Abstract
Purpose
Neuraminidase (NA) of influenza virus contains stalk region that shows a great deal of variability in both amino acid sequence and length. In this paper, we investigated generation of recombinant influenza viruses that had hepatitis B virus (HBV) B cell epitopes in the NA stalk region as a dual vaccine candidate.
Materials and Methods
We used the WSH-HK reassortant helper virus for rescue of recombinant influenza virus containing HBV epitopes and reverse genetic protocol based on the use of micrococcal nuclease-treated virus cores for reconstitution of ribonucleoproteins.
Results
We successfully generated a chimeric influenza viruses which contained 22 amino acid peptides in the stalk region derived from the surface and pre-surface protein HBV. The growth kinetics of the recombinant viruses was investigated after infection of Madin-Darby canine kidney (MDCK) and Madin-Darby bovine kidney (MDBK) cells and the rIV-BVPreS virus showed higher titer than other viruses in MDCK cells. We also confirmed the presence of HBV epitopes in the chimeric viruses by enzyme-linked immunosorbent assay (ELISA) using anti-HBV polyclonal antibody. When the ratio of recombinant virus verse wild type virus was calculated by ELISA, recombinant viruses exhibited 2 fold higher values than the wild type virus.
Conclusion
These results suggest that chimeric influenza virus which contained foreign antigens can be used as dual vaccine against both HBV and influenza viruses.
Keywords: NA stalk, Chimeric virus, Dual vaccine
Introduction
Viruses have been widely used as vectors to express a variety of genes in vitro and in vivo [1-3]. A lot of effort is being put into the development of viruses as agents to immunize against other infectious agents, including other viruses. Such an approach has a number of advantages. There is a large body of experience in the use of attenuated or avirulent viruses as vaccines. Many of these, such as vaccinia virus or adenovirus has been used to immunize many millions of people, can be potentially developed as vectors to express other antigens, such as those in hepatitis C virus, malaria or human immunodeficiency virus [4-7]. Use of a live virus as a vector to express antigens of other pathogens has many of the advantages of live virus vaccines. This includes the fact that only low initial dose are required, and therefore the expense of vaccine production may be less; that subsequent virus replication leads to the expression of large amounts of the antigen over an extended period of time, and the antigen folds in a more or less native conformation; and that a full range of immunity, including production of cytotoxic T lymphocytes as well of humoral immunity [8-11].
As one of the world's most common infectious diseases, hepatitis B virus (HBV) is a serious worldwide public health concern, with HBV-associated liver disease accounting for more than half a million deaths early year [12]. Although there is an effective prophylactic vaccine currently available to prevention infection, it has a number of characteristics that are suboptimal-multiple doses are needed to elicit long lasting immunity, immunity declines over time, and the vaccine is not effective therapeutically [12].
The reverse genetics system established by Seong and Brownlee [13] to reconstitute influenza gene with viral core proteins for rescue genes and generation of recombinant influenza virus has made it possible to modify the influenza virus genome. In early study, the enzymatic domain of the neuramidase (NA) is held away from the virus envelope by a polypeptide stalk of variable length [14]. Using this method, here, we report the use of reverse genetics to generate mutant influenza viruses expressing a B cell specific epitope of the HBV surface or pre-surface proteins in the NA stalk for the use of dual vaccine to prevent both influenza and HBV infection.
Materials and Methods
Viruses and cells
Influenza virus WSN-HK that contained the NA gene from A/Hong Kong/1/68 (H3N2) and all other genes from A/WSN/33 (H1N1), was obtained from Dr. Yoshi Kawaoka and used to rescue the mutant WSN NA gene. The Madin-Darby bovine kidney (MDBK) cell line was cultured in minimal essential medium containing 10% fetal bovine serum. Madin-Darby canine kidney (MDCK) cells were cultured in the same conditions as were MDBK cells.
