Abstract
Recombinant influenza A(H1N1)pdm09 wild-type (WT) and zanamivir-resistant E119G and Q136K neuraminidase mutants were generated to determine their enzymatic and replicative properties in vitro, as well as their infectivity and transmissibility in mice and ferrets. Viral titers of recombinant E119G and Q136K mutants were significantly lower than those of the WT in the first 36 h postinoculation (p.i.) in vitro. The E119G and Q136K mutations were both associated with a significant reduction of total neuraminidase (NA) activity at the cell surface of 293T cells, with relative total NA activities of 14% (P < 0.01) and 20% (P < 0.01), respectively, compared to the WT. The E119G mutation significantly reduced the affinity (8-fold increase in Km) but not the Vmax. The Q136K mutation increased the affinity (5-fold decrease in Km) with a reduction in Vmax (8% Vmax ratio versus the WT). In mice, infection with the E119G and Q136K mutants resulted in lung viral titers that were significantly lower than those of the WT on days 3 p.i. (3.4 × 106 ± 0.8 × 106 and 2.1 × 107 ± 0.4 × 107 PFU/ml, respectively, versus 8.8 × 107 ± 1.1 × 107; P < 0.05) and 6 p.i. (3.0 × 105 ± 0.5 × 105 and 8.6 × 105 ± 1.4 ×105 PFU/ml, respectively, versus 5.8 × 107 ± 0.3 × 107; P < 0.01). In experimentally infected ferrets, the E119G mutation rapidly reverted to the WT in donor and contact animals. The Q136K mutation was maintained in ferrets, although nasal wash viral titers from the Q136K contact group were significantly lower than those of the WT on days 3 to 5 p.i. Our results demonstrate that zanamivir-resistant E119G and Q136K mutations compromise viral fitness and transmissibility in A(H1N1)pdm09 viruses.
INTRODUCTION
Anovel influenza A/H1N1 virus emerged in Mexico in April 2009, and it has since spread worldwide to cause the first influenza pandemic of the 21st century. Phylogenetic studies demonstrated that the A(H1N1)pdm09 virus resulted from a series of reassortment events involving human, swine, and avian influenza A virus strains, with the neuraminidase (NA) gene originating from an avian-like Eurasian swine A/H1N1 lineage (1). Given the ancestral origin of the A(H1N1)pdm09 NA gene, the in vitro and in vivo behavior of A(H1N1)pdm09 variants containing mutations of resistance to NA inhibitors (NAIs) could be different than those of prior seasonal A/H1N1 viruses.
At present, little information regarding zanamivir resistance is available for A(H1N1)pdm09 viruses, which is probably related to the fact that mutations conferring highly reduced susceptibility to zanamivir have not yet emerged among clinical A(H1N1)pdm09 isolates. The aim of this study was to evaluate, in the A(H1N1)pdm09 background, the impact of certain NA mutations previously associated with reduced susceptibility to zanamivir in influenza A virus variants of the N1 and N2 subtypes. We were particularly interested in two NA mutations, E119G and Q136K, which were reported to confer highly reduced susceptibility to zanamivir. The E119G mutation occurred in both influenza A/Vietnam/1203/2004 and A/Chicken/Laos/26/2006 H5N1 viruses under zanamivir pressure in vitro, and this variant showed a 1,400-fold increase in zanamivir 50% inhibitory concentration (IC50) but remained susceptible to oseltamivir (2). The Q136K mutation was recently described in clinical samples of influenza A/H3N2 circulating in 2007 and 2008 in Myanmar, exhibiting 30- to 50-fold increases in zanamivir IC50 (3). This substitution has also been reported in seasonal A/H1N1 viruses isolated between 2006 and 2008 in Australia and southeast Asia, although its clinical relevance is debatable, since the mutation could not be detected in the primary clinical specimens (4).
Given the importance of determining whether the zanamivir-resistant variants retain their fitness and pathogenicity, we generated by reverse genetics a recombinant A(H1N1)pdm09 wild-type (WT) virus and two (E119G and Q136K) variants and compared their enzymatic and replicative properties in vitro, as well as their infectivity and transmissibility in mice and ferrets.
MATERIALS AND METHODS
Generation of recombinant viruses.
A recombinant influenza A(H1N1)pdm09 wild-type (WT) virus, as well as two NA mutants (E119G and Q136K), were generated from the A/Québec/144147/09 virus (GenBank accession numbers FN434457 to FN434464) by reverse genetics and site-directed mutagenesis as previously described (5). The recombinant viruses were amplified and subsequently titrated by standard plaque assays in ST6GalI Madin-Darby canine kidney (ST6GalI-MDCK) cells overexpressing the α2,6 sialic acid receptors, which were kindly provided by Y. Kawaoka from the University of Wisconsin, Madison, WI (6).
Drug susceptibility assays.
