder may cause some individuals to more frequently experience the stress of striving to control or dominate, whereas others more frequently experience the stress of being subordinated. Yet any individual, when interacting with others of higher or lower status, may experience agonistic stress in one social encounter or subordination stress in another. Thus, it would seem that agonistic motives and subordination appraisals may be interrelated or independent. Some individuals or groups may experience one form of stress more frequently than the other, but most experience both forms to varying degrees.
Given these possibilities, what patterns emerge when young people are exposed to disadvantaged and disordered living environments? Do subordination and agonistic striving evolve together, as different aspects of the same process? Or are they independent processes, with each forming its own unique pathway from environment to illness? Must preventive intervention target a single phenomenon, or different phenomena that often co-occur? We here examine new data from the second community study (Ewart et al., 2011, 2012) to discover if cross-sectional relationships among the variables suggest that the perception of neighborhood disorder might raise prevailing blood pressure levels in adolescents by generating agonistic striving and/or self-appraisals of social subordination. In the prior study we asked if patterns of anger arousal explain the impact of agonistic striving on cardiovascular responses to social stressors and prevailing blood pressure levels during daily activities. We now explore a different question by proposing that agonistic striving and subordination appraisals are associated with increased perception of neighborhood disorder, and that they independently predict (“mediate”) the effects of such perceptions on ambulatory blood pressure during daily activities in low- to middle-income Black and White youth. These analyses include novel, in vivo indices of social denigration and low social power that have not been reported previously. More important, this study is the first to assess denigration events and low social power appraisals together in the natural social environment, and to examine how they may combine with agonistic motives to increase blood pressure.
We used path models to test the hypothesized mediators. Given evidence that human societies tend to be characterized by power stratification—some individuals dominate, or are dominated, more regularly than others—our simplest (primary) hypothesis was that path modeling of cross-sectional associations would reveal two independent “associative” pathways linking perceptions of neighborhood disorder to increased ambulatory blood pressure: (a) an associative path through agonistic striving, and (b) an associative path through subordination. We hypothesized that, due to stable social stratification, these two paths would be shown in path models to be statistically independent.
However, other more complex relationships involving interactions among perceived neighborhood disorder, agonistic striving, and subordination processes are supported by social action theory and empirical evidence. We therefore tested several alternative, more complicated models to examine associative paths that are suggested by the following causal processes: (1) environmentally induced agonistic striving fosters subordination threats, which in turn elevate blood pressure; and (2) agonistic striving moderates (increases) the association between: (a) perception of neighborhood disorder and blood pressure, and (b) subordination and blood pressure. Finally, we compared the above models with an alternative model suggested by a different causal mechanism, namely, the notion that agonistic striving and subordination experiences are emergent by-products of negative emotional reactions to perceived neighborhood disorder (Gallo & Matthews, 2003; Suls & Bunde, 2005). Although we previously reported that agonistic striving and ambulatory blood pressure are unrelated to the intensity and frequency of anger, those analyses did not consider the possibility that negative affect related to perceived neighborhood disorder may increase ambulatory blood pressure, subordination appraisals, and agonistic striving.
Method
Participants
The sample included 167 ninth grade students from low to middle income neighborhoods who attended a large public high school in Syracuse, NY, that draws students from throughout the city. The mean age of the participants at the time they entered the study was 14.4 years (SD = 0.5 years). The sample was 54 % female; 41 % of participants identified their race as African American, 41 % as White, and 18 % as Native American, Latino, or Asian. The median household income reported by participants’ parents was $25,000; 50 % of the parents had graduated from high school. The research was part of Project Heart 5, a study of social-emotional stress and cardiovascular risk in low- to middle-income urban youth. Nearly two-thirds of eligible students took part in the project, which had been approved by the institutional review board of Syracuse University. Participants were informed in advance that the study was designed to yield information about factors affecting heart health in high school students. They were unaware of study hypotheses. Two previous studies in this sample (Ewart et al. 2011, 2012) investigated the role of anger regulation skills in moderating the impact of agonistic striving on ambulatory blood pressure; the present study investigates a very different set of questions, using new data on exposure to neighborhood disorder and subordination experiences that have not been analyzed or reported previously.
Assessment procedure
Participants were excused from classes to complete the assessment protocols, which were conducted in the Project Heart laboratory, located in a quiet office in the school. At the first session, participants’ height, weight, and waist circumference were measured and, after 10 min quiet rest, 3 blood pressure recordings were obtained at 2-min intervals with a Dinamap Vital Signs Monitor (Model #8100, Critikon, Tampa, FL, USA); the second and third reading were averaged to estimate initial resting blood pressure. Then they completed a stress questionnaire and the stress interview assessment of implicit agonistic motives. Approximately 2.5 months later, they returned to this lab to be fitted with an ambulatory blood pressure monitor and instructed in the electronic diary protocol for ecological momentary assessment. The blood pressure monitor (Oscar, SunTech Medical, Morrisville, NC, USA; Goodwin et al., 2007) was programmed to record blood pressure at 30-min intervals during the day and at 60-min intervals during nighttime sleep. During the 48-h recording period (2 days and two nights), participants recorded their activities, subordination appraisals, and emotions on the electronic diary using custom software (Palm Pilot zire22, Sunnyvale, CA, USA) which prompted them to answer a short series of questions each time blood pressure was recorded, after the reading was taken. The entries included their location, position, activity level, whether they had interacted with someone in the past 10 min, and negative affect. “Interacting” was defined as talking with someone in person, on the phone, or online. Every 3 h, the diary prompted them to complete a short survey about recent subordination (social denigration) experiences; a second set of subordination (low power) items was administered at bedtime. Participants visited the Project Heart lab at school the next morning to have the Oscar re-attached after their morning shower. They returned it at the end of the 48-h recording period. A detailed description of the recording procedure, data editing, and analysis is available elsewhere (Ewart et al., 2011).
Social competence interview
Implicit social control motives were assessed with the Social Competence Interview (SCI), which has been described in detail elsewhere (Ewart et al., 2002, 2007; Ewart & Jorgensen, 2004). Participants describe and re-experience a problem situation that causes them recurring personal distress; next, they pretend that they are a movie director making a documentary film about someone like themselves with a similar problem. They are asked to invent a desirable but realistic ending and plot line for the film, and then to indicate how they would apply the goals and strategies of the film narrative to their own personal problem. The film ending and plot indicate the participant’s implicit goal for resolving difficulties that frequently cause stress; the ability to vividly describe the situation, and to convey the emotions aroused, indexes the likelihood that the goal will induce stress in everyday life. The interviewers—White female graduate students in clinical psychology—were trained and supervised by Dr. Ewart, following procedures described elsewhere (Ewart & Suchday, 2002). Interviewers were not aware of the study hypotheses.
