Abstract
Background
Managing Type 1 diabetes (T1D) during adolescence can be challenging, and there is a need for accessible interventions to help adolescents cope with diabetes-related stress.
Objectives
The aim of this study was to compare an Internet coping skills training (TEENCOPE) intervention to an Internet educational intervention (Managing Diabetes) for adolescents with T1D. Moderators of program efficacy were evaluated.
Methods
The study was a multisite clinical trial (n = 320) with data collected at baseline, 3 months, and 6 months. Data were collected on the primary outcomes of physiologic (A1C) and psychosocial (quality of life) and on the secondary outcomes of behavioral (self-management) and psychosocial (stress, coping self-efficacy, social competence, family conflict) variables consistent with the conceptual framework. Data were analyzed using mixed-model analyses with an intent-to-treat approach.
Results
There were no significant between-group treatment effects 6 months postintervention on primary outcomes. The Managing Diabetes youth showed a significant increase in social competence compared to the TEENCOPE youth. There were significant time effects for TEENCOPE (decreased stress and increased coping) and Managing Diabetes (improved diabetes quality of life).
Discussion
Youth with T1D transitioning to adolescence may need both structured diabetes education and coping skills to improve health outcomes. There may be a higher potential to reach adolescents with Type 1 diabetes of varying race and ethnicity via Internet interventions.
Keywords: coping skills training, interactive diabetes education, internet, Type 1 diabetes
Type 1 diabetes (T1D) is one of the most common chronic childhood diseases, affecting 1 in 400 youth (SEARCH for Diabetes in Youth Study Group et al., 2006), and the incidence appears to be rising (Gale, 2002). On the basis of national estimates of the prevalence of diabetes in youth ages 10–19 years, T1D is diagnosed most commonly in non-Hispanic White adolescents (2.88 cases per 1,000 youth), with rates somewhat lower among Black adolescents (2.07 cases per 1,000) and Hispanic adolescents (1.60 cases per 1,000) (SEARCH for Diabetes in Youth Study Group et al., 2006). The intensive treatment regimen for T1D is complex and demanding, requiring multiple daily doses of insulin (administered by injections or pump), frequent monitoring of blood glucose levels, accounting for carbohydrate intake, and making adjustments to insulin intake based on changes in diet and activity (American Diabetes Association, 2011). As children reach adolescence, metabolic control often deteriorates because of the hormonal changes of puberty associated with insulin resistance (Amiel, Sherwin, Simonson, Lauritano, & Tamborlane, 1986) and because of increasing self-management autonomy leading to lower adherence to the treatment regimen (Anderson et al., 2002). Youth with T1D from minority backgrounds have been shown to have poorer metabolic control than youth from nonminority backgrounds (Delamater et al., 1999). Furthermore, negotiating responsibility for treatment management is burdensome and stressful for adolescents and their families (Davidson, Penney, Muller, & Grey, 2004). Interventions are needed to help adolescents and families cope with the stress of modern diabetes management.
Diabetes education is a standard of care for youth with T1D (Silverstein et al., 2005). In addition, psychoeducational and family-based approaches have been applied successfully to improve diabetes-related outcomes (e.g., Anderson, Brackett, Ho, & Laffel, 1999; Harris, Harris, & Mertlich, 2005; Wysocki et al., 2008). For example, Anderson et al. (1999) found that an office-based intervention to promote parent–child teamwork improved metabolic control and parental involvement in diabetes management. Similarly, a behavioral family therapy intervention for adolescents with T1D improved metabolic control and parent–child communication over time (Wysocki et al., 2007, 2008). Coping skills training has been shown to improve quality of life (QOL) and metabolic control in adolescents with T1D (Grey, Boland, Davidson, Li, & Tamborlane, 2000). These interventions show promise for improving family functioning and adolescent outcomes, but they required in-person visits, which limits accessibility, particularly for minority and low-income adolescents and those from rural areas. It is important to consider interventions with broader reach.
Rapid advances in technology and access to the Internet have made it not only a viable mode for the delivery of psychoeducational interventions but also a platform that can be disseminated and implemented widely. In addition, Internet interventions allow for standardized program content, can be targeted to specific ages and developmental phases, allow for social interaction, and can be easily updated. Access to the Internet is becoming increasingly available nationwide and has risen to its highest level ever, with 93% of youth using the Internet regularly for school assignments, hobbies, or special interests; entertainment; and connection with others (Nielsen, 2005; Pew Research Center, 2009). Psychoeducational interventions delivered via the Internet have shown efficacy in a variety of ages and illness experiences, improving various symptoms and health behaviors (Nguyen, Kornman, & Baur, 2011; Pacifici, White, Cummings, & Nelson, 2005; Siemer, Fogel, & Van Voorhees, 2011; Williamson et al., 2005). The Internet, therefore, may represent an efficient way to deliver psychoeducational interventions to youth with T1D.
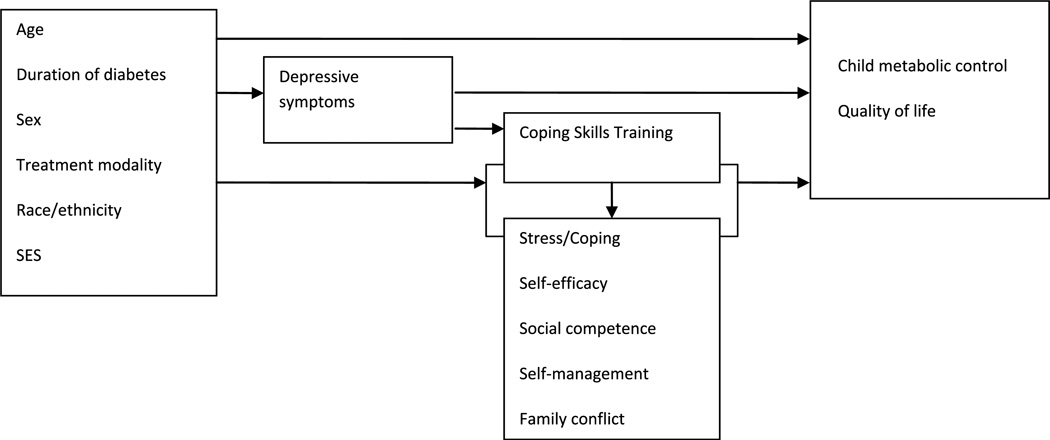
Conceptual Framework
The conceptual framework for this study was based on a stress adaptation model (Pollock, 1986) that describes the process of adaptation specific to childhood T1D (Whittemore, Jaser, Guo, & Grey, 2010). As seen in Figure 1, this framework suggests that pre-existing characteristics, such as age, duration, gender, treatment modality, race or ethnicity, and socioeconomic status, as well as individual responses such as depressive symptoms, moderate the level of individual adaptation. In addition, stress and coping, self-efficacy, social competence, self-management, and family conflict mediate these outcomes. Psychoeducational interventions are hypothesized to influence the individual’s adaptation directly and indirectly through effects on stress/coping, self-efficacy, problem solving, and self-management (Whittemore, Jaser, et al., 2010).