The NAI susceptibilities of the three recombinant viruses were determined by NA inhibition assays as described elsewhere (7), with minor modifications. Viruses were standardized to an NA activity level 10-fold higher than that of the background, as measured by the production of a fluorescent product from the 2′-(4-methylumbelliferyl)-α-d-N-acetylneuraminic acid (MUNANA; Sigma, St. Louis, MO) substrate. The drug susceptibility profiles were determined by the extent of NA inhibition after incubation with serial 3-fold dilutions of the drug oseltamivir carboxylate (Hoffmann-La Roche, Basel, Switzerland) or zanamivir (GlaxoSmithKline, Stevenage, United Kingdom) at final concentrations between 0 and 1,800 nM. The IC50s were determined from the dose-response curve.
In vitro replication assays.
Replicative capacities of the recombinant viruses were evaluated by infecting ST6GalI-MDCK cells at a multiplicity of infection (MOI) of 0.001 plaque-forming units (PFU)/cell in 12-well plates (8). Supernatants were collected at 12, 24, 36, 48, 60, and 72 h postinfection and titrated by plaque assays. The mean viral plaque area of recombinant viruses was determined from a minimum of 20 plaques obtained after 60 h of incubation under agarose overlay using ImageJ software (version 1.41), developed by Wayne Rasband of the National Institutes of Health, as previously described (5).
Enzymatic assays.
To measure the total NA enzymatic activity per infectious virus, fluorometric assays were conducted using MUNANA as the substrate. Briefly, all recombinant viruses were standardized to an equivalent dose of 106.5 PFU/ml and incubated at 37°C in 50-μl reaction mixtures with different concentrations (from 0 to 3,000 μM) of MUNANA (9). Fluorescence was monitored every 90 s for 53 min (35 measurements). The Michaelis constant (Km) and the maximum velocity (Vmax) were calculated by nonlinear regression with Prism software (version 5; GraphPad).
Cell surface NA activity.
Recombinant WT and mutant (E119G and Q136K) NA proteins were expressed in 293T cells by cotransfection with the pLLBA-NA and pCAGGS-PA, -PB1, -PB2, and -NP plasmids (10). The empty pLLBA and pLLBA-HA plasmids were used as mock and negative controls, respectively. Twenty-four h posttransfection, the cells were briefly treated with 0.02% EDTA in phosphate-buffered saline (PBS) and neutralized by the addition of 2% fetal bovine serum. Cells were subsequently centrifuged at 3,000 rpm for 5 min, washed twice with PBS, and resuspended in a nonlysing buffer (15 mM morpholinepropanesulfonic acid, 145 mM sodium chloride, 2.7 mM potassium chloride, 4 mM calcium chloride, adjusted to pH 7.4) to be used in an NA assay with MUNANA as the substrate. Final values were normalized by the fluorescence of cells transfected with the empty pLLBA plasmid.
Mouse studies.
Three groups of 12 (18 to 22 g) female BALB/c mice (Charles River, Lasalle, Quebec City, Canada) were housed 4 per cage and kept under conditions that prevented cage-to-cage infections. Mice were inoculated intranasally under isoflurane anesthesia with 104 PFU of the recombinant WT, E119G, or Q136K virus. Another group of mice was kept as uninfected controls. All mice were monitored daily for weight loss during 12 days, and four mice per group were sacrificed on days 3 and 6 p.i. for determination of lung viral titers (LVTs) by plaque assays in ST6GalI-MDCK cells.
Ferret studies.
Three groups of four seronegative (800 to 1,200 g) male ferrets (Marshall BioResources, North Rose, NY) housed in individual cages were lightly anesthetized by isoflurane and received an intranasal instillation of 105.2 PFU of one of the recombinant viruses. Donor-contact animal pairs were established by placing a naïve ferret into each cage 24 h after inoculation of the donor ferret (11). Weight, temperature, and clinical signs were monitored daily. Nasal wash samples were collected from donor animals on days 1 to 8 p.i. (24 h later from contacts) with 5 ml of PBS containing 2% bovine serum albumin and then immediately stored at −80°C. Virus titers in nasal wash samples were determined by plaque assays in ST6GalI-MDCK cells. Serum samples were collected from each ferret before intranasal infection (day 0) and on day 14 p.i. to evaluate specific antibody levels against the A/Québec/144147/09 strain using standard hemagglutination inhibition (HAI) assays with 0.7% turkey red blood cells. Animals were sacrificed on day 14 p.i.
All animal procedures were approved by the Institutional Animal Care Committee of Laval University according to the guidelines of the Canadian Council on Animal Care.
Sequencing.
NA genes of viruses recovered from in vitro replication assays, and mouse lung homogenates and ferret nasal wash samples were amplified and sequenced using the ABI 3730xl DNA Analyzer (Applied Biosystems, Carlsbad, CA) to confirm both the presence of the desired mutations and the absence of additional mutations.
