Abstract
Inactivated foot-and-mouth disease (FMD) vaccines are currently used worldwide. With the emergence of various FMD virus serotypes and subtypes, vaccines must become more suitable for field-based uses under the current circumstances in terms of the fast and proper selection of vaccine strains, an extended vaccine development period for new viruses, protecting against the risk of virus leakage during vaccine manufacture, counteracting the delayed onset of immune response, counteracting shorter durations of immunity, and the accurate serological differentiation of infected and vaccinated animals and multiple vaccination. The quality of vaccines should then be improved to effectively control FMD outbreaks and minimize the problems that can arise among livestock after vaccinations. Vaccine improvement should be based on using attenuated virus strains with high levels of safety. Moreover, when vaccines are urgently required for newly spread field strains, the seed viruses for new vaccines should be developed for only a short period. Improved vaccines should offer superior immunization to all susceptible animals including cattle and swine. In addition, they should have highly protective effects without persistent infection. In this way, if vaccines are developed using new methods such as reverse genetics or vector vaccine technology, in which live viruses can be easily made by replacing specific protective antigens, even a single vaccination is likely to generate highly protective effects with an extended duration of immunity, and the safety and stability of the vaccines will be assured. We therefore reviewed the current FMD vaccines and their adjuvants, and evaluated if they provide superior immunization to all susceptible animals including cattle and swine.
Keywords: Foot-and-mouth disease, Vaccine, Development, Improvement
Introduction
Foot-and-mouth disease virus (FMDV) causes foot-and-mouth disease (FMD), a contagious and fatal disease in cloven-hoofed animals, characterized by vesicles in the mouth, tongue, hoofs, and nipples and increase in body temperature and appetite loss.
Control of FMD becomes a challenge as soon as it infects a host as it replicates and spreads rapidly [1]. FMDV belongs to the Picornaviridae family, the same family to which poliovirus (humans), encephalomyocarditis virus (swine), vesicular disease virus (swine), hand-foot-and-mouth disease virus (humans), enterovirus, and rhinovirus belong [2].
Over 3.5 million animals were culled when an FMD outbreak hit South Korea in November 2010. A month later, the government responded by implementing emergency vaccinations with O1 Manisa vaccine (at least 6PD50) among of cows and pigs [3] which made FMD cases to decline until it was completely suppressed the following year (the last case reported was in April 2011). The monovalent O1 Manisa used to control the outbreak was converted to a trivalent vaccine (composed of O1 Manisa, A Malaysia 97, and Asia1 Shamir) to increase the potency to at least 6PD50. However, despite the powerful effects of the vaccines that reduced the enormous FMD outbreak, the current vaccines were evaluated as having many problems to overcome with when applied to emergency and routine vaccination. In addition, FMD vaccination countries with FMD-free status and the countries that have the potential to urgently use vaccines upon a FMD outbreak need to clearly review the strengths and weaknesses of their vaccination practices in preparation for contingencies. Therefore, the present review requires an in-depth consideration on the characteristics of the currently used vaccines, which include the oil used for vaccine adjuvants, immune responses after vaccinations, and species-specific immunizations. Through such a process, this study is intended to contemplate what we must research and develop in order to improve vaccines.
Characterization of Current FMD Vaccines and Their Uses in FMD Outbreaks
Characterization of FMD vaccines and restrictions on their use
FMD is a highly significant disease in the field of veterinary science. It is the first viral disease for which the causative agent was identified in 1897 [4]. FMD studies began with a study that produced vaccines by inactivating live viruses with formalin in 1926. Since 1970, vaccine adjuvants have been converted from gel to oil for the pigs, thereby resolving the problem of poor immunization in pigs. Among such adjuvants, the adjuvants using double-oil emulsion improved both the inducement of emergent immune responses and duration [5, 6]. FMD vaccines have the shortcoming of having effects only within the same serotypes and not protecting against other serotype viruses. Therefore, synergistic effects of protective coverage can be elicited through the manufacturing of polyvalent vaccines containing antigens of two to four serotypes or subtypes that have a risk of occurrence [7]. Among the seven serotypes that have been discovered to date, the combination of serotypes O, A, and Asia1 is frequently used and stored in many countries that are vulnerable to FMD, except those in Africa [8,9]. Most Southeast Asian countries chiefly use serotype O monovalent vaccines, while occasionally including several virus subtypes for serotype O. Most vaccines are designed to include the antigens at 0.5-9.2 µg per dose. Serotype O and SAT viruses include more antigens as compared to serotype A, Asia1, and C [10-12].
Live vaccines are widely used to prevent most viral diseases, and research activities for the development of live FMD vaccines are also underway. Currently, however, all of the FMD vaccines used worldwide are inactivated ones. Despite the continuous and strenuous research efforts of FMD researchers since the first identification of FMDV, the research on virus attenuation eventually failed [13]. When the A24 Cruzeiro strain was attenuated and its virus titers were measured, the strain exhibited 100 to 1,000 times lower growth than field strains did. Through this, an attenuated virus was produced and used as a vaccine candidate for cattle and swine. However, stressed cattle vaccinated with this live attenuated virus results to clinical manifestations. Furthermore, serial passages of the attenuated FMDV in BHK-21 cells caused the virus to multiply in the same way as those in the field strains [14,15]. This implies that this attenuated virus has the potential to recover its pathogenicity and thus a threat rather than an aide among livestock. For this reason, live vaccines are not currently in use worldwide.
Adjuvants of FMD vaccine
Inactivated FMD vaccines are commonly produced with as gel- or oil-adjuvants depending on the serotype [16]. Gel vaccines are only used in cattle and are not suitable for pigs due to their short duration of immunity. Therefore, they cannot be applied in the pigs. As a result, the vaccines that have recently been used worldwide are improving in terms of the level of immunity conferred and securing long lasting antibody by using oil for adjuvants. On the other hand, oil-adjuvanted vaccines are known to significantly increase humoral immunity and have superior antibody formation [17]. Oil-adjuvanted vaccines are produced by making antigens through the inactivation of FMDV, purifying the antigens for the removal of non-structural proteins (NSP). While oil adjuvants have various types, the FMD vaccines produced are mainly of the water-in-oil-in-water (W/O/W) type, which are generally created using Montanide ISA206 (Seppic, Paris, France). The oil-adjuvanted vaccines used for FMD are designed to enhance immunity not only in cattle but also in pigs. Oil adjuvants include Montanide ISA50 (water-in-oil [W/O]), ISA70 (W/O), and ISA25 (oil-in-water [O/W]). These show differences in terms of immunity and safety according to oil types [18]. W/O induces cell-mediated immune response, whereas W/O/W and O/W strengthen humoral immunity [18].
