Abstract
Objectives
To understand how community pharmacists use electronic prescribing (e-prescribing) technology; and to describe the workflow challenges pharmacy personnel encounter as a result of using e-prescribing technology.
Design
Cross-sectional qualitative study.
Setting
Seven community pharmacies in Wisconsin from December 2010 to March 2011
Participants
16 pharmacists and 14 pharmacy technicians (in three chain and four independent pharmacies).
Interventions
Think-aloud protocol and pharmacy group interviews.
Main outcome measures
Pharmacy staff description of their use of e-prescribing technology and challenges encountered in their daily workflow related to this technology.
Results
Two contributing factors were perceived to influence e-prescribing workflow: issues stemming from prescribing or transmitting software, and issues from within the pharmacy. Pharmacies experienced both delays in receiving, and inaccurate e-prescriptions from physician offices. Receiving an overwhelming number of e-prescriptions with inaccurate or unclear information resulted in significant time delays for patients as pharmacists contacted physicians to clarify wrong information. In addition, pharmacy personnel reported that lack of formal training and the disconnect between the way pharmacists verify accuracy and conduct drug utilization review and the presentation of e-prescription information on the computer screen significantly influenced the speed of processing an e-prescription.
Conclusion
E-prescriptions processing can hinder pharmacy workflow. As the number of e-prescriptions transmitted to pharmacies increases due to legislative mandates; it is essential that the technology that supports e-prescriptions (both on the prescriber and pharmacy operating systems) be redesigned to facilitate pharmacy workflow processes and to prevent unintended consequences, such as increased medication errors, user frustration, and stress.
Keywords: E-prescribing, electronic prescribing, community pharmacy, workflow
Introduction
Community pharmacies were forerunners in adopting various types of health information technology (HIT) to improve patient care.1 Electronic prescribing (e-prescribing) is one form of HIT that is increasingly being used in pharmacies.2 E-prescribing is defined as the direct computer-to-computer transmission of electronic prescriptions (e-prescriptions) from prescriber offices to community pharmacies.3 E-prescribing is being used in different clinical settings to reduce medication errors and improve efficiency.4 Consequently the number of e-prescriptions are received in pharmacies is increasing annually.2 In 2011, over 570 million e-prescriptions were received in pharmacies in the US as compared to only 320 million in 2010.2 As the adoption of e-prescribing in the US healthcare system grows, it has become necessary for community pharmacies to rapidly adapt to this change in delivery of healthcare.
Questions have arisen regarding e-prescribing technology’s ability to facilitate or hinder safety and efficiency of dispensing in pharmacies. The use of technology to generate prescriptions also has been reported to result in medication errors such as wrong drug, wrong patient, wrong and drug directions due to inaccurate or omitted information.5 One study reported that one in 10 computer generated prescriptions received in pharmacies had at least one medication error and a third of these errors were potentially harmful.6 Only a few studies have investigated the consequences of receiving e-prescriptions in pharmacies. Results from these studies indicate a growing concern among community pharmacists about the patient safety implications related to new kinds of medication errors and information omissions caused by the use of e-prescribing.5, 7 E-prescribing may be a threat to medication safety related to prescription processing in community pharmacies.5
E-prescribing processing is gradually becoming an integral part of community pharmacy workflow. Pharmacy workflow generally refers to a series of tasks that are performed in order to dispense medications to patients safely and efficiently. Workflow processes and design can significantly affect patient care in community pharmacies. The use of automation in pharmacies has been associated with improved workflow efficiency.8 However, implementation of HIT such as e-prescribing in the healthcare settings has been reported to result in changes and disruptions in normal workflow that may negatively affect patient care.9 Indeed, one study reported that community pharmacists required an average of 6.07 minutes to resolve problematic e-prescription orders5; this suggests that issues arising from e-prescribing use in community pharmacies may slow down pharmacy regular workflow.
Objectives
We sought to understand how community pharmacy personnel use e-prescribing technology and to describe their perspectives regarding workflow challenges encountered when utilizing e-prescribing.
Methods
Sampling and Recruitment of Participants
We selected community pharmacies that met the following inclusion criteria: must be a retail community pharmacy, must process at least 10 e-prescriptions daily, and must initiate the processing of e-prescriptions from the electronic order. These inclusion criteria were developed to ensure recruitment of pharmacies that were familiar with e-prescribing and used the technology as originally intended by designers.