Social control motives
The three motive profiles associated with chronic stress (agonistic striving, transcendence striving, dissipated striving) are identified by rating (a) the goals that are implied in a participant’s SCI film narrative, and (b) the participant’s level of emotional expressiveness during the interview. Sample agonistic goals include trying to get others to be less demanding, or hostile, or critical; to be more friendly, cooperative, or sympathetic; and trying to get even with someone. Goal items were rated by trained SCI interviewers using 7-point scales (1 = Not at all to 7 = Very much). The 8-item Agonistic Striving scale had good internal reliability (Cronbach’s alpha = .86); 3-month temporal stability of SCI goal scales (Pearson r) in an earlier study ranged from r = .40 to r = .79 (Ewart et al., 2002). The agonistic striving, transcendence striving, and dissipated striving profile groups in the present study were identified through cluster analysis of participants’ striving and emotional expressiveness scores; the clustering procedure and profile group characteristics are described in a previous report (Ewart et al., 2011), which provides the profile scores for each group. The groups contained similar percentages of the study sample: agonistic, 30 %; transcendent, 36 %; and dissipated, 34 %; the composition of the groups did not differ with respect to gender or race, assessed by Chi square tests, or body mass index (BMI) or resting blood pressure assessed by ANOVA (all values of p > .35). In the present analyses, agonistic control motivation was defined categorically as membership in the Agonistic Striving profile group (1 = yes, 0 = no). Thus, an agonistic striving score of “1” in this study indicated that the SCI film narrative revealed strong agonistic motivation to influence or control others (agonistic striving profile group), whereas a score of “0” indicated that the narrative revealed little or no agonistic motivation (transcendence striving or dissipated striving profile group). Findings published previously show that the three profiles occur with similar frequency across differences of race, gender, and geographic region, and that the agonistic striving profile is associated with significantly higher blood pressure during daily activities relative to the transcendence striving and dissipated striving profiles (Ewart et al., 2011; Ewart & Jorgensen, 2004).
Perceived neighborhood disorder
Perceptions of neighborhood disorder were assessed with the 11-item Neighborhood Disorder subscale of the City Stress Inventory (Ewart & Suchday, 2002), administered at the first lab session. Neighborhood Disorder items (rated on 4-point scale of frequency, from 1 = Never to 4 = Often) include these events or conditions: ‘neighbors complain about crime,’ ‘a ‘crack house’ near my home,’ ‘strangers who are drunk or high near my home,’ ‘people harassed by police,’ ‘adults arguing loudly on street,’ ‘gang fight near my home,’ ‘drug dealing near my home,’ ‘cars speeding on my street,’ ‘someone I knew was arrested,’ and the number of ‘neighbors on food stamps’/‘vacant houses in my neighborhood.’ The Neighborhood Disorder scale, scored by summing the ratings (score range = 11–44), has acceptable reliability (alpha = .88; 1-year test–retest stability of r = .82), and is significantly correlated with objective indices of SES (e.g., neighborhood income, r = −.39, education, r = −.35; Ewart & Suchday, 2002).
Subordination
Subordination appraisals, recorded on electronic diaries, were assessed at two levels: (1) social denigration experiences (Sidanius & Pratto, 1999) when interacting with others reported at 3-h intervals throughout the day; and (2) resulting appraisals of low social power (Keltner et al., 2003) assessed at the end of the day, before bed. Ratings were made on 7-point Likert scales (1 = Not at all; 7 = Very much). Each scale contained 6 items, yielding summary scores ranging from 6 to 42). The Social Denigration Experiences scale asked participants to indicate how often during the preceding 3 h they had interacted with someone who ‘says mean things about you behind your back,’ ‘doesn’t like the way you look or dress,’ ‘believes untrue stories they heard about you,’ ‘thinks you can be pushed around,’ ‘doesn’t want you around,’ ‘thinks that they are better than you.’ The Low Social Power scale, completed immediately before going to bed, asked ‘When interacting with people at school and at home today, how often did you feel: ‘ignored,’ ‘self-conscious or embarrassed,’ ‘cautious or distant,’ ‘defensive—alone,’ ‘bossed around,’ ‘criticized or put down.’ Both the Social Denigration Experiences and Low Social Power scales, which were developed for this study (Ewart et al., 2006), exhibited good levels of internal validity (alphas of .92 and .86, respectively).
Obesity indices
Body mass was calculated as the ratio of weight to height squared (kg/m2). Central adiposity, which has been recommended as the best proxy for abdominal adiposity (NIH Expert Panel, 1998) was assessed using waist circumference, measured in centimeters at the level of the umbilicus.
Ambulatory blood pressure
Levels of ambulatory pressure were used to index the outcome variable, risk of developing hypertension in early adulthood. The prevailing level of blood pressure during social interactions, represented by the mean, was used to index an individual’s aggregate level of risk. This mean served as the dependent variable in tests of study hypotheses. Social interactions were our primary focus because they are hypothesized to activate mechanisms of agonistic striving and subordination, and because prior data showed that they occur with high frequency throughout the day.
Negative affect
Negative affect was assessed with single-item ratings of anger and sadness; these two affect domains were sampled due to their prominent association with cardiovascular disease risk (Suls & Bunde, 2005). Single-item ratings of each emotion were used to limit the response burden of repeated EMA surveys. Emotions were recorded on the electronic diary each time blood pressure was recorded (30-min intervals) during waking hours. Participants rated the degree to which they felt ‘angry-upset’ and ‘sad’ on 1-item 7-point scales (1 = Not at all, 7 = Very much). The correlation between self-reported levels of anger and sadness experienced during daily activities was r = .65, p < .0001. A participant’s mean Sadness ratings and mean Anger ratings were added to create a summary Negative Affect score (range from 2 to 14) for the mediation analyses reported here (these emotions also were examined separately in secondary analyses described below). Anxiety, a negative affect also associated with increased cardiovascular arousal and illness risk (Suls & Bunde, 2005), was not included in the EMA surveys due to our previously published finding (Ewart & Kolodner, 1994) that adolescents’ self-ratings of anxiety overlap extensively with their self-ratings of sadness—a finding reported also by other investigators (Kendall et al., 1992).
Analytic approach
The path analyses tested our primary hypothesis that agonistic striving and subordination stress form separate pathways by which perceptions of neighborhood disorder increase ambulatory blood pressure. The analyses also examined more complicated models in which subordination mediates the link between environmentally induced agonistic striving and blood pressure, agonistic striving moderates (magnifies) the cardiovascular effects of perceived neighborhood disorder and subordination, and agonistic striving and subordination stress are emergent by-products of negative emotional reactions to perceptions of a disordered neighborhood environment. The proposed mediator variables that exhibited statistically significant bivariate correlations with perception of neighborhood disorder and blood pressure were tested together in a multivariate path model to determine if the structure of interrelationships among the predictor, mediator, and dependent variables was consistent with the above hypotheses.