Administration routes reinforce the efficacy of the vaccine to elicit local immune responses. For example, even with the administration of same vaccines, subcutaneous or intramuscular injections can induce different immune responses. Barnett et al. [19] reported that local reactions were not observed in the first and second intramuscular injections for cattle, whereas local reactions were detected in injections over 2 mL or the second injections for pigs. According to a report on the side-effects of vaccinations in Israel, eight days after the vaccinations, dairy cattle exhibited urticarial, exudative and necrotic dermatitis that was accompanied by edemas and blisters. The average loss of milk production for an affected cow on this farm was 21.5% per day for seven consecutive days [20].
In Korea, vaccines have been administered, maintaining injection temperatures around 20℃, and animals were treated with extra care to reduce their vaccination stress levels. According to the results of a survey on animal responses after such FMD inoculation practices, no deaths directly resulting from the inoculations were confirmed. In some cases, however, stress, fever, pain, loss of appetite, lethargy, and temporary decrease in milk production and growth rate were observed among the vaccinated animals.
Some complaints have been reported about the vaccinations. Such complaints were likely to have resulted from the fact that the FMD vaccines were oil-based, unlike the vaccine adjuvants that had generally been used in the Korean livestock environment. Moreover, indiscriminate vaccinations in the early stage of FMD outbreaks and vaccine stresses from severe cold were inferred to have generated more complaints about vaccination responses as compared to the response to other conventional vaccines.
Immunogenicity and protection of FMD vaccines in susceptible livestock
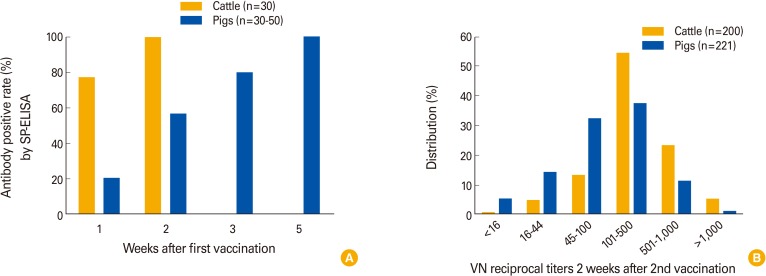
Humoral immunity is known to be the most influential factor in preventing FMD [16]. According to a Korean case in 2010, when FMD vaccines were administered to farm animals with no maternal-derived antibodies, immune antibodies were mostly formed in cattle two weeks after the vaccinations and in pigs four weeks after the vaccinations (Fig. 1A).
Fig. 1.
Antibody levels against the foot-and-mouth disease (FMD) virus O type in susceptible animals after FMD vaccination in the field without maternal-derived antibody during the 2010 to 2011 epidemic in Korea. (A) Antibody levels determined by enzyme-linked immunosorbent assay to viral structural proteins (SP-ELISA) after the first vaccination (or second vaccination). The second vaccination in case of pigs (tested 30-50 animals per week) were vaccinated 4 weeks after first vaccination. (B) Virus neutralizing (VN) reciprocal titers using the field strain (O/Andong/KOR/2010) two weeks after the second vaccination.
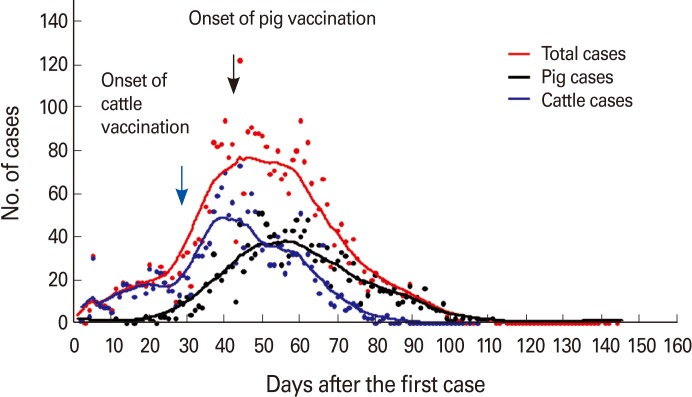
FMD spread in Korean livestock rapidly in late 2010, but nationwide vaccinations prevented its further expansion. The decline in the frequency of FMD occurrences was observed in pigs three weeks after the vaccinations and in cattle two weeks after the vaccinations (Fig. 2). In order to gain the same neutralizing antibody level through vaccination, pigs require a longer period of immunity than cattle do (Fig. 1A, B). In addition, for pigs, which excrete a vast amount of the virus after being infected by FMD, the amount of excreted virus can be reduced greatly after vaccination [10]. In a virus challenge test, the cattle that were put into contact with infected animals for five days, 21 days after the administration of vaccines with high antigen doses, could clinically protect themselves from infection. However, the cattle immunized for ten days with vaccine failed to protect themselves [10]. As for pigs, the pigs immunized for ten days failed to protect against infection in a nine-hour contact challenge test. On the other hand, 75% of the pigs for 28 days after their vaccinations could protect themselves. As for lambs, when they were challenged via contact with infected pigs for nine hours, four days and ten days after their vaccination, they could all protect themselves against the challenge. However, apart from the expression of clinical signs, the amount of excreted virus was confirmed to decrease substantially in vaccinated animals as compared to non-vaccinated animals [10].
Fig. 2.
Diminishment of the foot-and-mouth disease outbreaks after vaccination during the 2010 to 2011 epidemic in Korea. The arrows show the onset of vaccination.