FIGURE 1.
Conceptual framework.
Purpose
The purpose of this randomized clinical trial was to determine the short-term effects of an Internet coping skills training program (TEENCOPE) for youth with T1D (ages 11–14 years) compared with an Internet educational program (Managing Diabetes) on the primary outcomes of metabolic control (i.e., A1C) and youth QOL and secondary outcomes of self-management, stress, coping, self-efficacy, social competence, and family conflict. In addition, moderators of program efficacy were also evaluated.
Methods
This study was a multisite (four sites), randomized, controlled, parallel-group trial conducted in the United States. Eligible participants were youth ages 11–14 years who had T1D for at least 6 months, were in a school grade appropriate for their age within a year, had never been exposed to coping skills training materials, had no other significant health problem, and had access to high-speed Internet service. Research staff assisted any adolescent without home Internet to gain access at a school, local library, or clinic. The sample of 300 participants was determined by several power analyses based on the effect sizes seen in previous studies of adolescents, accounting for 20% attrition.
Youth were recruited during follow-up visits at pediatric diabetes clinics associated with four university sites (Yale, The Children’s Hospital of Philadelphia, University of Arizona, and University of Miami) representing a range of racial, ethnic, and socioeconomic backgrounds, reflective of the national prevalence of T1D in youth. After institutional-review-board-approved consent or assent was obtained, study participants were assigned sequentially to study identification numbers that had been randomized through a computer technique created by a member of the programming team with no clinical involvement in the study. Randomization was in blocks of 10 at each site, and allocation was in a 1:1 ratio to either TEENCOPE or Managing Diabetes. Enrollment in the study was determined after participants completed informed consent and baseline surveys. When all baseline instruments were complete, the system generated an e-mail message informing the study participant of group assignment.
Investigators, clinicians, and research staff who completed informed consent and data collection were kept blinded to study assignment. Study participants were blind to assignment until after the completion of baseline data collection. Two staff members at Yale who were not involved in data collection were able to access participants’ assignments to answer questions or troubleshoot issues youth had in accessing programs. Staff members took all efforts to maintain masking and equipoise during the study.
Interventions
TEENCOPE is an Internet program based on a successful in-person coping skills training program for youth with T1D (Grey et al., 2000). Coping skills training is derived from Bandura’s social cognitive theory and involves practicing and rehearsing a new behavior (i.e., coping skills) to enhance self-efficacy and promote positive behaviors (Bandura, 1986). The goal of coping skills training is to increase competence and mastery by retraining nonconstructive coping styles and behaviors into more constructive behaviors.
TEENCOPE was designed using a graphic novel format and a cast of ethnically diverse characters with T1D who present challenging social situations, approaches to solving problems, and consequences of decisions. Specific content includes social skills training, cognitive behavior modification, assertive communication, stress reduction, and conflict resolution. There were five sessions released weekly that were highly interactive and encouraged self-assessment and the use of coping skills. Upon completion of sessions, responses to interactive aspects were posted on a personal profile so that participants were able to learn from each other. At the end of each session, participants were asked to practice the new coping skills that were presented in that session during the upcoming week and to share experiences on a discussion board moderated by a health professional (PhD or RN). A description of the program development has been published (Whittemore, Grey, Lindemann, Ambrosino, & Jaser, 2010).
Managing Diabetes is an Internet diabetes educational program also modeled after an in-person educational program for adolescents with T1D. Managing Diabetes served as the attention control condition in this study. To parallel the TEENCOPE program, Managing Diabetes consisted of five sessions that were released to teens weekly over 5 weeks. The sessions included case studies and problem-solving exercises intended to enhance teens’ capacity to make diabetes-related decisions. Although all youth with T1D receive ongoing education in routine care, Managing Diabetes was designed to provide additional knowledge and problem-solving skills on intensive insulin regimens (multiple daily injections or pump), carbohydrate counting, sports and sick days, and healthy lifestyles. The sessions contained culturally relevant content (i.e., the inclusion of diverse foods) and problem-solving activities (i.e., rate this plate). The sessions were enhanced with pictures and were highly interactive; programmed responses were used to give youth tailored feedback on their answers to questions and problem-solving activities. No interaction with other teens occurred in the Managing Diabetes program.
Measures
Data were collected at baseline, 3 months, and 6 months (12-and 18-month data collection is ongoing). The primary outcomes included physiological (A1C) and psychosocial (QOL) variables. Secondary outcomes included behavioral (self-management) and psychosocial (stress, coping, self-efficacy, social competence, and family conflict) variables consistent with the conceptual framework. Satisfaction was evaluated using a brief survey with a total score ranging from 0 to 5. All data were collected via online survey with the exception of clinical data that were collected by retrospective chart review and demographic data that were completed at the time of consent by parents. Reliability and validity of all measures have been reported previously (Grey, Whittemore, Liberti, Delamater, Murphy, & Faulkner, 2012).
Primary Outcomes
Physiological Adaptation
Glycosylated hemoglobin (A1C) is measured routinely every 3 months in patients with diabetes. The glycosylation of the hemoglobin molecule provides objective criteria of metabolic control over the past 8–12 weeks and was the primary outcome. Analyses were performed using the Bayer Diagnostics DCA2000, which provides results in 6 minutes on a fingerstick blood sample (normal range = 4.2%–6.3%; American Diabetes Association, 2007). A small percentage of clinics (12%) measured A1C using alternative methods (i.e., HPLC, Roche Tina-quant, immunoturbidimetry). Statistical analyses indicated no significant variability in measurements analyzed using different methods.
Psychosocial Adaptation
Quality of life was evaluated using the Pediatric QOL Inventory designed for children with chronic health conditions (Varni, Seid, & Rode, 1999). The instrument consists of a 15-item core measure of global health-related QOL and a 28-item supplemental measure assessing diabetes-specific QOL. Higher scores reflect better QOL. High reliability and validity have been established in various clinical and community samples (Varni, Seid, & Kurtin, 2001; Varni et al., 1999). Cronbach’s alpha was .87 for the global measure and .90 for the diabetes-specific measure.
Secondary Outcomes
Diabetes self-management was measured with the Self-Management of Type 1 Diabetes in Adolescence, a 52-item scale evaluated on a 4-point Likert scale (Schilling et al., 2007). The instrument measures youth reports of five domains of self-management of diabetes (collaboration with parents, diabetes care activities, problem solving, communication, and goals). Cronbach’s alpha ranged from .63 for the goal subscale to .80 for the collaboration with parents subscale. The low internal consistency of the goal subscale may be a result of having few items (n = 7).
