ABSTRACT
A novel betacoronavirus, human coronavirus (HCoV-EMC), has recently been detected in humans with severe respiratory disease. Further characterization of HCoV-EMC suggests that this virus is different from severe acute respiratory syndrome coronavirus (SARS-CoV) because it is able to replicate in multiple mammalian cell lines and it does not use angiotensin-converting enzyme 2 as a receptor to achieve infection. Additional research is urgently needed to better understand the pathogenicity and tissue tropism of this virus in humans. In their recent study published in mBio, Kindler et al. shed some light on these important topics (E. Kindler, H. R. Jónsdóttir, M. Muth, O. J. Hamming, R. Hartmann, R. Rodriguez, R. Geffers, R. A. Fouchier, C. Drosten, M. A. Müller, R. Dijkman, and V. Thiel, mBio 4[1]:e00611-12, 2013). These authors report the use of differentiated pseudostratified human primary airway epithelial cells, an in vitro model with high physiological relevance to the human airway epithelium, to characterize the cellular tropism of HCoV-EMC. More importantly, the authors demonstrate the potential use of type I and type III interferons (IFNs) to control viral infection.
Commentary
In late 2002, severe acute respiratory syndrome coronavirus (SARS-CoV) crossed the species barrier from animals to humans. SARS first struck in Guangdong Province, China, and was officially recognized by the World Health Organization (WHO) in February 2003. After its introduction into human populations in Hong Kong in February 2003, the virus spread across the globe within weeks. A number of superspreading events occurred in several health care settings during the epidemic. When SARS was declared to have been contained (5 July 2003), there were 8,098 confirmed SARS cases, and 774 of these patients died from the disease. After this catastrophic event, one of the most frequently asked questions was whether SARS would come back.
Ten years after the introduction of SARS, yet another novel coronavirus (NCoV, or HCoV-EMC hereafter) jumped from animals to humans (1, 2). At the time of writing, there are 17 confirmed human cases, including 11 deaths. Recent findings related to this novel virus are alarming. The virus can readily infect cell lines from multiple hosts, including humans, swine, monkeys, and bats, suggesting that it might have a relatively weak species barrier. In addition, many of these human cases/clusters are not epidemiologically linked. The first detected case dates back to April 2012 in the Middle East. It is not known whether there is a low level of circulation of this novel coronavirus in asymptomatic human carriers or if there is an animal reservoir that allows for multiple introductions of HCoV-EMC into humans. While the transmission route (or routes) from animals to humans is not yet identified, a recent report of three human cases from a family cluster in the United Kingdom indicates that this virus is transmissible between humans.
CHARACTERIZATION OF HCoV-EMC IN PRIMARY HUMAN RESPIRATORY EPITHELIAL CELL CULTURE
Since the first discovery of HCoV-EMC as the etiological agent of this novel severe respiratory disease (1, 2), researchers have used various strategies to understand virus entry and its replication capability in mammalian cell lines (3, 4). In the absence of autopsy reports of patients who died from HCoV-EMC, our understanding of virus tropism and pathogenesis in humans is inadequate. Kindler et al. (5) describe the efficient infection and replication of HCoV-EMC in differentiated human primary airway epithelial (HAE) cell cultures in vitro. This model was used to culture other human coronaviruses such as HCoV-OC43 and HCoV-NL63 (6). This well-characterized primary culture system exhibits high physiological relevance, reflecting the anatomy of the human conducting airway (7), and allows better understanding of the cellular tropism of this newly emerged virus.
FIG 1 .
