Abstract
To meet the needs of a global community, an immunoassay for cryptococcal antigen (CrAg) must have high sensitivity for CrAg of all major serotypes. A new immunoassay for CrAg in lateral flow format was evaluated and found to have a high sensitivity for detection of serotypes A, B, C, and D.
TEXT
With a global burden of more than 1 million cases annually, cryptococcosis has emerged as a leading cause of death in patients with HIV or AIDS, killing an estimated 500,000 people (estimate range, 100,000 to 900,000) each year in sub-Saharan Africa alone (1). Early diagnosis is critical to effective treatment (2). The high burden of cryptococcosis in resource-limited settings underscores the need for an affordable, sensitive, and equipment-free diagnostic and has resulted in the development of the cryptococcal antigen lateral flow assay (CrAg LFA), a rapid point-of-care (POC) immunoassay (3).
The CrAg LFA (Immuno-Mycologics, Inc.) was constructed using monoclonal antibodies reactive with the capsular polysaccharide glucuronoxylomannan (GXM), the primary cryptococcal antigen (CrAg) that is shed during infection. The CrAg LFA has a dipstick format capable of detecting GXM in either serum or cerebrospinal fluid. GXM has variable levels of O-acetylation that contribute to serotype specificity and is classified into four major serotypes—A, B, C, and D (4). Although most cases of cryptococcosis are caused by isolates of serotype A, the need for sensitive diagnostics capable of detecting all four serotypes is emphasized by the report of serotype C infections in HIV patients in sub-Saharan Africa (5) and an increasing number of temperate regions reporting serotype B infections in otherwise healthy individuals (6). Moreover, serotype D is found with a high frequency in clinical cases in Europe (7–9). Several of the leading CrAg immunoassays for cryptococcosis display serotype bias, having a markedly reduced sensitivity for serotype C (10). In this study, the CrAg LFA serotype sensitivity was evaluated using endpoints determined visually and by densitometry scanning to determine the limit of detection, with GXM isolated from strains representing each of the four major serotypes.
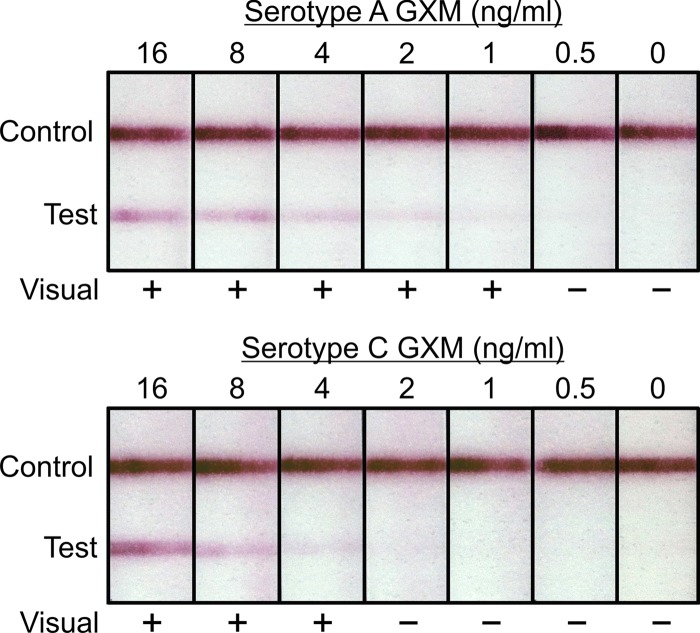
The nine representative Cryptococcus strains used in this study were selected on the basis of the chemotype and structure reporter groups typical of each of the four major serotypes (10, 11). GXM was isolated from culture supernatant fluids as previously described (10). Assays were performed by inserting CrAg LFA dipsticks into samples (100 μl) containing GXM that was serially diluted 2-fold from 32 ng/ml to 0.25 ng/ml in phosphate-buffered saline (PBS). Assays were allowed to develop for 10 min and then read in a blinded fashion by 4 different individuals instructed to evaluate tests as either positive or negative. The visual limit of detection was defined as the lowest concentration where at least 50% of observers stated the test was positive. Examples of LFAs tested with GXM from serotypes A and C are shown in Fig. 1. Tests were then read via densitometry scanning with an ESE lateral flow immunoassay reader (Qiagen, Inc.). The ESE reader generates quantitative data by performing a densitometer scan of the dipstick, where test line width (mm) is plotted against signal intensity (mV). Results yielding the calculated area of each peak (mm · mV) were plotted against corresponding concentrations, and the slope was then used to calculate a limit of detection with an endpoint of 50 mm · mV.
