Abstract
Background
A review of the literature was conducted to examine substance use screening instruments commonly used with adolescents in medical settings, their comparative usefulness, and SBIRT (Screening, Brief Intervention, and Referral to Treatment).
Methods
We screened two databases (Ovid MEDLINE and PsycINFO) targeting journal articles dealing with screening for alcohol and drug use in adolescence as well as adolescent SBIRT.
Results
Adolescents preferred paper forms and computerized questionnaires over interviews with physicians or nurses. The CRAFFT was the best studied instrument for screening for alcohol/drug use and related problems, and is the only tool with data to support its use in medical settings. Other screening instruments require more testing/evaluation in more representative samples of adolescents in primary care settings. Long term follow-up data to establish the efficacy of SBIRT in adolescence are not available. Innovative computerized approaches to screening for substance use in this population have recently been proposed. Although promising, they require further evaluation.
Conclusions
The CRAFFT has the most consistent data to support its use in primary care settings. The effects of SBIRT in adolescence have not been adequately evaluated. Adolescents’ opinions and preferences for SBIRT should be studied to improve their acceptance.
Keywords: adolescents, screening, alcohol screening, drug screening, SBIRT, brief interventions, substance use, substance abuse
1. INTRODUCTION
The use and misuse of alcohol and illicit drugs is highly prevalent in adolescence (Fournier & Levy, 2006) in the US and elsewhere. An estimated 37.0% of American adolescents aged 12–17 years used alcohol or drugs in the past year, and 7.9% met criteria for a substance-related disorder (Wu, Woody, Yang, Pan, & Blazer, 2011). In a survey of adolescents (high school students) in six European countries the prevalence range for any lifetime use of illegal drugs (predominantly cannabis) was 10.2% (Romania) to 40.8% (United Kingdom) among boys, and 9.1% (Romania) to 34.2% (United Kingdom) among girls. The prevalence range for using alcohol 10 or more times in the last 30 days ranged from 5.4% (Bulgaria) to 18.9% (Greece) among boys, and from 4.2% (Slovenia) to 10.1% (Greece) among girls (Kokkevi, Richardson, Florescu, Kuzman, & Stergar, 2007). Among Australian adolescents/young adults (aged 16–24), 15.6% and 8.3% met criteria for DSM-IV lifetime and 12-month alcohol abuse, respectively (Teesson, et al., 2010). Among the nonmedical or illicit drugs used by adolescents, marijuana and analgesic opioids are the primary drugs of abuse (Wu, Woody, Yang, Pan, & Blazer, 2011). Early substance use is associated with an increased risk of substance dependence, psychiatric and medical disorders, and mortality (Aarons, et al., 1999; DuRant, Smith, Kreiter, & Krowchuk, 1999; Swahn, Bossarte, Ashby, & Meyers, 2010; Swahn, Bossarte, & Sullivent, 2008; Wu, et al., 2011). In view of the risks associated with early initiation of substance use and its high prevalence in adolescence, screening for substance use is important in this population.
While screening for substance use among adults has been extensively studied, and the US Preventive Services Task Force (USPSTF) has issued recommendations for screening and behavioral counseling for alcohol use problems among adults in primary care (USPSTF, 2004), screening in adolescence has received less attention from investigators and clinicians. The recent approval in the US of the Patient Protection and Affordable Care Act (PPACA) of 2010 supports the integration of substance abuse interventions and treatments into the mainstream health care system. Thus, there is hope that its implementation will bring about funding for screening and brief interventions (Pilowsky & Wu, 2012). The objectives of this paper are to (1) describe the most common screens to detect risky substance use in adolescents in primary care; (2) review Screening, Brief Intervention and Referral to Treatment (SBIRT); and (3) review biological substance use screens and ethical considerations regarding their use in youth. This review emphasizes recent findings in each of these domains, and includes screening for illicit drug use rather than limiting it to alcohol as recent reviews did (Clark, Gordon, Ettaro, Owens, & Moss, 2010; Clark & Moss, 2010). A few older reviews included screening for drug use and are useful resources on adolescent screening (KC Winters, 1999; K Winters & Zenilman, 1994).
Screening refers to tools used to find individuals who have or at high risk for a disorder or a maladaptive behavior in a population of interest, such as adolescents. Screening does not establish a diagnosis. Establishing a diagnosis is the following step in many but not all cases. For example, screening for tobacco use may not be followed by determining a diagnosis of tobacco dependence because adolescents screening positive for tobacco use should be referred to a smoking cessation program regardless of whether or not they are tobacco-dependent; and most adolescent smokers want to quit but find it hard to maintain tobacco abstinence (Burt & Peterson, 1998). On the other hand, in the case of diabetes screening, a diagnosis should follow because treatment should be provided only to those with the disease. As a general principle screening instruments should be brief and as non-intrusive as possible because the majority of adolescents screened in primary care settings will not be positive. Adolescents who screen positive should be given more detailed assessments for diagnosis and treatment planning.
Screening may consist of questionnaires, or, less commonly, biomarkers. We have recently reviewed the conceptual framework underlying screening in adults (Pilowsky & Wu, 2012). Briefly, a good screening instrument has high sensitivity (i.e. identifies most cases with a disorder) and high specificity (i.e. avoids positive screens of individuals without the disorder). Cutoff scores for screening tests are designed to maximize sensitivity and specificity in order to minimize false positives and false negatives (Stewart & Connors, 2004). Additionally, screening instruments and interventions for use with adolescents and related interventions need to be developmentally appropriate, feasible in the clinical context and acceptable to patients.
A positive screening should be followed by an intervention that prevents progression to disease or by a treatment for a disease if a diagnostic instrument confirms it. Thus, the traditional approach has been to screen and refer for treatment. However, individuals with Substance Use Disorders (SUDs) referred to treatment often do not follow-up (Bernstein, Bernstein, & Levenson, 1997), and referrals are not always made. A study of follow-up recommendations for adolescent patients screened for risky substance use in seven primary care practices showed that one in five patients engaging in risky use did not receive a recommendation for an active intervention. In the same study, primary care providers recommended a return visit to their office more than twice as often as referral to counseling, and providers were more likely to recommend active intervention for patients whom they believe had a high severity of substance use problems (Hassan, et al., 2009).
