Abstract
OBJECTIVE
To study the medical and financial outcomes associated with surgery in the elderly obese patient and ask if obesity itself influences outcomes above and beyond effects from comorbidities known to be associated with obesity.
BACKGROUND
Obesity is a surgical risk factor not present in Medicare’s risk adjustment or payment algorithms, as BMI is not collected in administrative claims.
METHODS
2045 severely or morbidly obese patients (BMI ≥ 35 kg/m2, age between 65 and 80) selected from 15,914 elderly patients in 47 hospitals undergoing hip and knee surgery, colectomy, and thoracotomy were matched to two sets of 2045 non-obese patients (BMI = 20 – 30 kg/m2). A “limited match” controlled for age, sex, race, procedure and hospital. A “complete match” also controlled for 30 additional factors such as diabetes and admission clinical data from chart abstraction.
RESULTS
Mean BMI in the obese was 40kg/m2 versus 26kg/m2 in the non-obese. In the complete match, obese patients displayed increased odds of wound infection: OR = 1.64 (95% CI 1.21, 2.21); renal dysfunction: OR = 2.05(1.39, 3.05); urinary tract infection: OR = 1.55 (1.24, 1.94); hypotension: OR = 1.38 (1.07, 1.80); respiratory events: OR = 1.44 (1.19, 1.75); 30-day readmission: OR = 1.38 (1.08, 1.77); and a 12% longer length of stay (8%, 17%); Provider costs were 10% (7%, 12%) greater in the obese than non-obese, while Medicare payments increased only 3% (2%, 5%). Findings were similar in the limited match.
CONCLUSIONS
Obesity increases the risks and costs of surgery. Better approaches are needed to reduce these risks. Furthermore, to avoid incentives to under-serve this population, Medicare should consider incorporating incremental costs of caring for obese patients into payment policy and include obesity in severity adjustment models.
INTRODUCTION
The epidemic of obesity in American now extends to the elderly population, where over 38 percent of 65 to 80 year olds have a Body Mass Index (BMI) that exceeds 30 kg/m2, and 15 percent exceed 35 kg/m2.1 Though obesity may increase the need for surgery, the decision to perform general and orthopedic surgery on the obese elderly patient is a difficult one, requiring caregivers to calculate potential risks and benefits with a paucity of information.2–21 Given the scope of the problem, there have been relatively few large studies concerning the surgical risks associated with obesity in the elderly,2, 3, 16–19, 21 in part because administrative claims do not collect BMI22. Furthermore, as BMI is not collected, it cannot be used for severity adjustment in Medicare’s payment algorithms. Hence, obesity in the elderly represents a challenge that is important, complex and at the same time understudied in the Medicare population.
In a 47 hospital study of Medicare patients in three states,23 we use claims analysis and chart review with multivariate matching24–28 to study differences in medical and financial outcomes between obese and non-obese elderly patients 65 to 80 years of age. The obese are compared to two matched comparison groups, a “limited match” that controls for age, sex, race, procedure and hospital, and a “complete match” that also controls for comorbid conditions commonly associated with obesity. The complete match asks a hypothetical question: How would the outcomes and costs of an obese and a non-obese patient compare if both patients had comorbities, such as hypertension and diabetes, often found among the obese? Outcomes examined in this study will be that of mortality, complications, readmissions, length of stay, and financial costs and payments. We find important “specific” effects from obesity, above and beyond those problems attributed to its associated comorbidities, suggesting a need for new approaches to care for, and pay for, the elderly obese surgical patient.
METHODS
Study Overview
The Obesity and Surgical Outcomes Study (OBSOS)23 is a study of surgery at 47 hospitals located throughout Illinois, New York and Texas. Using Medicare claims, elderly patients between the ages of 65 and 80 were identified undergoing one of five types of surgery between 2002 and 2006: (1) hip replacement or revision excluding fracture (ICD9CM Principal Procedure codes 81.51-81.53); (2) knee replacement or revision (ICD9CM Principal Procedure 81.54, 81.55); (3) colectomy for cancer (ICD9CM Principal Procedure codes 45.7-45.79, 45.8) (ICD9CM Principal Diagnosis codes 153-153.9, 154-154.8, 230.3-6); (4) colectomy not for cancer (ICD9CM Principle Procedure 45.7-45.79, 45.8) and (ICD9CM Principal Diagnosis codes 562.1-562.13); and (5) thoracotomy (ICD9CM Principal Procedure codes 32-32.9).
Hospitals were contacted by the Oklahoma Foundation for Medical Quality (OFMQ), and requested to abstract between 300 and 400 pre-specified charts in order to collect baseline information including body mass index (BMI), admission vital signs and laboratory tests, and information on the surgical procedure. All data collected was de-identified and merged with encrypted Medicare claims files and sent to the study investigators for analysis. Approval was obtained from The Children’s Hospital of Philadelphia IRB (the IRB associated with the PI of the study), as well as hospital specific IRBs when requested.
Statistical Methods
Overview
We define obesity as a BMI > 30.29 Furthermore, for descriptive ease, we define a BMI ≥ 35 but less than 40 as “severely” obese and a BMI ≥ 40 as “morbidly” obese. Building upon our earlier Surgical Outcomes Study,24, 27, 30 the present OBSOS study was designed to compare cases of patients who were severely and morbidly obese (BMI ≥ 35 kg/m2) to non-obese (20 ≤ BMI < 30) elderly surgical controls in Medicare with respect to outcomes, such as survival and complications, length of stay and readmission rates, and Medicare payments and resource utilization costs. The study design called for matching with different subsets of prognostic factors.
The Matching Algorithm
As described above, a “limited” match and a “complete” match were constructed using the same matching methods but different matching variables. The limited match controlled for procedure, age, sex, race, and hospital, while the complete match also controlled for 30 conditions associated with obesity, other clinical data from chart abstraction such as an approximate APACHE score 27, 30, 31, transfer status, and admission from the emergency department. Diabetes was defined using both information abstracted from the chart and information obtained from claims. Using the variables appropriate for that match, the match was implemented using fine balance,25, 32 a propensity score25, 33 for being obese, as well as a risk of mortality or prognostic score34 based on claims data whose parameters were independently estimated from all hospitals in Illinois, New York and Texas not included in this study. Fine balance ensured that a hospital that provided, say, 100 obese knee surgery patients for the match also provided 100 non-obese knee surgery patients for the match, so that the distribution of knee surgery patients over hospitals is identical in the obese and non-obese groups.