Preparation of micrococcal nuclease-treated virus cores
Viral cores, nucleoprotein protein (NP) and polymerase protein (P) were isolated by glycerol and glycerol-cesium chloride (CsCl) gradient centrifugation from Influenza A virus, strain X-31, a reassortant of A/HK/68 and A/PR/8/34, after viral particle disruption with detergents (100 mM Tris-HCl [pH 7.4], 100 mM NaCl, 5 mM MgCl2, 1 mM dithiothreitol, 5% glycerol, 1% NP40). Viral core fraction were separated from sodium dodecyl sulfate polyacrylamide gel electrophoresis and treated with micrococcal nuclease (Sigma, St. Louis, MO, USA) to degrade RNA [13]. Final core proteins were stored at -20℃ for further experiment.
Plasmids for cloning of HBV epitopes
A plasmid pT3WSN (NA15) containing the WSN NA gene flanked by the Ksp632I site and T3 RNA polymerase promoter sequence, was obtained from Dr. Peter Palese (Mount Sinai School of Medicine, New York, NY, USA) [15]. A second plasmid, pT3WSN-NAmut which had additional restriction enzyme sites, SacI and KpnI in the stalk region was made by polymerase chain reaction. Plasmids for the generation of recombinant influenza A viruses were constructed from pT3WSN-NAmut by inserting nucleotides derived from HBV surface antigen between 139-147 or pre-surface antigen in the region encoding the NA stalk respectively. An NA ribonucleoprotein (RNP) complex was prepared by in vitro transcription of pT3WSN-NAmut with T3 RNA polymerase in the presence of the NP and P for the generation of mutant influenza viruses after these plasmids were digested with Ksp632I and filled in with Klenow fragment.
Recombinant influenza A viruses rescue
The NA RNP complex was transfected into 70% to 80% confluent MDBK cells infected 1 hour before transfection with WSN-HK at a multiplicity of infection (MOI) of 1. Eighteen hours after transfection, transfectants in the supernatant were plaqued on MDBK cells and then plaque purified three times in MDBK cells.
Viral growth properties in vitro
The ability of recombinant viruses to grow in MDBK and MDCK cells was determined by analyzing multiple replication cycles. Confluent MDBK and MDCK cell monolayers grown on 6 well plates were washed with phosphate-buffered saline, overlaid with 0.5 mL of diluted virus suspension (to achieve a MOI of 0.01 plaque-forming unit [PFU]/cell), and incubated at room temperature (RT) for 40 minutes. The virus suspension was then removed by aspiration, and 3 mL of minimal essential medium was added. Sample supernatants were collected at 12-hour intervals until 72 hours after inoculation. The virus titer of the sample was determined by plaque assay on MDBK and MDCK cells.
Enzyme-linked immunosorbent assay (ELISA)
Recombinant influenza viruses expressing HBV epitopes at 80 hemagglutination unit (HAU)/50 µL concentration with two fold serial dilution were used as a coating antigen on 96-well microtiter plates. After incubation for 1 hour at RT, plates were washed once with phosphate buffered saline (PBS) and then incubated at 37℃ for 1 hour in 0.1% bovine serum albumin-PBS to block the remaining binding sites. After removal of the blocking buffer and washing, HBV polyclonal antibody at 2 µg/mL was added in each well of microtiter plates and the plates were incubated at 37℃ for 1 hour. The plates were washed again (3 times with PBST), a 1:1,000 dilution of alkaline phosphatase conjugated solution for 1 hour at RT. This was followed by removal of the conjugate, washing and addition of p-nitrophenyl phosphate as a substrate. Finally, absorbance was read at 405 nm.
Results
Generation of recombinant viruses with an HBV surface or pre-surface protein epitopes in the NA stalk
Recombinant influenza A viruses were generated by a RNP transfection based reverse genetic system. In previous study, Seong and Brownlee [13] used RNA transcribed in vitro and micrococcal nuclease-treated virus cores proteins (purified NP and P) for genetic rescue into influenza virus. Using the same procedure, we attempted to rescue recombinant influenza A viruses which contained additional amino acid peptides in the stalk region derived from the surface and pre-surface protein of HBV. The rescue system depends on the fact that the NA gene of WSN (H1N1) virus is responsible for plaque formation of the virus in MDBK cells without trypsin protease. Hence, the WSN-HK reassortant virus, which contains only the NA gene from A/Hong Kong/1/68 (H3N2) virus and the rest of the genes from WSN virus, can be used as a helper virus to rescue the WSN NA gene (Fig. 1). Because the WSN-HK virus does not plaque on MDBK cells, the rescue of the WSN NA gene allows the virus to plaque in these cells. In this study, we generated two chimeric influenza A viruses rIV-BVS which has additional 22 amino acids derived from HBV surface antigen and rIV-BVPreS2 which has same number of epitope sequences derived from HBV pre-S2 genome in the same place in stalk region (Fig. 2) and wild type virus using wild type NA gene from WSN virus as a control. These recombinant viruses were harvested at 18 hours after transfection of RNP complex in the cell supernatants and then plaque purified three times in MDBK cells.
