Abstract
Background The mental health functioning of military spouses and intimate partners prior to the combat deployments of their loved ones is poorly studied.
Aims Whereas service members and veterans often receive healthcare directly from the military or the Department of Veterans Affairs, family members may be more likely to present in family care settings. An understanding of mental health problems commonly occurring in this population is therefore important.
Method National Guard soldiers and their spouses or cohabitating partners (n = 223 couples) were surveyed about mental health symptoms, social functioning and mental health service utilisation one to two months prior to a combat deployment to Afghanistan.
Results Screening rates for partner post-traumatic stress disorder, depression, alcohol problems and social impairment were 2.4, 15.3, 3.7 and 10.7%, respectively, and were significantly higher for partners than soldiers with regards to depression and social impairment. The majority of partners screening positive for psychiatric distress did not report utilising mental health services or military support services (i.e. family readiness groups). Clinical implications are discussed.
Keywords: combat deployment, deployment cycle, depression, family well-being, PTSD
Introduction
The wars of the 21st century pose a major challenge not just to the nation's military service members, but also to their families. The duration of the wars in Iraq (Operations Iraqi Freedom (OIF) and New Dawn or (OND)) and Afghanistan (Operation Enduring Freedom (OEF)), along with the nature of operations and the often repeated deployments, are all sources of great stress for military service members and military families. Although a great deal of research has documented potential mental health problems among military service members following the wars in Iraq and Afghanistan, including post-traumatic stress disorder (PTSD), depression, other anxiety disorders and substance abuse,1,2 much less is known about the well-being and mental health of their family members. Nonetheless, clinical observation and preliminary research findings suggest that family members of deployed military service members, particularly spouses, may be at risk for elevated distress before, during and after the combat deployments of their loved ones.3,4 The development of systematic knowledge about the needs and service utilisation of military family members in the context of combat deployments may be particularly salient for primary care settings, where many family members may present for care with potentially unrecognised concerns.
The Emotional Cycle of Deployment Model3 and later elaborations4 posit that unique stressors present before, during and after a combat deployment can lead to distress and mental health problems in military family members, especially spouses or intimate partners. During a service member's deployment, research finds increased rates of mental health service utilisation and mental health diagnoses for the spouses of deployed service members,5 elevated rates of internalising and externalising symptoms among children of combat-deployed personnel6 and increased rates of child maltreatment at home.7 After combat deployment, long-term studies of spouses of combat Vietnam veterans, often 20 or more years after the war, have shown that spouses of veterans with PTSD are at higher risk for symptoms of many mental health diagnoses, including depression, anxiety, somatisation and PTSD.7–10 This distress is often viewed as resulting from either the stress of caring for sometimes very impaired veterans or secondary traumatic stress.11–13
The Emotional Cycle of Deployment Model also suggests that prior to a military deployment, emotional distress may arise as intimate partners are simultaneously anticipating the absence of their soldier, denying that it will occur and trying to prepare for the departure.3 Unfortunately, in contrast to the above research on the functioning of spouses/partners during and after combat deployments, there has been less of a focus on intimate partner well-being in the months and weeks prior to combat deployments. Although studies of soldier mental health prior to combat deployments have found low rates of reported distress,1,14 much less is known about intimate partner well-being prior to deployment. To the best of our knowledge, no prior research has examined rates or predictors of distress among intimate partners prior to deployment, limiting our understanding of the need for predeployment mental health and support services that may emerge in primary care visits. Although the military does offer family readiness groups that provide support and information to family members while soldiers are preparing for and undergoing deployments, it is important to identify levels of clinical distress and mental health service utilisation in this population so that the adequacy of these services can be evaluated.
Two potentially important predictors of partners' distress prior to deployment include service members' prior combat deployments and service members' pre-deployment level of psychiatric distress. Partners of service members who have already been through a combat deployment may be more confident and less distressed because of their experience of successfully navigating the stresses of a deployment in the past. However, if prior combat deployments have been especially trying, partners may show elevated rates of distress as they anticipate another long and painful separation with similar stressors. Soldiers who have been through prior combat deployments do tend to report slightly higher rates of distress prior to subsequent deployments.14 Findings of elevated distress post deployment among partners of veterans with PTSD8–10 also suggest that partners' distress may be correlated with soldiers' own mental health symptoms.