Stress was measured by the Perceived Stress Scale, a 14-item scale designed to evaluate the degree to which situations in one’s life are unpredictable, uncontrollable, and overloading (Cohen, Kamarck, & Mermelstein, 1983). Items are used to assess feelings of stress, hassles, and coping during the past month. Respondents rate items on a 5-point Likert scale ranging from 0 (never) to 4 (very often), with higher scores indicative of greater perceived stress. Cronbach’s alpha was .80.
Coping style in response to diabetes-related stressors was measured with the Responses to Stress Questionnaire (Connor-Smith, Compas, Wadsworth, Thomsen, & Saltzman, 2000). The first 10 items of the measure list stressors specific to adolescents with T1D (Davidson et al., 2004), followed by 57 items asking how the individual responds to these stressors. The scale includes three coping factors: primary control engagement coping (problem solving, emotional modulation, emotional expression), secondary control engagement coping (positive thinking, cognitive restructuring, acceptance, distraction), and disengagement coping (avoidance, denial, wishful thinking). To control for response bias and individual differences in base rates of item endorsement (e.g., gender differences in total number of coping strategies endorsed), pro-portion scores were used for all analyses. Cronbach’s alpha for our sample ranged from .77 to .87.
The Self-Efficacy for Diabetes Scale measures the self-perceptions held by youth with diabetes about their personal competence, power, and resourcefulness for managing their diabetes successfully (Grossman, Brink, & Hauser, 1987). The scale consists of 35 items in three subscales: diabetes-specific self-efficacy (24 items), medical self-efficacy (5 items), and general self-efficacy (6 items). Youth are asked to rate their degree of confidence for items on a 5-point scale (very sure I can’t to very sure I can); higher scores are indicative of lower self-efficacy. Items have been modified from the original version to include current T1D modalities (i.e., pump therapy). Only the diabetes subscale was used, which had a Cronbach’s alpha of .90 in this sample.
Social competence was measured via the social acceptance subscale of the Self-Perception Profile for Adolescents (Harter, 1988). The subscale consists of five items, and each item consists of a statement about two groups of people who are dissimilar (e.g., some people are able to make really close friends but other people are unable to make really close friends). Youth choose which group he or she resembles the most and then indicate whether the statement is “really true for me” or “sort of true for me.” Statements are scored on a 4-point rating scale, such that high scores reflect greater perceived competence. Cronbach’s alpha for this sample was .75.
The revised Diabetes Family Conflict Scale was used to evaluate diabetes treatment conflict (Hood, Butler, Anderson, & Laffel, 2007). The scale is a 19-item questionnaire adapted from the Diabetes Responsibility and Conflict Checklist (Rubin, Young-Hyman, & Peyrot, 1989) and is used to measure the degree of conflict between family members on diabetes management activities. Diabetes conflict is rated on a 3-point scale (1 = never argue, 2 = sometimes argue, and 3 = always argue), with higher scores indicative of greater conflict. Cronbach’s alpha for this sample was .87.
The Children’s Depression Inventory was used to measure self-reported depressive symptoms, including disturbance in mood, self-evaluation, vegetative functions, and interpersonal behaviors of youth (Kovacs, 1985). It contains 27 multiple-choice items that yield total scores from 0 to 54. The item that addresses suicidal ideation was eliminated due to the inability to respond immediately to a positive endorsement. Higher scores reflect a higher number of symptoms. Youth who scored above the threshold for depression (12 or higher) were contacted by a qualified study staff member (psychologist, nurse, or social worker) who conducted a depression assessment and made appropriate referrals. Cronbach’s alpha in this sample was .90.
Data Analysis
The sample and each of the variables were described using frequency distributions and appropriate summary statistics for central tendency and variability. Differences between groups at baseline were tested with t tests or Chi-square tests, depending on the type of measurement. The principal aim of the study was to test the hypothesis that youth who received the TEENCOPE program will demonstrate better physiologic (A1C) and psychosocial (QOL) adaptation than youth who received an Internet educational program. The effect of the intervention on secondary endpoints of self-management, perceived stress, coping, self-efficacy, social competence, and family conflict was evaluated. To accomplish these aims, a series of mixed effects linear regression models (repeated measures ANOVA with arbitrary within-subject correlation structures) in the SAS procedures MIXED (for continuous outcomes) and the generalized estimating equations methods provided by GENMOD (for dichotomous outcomes) were conducted using an intent-to-treat approach. Indicator variables to test for differences of the experimental (TEENCOPE) and control groups and baseline covariates, such as age, gender, race or ethnicity, treatment modality, and income, were included in these regression models.
Moderation analysis was performed to see if the time effect on outcome variables was moderated by demographic (age, gender, race or ethnicity, income) or clinical (therapy type, elevated depressive symptoms) variables consistent with the conceptual model. Moderation effects (moderating time effect on the primary outcomes in each intervention) were tested using a longitudinal effect model adjusted for the covariates.