Specific effects of obesity on outcomes would be suggested if both ‘limited” and “complete” match results displayed similar differences between the obese and the non-obese. If the “limited” match detected differences between the obese and the non-obese patients but these differences disappeared in the “complete” match, this would suggest that the differences in outcomes observed between groups could be explained in terms of comorbidities associated with obesity and not by obesity itself.
In order to ensure good matching quality, we sought a minimum pool of 2.5 controls (non-obese elderly patients with BMI’s ≥ 20 kg/m2 and < 30 kg/m2) to each obese elderly case (where cases needed to be severely or morbidly obese with BMI’s at least 35 kg/m2). For all procedures, except knees, the matching ratio was greater than 2.5. For knee procedures, the proportion of obese patients was higher, so that the matching ratio was less than 2.5. To ensure a matching ratio greater than 2.5, we randomly sampled a subset of patients from the knee group that were severely or morbidly obese, to ensure the minimum ratio. Of 1,425 severely or morbidly obese knee patients, we randomly sampled 1028 to achieve a matching ratio of 2.6. For all other procedures, we utilized all available obese patients (with BMIs ≥ 35 kg/m2). The overall matching ratio in the study was 4.5 controls per case (2045 cases and 9177 potential controls).
Defining Payments and Costs
Total payments and costs reflect expenses incurred during the patient’s index admission, as well as during any subsequent encounters beginning after discharge but within 30 days of admission, regardless of length, excluding non-acute care and rehabilitation costs (Diagnosis Related Groups [DRG] 462). All results are expressed in 2008 dollars. Payments were defined by applying the standardized Payment Calculation Worksheets, available from ResDAC,35 to the Medicare Inpatient, Hospital Outpatient and Carrier files. Total payments equal the sum of payments from Medicare (both DRG-based and per diem amounts), beneficiary coinsurance and deductibles, and payments from other primary payers.
Hospital costs were calculated using two methods. Method 1 was based on resource utilization.36, 37 Each patient’s stay was categorized into critical care days or non-critical care days based on revenue center in the inpatient file, and assigned national daily average prices for each category.38 For the patient’s index admission, the cost of the operating room time was added by multiplying the anesthesia time obtained from the Physician Part B/Carrier file by an average per-minute operating room cost.39 If anesthesia time was not available, the patient was assigned the median anesthesia time for their procedure category. Physician services were priced by assigning each service recorded in the Carrier file its 2008 Relative Value Units, which were then converted to dollar amounts. Finally, to capture the additional cost of visits to an emergency department following discharge (as opposed to follow-up care in a physician’s office), patients were assigned an additional cost for each unique emergency department visit, reflecting the facility component of the cost.40 Method 2 was based on total hospital charges drawn from the Medicare Inpatient and Outpatient files multiplied by annual, hospital-specific cost-to-charge ratios obtained from CMS Cost Reports, and also included resource use estimates for office encounters. Method 1 will yield more conservative estimates of cost because it is difficult to account for all dimensions of resources and overheads, but viewing both methods can be thought of as lower and upper estimates, as one builds cost from the ground up while the other does the reverse. See technical appendix for details.
Statistical Tests
Balance on observed variables after matching was appraised using standard two-sample tests that contrast achieved balance with the magnitude of covariate balance anticipated from completely random assignment.33 When testing the hypothesis of no difference in outcomes between the matched obese and non-obese patients, the Wilcoxon sign-rank statistic41 for paired data and its associated confidence interval and Hodges-Lehmann point estimate were used for continuous variables, and the McNemar statistic42 for paired data was used for categorical variables. When comparing survival-type distributions between the matched groups, the paired Prentice-Wilcoxon test43 for censored data was used.
RESULTS
Study Hospital Characteristics
Table 1 describes the 47 hospitals. Names of the hospitals are in the electronic appendix. Approximately 47% of hospitals were non-teaching, and 6% were “very major” teaching hospitals (having a resident-to-bed ratio greater than 0.60).44–46 Hospital size varied considerably, with the inter-quartile range being between 256 and 539 beds.
Table 1.
Study Hospital Characteristics
| Number of Hospitals | 47 |
|
| |
| Size (Beds) mean (std) | 423 (285) |
| Size Distribution, % | |
| 0–200 | 15 |
| 201–400 | 40 |
| 401–600 | 28 |
| 601–800 | 11 |
| 800 | 6 |
|
| |
| Nurse to bed ratio,* mean (SD) | 1.64 (0.44) |
|
| |
| Nurse Mix,† mean (SD) | 0.91 (0.08) |
|
| |
| Technology index,‡ % | 77 |
|
| |
| Teaching intensity based on resident to bed ratio, % | |
| Nonteaching (RB ratio = 0) | 47 |
| Very minor (0 < RB ≤ 0.05) | 15 |
| Minor (0.05 < RB ≤ 0.25) | 19 |
| Major (0.25 <RB ≤ 0.6) | 13 |
| Very major (0.6 < RB ≤ 1.1) | 6 |
|
| |
| Location, (%) | |
| Illinois | 38 |
| New York | 17 |
| Texas | 45 |
Full time equivalent registered nurses/number of beds.
Registered nurses/(registered nurses + licensed practical nurses)
Technology index = 1 if hospital performs open-heart surgery, organ transplantation, or has a burn unit; otherwise index = 0.
Match Quality: Did Each Match Achieve Balance in the Variables Matched On?
The quality of the limited and complete matches is presented in Table 2, which describes the obese, the non-obese matched for many variables by the “complete” algorithm, and the non-obese matched for a few variables by the “limited” algorithm. A complete list of matching variables is in the electronic appendix. Each match successfully balanced those specific variables it was supposed to balance. In the limited match that meant no significant difference in age, sex, race and procedure (and the risk and propensity scores based on these variables). In the complete match that meant no difference in age, sex, race, procedure as well as all additional variables in the complete match such as diabetes and history variables as well as a more complex propensity score and risk score now comprised of far more variables than in the limited match. In both matches, all hospital attributes are perfectly balanced.