Pharmacies were initially recruited through the Pharmacy Society of Wisconsin (PSW) “Fast Facts” email listserv in December 2010. Fourteen pharmacists and sixteen technicians (at least four workers from each pharmacy) were recruited from participating pharmacies through the pharmacy manager. Written informed consent forms were obtained from all participants and human subjects’ approval for the study was granted by the researchers’ Institutional Review Board.
Data Collection
A qualitative data collection approach was used to provide an in-depth and detailed description of workflow practices when using e-prescribing technology in pharmacies. Data were obtained using two qualitative data collection techniques: think-aloud protocol and pharmacy group interviews. We employed two qualitative data collection methods to ensure validation of information provided by each participant. The combination of these methods provided in-depth information and triangulation on the workflow challenges, mental recall, and information needs of pharmacy personnel when processing e-prescriptions.
Think-aloud protocol (TAP)
TAPs are used by human factors researchers to provide procedural information on tasks. In TAP, participants verbalize their task performance to yield insight into cognitive components of the task. 10–13 This method was used to elucidate the stepwise processing of an e-prescription and to identify pharmacy personnel’s cognitive and information needs when handling e-prescriptions. TAP took place between January and February 2011and involved the primary investigator observing pharmacy staff use e-prescribing and taking field notes. Responses from the TAPs were audio recorded and transcribed. The duration of TAP ranged from two to five hours as two to three pharmacy staff (one pharmacist and one or two technicians) were observed in each pharmacy. Fifteen pharmacy staff took part in this phase of data collection.
Pharmacists and technicians were observed processing at least five consecutive e-prescriptions. Prior to each TAP session, participants were instructed with examples on how to think-aloud each aspect of handling the e-prescription. As an e-prescription was transmitted to the pharmacy, the pharmacist or technician was observed and questioned about their dispensing workflow. With every step in the dispensing process, pharmacy personnel were asked to verbalize what they were doing, their thoughts, what information was needed to fulfill each step, information that needed clarity, and how they would proceed to the next step.
Pharmacy group interviews
Interviewing has been found to be useful in capturing information on user-computer interactions in actual clinical work environments which are chaotic complex, and difficult to simulate in laboratories during usability testing.14 Within-pharmacy group interviews provide insight into things which are not easily observed and can provide perspectives of multiple users of the same organization and dispensing system. Events related to the technology use which do not occur frequently can be readily described by someone who has been using the technology for months or years. Data were collected by interviewing pharmacists and technicians who frequently process e-prescriptions in the pharmacy team with the aim to take advantage of their insight into how e-prescribing is impacting pharmacy workflow. These interviews were scheduled two weeks after the TAPs were conducted.
Seven group interviews were conducted between February and March 2011 to clarify information provided during the think-aloud sessions and to provide additional information on past experiences using this technology. For each pharmacy interview, the pharmacy manager selected four pharmacy personnel (two pharmacists and two technicians) that were interviewed for about one hour. A semi-structured interview guide was used to ask pharmacy personnel about their experiences with e-prescribing and how they perceived e-prescribing impacted their workflow. Prior to commencing the interview, the participants were reassured of the confidentiality of the information obtained. All responses from the seven group interviews were audio recorded and transcribed verbatim for analysis.
Data analysis
The data obtained from the TAPs and the group interviews were subjected to qualitative thematic analysis. Thematic analysis involved identifying themes or patterns within data. Audio tapes of TAPs and interviews were transcribed for analysis. The primary investigator initially reviewed to identify recurrent themes relevant to e-prescribing in all seven community pharmacies. Identified themes and subthemes were vetted and refined by the co-investigator. Verbatim quotes reported during TAPs and interviews are provided in the results section to enable readers to assess the concordance between original data and the researchers’ interpretation. Methodological triangulation was conducted to validate the data provided during the TAPs and interviews. This involved a comparison of the data obtained from the different data collection methods to ensure cross validity between themes identified.
