Abstract
Background
Improving adherence to insulin treatment for better glycemic control remains a challenge in the management of diabetes. New technological aids are required to help support adherence. This study evaluated preference for the NovoPen® 5 (NP5), a durable insulin pen with memory function, compared with the HumaPen Luxura® (HPL) among patients with diabetes and health care professionals.
Methods
This crossover, multicenter usability study included insulin pen-experienced patients with diabetes and health care professionals treating patients with diabetes in Canada, China, and Germany. Participants evaluated NP5 and HPL in a randomized order by performing handling tasks in a usability test related to everyday use during a face-to-face interview. Tasks, pens, and preferences were assessed by completing a questionnaire comprised of rating and open-ended questions relating to confidence in everyday diabetes management.
Results
Overall, 300 patients with diabetes and 150 health care professionals participated in the study. Significantly more participants preferred NP5 (81%) to HPL (18%) (P < 0.001). Also, 82% of patients with diabetes had more confidence in NP5 for managing their daily injections versus 11% with HPL (P < 0.001), and 7% had no preference. Memory function was most helpful in giving patients with diabetes confidence about when they last injected (63%), how much insulin they last injected (62%) and improving diabetes management (55%). Participants gave higher ratings to NP5 than to HPL on all parameters relating to performing an injection (ease of handling, satisfaction when using the pen, convenience of using the pen day-to-day, quality of the pen, and the extent to which the pen meets their needs; P < 0.05 for all comparisons).
Conclusion
NP5 was preferred to HPL by most participants. Significantly more patients with diabetes had more confidence for managing daily insulin injections when using NP5, the pen with a memory function.
Keywords: diabetes, durable insulin pen, memory function, confidence, usability, patient preference
Introduction
Diabetes imposes an increasing health and economic burden worldwide.1 Globally, 12% of health expenditure was spent on diabetes in 2010.2 The worldwide prevalence of diabetes was estimated to be 8.3% in 2011, and is predicted to rise to 9.9% by 2030.2 Among the factors associated with this growing epidemic, self-management of the disease and maintaining independence are important life goals for patients with diabetes.3
All people with type 1 diabetes require life-long insulin administration,4 and many patients with type 2 diabetes will eventually require treatment with exogenous insulin for effective glycemic control.5,6 Management of diabetes is complicated, and considerable heterogeneity is found in the insulin treatment regimens used in everyday diabetes care.7 However, many patients require complex insulin regimens, involving multiple injections each day. Patient adherence to these complex regimens is a major factor in the success of treatment. Diabetes poses a particular challenge for adherence because it is a chronic illness, and patients may not be immediately aware of the long-term consequences of poor adherence.8 Forgotten or omitted insulin injections occur among all populations of insulin users and lead to poor glycemic control.9–12 Fear of hypoglycemia through double-dosing may be a factor in the omission of insulin doses.13
Several studies have shown that patients with diabetes prefer the ease of use, discretion, flexibility, portability, and convenience of insulin pens compared with insulin injection using vials and syringes.14–18 Possibly because of these factors, adherence to insulin treatment improves when patients switch from vials and syringes to insulin pens.19–21
Many patients with diabetes, and particularly those who have to adjust premeal insulin doses in response to daily changes in their glucose levels, would benefit from a memory aid such as a memory function on insulin pens.22 The memory function of an insulin pen may be an important feature for patients with diabetes who are prone to omitting or forgetting their insulin injections, including people with demanding lifestyles and those who may be cared for by others, such as people in nursing and residential homes.
NovoPen® 5 (NP5, Novo Nordisk A/S, Bagsværd, Denmark) is a durable new insulin pen based on the design and technology of NovoPen® 4 (NP4, Novo Nordisk A/S), but with the addition of a simple memory function that records the dose of and hours passed since the last injection.
In a previous study, patients with diabetes and health care professionals reported a significant preference for NP5, in relation to ease of use, and ease of learning to use, compared with HumaPen® Memoir™, another commercially available insulin pen with a memory function.23 The purpose of this study was to evaluate preference for NP5 compared with HumaPen Luxura® (HPL), a durable and widely used insulin pen (without a memory function), among patients and health care professionals in Canada, China, and Germany.