The need for implementing SBIRT an approach appropriate to all stages of the substance use, abuse, and dependence spectrum has been increasingly recognized and emphasized (Committee-on-Substance-Abuse, 2011). For early stages of substance use, a brief intervention by a primary care physician or nurse may suffice. For individuals who have progressed to a disorder, a brief intervention may help them acknowledge the problem and motivate them to comply with a treatment referral. To facilitate acknowledgement of the problem, most SBIRT protocols use Motivational Interviewing (MI) techniques, as described below. In the following section, we describe the methods used to select studies for inclusion in this review.
2. METHODS
2.1 Selection of Studies
Relevant studies were identified by searching the Medline and PsychInfo databases. The first step in the Medline search was to search the terms “alcohol screening” and “drug screening” and combine them with the operator “or” (Fig. 1). The second step was to search for the term “adolescence.” The third step consisted of combining the two previous searches with the operator “and.” This step yielded 6 references. The fourth step was to search for the term “SBIRT” and combine the result with the 6 references using the operator “or.” Last, we restricted the results to “English Language” and “Journal Article.”
Figure 1.
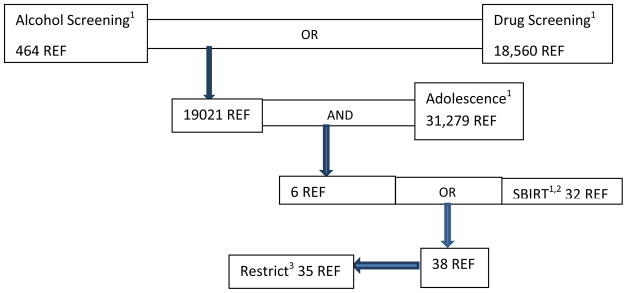
Schematic Representation of Medline Search
REF=References
1Searched as Keyword
2Screening, Brief Intervention, and Referral to Treatment
3Restrict to “English Language” and “Journal Article”
2.2 Inclusion criteria
Because the above steps yielded only 35 journal articles in Medline (Fig. 1) and not all were relevant, we used the “Find Similar” feature of Medline and references from the identified publications. This strategy yielded over 100 publications. We then reviewed and removed irrelevant publications, i.e. those whose main focus was not screening for alcohol/ drug use and/or SBIRT in adolescence. With a few exceptions, the PsychInfo database yielded the same references using a similar strategy.
Investigators often use terms such as “misuse” or “risky use” or “problematic use” to refer to substance use that puts users at risk for negative consequences but does not necessarily meet criteria for a DSM-IV or ICD-9 SUD. Here, we use the term “risky use”, and provide references so that the reader can access the definition provided by each investigator. Given that there are no widely accepted criteria for “risky use,” investigators provide study-specific definitions. Last, we present the verbatim text of brief and widely used instruments so that readers can become aware of the specific queries without searching the literature.
3 Results
3.1 Screening for alcohol/drug use in adolescence
Although the screening instruments and interventions described below may be used in a variety of settings, the focus of this paper is on their use in primary care. Before describing the various screening instruments available for use with adolescents, it is important to consider how they are administered (i.e., interviews, paper forms, or computerized questionnaires). There is evidence that adolescents prefer paper forms and computerized questionnaires over interviews with physicians or nurses (Knight, et al., 2007a). Furthermore, adolescents report being “very likely” to be truthful when answering substance use related questions using paper forms or computers (Knight, et al., 2007a). The reason for this preference is not entirely clear, but not having to face a questioning adult may free teenagers to report socially unacceptable behaviors. The screening instruments described below can be used in any of these formats but to the best of our knowledge they have been used predominantly as forms or interviews. We anticipate that computerized use will increase over time. When administered as interviews, screeners are usually administered without the parents in the room. There is evidence that adolescents are often not truthful when answering questions about substance use in the presence of their parents (Friedman, Johnson, & Brett, 1990). Another preliminary consideration is that multiple characteristics such as appropriateness, reliability, validity, responsiveness, precision, interpretability, acceptability, and feasibility (Fitzpatrick, Davey, Buxton, & Jones) of instruments used for screening should be considered in the relevant publications. Unfortunately, most focus solely on reliability and validity. However, when available in the publication we report on other characteristics.
3.2 Screening Instruments for Use with Adolescents
3.2.1 CRAFFT
The most thoroughly studied instrument to detect substance use and related problems in adolescence is the CRAFFT (Stewart & Connors, 2004). Each letter in this acronym stands for one of the six questions included in the screener:
”Have you ever ridden in a Car driven by someone (including yourself) who was high or had been using alcohol or drugs?”
“Do you ever use alcohol or drugs to Relax, feel better about yourself, or fit in?”
Do you ever use alcohol or drugs when you are by yourself, Alone?”
“Do you ever Forget things you did while using alcohol or drugs?”
“Do your family or Friends ever tell you that you should cut down on your drinking or drug use?”
“Have you ever gotten into Trouble while you were using alcohol or drugs?”
The CRAFFT is easy to administer and score (each “yes” answer =1). When administering the CRAFFT, questions on lifetime or past year use of alcohol or drugs are usually asked prior to CRAFFT items. A CRAFFT score of 2 or higher is considered optimal for identifying risky use (sensitivity 0.76; specificity 0.94), any SUD (0.80; 0.86; See Table 1) and dependence (0.92; 0.80) (Knight, Sherritt, Shrier, Harris, & Chang, 2002). A pilot study (Knight, et al., 1999) and a larger study in an adolescent clinic (Knight, et al., 2002) have demonstrated the criterion validity and internal consistency of the CRAFFT. Five hundred and thirty eight adolescents participated in the larger study. About half had not used any substances; nearly a quarter and a tenth reported occasional and risky use, respectively. The remaining adolescents met criteria for at least one SUD (Knight, et al., 2002). A score of two or higher indicates a need for further evaluation.
Table 1.