Results
Pharmacy and Participant Characteristics
Nineteen pharmacies responded to the PSW solicitation but fifteen of these pharmacies did not meet the study criteria and were excluded from the study because they initiated the prescription workflow by printing e-prescriptions and handled them as traditional paper prescriptions. Only four pharmacies met the study criteria. Three additional pharmacies were then recruited through a targeted snowball sampling, resulting in seven community pharmacy participants. Table 1 shows the characteristics of pharmacies that participated in this study. In total, seven community pharmacies located in suburban or rural regions in Wisconsin were recruited. Four were independent pharmacies while three were chain pharmacies. A total of 14 pharmacists and 16 technicians participated in the study. However two pharmacy technicians were unable to participate in the pharmacy group interviews, hence only 28 pharmacy personnel participated in the group interviews.
Table 1.
Characteristics of Pharmacies
| Pharmacy | Dispensing system | e-Rx experience (in Years) | Average proportion of daily e-Rx to total Rx volume | Average daily Rx volume | Daily staffing | Practice setting |
|---|---|---|---|---|---|---|
| 1 | PDX™ | 3 | 33% | 175 | 1 RPh 3 Techs |
Chain |
| 2 | PDX™ | 2.5 | 90% | 150 | 1 RPh 4 Techs |
Chain |
| 3 | PDX™ | 5 | 50% | 155 | 1 RPh 1 Tech |
Chain |
| 4 | QS/1™ | 2 | 50% | 360 | 3 RPhs 5 Techs |
Independent |
| 5 | QS/1 NRx™ | 0.5 | 90% | 200 | 1 RPh 2 Techs |
Independent |
| 6 | Pharmaserv™ | 1 | 50% | 325 | 2 RPhs 5 Techs |
Independent |
| 7 | Pharmaserv™ | 2 | 80% | 350 | 1 RPh 4 Techs |
Independent |
e-Rx – e-prescription; e-Rx experience – Number of years of e-prescribing adoption by the pharmacy; Average daily proportion of eRx to total Rx volume – Percentage of Rxs that are received as e-prescriptions in the pharmacy; Daily staffing – Average number of pharmacy staff present in the pharmacy daily.
Themes identified
In conducting thematic analysis, several themes and sub-themes were identified pertaining to e-prescribing use. Issues that arose in the pharmacy workflow due to the use of e-prescribing technology were categorized into two major themes:
-
Workflow challenges stemming from the prescribing or transmission software
Confusing or inaccurate e-prescriptions
Time delays and “bundling” associated with transmission of e-prescriptions
-
Workflow challenges from other factors within the pharmacies.
Lack of formal training on using e-prescribing technology
Impact of e-prescriptions design on pharmacy workflow
A. Challenges stemming from prescribing or transmission software
On observation, the overall workflow of e-prescriptions was similar to conventional prescriptions (paper, telephone, and fax). The major difference in workflow between e-prescriptions and conventional prescriptions was in how prescription information was presented to the pharmacist or technician. Overall participants stated that e-prescriptions marginally increased workflow efficiency, when e-prescriptions were problem free.
1. Time delays and “bundling” associated with transmission of e-prescriptions
Participants stated that it was normal for e-prescriptions to not arrive when the patient thought it would (or was told it would) arrive in the pharmacy. Several unintended consequences arose from the time delay. When there were delays in receiving e-prescriptions from physician offices this resulted in time delays for patients at the pharmacy. Patients could not understand why the e-prescription was delayed when they perceived that it was transmitted in their presence at the physician’s office. Consequently, pharmacy personnel would have to address why they had not received the e-prescription by contacting the physician’s office to remind them to send the e-prescription or ask if the office may have sent the e-prescription to a different pharmacy. In addition, delayed e-prescriptions were sometimes bundled and transmitted at once late in the work day. This led to an overwhelming number of e-prescriptions arriving in the pharmacy at one time. One pharmacy reported receiving 25 or more e-prescriptions within a few minutes for different patients from various prescribers, significantly more than was possible with conventional prescriptions (paper, fax, or phone). The uncontrollable increase in the number of e-prescriptions received at within a brief period created tension in the pharmacy environment as participants struggled to process each prescription rapidly and accurately.
“It happens where we are so backed up that we can’t get to it. And it’s here and patients come in. And we also have where they [patients] are here already and the doctor hasn’t sent it [e-prescriptions].”
The bundling of e-prescriptions created a second workflow concern. Paper, fax, or phone prescriptions are typically bundled together either physically (paper) or temporally (phone, fax) so that pharmacy personnel would know how many distinct prescriptions one patient or one family was receiving. E-prescriptions for the same patient, however, could be electronically transmitted at different times. To compound the issue, controlled substance prescriptions could not be sent electronically and pharmacy personnel were frequently unaware that there may be controlled substance paper prescriptions in addition to the e-prescriptions they needed to fill for the same patient.
