Abstract
Highly pathogenic porcine reproductive and respiratory syndrome virus (HP-PRRSV) continues to evolve when serially passaged in Marc-145 cells. In this study, we analyzed the genomic and antigenic variants of HP-PRRSV strain JXA1 during in vitro passage. Protective efficacies of JXA1 from passages 100, 110, 120, 140, and 170 against the high-virulence parental virus were evaluated by inoculating pigs with each of these viruses and then challenging with JXA1 from passage 5 at 28 days postimmunization. We found that the antigenicities of JXA1 from passages after 110 were significantly reduced. Inoculation with JXA1 from passages after 110 provided only insufficient protection against the parental strain challenge, indicating that the immunogenicity of JXA1 is significantly decreased when it is in vitro passaged for 110 times and more. To identify the genomic variants that emerged during the overattenuation, eight complete genomes of highly passaged JXA1 were sequenced. One guanine deletion in the 5′ untranslated region (UTR), two nucleotide substitutions in the 3′ UTR, and 65 amino acid mutations in nonstructural and structural proteins that accompanied with the attenuation and overattenuation were determined. Genomic sequencing of in vitro serially passaged HP-PRRSV first identified the mutations potentially correlated with the overattenuation of a HP-PRRSV strain. These results facilitate the research aimed at elucidating the mechanisms for PRRSV genomic and antigenic changes and may also contribute to developing a safe and effective PRRSV vaccine.
INTRODUCTION
Porcine reproductive and respiratory syndrome (PRRS) is a clinically severe and economically important swine disease that emerged almost simultaneously in the United States and in Europe in the late 1980s and subsequently spread worldwide, causing enormous losses for the world swine industry (1, 2). A 2011 study found that PRRS could cost the U.S. pork industry $664 million per year rather than the $560 million reported in 2005 (1, 3). Since 2006, a highly pathogenic PRRS virus (HP-PRRSV), causing high fever and high morbidity and mortality, has emerged in China and affected more than 20 million pigs (4–6). Currently, the outbreaks of HP-PRRS are also reported in other Asian countries, resulting in a destructive impact on the local pig husbandries (7).
The etiological agent of PRRS, PRRSV, is an enveloped, positive-sense, single-stranded RNA virus belonging to the genus Arterivirus, family Arteriviridae, order Nidovirales (8). The genome of PRRSV is about 15 kb, containing a 5′ capped structure, a 3′ polyadenylated tail, and 10 open reading frames (ORFs) flanked by an untranslated region (UTR) at both 5′ and 3′ ends. ORF1a and ORF1b encode at least 14 nonstructural proteins (nsps) engaging in viral transcription and replication (9, 10). ORF2 to ORF7 encode 8 structural proteins which are important for virus infectivity (10–13). PRRSV can be divided into two genotypes, type 1 and type 2, represented by Lelystad virus (LV) and ATCC VR-2332 based on their genetic, antigenic, and pathological differences (14–16). HP-PRRS is caused by HP-PRRSV, which is a variant of type 2 PRRSV containing a novel discontinuous 30-amino-acid (aa) deletion in nsp2 (5).
Vaccination is one of the most effective strategies to prevent and control PRRS. Both killed and modified live virus (MLV) vaccines have been developed and are used in the Chinese market; however, live attenuated PRRSV vaccines have become predominant owing to their having higher efficacies than the killed vaccines (17, 18). To date, all three commercially available live attenuated HP-PRRSV vaccines, including JXA1-R, HuN4-F112, and TJM, are developed by in vitro serial passaging in nonhost cell lines (Marc-145 cells) (19–21). Another PRRSV vaccine used worldwide, Ingelvac PRRS MLV, is also obtained by continuously passaging in Marc-145 cells (22). The PRRSV MLV vaccine candidates are usually passaged more than 70 times because of the high risk of virulence reversion when lower numbers of passages are used (23).
By a certain number of times of in vitro passaging, PRRSV can be effectively attenuated but can still maintain strong immunogenicity, and such attenuated virus can be used to prepare the vaccine; however, little is known about the genomic, antigenic, and pathogenic characteristics of the overpassaged PRRSV. Here, we report in vitro and in vivo genomic sequencing and immunization and challenge studies of high numbers of passages of JXA1. The analyses of the correlation between genetic mutations and antigenic variants during in vitro serial passage will help to elucidate the mechanisms of PRRSV attenuation and overattenuation.
MATERIALS AND METHODS
(i) Serial in vitro passages of JXA1 in Marc-145 cells.
Strain JXA1 HP-PRRSV (GenBank accession no. EF112445) was serially passaged in Marc-145 cells using Dulbecco modified Eagle medium (DMEM), 2% fetal bovine serum (FBS), and penicillin-streptomycin solution at a final concentration of 100 IU/ml penicillin and 100 μg/ml streptomycin at 37°C with 5% CO2. We harvested the virus by freeze-thaw techniques when approximately 70% to 80% of the infected Marc-145 cells showed the cytopathic effect (CPE) as previously described (20). The same techniques were used during the process of in vitro serial passage. JXA1 from passage 82 was identified as an attenuated virus and was used as the seed virus for a HP-PRRSV vaccine designated JXA1-R. Here we kept passaging JXA1 until passage 170 and tested the pathogenic, antigenic, and genomic variants of the overpassaged viruses.
(ii) Virulence and protective efficacy test of the highly passaged JXA1.