Our approach was to test first the bivariate associations between the study variables and the primary dependent variable, ambulatory blood pressure. Two variables included with obesity as potential covariates were sex and race, which often are associated with hypertension risk. Preliminary regression models then regressed blood pressure on the three potential covariates—sex, race, and obesity (BMI/Waist Circumference), followed by agonistic striving, subordination, and the interaction of each covariate with each of the two mediator variables. In these regressions, the main effects of race, sex, and all of the interactions between the covariates and the primary study variables, were nonsignificant. Thus, only obesity was retained as a covariate.
Path models were tested with Mplus version 5.1 (Muthen & Muthen, 2007) with a means and variance adjusted weighted least squares estimator (WLSMV) which is recommended for models that include both categorical and continuous variables. Chi square, comparative fit index (CFI), Tucker-Lewis fit index (TLI), root mean square error of approximation (RMSEA), and means and variance adjusted weighted root mean square residual (WRMR) were used to assess model fit. Indirect effects were tested using the product of coefficients technique with bias-corrected bootstrapping (based on 2,000 draws) and 95 % confidence intervals (MacKinnon et al., 2004; Preacher & Hayes, 2008; Preacher et al., 2007). All path models were initially tested as saturated models. Nonsignificant paths were sequentially dropped from the model in a step-wise approach based on theoretical expectations and prior research. Models were re-specified based on assessment of fit indices and significance of path coefficients.
Tests of hypothesized associative paths used ambulatory mean arterial pressure (MAP) during social interactions as the primary dependent variable. MAP was used to index risk given that it is likely to reflect the integrated effects of environmental influences on both myocardial and vascular mechanisms of blood pressure regulation that are believed to foster the development of sustained hypertension (Schwartz et al., 2003). Secondary analyses then tested the path model with ambulatory diastolic pressure and systolic pressure as the outcomes. Blood pressure during social interactions was the primary focus because the proposed motivational and subordination mechanisms are presumed to operate by altering daily social interactions and relationships.
The two forms of subordination, social denigration experiences and appraisals of low social power, were represented as separate variables in the path model because denigration represents a discrete appraisal of a social interaction event recorded shortly after the event occurs, whereas low social power represents a resultant global summary assessment of one’s ability to exercise social influence, or ‘power.’ Self-appraisals of low social power are the products of multiple denigration events that repeatedly occur over time (Keltner et al., 2003). We hypothesized that denigration events affect prevailing blood pressure levels by shaping global summary appraisals of low social power.
Agonistic striving was represented by a contrast variable which contrasts the agonistic profile group with the combined transcendence and dissipated profile groups in order to determine whether, relative to these two groups, agonistic striving (a) is induced by greater perceived neighborhood disorder, and (b) leads to higher ambulatory pressure.
Results
Measures of resting systolic and diastolic blood pressure, body mass, and waist circumference recorded during the initial assessment session yielded the following mean values: Systolic = 116.4 mmHg (SD = 14.8 mmHg), diastolic = 63.3 mmHg (SD = 8.9 mmHg), body mass index = 25.4 (SD = 6.1), and waist circumference = 83.1 cm (SD = 14.1 cm). EMA data showed that the mean number of ambulatory blood pressure readings during social interaction was 21.2 (SD = 12.6); the mean number of readings obtained when not interacting was 5.6 (SD = 6.6). The mean levels of systolic and diastolic pressure during social interactions were 127.8 mmHg (11.5 mmHg) and 72.8 mmHg (SD = 8.2 mmHg); corresponding means recorded when not interacting were 127.0 mm Hg (SD = 4.7 mmHg) and 71.1 mmHg (SD = 10.8 mmHg). The mean levels of the psychosocial predictor and mediator variables were: Perceived Neighborhood Disorder, 21.4 (SD = 6.7); Social Denigration, 13.6 (SD = 6.8); Low Social Power, 15.0 (SD = 6.3); Negative Affect, 2.8 (SD = 1.7). Cluster analysis of the SCI motive ratings produced the three predicted Motive Profile groups: Agonistic (30 %), Transcendent (36 %), and Dissipated (34 %). The group profiles were virtually identical to the group profiles we reported in a cluster analysis of data obtained in an earlier adolescent sample (Ewart & Jorgensen, 2004).
Preliminary analyses
Before testing the predicted mediational paths, we compared the motivational profile groups on the numbers of blood pressure readings recorded during the following activity categories, as reported on the electronic diaries: (a) Social Interaction (yes/no); and (b) Position/Activity Level (reclining, sitting, standing, walking/running).
Sixty-four percent of the blood pressure readings were accompanied by a diary entry indicating if a social interaction occurred within 10 min of the reading (yes/no); this value was nearly identical across the three groups (63–65 %). Inspection of the diary activity categories revealed that 78 % of the EMA entries during the 48-h monitoring period reported current social interactions. GLM analyses disclosed that the numbers of blood pressure readings, and the numbers of readings in each activity category, did not differ among the three profile groups; values of t(166) ranged from 0.09 (p = .99), to 1.80 (p = .20). Nor were the number of readings in any activity category correlated with any of the hypothesized mediating variables (all values of p > .19).
Bivariate correlations among the candidate variables (Table 1) indicated that erceived Neighborhood Disorder showed the predicted positive association with ambulatory pressure during social interactions as indexed by MAP (correlations with systolic and diastolic pressure, respectively, were r = .15, p < .05, and r = .13, p < .08). Agonistic Striving and Low Social Power, however, although correlated with Neighborhood Disorder and blood pressure, did not correlate significantly with each other; this finding was consistent with the primary hypothesis that they represent independent associative pathways. Bivariate correlations also failed to support two alternative mediational hypotheses: (1) that subordination mediates the impact of agonistic striving, or (2) that Negative Affect mediates the impact of perceived Neighborhood Disorder on Agonistic Striving, Subordination, and blood pressure. Agonistic Striving was not significantly correlated with the Subordination indices or Negative Affect. Neither index of obesity was correlated with any other variables apart from perceived Neighborhood Disorder and blood pressure.
Table 1.
Bivariate correlations among model variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Neighborhood disorder | |||||||
| 2. Mean arterial pressure | .16* | ||||||
| 3. Agonistic striving | .18* | .23** | |||||
| 4. Social denigration | .20** | .14 | .02 | ||||
| 5. Low social power | .16* | .17* | .11 | .58*** | |||
| 6. Negative affect | .21** | −.02 | .07 | .41*** | .52*** | ||
| 7. Body mass index | .19** | .20** | .06 | .07 | −.06 | −.07 | |
| 8. Waist circumference | .17** | .27*** | .13 | .14 | −.01 | .03 | .90**** |
p < .05;
p < .01;
p < .001;
p < .0001
The pattern of correlations suggested that perception of Neighborhood Disorder and subordination appraisals may induce negative emotions, but that Negative Affect does not mediate the relationship between perceived Neighborhood Disorder and elevated blood pressure. The same result was obtained when the two subcomponents of Negative Affect (anger, sadness) were correlated separately with MAP (and also with systolic and diastolic pressure). Hence, negative affect was not included in the path models; the hypothesis that observed associations between perceptions of Neighborhood Disorder, Agonistic Striving, Subordination, and obesity are byproducts of negative emotional reactions to environmental stress was not tested. Instead, the path models tested the primary hypothesis that Agonistic Striving and Subordination represent separate associative paths, as well as the two moderation hypotheses that Agonistic Striving magnifies the association between blood pressure and: (a) perceived Neighborhood Disorder, and (b) Subordination. These models included obesity to control for the association of obesity with ambulatory blood pressure, as well as to determine if the proportion of environment-blood pressure variance associated with Agonistic Striving and Subordination matched the proportion of variance associated with obesity, a cardiovascular risk factor correlated with increased exposure to adverse, disadvantaged living conditions (Goldbacher et al., 2005). BMI and Waist Circumference indices of obesity were highly correlated, and exhibited the same pattern of correlations with the other study variables. We therefore used both obesity indices in the path models, testing each model first with one and then with the other.