Results
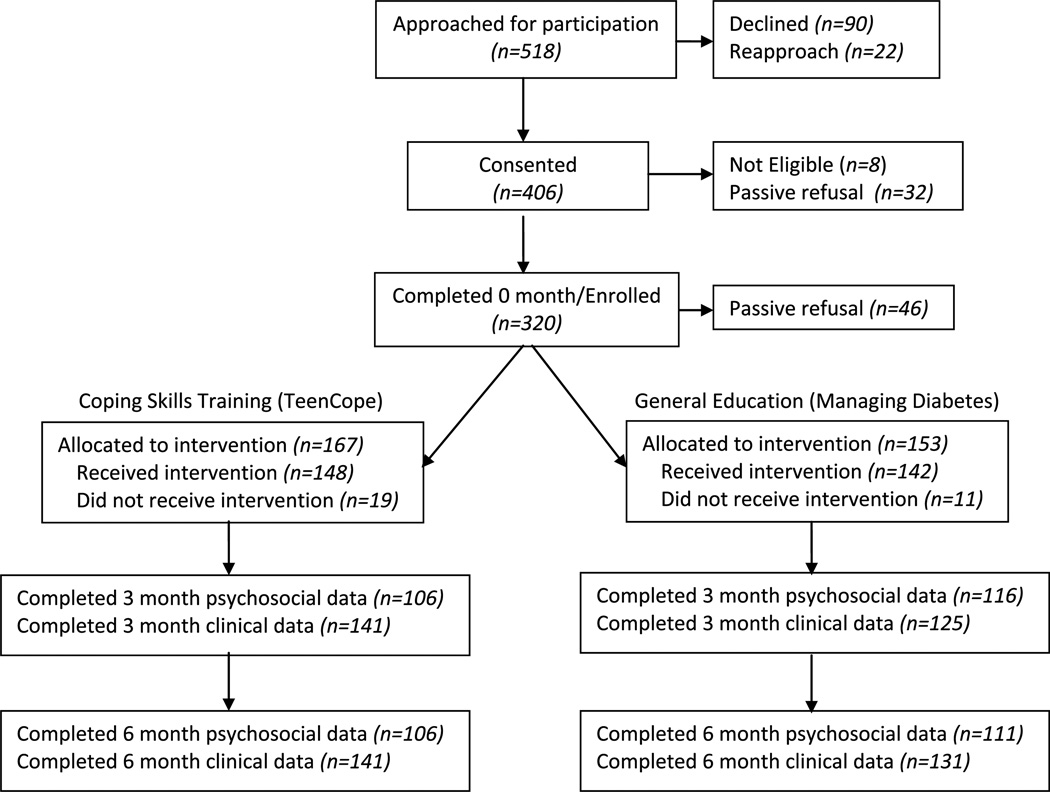
The sample included 320 youth with T1D (Figure 2). The mean age was 12.3 (±1.1) years, mean duration of diabetes was 6.1 (±3.5) years, mean A1C was 8.3% (±1.5%), and 60% were on pump therapy. Most participants were White (72%) and women (55%), and 51% had high family income (≥$80,000/year). There were no significant differences between groups on demographic or clinical variables with the exception of parent education, which was significantly higher in the Managing Diabetes group (Table 1). There were also significant differences between sites with respect to race or ethnicity, income, therapy time, parent education, and A1C, so site was controlled in all mixed model analyses.
FIGURE 2.
Consort table.
TABLE 1.
Comparison of Demographic and Clinical Characteristics by Group
| TEENCOPE, n = 167 n (%) |
Managing diabetes, n = 153 n (%) |
p | |
|---|---|---|---|
| Age (in years) | |||
| 11–12 | 95 (56.9) | 90 (58.8) | .7259 |
| 13–14 | 72 (43.1) | 63 (41.2) | |
| Gender | |||
| Male | 74 (44.3) | 69 (45.1) | .8876 |
| Female | 93 (55.7) | 84 (54.9) | |
| Race | |||
| White, non-Hispanic/non-Latino | 107 (64.5) | 93 (61.2) | .8820 |
| White, Hispanic/Latino | 30 (18.1) | 34 (22.4) | |
| Black | 14 (8.4) | 11 (7.2) | |
| Multiracial | 12 (7.2) | 12 (7.9) | |
| Other | 3 (1.8) | 2 (1.3) | |
| Socioeconomic status | |||
| <$40,000 | 35 (22.2) | 30 (19.9) | .6627 |
| $40,000–$79,999 | 44 (27.8) | 43 (28.5) | |
| $80,000+ | 79 (50.0) | 78 (51.6) | |
| Therapy type | |||
| Pump | 99 (59.3) | 91 (59.5) | .9716 |
| Injection | 68 (40.7) | 62 (40.5) | |
| Mean (SD) | Mean (SD) | ||
| Parent/guardian education (in years) | 14.3 (2.7) | 15.0 (2.9) | .0320 |
| Duration (months) | 365 (230) | 342 (208) | .3481 |
| A1C at baseline (%) | 8.4 (1.6) | 8.2 (1.3) | .1439 |
Adherence to the completion of sessions was high: 77% of TEENCOPE and 79% of Managing Diabetes participants completed four or more of the five sessions. In addition, 52% of youth in TEENCOPE participated in the discussion board component of the program. Satisfaction with programs was high with no significant difference between TEENCOPE (3.97 ± 0.71) and Managing Diabetes (3.89 ± 0.56) participants. Girls (p < .001), non-White youth (p = .017), and low-income youth (p = .024) reported higher satisfaction compared with boys, White, and high-income youth.
Youth reported moderate self-management activities (collaboration with parents, diabetes care activities, problem solving, goal setting), social acceptance, and diabetes QOL; low perceived stress and family conflict; and high general QOL. Seventeen percent of youth indicated elevated depressive symptoms (Table 2).
TABLE 2.
Baseline Comparison of Psychosocial Variables by Group
| TEENCOPE, n = 167 mean (SD) | Managing diabetes, n = 153 mean (SD) | p | |
|---|---|---|---|
| Self-management of Type 1 diabetes | |||
| Collaboration with parents | 22.1 (6.5) | 21.4 (6.9) | .3787 |
| Diabetes care activity | 31.8 (5.6) | 32.6 (5.9) | .2071 |
| Diabetes problem solving | 14.7 (3.7) | 14.2 (4.2) | .2158 |
| Diabetes communication | 17.7 (5.0) | 17.8 (5.6) | .8758 |
| Goal | 15.5 (2.9) | 15.7 (2.6) | .5482 |
| Self-perception profile | |||
| Social acceptance | 16.5 (2.9) | 16.3 (3.3) | .4540 |
| Perceived stress scale | 21.7 (7.7) | 20.9 (8.1) | .3180 |
| Diabetes family conflict scale | 26.6 (5.9) | 26.0 (5.8) | .3262 |
| Self-efficacy for diabetes | |||
| Diabetes specific | 45.4 (11.2) | 44.6 (11.2) | .5175 |
| Pediatric quality of life inventory | 80.3 (10.9) | 81.4 (11.3) | .4006 |
| Physical health | 87.0 (11.6) | 88.4 (11.0) | .3190 |
| Psychological health | 76.8 (12.7) | 77.6 (13.3) | .5584 |
| PedsQL diabetes module | 63.8 (15.2) | 64.0 (15.8) | .8970 |
| Responses to stress questionnaire | |||
| Primary control coping | 0.19 (0.04) | 0.20 (0.04) | .0160 |
| Secondary control coping | 0.26 (0.05) | 0.27 (0.06) | .1564 |
| Disengagement coping | 0.15 (0.03) | 0.14 (0.03) | .2095 |
| Stress reactivity | 0.19 (0.04) | 0.18 (0.04) | .0495 |
There were no significant differences between TEENCOPE and Managing Diabetes participants on the primary outcomes of physiologic (A1C) or psychosocial (QOL) adaptation. With respect to secondary outcomes, there was a significant increase in perceived social acceptance by Managing Diabetes participants compared with TEENCOPE participants (p = .013); however, there were no differences between groups on any other secondary outcomes. The hypothesis that TEENCOPE participants would have significant improvement in outcomes compared with Managing Diabetes was not supported at 6-month follow-up.