Characteristics of screening instrument used to detect alcohol/drug use and related disorders in adolescence1
| Instrument | Cutoff | Sensitivity | Specificity | PPV | NPV | Alpha2 | Number of Items | Reference3 |
|---|---|---|---|---|---|---|---|---|
| CRAFFT | ≥2 | 0.80 | 0.86 | 0.53 | 0.96 | 0.68 | 6 | (Knight et al., 2002) |
| RAFFT | ≥2 | 0.89 | 0.69 | 0.73 | 0.87 | N/A | 5 | (Bastiaens et al., 2000) |
| CAGE4 | ≥1 | 0.67 | 0.82 | 0.59 | 0.86 | 0.74 | 4 | (Chung et al., 2000; Knight et al., 2000) |
| TWEAK5 | ≥2 | 0.73 | 0.90 | 0.74 | 0.89 | N/A | 6 | (Chung et al., 2000) |
| AUDIT6 | ≥4 | 0.94 | 0.80 | 0.64 | 0.97 | N/A | 10 | (Chung et al., 2000) |
Abbreviations: SUD Substance use disorder; PPV Positive predictive value; NPV Negative predictive value
Only screeners with adolescent sensitivity/specificity and PPV/NPV data were included in this table.
Measures internal consistency of questionnaires/assessments
References provided in this table correspond to the publication providing the data shown in the table (i.e. not to the original description of each instrument).
Modified version of the adult CAGE. The cutoff score for the adult version is ≥2.
Modified version of the adult TWEAK. Similar data in an adult sample is found in Chan et al. (Chan et al., 1993)
Modified version of the adult AUDIT. The cutoff score for the adult version is ≥8.
Using the CRAFFT, Knight and colleagues estimated the prevalence of positive substance abuse screen results among adolescent patients aged 12–18 years in primary care. About 1 in 7 adolescents (14.8%) screened positive with higher prevalences in school-based health centers (29.5%) and a rural family practice (24.2%), and lower rates in adolescent and pediatric clinics and a health maintenance organization. Their results underline the impact of various settings on prevalence estimates of positive screens. Overall, 11.3% of patients engaged in problematic use; and 3.2% and 7.1% met criteria for abuse and dependence, respectively (Knight, et al., 2007b).
3.2.2 RAFFT
Another instrument used to screen for substance use and risky use in adolescence is the RAFFT (L. Bastiaens, Francis, & Lewis, 2000; Leo Bastiaens, Riccardi, & Sakhrani, 2002). Each letter in the acronym refers to a question asked as part of the screening. It was studied with a sample of patients aged 13–18 (N=226) who were referred for emergency department or ambulatory psychiatric assessments. The RAFFT questions are:
Do you drink/drug to relax, feel better about yourself, or fit in?
Do you ever drink/drug while you are by yourself, alone?
Do any of your closest friends drink/drug?
Does a close family member have a problem with alcohol/drugs?
Have you ever gotten into trouble for drinking/drugging?
As shown in Table 1, the RAFFT with two or more positive answers had a sensitivity of 0.89 and a specificity of 0.69 in the initial study (L. Bastiaens, et al., 2000). However, these estimates were based on a sample of teenagers referred for a psychiatric assessment in a hospital known for its addiction services. Thus, its sensitivity and specificity estimates may not be applicable to the general adolescent population or adolescents seen in primary care settings (Leo Bastiaens, et al., 2002). Further research of this instrument in these settings would be useful to inform the utility of the RAFFT for adolescents. By comparison, the CRAFTT was studied in adolescent primary care practices, where screening is most likely to take place. The CRAFFT is used more often than the RAFFT, and is arguably the most widely used screening instrument for adolescent substance use in the U.S.
3.2.3 Other Screening Tools
In this section. we discuss instruments that have not been studied in depth with adolescents but show varying degrees of potential for use with this population, often with some modifications determined by patterns of substance use among adolescents.
3.2.3.1 AUDIT
The AUDIT is a screening tool for detecting alcohol-related problems in primary care settings. Although it was designed for use with adults, it has also been used with adolescents. The AUDIT consists of 10 questions that address the extent of alcohol use, its negative consequences, and evidence that others have observed behaviors, which suggest a drinking problem (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993). The sensitivity/specificity values of the modified AUDIT for use with adolescents are shown in Table 1 (Chung, et al., 2000).
3.2.3.2 CAGE
The CAGE is an alcohol-focused screener widely used with adults. It consists of four questions that aim at detecting excessive alcohol use (Ewing, 1984; USPSTF, 2004). The adult version is seldom used with adolescents. Although the adolescent version has good test-retest reliability, the internal consistency of this version is low (α=0.60) (Knight, Goodman, Pulerwitz, & DuRant, 2000). The sensitivity/specificity values of the adolescent version are shown in Table 1 (Chung, et al., 2000).
3.2.3.3 TWEAK
The TWEAK is a short screener for alcohol-related problems, e.g. it ascertains whether family members worry about the respondent’s drinking, and inquires about a perceived need to “cut down.” Although this 6-item screener was designed to assess drinking during pregnancy (Chan, Pristach, Welte, & Russell, 1993; Russell, et al., 1994; Russell, et al., 1996), it has been used with other populations, including adolescents. The sensitivity/specificity of the adolescent version are shown in Table 1 (Chung, et al., 2000).
3.2.3.4 SSI-AOD
The SSI-AOD is a 16 item screening instrument for alcohol or drug abuse designed for use by a variety of adolescent service providers (Winters and Zenilman, 1994). Although it has good internal validity (α=0.74) and good test-retest reliability (r [correlation coefficient]=0.90) (Knight et al., 2000), it has not been widely used or studied with adolescent populations.
3.2.3.5 DAP-4
The DAP QuickScreen consists of 30 questions about alcohol and drug use (Klitzner et al., 1987). Because the 4 of the 30 questions account for most of the variance between high and low risk substance users, these four questions were used to propose a short screener known as DAP-4 (Knight et al., 2000; Schwartz and Wirtz, 1990). The DAP-4 was found to have a low internal consistency coefficient (alpha = 0.46) in an adolescent sample (Knight, et al., 2000). The four questions are: (1) “Do you use tobacco products (cigarettes, snuff, etc.)?”; (2) “Have you ever had an in-school or out-of-school suspension for any reason?”; (3) “Do you sometimes ride in a car driven by someone, including yourself, who is high or who appears to have had too much to drink?” and (4) “Has anyone (friend, parent, teacher or counselor) ever told you that they believe that you may have a drinking or drug problem?”.