A number of T-cell epitopes were identified in the NSP of FMDV. Immunologically, the inducement of cell-mediated immune responses in vaccinated animals is known to decrease due to the removal of NSP, which is aimed to identify vaccinated and infected animals in the purification process of FMD vaccine manufacturing. Helper T-cells (Th) also recognize epitopes in the capsid proteins and NSP of viruses. Ultimately, T-cell responses induced by CD4+ cells contribute to the protection against FMD by engaging in the production of antibodies to FMDV [21]. In cattle and pigs, the importance of major histocompatibility complex (MHC) II responses against FMD has been demonstrated. Dendritic cells respond to B-cells and act like an antigen presenter. However, they mainly serve as an antigen carrier. Moreover, when a small amount of antigen administrated, the help of T-cells becomes essential. As the polymorphism of MHC molecules exists among animals, resistance levels can also vary across animals. In addition, single factor of humoral immunity is only not involved in the protection against virus challenges. Capsid proteins VP1, VP2, VP3, VP4, and NSP of FMDV are Th epitopes. In fact, immune cells in vaccinated pigs were found to be highly reactive to VP1 and VP4 [21].
In a vaccination case in Korea, pigs were relatively slower to form antibodies and had lower antibody titers, raising the issue of the effectiveness of the vaccine. The vaccine produced higher levels of immunity in cattle. In the initial stage of the vaccinations in Korea, animals were not affected by maternal-derived antibodies, suggesting the likelihood of antibody formation directly following the vaccinations. Moreover, when a large number of piglets were dying, the vaccination of all pigs, even young ones, is assessed to have been an appropriate measure for interrupting of further spread. However, one year after the vaccinations, all animals, including cattle and pigs, inevitably experienced the intervention of maternal-derived antibodies. Therefore, they needed to be re-vaccinated in time for the disappearance of maternal-derived antibodies [22]. In Korea, cattle are vaccinated more than twice as a standard practice, whereas piglets are usually vaccinated only once. However, sows are vaccinated at least three times a year, thereby maintaining high antibody titers. As for piglets, they are vaccinated around 12 to 14 weeks after birth. Korea's nationwide antibody formation rates are determined as being over 95% in cattle and 60-80% in pigs from July 2011 to June 2012, according to enzyme-linked immunosorbent assay tests for antibodies to viral structural proteins.
Given the Korean case in which antibody formation rates were relatively low, the obstacles to antibody formation are inferred to be the intervention of maternal-derived antibodies and improper vaccination sites or methods. As a result, the practice of one shot with one needle is considered essential.
Development Strategy for Improved FMD Vaccine
Shift of vaccine frames using non-pathogenic viruses
The FMD vaccines that are currently used worldwide only consist of inactivated vaccines without introducing live vaccines [17]. When inactivated vaccines are used, live pathogenic viruses are inactivated, thereby completely removing pathogenicity. As a result, they pose no risk of FMD occurrences and guarantee higher levels of safety as compared to live vaccines. However, even the inactivated vaccines go through the process of the mass culturing of live viruses during their manufacturing. Therefore, concerns over the leakage of live viruses remain, and a high level of biosafety is required during production process. In order to resolve such problems, some previous studies made an attempt to switch from inactivated to live vaccines [23,24].
In addition, if live vaccines are used, they might cause the formation of virus carriers. This vaccine type makes it difficult to differentiated from infected and vaccinated animals through serological tests. Furthermore, given the fact that FMD outbreaks are highly likely to be simultaneous and on a large scale, new virus can also make by a recombination of field and vaccine strain [25-27]. For all these reasons, the application of live vaccines is not practical. Therefore, inactivated vaccines are widely used for FMD vaccines, although they confer relatively low levels of immunity and require occasional supplementary vaccinations. Moreover, even when a large amount of virus is cultured in biosafety laboratories or strictly shielded vaccine manufacturing plants, the risk of virus leakage increases in proportion to production volume. Therefore, the handling of live viruses for virus production is not an easy task, and all conditions must be perfectly satisfied [28].
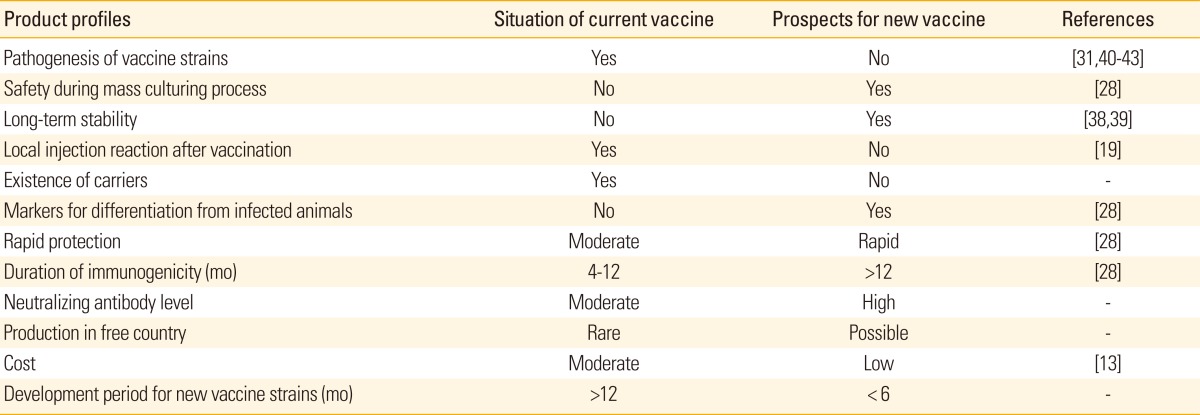
A generally attempted method is to attenuate pathogenic viruses through serial passages in susceptible cells or animals. In relation to this method, studies that attenuate a part of pathogenic viruses by producing infectious cDNA clones using reverse genetics, which is a genetic engineering technique used to secure genome of viruses through cloning, have been actively carried out [23,24,29-31]. If the attenuated strains developed in such a manner are used as seed viruses for inactivated vaccines, even the leakage from mass cultures is likely to reduce the risk of FMD outbreaks (Table 1). If the viruses go through the process of artificial attenuation by deleting or partly replacing some pathogenic FMD genes, such as L, 3A, 3B, 3D and UTR which is aimed at removing pathogenicity in target animals, the attenuated viruses have the potential to be used as vaccine strains [32-35]. Meanwhile, even if attenuated viruses are used, they can cause persistent viral infections in the laryngopharynx of ruminants. Thus, sufficient reviews are necessary for their use, along with paying particular attention to preventing their creation of new pathogenic viruses through recombination with field viruses. Ruminants, such as cattle and goats, have the potential to form carriers due to FMDV. Therefore, the ideal vaccines for ruminants may need to be specifically designed to prevent the creation of carriers (Table 1). While the correlations between carrier formation and vaccination have not been proven to date, animals show no clinical signs once vaccinated, even if they are infected. This difficulty with the observation of clinical signs, in turn, makes the search for removing carrier animals problematic. In terms of a method to prevent persistent infections, the insertion of the genes that can induce an interferon, which is known to be an antiviral substance, or other similar substances into infected target cells may be considered [36,37].