Table 2.
Matching Results
| Variables | Obese N = 2045 | Complete Match (Nonobese) N = 2045 | Limited Match (Nonobese) N = 2045 |
|---|---|---|---|
| BMI, mean | 39.74 | 26.30f | 26.14f |
| Weight, mean, kg | 108.20 | 74.43f | 73.78f |
| Height, mean, cm | 164.85 | 167.91f | 167.68f |
| Limited matching variables (controlled in both matches) | |||
| Age, yrs | 71.54 | 71.53 | 71.43 |
| Sex, male, % | 33.40 | 34.87 | 33.55 |
| Race: | |||
| White, % | 90.66 | 91.83 | 91.30 |
| Black, % | 6.85 | 5.62 | 6.50 |
| Other, % | 2.49 | 2.54 | 2.20 |
| Procedure: | |||
| Hip, % | 25.33 | 25.33 | 25.33 |
| Knee, % | 50.27 | 50.27 | 50.27 |
| Colectomy for cancer, % | 10.42 | 10.42 | 10.42 |
| Colectomy not for cancer, % | 4.84 | 4.84 | 4.84 |
| Thoracotomy, % | 9.14 | 9.14 | 9.14 |
| 30-day mortality (predicted probability) | 0.01 | 0.01 | 0.01 |
| Propensity to be obese (probability) | 0.25 | 0.24 | 0.21 |
| Additional variables for complete match (controlled in the complete but not the limited match) | |||
| Diabetes: | |||
| No Diabetes, % | 61.22 | 60.73 | 81.32f |
| Diabetes w/o meds, % | 12.03 | 12.13 | 7.97f |
| Diabetes with meds, % | 26.75 | 27.14 | 10.71f |
| Transfer-in, % | 0.44 | 0.24 | 0.24 |
| Admission from emergency department, % | 4.50 | 3.96 | 4.50 |
| APACHE score (mean) | 23.88 | 23.81 | 22.95f |
| Hx asthma, % | 11.39 | 9.88 | 6.85f |
| Hx chronic lung disease, % | 19.66 | 18.88 | 18.88 |
| Hx collagen vascular disease, % | 4.79 | 3.81 | 6.70a |
| Hx dementia, % | 1.86 | 1.17 | 3.23b |
| Hx hypothyroidism, % | 20.59 | 18.44 | 17.36b |
| Hx hepatic abnormalities, % | 3.47 | 3.13 | 4.79a |
| Hx renal dysfunction, % | 4.65 | 4.55 | 2.25f |
| Hx renal failure, % | 3.77 | 3.47 | 1.86e |
| Hx smoking, % | 7.87 | 7.19 | 9.54 |
| Hx weight loss, % | 1.47 | 1.27 | 2.89c |
| Hx stroke, % | 3.91 | 3.37 | 4.11 |
| Hx paraplegia, % | 0.49 | 0.39 | 0.49 |
| Hx hypertension, % | 85.57 | 85.87 | 71.44f |
| Hx congestive heart failure, % | 15.40 | 14.77 | 8.26f |
| Hx myocardial infarction, % | 5.43 | 5.48 | 4.60 |
| Hx arrhythmia, % | 20.73 | 21.52 | 17.80a |
| Hx angina, % | 3.18 | 2.74 | 3.67 |
| Hx valvular heart disease, % | 11.54 | 11.25 | 10.46 |
P values compare nonobese to obese
< 0.05;
< 0.01;
< 0.005;
< 0.001;
< 0.0005;
<0.0001. The limited match includes Age, Sex, Procedure, and Race, as well as a limited risk and propensity score using these 4 variables. The complete match adds a total of 36 patient variables including those listed previously. Look, for instance, at diabetes. For full list, see Electronic Appendix. Displayed earlier included, but not limited to, all variables where there were any significant differences between obese and nonobese.
Table 2 is organized so that the description of the non-obese patients of the complete match is to the immediate right of the obese patients, and farther to the right are the non-obese patients in the limited match. At the top of Table 2 are the unmatched variables that define obesity (BMI, height and weight), followed by variables controlled for in both matches, followed by variables controlled in the complete match but not the limited match. If a variable, such as diabetes, was controlled for in the complete but not the limited match, then we expect to see a rate of diabetes in the limited match controls that is typical of leaner patients and a rate of diabetes in the complete match controls that is typical of severely obese patients, though both matched controls are not obese. In obese patients, the rate of diabetes was 39%. The non-obese in the complete match had a diabetes rate of 39% (no different than the obese), whereas in the limited match, which did not match on diabetes, the rate of diabetes in the non-obese was only 19%, which was different beyond the P < 0.0001 level. In other words, as expected, non-obese patients undergoing the same surgical procedures as the obese had a much lower rate of diabetes, but after matching for diabetes, along with many other comorbidities, there was no difference in the rate of diabetes between groups. This same result applies to each characteristic that was matched in the complete match, and not in the limited match. For all variables that were matched on, there was no difference between the obese and the non-obese.
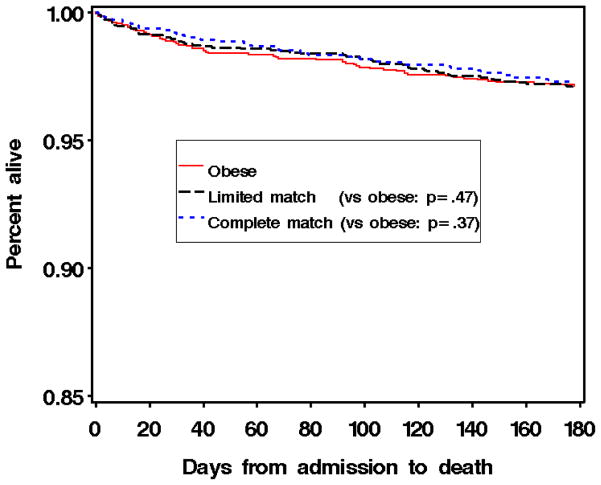
Medical Outcomes
Table 3 describes the 30- and 180-day mortality, in-hospital or 30-day complications, length of stay, readmission rates, costs and payments. There were no significant differences in mortality between the obese and non-obese patients. Figure 1 displays the overlapping Kaplan-Meier survival curves for the obese, and the matched pairs using the limited and complete matching algorithms.