Explanatory models
The first path model tested the primary hypothesis that Agonistic Striving and subordination appraisal mechanisms may independently mediate the association between perceived neighborhood disorder and higher blood pressure during daily social interactions. The model included obesity as a separate associative path. This approach enabled us to test simultaneously the separate indirect effects of Neighborhood Disorder on blood pressure as mediated by Agonistic Striving, Subordination, and obesity. It also made it possible to compare the proportion of the relationship between Neighborhood Disorder and blood pressure that was associated with obesity and the two mediators.
The model included hypothesized direct effects of perceived Neighborhood Disorder, Agonistic Striving, Social Denigration, Low Social Power, and BMI/Waist Circumference on MAP; as well as direct effects of Neighborhood Disorder on Agonistic Striving, Social Denigration, and Low Social Power. We also tested whether the effect of Neighborhood Disorder on MAP is better characterized by indirect effects on MAP through: (1) Agonistic Striving, (2) Subordination, and (3) Body Mass/Waist Circumference. Initial models included all possible paths among variables (i.e., a saturated model). In the first step, non-significant paths between obesity and Denigration, Low Social Power, and Agonistic Striving were deleted; the resultant model had acceptable model fit across indices, X2(3) = 4.68, p = .20, comparative fit index (CFI) = .99, Tucker-Lewis fit index (TLI) = .94, root mean square error of approximation (RMSEA) = 0.06, means and variance adjusted weighted root mean square residual (WRMR) = 0.29. In the second step, nonsignificant paths between Agonistic Striving and Denigration, Low Social Power were removed; the resultant model had excellent fit across all indices, X2 (5) = 6.50, p = .26, CFI = .99, TLI = .97, RMSEA = 0.03, WRMR = 0.35. Finally, the remaining two nonsignificant paths between Low Social Power and Neighborhood Disorder, and MAP and Denigration were removed; the resultant model had excellent fit across all indices, X2 (7) = 7.53, p = .38, CFI = .99, TLI = .99, RMSEA = 0.02, WRMR = 0.38. This final model was chosen based on theory and parsimony.
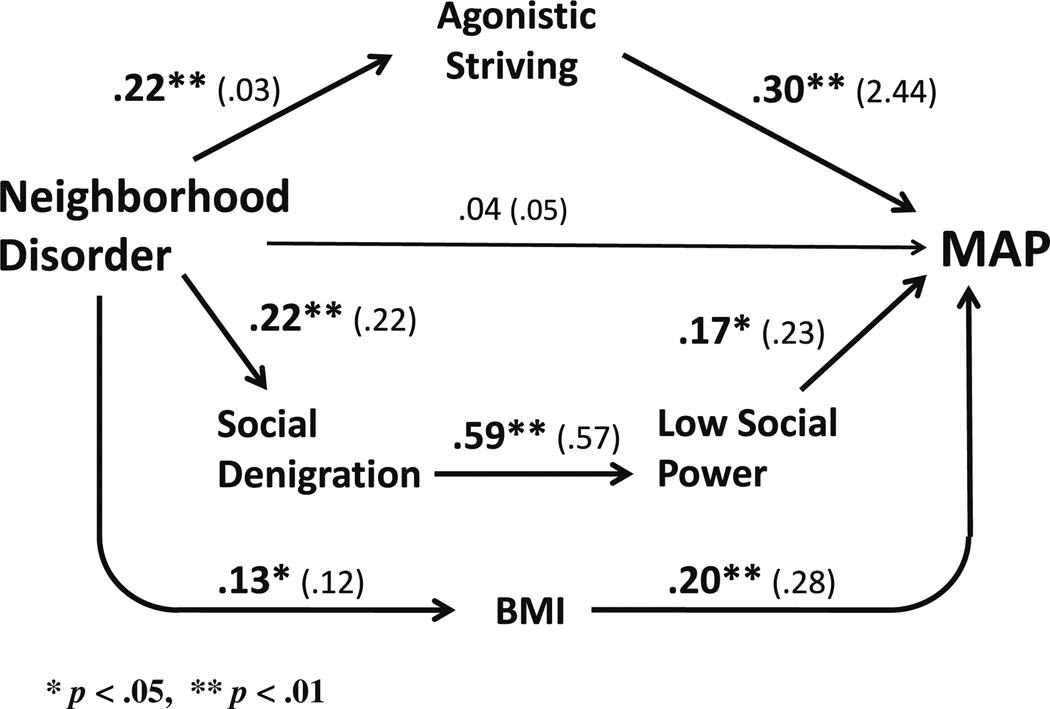
The final model is shown in Fig. 1, which provides the standardized and unstandardized path coefficients. Together, Neighborhood Disorder, obesity, and the two mediators accounted for 17 % of the variation in MAP during daily social encounters. Individually, the separate path coefficients generally support the hypothesized model. Due to the significant path between BMI and perceived Neighborhood Disorder, this path was retained; thus, statistically, the other two theoretically predicted paths controlled for the covariation between Neighborhood Disorder, BMI, and MAP. The direct relationship between perceived Neighborhood Disorder and blood pressure is not significant when Agonistic Striving, Subordination, and BMI are included in the model. Results thus are consistent with the hypothesis that Agonistic Striving, Subordination, and obesity independently mediate the relationship between perception of Neighborhood Disorder and blood pressure. Perceived Neighborhood Disorder predicts a higher level of Agonistic Striving, more frequent experiences of subordination, and increased obesity. Higher MAP during social interaction was associated with Agonistic Striving, Subordination, and higher BMI. Tests of indirect effects (Table 2) indicate that 73 % of the association between perceived Neighborhood Disorder and MAP is accounted for by the two hypothesized mediational pathways and obesity: 42 % by Agonistic Striving, 15 % by Subordination, and 16 % by BMI. The same model with Waist Circumference substituted for body mass yielded very similar results.
Figure 1.
