Abstract
Significance
The process of wound healing includes the regulated destruction of proteins via enzymes called proteinases. However, when the proteolytic process becomes excessive, pro-healing factors are destroyed and the wound healing process stalls. Matrix metalloproteinases (MMPs) are one key class of proteinases that have been observed to be elevated in many cases of failed wound healing.
Recent Advances
Two key advances have been made in recent years. First is that, until recently, MMPs were only implicated in impaired healing of chronic wounds. Measurements of MMPs in wound fluids and serum from individuals with acute traumatic wounds have revealed that elevated MMPs are predictive of both impaired healing and of dehiscence of surgically closed wounds. The second advance is in the development of at least three clinically viable methods for measuring MMPs at the point of care.
Critical Issues
At present there is no objective method of determining proteinase levels within a wound. Since elevated MMPs have now been shown to be predictive of dehiscence in surgically closed acute wounds, a new clinical utility for measuring MMPs has been established. With the advent of several new technologies to measure MMPs, the translation of this valuable molecular knowledge into improved therapeutic regimens is nearly complete.
Future Directions
The clinical utility of measuring MMPs continues to expand and be further validated with each new investigation. The tools that will enable clinicians to leverage this valuable information are nearing maturity and integration into the clinic.

Daniel J. Gibson, PhD
Scope
Over the last decade, the understanding of the molecular causes of failed healing has dramatically improved. Across many different studies of a variety of wound etiologies, one consistent fact continues to emerge: excessive proteinase activities impair wound healing.1–7 Initially, elevated levels of proteinase activity were linked to reduced healing rates of chronic wounds, but recent research has revealed that excessive proteinases in acute wound fluids and patient serum also correlate with impaired healing and wound dehiscence of surgically closed traumatic acute wounds.1 In both cases, excessive proteinases are responsible for destroying endogenous pro-healing growth factors, co-factors, receptors, and the underlying extracellular matrix.8,9 While effective pro-healing biological therapies, such as recombinant growth factors, acellular matrices, and grafts, have been shown to effectively aid in wound closure, they too can be destroyed by excessive proteinases in the wound. Thus, consistent success in closing wounds appears to hinge on clinicians having timely knowledge of the levels of proteolytic activities in the wound. A solution to this critical clinical need would be a rapid, point-of-care, molecular indicator that would provide clinicians with an indication of the proteolytic activity level within a wound. With this information in hand, the clinician can make an informed decision about whether a wound is ready for surgical closure or an advanced biological therapeutic, or whether the wound bed requires additional preparation or proteinase modulating therapy. Ultimately, such a technology is expected to aid in more consistent and rapid closure of wounds in an economically feasible manner.
Target Articles.
1. Utz ER, Elster EA, Tadaki DK, Gage F, Perdue PW, Forsberg JA, et al.: Metalloproteinase expression is associated with traumatic wound failure. J Surg Res 2010; 159: 633.