If multiple e-prescriptions were transmitted simultaneously for different patients, these prescriptions were sometimes mixed together. It was more difficult for pharmacy personnel to sort through the stack of e-prescriptions to track the bundled e-prescriptions for each patient. A consequence on workflow was wasted time and omission of a prescription.
2. Confusing or inaccurate e-prescriptions
E-prescribing technology was originally conceptualized to improve the accuracy of prescription information sent to pharmacies; this assumption is not always the case. When pharmacies received inaccurate e-prescriptions there was more work in clarifying the intent of the prescriber. One source of inaccurate e-prescriptions was prescribers selecting the wrong patient, drug, or dose, possibly from auto-filled functions on the prescriber’s system. Specifically, the prescription directions (i.e., sig) proved to be the most problematic for pharmacy personnel, as pharmacies frequently received incomplete or duplicated directions in the prescription direction textbox.
Poorly written drug directions sent from prescribers were sometimes misinterpreted in the pharmacy or were written in a format that could not be easily understood by patients. Pharmacy personnel were required to stop their dispensing process and call prescribers to clarify prescription directions. In some cases, participants had seen recurrent problematic e-prescriptions from the same prescriber and made assumptions about the drug directions (i.e., the pharmacy personnel assumed that the prescriber provided an explanation of the medication to the patient). For incomplete or duplicated directions, participants deleted the directions and re-entered new directions in a way that could be easily understood by the pharmacist and patient. The pharmacist did not always clarify with the prescriber when such changes were made.
“Sometimes it might say, take a half tablet and there will be a period and then it will say take two tablets. They will give us two different amounts and we would at that point call.”
“I don’t like the way this sig [drug directions] sounds…The doctor sent it kind of funny… I am going to clean it up a little bit because it came through sort of silly….We rewrote it because we want it to be a little more flowing… make it sound straightforward so the patient is not confused.”
B. Challenges in pharmacy workflow from within the pharmacy
1. Lack of formal training on using e-prescribing technology
Pharmacy workflow was found to be influenced by participants’ lack of knowledge and skill in using available e-prescribing technology. Participants reported that they received little to no training on e-prescribing technology. Participants were expected to “figure it out” as e-prescription technology was implemented in their pharmacies. New employees had limited formal training in part because computer terminals were used to fill prescriptions and none could be dedicated to training. These individuals instead learned on the job as they filled prescriptions. As a result, not all participants knew all of the nuances, special features, quick short cuts and codes that were available in the e-prescribing technology. The speed of processing an e-prescription was reduced if pharmacy personnel did not have a good understanding of how to maneuver challenging aspects of the available e-prescribing technology.
“When it first came out they gave us screen prints that said, ‘When you get the prescription…’ And the screen prints walked us through the steps, but that was all the training we got, a series of screen prints. Then it was just figuring it out as you’re going and realizing that ‘Oh, this is how you do it and this is how to get around this and do it that way.’ There was a lot of on the spot, on the job, trial and error.”
2. Impact of e-prescriptions design on pharmacy workflow
Figure 1 depicts the basic steps processing e-prescriptions in pharmacy workflow that were reported during the TAPs in three different dispensing systems.
Figure 1.
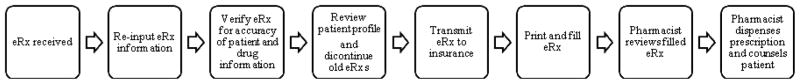
Workflow Map of E-prescribing Processing in Community Pharmacies
When paper, telephone, or faxed prescriptions are presented in the pharmacy, the information on the paper prescription is standardized to include what is legally necessary to dispense a prescription, and formatted similarly so that for instance, the drug strength follows the drug name. The design of the pharmacy computer software and how it presents e-prescriptions information can impact the ease of accessing information and affect the pharmacy workflow. The presentation of e-prescriptions on the computer screen significantly influenced how fast or slow e-prescriptions were processed.