Statistical analyses.
Viral titers, plaque sizes, NA kinetic parameters, and body weight loss were compared by one-way analysis of variance (ANOVA) with Tukey's multiple-comparison posttest. The amount of NA activity at the cell surface for each mutant protein was compared to that of the WT by the use of unpaired two-tailed t tests.
RESULTS
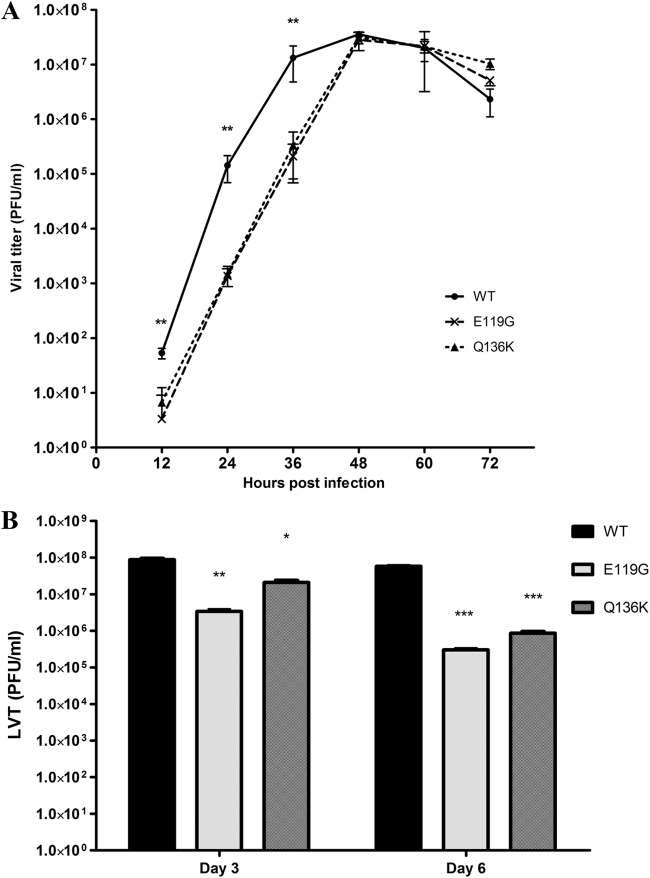
In NA inhibition assays, both E119G and Q136K mutant viruses remained susceptible to oseltamivir but showed a highly reduced susceptibility profile to zanamivir, with 821- and 749-fold increases in IC50s, respectively, compared to the recombinant WT virus (Table 1). In enzymatic assays, the E119G mutation significantly reduced the affinity (8-fold increase in Km versus the WT; P < 0.01) but not the Vmax. The Q136K mutation increased the affinity (5-fold decrease in Km versus the WT; P < 0.01) with a reduction of Vmax (8% Vmax ratio versus the WT; P < 0.01). Also, using recombinant NA proteins expressed in 293T cells, we observed that the E119G and Q136K mutants were both associated with a significant reduction of total NA activity at the cell surface, with relative total NA activities of 14% (P < 0.01) and 20% (P < 0.01), respectively, compared to the WT protein (Fig. 1).
Table 1.
Neuraminidase properties of the recombinant pandemic A/Québec/144147/09 viruses
| Virus | IC50a (nM [ratio]) of: |
Kma (μM [ratio]) | Vmaxa (U/s [ratio]) | Plaque areab (mm2) | |
|---|---|---|---|---|---|
| Oseltamivir | Zanamivir IC50a nM [ratio]) | ||||
| WT | 0.46 ± 0.02 (1) | 0.15 ± 0.01 (1) | 80.9 ± 17.5 (1) | 269.9 ± 4.3 (1) | 0.50 ± 0.13 |
| E119G | 1.52 ± 0.13 (3.3) | 123.1 ± 21.7 (821) | 690.2 ± 37.3 (8.5) | 238.1 ± 6.6 (0.9) | 0.33 ± 0.11* |
| Q136K | 0.08 ± 0.01 (0.2) | 112.3 ± 15.8 (749) | 16.6 ± 0.9 (0.2) | 20.5 ± 3.5 (0.1) | 0.42 ± 0.14 |
Values indicate means ± standard deviations from 3 experiments. Ratios are from comparisons to the recombinant wild-type (WT) virus.
Values indicate means ± standard deviations from 20 measures. *, P < 0.05 compared to the WT virus by one-way ANOVA.
Fig 1.
Cell surface activity of recombinant A/Québec/144147/09 neuraminidase (NA) proteins. Recombinant WT and mutant (E119G and Q136K) NA proteins were expressed in 293T cells. The empty pLLBA and pLLBA-HA plasmids were used as mock and negative controls, respectively. Twenty-four h posttransfection, the cells were briefly treated and resuspended in a nonlysing buffer to be used in an NA assay with MUNANA as the substrate. Final values were normalized by the fluorescence of cells transfected with the empty pLLBA plasmid. The mean values for three experiments ± standard deviations are shown (**, P < 0.01).