Table 1.
The research trends for the development of new foot-and-mouth disease vaccines
In addition to the method based on reverse genetics, which makes direct use of FMDV genome, the method based on vaccine vectors can be an alternative. In addition, virus-like particles or protein antigens (subunits) can be expressed by reproducing them through the manipulation of FMD protective genes (sequences in P1, VP1, and neutralizing epitopes) so as to make them become expressed in Escherichia coli or mammalian cells in totally different forms. This method has the advantage of safely producing a large volume of vaccines in general live production facilities. In addition, the methods of using human adenoviruses, bacilli, insect viruses, herpes viruses, and mammal cells have recently been introduced. Among these, some methods have shown fairly successful results, including the protective effects of replication-defective systems, such as human adenoviruses [44-53].
Extended shelf life and short development periods
Oil-adjuvanted FMD vaccines are widely used in Korea and in most countries throughout the world. Oil-based adjuvants have slower antigen release rates compared to gel adjuvants, which makes them quick to be absorbed by the body and quick to disappear. Oil-adjuvanted vaccines respond more powerfully to the body. The shelf life of FMD vaccines ranges from 12 to 18 months, which is relatively short given that some other vaccines last more than two years. Thus, the shelf life of FMD vaccines needs to be extended [28].
Development of an inactivated vaccine using a new virus strain takes at least 12 months and the prevention of the spread of novel FMDV types using such a newly developed vaccine is highly difficult. Therefore, manufacture of vaccine should be completed within six months for an immediate application to the circumstances of a new FMD outbreak (Table 1). In this regard, the methods to secure safety and immunogenicity within a short period based on the partial replacement technique targeting certain important protective genes (epitopes) in existing vaccine strains are also under development. In addition, if the stability of vaccine antigens can be improved by adjusting the nature of cold-chain system, this will then eventually lead to a prolonged shelf life of vaccines. Researchers have made an attempt to produce viruses with improved levels of stability by replacing some of the genes in FMDV. To overcome drawbacks of FMDV as a vaccine antigen, which are inactivated at a pH of 6.8 or below and at 56℃ or above, researchers produced viruses in a more stable form under susceptible environments by manipulating the regions related to heat (VP2, VP3) and low-pH resistance (VP1) in FMDV [38,39,54].
Enhancement of immunity/protection and the replacement of adjuvants
When the effects of the FMD vaccines that were recently used in Korea were compared, the immunity in swine was revealed to be lower than that in cattle. In light of this, FMD vaccinations for swine, other than ruminants such as cattle and goats, need to be administered in an accurate and clear manner in consideration of the above result. Because they had already been infected before vaccination or were infected immediately after vaccination, the viruses are occasionally excreted from the animals despite the vaccination [10]. The onset of immunity through inactivated vaccines takes a longer period than that achieved through live vaccines. Moreover, animals inoculated with inactivated vaccines require re-vaccination every four to twelve months for protective immunization [28]. As oil immune adjuvants are absorbed more slowly than their gel equivalents, they can cause local reactions in vaccinated sites. In order to remove such effects, the use of other immune adjuvant types than the oil type, such as nanoparticles and toll-like receptor ligands, should also be taken into account [10,55-57]. However, the global market has not proposed new immune adjuvants that are sufficiently proven to allow them to replace the oil-type adjuvants thus far.
Selection of vaccine strains and the prediction of protective level
Classically, researchers have studied the method for blocking the replication of FMDV in the field, which have the fast formation of variants, by producing inactivated vaccines that have broad antigenic spectrum. However, FMD, by its nature, there is complexity to be prepared polyvalent vaccines that contain multi-serotype viruses. Moreover, preparatory measures are necessary to account for the variations in the viruses spread throughout surrounding regions [28]. When FMD persists for an extended period in a certain region, mutant versions of the field viruses are likely to form. Thus, the vaccine strains capable of against such variations should be selected. In preparation for this, the banks for protective genes of FMDV with broad-range are necessary. Moreover, protective genes should become promptly replaceable via the new methods mentioned earlier. While the development of currently-used antigen banks is important, in the long term, vaccines should be manufactured within short periods so that protective antigens (i.e., gene P1) can be swiftly applied to any contingencies [32]. In addition, the vaccine matching test for field viruses generally takes about one month. Therefore, a system that can quickly project the effects of vaccines through the analysis of the genes related to protection must be established [10].
Differential diagnosis and detection of NSP antibody after routine FMD vaccination
In FMD vaccination, the NSP antibody test can prove which animal is infected, and the test results can be an effective form of evidence confirming FMD infection. The NSP antibody test can prove the absence of FMD within farms [58]. In a South American case involving FMD vaccinations for cattle, the specificity of NSP ELISA tests was 99.05% (n=12,804) in non-vaccinations, 98.49% (n=3,500) in single vaccinations, 97.90% (n=79,649) in multiple vaccinated cattle under two years old, and 95.20% (n=2,517) in multiple vaccinated cattle two years old or older. This confirmed that when vaccinations are applied, vaccination can create the NSP antibody positive animals [59]. When clinical signs or epidemiologic correlations do not exist, it is important to secure the reliability of test results through the evaluation of the profiling of electro-immuno transfer blotting (EITB) and multiple NSP antibodies for the confirmation of the test results [60]. However, while EITB is used only in certain regions, such as South America, it is not globally commercialized, making it difficult to use and evaluate. Currently, regarding animals with NSP antibodies, regular tests are conducted to identify whether virus circulation have occurred, thereby increasing the number of affected animals. However, the culling of animals with NSP antibodies is considered to be the best measure for now. First of all, it is of primary importance that no FMD clinical signs should be observed across all animals. In addition, NSP tests generally confirm that a number of animals have NSP antibodies within a livestock group, rather than a single animal.
