Abstract
There are no vaccines or therapeutics currently approved for the prevention or treatment of ebolavirus infection. Previously, a replicon vaccine based on Venezuelan equine encephalitis virus (VEEV) demonstrated protective efficacy against Marburg virus in nonhuman primates. Here, we report the protective efficacy of Sudan virus (SUDV)- and Ebola virus (EBOV)-specific VEEV replicon particle (VRP) vaccines in nonhuman primates. VRP vaccines were developed to express the glycoprotein (GP) of either SUDV or EBOV. A single intramuscular vaccination of cynomolgus macaques with VRP expressing SUDV GP provided complete protection against intramuscular challenge with SUDV. Vaccination against SUDV and subsequent survival of SUDV challenge did not fully protect cynomolgus macaques against intramuscular EBOV back-challenge. However, a single simultaneous intramuscular vaccination with VRP expressing SUDV GP combined with VRP expressing EBOV GP did provide complete protection against intramuscular challenge with either SUDV or EBOV in cynomolgus macaques. Finally, intramuscular vaccination with VRP expressing SUDV GP completely protected cynomolgus macaques when challenged with aerosolized SUDV, although complete protection against aerosol challenge required two vaccinations with this vaccine.
INTRODUCTION
Ebolaviruses and marburgviruses, members of the family Filoviridae, cause sporadic viral hemorrhagic fever outbreaks that primarily affect areas of equatorial Africa (1). Two marburgviruses, Marburg virus (MARV) and Ravn virus (RAVV), and five ebolaviruses, Bundibugyo virus (BDBV), Reston virus (RESTV), Sudan virus (SUDV), Tai Forest virus (TAFV), and Ebola virus (EBOV), are currently recognized. (2). The filovirus genome consists of a nonsegmented, single-strand negative-sense RNA molecule 19 kb in length encoding the following genes: 3′-NP-VP35-VP40-GP-VP30-VP24-L-5′ (3). These enveloped viruses have filamentous morphology with a uniform diameter of 80 nm and highly variable lengths. Primates represent accidental hosts for filoviruses with devastating consequences since fatality rates associated with infection can be as high as 90% in humans (4). African fruit bats are the presumptive natural reservoir host for filoviruses (5–8), although the mechanism by which these viruses make the jump from their reservoir host into human and nonhuman primate (NHP) populations is not well understood (9). Once introduced into primate populations, filovirus transmission occurs primarily through contact with bodily fluids, although recent evidence suggests that other modes of transmission may exist, including aerosol (10, 11). Experimental evidence has clearly demonstrated the ease with which nonhuman primates can be infected with filoviruses by the aerosol route under controlled laboratory conditions (12, 13). Aerosol transmission is of particular importance for biodefense since this represents the most likely means of dissemination (14). Accordingly, filovirus vaccine development efforts will likely need to focus on providing protection against aerosol exposure, in addition to other routes of infection.
EBOV and SUDV are responsible for the largest number of human ebolavirus infection cases to date and represent the chief ebolaviruses for which vaccines are currently being developed. Several efficacious ebolavirus vaccines developed over the last decade have demonstrated that a single ebolavirus antigen, glycoprotein (GP), is sufficient to provide protection against homologous challenge (15). GP, the sole surface viral protein, is responsible for mediating cell attachment and viral entry and is the primary target of humoral immunity (16, 17). Due to the limited amino acid homology of GP across ebolaviruses (55 to 60% homologous) (3), vaccines employing GP from a single ebolavirus have yet to demonstrate complete cross-protection against heterologous ebolavirus challenge. However, ebolavirus vaccines based on vesicular stomatitis virus (VSV) and adenovirus vectors expressing homologous ebolavirus genes have shown protective efficacy in NHPs against multiple ebolaviruses after intramuscular (i.m.) challenge (18, 19). Prior to the current studies, the VSV- and adenovirus-based vaccine platforms are the only ebolavirus vaccine candidates reported to protect NHPs from aerosol exposure to ebolavirus, and the adenovirus-based vaccine is the only vaccine that has demonstrated protection against aerosolized SUDV (19, 20). At present, there are no filovirus vaccines approved for human use, although several candidate vaccines are being readied for clinical trials (21).
The Venezuelan equine encephalitis virus (VEEV) replicon particle vaccine platform, first developed by Pushko et al. (22), is a promising vaccine platform, due in part to its tropism for dendritic cells and its ability to produce high levels of target antigen (22, 23). The platform relies on a modified alphavirus genome in which the structural genes downstream of a subgenomic promoter are replaced by a heterologous gene of interest (24). Replicon RNAs, containing all genes for the replicase complex, are assembled into replicon particles by coexpressing alphavirus structural proteins in trans (25, 26). Upon delivery of the VEEV replicon particle (VRP), the replicase complex drives the expression of the heterologous gene of interest from the subgenomic RNA. Replicon RNA delivered to cells by the VRP contains no structural genes since the structural genes supplied in trans during production lack packaging signals, resulting in a single round of replication (27). The VRP platform has been utilized to develop vaccines for numerous tumor, viral, and bacterial antigens (27). The expression of filovirus proteins by VRPs provides protection against filoviruses in rodent models (28, 29), and the VRP vaccine was the first vaccine platform to demonstrate protection of NHPs against filovirus challenge (30). In these studies, cynomolgus macaques were completely protected against subcutaneous (s.c.) challenge with MARV when vaccinated s.c. with VRP expressing MARV GP alone or MARV GP in combination with MARV NP but only partially protected (two of three animals) when vaccinated with VRP expressing MARV NP alone. However, an analogous study designed to protect macaques against i.m. challenge with EBOV using VRP expressing EBOV GP or NP proved unsuccessful (31). Subsequent studies were carried out using higher doses of VRP vaccine, made possible by improvements in VRP manufacturing and downstream processing (32–35). Here, we report that VRPs expressing EBOV GP or SUDV GP can elicit immune responses that are sufficient to protect NHPs against, not only i.m. challenge, but also against aerosol exposure to homologous virus.
MATERIALS AND METHODS
Ethics statement.