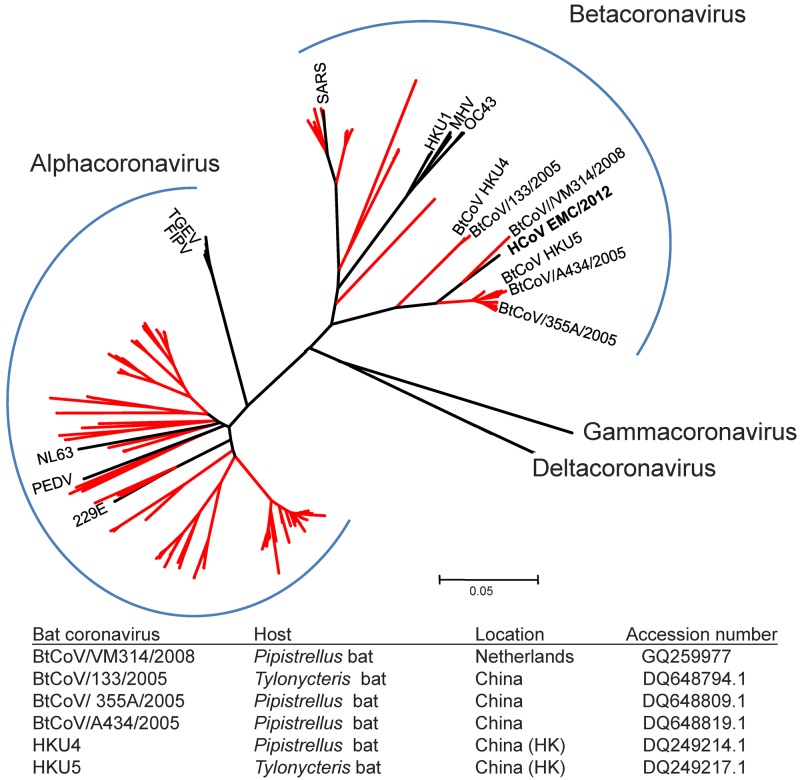
Phylogenetic analysis of partial RdRp sequences (306 nucleotides [nt]) of bat and other representative coronaviruses. HCoV-EMC is in bold. Branches representing bat coronavirus sequences are in red. All sequences were retrieved from the Taxonomy Browser of NCBI (http://www.ncbi.nlm.nih.gov/Taxonomy/Browser/wwwtax.cgi?mode=Undef&id=11118&lvl=3&keep=1&srchmode=1&unlock). The tree was generated by using the neighbor-joining method in MEGA5 (http://www.megasoftware.net/). Details of bat coronaviruses that are genetically related to HCoV-EMC are as shown.
Kindler et al. report that HCoV-EMC has faster replication kinetics than SARS-CoV in HAE cells (5). SARS-CoV has a mean incubation period of about 5 days in humans. This relatively “long” incubation period allowed the identification and isolation of SARS patients before they became highly infectious during the SARS epidemic. If HCoV-EMC has a very efficient replication rate in the upper human respiratory tract, the potential use of quarantine and isolation policy to contain a possible epidemic would be extremely limited.
In terms of cellular tropism, Kindler et al. are the first to show the cellular preference of HCoV-EMC for human non-ciliated bronchial epithelial cells. So far, susceptibilities of the human pseudostratified bronchial epithelial culture to coronaviruses causing the common cold (e.g., HCoV-229E, HCoV-OC43, HCoV-NL63) (6) and to SARS-CoV are comparable to that observed after HCoV-EMC infection. Interestingly, these human coronaviruses seem to have different cell specificities; non-ciliated cells are infected by HCoV-229E and HCoV-EMC, while ciliated cells are more prone to infections by HCoV-OC43, HCoV-NL63, and SARS-CoV. Nevertheless, this finding alone is not sufficient to explain their differential pathogenicities in humans. As acute pneumonia is one of the key presentations in HCoV-EMC infection in humans, the characterization of HCoV-EMC in tissues from lower respiratory tracts such as alveolar epithelial cells or alveolar macrophages might provide a more comprehensive picture of this novel disease.
The unusual severity of HCoV-EMC in humans, combined with its high fatality rate, is reminiscent of the clinical presentation of the SARS outbreak in 2003. SARS-CoV has strategies to limit host antiviral mechanisms by evading interferon (IFN) responses (8). On the other hand, evidence from clinical and experimental studies suggests that SARS-CoV can induce cytokine dysregulation. Kindler et al. (5) delineate the immune response triggered by HCoV-EMC in HAE cultures by studying the proinflammatory gene expression profile upon HCoV-229E, HCoV-EMC, and SARS-CoV infection. The authors observed that both HCoV-229E and highly pathogenic coronaviruses can only marginally induce IFN and interferon-stimulating gene responses. In particular, HCoV-229E is found to be more capable of inducing proinflammatory gene expression, including tumor necrosis factor alpha (TNF-α) and CXCL10, than the more pathogenic human coronaviruses. In contrast to the findings of Kindler et al., another previous study using well-differentiated normal human bronchial epithelial cells indicated that SARS-CoV induced higher cytokine and chemokine levels than HCoV-229E (9). This discrepancy may be attributed to different sampling times for cytokine and chemokine detection. In addition, one should note that SARS-CoV is known to modulate cytokine production by other key cells responsible for innate immunity in the lung (e.g., macrophage and dendritic cells) (10). It is therefore essential to study HCoV-EMC-infected macrophages and dendritic cells. Furthermore, due to the nature of purified cell culture (e.g., HAE) models, cross talk between epithelial cells, macrophages, and dendritic cells cannot be evaluated. Additional experimental systems, such as ex vivo respiratory organ cultures and animal models, may provide further understanding of diseases caused by HCoV-EMC. In addition, clinical parameters determined from HCoV-EMC-infected patients would be extremely valuable for understanding the disease process in humans and could be used as a reference for data generated from in vitro and animal experiments.