There were 35 PRRSV-free piglets (4 to 6 weeks old) used in the animal infection studies. These pigs were also free from classical swine fever virus, swine influenza virus, porcine circovirus type 2, porcine parvovirus, pseudorabies virus, and porcine torque teno virus. All the pigs were randomly divided into seven groups (five pigs per group), and five groups were inoculated with virus from passages 100, 110, 120, 140, and 170, respectively, while the other two groups were mock inoculated with DMEM as a negative control. The virus load of intramuscular inoculation was 2.0 ml of 106.0 50% tissue culture infective dose (TCID50)/ml virus culture. At 28 days postimmunization (dpi), the five infected groups and one mock-inoculated group were challenged with 3.0 ml of 104.5 TCID50/ml of JXA1 from passage 5 (high virulence), while another mock-inoculated group was injected with DMEM again as the negative control. The pigs were maintained separately for a total of 7 weeks (immunization for 4 weeks and challenge for 3 weeks) and monitored daily for rectal temperature and clinical signs. Serum samples were collected at 0, 14, 28, 35, 42, and 49 dpi for PRRSV antibody and antigen tests by a commercial enzyme-linked immunosorbent assay (ELISA) kit (HerdChek PRRS 2XR; IDEXX Inc.) and the conventional reverse transcription-PCR (RT-PCR) assay described previously (24). Surviving pigs were euthanized at 21 days postchallenge (dpc), which was 49 dpi, for the pathology detection. Animal immunization and challenge studies were approved by the China Animal Disease Control Center (CADC) ethics committee (permit numbers CADC-AEC-2008016 and CADC-AEC-2008026).
(iii) RNA isolation and complete genomic sequencing.
Eight highly passaged JXA1 samples (passages 100, 110, 120, 130, 140, 150, 160, and 170) were submitted to complete-genome sequencing. Viral RNA from these passages was extracted using a Qiagen RNeasy minikit (Qiagen, Hilden, Germany) according to the manufacturer's instructions. Eighteen pairs of primers for amplifying 18 overlapped fragments were used to determine the entire genomes of these highly passaged JXA1 viruses. The primer sequences and amplification conditions were previously described (20). The amplicons were purified and cloned into pGEM-T Easy Vector (Promega, Madison, WI) and then sequenced by the use of an ABI Prism 3730 sequencer (Applied Biosystems, Foster, CA). Each fragment was independently sequenced at least three times. The sequenced products were spliced artificially to obtain the consensus genome sequences.
(iii) Nucleotide sequence accession numbers.
The sequences of the JXA1 samples from passages 100, 110, 120, 130, 140, 150, 160, and 170 are available under GenBank accession no. KC422725 to KC422731 and JQ804986.
RESULTS
(i) At high numbers of passages, JXA1 was effectively attenuated.
Within 28 dpi, no fever, sickness, or death was observed in either the groups inoculated with JXA1 from high numbers of passages (100, 110, 120, 140, and 170) or the mock-infected groups (Fig. 1). Furthermore, no pigs in the groups immunized with JXA1 from high numbers of passages or in the negative-control groups showed any clinical symptoms, such as skin cyanopathy, anorexia, and dyspnea, during the course of immunization. In addition, the weight gains seen in the immunized groups and the negative-control groups were almost the same within 28 dpi (data not shown). The results indicated that the JXA1 strains from all these high numbers of passages were attenuated.
Fig 1.
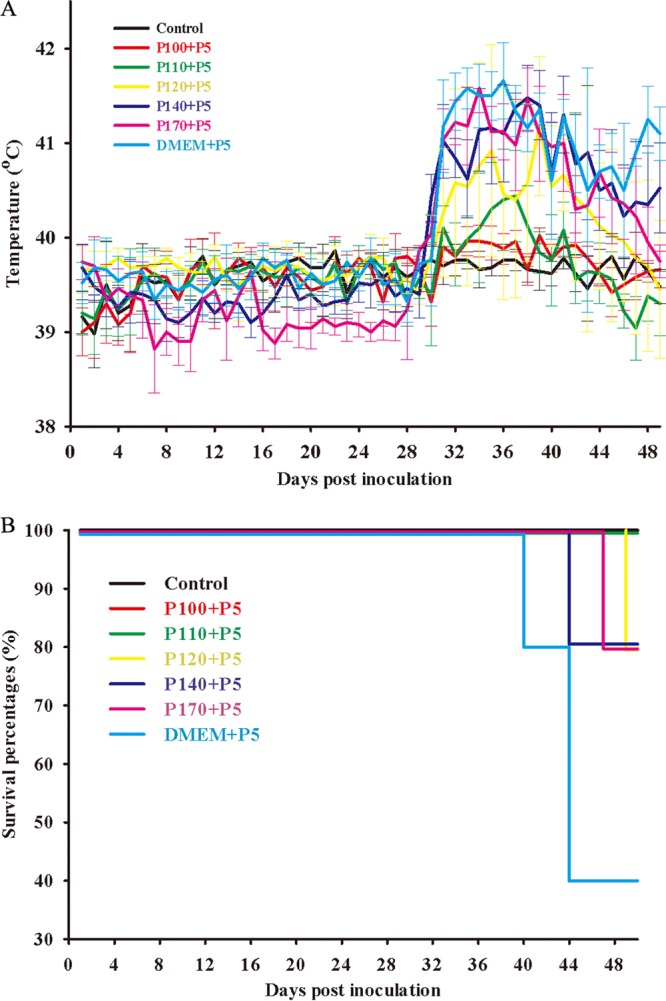
Immunization and challenge studies of highly passaged JXA1. Rectal temperatures (A) and survival rates (B) for each group of pigs (five pigs per group) are shown. Body temperatures are shown in means ± standard deviations. Pigs immunized with JXA1 from passage 100 obtain sufficient protection against the parental virus (P5) challenge, while those from passages 110 to 170 provide only insufficient protection for pigs against the parental virus.
(ii) The infectivity and antigenicity of highly passaged JXA1 were reduced.