Animal research was conducted in compliance with the Animal Welfare Act and other federal statutes and regulations relating to animals and experiments involving animals and adhered to the principles stated in the Guide for the Care and Use of Laboratory Animals (National Research Council, 2011). The facility is fully accredited by the Association for the Assessment and Accreditation of Laboratory Animal Care International. All challenge studies were conducted under maximum containment in an animal biosafety level 4 (BSL-4) facility at U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) and were approved by the USAMRIID Institutional Animal Care and Use Committee. Due to ethical considerations stemming from the near universal lethality of infection and as is standard practice for NHP studies with filoviruses, historical controls were sometimes used to limit the number of animals required. In these studies, all control animals succumbed to filovirus challenge within the normal time to death.
Cells and viruses.
Vero E6 cells utilized for plaque assays were maintained in Eagle minimal essential medium (EMEM) supplemented with 5% heat-inactivated fetal bovine serum (FBS) and gentamicin (50 μg/ml) at 37°C, 5% CO2, and 80% humidity. BHK-21 cells utilized for VRP analysis were maintained in EMEM supplemented with 10% heat-inactivated FBS, 2 mM l-glutamine, and gentamicin (50 μg/ml) at 37°C, 5% CO2, and 80% humidity. The Boniface isolate of SUDV was used for all SUDV challenge experiments and the Kikwit 95 isolate of EBOV was used for all EBOV challenge experiments.
Vaccination and challenge.
Naive cynomolgus macaques, 2.6 to 6.7 kg, were vaccinated intramuscularly (i.m.) with 1010 focus-forming units (FFU) of indicated VRP vaccine diluted in 0.5 ml of phosphate-buffered saline (PBS). For simultaneous vaccinations with VRP-SUDV GP and VRP-EBOV GP, vaccines were delivered in the quadriceps muscle of opposing legs. NHPs receiving multiple doses of VRP-SUDV GP received an additional vaccination, as described above, 28 days after the initial dose. For i.m. challenge experiments, NHPs were challenged by i.m. injection with a target dose of 1,000 PFU of indicated virus diluted in 0.5 ml of PBS. Titration of challenge inocula determined that NHPs received between 887 and 1,050 PFU of SUDV and between 943 and 1,012 PFU of EBOV. For aerosol challenge experiments, NHPs were challenged with a target dose of 100 PFU The method used for aerosol exposures has been previously described (36). In brief, the NHPs were anesthetized by i.m. injection with tiletamine/zolazepam (6 mg/kg) or ketamine-acepromazine (9 mg of ketamine and 0.1 mg of acepromazine/kg). Whole-body plethysomography was performed under the plane of anesthesia (Buxco Research Systems, Wilmington, NC) for calculation of the respiratory minute volume. Animals were then exposed to SUDV in a head-only aerosol chamber within a class III biological safety cabinet for a time-calculated aerosol exposure. Aerosols were generated using a 3-jet Collison nebulizer (BGI, Inc., Waltham, MA) controlled by the automated exposure control system. The generated aerosol was sampled with an all-glass impinger (AGI) containing 10 ml of collection medium (EMEM/nonessential amino acids, 10% FBS, 0.1% gentamicin, and 0.001% antifoam A). Immediately after the exposure, AGI samples were analyzed by plaque assay. The inhaled dose was calculated for each NHP by using the following formula: dose = Vm × t × Ce, where Vm is the respiratory minute volume, t is the duration of the exposure, and Ce is the aerosol concentration (37). The exposure time was calculated based on the minute volume of each NHP so that the same inhaled dose could be delivered to each dose group. Titration of challenge inocula for aerosol exposures determined that NHPs received between 16 and 132 PFU of SUDV. Challenged animals were monitored closely for at least 28 days after challenge.
Hematology and blood biochemistry.
Phlebotomy was performed while the animals were anesthetized, and blood was collected from the femoral vein using a venous blood collection system (Becton Dickinson, Franklin, NJ). Viremia was determined using traditional plaque assay (38). Hematological values for blood samples collected in tubes containing EDTA were determined using a hematologic analyzer (Coulter Electronics, Hialeah, FL). Serum biochemistry panels were measured using a Piccolo point-of-care blood analyzer (Abaxis, Sunnyvale, CA).
Postmortem examination.
For all of the animal studies described above, the body of each NHP that succumbed or was euthanized due to the severity of clinical disease was submitted for a gross necropsy in BSL-4 containment. In addition, the three animals vaccinated twice with VRP-SUDV GP (experimental animals 16, 17, and 18), which survived a challenge with aerosolized SUDV, were euthanized at the end of the study and submitted for necropsy. Euthanasia and necropsy were also performed on four animals that survived an initial viral challenge with SUDV and back-challenge with EBOV: two NHPs (experimental animals 3 and 4) which had been vaccinated with just VRP-SUDV GP and two NHPs (experimental animals 11 and 12) which received vaccination with both VRP-SUDV GP and VRP-EBOV GP.
For experiments in which the route of viral challenge was i.m., partial necropsies were conducted on all control animals and four of the vaccinated animals. Complete necropsies were performed on five of the vaccinated NHPs from the i.m. challenge studies and on all animals that had been exposed by an aerosol route of challenge. The partial necropsies were done to confirm the presence (or absence) of lesions in organs typically affected by ebolaviruses following a lethal i.m. challenge; samples of the following organs were collected from each animal and fixed in 10% buffered formalin for histology: liver, spleen, adrenal gland, kidney, gonad, and axillary, inguinal, and mesenteric lymph nodes. The same organs were sampled for histology during complete necropsies and, in addition, samples of brain, pituitary gland, eyes, heart, upper and lower respiratory tract, tonsil, mandibular lymph node, mediastinal lymph node, urinary bladder, bone marrow, tongue, esophagus, pancreas, and all levels of the gastrointestinal tract were collected.
The set of formalin-fixed tissue samples from each NHP was held in BSL-4 containment for a minimum of 21 days and then transferred to the USAMRIID histopathology laboratory. All tissue samples were trimmed, routinely processed, and embedded in paraffin. Sections of the paraffin-embedded tissues were cut (5 μm thick) for histology. The histology slides were deparaffinized, stained using hematoxylin and eosin, and placed under coverslips.