The present study begins to address gaps in the literature through a cross-sectional survey of intimate partners and National Guard soldiers who were due to be deployed to a combat mission in Afghanistan within 1–2 months of the survey. For both partners and soldiers, rates of depression, PTSD, problem drinking and impaired social functioning were assessed using standardised self-report surveys. Rates of distress among partners and rates of distress among soldiers were examined separately, and soldiers and partners who had prior experience with combat deployment were compared with those without such experience. The relationship between soldier and partner psychiatric distress was also examined. Finally, we examined self-reports of mental health service utilisation and family readiness group attendance among those partners reporting mental health problems. The hypotheses were that: (1) rates of depression and alcohol abuse would be elevated among the partners of deploying soldiers, (2) soldiers and partners who had been through prior deployments to OEF/OIF would report higher rates of psychiatric distress, and (3) soldier psychiatric distress would be related to partner distress.
Methods
Procedures and participants
The participants for this report were National Guard soldiers who were mobilised to be deployed to Afghanistan, and their intimate partners. Approximately 1 month prior to deployment, soldiers responded to a mailed survey in which they completed measures of distress and preparedness (to be detailed in another report) and also were asked to nominate their spouses or cohabitating partners to participate by providing their partner's name and address. Intimate partners who were nominated were sent a survey by mail that included questionnaires about current overall well-being, stressors, concerns about the deployment and psychiatric symptoms. Soldier and spouse participants were sent $10 as part of their initial mailing, and those spouses who did not respond within 2 weeks were sent a reminder postcard and two additional mailings. The study protocol was approved by the Institutional Review Board (IRB) of the Minneapolis VA Healthcare System and the University of Minnesota. All participants were provided with all elements of informed consent in a covering letter, which also informed them that their responses were entirely confidential and would not be shared with military personnel or command. A waiver of written documentation of informed consent was granted by the IRB.
Surveys were sent to 2401 deploying soldiers, of whom 623 responded (a response rate of 26%). Of the 623 responding soldiers, 388 were either married or living with a partner, and 290 of those nominated their spouse or partner for participation. Of 290 spouse/partners nominated by soldiers, 223 (77%) responded to the partner survey. Of the 223 soldier and partner pairs who had responded to the surveys, 216 (96.9%) had complete data on all outcome variables and were included in the present analyses. Soldiers were mostly male (n = 206, 95%), married (n = 194, 90%) and Caucasian (n = 206, 95%), with another 2% who reported Hispanic American ethnicity, 1% Native American ethnicity and 2% reporting other ethnicities. In terms of education, 16% (n = 35) had completed a high school diploma or GED, 53% had completed some college coursework but not a 4-year degree (n = 116), 24% had a 4-year degree (n = 51) and 7% had completed a graduate degree (n = 14). Most soldiers were enlisted rank (n = 175, 81%), with 39 officers (18%) and 3 warrant officers (1%). Spouses were mostly female (n = 206, 95%) and Caucasian (n = 202, 94%) with others reporting Hispanic American (2%), Native American (1%), Asian American (1%) or other ethnicities (1%). Education among spouses/partners included high school diploma or GED (n = 25, 12%), some college without a 4-year degree for 60% (n = 130), 4-year degree (n = 52, 24%) and graduate degrees (n = 9, 4%). Most spouses/partners (n = 157, 73%) reported working outside the home. Mean age for soldiers was 34.34 years (range 20–34, SD = 8.68) and for partners was 33.55 years (range 18–60, SD = 9.55).
Measures
PTSD Checklist – Civilian Version (PCL)15
The PCL is a widely used 17-item self-report measure that assesses each of the 17 symptoms of PTSD, with established internal consistency and test–retest reliability and concurrent and criterion validity based on its relationship with other self-report scales and clinical diagnoses of PTSD. Participants were considered as screening positive for PTSD if their total score was above 49 and they endorsed 1, re-experiencing; 3, avoidance; and 2, hyperarousal symptoms as being at least ‘moderately’ present.1
Patient Health Questionnaire-8 (PHQ-8)16
Depression was assessed with the PHQ-8, a selfreport measure that has shown strong correlations with other self-report measures of depression as well as indices of functional impairment. A score of 10 or higher on the PHQ-8 has been shown to predict clinical diagnoses of depression.17
Alcohol Use Disorders Identification Test (AUDIT)18
The AUDIT is a 10-item self-report measure that assesses quantity and frequency of alcohol use as well as consequences of problematic alcohol use. Its reliability and validity have been established in numerous clinical and community populations.18 Scores from 8 to 15 on the AUDIT are considered to indicate risky levels of drinking, while those exceeding 16 suggest harmful levels of drinking.19
Social Functioning Scale (SFS)20
The SFS is an 8-item measure of social functioning and impairment that has been shown to have good test–retest and internal consistency reliability, to correlate with clinician ratings and to discriminate between varying levels of psychopathology.20 A score of 10 or more indicates deficits in social functioning.