2. Gibson D, Cullen B, Legerstee R, Harding KG, and Schultz G: MMP's made easy. Wounds Int 2009; 1.
3. Gibson DJ and Schultz G: Chronic wound diagnostic for matrix metalloproteinase. Wound Heal South Afr 2009; 2: 68.
Translational Relevance
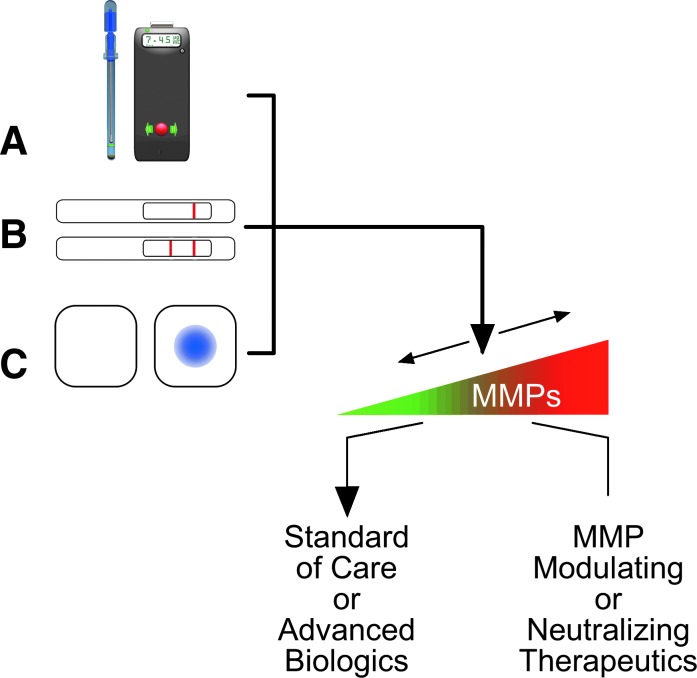
As shown in Fig. 1, matrix metalloproteinases (MMPs) play key roles in at least five essential processes of wound healing. MMPs released by inflammatory cells during the first few days after skin injury provide the initial debridement of extracellular matrix proteins and tissues that were damaged and denatured during the injury. MMPs secreted by vascular endothelial cells in response to angiogenic growth factors like vascular endothelial growth factor “erode holes” in the basement membrane of arterioles, through which new capillary endothelial cells migrate into the ischemic wound bed, generating granulation tissue. Myofibroblasts secrete MMPs that aid in the contraction of new scar tissue, and epithelial cells use MMPs to migrate under the eschar/scab and over the surface of the new wound bed. Finally, fibroblasts secrete MMPs to help remove portions of the initial, irregular scar matrix during the remodeling phase of healing. Thus, MMPs play essential roles in normal healing of skin wounds when they are secreted in the right amounts, at the right times, and in the right places. However, when proteinases like MMPs or neutrophil elastase remain elevated at levels 50 to 100 times what are needed to perform their beneficial functions in normal healing, they begin to degrade proteins that are not their normal substrates, such as growth factors, receptors, and extracellular matrix proteins that are essential for healing.9–11 Destruction of these “off-target” proteins impairs healing and leads to dehiscence of acute wounds and eventually to chronic wounds.
Figure 1.
Excessive proteinase activity impairs wound healing by various mechanisms. Matrix metalloproteinases (MMPs) are required for normal healing. However, if the proteolytic activity levels are too high, then the MMPs can destroy growth factors, co-factors, and cell-surface receptors. Without growth factors, receptors, or a stable extracellular matrix, cells cannot respond to normal growth and repair signals. Also, the wound bed gets further eroded, which prevents cellular adhesion and migration, both of which can lead to an increase in total wound volume. The net clinical effect is that acute wounds with high MMPs can dehisce and chronic wounds remain unhealed.
Clinical Relevance
There is abundant evidence that proteinases are necessary for normal healing, but that elevated levels of proteinases, especially MMPs, correlate with impaired healing. This knowledge has given rise to advanced therapeutics that inhibit or diminish the effects of MMPs and that have been demonstrated to subsequently improve healing.12 The excessive MMP activities have also been implicated in the inconsistent response of wounds to advanced biological therapies or to grafting.12 However, there are no assays a clinician can use to assess the levels of MMPs in wounds, leaving the clinician to make an educated guess as to when to use a proteinase modulating dressing, or when to apply a biological therapy. Work has been ongoing to develop and get rapid point-of-care assays into the clinic that would address this current shortcoming.13–15 More recently, MMPs have been implicated in a separate, but related clinical problem: the timing of when to surgically close an acute traumatic wound.1 At present, the inability to assess the MMP levels within wounds leads to increased costs and risks across the board. Time, effort, and money are wasted when a proteinase-modulating therapy is not employed when it should have been, when an advanced biologic therapy or an autograft is placed on an MMP-rich wound and subsequently destroyed, or when an MMP-rich acute trauma wound is surgically closed only to dehisce shortly thereafter. Finally, in addition to the economic losses, the increased time in clinic with an open wound increases the patient's risk for acquiring a severe infection. The target articles identified here address differing aspects of the clinical problem caused by excessive MMPs in wounds and what is being done to aid clinicians in solving the problem.