Table 3.
Surgical Outcome Results
| Outcome Measures | Obese % | Nonobese Complete Match % | Nonobese Limited Match % | Nonobese Complete Match | Nonobese Limited Match | |||
|---|---|---|---|---|---|---|---|---|
| OR† | 95% CI | OR† | 95% CI | |||||
|
| ||||||||
| Death 30 days | 1.18 | 0.83 | 1.03 | 1.50 | (0.73, 3.19) | 1.16 | (0.60, 2.26) | |
|
| ||||||||
| Death 180 days | 2.85 | 2.75 | 2.99 | 1.04 | (0.69, 1.58) | 0.95 | (0.64, 1.40) | |
|
| ||||||||
| Complications 30 days | ||||||||
|
| ||||||||
| Wound infection | 6.33 | 3.97 | 4.17 | 1.64 | (1.21, 2.21)d | 1.59 | (1.18, 2.16)c | |
|
| ||||||||
| Sepsis | 3.09 | 1.91 | 1.72 | 1.81 | (1.14, 2.90)b | 1.9 | (1.21, 3.04)c | |
|
| ||||||||
| Respiratory | 19.53 | 15.65 | 15.46 | 1.44 | (1.19, 1.75)e | 1.44 | (1.19, 1.75)e | |
|
| ||||||||
| Venous thromboembolism | 5.74 | 3.92 | 4.76 | 1.47 | (1.09, 2.00)a | 1.23 | (0.92, 1.64) | |
|
| ||||||||
| Central neurological events | 4.91 | 4.66 | 5.55 | 1.06 | (0.78, 1.44) | 0.87 | (0.65, 1.16) | |
|
| ||||||||
| Cardiac events | 11.04 | 9.12 | 6.87 | 1.32 | (1.04, 1.67)a | 1.69 | (1.35, 2.14)f | |
|
| ||||||||
| Hypotension/shock | 8.24 | 6.23 | 6.63 | 1.38 | (1.07, 1.80)a | 1.27 | (0.99, 1.63) | |
|
| ||||||||
| Urinary T=tract infection | 10.99 | 7.41 | 6.33 | 1.55 | (1.24, 1.94)e | 1.85 | (1.46, 2.35)f | |
|
| ||||||||
| Pyelonephritis | 0.39 | 0.20 | 0.05 | 2.00 | (0.54, 9.07) | 8.00 | (1.07, 355)a | |
|
| ||||||||
| Renal dysfunction | 4.50 | 2.40 | 1.81 | 2.05 | (1.39, 3.05)e | 2.67 | (1.77, 4.11)f | |
|
| ||||||||
| Internal organ damage | 9.03 | 7.65 | 8.10 | 1.25 | (0.95, 1.64) | 1.16 | (0.90, 1.49) | |
|
| ||||||||
| Bleeding (surgical or GI) | 26.40 | 28.20 | 26.90 | 0.91 | (0.79, 1.05) | 0.97 | (0.84, 1.13) | |
|
| ||||||||
| Decubitis ulcer | 1.37 | 1.13 | 0.88 | 1.23 | (0.67, 2.26) | 1.59 | (0.83, 3.10) | |
|
| ||||||||
| Orthopedic complications | 4.17 | 4.46 | 4.22 | 0.92 | (0.66, 1.29) | 0.99 | (0.70, 1.39) | |
|
| ||||||||
| Length of stay, days | ||||||||
| Median (95% CI) | 4.0 (4.0, 4.0) | 4.0 (4.0, 4.0) | 4.0 (4.0, 4.0) | Ratio* (Obese to Nonobese) | Ratio* (Obese to Nonobese) | |||
| 90th percentile (95% CI) | 10.0 (9, 10) | 9.0 (8, 9) | 8.0 (8, 9) | 1.12f | 95% CI (1.08, 1.17) | 1.15f | 95% CI (1.11, 1.21) | |
|
| ||||||||
| Readmission or death | ||||||||
|
| ||||||||
| 7 days | 3.90 | 2.44 | 2.50 | 1.56 | (1.08, 2.27)a | 1.67 | (1.13, 2.50)a | |
|
| ||||||||
| 30 days | 9.24 | 6.92 | 6.25 | 1.38 | (1.08, 1.77)b | 1.53 | (1.20, 1.96)d | |
|
| ||||||||
| Costs and Payments, In-hospital or Within 30 Days | Obese | Nonobese Complete | Nonobese Limited | Ratio* (Obese to Nonobese) Complete | Cost Ratio Minus PMT Ratio Complete | Ratio* (Obese to Nonobese) Limited | Cost Ratio Minus PMT Ratio Limited | |
|
| ||||||||
| Costs ($) (Estimated Using Cost-to-Charge Ratios) | Median (95% CI) | 16,779 (16,443, 16,994) | 15,970 (15,698, 16,213) | 15,993 (15,661, 16,260) | 1.10f (1.07, 1.12) | 0.06f (0.04, 0.08) | 1.10f (1.08, 1.13) | 0.06f (0.04, 0.08) |
| 90thpercentile (95% CI) | 31,798 (30,069, 33,562) | 27,822 (26,614, 29,647) | 27,534 (26,331, 29,339) | |||||
|
| ||||||||
| Costs ($)(Estimated Using Resources) | Median (95% CI) | 11,655 (11,469 11,938) | 11,251 (11,003, 11,443) | 11,211 (10,997, 11,433) | 1.10f (1.08, 1.13) | 0.08f (0.05, 0.10) | 1.11f (1.09, 1.14) | 0.08f (0.06, 0.10) |
| 90thpercentile (95% CI) | 33,164 (30,329, 35,757) | 29,388 (27,370, 32,164) | 28,716 (25,981, 30,644) | |||||
|
| ||||||||
| Medicare Payments (Payment) †($) | Median (95% CI) | 15,736 (15,541, 15,952) | 15,622 (15,422, 15,835) | 15,542 (15,344 15,748) | 1.03f (1.02, 1.05) | ------- | 1.03f (1.02, 1.05) | ------- |
| 90thpercentile (95% CI) | 29,872 (28,746, 31,052) | 28,768 (27,504, 29,880) | 28,160 (27,155 29,448) | |||||
P values compare obese to nonobese:
< 0.05;
< 0.01;
< 0.005;
< 0.001;
< 0.0005;
<0.0001.