Mental Health Services
Partners were also asked if they had received any ‘mental health or support services’ including individual therapy (‘one-to-one counseling for personal concerns’), psychiatric medications (‘medications, such as antidepressants’) and if they had attended family readiness groups since learning of their soldier's impending deployment.
Analyses
Rates of distress were established by examining the numbers of soldiers and partners exceeding cut-offs for probable problems on measures of PTSD, depression, alcohol problems and social functioning. Descriptive analyses revealed significant positive skew and heteroskedasticity for scales measuring PTSD, depression, alcohol use and social functioning problems. Consequently, scale scores for PTSD and depression were subjected to a reflected inverse transformation and scores on the AUDIT and SFQ were subjected to a square root transformation in order to normalise distributions while retaining directionality prior to parametric analyses. Independent t-tests were used for comparing soldiers and partners who had or had not had previous OEF/OIF deployments and paired t-tests were used for comparing levels of distress between soldiers and partners. Rates of positive screens for mental disorders were compared across prior deployment statuses and roles (soldier vs. partner) using 2 × 2 chi square analyses with Fisher's exact test. Pearson bivariate correlations were also computed between all outcome variables within soldiers and partners, as well as between soldiers and partners.
Results
Rates of distress for soldiers and partners, both in terms of numbers screening positive for problems and raw (untransformed) scale scores, are listed in Table 1. Partners reported significantly more depression, PTSD symptoms and social impairment than soldiers, whereas soldiers reported higher levels of problematic alcohol use. Differences in rates of screening positive were also significant for problems with depression and alcohol use but not for social functioning (P-values for Fisher's exact test for 2 × 2 contingency tables were 0.0007, 0.0001 and 0.1683, respectively). Table 2 lists levels of self-reported mental health symptoms based on prior OEF/OIF deployment status. As shown, soldiers had slightly higher levels of PTSD if they had been previously deployed, but did not show differences in other mental health symptoms. There were no differences on any of the variables assessed between partners of soldiers previously deployed and partners of soldiers preparing for their first deployment to OEF/OIF.
Table 1.
Rates of mental health problems and distress for spouses and soldiers
| Spouse/partner (n = 216) | Soldier (n = 216) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | % Positive | Mean | SD | Median | % Positive | Mean | SD | Median | Comparison1 | P |
| PTSD2 | 2.4 (n = 5) | 26.64 | 9.33 | 25 | 2.8 (n = 6) | 24.26 | 9.60 | 21 | 3.78 | < 0.001 |
| Depression2 | 15.3 (n = 33) | 4.65 | 4.41 | 3 | 5.1 (n = 11) | 2.60 | 4.02 | 1 | 6.77 | < 0.001 |
| Alcohol Use3 | Risky: 3.2 (n = 7) Harmful: 0.5 (n = 1) |
2.57 | 2.36 | 2 | Risky: 10.2 (n = 22) Harmful: 5.6 (n = 12) |
4.91 | 4.29 | 4 | −9.60 | < 0.001 |
| Social Impairment3 | 10.7 (n = 23) | 5.43 | 3.109 | 15 | 6.5 (n = 14) | 4.23 | 3.25 | 4 | 14.88 | < 0.001 |
Raw mean and median values are displayed. % positive = per cent screening positive on each measure.
1 Paired groups t-test comparing continuous scores with df = 215.
2 Reflected inverse transform used in t-test.
3 Square root transform used in t-test.
Table 2.