Based on the lack of IFN response found upon HCoV-EMC infection in HAE cultures, Kindler et al. conducted a key experiment and demonstrated the effective suppression of HCoV-EMC replication by administration of type I or type III IFN in the cultures. Zielecki et al. have recently confirmed that HCoV-EMC is sensitive to the antiviral action of type I IFN by using primary non-differentiated tracheobronchial epithelial cells and other epithelial cell lines (11). Again, the confirmation of IFN effectiveness in other models, particularly those relevant to lower respiratory tract infections, will strengthen the use of IFN as a possible therapeutic strategy to control HCoV-EMC infection. Nonetheless, Kindler et al. have pointed out a promising therapy for treating HCoV-EMC infection.
WHERE DOES HCoV-EMC ORIGINATE?
The SARS event has led to intense scientific interest in coronaviruses and to the discovery of many other novel coronaviruses in humans and animals. With these intense efforts, a great diversity of alphacoronaviruses and betacoronaviruses has been detected in bats (Fig. 1). These findings suggest that bats might be the natural reservoirs of these two viral genera and that some of the bat coronaviruses might have adapted to other mammals in occasional spillover events in the past. Although the natural host for HCoV-EMC is yet to be identified, it is tempting to speculate that HCoV-EMC is of bat origin. In fact, recent bat coronavirus surveillance studies have indicated that a bat coronavirus (e.g., BtCoV/VM314/2008) which is genetically closely related to HCoV-EMC can be detected in different countries in Europe (12). But the sequence of this group of bat coronaviruses is still quite distinct from that of HCoV-EMC. This suggests that HCoV-EMC might be carried by an unknown bat species. Notably, bat coronaviruses that are genetically related to HCoV-EMC are all detected from Pipistrellus or Tylonycteris bats (Fig. 1). Comprehensive virus surveillance of bats from these genera and others in the Middle East should be of top priority. Given the fact that SARS-CoV spread to humans via an intermediate host (civet cat) (13), other animals (e.g., poultry, pets, and game animals) that have frequent contacts with humans should also be tested. Assuming that the confirmed human cases/clusters were caused by multiple introductions of HCoV-EMC from animals to humans, identifying the source of this novel pathogen is still the key to preventing further spillover events.
In clinical and epidemiological settings, further development of serological tests for HCoV-EMC is urgently needed. So far, a few immunofluorescence assays specific for HCoV-EMC have been reported (14). It is essential to have reliable serological tools to determine whether HCoV-EMC has been circulating widely in the general population in the affected areas. This would also help answer whether there is sustained transmission of this novel coronavirus in humans. This key information can also help reveal the spectrum of disease severity caused by HCoV-EMC in humans.
IF WE ARE LUCKY, THEN WHAT’S NEXT?
It is not known whether HCoV-EMC is going to be fully established in humans. Extensive efforts have been made and will continue to be needed to fight against this possible epidemic. If we are “lucky” enough to control this novel disease, more resources should be allocated to different areas of coronavirus studies. Currently, we know some animal coronaviruses in wildlife only at the nucleotide level. In fact, the number of bat species tested for coronaviruses is only a fraction of the total number (>1,200) of bat species. In addition, there is a lack of biological/biochemical characterization of these animal viruses. Ideally, we should develop an effective universal strategy to treat and prevent human infections caused by animal coronaviruses. The phylogenetic relationships of coronaviruses (Fig. 1) suggest that there have been a number of introductions of animal coronaviruses (e.g., SARS-CoV and 229E) into humans in the past. The great diversity of coronavirus in bats will surely increase the odds of yet another zoonotic event occurring in the future.
ACKNOWLEDGMENT
This work was partly supported by EMPERIE (grant no. EU FP7 223498).
Footnotes
Citation Chan RWY, Poon LLM. 2013. The emergence of human coronavirus EMC: how scared should we be? mBio 4(2):e00191-13. doi:10.1128/mBio.00191-13.