H-L: Hodges-Lehmann Estimator.
OR: Odds ratio comparing obese with nonobese.
Figure 1. Kaplan Meier plot of percent alive by days from admission.
The obese group is depicted by a solid red line, the non-obese limited match is depicted by the gray short-dashed line, and the non-obese complete match is the blue long-dashed line. As can be seen, there is no difference in survival between the obese and either the complete or limited match.
Complications were more common in the obese patients when compared to both the limited and complete matched non-obese patients. In the limited match, the odds of a wound infection were increased almost two-fold in the obese patients, and after complete adjustment, the two-fold increase was maintained (P < 0.0009). The odds of developing sepsis was significantly increased by 90% in the limited match (P < 0.0042) and stayed elevated at 81% increase (P < 0.0097) after adding the complete matching variables. The odds of respiratory system complications were increased by 44% in the obese, (P < 0.00012) and this increased risk remained similar in the complete match. The odds of developing a venous thromboembolism (VTE) were 47% higher (P < 0.01) in the obese in the complete match, but were not significantly elevated in the limited match. The odds of developing a urinary tract infection (UTI) were 85% higher (P < 0.00001) in the obese using the limited match and declined to 55% higher (P < 0.0001) using the complete match. Pyelonephritis was rare, but more common in the obese when using the limited match (P < 0.039), but failed to reach significance in the complete match. Renal complications were increased almost three-fold in the obese using the limited match (P<0.00001), and two-fold in the complete match (P < 0.00015). Similarly, the odds of hypotension were increased 27% in the obese using the limited match (P < 0.059), and a 38% elevation was observed in the complete matched analysis (P < 0.013). The odds of a cardiac event were twice as high in the obese than in the non-obese using the limited match (P < 0.00001). However, the odds were less elevated after using the complete matching variables, suggesting less of a specific effect from obesity because non-obese patients with similar comorbidities also developed similar rates of cardiac complications. The odds of central nervous system complications, internal organ damage, post-operative bleeding, decubitus ulcers, and orthopedic complications were not significantly different between obese and non-obese patients.
The obese also displayed a 12% longer length of stay than their non-obese counterparts in the complete match (P < 0.00001), and 15% longer in the limited match (P < 0.00001). Of note, the upper 90th percentiles were 10 days in the obese and 9 and 8 days in the complete and limited matches respectively.
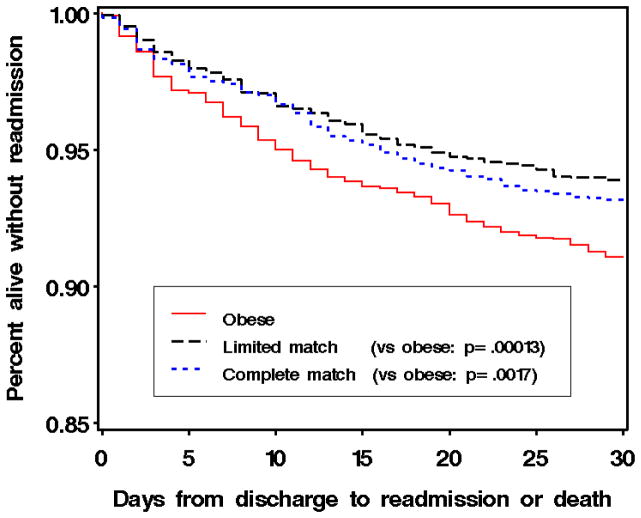
The odds of being readmitted were between 40% to 60% higher in the obese than in the non-obese. Figure 2 displays a Kaplan-Meier plot of alive without readmission over the first 30 days from discharge. These increased readmission rates were apparent using both the limited and complete matches.
Figure 2. Kaplan Meier plot of percent alive without readmission by days from discharge.
The obese group is depicted by a solid red line, the non-obese limited match is depicted by the gray short-dashed line, and the non-obese complete match is the blue long-dashed line. There is a considerable difference in the readmission rates between the obese and both non-obese groups.
Financial Outcomes, Financial Risks
For the complete match, Medicare payments were 3% greater for the obese than the non-obese, P < 0.00001. However, using cost to charge ratios, costs were 10% greater for the obese than the non-obese (P < 0.00001), and 10% greater using resource derived costs (P < 0.00001). As shown in Table 3, formally testing the difference between these cost and payment ratios displayed large and highly significant results, suggesting that the increased costs associated with the obese were not accompanied by similar increases in payments. We found similar differences in the limited match.
To better understand the financial risks associated with performing surgery on the obese as compared to the non-obese, we calculated the difference in “contribution margin” or profit (payment – cost) between the obese and the non-obese, and studied how obesity was associated with profitability (profit in the obese - profit in the non-obese). In one sense, studying the profit from a single surgical procedure is difficult, because there are many costs, such as the costs associated with preventing hospital acquired infections or having spare capacity in the ICU, that cannot be assigned to individual patients, yet presumably are not reasonably assigned equally to procedures that differ greatly in their length and complexity. In another sense, with our matched pairs, studying the difference in profit, obese-versus-nonobese, is less difficult because every hospital contributes the same number of patients to the obese and nonobese groups from every surgical category. If a hospital’s overhead cost for colectomy with cancer differs from overhead cost for knee surgery, this fixed difference will cancel in our matched comparison of obese and nonobese. Using the complete match, and costs based on resource consumption, we grouped each of the study matched pairs (obese to non-obese) into categories of profitability by displaying the absolute value of the difference in profit between the obese and non-obese. Table 4 breaks the 2,009 matched pairs (36 of the 2,045 pairs were not analyzed due to missing resource data) into three groups: the pairs with less than a $1,000 difference in profitability; pairs having between a $1,001 and $10,000 difference, and pairs with more than a $10,000 difference in profit between the obese and non-obese matched pair. We then ask which member of the pair was more profitable. There were 322 matched pairs where the difference in profitability was small, (less than $1,000). Among these, the obese patient was less profitable than the non-obese matched control in 171/322 of these pairs and in 151/322 pairs the obese patient was more profitable than the non-obese matched control, yielding an odds of 1.13 (95% CI .90, 1.42), P = 0.290, suggesting no significant association between obesity and profit status among the matched pairs when there was only a small difference in profitability. However, as the size of the difference in profitability increased, the odds that the less profitable patient in the matched pair was obese became larger and statistically significant. In 539 pairs where the difference in profitability was more than $10,000, the obese patient was less profitable than the non-obese matched control in 313/539 of these pairs and in 226/539 pairs the obese patient was more profitable than the non-obese matched control, yielding an odds of 1.38 (95% CI 1.16, 1.65), P < 0.00021, suggesting a strong association between obesity and less profitable status when large differences in profitability were observed.