Soldier and partner distress by prior deployment status
| No prior deployment (n = 105) | Prior deployment (n = 111) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | % Positive | Mean | SD | Median | % Positive | Mean | SD | Median | Comparison1 | P |
| Soldier | ||||||||||
| PTSD2 | 1 (n = 1) | 22.75 | 7.90 | 20 | 5 (n = 5) | 25.69 | 10.82 | 22 | 2.19 | 0.029 |
| Depression2 | 4 (n = 4) | 2.83 | 4.49 | 1 | 7 (n = 7) | 2.39 | 3.52 | 1 | −0.33 | 0.746 |
| Alcohol Use3 | Risky: 9 (n = 10) Harmful: 4 (n = 4) |
5.20 | 4.83 | 4 | Risky: 11 (n = 12) Harmful: 8 (n = 8) |
4.63 | 3.71 | 4 | 0.65 | 0.515 |
| Social Impairment3 | 8 (n = 18) | 4.17 | 12.98 | 13 | 15 (n = 6) | 4.34 | 3.52 | 4 | −0.65 | 0.517 |
| Partner PTSD2 | 2 (n = 2) | 27.17 | 9.50 | 26 | 3 (n = 3) | 26.13 | 9.18 | 23 | −0.82 | 0.416 |
| Depression2 | 14 (n = 15) | 4.87 | 4.21 | 4 | 17 (n = 18) | 4.43 | 4.61 | 3 | −1.14 | 0.256 |
| Alcohol Use3 | Risky: 3 (n = 3) Harmful: 1 (n = 1) |
2.66 | 2.37 | 2 | Risky: 4 (n = 4) Harmful: 0 (n = 0) |
2.48 | 2.36 | 2 | 0.53 | 0.596 |
| Social Impairment3 | 10 (n = 11) | 15.52 | 3.07 | 5 | 11 (n = 12) | 5.33 | 3.11 | 5 | 0.52 | 0.604 |
Raw mean and median values are displayed. % Positive = per cent screening positive on each measure.
1 Independent groups t-test comparing continuous scores with df = 214.
2 Reflected inverse transform used for t-test.
3 Square root transform used for t-test.
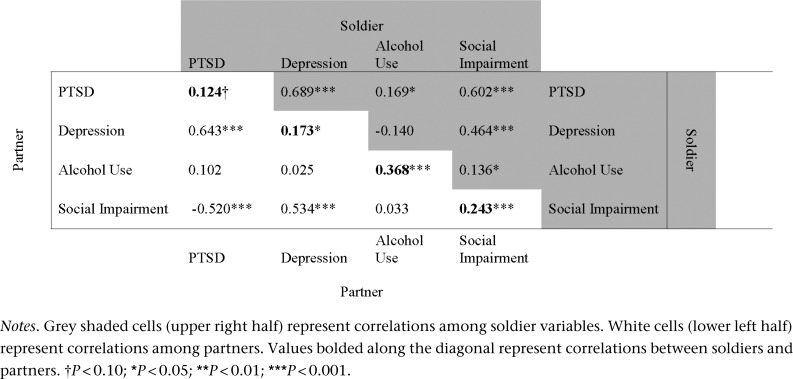
Figure 1 lists the correlations between distress variables among soldiers and partners, and between soldiers and partners. Correlations among soldiers are shown in the upper right half of the table, and correlations of these variables among partners are listed in the lower left half; correlations between soldier and partner levels of distress are given in bold along the diagonal. There was substantial intercorrelation between symptoms of PTSD, depression and social impairment for both soldiers and partners, and smaller correlations between these variables and problematic alcohol use. Soldier and partner ratings of depression, social impairment and alcohol use were significantly related.
Figure 1.
Correlations between psychiatric symptoms for and between soldiers and partners
Among the 40 spouses who reported any mental health concern (depression, PTSD or risky/harmful alcohol use): 6 (15%) reported that they had received individual therapy since learning of the deployment, 11 (28%) reported taking psychiatric medications in that time and 15 (38%) reported attending family readiness groups. Fisher's exact tests for differences in proportion found that those screening positive for mental health problems were more likely to receive psychiatric medication (P < 0.001) but not more likely to receive individual therapy (P = 0.237) or attend family readiness groups (P = 0.161).
Discussion
Current findings suggest that intimate partners are at significant risk for mental health difficulties immediately prior to the combat deployments of soldiers. While rates of soldier mental health distress were relatively low, and below levels reported in general epidemiological surveys [e.g. the National Comorbidity Study Replication (NCS-R)],21 intimate partners reported significantly more symptoms of depression, PTSD and social impairment. The screening rates of depression for partners were considerably higher than 12-month prevalence rates of depressive disorders reported in epidemiological studies (e.g. 1.5–6.7% in the NCS-R).22 In addition, the positive correlation between partner depression symptoms and social functioning problems, suggest that these problems, along with accompanying stressors, pose a possible challenge to social functioning. Although partners did report a statistically significant increase in PTSD symptoms compared with soldiers, this is likely due to the high correlation between PTSD and depression, which is further supported by the lack of a difference in positive screens for PTSD between soldiers and partners. In contrast to intimate partners, soldiers reported low levels of distress on PTSD, depression and social impairment, but higher levels of problematic alcohol use, which is common in this population prior to deployment.23 These findings support assertions made by the Emotional Cycle of Deployment Model3 and suggest that clinical services may be important and indicated for this population prior to combat deployments. Unfortunately, we also found low rates of treatment utilisation among those intimate partners screening positive for mental health problems, indicating a need for greater assessment, outreach and provision of mental health services for these individuals.