IHC.
Immunohistochemistry (IHC) to detect the presence of viral antigen in tissue samples was performed on all NHPs that had been exposed to aerosolized virus. A replicate set of unstained sections from the paraffin-embedded tissues used for histology was made and attached to glass slides. Sections were deparaffinized and exposed for 60 min to a rabbit polyclonal antibody produced against EBOV (cross-reactive with SUDV) or 30 min to an equal mix of two mouse monoclonal antibodies against MARV. Peroxidase-labeled secondary antibody and chromogen was then applied to the fixed tissues. Slides were counterstained with hematoxylin and then covered with a glass coverslip.
ELISA.
Filovirus-specific serum IgG titers were determined by enzyme linked immunosorbent assay (ELISA) using recombinant SUDV or recombinant EBOV GP and as previously described (39). Briefly, polyvinyl chloride ELISA plates (Dynatech Laboratories, Chantilly, VA) were incubated with respective recombinant GP antigens, diluted in PBS (2 μg/ml, 50 μl/well), overnight at 4°C. Plates were blocked with 5% milk protein in PBS–0.02% Tween 20 at room temperature. Serum samples were diluted in blocking buffer supplemented with 1% goat serum and serial 0.5-log dilutions were performed. Antigen-coated ELISA plates were incubated with diluted serum samples for 2 h at room temperature and then washed with wash buffer (PBS, 0.02% Tween 20). Plates were incubated with horseradish peroxidase-conjugated goat anti-NHP IgG (Rockland, Gilbertsville, PA) diluted in blocking buffer for 1 h at room temperature. The plates were washed as described above prior to the addition of ABTS [2, 2′-azino-di(3-ethylbenzthiazoline-6-sulfonate)] substrate (Kirkegaard and Perry Laboratories, Inc., Gaithersburg, MD). Absorbance values were read at 405 nm using a Spectramax plate reader (Molecular Devices, LLC, Sunnyvale, CA). To determine the cutoff values for each dilution, prevaccination serum samples from each individual NHP were run in parallel with postvaccination and postchallenge samples. Cutoff values for each dilution were calculated using absorbance values of prevaccination serum for that dilution and the following formula; average prevaccination serum absorbance + 3× the standard deviation. Endpoint titers for each serum sample are expressed as the last dilution to exceed the cutoff value for a given dilution.
Immunofluorescence microscopy.
BHK cells grown on coverslips were infected with VRP expressing influenza virus hemagglutinin, EBOV GP, or SUDV GP at a multiplicity of infection of 10, followed by incubation at 37°C, 5% CO2, and 80% humidity for 24 h. The cells were then washed three times with PBS and fixed using ice-cold methanol for 5 min. The methanol was removed and the cells were allowed to air dry before incubating them with blocking buffer (5% milk protein in PBS–0.02% Tween 20) overnight at 4°C. The fixed cells were then incubated with EBOV GP-specific human monoclonal antibody KZ52 (kindly provided by Dennis Burton, The Scripps Research Institute, La Jolla, CA) or SUDV GP specific mouse monoclonal antibodies 3C10. Cells were incubated with secondary antibody goat anti-human IgG-488 or goat anti-mouse IgG-488 (Molecular Probes, Eugene, OR) prior to mounting the coverslips on glass slides using Prolong Gold antifade reagent with DAPI (4′,6′-diamidino-2-phenylindole; Molecular Probes). Images were capture on a Zeiss Axio Observer.Z1 microscope using Zen 2011 image acquisition software (Carl Zeiss, Oberkochen, Germany).
Real-time RT-PCR assay.
Real-time reverse transcription PCR (RT-PCR) assays were completed as previously reported (40). Briefly, RNA was purified from whole blood that was collected 7 days postchallenge using TRIzol-LS reagent (Invitrogen, Inc., Carlsbad, CA). Real-time RT-PCR was accomplished using a SuperScript One-Step RT-PCR kit (Invitrogen) with a final concentration of 3 mM MgSO4 and one of the following primer-probe sets: for MARV, F6121 (1 μM), F6121-1 (1.5 μM), R6184 (1 μM), and p6144 (0.2 μM); for EBOV, F2000 (1 μM), R2079 (1 μM), and p2058A (0.1 μM); and for SUDV, F583 (0.8 μM), R659 (0.8 μM), and p608SB (0.1 μM) (40). Real-time RT-PCR amplification was performed as follows: 50°C for 15 min (1 cycle), 95°C for 5 min (1 cycle), 95°C for 1 s and 60°C for 20 s (45 cycles), and 40°C for 30 s (1 cycle), using a LightCycler 2.0 (Roche Applied Sciences, Penzberg, Germany) thermal cycler. Fluorescence was measured at the end of each 60°C step.
Statistical analysis.
Prism software (GraphPad, Inc., San Diego, CA) was used to graph and to conduct statistical comparisons of all data as described in the text. The Fisher exact test (two-tailed) was used to determine statistical differences in survival between the groups that received the ebolavirus VRP vaccines and between the corresponding negative control groups.
RESULTS
SUDV GP expressing VRP vaccine elicits protective immunity against i.m. challenge with SUDV.
VRPs expressing SUDV (Boniface) GP or EBOV (Kikwit) GP were generated using production methods previously described (28, 32–35). SUDV GP and EBOV GP expression was evaluated by immunofluorescence in vitro prior to vaccination (Fig. 1). To determine the protective efficacy of filovirus VRP vaccines in NHPs against i.m. ebolavirus exposure, we vaccinated six experimental cynomolgus macaques i.m. with a single dose of 1010 FFU of VRP-SUDV GP and two control cynomolgus macaques i.m. with 1010 FFU of VRP expressing an irrelevant antigen (smallpox A33R). No adverse events were reported in the days following vaccination, and no local reactions were observed in any of the animals, either in the present study or subsequent studies. Serum samples were collected following vaccination and evaluated by ELISA to determine SUDV GP-specific antibody titers. The VRP-SUDV GP vaccine induced elevated (4.5 to 5.75 logs) SUDV GP-specific serum IgG titers in all NHPs 14 days after vaccination, and these titers remained high in five of the six NHPs out to 28 days postvaccination (Fig. 2A). All NHPs were challenged 28 days postvaccination with a target dose of 1,000 PFU of SUDV delivered by i.m. injection. Control animals succumbed to infection on days 8 and 9 postinfection with classic clinical signs of ebolavirus disease, including elevated serum enzymes, rash, thrombocytopenia, and viremia. Postmortem examination confirmed that these NHPs died due to ebolavirus infection, and there were no other confounding diseases noted. In contrast, all VRP-SUDV GP vaccinated animals survived i.m. challenge with few clinical signs of disease and no detectable viremia (Fig. 2C, Table 1).