3.2.3.6
The Drug Alcohol Brief Intervention Team (DABIT), in use in Australia, although not specifically designed for adolescents can be used with young drinkers (Daglish, 2011). No published data are available on sensitivity or specificity.
3.2.3.7 Personality based interventions
Recent attempts to intervene with adolescents and young adults targeting personality traits are noteworthy but beyond the scope of this review (Conrod, Castellanos-Ryan, & Mackie, 2011; Woicik, Stewart, Pihl, & Conrod, 2009).
3.2.4 Comparison of Screening Tools in Adolescent Samples
The main characteristics of frequently used instruments in adolescents are summarized in Table 1. An examination of the data shown in Table 1 suggests that the sensitivity and specificity of CRAFFT and AUDIT equals or exceeds 0.80. However, the AUDIT targets only alcohol use and related problems. In contrast, the CRAFFT includes both alcohol and drugs. A comparison of the number of items included in each instrument reveals that the AUDIT is the longest instrument with a total of 10 items (compared to 4–6 items for the remaining instruments listed in Table 1).
A few studies have compared adolescent-focused screening instruments. Chung et al. tested in an adolescent sample modified versions of three adult alcohol screeners (Chung et al., 2000), i.e. the CAGE (Ewing, 1984), TWEAK (Chan et al., 1993) and the AUDIT (Bradley et al., 2007). Their sample consisted of injured adolescents seen in an emergency department (N=415 adolescents aged 13–19 years). The AUDIT demonstrated the best performance, with optimal performance at a cutoff score of 4. Because the sample consisted of adolescents with injuries, the generalizability of these findings to general adolescent practices requires further research.
Knight and colleagues tested with an adolescent sample (N=173) the internal consistency and test-retest reliability of the Simple Screening for Alcohol and Drug Abuse (SSI-AOD), the CAGE-AA (CAGE questions adapted for adolescents), and the DAP-4. While only the SSI-AOD had a high internal consistency (alpha = 0.83), all three instruments showed a high test retest reliability (range r = 0.82–0.90). The investigators concluded that the SSI-AOD is a reliable substance abuse screening instrument (Knight, et al., 2000).
The sensitivity/specificity of the CRAFFT in identifying any SUD (0.80/0.86, respectively) reported by Knight et al. (Knight, et al., 2002) compare somewhat favorably with the RAFFT (sensitivity/specificity: 0.89/0.69, respectively) (L. Bastiaens, et al., 2000), a substantively dissimilar instrument.
In summary, the CRAFFT is the most widely used instrument to screen for substance use and related problems in adolescents in the U.S. Furthermore, it is the only tool with consistent data to support its use in primary care settings. Other screening instruments require additional evaluation in more representative samples of adolescents in these settings. The limited evidence suggests that adolescents prefer screening administered via paper forms or computerized questionnaires over face-to-face interviews with health professionals.
3.3 Intervention and Referral to Treatment According to Risk Level
SBIRT includes three components delivered sequentially, i.e. screening, brief intervention, and referral for treatment. The number of components delivered is related to the level of risk. Usually brief interventions follow the use of one of the screening instruments discussed above. The use of biological screeners is not a routine component of SBIRT because of ethical concerns and limitations discussed in a separate section of this review.
The American Academy of Pediatrics (AAP) has proposed different avenues for intervening with substance using adolescents according to the level of risk (low, moderate, high), as estimated using the CRAFFT (Committee-on-Substance-Abuse, 2011). Here, we discuss brief interventions by risk categories because this approach is clinically useful.
3.3.1 Low Risk
Adolescents who report not using any substances (including tobacco), and deny riding a car with a peer who was driving under the influence of substances, should receive praise and encouragement. All adolescents who report driving under the influence of substances or riding with a driver who has used alcohol or drugs should be asked to make a safety plan, such as the plan promoted by Students Against Destructive Decisions (http://www.sadd.org/contract.htm). These plans often include a commitment not to drive under the influence of alcohol/drugs or with an impaired driver, and to seek help from a parent or a responsible adult if the adolescent is in a situation that endangers her/his safety. For example, in a situation where an adolescent needs a ride to avoid driving while intoxicated or riding with a drunk driver, she/he may seek help in arranging alternative transportation. The AAP policy statement suggests that pediatricians may break confidentiality when an adolescent responds affirmatively to the CRAFFT car question and will not commit to avoiding such situations.
3.3.2 Moderate Risk
Adolescents who report using alcohol or drugs and scoring 0–1 on the CRAFFT are considered at moderate risk for problems related to substance use (Committee-on-Substance-Abuse, 2011). A brief intervention with these adolescents would include a clear recommendation to stop alcohol and other drug use, and counseling about the health consequences of drug use. This psychoeducational approach is often coupled with the recognition of strengths and personal attributes, e.g. “you are such a great athlete, and you would not want to undermine your chances to play college basketball”.
3.3.4 High Risk
Adolescents screening positive on the CRAFFT (score ≥2) are considered at heightened risk for substance use disorders. These adolescents require further evaluation to assess for signs of addiction and related high risk behaviors. A CRAFFT score ≥2, daily or nearly daily use of substances, and/or alcohol-related blackouts, are considered signs of possible dependence leading to a referral for further evaluation and treatment (Committee-on-Substance-Abuse, 2011). To enhance the probability of compliance with a referral for substance abuse treatment, the following are recommended: (a) parental involvement, preferably but not necessarily with the consent of the adolescent; and (b) using motivational interviewing (MI) techniques to increase the adolescent’s own motivation for change. For example, a nurse or physician might say “I see that you enjoy having a marijuana joint, and often more than one, yet you also told me that your grades are going down and that you are upset about it.” As illustrated in this example, MI focuses on the ambivalence and the mixed consequences underlying a maladaptive behavior in order to increase motivation for change (Miller & Rollnick, 2002).