Inactivated vaccines used in the world differentiate infected animals from vaccinated animals by using the differences in antibody reactivity through the culturing and purification of viruses. Meanwhile, newly developed vaccines should be a method to distinguish between vaccination and field infection through serological tests, with the introduction of differentiating markers during the vaccine production stage by either deleting or inserting certain genes involved in antibody formation (Table 1). The candidates for the target regions can be 3A or 3B [61].
Evaluation of FMD vaccine
Current antibody detection methods include ELISA and neutralization test. However, they involve the difficulty that individual analyses should be performed on the antibodies against multiple serotypes if polyvalent vaccines are administered. In addition, the antibody titers and actual protection levels in the field often exhibit differences. If evaluations are based on neutralizing antibody levels, the protective efficacy of antibodies can be predicted to some extent in cattle [62]. Even with this method, however, determination of antibody and protection levels using typical viruses cannot perfectly match with those of various viruses [62,63].
As a number of susceptible animals are subject to FMD vaccination, the test methods that use target animals are not readily applicable in practical terms and do not perfectly match with the results of protective efficacy and serological tests. Generally, the evaluation of FMD vaccines is performed through an immunogenicity experiments in cattle. Evaluation of vaccine using small laboratory animals, which is an alternative test method, is known to be difficult [64]. Another problem is the assessment of vaccine efficacy which have not been sufficiently accumulated in pigs. In fact, such tests involve substantial difficulties in their executions because they essentially require biosafety facilities for animal experiment and research.
Ideally, the efficacy of new vaccines should be tested through target animals. However, in light of global trends, verification using only target animals is difficult. Therefore, an appropriate method is likely to be developed by using small animal models with high levels of susceptibility, vaccinating them, and eventually confirming their protection levels. However, given the diversity of FMDVs, a number of challenge viruses should be checked or developed. Whenever vaccine strains are changed, their protective efficacy and antibody formation rates should be re-verified. Furthermore, even though measurement of protection level using immune cells that originate from immunized animals can be an important method of predicting FMD protection [65] with determination of antibody level, a new method that realizes an easier form of detection whenever necessary, in a similar manner to the antibody detection method, should also be developed.
Summary and Conclusions
Nationwide monitoring of vaccination strategies in Korea for over a year revealed that O1 Manisa strain produced lower levels of immune responses in swine as compared to those in cattle. This caused the largest FMD-related controversy in the country. This finding may have resulted from the lower responses of pig immune cells, which appear to be related to the host cells that respond to FMDV [66]. Certain issues also remain to be addressed including the prediction of the immunological correlations between vaccine antigens and field virus, the controversy over the side-effects of oil-adjuvanted vaccines, and the formation of NSP antibodies.
Therefore, the vaccines developed in the future should demonstrate superior effects in terms of the immunogenicity in every species. In addition, a simple selection method for vaccine strains, the improvement of vaccine adjuvants, and the advanced control of vaccines from the stage of vaccine production so as not to create NSP antibodies in the field are all essential requirements. Additionally, the upcoming vaccines should be able to broadly protect immunized animals against various virus types with a single vaccination, regardless of serotypes, topotypes, and subtypes. In both pigs and ruminants, these vaccines should induce high neutralizing antibodies. They must also offer high levels of safety and protective effects after vaccination. In view of this, B- and T-cell epitopes related to protection against each FMDV antigen according to susceptible species should be researched. Moreover, the effective protection mechanism that realizes the cross-immunity of common antigens and emergent protection should also become a research topic.
To develop new FMD vaccines, various approaches with high-technology are necessary. A desirable form is likely to combine the advantages of live and inactivated vaccines. Such vaccines should form high levels of immunity across all susceptible animals. In particular, they should generate sufficient protective effects in ruminants, without persistent infections. The largest change is expected to occur via the development of new vaccine production methods. This includes the use of attenuated high-safety vaccine strains based on techniques such as infectious cDNA cloning, which are, in turn, based on reverse genetics or the use of safe vector vaccines that can be expressed in virus-like particles and directly delivered to animals, instead of the classical method of virus inactivation through the cell culture adaptation of field viruses. If such new methods are developed, even a single vaccination is expected to generate long-term highly protective effects while securing vaccine safety and stability. If vaccines are urgently required for newly spread viruses, to achieve this, an applicable method is likely to be swiftly replacing the specific genes of existing vaccine strains so as to protect against the new viruses. This method should also be done in just a short period of time particularly in the case of an outbreak. In order to select such effective vaccine strains, researchers will need to characterize antigens further as vaccine candidates, build their gene banks, and develop appropriate vaccine strains that can provide a broader range of protection even within the same serotype.
Acknowledgments
We thank the staff of the Disease Control Department at the Animal, Plant and Fisheries Quarantine and Inspection Agency (QIA).
Footnotes
No potential conflict of interest relevant to this article was reported.
This review was supported by the QIA.