Materials and methods
This crossover, multicenter usability study recruited patients with diabetes and experience of using insulin pens and health care professionals who had at least 2 years’ experience of treating patients with diabetes. The test was managed, conducted, and analyzed by an independent clinical research organization (Aequus Research Ltd, London, UK). Participants were recruited from Canada, China, and Germany by local market research institutes familiar with health care industry research procedures. The study was carried out in accordance with the Declaration of Helsinki Ethical Principles for Medical Research in Human Subjects.24 In line with good medical practice procedures, informed consent and confidentiality agreements regarding test products were obtained before any test-related activities were initiated.
Inclusion criteria
Inclusion criteria were male or female gender, age ≥ 18 years, either type 1 or type 2 diabetes, and using an insulin pen for at least 3 months previously. A minimum of 25% of patients were to be injecting basal insulin alone, a minimum of 25% were to be injecting premixed insulin, and a minimum of 25% were to be injecting basal plus bolus insulin. The study also recruited health care professionals with a minimum of 2 years’ experience of treating diabetes, of whom 33% were diabetes specialists, 33% were specialist diabetes nurses, and 33% were general practitioners. A maximum of 33% of patients were to be NP4 users and a maximum of 33% of patients were to be HPL users.
Exclusion criteria
Exclusion criteria included mental or physical incapacity precluding an adequate understanding of the test procedure, any personal or family ties to a pharmaceutical or market research company, any known allergy to the test products, any disease that may interfere with the tests, and participation in a previous usability test or market research with insulin pens within the previous 3 months.
Materials and procedures
The insulin pens tested were NP5 (lot numbers BV40107, BV40108) fitted with PenFill® cartridges (lot number YS64107) containing inert test medium (Novo Nordisk A/S) and HPL (lot numbers A131297, A822895, A742762, A802480) with 3 mL Humalog® cartridges (lot number A954149; Eli Lilly and Co, Indianapolis, IN). All pens were fitted with NovoFine® 6 mm 32-gauge tip extra-thin wall needles (Novo Nordisk A/S), which were compatible with both pens tested.25
Participants were prescreened by telephone for suitability and then invited to participate in the test, which was carried out during one face-to-face interview lasting approximately 60 minutes. Each participant was randomly assigned to start with either NP5 or HPL, with 50% of the participants evaluating NP5 first and 50% of the participants evaluating HPL first. During the test, the participants were asked to fill out three questionnaires, as summarized in Table 1. The participants were introduced to one pen at a time by a trained interviewer and during this process, the participants were instructed on how to use the pens according to the manufacturer’s guide for each pen.
Table 1.
Summary of the three questionnaires handed out during and after the test
| Question | Available responses on a 5-point, 6-point, or 10-point scale |
|---|---|
| How would you rate the length of this pen? | 1 = far too short; 3 = just right; 5 = far too long |
| How would you rate the width/diameter of this pen? | 1 = far too narrow; 3 = just right; 5 = far too wide |
| How robust does the pen feel? | 1 = not robust at all; 6 = very robust |
| How much do you like the grip of this pen? | 1 = do not like it at all; 6 = like it very much |
| How much do you like the color of this pen? | 1 = do not like it at all; 6 = like it very much |
| How much do you like the shape of this pen? | 1 = do not like it at all; 6 = like it very much |
| Overall, how much do you like the appearance of this pen? | 1 = do not like it at all; 6 = like it very much |
| How easy or difficult was it to handle this device? | 1 = very difficult; 6 = very easy |