Fig 1.

VRP expression of Ebola virus and Sudan virus GP. BHK cells were infected with VRP expressing influenza virus hemagglutinin (A and B), EBOV GP (C), or SUDV GP (D). GP expression was detected using EBOV GP specific monoclonal antibody KZ52 (A and C) or SUDV GP specific monoclonal antibody 3C10 (B and D), and nuclei were stained with DAPI.
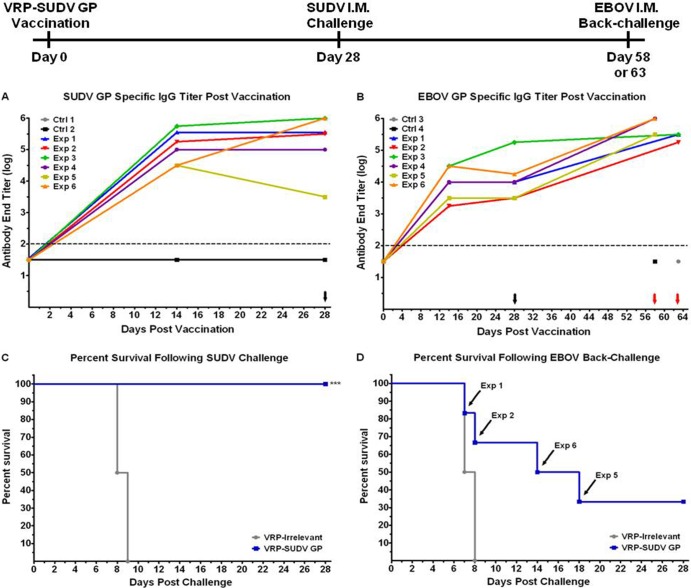
Fig 2.
VRP-SUDV GP protects cynomolgus macaques from SUDV i.m. challenge. NHPs were vaccinated with VRP expressing irrelevant antigen (n = 2) or VRP expressing SUDV GP (n = 6). SUDV GP (A) or EBOV GP (B) specific serum antibody end titers were determined by ELISA at the indicated times postvaccination or challenge. Dotted line indicates assay limit of detection. Black and red arrows indicate time of SUDV challenge and EBOV back-challenge, respectively. (C) NHPs were challenged by i.m. injection of 1,000 PFU of SUDV 28 days postvaccination. (D) Surviving NHPs were then back-challenged by i.m. injection of 1,000 PFU of EBOV 30 or 35 days post-SUDV challenge. ***, P ≤ 0.001 (as determined by the Fisher exact test).
Table 1.
VRP-SUDV GP-vaccinated macaques following i.m. filovirus challenge
| Challenge type and NHPa | Adverse events on days 1 to 28 after challengeb | Status |
|---|---|---|
| After challenge with 1,000 PFU of SUDV i.m. | ||
| Ctrl 1 | Fever (day 7), depression (day 7), mild rash (day 7), viremia (days 5 and 7), thrombocytopenia (day 7), 2- to 3-fold increase in ALT, AST, and ALP, 2- to 3-fold decrease in AMY | Succumbed on day 9 |
| Ctrl 2 | Fever (days 5 and 7), depression (day 6–8), widespread rash (days 7 and 8), anorexia (days 7 and 8), viremia (days 5 and 7), thrombocytopenia (days 5 and 7), >3-fold increase in ALT, AST, and ALP | Succumbed on day 8 |
| Exp 1 | 2- to 3-fold increase in AST and ALP (days 7 and 10) | Survived |
| Exp 2 | Fever (day 7), thrombocytopenia (day 5), 2- to 3-fold increase in ALP (days 7 and 10) | Survived |
| Exp 3 | Fever (day 7), depression (day 7), thrombocytopenia (day 5), 2- to 3-fold increase in AST and ALP (days 7 and 10) | Survived |
| Exp 4 | Anorexia (days 8 and 9), | Survived |
| Exp 5 | Anorexia (days 9 and 10), thrombocytopenia (day 5) | Survived |
| Exp 6 | Thrombocytopenia (day 5) | Survived |
| After back-challenge with 1,000 PFU of EBOV i.m. | ||
| Ctrl 3 | Fever (day 5), hypothermia (day 7), depression (days 6 and 7), mild rash (day 7), anorexia (days 6 and 7), viremia (days 5 and 7), thrombocytopenia (day 7), 2- to 3-fold increase in ALT, >5-fold increase in AST and ALP | Succumbed on day 7 |
| Ctrl 4 | Fever (days 5 and 7), depression (days 6 and 7), mild rash (days 6 and 7), anorexia (day 7), viremia (days 5 and 7), thrombocytopenia (days 5 and 7), >5-fold increase in ALT and AST, 4- to 5-fold increase in ALP | Succumbed on day 8 |
| Exp 1 | Fever (day 5), hypothermia (day 7), depression (days 6 and 7), mild rash (day 7), anorexia (days 6 and 7), viremia (days 5 and 7), thrombocytopenia (day 7), 2- to 3-fold increase in ALT, >5 fold increase in ALP | Succumbed on day 7 |
| Exp 2 | Fever (days 5 and 7), depression (days 6 and 7), mild rash (days 6 and 7), anorexia (day 7), viremia (day 7), thrombocytopenia (days 5 and 7), >5-fold increase in ALT, AST, and ALP | Succumbed on day 8 |
| Exp 3 | Fever (days 5, 7, and 10), depression (days 6 to 10), 2- to 3-fold increase in ALT, >5-fold increase in ALP and AST | Survived |
| Exp 4 | Fever (day 7) | Survived |
| Exp 5 | Fever (day 7), depression (day 18), anorexia (days 16 to 18) | Succumbed on day 18 |
| Exp 6 | Fever (day 7), depression (day 14), mild rash (day 14), anorexia (day 14), thrombocytopenia (day 14), >5-fold increase in ALT, AST, and ALP | Succumbed on day 14 |
Ctrl, control animals; Exp, experimental animals.
ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALP, alkaline phosphatase; AMY, amylase.
Vaccination against SUDV and subsequent survival of SUDV challenge does not confer protection against EBOV challenge.
Despite eliciting high levels of cross-reactive EBOV GP specific serum IgG antibodies (Fig. 2B), VRP-SUDV GP vaccination and survival of SUDV challenge provided only partial protection against heterologous EBOV challenge. Only two of six SUDV survivors were protected against EBOV back-challenge when exposed to a target dose of 1,000 PFU of EBOV i.m. 30 or 35 days after SUDV challenge (Fig. 2D, Table 1). Both naive NHP controls in this experiment and two SUDV survivors succumbed to EBOV challenge on days 7 and 8, within the expected time-to-death window for naive cynomolgus macaques given a lethal i.m. dose of EBOV (18, 19, 31). Two other SUDV survivors succumbed to EBOV challenge on days 14 and 18, several days outside of the expected time-to-death window. Nonetheless, all six NHPs that died after EBOV challenge, including the two controls, presented clinical signs typical of EBOV infection at the time of death and lesions found postmortem were also characteristic of EBOV disease in cynomolgus macaques (Table 1). Of the two SUDV survivors that also survived EBOV challenge, one displayed mild clinical signs of EBOV infection (fever and increased serum liver enzymes), but with no detectable viremia (Table 1). The other surviving NHP presented with mild fever on day 7 but otherwise had no clinical signs of disease. Postmortem examination of the two surviving NHPs revealed scattered hepatic microscopic foci of very mild inflammation; however, there were no indications of an ongoing viral infection at the time that these NHPs were euthanized, as indicated by the lack of viremia. Moderate to marked lymphoid hyperplasia was also present in their spleens and lymph nodes.
Simultaneous vaccination with EBOV GP- and SUDV GP-expressing VRP vaccines protects against EBOV and SUDV i.m. challenge.
Previous studies (41), in combination with the limited protection of SUDV survivors against EBOV challenge observed in the present studies, suggest that a bivalent ebolavirus vaccine may be required to confer protection against both SUDV and EBOV. To address this question we vaccinated six cynomolgus macaques simultaneously with 1010 FFU of VRP-SUDV GP combined with 1010 FFU of VRP-EBOV GP by i.m. injection. Control NHPs received 1010 FFU of VRP expressing an irrelevant antigen (influenza virus hemagglutinin), also by i.m. injection. As before, serum was collected following vaccination to determine SUDV and EBOV specific antibody titers. The dual VRP vaccination elicited SUDV GP specific serum IgG titers of 5 to 6 logs at 14 days postvaccination that then waned to 3.5 to 5 logs by day 28 postvaccination (Fig. 3A and B). EBOV GP specific serum IgG titers were between 4 and 4.5 logs at day 14 postvaccination, and these titers remained elevated or increased slightly to 4 to 5 logs by day 28 postvaccination (Fig. 3B and 4A). On day 28 postvaccination, three vaccinated NHPs and one control NHP were challenged i.m. with a target dose of 1,000 PFU of either SUDV or EBOV. The control NHP challenged with SUDV succumbed on day 8 postinfection, and postmortem examination confirmed that it succumbed due to systemic SUDV infection. All vaccinated NHPs were protected and showed no clinical signs of disease (Fig. 3C, Table 2). Likewise, all vaccinated NHPs were protected against an initial EBOV challenge, with no clinical signs of disease, whereas the control NHP died on day 6 postinfection with classic clinical signs and lesions of EBOV infection (Fig. 4C, Table 2). Having survived exposure to either SUDV or EBOV, the six vaccinated NHPs and two new control NHPs were then challenged 28 or 30 days after the initial challenge with a target dose of 1,000 PFU of the heterologous virus (SUDV survivors with EBOV on day 30 and EBOV survivors with SUDV on day 28). At the time of heterologous challenge, EBOV GP and SUDV GP-specific serum IgG titers remained elevated at 4.5 to 5.5 logs (Fig. 3B) and 5 to 5.5 logs (Fig. 4B), respectively. After back-challenge, control NHPs succumbed to EBOV (Fig. 3D, Table 2) or SUDV (Fig. 4D, Table 2) infection on days 8 and 7, respectively, and postmortem findings confirmed that the NHPs died due to ebolavirus infection. Vaccinated NHPs survived back-challenge with EBOV and displayed no clinical signs of EBOV infection (Fig. 3D, Table 2). Surprisingly, only two of three vaccinated NHPs survived SUDV back-challenge, with these surviving NHPs having no clinical signs of disease (Fig. 4D, Table 2). The vaccinated NHP (experimental 10) that did not survive this SUDV back-challenge experiment began to display clinical signs typical of filovirus infection on day 7 post-SUDV challenge and succumbed on day 10 (Fig. 4D, Table 2). Postmortem examination revealed gross and histologic lesions compatible with a systemic filovirus infection; however, immunohistochemistry (IHC) studies of the liver, spleen, and other selected organs failed to detect the presence of ebolavirus antigens (Fig. 5). Further investigation into the cause of death for this NHP revealed that this animal died not from SUDV but from MARV, likely through fomite or droplet transmission from MARV-infected NHPs housed in the same laboratory suite. At time of death, this NHP was IHC and PCR negative for SUDV and IHC and PCR positive for MARV (Fig. 5, Fig. 6). All other NHPs were PCR negative for MARV (data not shown).
Fig 3.