Contrary to expectations, there were no differences among intimate partners of soldiers facing their first deployment to those with a history of prior deployments. Additionally, although soldiers with previous deployments reported greater rates of symptoms of PTSD, these differences were small, and differences in distress on other indicators were non-significant. Perhaps couples with a deployment history have more confidence in their ability to successfully manage stressors associated with deployment and have established a support network that is readily mobilised. In addition, previously deployed soldiers experiencing the greatest distress may have left the military or been deemed ineligible for redeployment. Additionally, couples who experienced the greatest distress and mental health problems following previous deployments may no longer be together. Finally, it may be that the type of experiences from prior deployments, rather than the presence or absence of a prior deployment, that matters most. For example, deployment experiences marked by heavy combat exposure or followed by readjustment difficulties (i.e. relationship discord) and mental health problems (i.e. PTSD) may leave both soldiers and their intimate partners vulnerable to distress prior to future deployments. The finding that soldier and partner levels of distress were related supports this assertion.
Moderate associations were found between partners' and soldiers' levels of distress. This is consistent with the larger literature supporting reciprocal relationships between distress experienced among romantic partners24 and greater rates of distress and caregiver strain among the intimate partners of individuals with both mental11 and physical health problems.25 These associations may be due to individuals at risk for mental health problems selecting partners who are also at risk or to one individual's distress causing the other's distress indirectly through greater relationship discord and elevated caregiver burden (i.e. selective mating or emotional contagion).24
Ultimately, further research is needed to replicate these findings and examine how prior deployments impact individual and couple functioning over the course of the deployment cycle. Causal statements are precluded by our cross-sectional findings, and the long-term implications of elevated partner distress prior to deployment remain unclear. Longitudinal data are needed to determine the degree to which partners' individual distress symptoms persist during and after the combat deployment and also to examine whether partner distress predicts soldiers' well-being both during deployments and when soldiers return. It is possible that, as suggested by some models, distress will decrease as partners adjust to soldiers' absence.3 It is also possible, however, that the distress will only increase, as worries about soldier well-being, difficulties managing home demands and so forth mount.4
Conclusions
Most partners of deploying National Guard soldiers, like the soldiers themselves, appear to be resilient to the stresses of the anticipated deployment and are not reporting clinically significant depression, anxiety or alcohol use. However, an important minority do report increased distress, especially in terms of depression. The level of distress in National Guard spouses is related to the distress level of the soldiers themselves. In a primary care setting, it is especially important to note that the majority of National Guard spouses screening positive for mental health problems are not receiving psychiatric services or attending military family readiness groups. Thus, there may be a need for increased assessment and outreach efforts in primary care clinics, with appropriate referrals being made for psychiatric and psychotherapeutic services with this population. Supporting National Guard families before, during and after combat deployments may be an important way of supporting the soldiers themselves, and primary care settings are likely to be on the front lines of this particular battle.
ACKNOWLEDGEMENTS
This material is based upon work supported by the Department of Veterans Affairs. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
ETHICAL APPROVAL
This research was approved by the Institutional Review Boards of the University of Minnesota and the Minneapolis VA Healthcare System. In addition, it was approved by the Minnesota National Guard command. All participants voluntarily consented to the study after it was explained to them.
FUNDING
This research was funded by a small project grant from the VA HSR&D Center for Chronic Disease Outcomes Research (CCDOR) in Minneapolis, MN.
CONFLICTS OF INTEREST
The authors attest that they have no conflicts of interest regarding the topic and content of this manuscript.
Contributor Information
Christopher R Erbes, Staff Psychologist, Center for Chronic Disease Outcomes Research.
Laura A Meis, Staff Psychologist, Center for Chronic Disease Outcomes Research.
Melissa A Polusny, Staff Psychologist, Center for Chronic Disease Outcomes Research.
Paul A Arbisi, Staff Psychologist, University of Minnesota Medical School and Department of Psychology, Minneapolis, USA.