PRRSV antibody and antigen tests by ELISA and RT-PCR showed that pigs in all groups were PRRSV antibody and antigen negative before immunization (Table 1). At 14 dpi, pigs inoculated with virus from passages 100 and 110 were both PRRSV antibody and antigen positive; however, only 3/5 (three of five pigs), 0/5, and 1/5 pigs in the corresponding groups inoculated with virus from passages 120, 140, and 170 were PRRSV antibody positive, while 3/5, 1/5, and 1/5 pigs were antigen positive, respectively. At 28 dpi, there were still only 4/5, 1/5, and 1/5 pigs in the corresponding groups inoculated with virus from passages 120, 140, and 170 that were PRRSV antibody positive. All pigs in negative-control groups were PRRSV antibody and antigen negative within 28 dpi (Table 1). These results showed that only the virus strains from passages 100 and 110 have enough infectivity and antigenicity to induce a strong antibody response, while those from passages 120, 140, and 170 have weak or lost infectivity and significantly decreased antigenicity.
Table 1.
Seroconversion of PRRSV antibody and antigen during the course of immunization and challenge shown by numbers of positive samples versus numbers of tested samples
| Group | Immunization at day 0 | No. of positive samples/no. of tested samples |
Challenge at day 28 | No. of positive samples/no. of tested samples |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day 0 |
Day 14 |
Day 28 |
Day 35 |
Day 42 |
Day 49 |
|||||||||
| ELISA | PCR | ELISA | PCR | ELISA | PCR | ELISA | PCR | ELISA | PCR | ELISA | PCR | |||
| 1 | P100 | 0/5 | 0/5 | 5/5 | 5/5 | 5/5 | 0/5 | P5 | 5/5 | 5/5 | 5/5 | 4/5 | 5/5 | 2/5 |
| 2 | P110 | 0/5 | 0/5 | 5/5 | 5/5 | 5/5 | 1/5 | P5 | 5/5 | 5/5 | 5/5 | 5/5 | 5/5 | 4/5 |
| 3 | P120 | 0/5 | 0/5 | 3/5 | 3/5 | 4/5 | 2/5 | P5 | 5/5 | 5/5 | 5/5 | 4/5 | 4/4 | 2/4 |
| 4 | P140 | 0/5 | 0/5 | 0/5 | 1/5 | 1/5 | 2/5 | P5 | 2/5 | 5/5 | 5/5 | 3/5 | 4/4 | 2/4 |
| 5 | P170 | 0/5 | 0/5 | 1/5 | 1/5 | 1/5 | 1/5 | P5 | 2/5 | 5/5 | 3/5 | 3/5 | 4/4 | 1/4 |
| 6 | DMEM | 0/5 | 0/5 | 0/5 | 0/5 | 0/5 | 0/5 | P5 | 2/5 | 5/5 | 4/4 | 4/4 | 2/2 | 2/2 |
| 7 | DMEM | 0/5 | 0/5 | 0/5 | 0/5 | 0/5 | 0/5 | DMEM | 0/5 | 0/5 | 0/5 | 0/5 | 0/5 | 0/5 |
(iii) Highly passaged viruses could not provide sufficient protection against JXA1 challenge.
After being challenged with high-virulence JXA1 at 28 dpi, pigs immunized with virus from passage 100 still did not show any clinical signs, and there was no fever, sickness, or death during the course of 21 dpc, indicating that JXA1 from passage 100 could provide sufficient protection against the parental virus challenge. However, two pigs in the group inoculated with passage 110 virus presented with lethargy and dyspnea at 5 to 7 dpc and the clinical symptoms lasted for about 1 week. These two pigs also had 2 days of high fever (≥41°C), and another two pigs showed median levels of fever (between 40°C and 40.5°C), while the other one in this group did not display any clinical signs or fever. The results illustrated that JXA1 from passage 110 provided only insufficient protection against the parental virus JXA1. In addition, four of five pigs in groups immunized with virus from passages 120 and 140 showed at least 3 days of high fever, while all pigs inoculated with virus from passage 170 presented with more than 3 days of high fever, which was similar to the results seen with the positive-control group (mock immunized with DMEM and then challenged with JXA1 from passage 5). Except for one pig injected with virus from passage 120 that did not show clinical signs, all the other pigs immunized with virus from passages 120, 140, and 170 presented obvious clinical symptoms of PRRSV infection. Furthermore, one pig in each group inoculated with virus from passages 120, 140, and 170 was dead within 21 dpc (Fig. 1). The results illustrated that JXA1 from passages 120, 140, and 170 provided only weak or no protection against challenge with high-virulence JXA1. Pigs in the positive-control group showed high fever, 100% morbidity, and 60% mortality, while pigs in the negative-control group (both immunization and challenge with DMEM) were healthy during the process of the experiment (Fig. 1). Upon necropsy, pathological changes such as alveolar edema, lung necrosis, hemorrhagic spots in kidney, and hemorrhages in lymph nodes could be observed in several sick pigs (vaccinated with JXA1 from passages 110 to 170 and then challenged with JXA1 from passage 5), while pathological lesions could not be observed in negative-control pigs and pigs immunized with JXA1 from passage 100.
(iv) The antibody response to N protein of highly passaged JXA1 was decreased.
PRRSV antibody and antigen tests showed that the induced antibody response and infectivity of highly passaged JXA1 gradually decreased during the course of in vitro overpassage (Table 1). At 35 dpi (7 dpc), all pigs challenged with JXA1 from passage 5 were PRRSV antigen positive. Pigs immunized with virus from passages 100, 110, and 120 were PRRSV antibody positive, while only two of five (2/5) pigs in each group immunized with virus from passages 140 and 170 were PRRSV antibody positive. PRRSV antibody could also be detected in 2/5 pigs in the mock immunization group and then in the challenge group at 7 dpc. At 42 dpi (14 dpc), two pigs in the group inoculated with virus from passage 170 were still PRRSV antibody negative, while all the other challenged pigs were PRRSV antibody positive. At 49 dpi (21 dpc), all of the pigs that had survived were PRRSV antibody positive (Table 1). These results indicated that the antibody response to nucleocapsid (N) protein of highly passaged JXA1 was decreased due to the reduced antigenicity during in vitro overpassage.