Dual vaccination with VRP-SUDV GP and VRP-EBOV GP protects cynomolgus macaques from SUDV i.m. challenge. NHPs were vaccinated with VRP expressing irrelevant antigen (n = 1) or VRPs expressing both SUDV GP and EBOV GP (n = 3). SUDV GP (A) or EBOV GP (B) specific serum antibody end titers were determined by ELISA at the indicated times postvaccination or challenge. Dotted line indicates assay limit of detection. Black and red arrows indicate time of SUDV challenge and EBOV back-challenge, respectively. (C) NHPs were challenged by i.m. injection of 1,000 PFU of SUDV 28 days postvaccination. (D) Surviving NHPs were then back challenged by i.m. injection of 1,000 PFU of EBOV 30 days post-SUDV challenge. **, P ≤ 0.01 (as determined by the Fisher exact test).
Fig 4.
Dual vaccination with VRP-SUDV GP and VRP-EBOV GP protects cynomolgus macaques from EBOV i.m. challenge. NHPs were vaccinated with VRP expressing irrelevant antigen (n = 1) or VRPs expressing both SUDV GP and EBOV GP (n = 3). EBOV GP (A) or SUDV GP (B) specific serum antibody end titers were determined by ELISA at the indicated times postvaccination or challenge. Dotted line indicates assay limit of detection. Black and red arrows indicate time of EBOV challenge and SUDV back-challenge, respectively. (C) NHPs were challenged by i.m. injection of 1,000 PFU of EBOV 28 days postvaccination. (D) Surviving NHPs were then back challenged by i.m. injection of 1,000 PFU of SUDV 28 days post-EBOV challenge. **, P ≤ 0.01 (as determined by the Fisher exact test).
Table 2.
Pan-EBOV-vaccinated macaques following i.m. filovirus challenge
| Challenge type and NHPa | Adverse events on days 1 to 28 after challengeb | Status |
|---|---|---|
| After challenge with 1,000 PFU of SUDV i.m. | ||
| Ctrl 5 | Fever (days 5 and 7), depression (days 6 and 7), widespread rash (day 7), anorexia (days 5 to 7), viremia (days 5 and 7), thrombocytopenia (days 5 and 7), 4- to 5-fold increase in ALT and ALP, >5-fold increase in AST | Succumbed on day 8 |
| Exp 7 | No clinical signs | Survived |
| Exp 8 | No clinical signs | Survived |
| Exp 9 | No clinical signs | Survived |
| After back-challenge with 1,000 PFU of EBOV i.m. | ||
| Ctrl 6 | Depression (days 6 and 7), anorexia (days 6 and 7), viremia (days 5 and 7), thrombocytopenia (days 5 and 7), 4- to 5-fold increase in ALP, >5-fold increase in ALT and AST | Succumbed on day 8 |
| Exp 7 | No clinical signs | Survived |
| Exp 8 | No clinical signs | Survived |
| Exp 9 | No clinical signs | Survived |
| After challenge with 1,000 PFU of EBOV i.m. | ||
| Ctrl 7 | Fever (day 5), hypothermia (day 6), widespread rash (day 6), anorexia (days 5 and 6), viremia (days 3, 5, and 6), thrombocytopenia (days 5 and 6), 2- to 3-fold increase in ALP, >5-fold increase in ALT and AST | Succumbed on day 6 |
| Exp 10 | No clinical signs | Survived |
| Exp 11 | No clinical signs | Survived |
| Exp 12 | No clinical signs | Survived |
| After back-challenge with 1,000 PFU of SUDV i.m. | ||
| Ctrl 8 | Fever (days 5 and 7), depression (day 7), widespread rash (day 7), anorexia (days 6 and 7), viremia (days 5 and 7), thrombocytopenia (days 5 and 7), 4- to 5-fold increase in ALT and ALP, >5-fold increase in AST | Succumbed on day 7 |
| Exp 10 | Fever (day 7), depression (days 7 to 9), mild rash (day 9), anorexia (days 8 and 9), viremia (days 5 and 7), >5-fold increase in ALT and AST | Succumbed on day 10c |
| Exp 11 | No clinical signs | Survived |
| Exp 12 | No clinical signs | Survived |
Ctrl, control animals; Exp, experimental animals.
ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALP, alkaline phosphatase; AMY, amylase.
Succumbed to MARV infection. PCR and antigen negative for SUDV at time of death.
Fig 5.
Histologic lesions typical of filovirus infection in experimental animal 10. (A) Liver has diffuse vacuolar degeneration of hepatocytes adjacent to a central vein (V), with foci of hepatocellular necrosis (arrowheads). (B) Spleen, with markedly decreased numbers of lymphocytes (i.e., lymphoid depletion) and hemorrhage in a lymphoid nodule (N). Deposits of large amounts of fibrin in the surrounding red pulp appear as amorphous to fibrillar pink material. (C and D) IHC of liver and spleen, respectively, fails to detect the presence of ebolavirus antigen. The greenish-brown granules present in some hepatocytes are bile pigment. (E and F) IHC of liver and spleen, respectively, reveals abundant marburgvirus antigen (brown staining) within hepatic Kupffer cells, endothelial cells, hepatocytes, and splenic histiocytes. Extracellular viral antigen is also present in areas of hepatic necrosis and in fibrin deposits in the spleen. Objective magnification: 40× for liver photos and 10× for spleen photos.
Fig 6.

Real-time PCR detection of filovirus. RNA was purified from whole blood collected on day 7 postchallenge. One-step RT-PCRs were completed using filovirus species-specific primers. Reciprocal critical threshold (CT) values are reported. Dotted line indicates assay limit of detection (1 PFU/reaction).
Protection against aerosolized SUDV requires two vaccinations with SUDV GP expressing VRP vaccine.