| Overall, how satisfied were you when using this device? | 1 = not at all satisfied; 6 = very satisfied |
| Overall, how convenient would it be for you to use this pen on a day-to-day basis? | 1 = not at all convenient; 6 = very convenient |
| Overall, how would you rate the quality of this pen? | 1 = very poor; 6 = very high |
| To what extent, if any, does this pen meet your needs/the needs of your patients? | 1 = to no extent at all; 6 = completely meets needs |
| How much do you think the memory function would help you to feel more confident about: | |
| • When you took your last dose of insulin? | 0 = no help at all; 10 = extremely helpful |
| • How much insulin you last took? | 0 = no help at all; 10 = extremely helpful |
| How much do you think the memory function would reduce how often you measure your blood glucose levels when: | |
| • You have forgotten your last dose of insulin? | 0 = no help at all; 10 = extremely helpful |
| • You are unsure if you took your last dose of insulin? | 0 = no help at all; 10 = extremely helpful |
| • You are unsure how much insulin you took? | 0 = no help at all; 10 = extremely helpful |
| How much do you think the memory function would: | |
| • Help improve your diabetes management? | 0 = no help at all; 10 = extremely helpful |
| • Help you to be more compliant? | 0 = no help at all; 10 = extremely helpful |
| • Help you keep your blood sugar levels more stable? | 0 = no help at all; 10 = extremely helpful |
| Which of the two devices, with which you performed an injection earlier did you prefer? | 1 = device A; 2 = device D; 3 = neither |
| How likely are you to switch from your current device to device A/device D? | 1 = not likely at all; 6 = very likely |
| Which of the two devices would give you the most confidence in managing your/your patients’ daily insulin injections? | 1 = device A; 2 = device D; 3 = neither |
Participants were asked questions relating to the design of the pen (Table 1). They then performed the following tasks: inserted the cartridge; attached the needle to the pen; did a flow check; dialed a dose of 30 U; corrected the dose from 30 U to 15 U; and injected doses of 15 U, 7 U, and 35 U into a foam cushion. Participants also activated the memory function of NP5 and read the size of and hours elapsed since the last dose.
After handling the pen, participants were asked to rate the ease of handling and other questions related to the device (Table 1). Finally, all participants were asked about the importance of a memory function as a feature of an insulin pen. After participants had used and evaluated both pens, they were asked which of the two pens they preferred.
Statistical analysis
The statistical significance level applied throughout the statistical analyses was 5%, so all confidence intervals were 95%. All tests were conducted as two-sided tests.
The primary objective of the usability study was to evaluate preference for NP5 compared with HPL among patients with diabetes and health care professionals. A binomial proportion test was used to analyze the primary endpoint where the proportion preferring NP5 was equal to 50%. McNemar’s test was applied to analyze binomial responses for both test pens to compare the probability parameter when they were evaluated by the same person.
Secondary endpoints were the rating questions on the memory function, ease of handling, satisfaction, convenience, quality, and meeting needs (answers given on an ordinal 5-point or 6-point scale) and these were tested by the Wilcoxon signed rank test. Participants were also asked open-ended questions relating to the reasons for their preference (these questions were not compared statistically).
Results
The characteristics of the study participants are shown in Table 2. All patients participating in the study had at least 3 months’ experience of using insulin pens, with mean pen use duration of 6.6 years. Seventy-five percent (225/300) of the patients had type 2 diabetes. The proportion of patients with diabetes and experience with NP4 enrolled in the study (35%) was slightly over the target (33%).
Table 2.