Fig. 1.
Generation of recombinant influenza A virus. Reconstituted ribonucleoprotein (RNP) complex which has RNA in vitro transcribed with foreign epitopes and functional viral core proteins was transfected into Madin-Darby bovine kidney (MDBK) cells that had been infected with WSN-HK helper virus. Recombinant influenza A virus was selected by plaque assay on MDBK cells in the absence of protease and further amplified in MDBK cells. NA, neuraminidase; NP, nucleoprotein.
Fig. 2.
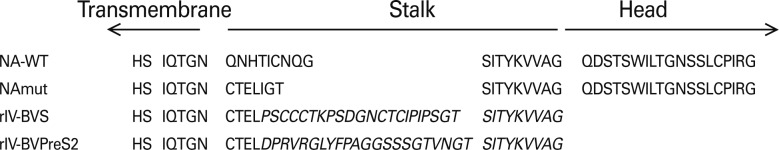
Amino acid sequences of the neuraminidase (NA) stalk mutants from residues 36 to 80 of WSN NA. The B cell epitope sequences derived from HBV surface (rIV-BVS) and PreS2 (rIV-BVPreS2) protein are italicized. NAmut is the partial amino acid sequences of mutant NA on the intermediate cloning vector, pT3WSN-NAmut, for introducing foreign epitopes.
Growth phenotype of recombinant influenza A viruses expressing a HBV epitope
To access the effect of the replacement of the NA gene segment in WSN virus on subsequent virus amplification in cells, we infected triplicate samples of near confluent MDBK cells with rIV-BVS, rIV-BVPreS2 and WSN virus at a low MOI (0.5) and monitored virus replication by assaying culture supernatants. Both rIV-BVS and rIV-BVPreS2 had maximal titers (7.7 and 7.9 log10 PFU/mL, respectively) similar to wild type WSN virus (7.4 log10 PFU/mL) (Fig. 3A). Although the peak titers of all three viruses were similar, rIV-BVS reach early to the maximum titer at 36 hours compare to WSN wt virus at 72 hours. Additionally, multiple cycle growth curves were performed using MDCK cells. Both rIV-BVS, rIV-BVPreS2 reached maximal titers of 8.3 log10 PFU/mL, at 72 hours (Fig. 3B). On the other hand, WSN wt virus showed lower maximal titer of 7.5 log10 PFU/mL at 36 hours then recombinant viruses (p<0.05) and the viral titer slightly decreased until 72 hours (Fig. 3B).
Fig. 3.
Growth properties of recombinant influenza A viruses. rIV-BVS and rIV-BVPreS2 were cultured in Madin-Darby bovine kidney (MDBK) (A) and Madin-Darby canine kidney (MDCK) (B) cells for 72 hours then the virus titer of the sample was determined by plaque assay. PFU, plaque-forming unit.
Binding reactivity of recombinant influenza A viruses against HBV specific antibody
To determine whether the HBV epitopes that expressed in the NA stalk are exposed on the surface of the recombinant influenza viruses, we tested the reactivity of the anti-HBV polyclonal antibody to rIV-BVS and rIV-BVPreS2. In an ELISA, the anti-HBV polyclonal antibody reacted with the rIV-BVS and rIV-BVPreS2 but the WSN virus that had wild type NA protein showed only background level in the lowest diluted fraction (Fig. 4). A polyclonal antibody to the HBV reacted with both rIV-BVS and rIV-BVPreS2 but the intensity of the reaction with the rIV-BVPreS2 was weaker than the intensity of the reaction with the rIV-BVS.