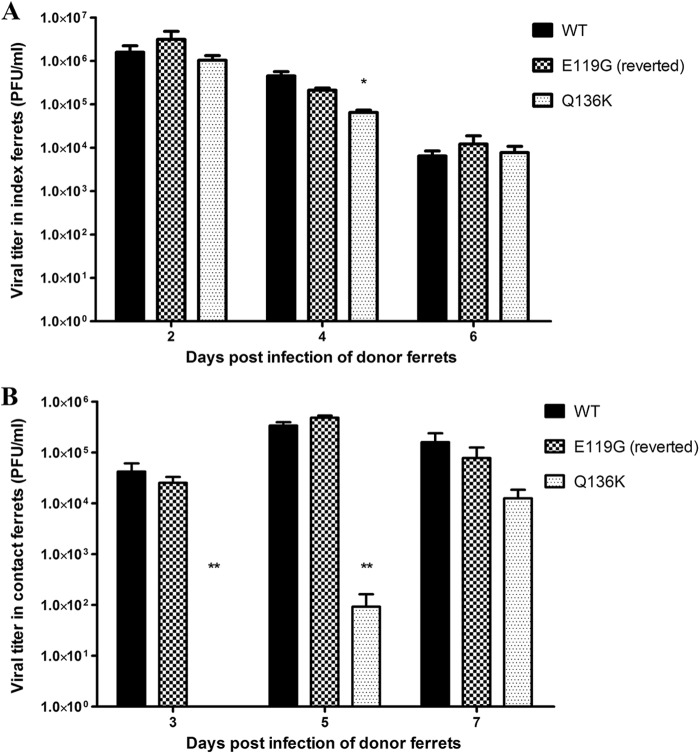
Replicative capacities in ST6GalI-MDCK cells showed that viral titers of the E119G and Q136K mutants were significantly lower than those of the WT in the first 36 h p.i., although similar peak titers (2.8 × 107 ± 0.5 × 107, 3.2 × 107 ± 0.8 × 107, and 3.6 × 107 ± 0.4 × 107 PFU/ml, respectively) were achieved for the three viruses at 48 h p.i. (Fig. 2A). The E119G mutant exhibited plaques significantly smaller than those of the WT (0.33 ± 0.11 versus 0.50 ± 0.13 mm2; P < 0.01), but there were no significant differences between the Q136K (0.42 ± 0.14 mm2) and the WT strains (Table 1). No unexpected mutations were found in viruses recovered at 36 or 72 h p.i.
Fig 2.
Replicative capacities of recombinant wild-type (WT), E119G, and Q136K A/Québec/144147/09 viruses in vitro and in vivo. (A) Confluent ST6Gal1-MDCK cells were infected with recombinant viruses at a multiplicity of infection (MOI) of 0.001 PFU/cell. Supernatants were harvested at 12, 24, 36, 48, 60, and 72 h postinfection and titrated by standard plaque assays. (B) Groups of 12 mice were inoculated intranasally with 104 PFU of the recombinant WT, E119G, or Q136K virus. Another group of mice was kept as an uninfected control (not shown). Four mice per group were sacrificed on day 3 and 6 p.i. for determination of lung viral titers (LVTs) by plaque assays in ST6GalI-MDCK cells. The mean values for three experiments ± standard deviations are shown (*, P < 0.05; **, P < 0.01; ***, P < 0.001).
No mortality was observed after intranasal inoculation of mice with 104 PFU of the recombinant WT, E119G, or Q136K virus. Also, no significant differences in body weight loss were observed among the three groups of infected mice, with maximal values of 7.0% ± 1.1%, 5.9% ± 0.8%, and 5.8% ± 0.9%, respectively, obtained on day 5 p.i. However, mean LVTs for the E119G and Q136K mutant groups were significantly lower than those of the WT group on days 3 p.i. (3.4 × 106 ± 0.8 × 106 and 2.1 × 107 ± 0.4 × 107 PFU/ml, respectively, versus 8.8 × 107 ± 1.1 × 107; P < 0.05) and 6 p.i. (3.0 × 105 ± 0.5 × 105 and 8.6 × 105 ± 1.4 × 105 PFU/ml, respectively, versus 5.8 × 107 ± 0.3 × 107; P < 0.001) (Fig. 2B). No unexpected mutations were found in viruses recovered from lung homogenates.