Baseline characteristics of participants
| Variable | %* |
|---|---|
| Patients with diabetes, n | 300 |
| Canada, n | 100 |
| China, n | 100 |
| Germany, n | 100 |
| Age | |
| 18–30 years | 11 |
| 31–64 years | 65 |
| ≥65 years | 24 |
| Gender, male:female | 50:50 |
| Type 1 diabetes | 25 |
| Type 2 diabetes | 75 |
| Mean years using a pen | 6.6 |
| Current pen use** | |
| NovoPen® 4 | 35 |
| HumaPen Luxura® | 26 |
| NovoPen® 3 | 17 |
| SoloStar® | 7 |
| BerliPen® | 5 |
| ClikStar® | 4 |
| FlexPen® | 4 |
| HumaPen® Ergo | 2 |
| TactiPen® | 2 |
| HumaPen® Memoir | 1 |
| KwikPen™ | 1 |
| OptiPen® Pro | 1 |
| HumaPen Luxura® HD | 1 |
| Other | 11 |
| Health care professionals, n | 150 |
| Canada, n | 50 |
| China, n | 50 |
| Germany, n | 50 |
| Diabetes physicians, n | 59 |
| Diabetes nurses, n | 34 |
| General practitioners, n | 57 |
| Age | |
| 18–30 years | 5 |
| 31–64 years | 91 |
| ≥65 years | 4 |
| Gender, male:female | 43:57 |
| Which pens for insulin use are you familiar with** | |
| NovoPen® 4 | 93 |
| NovoPen® 3 | 83 |
| HumaPen Luxura® | 76 |
| HumaPen® Memoir | 56 |
| SoloStar® | 55 |
| ClikStar® | 43 |
| FlexPen® | 35 |
| BerliPen® | 33 |
| KwikPen™ | 32 |
| BD Pen | 31 |
| Autopen® | 31 |
| OptiPen® Pro | 27 |
| HumaPen Luxura® HD | 25 |
| OptiClik® | 20 |
| HumaPen® Ergo | 19 |
| TactiPen® | 17 |
Notes: n, number of subjects;
percentage values unless otherwise stated;
more than one answer permitted.
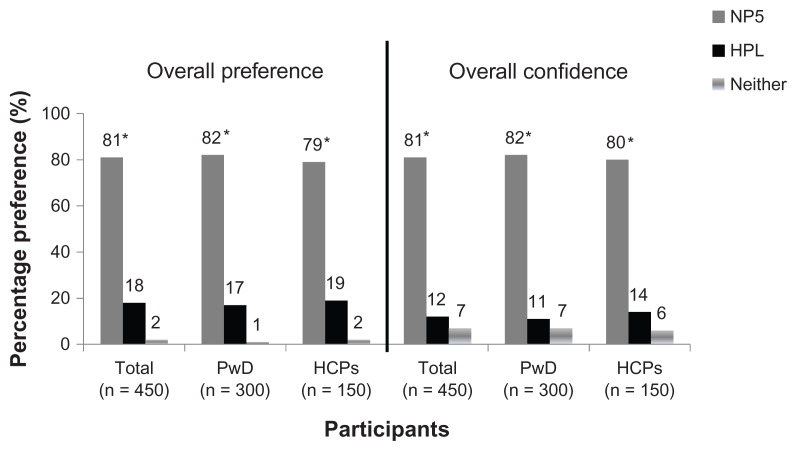
Preference
Significantly more patients rated NP5 as their preferred pen (82%) compared with HPL (17%), and 1% stated they had no preference (Figure 1, P < 0.001 for NP5 versus HPL). Similarly significantly more health care professionals rated NP5 as the pen they preferred (79%) compared with HPL (19%, P < 0.001) and 2% stated that they had no preference. In open-ended questions, 56% of the patients stated that presence of a memory function and 21% stated the shape of the pen as their main reason for preferring NP5. Among patients who preferred HPL, 34% stated the material of the pen and 33% stated its grip and feel was the main reason for their preference.
Figure 1.
Overall confidence of all participants (PwD and HCP) in NP5 compared with HPL for management of daily insulin injections (PwD) or patients’ ability to manage their daily injections (HCP).
Note: *P < 0.001 NP5 vs HPL.
Abbreviations: HCP, health care professionals; HPL, HumaPen Luxura®; NP5, NovoPen® 5; PwD, patients with diabetes.
Confidence in managing daily insulin injections
Significantly more patients stated that NP5 (82%) would give them more confidence in managing their daily insulin injections compared with HPL (11%, P < 0.001), and 7% had no preference for either pen (Figure 1). Similarly, significantly more health care professionals stated that NP5 (80%) would give their patients most confidence in managing their daily insulin injections compared with HPL (14%, P < 0.001), and 6% had no preference for either pen.