Table 4.
Profitability* in Obese and Nonobese Matched Pairs
| Absolute Difference in Profit Between Obese and Nonobese Matched Control, $ | Pairs Where Obese Patient Was Less Profitable | Pairs Where Nonobese Patient Was Less Profitable | Odds of Obese Being Less Profitable Than the Nonobese | 95% CI | P |
|---|---|---|---|---|---|
| 0–1000 | 171 | 151 | 1.13:1 | 0.90–1.42 | 0.28966 |
| 1001–10,000 | 600 | 548 | 1.09:1 | 0.98–1.23 | 0.12498 |
| >10,000 | 313 | 226 | 1.38:1 | 1.16–1.65 | 0.00021 |
Profitability is the difference in profit between the nonobese and the obese. Profit is payment minus cost, computed within each matched pair, using the complete match and resource-based costs. We analyzed 2009 of the 2045 pairs; 36 were deleted because of incomplete resource information. For profit differences greater than $10,000, obese patients were far more likely to be less profitable than their matched nonobese controls.
DISCUSSION
Our study found large and significant elevations in the risks of readmission in the elderly obese and greater risks of many complications, without a significant increase in mortality. Furthermore, consistent with these elevated risks, we found substantial differences in costs between the obese and non-obese, yet much smaller differences in payments.
Using limited and complete matches, we distinguished specific risks of obesity from risks caused by diseases associated with obesity. We found that the risks of complications and readmission due to obesity were often evident even after matching on comorbidities associated with obesity. This suggests that obesity’s specific adverse effects are, in part, separate from comorbidities associated with obesity. This important information should aid surgeons to more accurately risk-stratify patients during preoperative evaluation, appropriately educate patients about postoperative expectations, and provide information about areas of postoperative management that may be targets for quality improvement. For example, we observed an over 40% increase in readmission rates in the obese versus the non-obese, whether we matched using the limited or complete match. Given much higher rates of readmission, and the importance of readmissions to patient care and resource consumption,47 our study suggests a need to re-evaluate current discharge criteria for obese patients and a need to re-design how we manage obese elderly patients after discharge.48–50 Additionally, in an era of public reporting of surgical outcomes and pay for performance, measurement of and adjustment for patient BMI may be critical for accurate risk adjustment.
The matched design of this study also allowed us to better examine the extent that obesity influences Medicare payments and provider costs. Establishing that the specific effects of obesity are associated with excess medical risks and financial costs, beyond those costs from comorbidities associated with obesity (like diabetes and heart disease), would suggest that patient BMI should be included in administrative data. Under Medicare’s current reimbursement system, the obese are typically less profitable than similar non-obese patients, but separately and in addition, the obese also present a much greater risk of being substantially unprofitable patients. When an obese and non-obese pair of patients undergoing the same procedure differed substantially in profitability, by more than $10,000, the odds were 4-to-3 that the obese patient was the substantially less profitable patient. Medicare could compensate providers for the typically greater cost and greater risk in cost for the obese patient by incorporating BMI in its payment formula. In fact, current proposals head in the opposite direction. If Medicare reduces payments for readmissions when the obese are more likely to be readmitted, the difference in profitability will likely grow larger, not smaller.
The literature has often displayed conflicting results concerning the effect of obesity on outcomes, and none have utilized matching to formally analyze profitability differences between obese and non-obese patients. Dindo et al.,2 as well as others,11, 20 have suggested that obesity is not, with only some isolated exceptions, associated with increased complications. In contrast, there are studies reporting increased complications in the obese.3–5, 7, 9, 10, 12–14, 16–18, 21 Most studies have not demonstrated increased near-term mortality associated with obesity,2, 6, 7, 9, 10, 13 though some have reported an increased risk of mortality in the morbidly obese,21 or super obese17 (BMI’s greater than 50 kg/m2). With respect to our finding concerning renal complications, again, there have been disparate results. Suleiman et al.20 in a study of total knee and hip arthroplasty, did not observe an increase in renal complications, or any other complications. However, their population, with a mean age of 65 years, was younger than our study population and the sample included less than 500 severely or morbidly obese patients. Others have found increased renal complications.16,19 Our results of an elevated risk of renal abnormalities were consistent with a report by Merkow et al. in colon cancer surgery19. The Merkow study involved a comparison of obese and non-obese colectomy for cancer cases in which 12.4 percent had BMI’s above 35 kg/m2 (396 patients) and of those patients, roughly half were older than 65 years. They found approximately an odds ratio of 1.71 for developing renal failure when comparing their group having BMI greater than 35 kg/m2 to that having BMI between 25 and 29 kg/m2, whereas our study reports an odds ratio of 2.05 for a category having BMI 35 kg/m2 or greater compared to that having BMI between 20 and 30 kg/m2 in the complete match and 2.67 in the limited match. Of interest, we found that the odds of hypotension were also elevated for the obese in both the limited and complete matches. Exploring practice styles for fluid resuscitation, drug dosing and anesthetic techniques may help us understand the elevated rates observed in the obese for both of these complications.
Our study has limitations. The obese patients we examined all underwent surgery after having satisfied the preoperative risk stratification used by their surgeons, and therefore these patients may have had less risk than the typical obese patient desiring, but possibly not receiving, surgery. This would lead to underestimating differences in outcomes between the obese and non-obese that would have occurred without such selection. While selection bias is a possibility, it would have to have been produced by variables other than those controlled for in the complete match in Table 2. Furthermore, we did not study resources associated with non-acute care or rehabilitation, which may have been greater in the obese. Also, our economic analysis was dependent on Medicare claims, not specific hospital accounting systems. While we can precisely measure what Medicare paid to their providers, we cannot determine exact costs, which may vary by hospital. However, we did present two different methods for estimating these costs that yielded very similar differences in cost between obese and non-obese patients. Additionally, for each procedure group, say knee surgery, each of the 47 hospitals contributed exactly the same number of obese and non-obese patients to our study. As a consequence, an unmeasured fixed cost that affects in the same way all knee surgeries in one hospital will be equally represented in our obese and non-obese groups and will not bias our comparison.