On the other end of the risk spectrum, adolescents with a CRAFFT score ≥2 who do not show signs of possible dependence and present with relatively minor consequences resulting from their substance use may be engaged in a Brief Negotiated Interview (BNI). BNI is based on MI principles and aims at encouraging abstinence or risk reduction (Committee-on-Substance-Abuse, 2011). Briefly, BNI includes summarizing the assessment, listing problems associated with substance use reported by the adolescent, and asking the adolescent whether they are interested in changing their approach to substances. For example, one might say “you enjoy partying and drinking with your friends but you also told me that it bothers you to see that your parents are so upset about your drinking. What would you like to do about it?” The principle involved is that simply asking adolescents to discontinue the use of substances may elicit resistance or a defensive attitude. Instead, asking about their plans is less likely to elicit a negative reaction and might lead to adolescent-initiated plans for change that can be praised or reinforced.
Others have suggested that recommendations should depend on the age and developmental stage of the adolescent (Clark & Moss, 2010). In this view, when dealing with younger adolescents (aged 12–14 years), abstinence should be the SBIRT goal. In mid-adolescence (aged 15–17 years) the focus should be on screening for binge drinking because it would identify most adolescents with an alcohol use disorder, as well as those that can be targeted for preventive services. Last, in late adolescence the focus should be solely on alcohol use disorders (Clark & Moss, 2010).
3.4 Stepped Care
Stepped care approaches consist of using brief interventions for a wide variety of mental health and addiction problems, followed by more intensive interventions for those not benefiting from the initial brief intervention. Stepped care has been applied to adolescent substance use and it follows principles that are similar to those proposed by the American Pediatric Association (see 3.3). This approach has been used extensively in Australia and the United Kingdom. For example, Baker et al. used a brief intervention that included motivational interviewing and cognitive behavioral therapy to treat Australian amphetamine users with at least weekly use (Baker, et al., 2005). The main finding from their study was a significant increase in the proportion of those abstinent from amphetamines during the 6-maonth follow-up interval among those who received two or more treatment sessions. These investigators proposed the following steps with each consecutive step offered to those not responding to the prior steps: (1) structured assessment of amphetamine use; self-help materials; and monitoring of amphetamine use; (2) two sessions of motivational interviewing combined with CBT for treatment-seeking regular users; (3) a four-session intervention from the outset for those with moderate to severe co-occurring depression; and (4) pharmacotherapy and/or long term psychotherapy for those not responding to the above approaches (Baker, et al., 2005). Although this approach is described here in reference to amphetamines, it is applicable to other drugs that are misused or abused. For example, based on data from Canadian problem drinkers, Breslin et al. proposed using a stepped care approach to the treatment of problem drinkers (Breslin, Sobell, Sobell, Buchan, & Cunningham, 1997).
All the approaches described above have a common algorithm, i.e. start with brief simple interventions and offer more costly and longer interventions to those not responding to initial treatment, thus transitioning when necessary from SBIRT to long term addiction treatment.
3. 5 Brief Interventions: Summary and Future Directions
In summary, adolescents who use alcohol or drugs with no or minor consequences can be counseled by their own health care provider using MI techniques. Those at high risk for dependence, as reflected by a CRAFFT score ≥2, daily or nearly daily use of substances and/or alcohol-related blackouts should be referred for further evaluation and treatment. These referrals often require using MI techniques to motivate the adolescent and parental involvement to increase the likelihood of compliance with recommendations for evaluation and treatment.
The USPSTF report on adolescent SBIRT for illicit drug use concludes that the efficacy of SBIRT in adolescents has not been adequately evaluated, i.e. long term follow-up data are not available and the feasibility (e.g., costs and benefits) of routinely incorporating SBIRT into busy primary care practices is not known. More evidence is needed on the effectiveness and acceptance of SBIRT for substance use in adolescence (Polen, Whitlock, Wisdom, & al., 2008).
3.6 Biological Tests and Markers
3.6.1 Drug Screening
The use of urine samples to detect substances of abuse or their metabolites (urine drug screening) is common in substance abuse treatment settings. Although objective, urine drug screening has limitations. With few exceptions, it does not detect recent drug use (i.e. a few days before the test). Furthermore, as in most tests, there are false positives and false negatives, as well as technical problems, such as the appropriate handling of body fluids (Babor & Kadden, 2005). Unless handled appropriately, there is substantial risk for errors (Levy, Sherritt, Vaughan, Germak, & Knight, 2007). Research has shown that test results are often susceptible to positive or negative misinterpretation, e.g. 12% of urine drug screening in a drug treatment program were equivocal, and about a fifth of positive drug tests resulted from prescribed medications, most often stimulants (Levy, et al., 2007). Furthermore, adolescents can dilute their urine purposefully either in vitro or in vivo, thus distorting results. Last, routine panels used in drug screening do not detect inhalants and often fail to detect synthetic opioids such as oxycodone, a category of drugs increasingly used by adolescents (Wu, Pilowsky, & Patkar, 2008).
With very few exceptions, the AAP is opposed to urine drug screening of older competent adolescents without their consent, even when parents request a urine drug screen (American-Academy-of-Pediatrics, 1996). Not surprisingly, many more parents (81.7%) than teenagers (53.7%) in a sample drawn from suburban middle class pediatric practices believed that parents had the right to request a urine test for a problematic teenager without the teenager’s knowledge or consent (Schwartz, Silber, Heyman, Sheridan, & Estabrook, 2003). The ethical and practical issues relevant to screening adolescents for drug use are beyond the scope of this paper and have been discussed elsewhere (Schwartz, et al., 2003). Although the AAP is opposed to the use of urine drug screening with competent adolescents in general practice, it is not opposed to their use in substance abuse treatment settings. However, since this review focuses on its use as screening instruments, this topic is not reviewed in detail here. Interested readers are referred to relevant publications (Levy, et al., 2011; Levy, et al., 2007).
New approaches to SBIRT have used computerized brief interventions. In a study of adolescents with self-reported alcohol use and aggressive behavior, multiple outcomes improved significantly three months after a computerized screening followed by a brief computerized or therapist-led intervention. Brief intervention results were similar in both approaches, with improved alcohol-related attitudes and self-efficacy (Cunningham, et al., 2009). At 6 months, participants in the computerized or therapist-led interventions showed greater self-reported reductions in alcohol-related negative consequences compared with controls (Walton, et al., 2010).