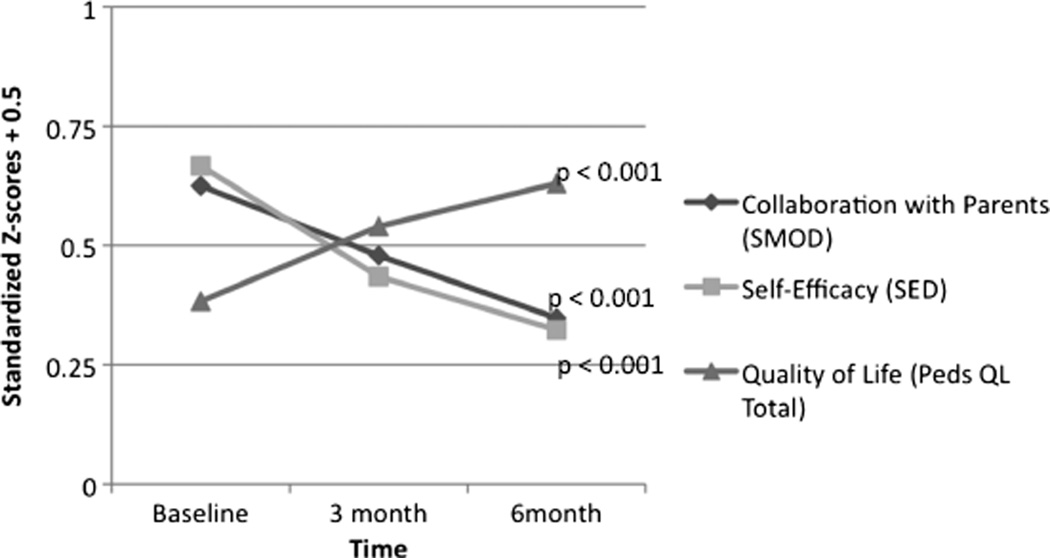
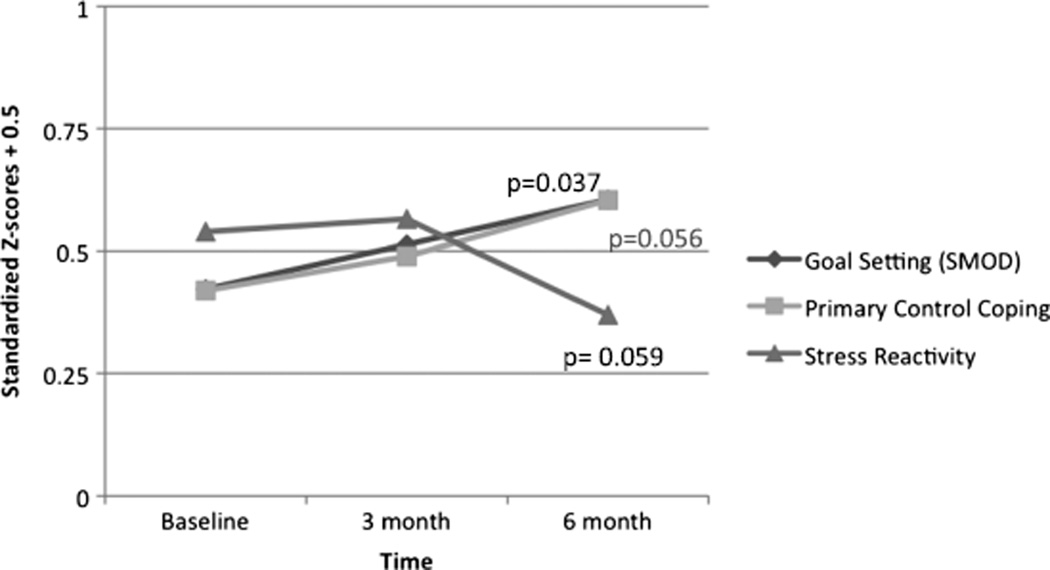
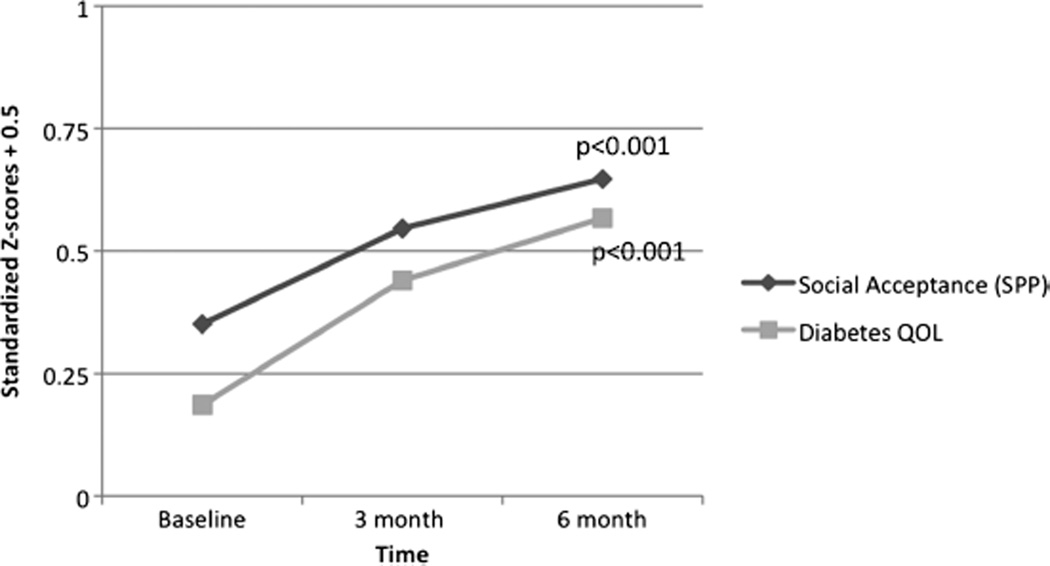
There were, however, significant time effects for both groups. Participants in both TEENCOPE and Managing Diabetes showed a significant decrease in collaboration with parents (p < .05) and a significant increase in diabetes self-efficacy (p < .001) and global QOL at 6 months (p < .05; Figure 3). For Managing Diabetes participants, there was a significant increase in social acceptance (p < .001) and diabetes QOL (p < .001; Figure 4). In addition, for TEENCOPE participants, there was a significant decrease in perceived stress (p < .05) and an increase in primary control coping (p = .06; Figure 5). Family conflict decreased over time in both groups; however, this was not statistically significant. The A1C levels increased in the Managing Diabetes group (p = .014). In Figures 3–5, standardized z scores are used to allow for comparison of data with different metrics.
FIGURE 3.
Time effects for TEENCOPE and Managing Diabetes combined.