Fig. 4.
Binding properties between recombinant influenza A viruses and hepatitis B virus (HBV) antibody. rIV-BVS and rIV-BVPreS2 were coated on the microtiter plates and tested the binding activity of the anti-HBV polyclonal antibody by enzyme-linked immunosorbent assay.
Discussion
The NA of influenza A viruses is a surface glycoprotein composed of a single polypeptide chain. The NA protein consists of a boxlike head composed of four roughly spherical subunits and a centrally attached stalk containing a hydrophobic region by which the molecule is embedded in the viral membrane. The number and sequence of the amino acid residues in the stalk region vary considerably among different viruses, even within the same subtypes. This suggests that the NA stalk does not impose rigid structural constraints on the insertion of amino acid sequences, making this portion an ideal region for inserting foreign epitopes [16,17]. In this paper, we generate the recombinant influenza A viruses containing a B cell-specific epitope of HBV surface or pre-S2 protein in the NA stalk. As we expected, the results revealed that recombinant influenza A viruses, rIV-BVS or rIV-BVPreS2 containing immunodominant B cell epitopes from HBV surface or pre-S2 proteins in the stalk region of the NA gene were effectively generated by reverse genetic system and showed similar biological properties in growth kinetics and plaque formation comparing wild type of parental virus in vitro.
One interesting finding is that the recombinant influenza virus rIV-BVPreS2 containing 22 additional amino acids from HBV PreS2 protein in NA stalk showed higher growth phenotype then neither rIV-BVS or wild type WSN in MDCK not MDBK cell culture. In fact, viral replication in tissue culture correlated closely with NA activity to prevent aggregation of the virus particles on the cell surface. Because the new influenza virions are assembled at the host-cell surface membrane and release by a process of budding in which both hemagglutinin and NA are involved. During this process, viral NA has the important function of cleaving sialic acid from viral and cellular glycoproteins, thus preventing virus aggregation and allowing individual virions to be release from the cells. But this also depends on the properties of the infected cell. Some cells may allow many viral replication cycles to occur without specific damage to themselves but need protease activity such as trypsin to activate the newly released virions. For example, MDCK cell required exogenous protease for vigorous influenza viral replication. So one possibility to explain high yield of rIV-BVPreS2 in MDCK cells is the additional amino acid residues in the stalk region may change the structural conformation of NA protein and this affect the NA activity to increase viral growth yield in MDCK cell culture even without exogeneous trypsin.
In recent reports, Castrucci et al. [18] reported protection against lethal lymphocytic choriomeningitis virus (LCMV) infection in mice immunized with influenza virus containing a LCMV epitope recognized by cytotoxic T lymphocytes. Another approach, foreign epitopes were inserted into the globular head portion of the hemagglutinin molecule [19]. Thus, both surface glycoproteins of influenza virus can be used for incorporating foreign epitopes. Finally, taken together, our result may provide a reliable approach to deliver efficacious vaccines against HBV and other infectious diseases even need further experiments such as a lethal challenge with both influenza virus and HBV.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Baum C, Schambach A, Bohne J, Galla M. Retrovirus vectors: toward the plentivirus? Mol Ther. 2006;13:1050–1063. doi: 10.1016/j.ymthe.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 2.Li C, Bowles DE, van Dyke T, Samulski RJ. Adeno-associated virus vectors: potential applications for cancer gene therapy. Cancer Gene Ther. 2005;12:913–925. doi: 10.1038/sj.cgt.7700876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Young LS, Searle PF, Onion D, Mautner V. Viral gene therapy strategies: from basic science to clinical application. J Pathol. 2006;208:299–318. doi: 10.1002/path.1896. [DOI] [PubMed] [Google Scholar]