In conclusion, surgery on the obese elderly patient is associated with significantly increased medical risks and financial costs. To reduce these risks, it will be important to understand and remedy specific problems associated with obesity itself, both in the hospital and after discharge. Furthermore, Medicare should include obesity status in risk adjustment models and consider incorporating the incremental costs of caring for the obese elderly patient into payment policy. Not doing so may create incentives to under-serve this population, especially since providers appear to be taking on far more financial risk when operating on obese patients than their non-obese counterparts.
Supplementary Material
Acknowledgments
SOURCE OF FUNDING: This research was funded through a grant from the National Institute of Diabetes, Digestive and Kidney Diseases (NIDDK R01 DK 073671) and the National Science Foundation (SES-0849370).
We thank Traci Frank, Rebecca Jones, Lanyu Mi, Hong Zhou, Bijan Niknam, and Thomas Wadden for their assistance in conducting this study.
Footnotes
CONFLICTS OF INTEREST: None
DISCLOSURE OF FUNDING: National Institutes of Health (NIH)
References
- 1.Centers for Disease Control and Prevention, National Center for Health Statistics. National Health and Nutrition Examination Survey. NHANES 2007 – 2008 Examination Files. Atlanta, GA: [Accessed September 12, 2011.]. Available at: http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/exam07_08.htm. [Google Scholar]
- 2.Dindo D, Muller MK, Weber M, Clavien P-A. Obesity in general elective surgery. Lancet. 2003;361:2032–2035. doi: 10.1016/S0140-6736(03)13640-9. [DOI] [PubMed] [Google Scholar]
- 3.Gendall KA, Raniga S, Kennedy R, Frizelle FA. The impact of obesity on outcome after major colorectal surgery. Dis Colon Rectum. 2007;50:2223–22237. doi: 10.1007/s10350-007-9051-0. [DOI] [PubMed] [Google Scholar]
- 4.Lee CT, Dunn RL, Chen BT, et al. Impact of body mass index on radical cystectomy. J Urol. 2004;172:1281–1285. doi: 10.1097/01.ju.0000138785.48347.aa. [DOI] [PubMed] [Google Scholar]
- 5.Bamgbade OA, Rutter TW, Nafiu OO, Dorje P. Postoperative complications in obese and nonobese patients. World J Surg. 2006;31:556–560. doi: 10.1007/s00268-006-0305-0. [DOI] [PubMed] [Google Scholar]
- 6.Flancbaum L, Choban PS. Surgical implications of obesity. Annu Rev Med. 1998;49:215–34. doi: 10.1146/annurev.med.49.1.215. [DOI] [PubMed] [Google Scholar]
- 7.Pasulka PS, Bistrian BR, Benotti PN, Blackburn GL. The risks of surgery in obese patients. Ann Intern Med. 1986;104:540–546. doi: 10.7326/0003-4819-104-4-540. [DOI] [PubMed] [Google Scholar]
- 8.Epstein AM, Read JL, Hoefer M. The relation of body weight to length of stay and charges for hospital services for patients undergoing elective surgery: A study of two procedures. Am J Public Health. 1987;77:993–997. doi: 10.2105/ajph.77.8.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mathur AK, Ghaferi AA, Sell K, et al. Influence of body mass index on complications and oncologic outcomes following hepatectomy for malignancy. J Gastrointest Surg. 2010;14:849–857. doi: 10.1007/s11605-010-1163-5. [DOI] [PubMed] [Google Scholar]
- 10.Lynch RJ, Ranney DN, Shijie C, et al. Obesity, surgical site infection, and outcome following renal transplantation. Ann Surg. 2009;250:1014–1020. doi: 10.1097/SLA.0b013e3181b4ee9a. [DOI] [PubMed] [Google Scholar]
- 11.Chang SS, Jacobs B, Wells N, et al. Increased body mass index predicts increased blood loss during radical cystectomy. J Urol. 2004;171:1077–1079. doi: 10.1097/01.ju.0000113229.45185.e5. [DOI] [PubMed] [Google Scholar]
- 12.Angrisani L, Lorenzo M, De Palma G, et al. Laparoscopic cholecystectomy in obese patients compared with nonobese patients. Surg Laparosc Endosc. 1995;5:197–201. [PubMed] [Google Scholar]
- 13.Rockx MA, Fox SA, Stitt LW, et al. Is obesity a predictor of mortality, morbidity and readmission after cardiac surgery? Can J Surg. 2004;47:34–38. [PMC free article] [PubMed] [Google Scholar]
- 14.Pikarsky AJ, Saida Y, Yamaguchi T, et al. Is obesity a high-risk factor for laparoscopic colorectal surgery? Surg Endosc. 2002;16:855–858. doi: 10.1007/s004640080069. [DOI] [PubMed] [Google Scholar]
- 15.Naylor JM, Harmer AR, Heard RC. Severe other joint disease and obesity independently influence recovery after joint replacement surgery: An observational study. Aust J Physiother. 2008;54:57–64. doi: 10.1016/s0004-9514(08)70067-9. [DOI] [PubMed] [Google Scholar]
- 16.Virani SS, Nambi V, Lee VV, et al. Obesity: An independent predictor of in-hospital postoperative renal insufficiency among patients undergoing cardiac surgery? Tex Heart Inst J. 2009;36:540–545. [PMC free article] [PubMed] [Google Scholar]
- 17.Glance LG, Wissler R, Mukamel DB, et al. Perioperative outcomes among patients with the modified metabolic syndrome who are undergoing noncardiac surgery. Anesthesiology. 2010;113:859–872. doi: 10.1097/ALN.0b013e3181eff32e. [DOI] [PubMed] [Google Scholar]
- 18.Namba RS, Paxton L, Fithian DC, Stone ML. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplasty. 2005;20:46–50. doi: 10.1016/j.arth.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 19.Merkow RP, Bilimoria KY, McCarter MD, Bentrem DJ. Effect of body mass index on short-term outcomes after colectomy for cancer. J Am Coll Surg. 2009;208:53–61. doi: 10.1016/j.jamcollsurg.2008.08.032. [DOI] [PubMed] [Google Scholar]