References
- 1.Bachrach HL. Foot-and-mouth disease. Annu Rev Microbiol. 1968;22:201–244. doi: 10.1146/annurev.mi.22.100168.001221. [DOI] [PubMed] [Google Scholar]
- 2.Hedger RS, Taylor WP, Barnett IT, Riek R, Harpham D. Simultaneous vaccination of cattle against foot-and-mouth disease and rinderpest. Trop Anim Health Prod. 1986;18:21–25. doi: 10.1007/BF02359652. [DOI] [PubMed] [Google Scholar]
- 3.Yoon H, Yoon SS, Wee SH, Kim YJ, Kim B. Clinical manifestations of foot-and-mouth disease during the 2010/2011 epidemic in the Republic of Korea. Transbound Emerg Dis. 2012;59:517–525. doi: 10.1111/j.1865-1682.2011.01304.x. [DOI] [PubMed] [Google Scholar]
- 4.Dupuis L, Ascarateil S, Aucouturier J, Ganne V. SEPPIC vaccine adjuvants for poultry. Ann N Y Acad Sci. 2006;1081:202–205. doi: 10.1196/annals.1373.024. [DOI] [PubMed] [Google Scholar]
- 5.Cloete M, Dungu B, Van Staden LI, Ismail-Cassim N, Vosloo W. Evaluation of different adjuvants for foot-and-mouth disease vaccine containing all the SAT serotypes. Onderstepoort J Vet Res. 2008;75:17–31. doi: 10.4102/ojvr.v75i1.84. [DOI] [PubMed] [Google Scholar]
- 6.McKercher PD, Graves JH. A review of the current status of oil adjuvants in foot-and-mouth disease vaccines. Dev Biol Stand. 1976;35:107–112. [PubMed] [Google Scholar]
- 7.Andersen AA, Campbell CH. Experimental placental transfer of foot-and-mouth disease virus in mice. Am J Vet Res. 1976;37:585–589. [PubMed] [Google Scholar]
- 8.Mackenzie JS, Slade WR. Evidence for recombination between two different immunological types of foot-and-mouth disease virus. Aust J Exp Biol Med Sci. 1975;53:251–256. doi: 10.1038/icb.1975.27. [DOI] [PubMed] [Google Scholar]
- 9.Knowles NJ, He J, Shang Y, et al. Southeast Asian foot-and-mouth disease viruses in Eastern Asia. Emerg Infect Dis. 2012;18:499–501. doi: 10.3201/eid1803.110908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parida S. Vaccination against foot-and-mouth disease virus: strategies and effectiveness. Expert Rev Vaccines. 2009;8:347–365. doi: 10.1586/14760584.8.3.347. [DOI] [PubMed] [Google Scholar]
- 11.Madhanmohan M, Nagendrakumar SB, Kumar R, et al. Clinical protection, sub-clinical infection and persistence following vaccination with extinction payloads of O1 Manisa foot-and-mouth disease monovalent vaccine and challenge in goats and comparison with sheep. Res Vet Sci. 2012;93:1050–1059. doi: 10.1016/j.rvsc.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 12.Doel TR. Optimisation of the immune response to foot-and-mouth disease vaccines. Vaccine. 1999;17:1767–1771. doi: 10.1016/s0264-410x(98)00444-7. [DOI] [PubMed] [Google Scholar]
- 13.Doel TR. FMD vaccines. Virus Res. 2003;91:81–99. doi: 10.1016/s0168-1702(02)00261-7. [DOI] [PubMed] [Google Scholar]
- 14.Mowat GN, Barr DA, Bennett JH. The development of an attenuated foot-and-mouth disease virus vaccine by modification and cloning in tissue cultures of BHK21 cells. Arch Gesamte Virusforsch. 1969;26:341–354. doi: 10.1007/BF01250944. [DOI] [PubMed] [Google Scholar]
- 15.Polacino P, Kaplan G, Yafal AG, Palma EL. Biochemical characterization of a foot-and-mouth disease virus strain attenuated for cattle: brief report. Arch Virol. 1986;88:143–150. doi: 10.1007/BF01310899. [DOI] [PubMed] [Google Scholar]
- 16.Saiz M, Nunez JI, Jimenez-Clavero MA, Baranowski E, Sobrino F. Foot-and-mouth disease virus: biology and prospects for disease control. Microbes Infect. 2002;4:1183–1192. doi: 10.1016/s1286-4579(02)01644-1. [DOI] [PubMed] [Google Scholar]
- 17.Doel TR. Natural and vaccine-induced immunity to foot and mouth disease: the prospects for improved vaccines. Rev Sci Tech. 1996;15:883–911. doi: 10.20506/rst.15.3.955. [DOI] [PubMed] [Google Scholar]
- 18.Aucouturier J, Dupuis L, Ganne V. Adjuvants designed for veterinary and human vaccines. Vaccine. 2001;19:2666–2672. doi: 10.1016/s0264-410x(00)00498-9. [DOI] [PubMed] [Google Scholar]
- 19.Barnett PV, Pullen L, Williams L, Doel TR. International bank for foot-and-mouth disease vaccine: assessment of Montanide ISA 25 and ISA 206, two commercially available oil adjuvants. Vaccine. 1996;14:1187–1198. doi: 10.1016/s0264-410x(96)00055-2. [DOI] [PubMed] [Google Scholar]
- 20.Yeruham I, Yadin H, Haymovich M, Perl S. Adverse reactions to FMD vaccine. Vet Dermatol. 2001;12:197–201. doi: 10.1046/j.0959-4493.2001.00221.x. [DOI] [PubMed] [Google Scholar]
- 21.McCullough KC, Sobrino F. Immunology of foot-and-mouth disease. In: Sobrino F, Domingo E, editors. Foot and mouth disease: current perspectives. Norfolk: Horizon Biosciences; 2004. pp. 173–222. [Google Scholar]
- 22.Spath EJ, Smitsaart E, Casaro AP, et al. Immune response of calves to foot-and-mouth disease virus vaccine emulsified with oil adjuvant: strategies of vaccination. Vaccine. 1995;13:909–914. doi: 10.1016/0264-410x(95)00009-p. [DOI] [PubMed] [Google Scholar]
- 23.Mason PW, Piccone ME, McKenna TS, Chinsangaram J, Grubman MJ. Evaluation of a live-attenuated foot-and-mouth disease virus as a vaccine candidate. Virology. 1997;227:96–102. doi: 10.1006/viro.1996.8309. [DOI] [PubMed] [Google Scholar]
- 24.Chinsangaram J, Mason PW, Grubman MJ. Protection of swine by live and inactivated vaccines prepared from a leader proteinase-deficient serotype A12 foot-and-mouth disease virus. Vaccine. 1998;16:1516–1522. doi: 10.1016/S0264-410X(98)00029-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jamal SM, Ferrari G, Ahmed S, Normann P, Belsham GJ. Molecular characterization of serotype Asia-1 foot-and-mouth disease viruses in Pakistan and Afghanistan: emergence of a new genetic group and evidence for a novel recombinant virus. Infect Genet Evol. 2011;11:2049–2062. doi: 10.1016/j.meegid.2011.09.015. [DOI] [PubMed] [Google Scholar]