(v) The genomic characteristics of attenuated and overattenuated JXA1 were identified.
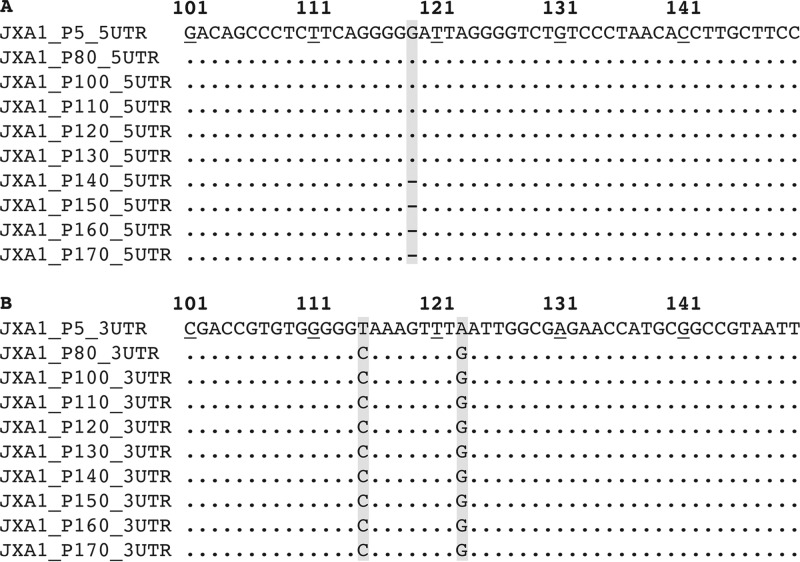
Highly passaged (passages 100 to 170) JXA1 shared high (between 99.2% and 99.3%) genomic homologies with JXA1 from passage 5. Excluding the 3′ poly(A) tail, the complete genomes of JXA1 from passages 100 to 130 were 15,320 nucleotides (nt), which is same as that of JXA1 from passage 5, while those from passages 140 to 170 were 15,319 nt due to one nucleotide deletion (guanine) at position 119 in the 5′ UTR (Fig. 2A). In addition, there were two nucleotide substitutions (T115C and A123G) between high-virulence JXA1 (passage 5) and effectively attenuated JXA1 (passages 100 to 170) in the 3′ UTR (Fig. 2B). The results indicated that both the 5′ UTR and 3′ UTR probably were engaged in the attenuation and overattenuation of JXA1. There were 106 nt mutations that emerged during the passaging from passage 5 to passage 100 of JXA1, leading to 50 aa variants, while 119 nt changes from passages 5 to 170 resulted in 65 aa substitutions.
Fig 2.
Both deletion and substitution emerged in the untranslated regions (UTR) during in vitro serial passage. One guanine deletion were identified at nt 119 in the 5′ UTR of JXA1 from passages 140 to 170 (A), while two substitutions (T115C and A123G) were found in the 3′ UTR of JXA1 from passages 80 to 170 (B). Both the deletion and substitutions are highlighted in black characters on a gray background.
(vi) Mutations increased more rapidly in structural proteins than in nonstructural proteins during the overattenuation of JXA1.
To compare the highly passaged JXA1 with the parental virus, a total of 65 aa mutation sites dispersed throughout 14 nonstructural and structural proteins were identified during in vitro overpassage (Table 2). There were 33/65 (50.8%) aa mutated positions spread throughout the nonstructural proteins, and the other 32/65 (49.2%) positions were in the structural proteins, indicating that both nonstructural and structural proteins were critical for the attenuation and overattenuation of JXA1. Comparison of the mutations between the fully attenuated virus (passage 100) and high-virulence virus (passage 5) showed that 28/50 (56%) aa mutations were in nonstructural proteins and 22/50 (44%) were in structural proteins (Table 2). During the overattenuation (from passages 100 to 170), 10 more aa mutations (from 22 to 32) happened in structural proteins, while only 5 more aa mutations (from 28 to 33) emerged in nonstructural proteins. The dramatically decreased antigenicity of JXA1 during the overattenuation could have been due to the rapidly increased mutations in structural proteins, indicating that structural proteins might play a more important role in the overattenuation of JXA1.
Table 2.