Experimental Model or Material: Advantages and Limitations
To date, patient-derived wound fluid, biopsies, and serum have been the experimental material used to study MMPs in wound healing. The choice of using these materials has ensured absolute clinical relevance of any eventual findings. What has been varied are the molecular measurement techniques that are employed. By far, the most popular techniques measure the amount of a given MMP present using a form of immunoassay. The strength of these assays lies in the highly accurate identification of precisely the proteins of interest. However, MMPs exist in wound as inactive pro-enzymes, as inhibited protein complexes, and as active enzymes. The immunoassays cannot distinguish between the active and inactive forms of MMPs. The other class of assays tends to measure enzyme activity, but the enzymatic assays are usually not as specific in that they can measure several different enzymes with similar activities. The lack of precise molecular accuracy in the enzymatic assays is not considered a shortcoming in a clinical setting, with the rationale being that if the assay molecule is being destroyed, so are the pro-healing factors in the wound. At present, most efforts on developing detectors for use in wound care are focused on devices that measure proteinase enzyme activities rather than immunologically detecting proteinase proteins.
Discussion of Findings and Relevant Literature
When considered in the most generic sense, the role of wound healing is to replace tissue that is lost during the injury with an organized mass of protein (i.e., extracellular matrix and cells). A failure in filling this void can occur due to a lack of protein synthesis, or due to excess protein destruction. Evidence for the latter was found when nonhealing wounds were found to be devoid of intact fibronectin, whereas healing wounds, or wounds that recover from being stalled, have abundant intact fibronectin.16 The culprit behind the destruction of fibronectin was found to be neutrophil-derived elastase (also known as human neutrophil elastase), and that the degraded fibronectin in turn stimulated the synthesis and release of MMPs.15,17,18 The relationship between elevated levels of these MMPs and the impairment of wound healing in chronic wounds has since been established and has been repeatedly observed.2–4 However, it is not ethically possible to directly test the hypothesis that chronically elevated MMPs are the central mechanism that causes wounds to fail to heal in patients by adding proteinases to acute wounds. Nevertheless, results of clinical studies that assessed the effects of therapies that reduce proteinase synthesis and/or activities have provided strong evidence that if the excessive proteolytic activities are reduced, then wounds can be steered toward a healing trajectory.12
Most of the investigations of MMPs and failed healing have been conducted with nonclinically infected chronic wounds. However, more recent investigations have been conducted with wound fluids and serum from soldiers with combat-derived acute trauma wounds. In this study, MMPs were found to be elevated in both the serum and wound fluids of patients prior to a wound becoming impaired (i.e., taking more than 21 days to heal) and prior to dehiscence of a surgically closed wound.1 These new data provided two new interesting insights and indicate a novel clinical utility of measuring MMPs. First, these data now provide direct evidence that elevated levels of MMPs in acute wounds lead to wound failure and wound chronicity. The investigators found that MMP levels were significantly elevated in wounds that started as acute wounds, and then began to regress toward chronicity. Second, these data indicated that the MMPs were elevated not only in the wound fluids, but also in serum, indicating that there is an accompanying systemic response in addition to the localized inflammation within the wound. The elevation of MMPs in serum may lay the groundwork for yet another approach to monitoring patients whose wounds are on a trajectory for failure. The data derived in this recent investigation also suggest that measuring MMPs in patients with acute traumatic wounds has clinical utility in that the MMPs provide a means of judging the appropriate timing of surgical closure of these wounds. In summation, with each new investigation, the hypothesis that elevated MMP activities contribute to failed healing in a variety of wound etiologies continues to be validated.