FIGURE 4.
Time effects for Managing Diabetes.
FIGURE 5.
Time effects for TEENCOPE.
The effects of the interventions on A1C were not moderated by any demographic variables. However, the effects of the interventions on diabetes QOL were moderated by gender and depressive symptoms (Table 3). Specifically, boys in the Managing Diabetes program had greater improvements in diabetes QOL compared with TEENCOPE participants (4.19 ± 1.01 vs. 1.03 ± 0.89; p = .019). Baseline depressive symptoms also moderated group effects on changes in overall QOL (6.86 ± 1.25 vs. 0.27 ± 0.50; p < .001) and diabetes QOL (5.75 ± 1.88 vs. 0.39 ± 0.76; p = .009). Youth with elevated depressive symptoms (Children’s Depression Inventory, ≥12) in the TEENCOPE group showed greater improvements in QOL compared with youth who did not have elevated depressive symptoms at baseline. This effect was not seen for Managing Diabetes participants.
TABLE 3.
Moderation Effects on the Primary Outcomes Over 6 Months
| Effect on HbA1c coefficients ± SE |
Effect on overall quality of life (total PedsQL) coefficients ± SE |
Effect on quality of life for diabetes (DAIBMOD) coefficients ± SE |
||||
|---|---|---|---|---|---|---|
| TEENCOPE | Managing diabetes |
TEENCOPE | Managing diabetes |
TEENCOPE | Managing diabetes |
|
| Gender | ||||||
| Male | 0.27 ± 0.27 | 0.39 ± 0.28 | 1.78 ± 0.73 | 2.09 ± 0.68 | 0.70 ± 1.07 | 4.19 ± 1.01 |
| Female | 0.24 ± 0.26 | 0.57 ± 0.27 | 0.76 ± 0.62 | 1.31 ± 0.60 | 1.45 ± 0.92 | 1.03 ± 0.89 |
| Difference by gender (p) | .9255 | .5745 | .2914 | .3936 | .5962 | .0199a |
| Income | ||||||
| High income ($60,000+) | 0.06 ± 0.23 | 0.35 ± 0.23 | 1.01 ± 0.58 | 1.77 ± 0.54 | 0.50 ± 0.86 | 2.77 ± 0.79 |
| Low income (<$60,000) | 0.66 ± 0.33 | 0.83 ± 0.36 | 1.56 ± 0.82 | 1.37 ± 0.84 | 2.42 ± 1.22 | 1.58 ± 1.25 |
| Difference by income (p) | .1286 | .2407 | .5845 | .6893 | .2001 | .4233 |
| Child age (years) | ||||||
| Older (11–12) | 0.26 ± 0.24 | 0.65 ± 0.25 | 2.00 ± 0.81 | 1.03 ± 0.67 | 2.33 ± 1.20 | 1.46 ± 1.00 |
| Younger (13–14) | 0.24 ± 0.30 | 0.26 ± 0.31 | 0.77 ± 0.58 | 2.16 ± 0.61 | 0.51 ± 0.87 | 3.19 ± 0.90 |
| Difference by child age (p) | .9402 | .3764 | .2190 | .2138 | .2224 | .2005 |
| Therapy type | ||||||
| Injection | −0.04 ± 0.31 | 0.62 ± 0.32 | 1.14 ± 0.76 | 1.67 ± 0.73 | 1.32 ± 1.13 | 2.98 ± 1.09 |
| Pump | 0.43 ± 0.24 | 0.41 ± 0.25 | 1.22 ± 0.61 | 1.64 ± 0.57 | 1.02 ± 0.90 | 2.07 ± 0.85 |
| Difference by therapy (p) | .2214 | .6816 | .9325 | .9710 | .8375 | .5121 |
| Race | ||||||
| White, non-Hispanic/non-Latino | 0.33 ± 0.23 | 0.45 ± 0.25 | 0.74 ± 0.57 | 1.41 ± 0.56 | 0.28 ± 0.85 | 2.25 ± 0.83 |
| Black/other ethnicity | 0.09 ± 0.33 | 0.55 ± 0.32 | 2.17 ± 0.84 | 2.10 ± 0.76 | 3.01 ± 1.25 | 2.72 ± 1.12 |
| Difference by race (p) | .5455 | .7378 | .1625 | .4608 | .0728 | .7414 |
| Depression | ||||||
| Low depression (CDI < 12) | 0.27 ± 0.20 | 0.43 ± 0.21 | 0.27 ± 0.50 | 1.55 ± 0.48 | 0.39 ± 0.76 | 2.12 ± 0.72 |
| High depression (CDI ≥ 12) | 0.12 ± 0.51 | 0.67 ± 0.47 | 6.86 ± 1.25 | 2.23 ± 1.17 | 5.75 ± 1.88 | 4.13 ± 1.77 |
| Difference by depression (p) | .7798 | .6448 | <.0001a | .5932 | .0090a | .2943 |
Note. CDI = Children’s Depression Inventory.
Significant moderation effect.
Discussion
The primary purpose of this study was to compare the efficacy of two Internet psychoeducational programs. The hypothesis that TEENCOPE would result in better adaptation after 6 months compared with Managing Diabetes was not supported. The use of a relatively sophisticated attention control condition may explain the lack of differential outcomes.
Despite the fact that the hypothesis was not supported, there is much to be learned from this study. Different but complementary effects of the two interventions occurred that were consistent with the conceptual framework. These results suggest that Managing Diabetes provides skills in healthy lifestyles and diabetes problem solving whereas TEENCOPE provides support for altering primary control coping. Because previous studies have shown that youth with T1D require both education as well as coping support (Grey et al., 2000), both may be necessary for youth to manage a complex condition like T1D and to improve both QOL as well as self-management and psychosocial outcomes. In future analyses, mediators of each program will be tested.
Because diabetes education is a standard of care for youth with T1D, it may be surprising that an Internet diabetes educational program like Managing Diabetes, based on standard diabetes education, resulted in improved outcomes. Providing the program via the Internet may be particularly appealing to youth who are very technologically savvy. The program was provided in a format that youth are very comfortable with, was easy to access, and allowed youth to go through the program at their own pace. In addition, the Managing Diabetes program was written specifically for youth, whereas written education materials provided to youth may be geared toward parents. In addition, delivery of an interactive educational program that included case studies and problem-solving exercises via the Internet enhanced teens’ capacity to make diabetes-related decisions due to the immediate feedback that the material provided. The average duration of diabetes was 6 years in this sample, suggesting that youth’s initial diabetes education may have been more focused on parents and less so on their own problem-solving skills necessary for self-management as youth transition to adolescence. Therefore, an Internet educational program at this developmental transition to greater independent diabetes self-management appears warranted.