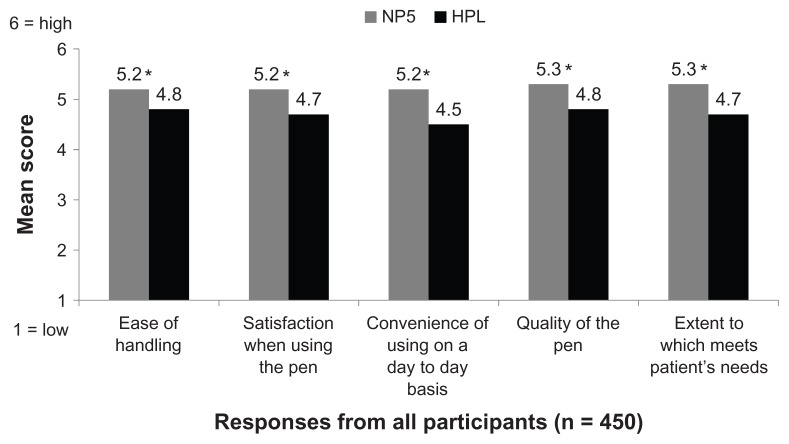
Pen handling
Participants rated NP5 significantly higher than HPL when asked how easy it was to handle the pen, how satisfied they were with using the pen, how convenient it would be to use the pen on a day-to-day basis, how they rated the quality of the pen, and to what extent the pen met their needs/the needs of their patients (Figure 2; P < 0.001 for all between-pen comparisons).
Figure 2.
Participants’ responses to handling questions relating to NP5 compared with HPL.
Note: *P < 0.001 NP5 vs HPL.
Abbreviations: HPL, HumaPen Luxura®; NP5, NovoPen® 5.
Among patients with diabetes who were not already using HPL, 116/216 (54%) would be likely to switch to NP5 but not to HPL, and 11/216 (5%) would be likely to switch to HPL but not to NP5 (P < 0.001).
Memory function
Patients with diabetes reported that the most helpful attribute of NP5 memory function was in assisting them to feel more confident about when they took their last dose of insulin and how much insulin they last took (Table 3). Other aspects the patients felt would be improved by a memory function included: it would help improve their daily diabetes management; it would reduce how often they had to monitor their blood glucose; and it would help keep blood sugar levels more stable (Table 3).
Table 3.
Responses of patients with diabetes (n = 300) to questions on “How much do you think memory function would…”
| Response of patients with diabetes (%) | ||||
|---|---|---|---|---|
|
|
||||
| 0–2 no help at all | 3–7 | 8–10 extremely helpful | Mean score | |
| Help feel more confident about when took last dose | 9 | 26 | 63 | 7.5 |
| Help feel more confident about how much insulin they last took | 10 | 28 | 62 | 7.4 |
| Reduce how often monitor blood glucose levels when have forgotten to inject | 22 | 34 | 44 | 6.0 |
| Reduce how often monitor blood glucose levels when unsure if took dose | 18 | 28 | 54 | 6.4 |
| Reduce how often monitor blood glucose levels when unsure how much taken | 18 | 33 | 48 | 6.3 |
| Improve diabetes management | 12 | 32 | 55 | 6.9 |
| Help to be more compliant | 17 | 32 | 50 | 6.3 |
| Help keep blood sugar levels more stable | 21 | 29 | 49 | 6.1 |
Health care professionals rated NP5 memory function significantly higher than patients for helping patients remember how much insulin was last injected; helping to prevent double-dosing; helping patients to remember their last injection time; and helping them adhere to therapy (all P < 0.05, Table 4). Overall, participants indicated that the memory function was most important in terms of helping patients remember how much insulin was last injected and preventing double-dosing.
Table 4.
Participant responses to questions on the importance of a memory function
| All participants (n = 450) | HCP (n = 150) | PwD (n = 300) | P value HCP versus PwD | |
|---|---|---|---|---|
| Helps patients adhere to therapy | 4.5 | 4.7 | 4.4 | <0.05 |
| Helps prevent double-dosing | 5.0 | 5.3 | 4.8 | <0.05 |
| Helps patients remember how much insulin was last injected | 5.1 | 5.5 | 4.9 | <0.05 |
| Helps patients remember their last injection time | 4.8 | 5.0 | 4.7 | <0.05 |
Note: Mean scores on a 1–6 scale where 1 = not at all important and 6 = extremely important.