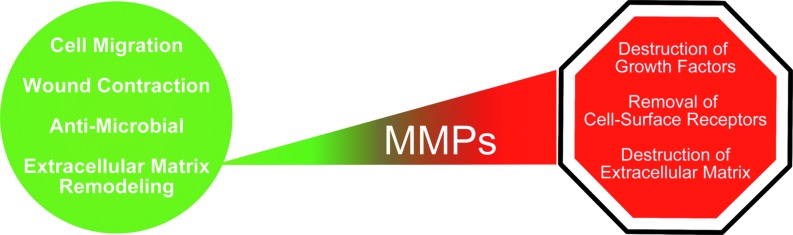
To bridge the gap between basic science findings and clinical utility, several devices that can measure MMP activities in wounds have begun to be developed and tried in clinical settings.13–15 The approaches taken by these different groups vary, but share one element in common: they all measure the proteolytic activity of the sampled wound fluid. Examples of these devices and their anticipated use are conceptualized in Fig. 2. In Fig. 2A, a mix-and-read approach is used. Wound fluids are absorbed by a swab, exposed to a detection reagent, and then quantified with a small handheld reader. Figure 2B depicts the common lateral flow strip assay that has been modified for use in measuring proteolytic activity in wound fluids that have been applied to the strip. Finally, Fig. 2C varies the greatest in that it has a detector that is built into a bandage that qualitatively reports the proteolytic activity in the interval between clinical observations. In their currently envisioned uses, two of the devices provide a measurement of the state of the wound at presentation (Fig. 2A, B), while the other provides an integrated measurement of how the proteinases varied over a time period (Fig. 2C). The outputs of the devices are expected to provide similar clinical guidance in steering decisions toward MMP modulation when necessary and away from surgical closure or advanced biologics prior to the wound being ready for them.
Figure 2.
Several methods for measuring MMPs in wounds are emerging. (A) An example of a mix-and-read fluorescent assay with a handheld meter for quantification. (B) An example of a lateral flow strip-based assay. (C) An example of a bandage that changes color. In general, these devices will apprise the clinician of the level of MMP activity in a patient's wound and which course of action is the most appropriate.
Innovation
At present it is generally accepted that excessive proteinases can impair wound healing, but there are no objective tests that clinicians can perform to assess levels of proteases in wounds. With the development of the novel devices for measuring proteinases at the point of care, wound care professionals could rapidly assess whether a particular wound is on course for healing, whether the wound would benefit from proteinase modulation, whether the wound would be receptive to advanced biologic therapeutics, or whether the wound is ready for surgical closure. With this molecular knowledge in hand, clinicians can be more pro-active in their treatment decisions. As the use of molecular indicators becomes integrated into normal wound treatment practice, the time from development to clinical integration of new devices will be expedited. We anticipate that the devices that can provide insight into the levels of pro-healing factors would enable custom treatment regimens that supplement a particular wound with whatever its deficiencies happen to be. We also anticipate that improved molecular insight into difficult-to-heal wounds will enable more etiology-centric treatment regimens, which should lead to more rapid and stable wound closure and restoration of tissue function.
Caution, Critical Remarks, and Recommendations
The evidence to date suggests that elevated MMPs are a molecular mechanism for failed wound healing, but as stated earlier, appropriate low levels of these enzymes are necessary for healing. Therapies targeted at totally eliminating MMP activity altogether should not be pursued. Additionally, while MMPs are the apparent mechanism, there are other underlying problems that initially give rise to the excessive proteinase levels. Accordingly, a treatment regimen consisting solely of proteinase reduction would not be expected to be sufficient. Instead, MMP modulation should be considered an additional component in an overall wound-healing strategy. Finally, when molecular indicators are adopted into clinical practice, these devices should inform, not supplant, a clinician's judgment. At best, the molecular indicators provide a small but important piece of the overall puzzle that still must be assembled into an actionable diagnosis by the attending clinician.