REFERENCES
- 1. Bermingham A, Chand MA, Brown CS, Aarons E, Tong C, Langrish C, Hoschler K, Brown K, Galiano M, Myers R, Pebody RG, Green HK, Boddington NL, Gopal R, Price N, Newsholme W, Drosten C, Fouchier RA, Zambon M. 2012. Severe respiratory illness caused by a novel coronavirus, in a patient transferred to the United Kingdom from the Middle East, September 2012. Euro Surveill. 17:20290. [PubMed] [Google Scholar]
- 2. Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. 2012. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N. Engl. J. Med. 367:1814–1820 [DOI] [PubMed] [Google Scholar]
- 3. Müller MA, Stalin Raj V, Muth D, Meyer B, Kallies S, Smits SL, Wollny R, Bestebroer TM, Specht S, Suliman T, Zimmermann K, Binger T, Eckerle I, Tschapka M, Zaki AM, Osterhaus ADME, Fouchier RAM, Haagmans BL, Drosten C. 2012. Human coronavirus EMC does not require the SARS-coronavirus receptor and maintains broad replicative capability in mammalian cell lines. mBio 3:e00515-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. van Boheemen S, de Graaf M, Lauber C, Bestebroer TM, Raj VS, Zaki AM, Osterhaus AD, Haagmans BL, Gorbalenya AE, Snijder EJ, Fouchier RA. 2012. Genomic characterization of a newly discovered coronavirus associated with acute respiratory distress syndrome in humans. mBio 3(6):e00473-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kindler E, Jónsdóttir HR, Muth D, Hamming OJ, Hartmann R, Rodriguez R, Geffers R, Fouchier RA, Drosten C, Müller MA, Dijkman R, Thiel V. 2013. Efficient replication of the novel human betacoronavirus EMC on primary human epithelium highlights its zoonotic potential. mBio 4(1):e00611-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dijkman R, Jebbink MF, Koekkoek SM, Deijs M, Jónsdóttir HR, Molenkamp R, Ieven M, Goossens H, Thiel V, van der Hoek L. 20 February 2013. Isolation and characterization of current human coronavirus strains in primary human epithelia cultures reveals differences in target cell tropism. J. Virol. http://dx.doi.org/10.1128/JVI.03368-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pyrc K, Sims AC, Dijkman R, Jebbink M, Long C, Deming D, Donaldson E, Vabret A, Baric R, van der Hoek L, Pickles R. 2010. Culturing the unculturable: human coronavirus HKU1 infects, replicates, and produces progeny virions in human ciliated airway epithelial cell cultures. J. Virol. 84:11255–11263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cheung CY, Poon LL, Ng IH, Luk W, Sia SF, Wu MH, Chan KH, Yuen KY, Gordon S, Guan Y, Peiris JS. 2005. Cytokine responses in severe acute respiratory syndrome coronavirus-infected macrophages in vitro: possible relevance to pathogenesis. J. Virol. 79:7819–7826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chan MC, Chan RW, Tsao GS, Peiris JS. 2011. Pathogenesis of SARS coronavirus infection using human lung epithelial cells: an in vitro model. Hong Kong Med. J. 17(Suppl. 6):31–35 [PubMed] [Google Scholar]
- 10. Frieman M, Heise M, Baric R. 2008. SARS coronavirus and innate immunity. Virus Res. 133:101–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zielecki F, Weber M, Eickmann M, Spiegelberg L, Zaki AM, Matrosovich M, Becker S, Weber F. 28 February 2013. Human cell tropism and innate immune system interactions of human respiratory coronavirus EMC compared to SARS-coronavirus. J. Virol. http://dx.doi.org/10.1128/JVI.03496-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Annan A, Baldwin HJ, Corman VM, Klose SM, Owusu M, Nkrumah EE, Badu EK, Anti P, Agbenyega O, Meyer B, Oppong S, Sarkodie YA, Kalko EKV, Lina PHC, Godlevska EV, Reusken C, Seebens A, Gloza-Rausch F, Vallo P, Tschapka M, Drosten C, Drexler JF. 2012. Human betacoronavirus 2c EMC/2012–related viruses in bats, Ghana and Europe. Emerg. Infect. Dis. 79:477–489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Guan Y, Zheng BJ, He YQ, Liu XL, Zhuang ZX, Cheung CL, Luo SW, Li PH, Zhang LJ, Guan YJ, Butt KM, Wong KL, Chan KW, Lim W, Shortridge KF, Yuen KY, Peiris JS, Poon LL. 2003. Isolation and characterization of viruses related to the SARS coronavirus from animals in southern China. Science 302:276–278 [DOI] [PubMed] [Google Scholar]
- 14. Corman VM, Müller MA, Costabel U, Timm J, Binger T, Meyer B, Kreher P, Lattwein E, Eschbach-Bludau M, Nitsche A, Bleicker T, Landt O, Schweiger B, Drexler JF, Osterhaus AD, Haagmans BL, Dittmer U, Bonin F, Wolff T, Drosten C. 2012. Assays for laboratory confirmation of novel human coronavirus (hCoV-EMC) infections. Euro Surveill. 17:20334. [DOI] [PubMed] [Google Scholar]