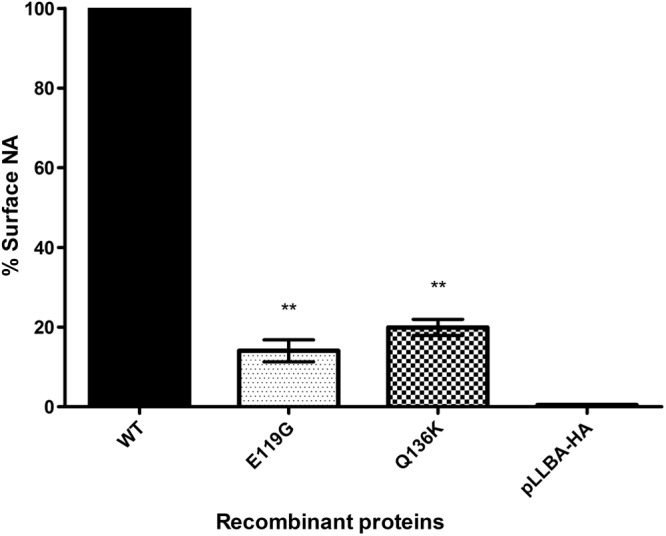
Inoculation of ferrets with 105.2 PFU of the recombinant WT, E119G, or Q136K virus yielded only mild clinical signs, and no significant differences in body weight loss (4.3% ± 1.2%, 3.8% ± 0.7%, and 3.3% ± 0.6%, respectively) or temperature were observed between groups. Interestingly, mean viral titers in nasal wash samples collected on days 2, 4, and 6 p.i. were comparable between the recombinant WT and E119G mutant donor groups, ranging from 1.6 × 106 ± 0.7 × 106 to 3.1 × 106 ± 1.7 × 106 PFU/ml (day 2), 4.6 × 105 ± 2.2 × 105 to 2.1 × 105 ± 0.4 × 105 PFU/ml (day 4), and 6.5 × 103 ± 3.8 × 103 to 7.8 × 103 ± 6.1 × 103 PFU/ml (day 6) (Fig. 3A). In contrast, the Q136K group showed significantly reduced viral titers on day 4 (6.5 × 104 ± 1.7 × 104 PFU/ml; P < 0.05) but not on days 2 (1.0 × 106 ± 0.6 × 106 PFU/ml) and 6 (7.7 × 103 ± 6.1 ×103 PFU/ml) p.i.
Fig 3.
Viral titers in nasal washes of ferrets infected with recombinant wild-type (WT), E119G, and Q136K A/Québec/144147/09 viruses. Groups of 4 ferrets were infected with 250 μl of PBS containing 105.2 PFU of the recombinant WT, E119G, or Q136K variant. Donor-contact pairs were established 24 h postinfection. Mean viral titers ± standard deviations in nasal wash samples of donor (A) and direct-contact (B) ferrets were determined by standard plaque assays in ST6Gal1-MDCK cells (*, P < 0.05; **, P < 0.01). The E119G mutation reverted to the WT genotype in all four donor and contact ferrets as soon as day 2 p.i.
All contact ferrets seroconverted for A/Québec/144147/09 with HAI reciprocal geometric mean titers of >1,280, compared to <10 on day 0. However, mean viral titers in nasal wash samples obtained from contact ferrets of the Q136K group were significantly lower than those of the recombinant WT and E119G groups on days 3 (<101 versus 4.2 × 104 ± 3.3 × 104 and 2.5 × 104 ± 1.4 × 104 PFU/ml; P < 0.01) and 5 p.i. (9.2 × 101 ± 6.9 × 101 versus 3.4× 105 ± 1.0 × 105 and 4.8 ± 0.9 × 105 PFU/ml; P < 0.01), respectively, but not on day 7 p.i. (1.3 × 104 ± 0.9 × 104 versus 1.6 × 105 ± 1.5 × 105 and 7.8 × 104 ± 6.5 × 104 PFU/ml) (Fig. 3B). Sequence analysis of the NA gene in nasal wash samples of ferrets confirmed the presence of the Q136K mutation in the respective donor and contact groups, in contrast to the E119G mutation, which reverted to the WT genotype. Indeed, mixed 119E/G viral populations with an approximate 80:20 ratio were detected in the four donor ferrets of the E119G group on day 2 p.i. At all subsequent time points, only the E119 genotype was detected in the four donor and contact ferrets.
DISCUSSION
Although the active site of the NA enzyme, which is the target of NAIs, is highly conserved, NAI-resistant influenza variants have been reported to contain different NA mutations that vary depending of the NA subtype as well as the inhibitor (12). In addition, we previously showed that the main mutation of resistance to oseltamivir (H275Y) affected differently the viral fitness of old and recent A/H1N1 viruses (13). As for seasonal A/H1N1 viruses, A(H1N1)pdm09 viruses harboring the H275Y NA mutation were found to confer resistance to oseltamivir but remained susceptible to zanamivir (5). Interestingly, we and others have reported that the replication and contact transmission of these oseltamivir-resistant A(H1N1)pdm09 H275Y variants were comparable to those of the WT virus in ferrets. However, there are contradictory data on the aerosol transmissibility of the H275Y mutant (11, 14, 15).