- 4.Arribillaga L, de Cerio AL, Sarobe P, et al. Vaccination with an adenoviral vector encoding hepatitis C virus (HCV) NS3 protein protects against infection with HCV-recombinant vaccinia virus. Vaccine. 2002;21:202–210. doi: 10.1016/s0264-410x(02)00456-5. [DOI] [PubMed] [Google Scholar]
- 5.Fournillier A, Gerossier E, Evlashev A, et al. An accelerated vaccine schedule with a poly-antigenic hepatitis C virus MVA-based candidate vaccine induces potent, long lasting and in vivo cross-reactive T cell responses. Vaccine. 2007;25:7339–7353. doi: 10.1016/j.vaccine.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 6.Kent S, De Rose R, Rollman E. Drug evaluation: DNA/MVA prime-boost HIV vaccine. Curr Opin Investig Drugs. 2007;8:159–167. [PubMed] [Google Scholar]
- 7.Reyes-Sandoval A, Berthoud T, Alder N, et al. Prime-boost immunization with adenoviral and modified vaccinia virus Ankara vectors enhances the durability and polyfunctionality of protective malaria CD8+ T-cell responses. Infect Immun. 2010;78:145–153. doi: 10.1128/IAI.00740-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu MA. Immunologic basis of vaccine vectors. Immunity. 2010;33:504–515. doi: 10.1016/j.immuni.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Bråve A, Ljungberg K, Wahren B, Liu MA. Vaccine delivery methods using viral vectors. Mol Pharm. 2007;4:18–32. doi: 10.1021/mp060098+. [DOI] [PubMed] [Google Scholar]
- 10.Flatz L, Hegazy AN, Bergthaler A, et al. Development of replication-defective lymphocytic choriomeningitis virus vectors for the induction of potent CD8+ T cell immunity. Nat Med. 2010;16:339–345. doi: 10.1038/nm.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ulmer JB, Wahren B, Liu MA. Gene-based vaccines: recent technical and clinical advances. Trends Mol Med. 2006;12:216–222. doi: 10.1016/j.molmed.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 12.Michel ML, Deng Q, Mancini-Bourgine M. Therapeutic vaccines and immune-based therapies for the treatment of chronic hepatitis B: perspectives and challenges. J Hepatol. 2011;54:1286–1296. doi: 10.1016/j.jhep.2010.12.031. [DOI] [PubMed] [Google Scholar]
- 13.Seong BL, Brownlee GG. A new method for reconstituting influenza polymerase and RNA in vitro: a study of the promoter elements for cRNA and vRNA synthesis in vitro and viral rescue in vivo. Virology. 1992;186:247–260. doi: 10.1016/0042-6822(92)90079-5. [DOI] [PubMed] [Google Scholar]
- 14.Blok J, Air GM. Variation in the membrane-insertion and "stalk" sequences in eight subtypes of influenza type A virus neuraminidase. Biochemistry. 1982;21:4001–4007. doi: 10.1021/bi00260a015. [DOI] [PubMed] [Google Scholar]
- 15.Enami M, Luytjes W, Krystal M, Palese P. Introduction of site-specific mutations into the genome of influenza virus. Proc Natl Acad Sci U S A. 1990;87:3802–3805. doi: 10.1073/pnas.87.10.3802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Castrucci MR, Kawaoka Y. Biologic importance of neuraminidase stalk length in influenza A virus. J Virol. 1993;67:759–764. doi: 10.1128/jvi.67.2.759-764.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Castrucci MR, Bilsel P, Kawaoka Y. Attenuation of influenza A virus by insertion of a foreign epitope into the neuraminidase. J Virol. 1992;66:4647–4653. doi: 10.1128/jvi.66.8.4647-4653.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Castrucci MR, Hou S, Doherty PC, Kawaoka Y. Protection against lethal lymphocytic choriomeningitis virus (LCMV) infection by immunization of mice with an influenza virus containing an LCMV epitope recognized by cytotoxic T lymphocytes. J Virol. 1994;68:3486–3490. doi: 10.1128/jvi.68.6.3486-3490.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kalyan NK, Lee SG, Wilhelm J, et al. Immunogenicity of recombinant influenza virus haemagglutinin carrying peptides from the envelope protein of human immunodeficiency virus type 1. Vaccine. 1994;12:753–760. doi: 10.1016/0264-410x(94)90228-3. [DOI] [PubMed] [Google Scholar]