Causal model of psychological paths from neighborhood disorder to high ambulatory blood pressure showing standardized path coefficients (unstandardized coefficients in parentheses). BMI body mass index, MAP mean arterial pressure. *p < .05, **p < .01
Table 2.
Association of neighborhood disorder (ND) with ambulatory mean arterial pressure (MAP) mediated by agonistic striving, subordination (SDE, LSP), and body mass index
| Effect | Indirecta | (95 %CI) |
Directa | Total | % mediated |
|---|---|---|---|---|---|
| ND on MAP through | |||||
| Agonistic striving | 0.08* | .02, .19 | 0.05 | 0.20* | 42 |
| Subordination (SDE, LSP) | 0.03* | .01, .08 | 0.05 | 0.20* | 15 |
| Body mass index | 0.03* | .01, .08 | 0.05 | 0.20* | 16 |
| Total indirect effects | 0.14* | .07, .27 | 0.05 | 0.20* | 73 |
ND neighborhood disorder, MAP mean arterial pressure, SDE social denigration experiences, LSP low social power
p < .05
All estimates are unstandardized path coefficients. Confidence intervals (CI) represent results from 2000 bootstrap draws
Next, two additional sets of path models were performed to test the alternative hypotheses that Agonistic Striving moderates the blood pressure effects of (a) perception of Neighborhood Disorder, or (b) Subordination. Alternative models considered (1) subordination paths as influenced by: (a) indirect paths arising from Agonistic Striving, and (b) moderated by Agonistic Striving; (2) whether Agonistic Striving moderated the effect of perceived Neighborhood Disorder on blood pressure; and (3) whether Agonistic Striving and Subordination were influenced by negative emotions. Nonsignificant paths between Agonistic Striving and Subordination paths indicated that alternative models considering indirect paths between Subordination and Agonistic Striving were not possible. For the model which examined Agonistic Striving as a moderator of the effect of Low Social Power on blood pressure, the interaction term was nonsignificant and model fit indices were well below acceptable levels on all indices, X2 (11) = 91.55, p = .00, CFI = .67, TLI = .41, RMSEA = 0.17, WRMR = 0.99. For the model which examined Agonistic Striving as a moderator of the relationship between perceived Neighborhood Disorder and blood pressure, the interaction term was again nonsignificant despite excellent model fit, X2 (10) = 8.18, p = .61, CFI = 1.00, TLI = 1.00, RMSEA = 0.00, WRMR = 0.44.
Finally, two secondary sets of path analyses were performed to determine if the model (Fig. 1) that predicted MAP during social interactions also predicted diastolic and systolic pressure. In the model for diastolic pressure, the indirect paths through Agonistic Striving and Subordination remained significant, b = .07 (95 % CI = .02, .18, p < .05), b = .03 (95 % CI = .01, .08, p < .05), respectively; the indirect path through BMI was not significant, b = .02 (95 % CI = .00, .06, p = .10), For systolic pressure, the indirect paths through Agonistic Striving and BMI were significant, b = .11 (95 % CI = .03, .25, p < .05), b = .06 (95 % CI = .01, .14, p < .05), respectively; the indirect path for Subordination was not significant, b = .03 (95 % CI = .00, .09, p < .07). All models exhibited adequate fit across all indices.
Further, although we had no a priori hypothesis that sex or race differences would alter the strength of the associative paths, two sets of multiple group analyses were estimated to test the invariance of relationships among study variables as a function of sex and race. Tests for sex and race differences among the paths were nonsignificant (all values of p > .21, for sex, and > .17, for race). The model shown in Fig. 1, without sex or race, yielded the best degree of fit across all indices. Finally, despite the fact that the bivariate relationships between Negative Affect and MAP (and systolic/diastolic pressure) were not significant, we estimated the causal model (Fig. 1) with Negative Affect included as one of the mediators. Results indicated that the indirect path through Negative Affect was not significant (b = −.03, CI = .00, −.10, p = .15).
Discussion
This study is the first to test predictions from social action theory that perceived neighborhood disorder increases adolescents’ future hypertension risk by inducing agonistic motives and perceptions of social subordination, which raise blood pressure levels during normal activities. We tested the hypothesis that agonistic striving and subordination appraisals are associated with increased perception of neighborhood disorder, and that both mediating variables are independently associated with higher ambulatory blood pressure. Path models were used to evaluate the predicted associations. Our basic (primary) hypothesis, guided by research on power stratification in human and other primate societies, was that the path models would support two independent associative pathways linking perceptions of neighborhood disorder with higher blood pressure: (a) a path through agonistic striving, and (b) a path through subordination. We also tested more complex models suggested by social action theory, namely, that subordination appraisals may mediate the link between agonistic striving and blood pressure, and that agonistic striving and subordination may moderate the blood pressure effects of perceived neighborhood disorder.
Path analyses supported our primary hypothesis that agonistic striving and subordination stress represent separate associative pathways by which perceived neighborhood disorder may increase future hypertension risk indexed by higher ambulatory blood pressure during daily activities. Indeed, results suggest that agonistic motives and subordination appraisals may independently explain large portions of the association between a stressful neighborhood environment and higher prevailing blood pressure levels. Although the size of the correlation between perceived neighborhood disorder and mean arterial pressure may appear relatively modest, the fact that this association already is detectable in adolescence, together with the finding that Agonistic Striving and Subordination experiences during everyday social interactions accounted for as much as 57 % of this association, suggests that the cumulative long-term impact on future cardiovascular health of persistent agonistic motives and recurring daily subordination events may be considerable (Bao et al., 1995). This seems especially likely considering the high frequency of social interactions throughout the day; for example, 78 % of the EMA survey entries reported current social interactions.
Tests of more complicated models in which Subordination mediated the link between environmentally induced Agonistic Striving and blood pressure, as well as tests of moderator effects, failed to yield statistically significant results. The reasons for the null findings are unclear. It is possible that more frequent intensive longitudinal assessment is needed to detect the hypothesized causal event sequences. A larger sample, as well as more intensive within-person measurement, may be required to generate the statistical power needed to detect interaction (moderator) effects. It also is possible that the nature of the relationships among living environments, agonistic striving, and cardiovascular risk indices, varies with a person’s age and level of social-emotional development. Initial findings from a recent study of 233 Black and White adults support this possibility; cluster analysis yielded the same agonistic, transcendent, and dissipated profiles, as well as the same correlations with ambulatory blood pressure and heart rate, that we have reported in adolescents. Perceived neighborhood disorder and subordination threats in this sample were associated with higher ambulatory heart rate levels during social interactions; these associations were magnified (moderated) by agonistic striving (Elder et al., 2012).