Amino acid mutations between JXA1 and the derivative viruses
| ORF | Positiona | Mutation at indicated no. of passagesb |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 5 | 80 | 100 | 110 | 120 | 130 | 140 | 150 | 160 | 170 | ||
| ORF1a | |||||||||||
| nsp1β | 187 | D | G | G | G | G | G | G | G | G | G |
| 239 | R | K | K | K | K | K | K | K | K | K | |
| 242 | F | L | L | L | L | L | L | L | L | L | |
| 378 | S | S | S | R | R | R | R | R | R | R | |
| nsp2 | 572 | L | L | L | S | S | S | S | S | S | S |
| 636 | T | A | A | A | A | A | A | A | A | A | |
| 679 | V | E | E | E | E | E | E | E | E | E | |
| 686 | E | D | D | D | D | D | D | D | D | D | |
| 780 | K | K | K | K | Q | E | E | E | E | E | |
| 782 | A | T | T | T | T | T | T | T | T | T | |
| 902 | G | G | G | G | G | G | G | G | E | E | |
| 928 | A | V | V | V | V | V | V | V | V | V | |
| 951 | G | R | R | R | R | R | R | R | R | R | |
| 957 | E | G | G | G | G | G | G | G | G | G | |
| 1062 | R | M | M | M | M | M | M | M | M | M | |
| 1128 | V | A | A | A | A | A | A | A | A | A | |
| 1155 | I | M | M | M | M | M | M | M | M | M | |
| 1179 | G | D | D | D | D | D | D | D | D | D | |
| 1392 | S | L | L | L | L | L | L | L | L | L | |
| 1561 | R | C | C | C | C | C | C | C | C | C | |
| nsp3 | 1629 | E | D | D | D | D | D | D | D | D | D |
| 1723 | I | I | I | T | T | T | T | T | T | T | |
| nsp7α | 2331 | N | S | S | S | S | S | S | S | S | S |
| ORF1b | |||||||||||
| nsp9 | 138 | K | E | E | E | E | E | E | E | E | E |
| 365 | I | M | M | M | M | M | M | M | M | M | |
| 423 | E | G | G | G | G | G | G | G | G | G | |
| nsp10 | 847 | R | H | H | H | H | H | H | H | H | H |
| 1036 | A | T | T | T | T | T | T | T | T | T | |
| 1038 | P | H | H | H | H | H | H | H | H | H | |
| 1040 | E | D | D | D | D | D | D | D | D | D | |
| 1059 | V | L | L | L | L | L | L | L | L | L | |
| 1136 | A | V | V | A | A | A | A | A | A | A | |
| nsp11 | 1181 | M | V | V | V | V | V | V | V | V | V |
| ORF2 | 10 | L | F | F | F | F | F | F | F | F | F |
| 23 | N | S | S | S | S | S | S | S | S | S | |
| 50 | Y | F | F | F | F | F | F | F | F | F | |
| 118 | I | V | V | V | V | V | V | V | V | V | |
| 168 | M | T | T | M | M | M | M | M | M | M | |
| 204 | H | H | H | N | N | N | N | N | N | N | |
| 251 | F | S | S | S | S | S | S | S | S | S | |
| E | 3 | S | S | S | A | A | A | A | A | A | A |
| 9 | D | H | H | H | H | H | H | H | H | H | |
| 48 | L | F | F | F | F | F | F | F | F | F | |
| ORF3 | 12 | F | L | L | L | L | L | L | L | L | L |
| 79 | H | N | N | N | N | Y | Y | Y | Y | Y | |
| 85 | N | N | N | N | N | N | N | S | S | S | |
| 165 | F | F | F | F | F | F | F | F | Y | Y | |
| 196 | V | V | V | V | V | V | V | V | I | I | |
| 216 | S | S | S | S | S | S | S | S | S | L | |
| 225 | T | A | A | A | A | A | A | A | A | A | |
| 248 | F | V | V | V | V | V | V | V | V | V | |
| ORF4 | 14 | C | C | C | C | C | C | C | C | Y | Y |
| 43 | D | G | G | G | G | G | G | G | G | G | |
| 66 | I | S | S | S | S | S | S | S | S | S | |
| 124 | I | I | V | V | V | V | V | V | V | V | |
| 132 | S | T | T | T | T | T | T | T | T | T | |
| 172 | L | V | V | F | F | F | F | F | F | F | |
| 173 | P | A | A | A | A | A | A | A | A | A | |
| 174 | S | I | I | I | I | I | I | I | I | I | |
| ORF5a | 36 | Q | Q | Q | R | R | R | R | R | R | R |
| 49 | N | D | D | D | D | D | D | D | D | D | |
| ORF5 | 33 | N | N | N | D | D | D | D | D | D | D |
| 59 | K | N | N | N | N | N | N | N | N | N | |
| 164 | G | R | R | R | R | R | R | R | R | R | |
| ORF7 | 11 | K | K | K | K | K | K | K | N | N | N |
The cleavage positions were determined based on a previous report (9).
Mutations correlated with the attenuation are shown in lightface characters without underlining; mutations responsible for the overattenuation are shown in boldface characters without underlining; mutations might also contribute to the overattenuation are shown in lightface characters with underlining; two reversion mutations (aa 1136 in nsp10 and aa 168 in ORF2) that are probably not correlated with the attenuation or overattenuation of JXA1 are shown in boldface characters with underlining.
(vii) Virulence determinants of JXA1 resided in both nonstructural and structural proteins.
Within the 65 mutations, 45 mutations were conserved in attenuated JXA1 (passages 80 to 170) but differed from those in high-virulence JXA1 (passage 5), indicating that those corresponding residues on JXA1 from passage 5 could be virulence determinants and that mutations played a vital role in the attenuation (Table 2). These mutations dispersed into seven nonstructural proteins (nsp1β, nsp2, nsp3, nsp7α, nsp9, nsp10, and nsp11) and six structural proteins (GP2, E, GP3, GP4, ORF5a, and GP5), supporting the notion that PRRSV virulence determinants had the multigenic trait.
(ix) Mutations potentially correlated with the overattenuation of JXA1 were identified.