REFERENCES
- 1.Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine 2004;351:13–22 [DOI] [PubMed] [Google Scholar]
- 2.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. Journal of the American Medical Association 2006;95:1023–32 [DOI] [PubMed] [Google Scholar]
- 3.Logan KV. The emotional cycle of deployment. US Naval Institute Proceedings 1987;113:43–47 [Google Scholar]
- 4.Peebles-Kleiger MJ, Kleiger JH. Re-integration stress for Desert Storm families: wartime deployments and family trauma. Journal of Traumatic Stress 1994;7:173–94 [DOI] [PubMed] [Google Scholar]
- 5.Mansfield AJ, Kaufman JS, Marshall SW, et al. Deployment and the use of mental health services among U.S. Army wives. New England Journal of Medicine 2010;362:101–9 [DOI] [PubMed] [Google Scholar]
- 6.Flake EM, Davis BE, Johnson PL, et al. The psychosocial effects of deployment on military children. Journal of Developmental and Behavioral Pediatrics 2009;30:271–8 [DOI] [PubMed] [Google Scholar]
- 7.Gibbs DA, Martin SL, Kupper LL, et al. Child maltreatment in enlisted soldiers' families during combat-related deployments. Journal of the American Medical Association 2007;298:528–35 [DOI] [PubMed] [Google Scholar]
- 8.Jordan BK, Marmar CR, Fairbank JA, et al. Problems in families of male Vietnam veterans with post-traumatic stress disorder. Journal of Consulting and Clinical Psychology 1992;60:916–26 [DOI] [PubMed] [Google Scholar]
- 9.Mikulincer M, Florian V, Solomon Z. Marital intimacy, family support, and secondary traumatization: a study of wives of veterans with combat stress reaction. Anxiety Stress and Coping 1995;8:203–13 [Google Scholar]
- 10.Sherman MD, Sautter F, Lyons JA, et al. Mental health needs of cohabiting partners of Vietnam veterans with combat-related PTSD. Psychiatric Services 2005;56:1150–2 [DOI] [PubMed] [Google Scholar]
- 11.Calhoun PS, Beckham JC, Bosworth HB. Caregiver burden and psychological distress in partners of veterans with chronic posttraumatic stress disorder. Journal of Traumatic Stress 2002;15:205–12 [DOI] [PubMed] [Google Scholar]
- 12.Goff BSN, Smith DB. Systemic traumatic stress: the couple adaptation to traumatic stress model. Journal of Marital and Family Therapy 2005;31:145–57 [DOI] [PubMed] [Google Scholar]
- 13.Hayes J, Wakefield B, Andresen EM, et al. Identification of domains and measures for assessment battery to examine well-being of spouses of OIF/OEF veterans with PTSD. Journal of Rehabilitation Research and Development 2011;47:825–40 [DOI] [PubMed] [Google Scholar]
- 14.Polusny MA, Erbes CR, Arbisi PA, et al. Impact of prior OEF/OIF combat duty on mental health in a pre-deployment cohort of National Guard Soldiers. Military Medicine 2009;174:1–6 [DOI] [PubMed] [Google Scholar]
- 15.Weathers FW, Litz BT, Herman DS, et al. The PTSD Checklist: reliability, validity, and diagnostic utility. Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies, 1993 [Google Scholar]
- 16.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine 2001;16:606–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatric Annals 2002;32:509–15 [Google Scholar]
- 18.Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction 1993;88:791–804 [DOI] [PubMed] [Google Scholar]
- 19.Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test (AUDIT): a review of recent research. Alcoholism: Clinical and Experimental Research 2002;26:272–9 [PubMed] [Google Scholar]
- 20.Tyrer P, Nur U, Crawford M, et al. The Social Functioning Questionnaire: a rapid and robust measure of perceived functioning. International Journal of Social Psychiatry 2005;51:265–75 [PubMed] [Google Scholar]
- 21.Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 2005;62:617–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kessler RC, Berglund P, Demler O, et al. (2003) The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). Journal of the American Medical Association 2003;289:3095–105 [DOI] [PubMed] [Google Scholar]
- 23.Ferrier-Auerbach AG, Kehle SM, et al. Predictors of alcohol use prior to deployment in National Guard soldiers. Addictive Behaviors 2009;34:625–31 [DOI] [PubMed] [Google Scholar]
- 24.Meyler D, Stimpson JP, Peek MK. Health concordance within couples: a systematic review. Social Science and Medicine 2007;64:2297–310 [DOI] [PubMed] [Google Scholar]
- 25.Marsh NV, Kersel DA, Havel JH, et al. Caregiver burden at 1 year following severe traumatic brain injury. Brain Injury 1998;12:1045–59 [DOI] [PubMed] [Google Scholar]