In order to process an e-prescription, participants had to tab through multiple screens to view the e-prescription in order to evaluate its appropriateness. For instance, the physician information may be on a different screen from the prescription medication information. Free text prescriber comments were not always visible or apparent to the individual verifying the prescription. At times, the pharmacist had to tab to a different screen in order to see those comments. Lastly, textboxes for drug names were sometimes too small to view the entire generic drug name, particularly for combination products (i.e., fluticasone/salmeterol). Although participants initiated processing of e-prescriptions directly from the electronic queue, e-prescriptions were still printed to paper some time during the workflow process to double check for accuracy and completeness of information presented on the electronic screen..
“So now on this screen I don’t have the doctor’s name. So if I am possibly hurrying I have already typed in the doctor’s name but what if I may have forgotten it because I typed it so fast. So now I am wondering who is the doctor who prescribed this?”
“It’s kind of awkward because we have to flip through these tabs to see the whole thing”
Discussion
Consistent with studies that have evaluated implementation of new technologies in health care settings15, this study found that the use of new technology such as e-prescribing may not have improved efficiency but could significantly change workflow for users. Pharmacies like other healthcare settings are complex systems in which attention must be paid to interactions between technology and pharmacy personnel, and how use of technological artifacts can affect the practice and the organization in which it becomes embedded.16 There are several reasons why use of e-prescribing could negatively affect pharmacy workflow. First, the advent of e-prescribing technology has led to tighter coupling between prescriber and pharmacy computer software. Pharmacies can now receive large number of prescriptions from prescribers faster than was previously possible with paper prescriptions. Second, the use of e-prescriptions requires pharmacists to adapt to a new approach when processing prescriptions. This is because unlike other types of prescriptions, e-prescriptions were unique in their mode of presentation and transmission. For example, e-prescriptions for one patient could be transmitted to the pharmacy at different times. This is atypical, since traditionally prescriptions for a particular patient are bundled together. In order to improve e-prescribing for pharmacy use, changes should be made to the design of e-prescriptions to be consistent with how pharmacists process other types of prescriptions. Also, pharmacists appear to evaluate all elements of each prescription (such as drug, dosage, and direction) as they view the entire prescription. This holistic approach helps the pharmacist determine the appropriateness of the medication (i.e., is the drug selection and dosage appropriate, or is the dosage form appropriate for a pediatric patient?). However, the piecemeal nature of presenting information on some e-prescribing computer screens requires pharmacy personnel to tab between screens to verify information. E-prescribing technology should have be designed to allow comprehensive assessment of orders during the dispensing process, and present the information in a way that allows pharmacists to optimally and efficiently conduct proper assessment.
Important issues related to e-prescription generation, transmission, and processing influence patient care provided by pharmacists and prescribers. For example, prescribers entering e-prescriptions have to select from drop-down menus, often a source of error17 which might lead to pharmacies receiving inaccurate e-prescriptions. Community pharmacists still have to intervene on e-prescriptions in order to prevent medication errors as they did with handwritten prescriptions.18 Studies have demonstrated that the most common e-prescribing errors requiring pharmacist intervention include excessive drug quantity, drug duration, and inaccurate drug directions.5, 18
E-prescribing issues in community pharmacies need to be recognized, reported and addressed. The identified deficiencies in the design and utilization of the pharmacy computer software used to process e-prescriptions reported in this study can help trigger future improvements in the design of this evolving technology. Although, not all issues reported are unique to e-prescriptions, the use of this technology has made such problems encountered in pharmacies more apparent and perhaps increased frequency of these incidents. One study has taken an important step in identifying best practice recommendations that can be implemented to improve e-prescribing in pharmacies.7 For example, physicians can carefully review e-prescriptions before transmitting to pharmacies to remove inaccurate or conflicting information, physicians can also bundle all e-prescriptions for a particular patient, and pharmacy organizations can improve pharmacy personnel training related to use of e-prescribing technology. These recommendations may help address some of e-prescribing issues reported in this study.
In addition, the recently published toolset by the Agency for Healthcare Research and Quality (AHRQ) for e-prescribing in pharmacies provides some useful tools which may improve e-prescribing in community pharmacies.19 One of the tools includes a patient flyer that information that provides patients with a realistic expectation of time needed by pharmacy personnel to processes e-prescriptions and the possibility of time delays that may occur due to transmission issues between the physician office and the pharmacy. The AHRQ report also provides a simplified diagram of pharmacy workflow when processing prescriptions which can be used in combination with the workflow map presented in this study to identify where and how to implement interventions to improve e-prescribing in community pharmacies.