We identified eight amino acid mutations (aa 378 in nsp1β, aa 572 in nsp2, aa 1723 in nsp3, aa 204 in GP2, aa 3 in E, aa 172 in GP4, aa 36 in ORF5a, and aa 33 in GP5) that were conserved in JXA1 from passages 110 to 170 but differed from those in JXA1 from passages 5 and 100. JXA1 from passages 5 and 100 had strong antigenicities, and JXA1 from passage 100 was well attenuated and could provide full protection for pigs against high-virulence JXA1 challenge; however, JXA1 from passages 110 to 170 had decreased antigenicities and could not provide sufficient protection against the parental virus challenge. The results illustrated that these mutations potentially correlated with the decreased antigenicity and could be considered the markers for the overattenuation of JXA1. Considering that the antibody response to highly passaged JXA1 was gradually reduced due to the decreased antigenicity, another 10 amino acid mutations (aa 780 and 902 in nsp2; aa 79, 85, 165, 196, and 216 in ORF3; aa 14 and 124 in ORF4; and aa 11 in ORF7) that emerged during the course of in vitro serial passage might also contribute to the overattenuation of JXA1. Two reversion mutations (aa 1136 in nsp10 and aa 168 in ORF2) might not be related to the attenuation or overattenuation of JXA1 during in vitro serial passage.
DISCUSSION
In this study, we continuously passaged JXA1 in Marc-145 cells 170 times and found that strains of highly passaged JXA1 (passages 110 to 170) were overattenuated. JXA1 from passages 110 to 170 had reduced antigenicities and provided only insufficient protection against the parental virus. Amino acid mutations that presumably correlated with the attenuation and overattenuation of JXA1 were identified in both the nonstructural and structural proteins. Mutations in the structural proteins increased more rapidly than in the nonstructural proteins during the overattenuation (from passages 100 to 170). In addition, one nucleotide deletion in the 5′ UTR and two nucleotide substitutions in the 3′ UTR during in vitro passage might also have contributed to the attenuation or overattenuation of JXA1. This is the first report of in vivo and in vitro data about the characteristics of the overattenuation of HP-PRRSV by overpassaging in Marc-145 cells.
The 5′ UTR and 3′ UTR of PRRSV are highly conserved and play pivotal roles in viral replication, subgenomic mRNA transcription, protein translation, and virus attenuation (25–27). A guanine deletion at position 119 in the 5′ UTR is within the type II PRRSV stem-loop 4a region (28). Due to the fact that the deletion emerged only after passage 140 and resulted in significantly decreased antigenicities compared to the results seen with JXA1 from the other, lower numbers of passages (Table 1), it might contribute to the overattenuation of JXA1 by decreasing the viral replication in the host and reducing the host immune responses to the virus. Two mutations (T115C and A123G) reside in the long bulged stem-loop region in 3′ UTR, which is highly conserved in both type 1 and type 2 PRRSV (26). The mutations in this region are conserved during in vitro overpassage, indicating that they might play a role in the virus attenuation.
PRRSV nsps play a critical role in processing and maturation of the repertoire of structural and nonstructural proteins of the virion, but little is known about the anti-nsp immune response. Both nsp1 and nsp2 are multifunctional regulatory proteins (9, 10), and the mutations S378R in nsp1β and L572S in nsp2 could contribute to overattenuation of JXA1 by impairing the infectivity and/or replication ability of virus. Meanwhile, it was previously reported that both nsp3 and nsp7α are important in forming the viral replication complex and that nsp7 is highly immunogenic (9, 10, 29); mutations in nsp3 might be critical for both attenuation and overattenuation of JXA1, while the N2331S mutation in nsp7α might play a role in the attenuation on the basis of this study (Table 2). For nsps encoded by ORF1b, mutations in nsp9, nsp10, and nsp11 were all conserved among the attenuated viruses (passages 80 to 170 of JXA1) but differed from those in the high-virulence virus (JXA1 from passage 5) except for one reversion mutation at aa 1136 in nsp10, indicating that mutations in the nsps encoded by ORF1b played an important role in the attenuation rather than the overattenuation of JXA1.
Four minor viral structural proteins can interact with each other and form a multimeric complex, which is essential for virus infectivity (30). The multimeric complex of the minor glycoproteins is involved in the direct interaction with cell surface receptor CD163 for virus entry (31). Minor structural proteins also help to induce a stronger immune response when they are coexpressed with major structural proteins (32). In addition, mutations in structural proteins were more rapidly increased during the overattenuation of JXA1 (from passages 100 to 170), supporting the notion that structural proteins might contain major immunogenic determinants (Table 2). Regarding the overattenuation-related mutations in structural proteins, most (10/13) of them reside in the minor glycoproteins, indicating the pivotal role of minor glycoproteins in the overattenuation of JXA1 (Table 2). Mutations in minor glycoproteins might reduce the virus infectivity and inhibit the virus entry, leading to decreased antigenicities of the minor glycoproteins; they might also be able to change the interaction between the minor and major glycoproteins, resulting in reduction in the antigenicities of the major glycoproteins, both of which contributed to the overattenuation of JXA1.
In the major glycoproteins, two mutations in ORF5a and three mutations in ORF5 were found. Given that N49D in ORF5a and K59N and G164R in GP5 were conserved in passages 80 to 170, these three mutations might contribute to the attenuation of JXA1. The N33D mutation in GP5, which emerged between passages 100 and 110 with different antigenicities, is located between the nonneutralizing A epitope (aa 27 to 30) and the neutralizing B epitope (aa 37 to 45) according to a previous report (33). It resides in a second neutralization epitope (aa 29 to 35) according to another study (34). Although the mutation does not change the N-glycosylation site, the mutation in the N-terminal portion of GP5 might also help to reduce the humoral immune response to PRRSV GP5 protein, which is consistent with the lower antibody responses to JXA1 from passages 110 to 170 than to JXA1 from passage 100 (Table 1). The function of the newly identified ORF5a protein is still unknown; the role of the Q36R mutation in ORF5a requires further investigation.