The study of adolescents reported here also sought to compare the path models of social-motivational and subordination mediators and moderators with a model suggested by the very different hypothesis that agonistic striving and subordination stress are emergent byproducts of negative emotional reactions to perceived neighborhood disorder. This alternative model, however, was not supported by the data. Further, although an earlier paper from this sample reported that persons with the agonistic striving profile exhibited increased anger and sadness during the SCI, as well as more intense anger during an anger-recall task (Ewart et al., 2011), the present analyses did not detect a significant correlation between Agonistic Striving and the Negative Affect indices. This lack of association was found even though Negative Affect was measured throughout the day via EMA, and despite secondary analyses that examined anger and sadness as separate emotions. Higher EMA ratings of Negative Affect were associated with increased perception of Neighborhood Disorder, experiences of Social Denigration, and appraisals of Low Social Power, but not with the Agonistic Striving profile, or prevailing blood pressure levels.
Thus, present data are compatible with the hypothesis that stressful neighborhood environments foster subordination appraisals that evoke anger and sadness. Yet the data do not suggest that negative emotions generate sustained blood pressure elevations. In fact, the data suggest another possibility, namely, that negative emotions and elevated blood pressure both are generated by experiences of social denigration and low social power (subordination). This hypothesis seems worthy of further research.
Several secondary analyses were performed to test the primary path model (Fig. 1) separately with diastolic and systolic blood pressure as outcomes. These analyses showed that results for diastolic pressure were the same as those for MAP; this may be unsurprising, considering that the computation of MAP weights DBP values more heavily than SBP values. However, the model for systolic pressure was slightly different. It indicated that the association between perceived neighborhood disorder and ambulatory systolic pressure is mediated by agonistic striving but not by subordination. One attractive (albeit speculative) explanation for this difference involves the well-established finding that different types of behavioral stressors tend to elicit different patterns of diastolic and systolic responding. Diastolic blood pressure levels are highly sensitive to changes in vascular resistance associated with increased vigilance to possible threats, or “threat appraisals,” whereas systolic blood pressure levels are highly sensitive to myocardial changes that are associated with active behavioral coping, or “challenge appraisals” (Tomaka et al., 1993, 1997). Present findings are compatible with the possibility that perceptions of denigration and low social power readily evoke vigilant threat appraisals and high diastolic pressure, but less readily evoke challenge appraisals and high systolic pressure. Agonistic striving, on the other hand, tends to generate both forms of appraisal, considering that agonistic striving often combines the challenge of seeking to exert influence (high systolic pressure), with the threat of having to vigilantly detect and be ready to deter unwanted counter-responses (high diastolic pressure).
Limitations and future directions
The present analysis has several limitations. Despite the fact that the variables in the path models were assessed at different time points, the study design is not capable of testing causal mediation by repeatedly assessing changes in the relevant variables over a long time period or, better yet, by manipulating hypothesized psychological mediators to produce variations in blood pressure. Even so, alternate hypotheses—such as the notion that blood pressure influences perceived neighborhood disorder or the agonistic striving and subordination mediators, or that agonistic control motives or subordination appraisals cause adverse neighborhood events—do not seem plausible (this is not to deny that subjective factors might affect reports of the publically observable neighborhood incidents and conditions that are assessed by the CSI). It also should be noted that the narrow age range of participants in the present study does not permit us to determine if the hypothesized mediator variables might exhibit different relationships to blood pressure or other cardiovascular risk indices at different points in the life span. It is possible, as we suggest above, that agonistic motivation or subordination experiences moderate the impact of neighborhood or occupational settings in adulthood, when individuals may enjoy somewhat wider latitude in selecting or shaping their daily environments. And negative emotions may influence cardiovascular risk indices differently in children or in the elderly than during the period of adolescence that characterized participants in the present sample (Kop & Cohen, 2001). Negative Affect in the present study was defined in terms of self-rated anger and sadness, reflecting the widespread emphasis on these emotions in cardiovascular health research. Anxiety, although also prominently associated with cardiovascular risk indices (Suls & Bunde, 2005), was not specifically assessed in this study due to evidence that, in adolescents, self-ratings of anxiety are highly correlated with self-ratings of sadness (Ewart & Kolodner, 1994), and due to concern to limit the response burden imposed by the EMA protocol. It is possible, however, that anxiety ratings might have mediated the association between perceptions of neighborhood disorder and ambulatory blood pressure levels. This possibility merits further study. Finally, as we have noted previously, the levels of Negative Affect assessed by EMA were comparatively low, a finding that is consistent with evidence that most people report feeling relatively happy most of the time (Kagan, 2007). EMA recording over a much longer time interval may be needed to identify patterns of affect that correlate with agonistic motives, subordination experiences, and prevailing blood pressure levels.
Despite these considerations, the present study design has important strengths. This study is unusual in linking perceptions of neighborhood disorder to an important physiologic risk factor—high ambulatory blood pressure—as opposed to a self-reported health outcome (Martin-Storey et al., 2012). The research is unique also in including objective assessments of implicit control motives that are not readily accessible to self-report (Ewart et al., 2012), as well as multiple in vivo EMA measures of subordination appraisals and negative emotions. Multiple assessments of proposed mediators bolster confidence in the study’s central findings. These results suggest promising directions for interventions to promote cardiovascular health. Agonistic motives and subordination appraisal mechanisms represent independent causal pathways, with qualitatively different sets of causal antecedents, behaviors, and outcomes. Agonistic striving is induced by challenges to interpersonal influence and control that foster chronic interpersonal conflict, harsh parenting, and abuse (Granic & Patterson, 2006). Subordination appraisals induced by social denigration, rejection, and mistreatment lower perceived self-worth and may foster social withdrawal and isolation (Hawkley & Cacioppo, 2007). Each psychological path thus yields different implications for clinical intervention and social policy. Mediation of neighborhood stress through agonistic striving suggests the importance of programs to enhance social-relational competence and to bolster family ties threatened by burdens of poverty and unemployment. Mediation by subordination appraisals supports the need for interventions to prevent or mitigate discrimination, stigmatization, and hostile treatment (e.g., bullying) in schools, workplaces, and communities. Given that these paths appear to contribute separately to future hypertension risk, and considering that some persons or groups are apt to be affected more by one mechanism than by the other, interventions to target both may be needed.
Acknowledgments
This research was supported by grant R01-HL75555 from the National Heart, Lung, and Blood Institute, awarded to Craig K. Ewart. We thank Mindi Ditmar and Michelle Hallahan who served as project coordinators, and Nina Stoeckel, Rachel Herman, and Erin Sullivan for assistance in data collection and coding. We also thank Jill Stewart for serving as liaison with Henninger High School. We thank Randall S. Jorgensen and Aesoon Park who commented on earlier drafts of the manuscript.