Abbreviations: PwD, patients with diabetes; HCP, health care professionals.
Design of pen
Participants rated the length of NP5 closer to ideal (mean score 3.2; where 1 = far too short; 3 = just right and 5 = far too long) compared with HPL (mean score 3.5, P < 0.001). Participants rated the width of NP5 as more appropriate compared with HPL (mean score NP5 3.1 versus HPL 3.8, P < 0.001). Participants rated NP5 significantly higher than HPL for grip (where 1 = do not like it and 6 = like it a lot, mean score NP5 5.0 versus 4.6 HPL, P < 0.01); and shape (mean score NP5 5.0 versus 4.4 HPL; P < 0.001). There was no difference between the pens in ratings of robustness (mean score NP5 5.2 versus 5.1 HPL; P = 0.23).
Discussion
In this study, 81% of participants preferred NP5 to HPL, and the presence of a memory function was the most frequent reason for preferring NP5. Significantly more participants in the study were confident about using NP5 for everyday clinical management of their insulin injections compared with HPL. Participants gave higher ratings to NP5 than HPL on all parameters relating to design and performing an injection.
This study builds on the data from a previous study which showed that NP5 was preferred by most patients with diabetes and health care professionals compared with other durable commercially available pens.23 Compared with HumaPen Memoir, a durable insulin pen with memory function, NP5, was rated as “very easy” to learn how to use by most patients with diabetes and significantly more health care professionals rated NP5 as “very easy” to teach others to use, which are two factors that may have contributed to the preference for NP5.23
NP5 was designed to assist patients with self-management of their diabetes by building confidence and providing reassurance that they have not missed an injection, and by reducing the likelihood of double-dosing.23
A recent study has shown that a number of different insulin regimens are effective in enabling blood glucose levels to reach target values.26,27 Some regimens may require multiple insulin injections each day, and in some instances may require adjustments to the amount of insulin that needs to be injected to maintain optimized glycemic control. Memory function should be beneficial to all groups of patients with diabetes, regardless of what insulin regimen they are prescribed, but may be particularly welcomed by patients who require regular adjustments of their insulin regimen. A memory function which records how much time has elapsed since the last insulin dose and how much insulin was injected at the last dose should reassure patients with diabetes.
The risk for people who are unsure how much insulin, or when, they last injected is that they will double-dose, which may lead to hypoglycemia. Among patients, hypoglycemia is feared more than the long-term complications of diabetes,28 and this fear may result in suboptimal treatment in order to avoid hypoglycemia.29 Consequently, being able to verify the time of the last insulin injection and read the amount of the last dose of insulin with NP5 may be beneficial for patients who have difficulty remembering how much insulin they have taken. A memory function may also be beneficial for caregivers of elderly patients with diabetes, given that this will allow them to track insulin injections administered by another caregiver more easily and potentially prevent dose omissions or double-dosing.
The biggest limitation of this study was that its results were based on a single personal interview rather than actual use by patients and interaction between health care professionals and patients. If they had more time, eg, 2–3 weeks, to familiarize themselves with the pen and use of the memory function, patients may have answered the questionnaire differently. Also, 35% of the patients were familiar with NP4 which was slightly higher than the 33% limit stated in the protocol, compared with 26% who were familiar with HPL, and this may have slightly influenced responses to the questionnaire. The study compared a durable pen with a memory function (NP5) with a durable pen without a memory function (HPL), so was not a like-for-like comparison. However, HPL was chosen as the comparator pen in this study because it was widely used in the participating countries. The inclusion of insulin pen-naïve patients in the study may have also yielded different responses to some of the items in the questionnaire because NP5 may have been perceived as being more complicated than HPL.
Conclusion
In summary, NP5 was preferred to HPL by 81% of participants. Significantly more participants in the study were confident about using NP5 for everyday clinical management of their insulin injections and preferred the design of NP5 to that of HPL. The memory function may be a factor contributing to higher ratings for NP5 than for HPL. The results of this study indicate that an insulin pen with a memory function could be of real benefit in everyday clinical practice.