In conclusion, we found that a HP-PRRSV strain was overattenuated during in vitro serial passage. Mutations potentially related to the overattenuation phenotype of JXA1 were first identified. The mutations accumulated when the virus was further adapted to Marc-145 cells, which decreased the viral antigenicity and reduced the PRRSV-specific antibody response due to the loss of infectivity and poor replication of the virus in vivo, resulting in insufficient protection even against the homologous virus. Our findings provide useful data to further explore the correlation between the PRRSV genome and antigenicity and might contribute to develop the next generation of PRRSV vaccine. The results indicate that we need to consider the balance between decreasing the pathogenicity and maintaining the antigenicity during the process of preparing attenuated PRRSV vaccine. Insufficiently attenuated vaccine might cause disease, while overattenuated vaccine might fail to provide enough protection; both result in the failure of vaccination.
ACKNOWLEDGMENT
This study was supported by the National Basic Research Program of China (grant no. 2008FY130100-2) and the Modern Agricultural Industry Technology System Beijing Innovation Team Foundation (grant no. GWZJ-2009-05).
Footnotes
Published ahead of print 13 February 2013
REFERENCES
- 1. Neumann EJ, Kliebenstein JB, Johnson CD, Mabry JW, Bush EJ, Seitzinger AH, Green AL, Zimmerman JJ. 2005. Assessment of the economic impact of porcine reproductive and respiratory syndrome on swine production in the United States. J. Am. Vet. Med. Assoc. 227: 385– 392 [DOI] [PubMed] [Google Scholar]
- 2. Keffaber KK. 1989. Reproductive failure of unknown etiology. Am. Assoc. Swine Pract. Newsl. 1: 1– 10 [Google Scholar]
- 3. Holtkamp DJ, Kliebenstein JB, Neumann EJ, Zimmerman JJ, Rotto H, Yoder TK, Wang C, Yeske P, Mowrer C, Haley C. 2011. Assessment of the economic impact of porcine reproductive and respiratory syndrome virus on U.S. pork producers. Abstr. 2011 Int. PRRS Symp., abstr 69, p 86 [Google Scholar]
- 4. Li Y, Wang X, Bo K, Wang X, Tang B, Yang B, Jiang W, Jiang P. 2007. Emergence of a highly pathogenic porcine reproductive and respiratory syndrome virus in the Mid-Eastern region of China. Vet. J. 174: 577– 584 [DOI] [PubMed] [Google Scholar]
- 5. Tian K, Yu X, Zhao T, Feng Y, Cao Z, Wang C, Hu Y, Chen X, Hu D, Tian X, Liu D, Zhang S, Deng X, Ding Y, Yang L, Zhang Y, Xiao H, Qiao M, Wang B, Hou L, Wang X, Yang X, Kang L, Sun M, Jin P, Wang S, Kitamura Y, Yan J, Gao GF. 2007. Emergence of fatal PRRSV variants: unparalleled outbreaks of atypical PRRS in China and molecular dissection of the unique hallmark. PLoS One 2: e526 doi:10.1371/journal.pone.0000526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tong GZ, Zhou YJ, Hao XF, Tian ZJ, An TQ, Qiu HJ. 2007. Highly pathogenic porcine reproductive and respiratory syndrome, China. Emerg. Infect. Dis. 13:1434– 1436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. An TQ, Tian ZJ, Leng CL, Peng JM, Tong GZ. 2011. Highly pathogenic porcine reproductive and respiratory syndrome virus, Asia. Emerg. Infect. Dis. 17: 1782– 1784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cavanagh D. 1997. Nidovirales: a new order comprising Coronaviridae and Arteriviridae. Arch. Virol. 142: 629– 633 [PubMed] [Google Scholar]
- 9. Fang Y, Snijder EJ. 2010. The PRRSV replicase: exploring the multifunctionality of an intriguing set of nonstructural proteins. Virus Res. 154: 61– 76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Music N, Gagnon CA. 2010. The role of porcine reproductive and respiratory syndrome (PRRS) virus structural and non-structural proteins in virus pathogenesis. Anim. Health Res. Rev. 11: 135– 163 [DOI] [PubMed] [Google Scholar]
- 11. Firth AE, Zevenhoven-Dobbe JC, Wills NM, Go YY, Balasuriya UB, Atkins JF, Snijder EJ, Posthuma CC. 2011. Discovery of a small arterivirus gene that overlaps the GP5 coding sequence and is important for virus production. J. Gen. Virol. 92: 1097– 1106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Johnson CR, Griggs TF, Gnanandarajah J, Murtaugh MP. 2011. Novel structural protein in porcine reproductive and respiratory syndrome virus encoded by an alternative ORF5 present in all arteriviruses. J. Gen. Virol. 92: 1107– 1116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Snijder EJ, Meulenberg JJ. 1998. The molecular biology of arteriviruses. J. Gen. Virol. 79(Pt 5):961–979 [DOI] [PubMed] [Google Scholar]
- 14. Meng XJ, Paul PS, Halbur PG, Lum MA. 1995. Phylogenetic analyses of the putative M (ORF 6) and N (ORF 7) genes of porcine reproductive and respiratory syndrome virus (PRRSV): implication for the existence of two genotypes of PRRSV in the U.S.A. and Europe. Arch. Virol. 140: 745– 755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Murtaugh MP, Elam MR, Kakach LT. 1995. Comparison of the structural protein coding sequences of the VR-2332 and Lelystad virus strains of the PRRS virus. Arch. Virol. 140: 1451– 1460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nelsen CJ, Murtaugh MP, Faaberg KS. 1999. Porcine reproductive and respiratory syndrome virus comparison: divergent evolution on two continents. J. Virol. 73: 270– 280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kimman TG, Cornelissen LA, Moormann RJ, Rebel JM, Stockhofe-Zurwieden N. 2009. Challenges for porcine reproductive and respiratory syndrome virus (PRRSV) vaccinology. Vaccine 27: 3704– 3718 [DOI] [PubMed] [Google Scholar]