References
- Aldarondo E, Sugarman DB. Risk marker analysis of the cessation and persistence of wife assault. Journal of Consulting and Clinical Psychology. 1996;64:1010–1019. doi: 10.1037//0022-006x.64.5.1010. [DOI] [PubMed] [Google Scholar]
- Bao W, Threefoot SA, Srinivasan SR, Berenson GS. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: The Bogalusa heart study. American Journal of Hypertension. 1995;8:657–665. doi: 10.1016/0895-7061(95)00116-7. [DOI] [PubMed] [Google Scholar]
- Beatty DL, Hall MH, Kamarck TW, Buysse DJ, Owens JF, Reis SE, et al. Unfair treatment is associated with poor sleep in African American and Caucasian adults: Pittsburgh SleepSCORE project. Health Psychology. 2011;30:351–359. doi: 10.1037/a0022976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beatty DL, Matthews KA. Unfair treatment and trait anger in relation to nighttime blood pressure in African American and White adolescents. Psychosomatic Medicine. 2009;71:813–820. doi: 10.1097/PSY.0b013e3181b3b6f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckett LA, Rosner B, Roche AF, Guo S. Serial changes in blood pressure from adolescence into adulthood. American Journal of Epidemiolgy. 1992;135:1166–1177. doi: 10.1093/oxfordjournals.aje.a116217. [DOI] [PubMed] [Google Scholar]
- Boehm C, Flack JC. The emergence of simple and complex power structures through social niche construction. In: Guinote A, Vescio TK, editors. The social psychology of power. New York: Guilford; 2010. pp. 46–86. [Google Scholar]
- Bullock HE, Lott B. Social class and power. In: Guinote A, Vescio TK, editors. The social psychology of power. New York: Guilford Press; 2010. [Google Scholar]
- Conger RD, Elder GH. Families in troubled times. New York: Aldine de Gruyter; 1994. [Google Scholar]
- Custers R, Aarts H. The unconscious will: How the pursuit of goals operates outside of conscious awareness. Science. 2010;329:47–50. doi: 10.1126/science.1188595. [DOI] [PubMed] [Google Scholar]
- Deng S, Lopez V, Roosa MW, Ryu E, Burrell GL, Tein J, et al. Family processes mediating the relationship of neighborhood disadvantage to early adolescent internalizing problems. The Journal of Early Adolescence. 2006;26:206–231. [Google Scholar]
- Dickerson SS, Gable SL, Irwin MR, Aziz N, Kemeny ME. Social-evaluative threat and proinflammatory cytokine regulation: An experimental laboratory investigation. Psychological Science. 2009;20:1237–1244. doi: 10.1111/j.1467-9280.2009.02437.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger NI, Lieberman MD, Williams KD. Does rejection hurt: An fMRI study of social exclusion. Science. 2003;302:290–292. doi: 10.1126/science.1089134. [DOI] [PubMed] [Google Scholar]
- Elder GH, Parekh M, Schoolman JH, Fitzgerald S, Ewart CK. Society of Behavioral Medicine: 33rd Annual Meeting and Scientific Sessions. New Orleans, LA: 2012. Do social control motives moderate the impact of ethnic discrimination and denigration on cardiovascular disease risk? [Google Scholar]
- Ewart CK. Nonshared environments and heart disease risk: Concepts and data for a model of coronary-prone behavior. In: Hetherington E, Reiss D, Plomin R, editors. The separate social worlds of siblings. Hillsdale, NJ: Erlbaum; 1994. pp. 175–203. [Google Scholar]
- Ewart CK. Agonistic striving, emotion regulation, and hypertension risk. In: Wright RA, Gendolla GHE, editors. Motivational perspectives on cardiovascular responses. Washington, DC: American Psychological Association; 2011. pp. 267–286. [Google Scholar]
- Ewart CK, Ditmar MM, Suchday S, Sonnega JR. Manual for the social competence interview. Syracuse University; 2007. [Google Scholar]
- Ewart CK, Elder GJ, Sliwinski M, Smyth JM, Jorgensen RS. Do agonistic motives matter more than anger? Three studies of cardiovascular risk in adolescents. Health Psychology. 2011;30:510–534. doi: 10.1037/a0023127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewart CK, Elder GH, Smyth JM. How implicit motives and everyday self-regulatory abilities shape cardiovascular risk in youth. Annals of Behavioral Medicine. 2012;43:286–298. doi: 10.1007/s12160-011-9336-3. [DOI] [PubMed] [Google Scholar]
- Ewart CK, Jorgensen RS. Agonistic interpersonal striving: Social-cognitive mechanism of cardiovascular risk in youth? Health Psychology. 2004;23:75–85. doi: 10.1037/0278-6133.23.1.75. [DOI] [PubMed] [Google Scholar]
- Ewart CK, Jorgensen RS, Schroder KE, Suchday S, Sherwood A. Vigilance to a persisting personal threat: Unmasking cardiovascular consequences in adolescents with the Social Competence Interview. Psychophysiology. 2004;41:799–804. doi: 10.1111/j.1469-8986.2004.00199.x. [DOI] [PubMed] [Google Scholar]
- Ewart CK, Jorgensen RS, Suchday S, Chen E, Matthews KA. Measuring stress resilience and coping in vulnerable youth: The social competence interview. Psychological Assessment. 2002;14:339–352. doi: 10.1037//1040-3590.14.3.339. [DOI] [PubMed] [Google Scholar]
- Ewart CK, Kadziolka M, Ditmar M, Herman R. American Psychosomatic Society: Sixty-Fourth Annual Meeting. Denver, CO: 2006. Power threats linked to agonistic striving and high blood pressure in urban youth. [Google Scholar]
- Ewart CK, Kolodner KB. Negative affect, gender, and expressive style predict ambulatory blood pressure in adolescents. Journal of Personality and Social Psychology. 1994;66:596–605. doi: 10.1037//0022-3514.66.3.596. [DOI] [PubMed] [Google Scholar]
- Ewart CK, Suchday S. Discovering how urban poverty and violence affect health: Development and validation of a neighborhood stress index. Health Psychology. 2002;21:254–262. doi: 10.1037//0278-6133.21.3.254. [DOI] [PubMed] [Google Scholar]
- Ewart CK, Taylor CB, Kraemer CH, Agras WS. High blood pressure and marital discord: Not being nasty matters more than being nice. Health Psychology. 1991;10:155–163. doi: 10.1037//0278-6133.10.3.155. [DOI] [PubMed] [Google Scholar]
- Feldman PJ, Steptoe A. How neighborhoods and physical functioning are related: The roles of neighborhood and socioeconomic status, perceived neighborhood strain, and individual health risk factors. Annals of Behavioral Medicine. 2004;27:91–99. doi: 10.1207/s15324796abm2702_3. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- Goldbacher EM, Matthews KA, Salomon K. Central adiposity is associated with cardiovascular reactivity to stress in adolescents. Health Psychology. 2005;24:375–384. doi: 10.1037/0278-6133.24.4.375. [DOI] [PubMed] [Google Scholar]
- Goodwin J, Bilous M, Winship S, Finn P, Jones SC. Validation of the Oscar 2 oscillometric 24-h ambulatory blood pressure monitor according to the British hypertension society protocol. Blood Pressure Monitoring. 2007;12:113–117. doi: 10.1097/MBP.0b013e3280acab1b. [DOI] [PubMed] [Google Scholar]