Fig 1.
Representative examples of the cryptococcal antigen lateral flow assay (CrAg LFA) tested with serial dilutions of GXM from serotype A strain CN6 and serotype C strain 24066. Shown are results from blinded visual inspection of strips by four independent observers. A positive (+) result is reported when 50% or more of the observers scored the result as positive.
The CrAg LFA showed high sensitivity for GXM from all four serotypes (Table 1). Comparing the visual limits of detection, the assay had the highest sensitivity for serotypes A and B, detecting GXM from two strains of each serotype at 1 ng/ml. Sensitivity levels for GXM of three serotype C strains were 16 ng/ml (strain 34), 8 ng/ml (strain 298), and 4 ng/ml (strain 24066). The sensitivity limits for GXM of serotype D strains M0024 and 127 were each 8 ng/ml. Endpoints based on densitometric scanning of strips were nearly identical to the visual results for serotypes A and B. Marginal differences were observed for serotype C and D samples. Overall there was a high correlation between limits of detection determined by visual inspection of the strips and limits of detection determined by densitometric scanning (Pearson product-moment correlation coefficient, 0.95; P = 0.00015). Despite the strong correlation between endpoints based on visual inspection and densitometric scanning, there was no obvious advantage in sensitivity determined by either method. Because the CrAg LFA is designed as a POC assay to be assessed without the use of equipment, densitometric scanning is not a substitute for direct observation, but rather an added method to experimentally quantify signal levels and validate visual results. However, the ability to electronically capture results of POC testing is consistent with the goal of using such data for patient follow-up, quality control, and public health surveillance (12).
Table 1.
Limit of detection of CrAg LFA for detection of GXM of different serotypes and comparison to previous report of sensitivity of latex agglutination assay
| CrAg serotype | C. neoformans strain | Limit of detection (CrAg ng/ml) for: |
||
|---|---|---|---|---|
| LFA |
Latex agglutinationc | |||
| Visual observationa | Densitometryb | |||
| A | CN6 | 1 | 1.3 | 24 |
| MU-1 | 1 | 1.0 | 32 | |
| B | 184 | 1 | 0.94 | 27 |
| 409 | 1 | 1.2 | 68 | |
| C | 34 | 16 | 27 | 432 |
| 298 | 8 | 4.4 | 260 | |
| 24066 | 4 | 2.2 | 460 | |
| D | 127 | 8 | 10 | 62 |
| M0024 | 8 | 11 | 63 | |
Lowest concentration at which 50% of observers considered a test to be positive.
Limit of detection calculated on the basis of densitometry scanning with an electronic reader.
Latex agglutination data are from a previous report of the serotype sensitivity of the Immuno-Mycologics Cryptococcus antigen latex agglutination test system (10).
This study demonstrated that the CrAg LFA has high sensitivity for GXM of all four serotypes, with A = B > C > D. The observed sensitivity of the CrAG LFA was greater than we previously reported for currently available CrAg immunoassays in latex agglutination or enzyme immunoassay formats (10). The previously reported serotype sensitivity of the Immuno-Mycologics, Inc., latex agglutination assay (10), one of the most sensitive assays in either the latex agglutination or enzyme-linked immunosorbent assay (ELISA) formats, is shown for comparison purposes in Table 1. The mean increase in sensitivity across CrAg from all four serotypes was 40-fold using the LFA format relative to the Immuno-Mycologics latex agglutination assay. The increase in sensitivity was greatest with CrAg of serotype C strain 24066 (150-fold) and least with the CrAg of the two serotype D strains (7-fold).
The performance and cost effectiveness of this new assay have prompted two recent reports recommending the use of the CrAg LFA to screen severely immunodeficient patients (CD4 < 100 cells/μl) (13, 14). Screening would allow for early diagnosis and treatment of patients with subclinical infections. This study demonstrates the high sensitivity of the CrAg LFA for detection of GXM, further validating its use for prospective screening of patients with HIV or AIDS and those presenting with clinical signs of cryptococcal meningitis.
ACKNOWLEDGMENTS
This study was supported by Public Health Service grants AI014209 and AI093365 from the National Institutes of Health.