In contrast to oseltamivir resistance studies, little information is available on resistance to zanamivir in influenza A/H1N1 viruses in general and specifically in the A(H1N1)pdm09 background. Although mutations conferring resistance to zanamivir have not emerged among clinical A(H1N1)pdm09 isolates, we sought to anticipate such an event. In a previous study, we generated a series of recombinant A(H1N1)pdm09 viruses containing NA mutations previously found in other viral backgrounds, with one of them (E119G) being associated with highly reduced susceptibility to zanamivir (5). In the present work, we also generated the Q136K NA mutant and analyzed the enzymatic and in vitro replicative properties, as well as the infectivity and transmissibility, of both recombinant E119G and Q136K variants in mice and ferrets.
Substitutions at residue E119 (G, D, A, and V) were previously reported in drug-resistant variants of influenza A/H3N2 in clinical virus (E119V) and also in A/H1N9, A/H3N2, and B viruses after passages in the presence of zanamivir (12). Interestingly, the E119G mutation was also described in prototypic influenza A/H5N1 viruses from clades 1 and 2.3 under zanamivir pressure in vitro. These variants showed a zanamivir-resistant phenotype but remained susceptible to oseltamivir (2). The carboxylate of the E119 side chain interacts with the 4-guanidino group on zanamivir, and the loss of this interaction in the E119G mutant results in a reduced binding of zanamivir (16). As peramivir and laninamivir also have a guanidine group, the E119G mutation would also confer cross-resistance to these two NAIs but not to oseltamivir, which possesses an acetamide group at that position. Accordingly, our A(H1N1)pdm09 E119G variant was resistant to zanamivir and peramivir and remained susceptible to oseltamivir (5). Susceptibility to laninamivir could not be tested in this study.
The Q136K mutation was previously described in two influenza A/H3N2 viruses isolated in Myanmar in 2007 and 2008 (3). In that report, the presence of this mutation was also confirmed in primary clinical samples (nasopharyngeal swabs). The Q136K mutation was further identified in seasonal influenza A/H1N1 viruses isolated between 2006 and 2008 in Australia and southeast Asia (4). In that case, however, the mutation could not be detected in primary clinical samples, suggesting either the presence of this variant at a very low proportion before cell culture amplification or its generation as an artifact due to in vitro passages in MDCK cells. Later, pyrosequencing analysis of a set of matching clinical samples and virus isolates submitted to the WHO supported the hypothesis that propagation of human seasonal A/H1N1 viruses in MDCK cells can lead to the emergence of variants carrying mutations of resistance to NAIs, such as Q136K (17). It is worth nothing that Hurt et al. (18) described the recovery of a Q136L NA mutant from nasal wash samples of a ferret infected with influenza A/Vietnam/1203/2004 (H5N1) and treated with zanamivir. This variant showed 350- and 26-fold increases in zanamivir and oseltamivir IC50s, respectively. Thus, at this time, the clinical relevance of the Q136K NA mutation is still questionable.
In the present work, the replication of the two mutant viruses with highly reduced susceptibility to zanamivir was impaired in ST6GalI-MDCK cells, as well as in mice, compared to that of the recombinant WT virus. The reduced total NA activity at the cell surface of both mutants can account for this phenomenon, although we cannot distinguish if it was due to either a loss of NA enzymatic activity, decreased levels of folded NA protein on the cell surface, or a combination of both factors. Interestingly, a recent paper by Kaminski et al. (19) showed that the Q136K mutant had reduced numbers of NA molecules in viral particles as well as reduced intrinsic enzymatic activity compared to the WT. Furthermore, the Q136K mutant showed reduced replication and delayed contact transmissibility in our ferret model, in contrast to a previous report using A/Philippines/1279/2006 (H1N1) viruses (4). In that regard, A/Philippines/1279/2006 is a seasonal A/H1N1 virus, whereas the recombinant A/Québec/144147/2009 used in this study is a 2009 pandemic A/H1N1 strain. Such important structural and functional differences between the two NA proteins may explain the differential effects on enzymatic activity and viral fitness.