To evaluate the protective efficacy of the SUDV VRP vaccine against aerosol exposure, cynomolgus macaques were vaccinated once (n = 3) or twice (n = 3), 28 days apart, with 1010 FFU of VRP-SUDV GP by i.m. injection. Control NHPs received either one dose (n = 1) or two doses (n = 3) of 1010 FFU of VRP expressing an irrelevant antigen (smallpox A33R) by i.m. injection. Serum was collected following vaccination to assess SUDV GP-specific IgG titers. NHPs that received a single vaccination had SUDV GP specific serum IgG titers of 3.5 to 4.75 logs 14 days following vaccination that waned to 2.75 to 3.75 logs by day 28 postvaccination (Fig. 7A). For NHPs that received two vaccinations, SUDV GP specific serum IgG titers increased from 3.5 to 4.5 logs at day 28 after primary vaccination to peak titers of 4.5 to 5.5 logs before diminishing to 3.5 logs at the time of SUDV challenge (Fig. 7B). NHPs were challenged 28 days following final vaccination with a target dose of 100 PFU of SUDV by the aerosol route. The four control animals developed clinical signs typical of ebolavirus infection and all succumbed between days 7 and 9 (Fig. 7, Table 3). In contrast to SUDV i.m. challenge, all three animals vaccinated with one dose of VRP-SUDV GP presented with severe clinical signs and succumbed on day 7 or 8 following SUDV aerosol exposure (Fig. 7C, Table 3). Postmortem examination revealed that these seven monkeys had lesions in their livers and other organs typical of those that occur with systemic SUDV infection after i.m. challenge. In addition, all of these animals had virus-induced lesions in their respiratory tracts that appear to be unique to an aerosol route of viral infection. Gross lung lesions included edema, multiple red to tan foci of consolidation, and fibrinous pleuritis causing adhesions between lung lobes and between the lobes and thoracic wall (Fig. 8A). Histologically, there were multiple foci of acute fibrinous to hemorrhagic pneumonia that often involved the overlying pleura (Fig. 8C). The mediastinal lymph nodes, which receive lymphatic drainage from the lungs, had acute necrotizing inflammation and lymphoid depletion. IHC revealed abundant ebolavirus antigen in the lung and lymph node lesions (Fig. 8D). All NHPs that received two doses of VRP-SUDV GP survived SUDV aerosol challenge with one asymptomatic animal, one displaying mild clinical signs (lymphopenia, fever, mild depression), and one experiencing severe signs of ebolavirus infection (increased serum liver enzymes, decreased platelets, lymphopenia, fever, depression, anorexia, weight loss) before making a full recovery (Fig. 7D, Table 3). Postmortem examination revealed multiple foci of chronic granulomatous pneumonia in the two macaques that had displayed clinical signs, and ebolavirus antigen was detected by IHC in some of these lesions but not in other areas of the lungs or in any other tissues (Fig. 8E and F). The other asymptomatic animal had only a few foci of mild chronic interstitial pneumonia with no detectable viral antigens in any tissues. All three of these survivors had moderate to marked lymphoid hyperplasia in their spleens and lymph nodes.
Fig 7.
Vaccination with VRP-SUDV GP protects cynomolgus macaques from SUDV aerosol challenge. NHPs were vaccinated with one (A and C) or two (B and D) doses of VRP expressing irrelevant antigen or VRP expressing SUDV GP. SUDV GP specific serum antibody end titers were determined by ELISA at the indicated times postvaccination with one (A) or two (B) doses of vaccine. Dotted line indicates assay limit of detection. (C) NHPs receiving one dose of irrelevant VRP (n = 1) or VRP-SUDV GP (n = 3) were challenged by aerosol exposure to 100 PFU of SUDV 28 days postvaccination. (D) NHPs receiving two doses of irrelevant VRP (n = 3) or VRP-SUDV GP (n = 3) were challenged by aerosol exposure to 100 PFU of SUDV 28 days following the second vaccination. **, P ≤ 0.01 (as determined by the Fisher exact test).
Table 3.
VRP-SUDV GP-vaccinated macaques after aerosol filovirus challenge
| NHPa | Adverse events on days 1 to 28 after challengeb | Status |
|---|---|---|
| Ctrl 9 | Depression (days 7 and 8), widespread rash (days 7 and 8), anorexia (days 7 and 8) viremia (days 3, 5, and 7), thrombocytopenia (days 3, 5, and 7), 2- to 3-fold increase in ALT and ALP, >5-fold increase in AST, 2- to 3-fold decrease in AMY | Succumbed on day 9 |
| Ctrl 10 | Depression (days 6 to 8), widespread rash (days 6 and 7), anorexia (days 7 and 8), viremia (days 3, 5, and 7), thrombocytopenia (days 5 and 7), >5-fold increase in AST | Succumbed on day 9 |
| Ctrl 11 | Fever (day 7), depression (days 7 to 9), widespread rash (days 8 and 9), anorexia (days 8 and 9), bleeding from nose (day 9), viremia (days 5 and 7), thrombocytopenia (days 5, 7, and 9), 2- to 3-fold increase in ALP, >5-fold increase in ALT and AST | Succumbed on day 9 |
| Ctrl 12 | Depression (days 6 and 7), widespread rash (day 7), anorexia (days 6 and 7), viremia (days 5 and 7), thrombocytopenia (days 5 and 7), >5-fold increase in ALT and ALP | Succumbed on day 7 |
| Exp 13 | Fever (day 5), depression (days 6 and 7), mild rash (day 7), anorexia (day 7), viremia (day 7), thrombocytopenia (days 3, 5, and 7), 2- to 3-fold increase in AST (day 7), 2- to 3-fold decrease in AMY | Succumbed on day 8 |
| Exp 14 | Depression (day 7), widespread rash (day 7), anorexia (day 7), viremia (day7), thrombocytopenia (day 7), 4- to 5-fold increase in ALT, >5-fold increase in AST and ALP, 2- to 3-fold decrease in AMY | Succumbed on day 8 |
| Exp 15 | Depression (day 6), mild rash (day 6), anorexia (day 6), thrombocytopenia (days 3 and 5), 2- to 3-fold decrease in AMY | Succumbed on day 7 |
| Exp 16 | Fever (day 10), depression (days 9 to 12), anorexia (days 9 to 12) | Survived |
| Exp 17 | No clinical signs | Survived |
| Exp 18 | Depression (days 6 to 14), anorexia (days 6 to 14), viremia (day 5), 2- to 3-fold increase in ALP | Survived |
Ctrl, control animals; Exp, experimental animals. All animals were challenged with 100 PFU of SUDV by aerosol.
ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALP, alkaline phosphatase; AMY, amylase.
Fig 8.