3.6.2 The use of biomarkers
Although most biological tests detect substances of abuse or their metabolites in urine samples (urine drug testing), a few biomarkers are available for a screening purpose. Biomarkers are often used to detect alcohol use because ethanol is rapidly metabolized and, consequently, it is the least amenable to detection (Skipper, et al., 2004). Persistent and excessive alcohol use is often associated with abnormal liver enzyme levels. However, other conditions, e.g. being overweight, may alter the level of these enzymes. Thus, these enzymes lack specificity (Niemela and Alatalo, 2010). Carbohydrate-deficient transferrin (CDT) has recently been used as a biomarker for detection of heavy alcohol consumption, and promises to be more specific than previously studied biomarkers. It is elevated in heavy drinkers; when drinking is discontinued, CDT slowly normalizes and reaches baseline levels in 3–5 weeks (Bergstrom and Helander, 2008). Because adolescents often have less chronic and heavy drinking patterns than adults, CDT might be less sensitive in this population.
Ethyl glucuronide, an ethanol metabolite, remains present in the urine well after the disappearance of ethanol from the urine. Numerous reports suggest that it is a sensitive, specific, and reliable marker for recent (up to 5 days) alcohol intake (Dahl, Stephanson, Beck, & Helander, 2002; Goll, Schmitt, Ganssmann, & Aderjan, 2002; Skipper, et al., 2004). Given these characteristics, its use in alcohol treatment centers is expected to increase over time and to complement a variety of treatment modalities.
4. CONCLUSIONS AND CLINICAL IMPLICATIONS
Substance use and misuse are common among American adolescents. Several interview-based screening instruments (mainly alcohol screening) have been studied extensively in adults (Pilowsky & Wu, 2012), but there is relatively limited research in the adolescent population. Among available instruments for screening alcohol/drug use and related problems, the CRAFFT has been more thoroughly studied than other screeners used with adolescents, and is the most often used screener in adolescence (Knight, et al., 2000).
Positive CRAFFT screens generally lead to brief interventions when substance use is not associated with major psychosocial consequences or evidence of addiction. In cases where an adolescent has experienced negative psychosocial consequences or meets criteria for a SUD, there is general consensus that a detailed evaluation and referral to treatment are warranted. While the use of urine drug screening is common among adolescents in treatment for substance abuse, its use in primary care is limited by ethical considerations and concerns about their validity (false results and technical errors). AAP policy clearly states that urine testing for screening purposes without the knowledge of adolescents with capacity to consent, a capacity usually present in older adolescents, is not ethically permissible. Furthermore, parental consent is not sufficient in the case of competent adolescents (Committee-on-Substance-Abuse, 2011). Although there have been advances in the design of SBIRT interventions for adolescent populations, their effectiveness has not been adequately evaluated.
To improve screening of adolescents, it is necessary to deal with practical barriers, including limited provider time. Screening itself can be brief and easy to administer. However, dealing with positive screens is often time consuming and requires effective guidelines. Providers need training and resource support to deal with positive screens (Van Hook, et al., 2007). To make the SBIRT efforts truly useful to adolescents and acceptable to clinicians, research is needed to better understand facilitators for and barriers to SBIRT (Van Hook, et al., 2007). One direction is to elucidate the role of parental involvement on following clinicians’ recommended interventions for adolescents (e.g., return visits, referrals) and outcomes (Hassan, et al., 2009). Additional research should examine clinicians’ preferences for intervention options, e.g. to elucidate why providers often recommend return visits over other options, such as school-based drug counseling programs, outpatient substance abuse clinics, day treatment programs, or inpatient residential programs (Hassan, et al., 2009). Adolescents’ opinions and preferences for SBIRT also should be studied to improve their acceptance. Finally, longitudinal studies are needed to determine whether SBIRT in adolescents is associated with sustainable abstinence or harm reduction, and whether it decreases risk for subsequent substance dependence.
Acknowledgments
Role of funding source This review is made possible by research grants from the U.S. National Institute on Drug Abuse of the National Institutes of Health (R33DA027503, R01DA019623, R01DA019901, and R01DA026652). The National Institutes of Health had no role in the preparation, review, or approval of the manuscript. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Footnotes
Contributors Both authors participated in the bibliographic research and the manuscript preparation. Both authors have approved the final version of the manuscript
Conflict of Interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Daniel J Pilowsky, Email: dp14@columbia.edu.
Li-Tzy Wu, Email: litzy.wu@duke.edu.