The Q136K mutation was maintained after its passage in ferrets, unlike the E119G mutation, which reverted rapidly to the WT genotype, explaining the comparable viral fitness and transmissibility of the WT and E119G groups. Therefore, the A(H1N1)pdm09 virus with the E119G NA mutation was severely compromised in the ferret model, which could be attributed to a significant reduction of NA activity expressed at the cell surface. Moreover, the crystallographic structure of the NA protein of the N9 subtype revealed a salt bridge between E119 and R156 (20). It was suggested that the E119G mutation could then lead to the instability of the NA tetramers. In a previous reverse genetics study, we failed to rescue the A/WSN/33 (H1N1) E119G variant despite many attempts (21). Similarly, the E119G recombinant A/Victoria/3/75 (H3N2) variant could only be rescued in the presence of exogenous NA (22). In that study, the E119G mutant also reverted to the WT genotype after one passage in MDCK cells. In the avian A/H5N1 background, the E119G mutant was also associated with a significant decrease of infectivity in MDCK cells (2). Finally, in vitro passaging of an A(H1N1)pdm09 virus in the presence of zanamivir failed to select for mutations of resistance (23).
In conclusion, our study demonstrates that, in the A(H1N1)pdm09 genetic context and similarly to other genetic backgrounds, NA mutations conferring high levels of resistance to zanamivir alter enzymatic properties to a level that significantly compromises viral viability and transmissibility. This may help to explain the very low frequency of these mutations, particularly in the N1 subtype. However, the fitness of the E119G and Q136K mutants will need to be reevaluated if they emerge in different viral backgrounds, especially when found in clinical samples.
ACKNOWLEDGMENTS
This work was supported by a grant from the Canadian Institutes of Health Research (no. 230187) and GlaxoSmithKline Canada.
G.B. is the holder of the Canada Research Chair on emerging viruses and antiviral resistance and is also the Canadian pandemic team leader on antiviral resistance and molecular evolution.
Footnotes
Published ahead of print 28 January 2013
REFERENCES
- 1. Garten RJ, Davis CT, Russell CA, Shu B, Lindstrom S, Balish A, Sessions WM, Xu X, Skepner E, Deyde V, Okomo-Adhiambo M, Gubareva L, Barnes J, Smith CB, Emery SL, Hillman MJ, Rivailler P, Smagala J, de Graaf M, Burke DF, Fouchier RA, Pappas C, Alpuche-Aranda CM, Lopez-Gatell H, Olivera H, Lopez I, Myers CA, Faix D, Blair PJ, Yu C, Keene KM, Dotson PD, Jr, Boxrud D, Sambol AR, Abid SH, St. George K, Bannerman T, Moore AL, Stringer DJ, Blevins P, Demmler-Harrison GJ, Ginsberg M, Kriner P, Waterman S, Smole S, Guevara HF, Belongia EA, Clark PA, Beatrice ST, Donis R, Katz J, Finelli L, Bridges CB, Shaw M, Jernigan DB, Uyeki TM, Smith DJ, Klimov AI, Cox NJ. 2009. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science 325:197–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hurt AC, Holien JK, Barr IG. 2009. In vitro generation of neuraminidase inhibitor resistance in A(H5N1) influenza viruses. Antimicrob. Agents Chemother. 53:4433–4440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dapat C, Suzuki Y, Saito R, Kyaw Y, Myint YY, Lin N, Oo HN, Oo KY, Win N, Naito M, Hasegawa G, Dapat IC, Zaraket H, Baranovich T, Nishikawa M, Saito T, Suzuki H. 2010. Rare influenza A (H3N2) variants with reduced sensitivity to antiviral drugs. Emerg. Infect. Dis. 16:493–496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hurt AC, Holien JK, Parker M, Kelso A, Barr IG. 2009. Zanamivir-resistant influenza viruses with a novel neuraminidase mutation. J. Virol. 83:10366–10373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pizzorno A, Bouhy X, Abed Y, Boivin G. 2011. Generation and characterization of recombinant pandemic influenza A(H1N1) viruses resistant to neuraminidase inhibitors. J. Infect. Dis. 203:25–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hatakeyama S, Sakai-Tagawa Y, Kiso M, Goto H, Kawakami C, Mitamura K, Sugaya N, Suzuki Y, Kawaoka Y. 2005. Enhanced expression of an alpha2,6-linked sialic acid on MDCK cells improves isolation of human influenza viruses and evaluation of their sensitivity to a neuraminidase inhibitor. J. Clin. Microbiol. 43:4139–4146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Potier M, Mameli L, Belisle M, Dallaire L, Melancon SB. 1979. Fluorometric assay of neuraminidase with a sodium (4-methylumbelliferyl-alpha-d-N-acetylneuraminate) substrate. Anal. Biochem. 94:287–296 [DOI] [PubMed] [Google Scholar]