Future Development of Interest
The current advance has identified MMPs as one of several factors that actively impair wound healing. Anticipated future developments include two distinct paths: (1) gaining insight into the underlying causes of elevated proteinases, including the presence of bacterial biofilms and/or patient metabolic disorders, and (2) gaining insight into what molecular deficiencies co-exist within the wound that could be a target for correction. To this end, basic science research is being conducted to elucidate novel molecules in the wound with clinical relevance and the development of novel measurement platforms that will enable simultaneous measurement of multiple biomarkers at the point of care. Success in these endeavors is expected to usher in a new era in molecularly-guided, personalized therapies to greatly expedite healing of acute and chronic wounds.
Take-Home Message.
Basic science advances
Excessive MMP activity leads to the destruction of growth factors, cell-surface receptors, and extracellular matrix. Customized adaptations of lab-based molecular assays have been developed for use at the point of care. The leading assays use similar methods that effectively measure the protein-destroying potential of the wound fluid. The basic idea is that if the measurement molecule is being destroyed, so are the critical components of the wounds.
Clinical science advances
The concerted destruction of proteins that are essential for healing has been identified as a mechanism that causes delayed or failed wound healing. Elevated MMP levels and activities have been found to be correlated with the persistence of chronic wounds and in acute wounds prior to dehiscence. These advances in clinical science have demonstrated the predictive value of MMP levels and provided a pathway to identify wounds on a nonhealing trajectory prior to patients presenting with stalled or dehisced wounds.
Relevance to clinical care
The basic science that gave rise to these novel assays will now enable the advances in clinical science to be translated into clinical utility. With these novel assays, clinicians will soon be able to have predictive insight about the state of the wound. It is anticipated that these devices will guide clinical judgments about when/if to use proteinase modulating dressings and when/if to use advanced biological therapies; both of which are expected to lead to more rapid and stable healing and reduced expenditures in the form of misused advanced therapies and reduced patient time in clinic.
Abbreviations and Acronyms
- MMP
matrix metalloproteinase
Acknowledgments and Funding Sources
NIH Grant EY05587 and NIH Grant U54 NS058185.
Author Disclosure and Ghostwriting
Inventor of an MMP-measuring device: D.J.G. and G.S.S.
Ownership in company developing/marketing device: D.J.G. and G.S.S.
No ghostwriters were used.
References
- 1.Utz ER. Elster EA. Tadaki DK. Gage F. Perdue PW. Forsberg JA, et al. Metalloproteinase expression is associated with traumatic wound failure. J Surg Res. 2010;159:633. doi: 10.1016/j.jss.2009.08.021. [DOI] [PubMed] [Google Scholar]
- 2.Ladwig GP. Robson MC. Liu R. Kuhn MA. Muir DF. Schultz GS. Ratios of activated matrix metalloproteinase-9 to tissue inhibitor of matrix metalloproteinase-1 in wound fluids are inversely correlated with healing of pressure ulcers. Wound Repair Regen. 2002;10:26. doi: 10.1046/j.1524-475x.2002.10903.x. [DOI] [PubMed] [Google Scholar]
- 3.Rayment EA. Upton Z. Shooter GK. Increased matrix metalloproteinase-9 (MMP-9) activity observed in chronic wound fluid is related to the clinical severity of the ulcer. Br J Dermatol. 2008;158:951. doi: 10.1111/j.1365-2133.2008.08462.x. [DOI] [PubMed] [Google Scholar]