- 26.Lee KN, Oem JK, Park JH, et al. Evidence of recombination in a new isolate of foot-and-mouth disease virus serotype Asia 1. Virus Res. 2009;139:117–121. doi: 10.1016/j.virusres.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 27.Lewis-Rogers N, McClellan DA, Crandall KA. The evolution of foot-and-mouth disease virus: impacts of recombination and selection. Infect Genet Evol. 2008;8:786–798. doi: 10.1016/j.meegid.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 28.Rodriguez LL, Gay CG. Development of vaccines toward the global control and eradication of foot-and-mouth disease. Expert Rev Vaccines. 2011;10:377–387. doi: 10.1586/erv.11.4. [DOI] [PubMed] [Google Scholar]
- 29.Li P, Bai X, Sun P, et al. Evaluation of a genetically modified foot-and-mouth disease virus vaccine candidate generated by reverse genetics. BMC Vet Res. 2012;8:57. doi: 10.1186/1746-6148-8-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li P, Bai X, Lu Z, et al. Construction of a full-length infectious cDNA clone of inter-genotypic chimeric foot-and-mouth disease virus. Wei Sheng Wu Xue Bao. 2012;52:114–119. [PubMed] [Google Scholar]
- 31.Pacheco JM, Piccone ME, Rieder E, Pauszek SJ, Borca MV, Rodriguez LL. Domain disruptions of individual 3B proteins of foot-and-mouth disease virus do not alter growth in cell culture or virulence in cattle. Virology. 2010;405:149–156. doi: 10.1016/j.virol.2010.05.036. [DOI] [PubMed] [Google Scholar]
- 32.Uddowla S, Hollister J, Pacheco JM, Rodriguez LL, Rieder E. A safe foot-and-mouth disease vaccine platform with two negative markers for differentiating infected from vaccinated animals. J Virol. 2012;86:11675–11685. doi: 10.1128/JVI.01254-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li S, Gao M, Zhang R, et al. A mutant of infectious Asia 1 serotype foot-and-mouth disease virus with the deletion of 10-amino-acid in the 3A protein. Virus Genes. 2010;41:406–413. doi: 10.1007/s11262-010-0529-9. [DOI] [PubMed] [Google Scholar]
- 34.Piccone ME, Pacheco JM, Pauszek SJ, et al. The region between the two polyprotein initiation codons of foot-and-mouth disease virus is critical for virulence in cattle. Virology. 2010;396:152–159. doi: 10.1016/j.virol.2009.10.020. [DOI] [PubMed] [Google Scholar]
- 35.Li P, Bai X, Cao Y, et al. Expression and stability of foreign epitopes introduced into 3A nonstructural protein of foot-and-mouth disease virus. PLoS One. 2012;7:e41486. doi: 10.1371/journal.pone.0041486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Avila Botton S, Brum MC, Bautista E, et al. Immunopotentiation of a foot-and-mouth disease virus subunit vaccine by interferon alpha. Vaccine. 2006;24:3446–3456. doi: 10.1016/j.vaccine.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 37.Moraes MP, Chinsangaram J, Brum MC, Grubman MJ. Immediate protection of swine from foot-and-mouth disease: a combination of adenoviruses expressing interferon alpha and a foot-and-mouth disease virus subunit vaccine. Vaccine. 2003;22:268–279. doi: 10.1016/s0264-410x(03)00560-7. [DOI] [PubMed] [Google Scholar]
- 38.Martin-Acebes MA, Vazquez-Calvo A, Rincon V, Mateu MG, Sobrino F. A single amino acid substitution in the capsid of foot-and-mouth disease virus can increase acid resistance. J Virol. 2011;85:2733–2740. doi: 10.1128/JVI.02245-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hegde NR, Maddur MS, Rao PP, Kaveri SV, Bayry J. Thermostable foot-and-mouth disease virus as a vaccine candidate for endemic countries: a perspective. Vaccine. 2009;27:2199–2201. doi: 10.1016/j.vaccine.2009.01.032. [DOI] [PubMed] [Google Scholar]
- 40.Zhu J, Weiss M, Grubman MJ, de los Santos T. Differential gene expression in bovine cells infected with wild type and leaderless foot-and-mouth disease virus. Virology. 2010;404:32–40. doi: 10.1016/j.virol.2010.04.021. [DOI] [PubMed] [Google Scholar]
- 41.Almeida MR, Rieder E, Chinsangaram J, et al. Construction and evaluation of an attenuated vaccine for foot-and-mouth disease: difficulty adapting the leader proteinase-deleted strategy to the serotype O1 virus. Virus Res. 1998;55:49–60. doi: 10.1016/s0168-1702(98)00031-8. [DOI] [PubMed] [Google Scholar]
- 42.Brown CC, Piccone ME, Mason PW, McKenna TS, Grubman MJ. Pathogenesis of wild-type and leaderless foot-and-mouth disease virus in cattle. J Virol. 1996;70:5638–5641. doi: 10.1128/jvi.70.8.5638-5641.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cottam EM, Wadsworth J, Shaw AE, et al. Transmission pathways of foot-and-mouth disease virus in the United Kingdom in 2007. PLoS Pathog. 2008;4:e1000050. doi: 10.1371/journal.ppat.1000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brake DA, McIlhaney M, Miller T, et al. Human adenovirus-vectored foot-and-mouth disease vaccines: establishment of a vaccine product profile through in vitro testing. Dev Biol (Basel) 2012;134:123–133. [PubMed] [Google Scholar]
- 45.D'Antuono A, Laimbacher AS, La Torre J, et al. HSV-1 amplicon vectors that direct the in situ production of foot-and-mouth disease virus antigens in mammalian cells can be used for genetic immunization. Vaccine. 2010;28:7363–7372. doi: 10.1016/j.vaccine.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 46.Ren XG, Xue F, Zhu YM, et al. Construction of a recombinant BHV-1 expressing the VP1 gene of foot and mouth disease virus and its immunogenicity in a rabbit model. Biotechnol Lett. 2009;31:1159–1165. doi: 10.1007/s10529-009-9988-2. [DOI] [PubMed] [Google Scholar]