Finally, training on how to use e-prescribing appears to be an important element that influences community pharmacy workflow. Pharmacy personnel in this study reported receiving little or no formal training on how to use e-prescribing. Unlike other healthcare settings where formalized training is seen as an essential component of HIT implementation, it appears that participating pharmacies in this study are yet to fully recognize and capitalize on the benefits of providing adequate training in order to improve workflow efficiency. Administrators and owners of community pharmacies should require HIT program developers or pharmacy software vendors to provide comprehensive e-prescribing training pre-implementation and assess pharmacy personnel understanding of the technology post-implementation. Pharmacies could also designate one pharmacist that has been trained by the software vendors as the “e-prescribing expert” that can be responsible for facilitating appropriate training for new employees post-implementation.
Limitations
A primary limitation of using quantitative data collection methods such as surveys is that they reflect only perceptions of users of the technology. We employed two qualitative data collection methods to ensure validation of information provided by participants, including TAP to capture processes in naturalistic and context-specific settings. The combination of these methods provided in-depth information on the workflow challenges of pharmacy personnel when processing e-prescriptions and reduced potential bias of using one data collection method. Triangulation was done to reduce potential bias in data obtained from one method. This involved an analysis and comparison of data obtained from each data collection method to develop information described in each theme identified to ensure cross validity of identified themes.
First, although 19 pharmacies indicated interest to participate in this study, 15 pharmacies had to be excluded because they did not utilize the computerized process to handle e-prescriptions as received from the electronic queue. In addition only pharmacy personnel from one state participated in this study. Hence, the findings may not be generalizable to all pharmacies. Second, the researchers chose to focus on only e-prescriptions and did not examine workflow processes related to other types of prescriptions received in the pharmacies such as paper or faxed prescriptions. Hence, the results should be interpreted with the context of the noted study limitations.
Conclusion
The implementation of technology in healthcare should facilitate efficient and high quality health care. Our findings suggest that there are problems with e-prescribing technology in pharmacies and possibly with the software used for prescribing and transmitting e-prescriptions to community pharmacies. Community pharmacy work is interruptive, reactive and involves multitasking. Hence, HIT such as e-prescribing should mitigate, not compound, these disruptive characteristics. However, our findings show that the implementation of e-prescriptions interrupted pharmacy workflow.
Since the number of e-prescriptions transmitted to community pharmacies will continue to increase due to recent federal government regulations mandating its use; it is essential that e-prescriptions issues and their impact on workflow in the community pharmacy setting continue to be studied. The implications of this study voiced by pharmacy staff who have been actively using e-prescribing are important for pharmacy practice and need to be disseminated to others in the profession to enhance knowledge sharing and learning. Further studies can provide evidence of ways to design e-prescriptions (both on the prescriber and pharmacy operating systems) to facilitate pharmacy workflow processes since problems in workflow may lead to an unintended increase in medication errors, user frustration, and stress.
Acknowledgments
Funding Support: The study was funded by a grant from the Community Pharmacy Foundation and by the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH;
Footnotes
Potential Conflicts of Interest Disclosure: The authors declare no conflicts of interest or financial interests in any product or service mentioned in this article, including grants, employment, gifts, stock holdings, or honoraria;
Previous presentation: Presented previously at the American Pharmacists Association Annual Meeting, New Orleans, LA, March 11, 2012;
Contributor Information
Olufunmilola K. Odukoya, School of Pharmacy, University of Wisconsin, Madison.
Michelle A. Chui, School of Pharmacy, University of Wisconsin, Madison.
References
- 1.Siska MH, Tribble DA. Opportunities and challenges related to technology in supporting optimal pharmacy practice models in hospitals and health systems. Am J Health Syst Pharm. 2011;68(12):1116–1126. doi: 10.2146/ajhp110059. [DOI] [PubMed] [Google Scholar]
- 2.Surescripts. [09/29, February 24, 2012];The national progress report on E-prescribing and interoperable healthcare. Accessed at www.surescripts.com/about-e-prescribing/progress-reports/national-progress-reports.aspx.