- 20.Suleiman LI, Ortega G, Ong’uti SK, et al. Does BMI affect perioperative complications following total knee and hip arthroplasty? J Surg Res. 2012;174:7–11. doi: 10.1016/j.jss.2011.05.057. [DOI] [PubMed] [Google Scholar]
- 21.Mullen JT, Moorman DW, Davenport DL. The obesity paradox: Body mass index and outcomes in patients undergoing nonbariatric general surgery. Ann Surg. 2009;250:166–172. doi: 10.1097/SLA.0b013e3181ad8935. [DOI] [PubMed] [Google Scholar]
- 22.Jain NB, Guller U, Pietrobon R, et al. Comorbidities increase complication rates in patients having arthroplasty. Clin Orthop Relat Res. 2005:232–238. doi: 10.1097/01.blo.0000156479.97488.a2. [DOI] [PubMed] [Google Scholar]
- 23.Silber JH, Rosenbaum PR, Even-Shoshan O, et al. Estimating anesthesia time using the Medicare claim: A validation study. Anesthesiology. 2011;115:322–333. doi: 10.1097/ALN.0b013e31821d6c81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Silber JH, Rosenbaum PR, Trudeau ME, et al. Multivariate matching and bias reduction in the surgical outcomes study. Med Care. 2001;39:1048–1064. doi: 10.1097/00005650-200110000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Rosenbaum PR. Design of Observational Studies. New York: Springer; 2010. [Google Scholar]
- 26.Silber JH, Rosenbaum PR, Polsky D, et al. Does ovarian cancer treatment and survival differ by the specialty providing chemotherapy? J Clin Oncol. 2007;25:1169–1175. doi: 10.1200/JCO.2006.08.2933. [DOI] [PubMed] [Google Scholar]
- 27.Silber JH, Rosenbaum PR, Trudeau ME, et al. Preoperative antibiotics and mortality in the elderly. Ann Surg. 2005;242:107–114. doi: 10.1097/01.sla.0000167850.49819.ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silber JH, Lorch SA, Rosenbaum PR, et al. Time to send the preemie home? Additional maturity at discharge and subsequent healthcare costs and outcomes. Health Serv Res. 2009;44:444–463. doi: 10.1111/j.1475-6773.2008.00938.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 30.Silber JH, Rosenbaum PR, Trudeau ME, et al. Changes in prognosis after the first postoperative complication. Med Care. 2005;43:122–131. doi: 10.1097/00005650-200502000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Knaus WA, Wagner DP, Draper EA, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100:1619–1636. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- 32.Rosenbaum PR, Ross RN, Silber JH. Minimum distance matched sampling with fine balance in an observational study of treatment for ovarian cancer. J Am Stat Assoc. 2007;102:75–83. [Google Scholar]
- 33.Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. 1985;39:33–38. [Google Scholar]
- 34.Hansen BB. The prognostic analogue of the propensity score. Biometrika. 2008;95:481–488. [Google Scholar]
- 35. [Accessed April 4, 2011.];Research Data Assistance Center. Available at: http://www.resdac.umn.edu.
- 36.Lave JR, Pashos CL, Anderson GF, et al. Costing medical care: Using Medicare administrative data. Med Care. 1994;32:JS77–89. [PubMed] [Google Scholar]
- 37.Wilson LS, Lightwood JM. Pancreatic cancer: Total costs and utilization of health services. J Surg Oncol. 1999;71:171–181. doi: 10.1002/(sici)1096-9098(199907)71:3<171::aid-jso7>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 38.Halpern NA, Pastores SM. Critical care medicine in the United States 2000–2005: An analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010;38:65–71. doi: 10.1097/CCM.0b013e3181b090d0. [DOI] [PubMed] [Google Scholar]
- 39.Chatterjee A, Chen L, Goldenberg EA, et al. Opportunity cost in the evaluation of surgical innovations: A case study of laparoscopic versus open colectomy. Surg Endosc. 2010;24:1075–1079. doi: 10.1007/s00464-009-0728-4. [DOI] [PubMed] [Google Scholar]
- 40.Bamezai A, Melnick G, Nawathe A. The cost of an emergency department visit and its relationship to emergency department volume. Ann Emerg Med. 2005;45:483–490. doi: 10.1016/j.annemergmed.2004.08.029. [DOI] [PubMed] [Google Scholar]
- 41.Hollander M, Wolfe DA. Nonparametric Statistical Methods. 2. New York, NY: John Wiley & Sons; 1999. [Google Scholar]
- 42.Bishop YMM, Fienberg SE, Holland PW. Discrete Multivariate Analysis: Theory and Practice. Cambridge: The MIT Press; 1975. Chapter 8: Analysis of Square Tables: Symmetry and Marginal Homogeneity; pp. 281–286. [Google Scholar]
- 43.O’Brien PC, Fleming TR. A paired Prentice-Wilcoxon test for censored paired data. Biometrics. 1987;43:169–180. [Google Scholar]
- 44.Volpp KG, Rosen AK, Rosenbaum PR, et al. Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298:975–983. doi: 10.1001/jama.298.9.975. [DOI] [PubMed] [Google Scholar]
- 45.Volpp KG, Rosen AK, Rosenbaum PR, et al. Mortality among patients in VA hospitals in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298:984–992. doi: 10.1001/jama.298.9.984. [DOI] [PubMed] [Google Scholar]
- 46.Silber JH, Rosenbaum PR, Romano PS, et al. Hospital teaching intensity, patient race, and surgical outcomes. Arch Surg. 2009;144:113–121. doi: 10.1001/archsurg.2008.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 48.Naylor M, Keating SA. Transitional care. Am J Nurs. 2008;108:58–63. doi: 10.1097/01.NAJ.0000336420.34946.3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized clinical trial. JAMA. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 50.Naylor MD, Brooten DA, Campbell RL, et al. Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. J Am Geriatr Soc. 2004;52:675–684. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.