The transition to adolescence in youth with T1D is a challenging period, developmentally, physiologically, and behaviorally. Hormonal influences as well as the drive toward independence and the resulting increase in conflict with parents and other authority figures have been associated with worsening metabolic control in youth with T1D (Anderson, Loughlin, Goldberg, & Laffel, 2001). Although it may seem counter-intuitive that the lack of difference in A1C is a positive outcome, under usual care conditions, it would be expected that A1C levels would deteriorate during this transitional time. Maintenance of metabolic control during this transition is likely an improvement over usual care. In addition, although a decrease in collaboration with parents would be expected at this age, it is a positive finding that family conflict did not increase and self-efficacy and QOL did improve.
Although primary outcomes did not improve significantly in the TEENCOPE group compared with the Managing Diabetes group, improvements in perceived stress and adaptive coping strategies and maintenance of A1C levels in the TEENCOPE group suggest that the program is effective in altering important mediators of outcomes. Similarly, Managing Diabetes resulted in improved social acceptance and diabetes QOL, again supporting several hypothesized relationships in the framework.
Program participation in both programs was very high compared with previous studies of in-person interventions (Grey et al., 2000). Internet-based interventions have the potential to reach more youth for several reasons. Probably most important is the high level of Internet access for youth today (Pew Research Center, 2009). Youth today also participate in many activities, making extra trips to a clinical center difficult, but the ability to access the Internet on their own time allows youth the opportunity to participate in psychoeducational programs.
In this study, youth of different races and ethnicities were recruited across four sites, so the data advance understanding not only of the impact of psychoeducational interventions in youth with T1D but also of the ability of Internet programs to reach youth of varying race and ethnicity. There were high participation rates across racial and ethnic subgroups in this study, suggesting that Internet interventions may be a way to successfully engage such youth in such programs. Indeed, non-White youth were highly satisfied with the Internet programs.
In this study, however, very few moderators were found. Managing Diabetes had a greater effect than TEENCOPE on diabetes QOL for boys. It may be that the timing and delivery format for diabetes education was particularly relevant for boys. On the other hand, TEENCOPE had a greater effect on QOL for youth with depressive symptoms. It is possible that depressed youth were able to benefit more from the coping skills taught in TEENCOPE, as depressive symptoms in youth have been associated with less use of adaptive coping strategies (Jaser et al., 2008).
Despite the multiple strengths of this study, such as theoretical consistency and an adequate sample, the study has limitations. It was conducted at four major pediatric diabetes centers, which may not represent the larger population of transitioning youth with T1D. For example, 51% of the sample used insulin pump therapy, which may be higher than the total population. Approximately 50% of the sample was also of high income. In addition, in this article, only short-term outcomes were reported. It is possible that, given the mediating effects suggested by the data, a longer period of follow-up is needed to see changes in outcomes.
Nonetheless, the results of the study suggest that youth with T1D transitioning to adolescence may benefit from both Internet diabetes education and coping skills to reduce stress, improve QOL, and maintain A1C. In addition, the use of Internet-based interventions resulted in high participation rates and satisfaction in both White and non-White populations. The use of such interventions to increase access to psychoeducational programming is warranted.
Acknowledgments
The following individuals and institutions constitute the TEENCOPE Study Group (1R01NR004009-12) (* indicates principal investigator or director): Yale University School of Nursing: M. Grey*, R. Whittemore*, W. Tamborlane, L. Liberti, S. Jaser, N. Hunter, S. Jeon, T. Ma; Children s Hospital of Philadelphia: K. Murphy*, S. Dumser; University of Arizona College of Nursing: M. Faulkner*, S. Michaliszyn, E. Crockett; University of Miami Department of Pediatrics: A. Delamater*, J. Hernandez, D. Wile.
Funding for this study was provided by Grant 2R01NR04009 from the National Institute of Nursing Research, Clinical Trial Registry NCT00684658.
Footnotes
A version of this study was presented at the annual meeting of the International Society for Pediatric and Adolescent Diabetes. October, 2011, Miami, FL. Special acknowledgment to Heather Jacobs, RN, MPH who assisted with the preparation of this manuscript.
The authors have no conflicts of interest to disclose.
Contributor Information
Robin Whittemore, School of Nursing, Yale University, New Haven, Connecticut.
Sarah S. Jaser, School of Nursing, Yale University, New Haven, Connecticut.
Sangchoon Jeon, School of Nursing, Yale University, New Haven, Connecticut.
Lauren Liberti, School of Nursing, Yale University, New Haven, Connecticut.
Alan Delamater, Department of Pediatrics, University of Miami, Coral Gables, Florida.
Kathleen Murphy, Diabetes Center for Children, The Children’s Hospital of Philadelphia, Pennsylvania.
Melissa S. Faulkner, Diabetes Research, College of Nursing, University of Arizona, Tucson.
Margaret Grey, School of Nursing, Yale University, New Haven, Connecticut.