- 3.Lapane KL, Waring ME, Schneider KL, Dube C, Quilliam BJ. A mixed method study of the merits of e-prescribing drug alerts in primary care. J Gen Intern Med. 2008;23(4):442–446. doi: 10.1007/s11606-008-0505-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ammenwerth E, Schnell-Inderst P, Machan C, Siebert U. The effect of electronic prescribing on medication errors and adverse drug events: A systematic review. J Am Med Inform Assoc. 2008;15(5):585–600. doi: 10.1197/jamia.M2667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warholak TL, Rupp MT. Analysis of community chain pharmacists’ interventions on electronic prescriptions. J Am Pharm Assoc (2003) 2009;49(1):59–64. doi: 10.1331/JAPhA.2009.08013. [DOI] [PubMed] [Google Scholar]
- 6.Nanji KC, Rothschild JM, Salzberg C, et al. Errors associated with outpatient computerized prescribing systems. J Am Med Inform Assoc. 2011 doi: 10.1136/amiajnl-2011-000205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rupp MT, Warholak TL. Evaluation of e-prescribing in chain community pharmacy: Best-practice recommendations. J Am Pharm Assoc (2003) 2008;48(3):364–370. doi: 10.1331/JAPhA.2008.07031. [DOI] [PubMed] [Google Scholar]
- 8.Angelo LB, Christensen DB, Ferreri SP. Impact of community pharmacy automation on workflow, workload, and patient interaction. Journal of the American Pharmacists Association. 2005;45(2):138–144. doi: 10.1331/1544345053623537. [DOI] [PubMed] [Google Scholar]
- 9.Campbell EM, Guappone KP, Sittig DF, Dykstra RH, Ash JS. Computerized provider order entry adoption: Implications for clinical workflow. J Gen Intern Med. 2009;24(1):21–26. doi: 10.1007/s11606-008-0857-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khajouei R, Hasman A, Jaspers MW. Determination of the effectiveness of two methods for usability evaluation using a CPOE medication ordering system. Int J Med Inform. 2011;80(5):341–350. doi: 10.1016/j.ijmedinf.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Fairbanks RJ, Caplan SH, Bishop PA, Marks AM, Shah MN. Usability study of two common defibrillators reveals hazards. Ann Emerg Med. 2007;50(4):424–432. doi: 10.1016/j.annemergmed.2007.03.029. [DOI] [PubMed] [Google Scholar]
- 12.Wu RC, Orr MS, Chignell M, Straus SE. Usability of a mobile electronic medical record prototype: A verbal protocol analysis. Inform Health Soc Care. 2008;33(2):139–149. doi: 10.1080/17538150802127223. [DOI] [PubMed] [Google Scholar]
- 13.Lundgren-Laine H, Salantera S. Think-aloud technique and protocol analysis in clinical decision-making research. Qual Health Res. 2010;20(4):565–575. doi: 10.1177/1049732309354278. [DOI] [PubMed] [Google Scholar]
- 14.Holden RJ. Cognitive performance-altering effects of electronic medical records: An application of the human factors paradigm for patient safety. Cogn Technol Work. 2011;13(1):11–29. doi: 10.1007/s10111-010-0141-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ash JS, Bates DW. Factors and forces affecting EHR system adoption: Report of a 2004 ACMI discussion. J Am Med Inform Assoc. 2005;12(1):8–12. doi: 10.1197/jamia.M1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wears RL, Berg M. Computer technology and clinical work: Still waiting for godot. JAMA. 2005;293(10):1261–1263. doi: 10.1001/jama.293.10.1261. [DOI] [PubMed] [Google Scholar]
- 17.Magrabi F, Ong MS, Runciman W, Coiera E. Using FDA reports to inform a classification for health information technology safety problems. J Am Med Inform Assoc. 2012;19(1):45–53. doi: 10.1136/amiajnl-2011-000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gilligan AM, Miller K, Mohney A, Montenegro C, Schwarz J, Warholak TL. Analysis of pharmacists’ interventions on electronic versus traditional prescriptions in 2 community pharmacies. Res in Soc & Admin Pharm. 2012 doi: 10.1016/j.sapharm.2011.12.005. in press. [DOI] [PubMed] [Google Scholar]
- 19.Agency for Healthcare Research and Quality. [June 29, 2012];Toolset for E-Prescribing Implementation in Independent Pharmacies. Accessed at http://healthit.ahrq.gov/portal/server.pt/community/health_it_tools_and_resources/919/a_toolset_for_e-prescribing_implementation_in_independent_pharmacies/30595.