Footnotes
Disclosure
The study was sponsored by Novo Nordisk A/S, and carried out by Aequus Research, London, UK. IH has received research funding from Novo Nordisk A/S. GK, IH, and XG are consultants for Novo Nordisk A/S. KHM and MQ are employees of Novo Nordisk A/S. Editorial assistance was provided by John Clarke, ESP Bioscience, Crowthorne, UK, and funded by Novo Nordisk A/S, Denmark.
References
- 1.Zhang P, Zhang X, Brown J, et al. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(3):293–301. doi: 10.1016/j.diabres.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 2.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311–321. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 3.Morrow AS, Haidet P, Skinner J, Naik AD. Integrating diabetes self-management with the health goals of older adults: a qualitative exploration. Patient Educ Couns. 2008;72(3):418–423. doi: 10.1016/j.pec.2008.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lernmark A. Type 1 diabetes. Clin Chem. 1999;45(8 Pt 2):1331–1338. [PubMed] [Google Scholar]
- 5.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837–853. [No authors listed] [PubMed] [Google Scholar]
- 6.Wright A, Burden AC, Paisey RB, Cull CA, Holman RR. Sulfonylurea inadequacy: efficacy of addition of insulin over 6 years in patients with type 2 diabetes in the UK Prospective Diabetes Study (UKPDS 57) Diabetes Care. 2002;25(2):330–336. doi: 10.2337/diacare.25.2.330. [DOI] [PubMed] [Google Scholar]
- 7.Charbonnel B, Penfornis A, Varroud-Vial M, Kusnik-Joinville O, Detournay B. Insulin therapy for diabetes mellitus: treatment regimens and associated costs. Diabetes Metab. 2012;38(2):156–163. doi: 10.1016/j.diabet.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Brunton S. Insulin delivery systems: reducing barriers to insulin therapy and advancing diabetes mellitus treatment. Am J Med. 2008;121(Suppl 6):S35–S41. doi: 10.1016/j.amjmed.2008.03.025. [DOI] [PubMed] [Google Scholar]
- 9.Donnelly LA, Morris AD, Evans JM. Adherence to insulin and its association with glycaemic control in patients with type 2 diabetes. QJM. 2007;100(6):345–350. doi: 10.1093/qjmed/hcm031. [DOI] [PubMed] [Google Scholar]
- 10.Morris AD, Boyle DI, McMahon AD, Greene SA, MacDonald TM, Newton RW. Adherence to insulin treatment, glycaemic control, and ketoacidosis in insulin-dependent diabetes mellitus. The DARTS/MEMO Collaboration. Diabetes Audit and Research in Tayside Scotland. Medicines Monitoring Unit. Lancet. 1997;350(9090):1505–1510. doi: 10.1016/s0140-6736(97)06234-x. [DOI] [PubMed] [Google Scholar]
- 11.Peyrot M, Rubin RR, Kruger DF, Travis LB. Correlates of insulin injection omission. Diabetes Care. 2010;33(2):240–245. doi: 10.2337/dc09-1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Randlov J, Poulsen JU. How much do forgotten insulin injections matter to hemoglobin A1c in people with diabetes? A simulation study. J Diabetes Sci Technol. 2008;2(2):229–235. doi: 10.1177/193229680800200209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ross SA, Tildesley HD, Ashkenas J. Barriers to effective insulin treatment: the persistence of poor glycemic control in type 2 diabetes. Curr Med Res Opin. 2011;27( Suppl 3):13–20. doi: 10.1185/03007995.2011.621416. [DOI] [PubMed] [Google Scholar]
- 14.Korytkowski M, Bell D, Jacobsen C, Suwannasari R. A multicenter, randomized, open-label, comparative, two-period crossover trial of preference, efficacy, and safety profiles of a prefilled, disposable pen and conventional vial/syringe for insulin injection in patients with type 1 or 2 diabetes mellitus. Clin Ther. 2003;25(11):2836–2848. doi: 10.1016/s0149-2918(03)80337-5. [DOI] [PubMed] [Google Scholar]