The University of Nevada, Reno, has licensed monoclonal antibodies used for construction of the CrAg LFA to Immuno-Mycologics, Inc.
Footnotes
Published ahead of print 30 January 2013
REFERENCES
- 1.Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM. 2009. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS 23:525–530 [DOI] [PubMed] [Google Scholar]
- 2.Cryptococcal Guideline Working Group WHO 2011. Rapid advice: diagnosis, prevention and management of cryptococcal disease in HIV-infected adults, adolescents and children. World Health Organization, Geneva, Switzerland: http://whqlibdoc.who.int/publications/2011/9789241502979_eng.pdf [PubMed] [Google Scholar]
- 3.Jarvis JN, Percival A, Bauman S, Pelfrey J, Meintjes G, Williams GN, Longley N, Harrison TS, Kozel TR. 2011. Evaluation of a novel point-of-care cryptococcal antigen test on serum, plasma, and urine from patients with HIV-associated cryptococcal meningitis. Clin. Infect. Dis. 53:1019–1023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilson DE, Bennett JE, Bailey JW. 1968. Serologic grouping of Cryptococcus neoformans. Proc. Soc. Exp. Biol. Med. 127:820–823 [DOI] [PubMed] [Google Scholar]
- 5.Litvintseva AP, Thakur R, Reller LB, Mitchell TG. 2005. Prevalence of clinical isolates of Cryptococcus gattii serotype C among patients with AIDS in sub-Saharan Africa. J. Infect. Dis. 192:888–892 [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention 2010. Emergence of Cryptococcus gattii—Pacific Northwest, 2004–2010. Morb. Mortal. Wkly. Rep. 59:865–868 [PubMed] [Google Scholar]
- 7.Dromer F, Mathoulin S, Dupont B, Letenneur L, Ronin O, French Cryptococcosis Study Group 1996. Individual and environmental factors associated with infection due to Cryptococcus neoformans serotype D. Clin. Infect. Dis. 23:91–96 [DOI] [PubMed] [Google Scholar]
- 8.Kwon-Chung KJ, Bennett JE. 1984. Epidemiologic differences between the two varieties of Cryptococcus neoformans. Am. J. Epidemiol. 120:123–130 [DOI] [PubMed] [Google Scholar]
- 9.Tortorano AM, Viviani MA, Rigoni AL, Cogliati M, Roverselli A, Pagano A. 1997. Prevalence of serotype D in Cryptococcus neoformans isolates from HIV positive and HIV negative patients in Italy. Mycoses 40:297–302 [DOI] [PubMed] [Google Scholar]
- 10.Percival A, Kozel TR, Thorkildson P. 2011. Monoclonal antibodies specific for immunorecessive epitopes of glucuronoxylomannan, the major capsular polysaccharide of Cryptococcus neoformans, reduce serotype bias in an immunoassay for cryptococcal antigen. Clin. Vaccine Immunol. 18:1292–1296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bacon BE, Cherniak R, Kwon-Chung KJ, Jacobson ES. 1996. Structure of the O-deacetylated glucuronoxylomannan from Cryptococcus neoformans Cap70 as determined by 2D NMR spectroscopy. Carbohydr. Res. 283:95–110 [DOI] [PubMed] [Google Scholar]
- 12.Reid A. 2012. Bringing the lab to the patient: developing point-of-care diagnostics for resource limited settings. American Academy of Microbiology, Washington, DC: http://academy.asm.org/index.php/colloquium-program/browse-all-reports/495-bringing-the-lab-to-the-patient-developing-point-of-care-diagnostics-for-resource-limited-settings-2012 [PubMed] [Google Scholar]
- 13.Rajasingham R, Boulware DR. 2012. Reconsidering cryptococcal antigen screening in the U.S. among persons with CD4 <100 cells/mcL. Clin. Infect. Dis. 55:1742–1744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jarvis JN, Govender N, Chiller T, Park BJ, Longley N, Meintjes G, Bekker LG, Wood R, Lawn SD, Harrison TS. 2012. Cryptococcal antigen screening and preemptive therapy in patients initiating antiretroviral therapy in resource-limited settings: a proposed algorithm for clinical implementation. J. Int. Assoc. Physicians AIDS Care (Chic.). 11:374–379 [DOI] [PubMed] [Google Scholar]