References
- American Diabetes Association. Standards of medical care in diabetes—2007. Diabetes Care. 2007;30(Suppl 1):S4–S41. doi: 10.2337/dc07-S004. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association. Standards of medical care in diabetes—2011. Diabetes Care. 2011;34(Suppl 1):S11–S61. doi: 10.2337/dc11-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amiel SA, Sherwin RS, Simonson DC, Lauritano AA, Tamborlane WV. Impaired insulin action in puberty. A contributing factor to poor glycemic control in adolescents with diabetes. The New England Journal of Medicine. 1986;315(4):215–219. doi: 10.1056/NEJM198607243150402. [DOI] [PubMed] [Google Scholar]
- Anderson B, Loughlin C, Goldberg E, Laffel L. Comprehensive, family-focused outpatient care for very young children living with chronic disease: Lessons from a program in pediatric diabetes. Children’s Services: Social Policy, Research, and Practice. 2001;4:235–250. [Google Scholar]
- Anderson BJ, Brackett J, Ho J, Laffel LM. An office-based intervention to maintain parent–adolescent teamwork in diabetes management. Impact on parent involvement, family conflict, and subsequent glycemic control. Diabetes Care. 1999;22(5):713–721. doi: 10.2337/diacare.22.5.713. [DOI] [PubMed] [Google Scholar]
- Anderson BJ, Vangsness L, Connell A, Butler D, Goebel-Fabbri A, Laffel LM. Family conflict, adherence, and glycaemic control in youth with short duration type 1 diabetes. Diabetic Medicine: A Journal of the British Diabetic Association. 2002;19(8):635–642. doi: 10.1046/j.1464-5491.2002.00752.x. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York, NY: W.H. Freedman; 1986. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology. 2000;68(6):976–992. [PubMed] [Google Scholar]
- Davidson M, Penney ED, Muller B, Grey M. Stressors and self-care challenges faced by adolescents living with type 1 diabetes. Applied Nursing Research. 2004;17(2):72–80. doi: 10.1016/j.apnr.2004.02.006. [DOI] [PubMed] [Google Scholar]
- Delamater AM, Shaw KH, Applegate EB, Pratt IA, Eidson M, Lancelotta GX, Richton S. Risk for metabolic control problems in minority youth with diabetes. Diabetes Care. 1999;22(5):700–705. doi: 10.2337/diacare.22.5.700. [DOI] [PubMed] [Google Scholar]
- Gale EA. The rise of childhood type 1 diabetes in the 20th century. Diabetes. 2002;51(12):3353–3361. doi: 10.2337/diabetes.51.12.3353. [DOI] [PubMed] [Google Scholar]
- Grey M, Boland EA, Davidson M, Li J, Tamborlane WV. Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. The Journal of Pediatrics. 2000;137(1):107–113. doi: 10.1067/mpd.2000.106568. [DOI] [PubMed] [Google Scholar]
- Grey M, Whittemore R, Liberti L, Delamater A, Murphy K, Faulkner MS. A comparison of two internet programs for adolescents with type 1 diabetes: Design and methods. Contemporary Clinical Trials. 2012;33:769–776. doi: 10.1016/j.cct.2012.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman HY, Brink S, Hauser ST. Self-efficacy in adolescent girls and boys with insulin-dependent diabetes mellitus. Diabetes Care. 1987;10(3):324–329. doi: 10.2337/diacare.10.3.324. [DOI] [PubMed] [Google Scholar]
- Harris MA, Harris BS, Mertlich D. Brief report: In-home family therapy for adolescents with poorly controlled diabetes: Failure to maintain benefits at 6-month follow-up. Journal of Pediatric Psychology. 2005;30(8):683–688. doi: 10.1093/jpepsy/jsi055. [DOI] [PubMed] [Google Scholar]
- Harter S. Manual for the adolescent self-perception profile. Denver, CO: University of Denver; 1988. [Google Scholar]
- Hood KK, Butler DA, Anderson BJ, Laffel LM. Updated and revised Diabetes Family Conflict Scale. Diabetes Care. 2007;30(7):1764–1769. doi: 10.2337/dc06-2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaser SS, Fear JM, Reeslund KL, Champion JE, Reising MM, Compas BE. Maternal sadness and adolescents’ responses to stress in offspring of mothers with and without a history of depression. Journal of Clinical Child and Adolescent Psychology. 2008;37(4):736–746. doi: 10.1080/15374410802359742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. The Children’s Depression Inventory (CDI) Psychopharmacology Bulletin. 1985;21(4):995–998. [PubMed] [Google Scholar]
- Nguyen B, Kornman KP, Baur LA. A review of electronic interventions for prevention and treatment of overweight and obesity in young people. Obesity Reviews. 2011;12(5):e298–e314. doi: 10.1111/j.1467-789X.2010.00830.x. [DOI] [PubMed] [Google Scholar]
- Nielsen J. Usability of websites for teenagers. 2005 Jan 31; [Website]. Retrieved from http://www.useit.com/alertbox/20050131.html.
- Pacifici C, White L, Cummings K, Nelson C. Vstreet.com: A Web-based community for at-risk teens. Child Welfare. 2005;84(1):25–46. [PubMed] [Google Scholar]
- Pew Research Center. Demographics of teen internet users. 2009 Retrieved from http://www.pewinternet.org/Static-Pages/Trend-Data-for-Teens/Whos-Online.aspx.
- Pollock SE. Human responses to chronic illness: Physiologic and psychosocial adaptation. Nursing Research. 1986;35(2):90–95. [PubMed] [Google Scholar]
- Rubin R, Young-Hyman D, Peyrot M. Parent–child responsibility and conflict in diabetes care. Diabetes. 1989;38:28. [Google Scholar]
- Schilling LS, Dixon JK, Knafl KA, Grey M, Ives B, Lynn MR. Determining content validity of a self-report instrument for adolescents using a heterogeneous expert panel. Nursing Research. 2007;56(5):361–366. doi: 10.1097/01.NNR.0000289505.30037.91. [DOI] [PubMed] [Google Scholar]
- SEARCH for Diabetes in Youth Study Group. Liese AD, D’Agostino RB, Jr, Hamman RF, Kilgo PD, Lawrence JM, Williams DE. The burden of diabetes mellitus among US youth: Prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics. 2006;118(4):1510–1518. doi: 10.1542/peds.2006-0690. [DOI] [PubMed] [Google Scholar]
- Siemer CP, Fogel J, Van Voorhees BW. Telemental health and web-based applications in children and adolescents. Child and Adolescent Psychiatric Clinics of North America. 2011;20(1):135–153. doi: 10.1016/j.chc.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein J, Klingensmith G, Copeland K, Plotnik L, Kaufman F, Laffel L American Diabetes Association. Care of children and adolescents with type 1 diabetes: A statement of the American Diabetes Association. Diabetes Care. 2005;28(1):186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- Varni JW, Seid M, Kurtin PS. PedsQL 4.0: Reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Medical Care. 2001;39(8):800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- Varni JW, Seid M, Rode CA. The PedsQL: Measurement model for the pediatric quality of life inventory. Medical Care. 1999;37(2):126–139. doi: 10.1097/00005650-199902000-00003. [DOI] [PubMed] [Google Scholar]
- Whittemore R, Grey M, Lindemann E, Ambrosino J, Jaser S. Development of an internet coping skills training program for teenagers with type 1 diabetes. Computers, Informatics, Nursing. 2010;28(2):103–111. doi: 10.1097/NCN.0b013e3181cd8199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittemore R, Jaser S, Guo J, Grey M. A conceptual model of childhood adaptation to type 1 diabetes. Nursing Outlook. 2010;58(5):242–251. doi: 10.1016/j.outlook.2010.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson DA, Martin PD, White MA, Newton R, Walden H, York-Crowe E, Ryan D. Efficacy of an internet-based behavioral weight loss program for overweight adolescent African-American girls. Eating and Weight Disorders. 2005;10(3):193–203. doi: 10.1007/BF03327547. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Mauras N, White NH. Randomized trial of behavioral family systems therapy for diabetes: Maintenance of effects on diabetes outcomes in adolescents. Diabetes Care. 2007;30(3):555–560. doi: 10.2337/dc06-1613. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Taylor A, White NH. Randomized, controlled trial of behavioral family systems therapy for diabetes: Maintenance and generalization of effects on parent-adolescent communication. Behavior Therapy. 2008;39(1):33–46. doi: 10.1016/j.beth.2007.04.001. [DOI] [PubMed] [Google Scholar]