- 18. Zhou L, Yang H. 2010. Porcine reproductive and respiratory syndrome in China. Virus Res. 154: 31– 37 [DOI] [PubMed] [Google Scholar]
- 19. An TQ, Tian ZJ, Zhou YJ, Xiao Y, Peng JM, Chen J, Jiang YF, Hao XF, Tong GZ. 2011. Comparative genomic analysis of five pairs of virulent parental/attenuated vaccine strains of PRRSV. Vet. Microbiol. 149: 104– 112 [DOI] [PubMed] [Google Scholar]
- 20. Han W, Wu JJ, Deng XY, Cao Z, Yu XL, Wang CB, Zhao TZ, Chen NH, Hu HH, Bin W, Hou LL, Wang LL, Tian KG, Zhang ZQ. 2009. Molecular mutations associated with the in vitro passage of virulent porcine reproductive and respiratory syndrome virus. Virus Genes 38: 276– 284 [DOI] [PubMed] [Google Scholar]
- 21. Leng X, Li Z, Xia M, Li X, Wang F, Wang W, Zhang X, Wu H. 2012. Mutations in the genome of the highly pathogenic porcine reproductive and respiratory syndrome virus potentially related to attenuation. Vet. Microbiol. 157: 50– 60 [DOI] [PubMed] [Google Scholar]
- 22. Opriessnig T, Halbur PG, Yoon KJ, Pogranichniy RM, Harmon KM, Evans R, Key KF, Pallares FJ, Thomas P, Meng XJ. 2002. Comparison of molecular and biological characteristics of a modified live porcine reproductive and respiratory syndrome virus (PRRSV) vaccine (ingelvac PRRS MLV), the parent strain of the vaccine (ATCC VR2332), ATCC VR2385, and two recent field isolates of PRRSV. J. Virol. 76: 11837– 11844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nielsen HS, Oleksiewicz MB, Forsberg R, Stadejek T, Botner A, Storgaard T. 2001. Reversion of a live porcine reproductive and respiratory syndrome virus vaccine investigated by parallel mutations. J. Gen. Virol. 82: 1263– 1272 [DOI] [PubMed] [Google Scholar]
- 24. Chen NH, Chen XZ, Hu DM, Yu XL, Wang LL, Han W, Wu JJ, Cao Z, Wang CB, Zhang Q, Wang BY, Tian KG. 2009. Rapid differential detection of classical and highly pathogenic North American Porcine Reproductive and Respiratory Syndrome virus in China by a duplex real-time RT-PCR. J. Virol. Methods 161: 192– 198 [DOI] [PubMed] [Google Scholar]
- 25. Gao F, Lu J, Yao H, Wei Z, Yang Q, Yuan S. 2012. Cis-acting structural element in 5′ UTR is essential for infectivity of porcine reproductive and respiratory syndrome virus. Virus Res. 163: 108– 119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sun Z, Liu C, Tan F, Gao F, Liu P, Qin A, Yuan S. 2010. Identification of dispensable nucleotide sequence in 3′ untranslated region of porcine reproductive and respiratory syndrome virus. Virus Res. 154: 38– 47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wang Y, Liang Y, Han J, Burkhart KM, Vaughn EM, Roof MB, Faaberg KS. 2008. Attenuation of porcine reproductive and respiratory syndrome virus strain MN184 using chimeric construction with vaccine sequence. Virology 371: 418– 429 [DOI] [PubMed] [Google Scholar]
- 28. Lu J, Gao F, Wei Z, Liu P, Liu C, Zheng H, Li Y, Lin T, Yuan S. 2011. A 5′-proximal stem-loop structure of 5′ untranslated region of porcine reproductive and respiratory syndrome virus genome is key for virus replication. Virol. J. 8: 172 doi:10.1186/1743-422X-8-172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Brown E, Lawson S, Welbon C, Gnanandarajah J, Li J, Murtaugh MP, Nelson EA, Molina RM, Zimmerman JJ, Rowland RR, Fang Y. 2009. Antibody response to porcine reproductive and respiratory syndrome virus (PRRSV) nonstructural proteins and implications for diagnostic detection and differentiation of PRRSV types I and II. Clin. Vaccine Immunol. 16:628– 635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wissink EH, Kroese MV, van Wijk HA, Rijsewijk FA, Meulenberg JJ, Rottier PJ. 2005. Envelope protein requirements for the assembly of infectious virions of porcine reproductive and respiratory syndrome virus. J. Virol. 79: 12495– 12506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Das PB, Dinh PX, Ansari IH, de Lima M, Osorio FA, Pattnaik AK. 2010. The minor envelope glycoproteins GP2a and GP4 of porcine reproductive and respiratory syndrome virus interact with the receptor CD163. J. Virol. 84: 1731– 1740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jiang W, Jiang P, Wang X, Li Y, Du Y, Wang X. 2008. Enhanced immune responses of mice inoculated recombinant adenoviruses expressing GP5 by fusion with GP3 and/or GP4 of PRRS virus. Virus Res. 136: 50– 57 [DOI] [PubMed] [Google Scholar]
- 33. Ostrowski M, Galeota JA, Jar AM, Platt KB, Osorio FA, Lopez OJ. 2002. Identification of neutralizing and nonneutralizing epitopes in the porcine reproductive and respiratory syndrome virus GP5 ectodomain. J. Virol. 76: 4241– 4250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wissink EH, van Wijk HA, Kroese MV, Weiland E, Meulenberg JJ, Rottier PJ, van Rijn PA. 2003. The major envelope protein, GP5, of a European porcine reproductive and respiratory syndrome virus contains a neutralization epitope in its N-terminal ectodomain. J. Gen. Virol. 84: 1535– 1543 [DOI] [PubMed] [Google Scholar]