- 4.Liu Y. Min D. Bolton T. Nube V. Twigg SM. Yue DK, et al. Increased matrix metalloproteinase-9 predicts poor wound healing in diabetic foot ulcers. Diabetes Care. 2009;32:117. doi: 10.2337/dc08-0763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yager DR. Nwomeh BC. The proteolytic environment of chronic wounds. Wound Repair Regen. 1999;7:433. doi: 10.1046/j.1524-475x.1999.00433.x. [DOI] [PubMed] [Google Scholar]
- 6.Yager DR. Zhang LY. Liang HX. Diegelmann RF. Cohen IK. Wound fluids from human pressure ulcers contain elevated matrix metalloproteinase levels and activity compared to surgical wound fluids. J Invest Dermatol. 1996;107:743. doi: 10.1111/1523-1747.ep12365637. [DOI] [PubMed] [Google Scholar]
- 7.Tarnuzzer RW. Schultz GS. Biochemical analysis of acute and chronic wound environments. Wound Repair Regen. 1996;4:321. doi: 10.1046/j.1524-475X.1996.40307.x. [DOI] [PubMed] [Google Scholar]
- 8.Mast BA. Schultz GS. Interactions of cytokines, growth factors, and proteases in acute and chronic wounds. Wound Repair Regen. 1996;4:411. doi: 10.1046/j.1524-475X.1996.40404.x. [DOI] [PubMed] [Google Scholar]
- 9.Chen SM. Ward SI. Olutoye OO. Diegelmann RF. Kelman Cohen I. Ability of chronic wound fluids to degrade peptide growth factors is associated with increased levels of elastase activity and diminished levels of proteinase inhibitors. Wound Repair Regen. 1997;5:23. doi: 10.1046/j.1524-475X.1997.50108.x. [DOI] [PubMed] [Google Scholar]
- 10.Cowin AJ. Hatzirodos N. Holding CA. Dunaiski V. Harries RH. Rayner TE, et al. Effect of healing on the expression of transforming growth factor beta(s) and their receptors in chronic venous leg ulcers. J Invest Dermatol. 2001;117:1282. doi: 10.1046/j.0022-202x.2001.01501.x. [DOI] [PubMed] [Google Scholar]
- 11.Grinnell F. Zhu M. Identification of neutrophil elastase as the proteinase in burn wound fluid responsible for degradation of fibronectin. J Invest Dermatol. 1994;103:155. doi: 10.1111/1523-1747.ep12392625. [DOI] [PubMed] [Google Scholar]
- 12.Gibson D. Cullen B. Legerstee R. Harding KG. Schultz G. MMP's made easy. Wounds Int. 2009;1 [Google Scholar]
- 13.Gibson DJ. Schultz G. Chronic wound diagnostic for matrix metalloproteinase. Wound Heal South Afr. 2009;2:68. [Google Scholar]
- 14.Davis MJ. Davis PJ. Burnapp M. Protease detection product. U.S. Patent Application 20090203059. Aug 13, 2009. http://appft1.uspto.gov/netacgi/nph-Parser?Sect1=PTO1&Sect2=HITOFF&d=PG01&p=1&u=/netahtml/PTO/srchnum.html&r=1&f=G&l=50&s1=20090203059 http://appft1.uspto.gov/netacgi/nph-Parser?Sect1=PTO1&Sect2=HITOFF&d=PG01&p=1&u=/netahtml/PTO/srchnum.html&r=1&f=G&l=50&s1=20090203059
- 15.Sanders MC. Lowe AM. Hamilton MA. Colpas GJ. Method for detecting microorganisms. U.S. Patent Cooperation Treaty PCT/US2003/003172. Jan 31, 2003. www.wipo.int/patentscope/search/en/WO2003063693 www.wipo.int/patentscope/search/en/WO2003063693
- 16.Herrick SE. Sloan P. McGurk M. Freak L. McCollum CN. Ferguson MW. Sequential changes in histologic pattern and extracellular matrix deposition during the healing of chronic venous ulcers. Am J Pathol. 1992;141:1085. [PMC free article] [PubMed] [Google Scholar]
- 17.Grinnell F. Ho CH. Wysocki A. Degradation of fibronectin and vitronectin in chronic wound fluid: analysis by cell blotting, immunoblotting, and cell adhesion assays. J Invest Dermatol. 1992;98:410. doi: 10.1111/1523-1747.ep12499839. [DOI] [PubMed] [Google Scholar]
- 18.Grinnell F. Zhu M. Fibronectin degradation in chronic wounds depends on the relative levels of elastase, alpha1-proteinase inhibitor, and alpha2-macroglobulin. J Invest Dermatol. 1996;106:335. doi: 10.1111/1523-1747.ep12342990. [DOI] [PubMed] [Google Scholar]