- 47.Wu Q, Moraes MP, Grubman MJ. Recombinant adenovirus co-expressing capsid proteins of two serotypes of foot-and-mouth disease virus (FMDV): in vitro characterization and induction of neutralizing antibodies against FMDV in swine. Virus Res. 2003;93:211–219. doi: 10.1016/s0168-1702(03)00116-3. [DOI] [PubMed] [Google Scholar]
- 48.Grubman MJ, Mason PW. Prospects, including time-frames, for improved foot and mouth disease vaccines. Rev Sci Tech. 2002;21:589–600. doi: 10.20506/rst.21.3.1360. [DOI] [PubMed] [Google Scholar]
- 49.Mohana Subramanian B, Madhanmohan M, Sriraman R, et al. Development of foot-and-mouth disease virus (FMDV) serotype O virus-like-particles (VLPs) vaccine and evaluation of its potency. Antiviral Res. 2012;96:288–295. doi: 10.1016/j.antiviral.2012.09.019. [DOI] [PubMed] [Google Scholar]
- 50.Remond M, Da Costa B, Riffault S, et al. Infectious bursal disease subviral particles displaying the foot-and-mouth disease virus major antigenic site. Vaccine. 2009;27:93–98. doi: 10.1016/j.vaccine.2008.10.036. [DOI] [PubMed] [Google Scholar]
- 51.Capozzo AV, Wilda M, Bucafusco D, et al. Vesicular stomatitis virus glycoprotein G carrying a tandem dimer of foot and mouth disease virus antigenic site A can be used as DNA and peptide vaccine for cattle. Antiviral Res. 2011;92:219–227. doi: 10.1016/j.antiviral.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 52.Li Z, Yi Y, Yin X, Zhang Z, Liu J. Expression of foot-and-mouth disease virus capsid proteins in silkworm-baculovirus expression system and its utilization as a subunit vaccine. PLoS One. 2008;3:e2273. doi: 10.1371/journal.pone.0002273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li G, Chen W, Yan W, et al. Comparison of immune responses against foot-and-mouth disease virus induced by fusion proteins using the swine IgG heavy chain constant region or beta-galactosidase as a carrier of immunogenic epitopes. Virology. 2004;328:274–281. doi: 10.1016/j.virol.2004.07.025. [DOI] [PubMed] [Google Scholar]
- 54.Mateo R, Luna E, Rincon V, Mateu MG. Engineering viable foot-and-mouth disease viruses with increased thermostability as a step in the development of improved vaccines. J Virol. 2008;82:12232–12240. doi: 10.1128/JVI.01553-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li D. Chitosan can stop or postpone the death of the suckling mice challenged with foot-and-mouth disease virus. Virol J. 2010;7:125. doi: 10.1186/1743-422X-7-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Quattrocchi V, Bianco V, Fondevila N, Pappalardo S, Sadir A, Zamorano P. Use of new adjuvants in an emergency vaccine against foot-and-mouth disease virus: evaluation of conferred immunity. Dev Biol (Basel) 2004;119:481–497. [PubMed] [Google Scholar]
- 57.Batista A, Quattrocchi V, Olivera V, et al. Adjuvant effect of Cliptox on the protective immune response induced by an inactivated vaccine against foot and mouth disease virus in mice. Vaccine. 2010;28:6361–6366. doi: 10.1016/j.vaccine.2010.06.098. [DOI] [PubMed] [Google Scholar]
- 58.Jaworski JP, Compaired D, Trotta M, Perez M, Trono K, Fondevila N. Validation of an r3AB1-FMDV-NSP ELISA to distinguish between cattle infected and vaccinated with foot-and-mouth disease virus. J Virol Methods. 2011;178:191–200. doi: 10.1016/j.jviromet.2011.09.011. [DOI] [PubMed] [Google Scholar]
- 59.Office International des Epizooties. Report of the Meeting of the OIE Ad Hoc Group on Evaluation of Nonstructural Protein Tests for Foot and Mouth Disease Diagnosis; 2002 Oct 2-4; Paris. Paris: Office International des Epizooties; 2002. [Google Scholar]
- 60.OIE World Organisation for Animal Health. Terrestrial Animal Health Code. Chapter 8.5. Foot and mouth disease. Paris: OIE World Organisation for Animal Health; 2012. [Google Scholar]
- 61.Sorensen KJ, Madsen KG, Madsen ES, Salt JS, Nqindi J, Mackay DK. Differentiation of infection from vaccination in foot-and-mouth disease by the detection of antibodies to the non-structural proteins 3D, 3AB and 3ABC in ELISA using antigens expressed in baculovirus. Arch Virol. 1998;143:1461–1476. doi: 10.1007/s007050050390. [DOI] [PubMed] [Google Scholar]
- 62.McCullough KC, De Simone F, Brocchi E, Capucci L, Crowther JR, Kihm U. Protective immune response against foot-and-mouth disease. J Virol. 1992;66:1835–1840. doi: 10.1128/jvi.66.4.1835-1840.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Black L, Francis MJ, Rweyemamu MM, Umebara O, Boge A. The relationship between serum antibody titres and protection from foot and mouth disease in pigs after oil emulsion vaccination. J Biol Stand. 1984;12:379–389. doi: 10.1016/s0092-1157(84)80062-1. [DOI] [PubMed] [Google Scholar]
- 64.OIE World Organisation for Animal Health. Manual of diagnostic tests and vaccines for terrestrial animals. Paris: OIE World Organisation for Animal Health; 2012. [Google Scholar]
- 65.Parida S, Oh Y, Reid SM, et al. Interferon-gamma production in vitro from whole blood of foot-and-mouth disease virus (FMDV) vaccinated and infected cattle after incubation with inactivated FMDV. Vaccine. 2006;24:964–969. doi: 10.1016/j.vaccine.2005.08.108. [DOI] [PubMed] [Google Scholar]
- 66.Sanz-Parra A, Jimenez-Clavero MA, Garcia-Briones MM, Blanco E, Sobrino F, Ley V. Recombinant viruses expressing the foot-and-mouth disease virus capsid precursor polypeptide (P1) induce cellular but not humoral antiviral immunity and partial protection in pigs. Virology. 1999;259:129–134. doi: 10.1006/viro.1999.9717. [DOI] [PubMed] [Google Scholar]