References
- Aarons GA, Brown SA, Coe MT, Myers MG, Garland AF, Ezzet-Lofstram R, Hazen AL, Hough RL. Adolescent alcohol and drug abuse and health. Journal of Adolescent Health. 1999;24:412–421. doi: 10.1016/s1054-139x(99)00006-3. [DOI] [PubMed] [Google Scholar]
- American-Academy-of-Pediatrics. Testing for drugs of abuse in children and adolescents. American Academy of Pediatrics Committee on Substance Abuse. Pediatrics. 1996;98:305–307. [PubMed] [Google Scholar]
- Babor TF, Kadden RM. Screening and interventions for alcohol and drug problems in medical settings: what works? Journal of Trauma-Injury Infection & Critical Care. 2005;59:S80–87. doi: 10.1097/01.ta.0000174664.88603.21. discussion S94–100. [DOI] [PubMed] [Google Scholar]
- Baker A, Lee NK, Claire M, Lewin TJ, Grant T, Pohlman S, Saunders JB, Kay-Lambkin F, Constable P, Jenner L, Carr VJ. Brief cognitive behavioural interventions for regular amphetamine users: A step in the right direction. Addiction. 2005;100:367–378. doi: 10.1111/j.1360-0443.2005.01002.x. [DOI] [PubMed] [Google Scholar]
- Bastiaens L, Francis G, Lewis K. The RAFFT as a screening tool for adolescent substance use disorders. American Journal on Addictions. 2000;9:10–16. doi: 10.1080/10550490050172182. [DOI] [PubMed] [Google Scholar]
- Bastiaens L, Riccardi K, Sakhrani D. The RAFFT as a screening tool for adult substance use disorders. American Journal of Drug & Alcohol Abuse. 2002;28:681–691. doi: 10.1081/ada-120015876. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Bernstein J, Levenson S. Project ASSERT: an ED-based intervention to increase access to primary care, preventive services, and the substance abuse treatment system. Annals of Emergency Medicine. 1997;30:181–189. doi: 10.1016/s0196-0644(97)70140-9. [DOI] [PubMed] [Google Scholar]
- Breslin F, Sobell MB, Sobell LC, Buchan G, Cunningham JA. Toward a stepped care approach to treating problem drinkers: The predictive utility of within-treatment variables and therapist prognostic ratings. Addiction. 1997;92:1479–1489. [PubMed] [Google Scholar]
- Burt RD, Peterson AV., Jr Smoking cessation among high school seniors. Preventive Medicine. 1998;27:319–327. doi: 10.1006/pmed.1998.0269. [DOI] [PubMed] [Google Scholar]
- Chan AW, Pristach EA, Welte JW, Russell M. Use of the TWEAK test in screening for alcoholism/heavy drinking in three populations. Alcoholism: Clinical & Experimental Research. 1993;17:1188–1192. doi: 10.1111/j.1530-0277.1993.tb05226.x. [DOI] [PubMed] [Google Scholar]
- Chung T, Colby SM, Barnett NP, Rohsenow DJ, Spirito A, Monti PM. Screening adolescents for problem drinking: performance of brief screens against DSM-IV alcohol diagnoses. Journal of Studies on Alcohol. 2000;61:579–587. doi: 10.15288/jsa.2000.61.579. [DOI] [PubMed] [Google Scholar]
- Clark DB, Gordon AJ, Ettaro LR, Owens JM, Moss HB. Screening and brief intervention for underage drinkers. Mayo Clinic Proceedings. 2010;85:380–391. doi: 10.4065/mcp.2008.0638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DB, Moss HB. Providing alcohol-related screening and brief interventions to adolescents through health care systems: obstacles and solutions. PLoS Medicine / Public Library of Science. 2010;7:e1000214. doi: 10.1371/journal.pmed.1000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee-on-Substance-Abuse. Substance use screening, brief intervention, and referral to treatment for pediatricians. Pediatrics. 2011;128:e1330–1340. doi: 10.1542/peds.2011-1754. [DOI] [PubMed] [Google Scholar]
- Conrod PJ, Castellanos-Ryan N, Mackie C. Long-term effects of a personality-targeted intervention to reduce alcohol use in adolescents. Journal of Consulting & Clinical Psychology. 2011;79:296–306. doi: 10.1037/a0022997. [DOI] [PubMed] [Google Scholar]
- Cunningham RM, Walton MA, Goldstein A, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC. Three-month follow-up of brief computerized and therapist interventions for alcohol and violence among teens. Academic Emergency Medicine. 2009;16:1193–1207. doi: 10.1111/j.1553-2712.2009.00513.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daglish M. Brief Interventions within emergency settings. Vol. 2012. University if Queensland; 2011. [Google Scholar]
- Dahl H, Stephanson N, Beck O, Helander A. Comparison of urinary excretion characteristics of ethanol and ethyl glucuronide. Journal of Analytical Toxicology. 2002;26:201–204. doi: 10.1093/jat/26.4.201. [DOI] [PubMed] [Google Scholar]
- DuRant RH, Smith JA, Kreiter SR, Krowchuk DP. The relationship between early age of onset of initial substance use and engaging in multiple health risk behaviors among young adolescents. Archives of Pediatrics & Adolescent Medicine. 1999;153:286–291. doi: 10.1001/archpedi.153.3.286. [DOI] [PubMed] [Google Scholar]
- Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA. 1984;252:1905–1907. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick R, Davey C, Buxton MJ, Jones DR. Evaluating patient-based outcome measures for use in clinical trials. Health Technology Assessment. 2:i–iv. [PubMed] [Google Scholar]
- Fournier ME, Levy S. Recent trends in adolescent substance use, primary care screening, and updates in treatment options. Current Opinion in Pediatrics. 2006;18:352–358. doi: 10.1097/01.mop.0000236381.33907.9d. [DOI] [PubMed] [Google Scholar]
- Goll M, Schmitt G, Ganssmann B, Aderjan RE. Excretion profiles of ethyl glucuronide in human urine after internal dilution. Journal of Analytical Toxicology. 2002;26:262–266. doi: 10.1093/jat/26.5.262. [DOI] [PubMed] [Google Scholar]
- Hassan A, Harris SK, Sherritt L, Van Hook S, Brooks T, Carey P, Kossack R, Kulig J, Knight JR. Primary care follow-up plans for adolescents with substance use problems. Pediatrics. 2009;124:144–150. doi: 10.1542/peds.2008-2979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight JR, Goodman E, Pulerwitz T, DuRant RH. Reliabilities of short substance abuse screening tests among adolescent medical patients. Pediatrics. 2000;105:948–953. [PubMed] [Google Scholar]
- Knight JR, Harris SK, Sherritt L, Van Hook S, Lawrence N, Brooks T, Carey P, Kossack R, Kulig J. Adolescents’ preference for substance abuse screening in primary care practice. Substance Abuse. 2007a;28:107–117. doi: 10.1300/J465v28n04_03. [DOI] [PubMed] [Google Scholar]