- 8. Pizzorno A, Abed Y, Bouhy X, Beaulieu E, Mallett C, Russell R, Boivin G. 2012. Impact of mutations at residue I223 of the neuraminidase protein on the resistance profile, replication level, and virulence of the 2009 pandemic influenza virus. Antimicrob. Agents Chemother. 56:1208–1214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yen HL, Ilyushina NA, Salomon R, Hoffmann E, Webster RG, Govorkova EA. 2007. Neuraminidase inhibitor-resistant recombinant A/Vietnam/1203/04 (H5N1) influenza viruses retain their replication efficiency and pathogenicity in vitro and in vivo. J. Virol. 81:12418–12426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Abed Y, Pizzorno A, Bouhy X, Boivin G. 2011. Role of permissive neuraminidase mutations in influenza A/Brisbane/59/2007-like (H1N1) viruses. PLoS Pathog. 7:e1002431 doi:10.1371/journal.ppat.1002431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hamelin ME, Baz M, Abed Y, Couture C, Joubert P, Beaulieu E, Bellerose N, Plante M, Mallett C, Schumer G, Kobinger GP, Boivin G. 2010. Oseltamivir-resistant pandemic A/H1N1 virus is as virulent as its wild-type counterpart in mice and ferrets. PLoS Pathog. 6:e1001015 doi:10.1371/journal.ppat.1001015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pizzorno A, Abed Y, Boivin G. 2011. Influenza drug resistance. Semin. Respir. Crit. Care Med. 32:409–422 [DOI] [PubMed] [Google Scholar]
- 13. Baz M, Abed Y, Simon P, Hamelin ME, Boivin G. 2010. Effect of the neuraminidase mutation H274Y conferring resistance to oseltamivir on the replicative capacity and virulence of old and recent human influenza A(H1N1) viruses. J. Infect. Dis. 201:740–745 [DOI] [PubMed] [Google Scholar]
- 14. Memoli MJ, Davis AS, Proudfoot K, Chertow DS, Hrabal RJ, Bristol T, Taubenberger JK. 2011. Multidrug-resistant 2009 pandemic influenza A(H1N1) viruses maintain fitness and transmissibility in ferrets. J. Infect. Dis. 203:348–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hurt AC, Chotpitayasunondh T, Cox NJ, Daniels R, Fry AM, Gubareva LV, Hayden FG, Hui DS, Hungnes O, Lackenby A, Lim W, Meijer A, Penn C, Tashiro M, Uyeki TM, Zambon M. 2012. Antiviral resistance during the 2009 influenza A H1N1 pandemic: public health, laboratory, and clinical perspectives. Lancet Infect. Dis. 12:240–248 [DOI] [PubMed] [Google Scholar]
- 16. Smith BJ, McKimm-Breshkin JL, McDonald M, Fernley RT, Varghese JN, Colman PM. 2002. Structural studies of the resistance of influenza virus neuraminidase to inhibitors. J. Med. Chem. 45:2207–2212 [DOI] [PubMed] [Google Scholar]
- 17. Okomo-Adhiambo M, Nguyen HT, Sleeman K, Sheu TG, Deyde VM, Garten RJ, Xu X, Shaw MW, Klimov AI, Gubareva LV. 2010. Host cell selection of influenza neuraminidase variants: implications for drug resistance monitoring in A(H1N1) viruses. Antiviral Res. 85:381–388 [DOI] [PubMed] [Google Scholar]
- 18. Hurt AC, Lowther S, Middleton D, Barr IG. 2010. Assessing the development of oseltamivir and zanamivir resistance in A(H5N1) influenza viruses using a ferret model. Antiviral Res. 87:361–366 [DOI] [PubMed] [Google Scholar]
- 19. Kaminski MM, Ohnemus A, Staeheli P, Rubbenstroth D. 2013. Pandemic 2009 H1N1 influenza A virus carrying a Q136K mutation in the neuraminidase gene is resistant to zanamivir but exhibits reduced fitness in the guinea pig transmission model. J. Virol. 87:1912–1915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Colacino JM, Chirgadze NY, Garman E, Murti KG, Loncharich RJ, Baxter AJ, Staschke KA, Laver WG. 1997. A single sequence change destabilizes the influenza virus neuraminidase tetramer. Virology 236:66–75 [DOI] [PubMed] [Google Scholar]
- 21. Abed Y, Goyette N, Boivin G. 2004. A reverse genetics study of resistance to neuraminidase inhibitors in an influenza A/H1N1 virus. Antivir. Ther. 9:577–581 [PubMed] [Google Scholar]
- 22. Zurcher T, Yates PJ, Daly J, Sahasrabudhe A, Walters M, Dash L, Tisdale M, McKimm-Breschkin JL. 2006. Mutations conferring zanamivir resistance in human influenza virus N2 neuraminidases compromise virus fitness and are not stably maintained in vitro. J. Antimicrob. Chemother. 58:723–732 [DOI] [PubMed] [Google Scholar]
- 23. McKimm-Breschkin JL, Rootes C, Mohr PG, Barrett S, Streltsov VA. 2012. In vitro passaging of a pandemic H1N1/09 virus selects for viruses with neuraminidase mutations conferring high-level resistance to oseltamivir and peramivir, but not to zanamivir. J. Antimicrob. Chemother. 67:1874–1883 [DOI] [PubMed] [Google Scholar]