- 15.Lombardo F, Salzano G, Messina MF, De Luca F. Compliance and administration methods in management of type 1 diabetes. Acta Biomed. 2005;76( Suppl 3):66–69. [PubMed] [Google Scholar]
- 16.Olsen BS, Lilleore SK, Korsholm CN, Kracht T. Novopen Echo for the delivery of insulin: a comparison of usability, functionality and preference among pediatric subjects, their parents and health care professionals. J Diabetes Sci Technol. 2010;4(6):1468–1475. doi: 10.1177/193229681000400622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sommavilla B, Jorgensen C, Jensen KH. Safety, simplicity and convenience of a modified prefilled insulin pen. Expert Opin Pharmacother. 2008;9(13):2223–2232. doi: 10.1517/14656566.9.13.2223. [DOI] [PubMed] [Google Scholar]
- 18.Summers KH, Szeinbach SL, Lenox SM. Preference for insulin delivery systems among current insulin users and nonusers. Clin Ther. 2004;26(9):1498–1505. doi: 10.1016/j.clinthera.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 19.Asche CV, Shane-McWhorter L, Raparla S. Health economics and compliance of vials/syringes versus pen devices: a review of the evidence. Diabetes Technol Ther. 2010;12( Suppl 1):S101–S108. doi: 10.1089/dia.2009.0180. [DOI] [PubMed] [Google Scholar]
- 20.Baser O, Bouchard J, DeLuzio T, Henk H, Aagren M. Assessment of adherence and healthcare costs of insulin device (FlexPen) versus conventional vial/syringe. Adv Ther. 2010;27(2):94–104. doi: 10.1007/s12325-010-0009-6. [DOI] [PubMed] [Google Scholar]
- 21.Lee WC, Balu S, Cobden D, Joshi AV, Pashos CL. Medication adherence and the associated health-economic impact among patients with type 2 diabetes mellitus converting to insulin pen therapy: an analysis of third-party managed care claims data. Clin Ther. 2006;28(10):1712–1725. doi: 10.1016/j.clinthera.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 22.Peyrot M, Barnett AH, Meneghini LF, Schumm-Draeger PM. Insulin adherence behaviours and barriers in the multinational Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabet Med. 2012;29(5):682–689. doi: 10.1111/j.1464-5491.2012.03605.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guo X, Sommavilla B, Vanterpool G, Qvist M, Bethien M, Lilleore SK. Evaluation of a new durable insulin pen with memory function among people with diabetes and healthcare professionals. Expert Opin Drug Deliv. 2012;9(4):355–356. doi: 10.1517/17425247.2012.671808. [DOI] [PubMed] [Google Scholar]
- 24.World Medical Association. Declaration of Helsinki – ethical principles for medical research involving human subjects. [Accessed November 8, 2011]. Available from: http://www.riip-influenza.org/wp-content/uploads/2011/08/Helsinki-2008-EN.pdf.
- 25.Buus P, Lilleore SK, Larsen K. Compatibility testing of two types of pen needles with a range of injection pens for diabetes medication. Curr Med Res Opin. 2011;27(3):589–592. doi: 10.1185/03007995.2010.547574. [DOI] [PubMed] [Google Scholar]
- 26.Holman RR, Farmer AJ, Davies MJ, et al. Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361(18):1736–1747. doi: 10.1056/NEJMoa0905479. [DOI] [PubMed] [Google Scholar]
- 27.Holman RR, Thorne KI, Farmer AJ, et al. Addition of biphasic, prandial, or basal insulin to oral therapy in type 2 diabetes. N Engl J Med. 2007;357(17):1716–1730. doi: 10.1056/NEJMoa075392. [DOI] [PubMed] [Google Scholar]
- 28.Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care. 2005;28(5):1245–1249. doi: 10.2337/diacare.28.5.1245. [No authors listed] [DOI] [PubMed] [Google Scholar]
- 29.Fidler C, Elmelund Christensen T, Gillard S. Hypoglycemia: an overview of fear of hypoglycemia, quality-of-life, and impact on costs. J Med Econ. 2011;14(5):646–655. doi: 10.3111/13696998.2011.610852. [DOI] [PubMed] [Google Scholar]