- Granic I, Patterson GR. Toward a comprehensive model of anti-social development: A dynamic systems approach. Psychological Review. 2006;113:101–131. doi: 10.1037/0033-295X.113.1.101. [DOI] [PubMed] [Google Scholar]
- Guinote A, Vescio TK, editors. The social psychology of power. New York: Guilford Press; 2010. [Google Scholar]
- Hawkley LC, Cacioppo JT. Aging and loneliness: Downhill quickly? Current Directions in Psychological Science. 2007;16:187–191. [Google Scholar]
- Kagan J. What is emotion? History, measures, meanings. New Haven, CT: Yale University Press; 2007. [Google Scholar]
- Kamarck TW, Lovallo WR. Cardiovascular reactivity to psychological challenge: Conceptual and measurement considerations. Psychosomatic Medicine. 2003;65:9–21. doi: 10.1097/01.psy.0000030390.34416.3e. [DOI] [PubMed] [Google Scholar]
- Keltner DG, Gruenfeld DH, Anderson C. Power, approach, and inhibition. Psychological Review. 2003;110:265–284. doi: 10.1037/0033-295x.110.2.265. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Kortlander E, Chansky TE, Brady EU. Comorbidity of anxiety and depression in youth: Treatment implications. Journal of Consulting and Clinical Psychology. 1992;60:869–880. doi: 10.1037/0022-006X.60.6.869. [DOI] [PubMed] [Google Scholar]
- Kop W, Cohen N. Psychological risk factors and immune system involvement in cardiovascular disease. In: Ader R, Felten D, Cohen N, editors. Psychoneuroimmunology. 3rd ed. New York: Academic; 2001. pp. 525–544. [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin-Storey A, Temcheff CE, Ruttle PL, Serbin LA, Stack DM, Schwartzman AE, et al. Perception of neighborhood disorder and health service usage in a Canadian sample. Annals of Behavioral Medicine. 2012;43:162–172. doi: 10.1007/s12160-011-9310-0. [DOI] [PubMed] [Google Scholar]
- McClelland DC, Koestner R, Weinberger J. How do self-attributed and implicit motives differ? Psychological Review. 1989;96:690–702. [Google Scholar]
- Miller G, Chen E, Cole SW. Health psychology: Developing biologically plausible models linking the social world and physical health. Annual Review of Psychology. 2009;60:501–524. doi: 10.1146/annurev.psych.60.110707.163551. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus user’s guide. Los Angeles: Muthen & Muthen; 2007. [Google Scholar]
- National Heart, Lung, and Blood Institute, editor. NIH Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Bethesda, MD: 1998. [Google Scholar]
- Nelson MJ, Ragland DR, Syme L. Longitudinal prediction of adult blood pressure from juvenile blood pressure levels. American Journal of Epidemiology. 1992;136:633–645. doi: 10.1093/oxfordjournals.aje.a116543. [DOI] [PubMed] [Google Scholar]
- O’Neil R, Parke RD, McDowell DJ. Objective and subjective features of children’s neighborhoods: Relations to parental regulatory strategies and children’s social competence. Applied Developmental Psychology. 2001;22:135–155. [Google Scholar]
- Perkins DD, Meeks JW, Taylor RB. The physical environment of street blocks and resident perceptions of crime and disorder: Implications for theory and measurement. Journal of Environmental Psychology. 1992;12:21–34. [Google Scholar]
- Perkins DD, Taylor RB. Ecological assessments of community disorder: Their relationship to fear of crime and theoretical implications. American Journal of Community Psychology. 1996;24:63–107. doi: 10.1007/BF02511883. [DOI] [PubMed] [Google Scholar]
- Perloff D, Sokolow M, Cowan R. The prognostic value of ambulatory blood pressure. Journal of the American Medical Association. 1983;249:2792–2798. [PubMed] [Google Scholar]
- Pickering TG, Harshfield GA, Devereux RB, Laragh JH. What is the role of ambulatory blood pressure monitoring in the management of hypertensive patients? Hypertension. 1985;7:171–177. doi: 10.1161/01.hyp.7.2.171. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Assessing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Sapolsky RM. The influence of social hierarchy on primate health. Science. 2005;308:648–652. doi: 10.1126/science.1106477. [DOI] [PubMed] [Google Scholar]
- Schwartz AR, Gerin W, Davidson KW, Pickering TG, Brosschot JF, Thayer JF, et al. Toward a causal model of cardiovascular responses to stress and the development of cardiovascular disease. Psychosomatic Medicine. 2003;65:22–35. doi: 10.1097/01.psy.0000046075.79922.61. [DOI] [PubMed] [Google Scholar]
- Sidanius J, Pratto F. Social dominance. New York: Cambridge University Press; 1999. [Google Scholar]
- Smith TW, Uchino BN, Berg CA, Florsheim P, Pearce G, Hawkins M, et al. Hostile personality traits and coronary artery calcification in middle-aged and older married couples: Different effects for self-reports versus spouse ratings. Psychosomatic Medicine. 2007;69:441–448. doi: 10.1097/PSY.0b013e3180600a65. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems, and associations with socioeconomic status and health. Annals of Behavioral Medicine. 2001;23:177–185. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- Suls J, Bunde J. Anger, anxiety, and depression as risk factors for cardiovascular disease: The problems and implications of overlapping affective dispositions. Psychological Bulletin. 2005;131:260–300. doi: 10.1037/0033-2909.131.2.260. [DOI] [PubMed] [Google Scholar]
- Tomaka J, Blascovich J, Kelsey RM, Leiten CL. Subjective, physiological, and behavioral effects of threat and challenge appraisal. Journal of Personality and Social Psychology. 1993;65:248–260. [Google Scholar]
- Tomaka J, Blascovich J, Kibler J, Ernst JM. Cognitive and physiological antecedents of threat and challenge appraisal. Journal of Personality and Social Psychology. 1997;73:63–72. doi: 10.1037//0022-3514.73.1.63. [DOI] [PubMed] [Google Scholar]
- Weden MM, Carpiano RM, Robert SA. Subjective and objective neighborhood characteristics and adult health. Social Science and Medicine. 2008;66:1256–1270. doi: 10.1016/j.socscimed.2007.11.041. [DOI] [PubMed] [Google Scholar]
- Wen M, Hawkley LC, Cacioppo JT. Objective and perceived neighborhood environment, individual SES and psychosocial factors, and self-rated health: An analysis of older adults in Cook County, Illinois. Social Science and Medicine. 2006;63:2575–2590. doi: 10.1016/j.socscimed.2006.06.025. [DOI] [PubMed] [Google Scholar]
- White WB, Schulman P, MCabe EJ, Dey M. Average daily blood pressure, not office blood pressure, determines cardiac function in patients with hypertension. Journal of the American Medical Association. 1989;261:873–877. [PubMed] [Google Scholar]