- Knight JR, Harris SK, Sherritt L, Van Hook S, Lawrence N, Brooks T, Carey P, Kossack R, Kulig J. Prevalence of positive substance abuse screen results among adolescent primary care patients. Archives of Pediatrics & Adolescent Medicine. 2007b;161:1035–1041. doi: 10.1001/archpedi.161.11.1035. [DOI] [PubMed] [Google Scholar]
- Knight JR, Sherritt L, Shrier LA, Harris SK, Chang G. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Archives of Pediatrics & Adolescent Medicine. 2002;156:607–614. doi: 10.1001/archpedi.156.6.607. [DOI] [PubMed] [Google Scholar]
- Knight JR, Shrier LA, Bravender TD, Farrell M, Vander Bilt J, Shaffer HJ. A new brief screen for adolescent substance abuse. Archives of Pediatrics & Adolescent Medicine. 1999;153:591–596. doi: 10.1001/archpedi.153.6.591. [DOI] [PubMed] [Google Scholar]
- Kokkevi A, Richardson C, Florescu S, Kuzman M, Stergar E. Psychosocial correlates of substance use in adolescence: A cross-national study in six European countries. Drug and Alcohol Dependence. 2007;86:67–74. doi: 10.1016/j.drugalcdep.2006.05.018. [DOI] [PubMed] [Google Scholar]
- Levy S, Knight JR, Moore T, Weinstein Z, Sherritt L, Weiss RD. Acceptability of drug testing in an outpatient substance abuse program for adolescents. Journal of Adolescent Health. 2011;48:229–233. doi: 10.1016/j.jadohealth.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy S, Sherritt L, Vaughan BL, Germak M, Knight JR. Results of random drug testing in an adolescent substance abuse program. Pediatrics. 2007;119:e843–848. doi: 10.1542/peds.2006-2278. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2. New York, NY: Guilford Press; US; 2002. [Google Scholar]
- Pilowsky D, Wu L. Screening for alcohol and drug use disorders among adults in primary care: areview. Substance Abuse and Rehabilitation. 2012;3:25–34. doi: 10.2147/SAR.S30057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polen M, Whitlock E, Wisdom J, et al. Screening in Primary Care Settings for Illicit Drug Use: Stage Systematic Review for the United States Preventive Services Task Force [Internet] 2008 [PubMed] [Google Scholar]
- Russell M, Martier SS, Sokol RJ, Mudar P, Bottoms S, Jacobson S, Jacobson J. Screening for pregnancy risk-drinking. Alcoholism: Clinical & Experimental Research. 1994;18:1156–1161. doi: 10.1111/j.1530-0277.1994.tb00097.x. [DOI] [PubMed] [Google Scholar]
- Russell M, Martier SS, Sokol RJ, Mudar P, Jacobson S, Jacobson J. Detecting risk drinking during pregnancy: a comparison of four screening questionnaires. American Journal of Public Health. 1996;86:1435–1439. doi: 10.2105/ajph.86.10.1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schwartz RH, Silber TJ, Heyman RB, Sheridan MJ, Estabrook DM. Urine testing for drugs of abuse: a survey of suburban parent-adolescent dyads. Archives of Pediatrics & Adolescent Medicine. 2003;157:158–161. doi: 10.1001/archpedi.157.2.158. [DOI] [PubMed] [Google Scholar]
- Skipper GE, Weinmann W, Thierauf A, Schaefer P, Wiesbeck G, Allen JP, Miller M, Wurst FM. Ethyl glucuronide: a biomarker to identify alcohol use by health professionals recovering from substance use disorders. Alcohol & Alcoholism. 2004;39:445–449. doi: 10.1093/alcalc/agh078. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Connors GJ. Screening for alcohol problems: what makes a test effective? Alcohol Research & Health: the Journal of the National Institute on Alcohol Abuse & Alcoholism. 2004;28:5–16. [PMC free article] [PubMed] [Google Scholar]
- Swahn MH, Bossarte RM, Ashby JS, Meyers J. Pre-teen alcohol use initiation and suicide attempts among middle and high school students: findings from the 2006 Georgia Student Health Survey. Addictive Behaviors. 2010;35:452–458. doi: 10.1016/j.addbeh.2009.12.017. [DOI] [PubMed] [Google Scholar]
- Swahn MH, Bossarte RM, Sullivent EE., 3rd Age of alcohol use initiation, suicidal behavior, and peer and dating violence victimization and perpetration among high-risk, seventh-grade adolescents. Pediatrics. 2008;121:297–305. doi: 10.1542/peds.2006-2348. [DOI] [PubMed] [Google Scholar]
- Teesson M, Hall W, Slade T, Mills K, Grove R, Mewton L, Baillie A, Haber P. Prevalence and correlates of DSM-IV alcohol abuse and dependence in Australia: findings of the 2007 National Survey of Mental Health and Wellbeing. Addiction. 2010;105:2085–2094. doi: 10.1111/j.1360-0443.2010.03096.x. [DOI] [PubMed] [Google Scholar]
- USPSTF. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: recommendation statement. Annals of Internal Medicine. 2004;140:554–556. doi: 10.7326/0003-4819-140-7-200404060-00016. [DOI] [PubMed] [Google Scholar]
- Van Hook S, Harris SK, Brooks T, Carey P, Kossack R, Kulig J, Knight JR New England Partnership for Substance Abuse R. The “Six T’s”: barriers to screening teens for substance abuse in primary care. Journal of Adolescent Health. 2007;40:456–461. doi: 10.1016/j.jadohealth.2006.12.007. [DOI] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Shope JT, Bingham C, Zimmerman MA, Blow FC, Cunningham RM. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: A randomized controlled trial. JAMA: Journal of the American Medical Association. 2010;304:527–535. doi: 10.1001/jama.2010.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters K. Screening and Assessing Adolescents for Substance Use Disorders. US Department of health and Human Services; 1999. [Google Scholar]
- Winters K, Zenilman J U. D. o. H. a. H. Services. Simple Screening Instruments for outreach for Alcohol and Other Drug Abuse and Infectious Diseases. Vol. 11. Rockville, MD: 1994. [PubMed] [Google Scholar]
- Woicik PA, Stewart SH, Pihl RO, Conrod PJ. The Substance Use Risk Profile Scale: a scale measuring traits linked to reinforcement-specific substance use profiles. Addictive Behaviors. 2009;34:1042–1055. doi: 10.1016/j.addbeh.2009.07.001. [DOI] [PubMed] [Google Scholar]
- Wu LT, Pilowsky DJ, Patkar AA. Non-prescribed use of pain relievers among adolescents in the United States. Drug & Alcohol Dependence. 2008;94:1–11. doi: 10.1016/j.drugalcdep.2007.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Woody GE, Yang C, Pan JJ, Blazer DG. Racial/ethnic variations in substance-related disorders among adolescents in the United States. Archives of General Psychiatry. 2011;68:1176–1185. doi: 10.1001/archgenpsychiatry.2011.120. [DOI] [PMC free article] [PubMed] [Google Scholar]