Pulmonary lesions associated with aerosolized SUDV. (A) Dorsal view of lungs and trachea (T) from experimental animal 13, after removal from the thoracic cavity. There is diffuse pulmonary edema and a large area of dark-red consolidation (arrow) in the caudal aspect of the left superior lung lobe (S). The pleural surface in this area and the left middle lung lobe (M) is covered with tan-white fibrinous exudate which causes adhesions between the left superior, middle, and inferior (I) lung lobes. (B) Histologic section of normal lung from a cynomolgus macaque that died after i.m. challenge with SUDV. Clear spaces are alveoli and are separated by thin-walled septa and small blood vessels (V). (C) Histologic section of lung from control animal 12, which died 7 days after challenge with aerosolized SUDV. The alveoli are filled by edema fluid, fibrin, and a mixture of macrophages, neutrophils, and red blood cells. Alveolar septa are congested and thickened with inflammatory cells. A small arteriole (A) is also present. (D) IHC of lung from control animal 12 reveals the presence of abundant intracellular and extracellular ebolavirus antigen (brown staining). (E) Histologic section of a pulmonary granuloma in experimental animal 18, which survived a challenge with aerosolized SUDV. The center of the granuloma (left 1/3 of the photo) contains suppurative inflammation, fibrin, and necrotic debris. The wall of the granuloma (right 2/3 of the photo) is composed of macrophages, lymphocytes, plasma cells, and fibrous connective tissue. (F) IHC of a replicate section of the image in panel E reveals ebolavirus antigen within macrophages and scattered extracellular antigen in the area of necrosis. Objective magnifications (B to F), ×20.
DISCUSSION
The results presented here clearly demonstrate, for the first time, the protective efficacy of ebolavirus VRP vaccines against SUDV and EBOV challenge in cynomolgus macaques. Improved manufacturing processes (32–34) have allowed us to vaccinate with higher doses (≥3 logs higher) of VRP vaccine compared to the previously reported attempt, which may in part explain the difference in outcomes (31). It is possible that differences in the results between the two studies may also be explained by differences in the route of vaccine delivery, s.c. versus i.m. injections, although a direct comparison of these two routes was not completed using the same dose and VRP material. The SUDV GP and EBOV GP VRP vaccines proved to be quite potent since protection against i.m. exposure to the corresponding ebolavirus was afforded following a single vaccination. The VRP, VSV, and adenovirus-based vaccines are the only filovirus vaccine candidates to provide full protection to NHPs after only one vaccination (19, 41, 42). Potency associated with the VRP-based vaccines may be partially attributed to the propensity of VRPs to infect antigen-presenting cells, in particular, dendritic cells (43). Natural adjuvant properties of VRPs are known to promote antigen-specific T cell immunity and regulate a balanced antigen specific antibody response, which may also contribute to the potency of the VRP vaccine platform (44).
Differences in genomic nucleotide (37 to 41% homologous) and amino acid (34 to 43% homologous) sequence homology among ebolaviruses have made cross-species protection difficult. This raises serious concerns about the efficacy of the current ebolavirus vaccine platforms against emerging filoviruses (45). Jones et al. previously reported that vaccination against EBOV and subsequent survival of an EBOV infection in NHPs does not confer complete protection against back-challenge with SUDV (41). We report similar findings in that vaccination against SUDV and subsequent survival of a SUDV infection in NHPs did not confer protection against back-challenge with EBOV. These findings lend further support to what others before us have concluded: that a pan-ebolavirus vaccine will likely require multiple components specific for each ebolavirus. Here, we demonstrated the immunogenicity and protective efficacy of a dual-ebolavirus VRP vaccine strategy that involves simultaneous vaccination with VRPs expressing SUDV and EBOV GPs. High antibody titers to both SUDV GP and EBOV GP were generated following vaccination, and all animals survived i.m. challenge with either virus. An effective multi-ebolavirus vaccination strategy has also been reported for adenovirus and VSV-based filovirus vaccine candidates in NHPs (18, 19). Collectively, these promising results suggest that immune interference between multiple ebolavirus antigens is unlikely to occur and does not adversely affect the downstream efficacy of these vaccine platforms. This illustrates the feasibility of a single, multifaceted ebolavirus vaccine that may protect against multiple ebolaviruses. This does not eliminate the possibility that a vaccine consisting of a single antigen will not be efficacious against diverse ebolaviruses or that heterologous cross-protection is not feasible. Hensley et al. recently provided evidence that a EBOV GP and SUDV GP specific DNA prime/adenovirus boost vaccination strategy provided complete cross-protection against BDBV exposure in NHPs (46). The authors stated that cross-reactive T cell populations and not cross-reactive antibodies (undetectable) may have contributed to this cross-protection. A more recent report demonstrated that vaccination with an EBOV-specific VSV vaccine provided partial (75%) protection against BDBV exposure in NHPs (47). Cross-reactive antibody titers to BDBV GP were developed in two of four NHPs following vaccination, although no correlation between BDBV GP antibody titers and protection could be drawn. A cross-reactive T cell evaluation was not reported. It is not clear whether the dual-ebolavirus VRP vaccine presented here will provide cross-protection against other ebolaviruses, known or yet to be discovered, nor is it understood what effect the addition of MARV components may have on the efficacy of a candidate pan-filovirus VRP vaccine. It is encouraging to note, however, that a filovirus VSV vaccine platform, consisting of EBOV, SUDV, and MARV specific components and delivered simultaneously, protected NHPs from exposure to all three viruses, as well as TAFV (18).
Protective efficacy against an aerosol exposure to filoviruses is of paramount concern given that aerosol transmission represents the most likely means of dispersing a biological weapon over a populated area (14). Few filovirus vaccine candidates have been tested against aerosolized filoviruses, and far less is known about filovirus pathology and disease following aerosol exposure in NHPs compared to i.m. challenge. The VSV vaccine platform was the first to demonstrate protective efficacy in NHPs against aerosolized MARV or EBOV (20). In these studies, NHPs were completely protected against aerosol exposure to MARV or EBOV following a single vaccination with recombinant VSV expressing MARV GP or EBOV GP, respectively. The authors noted that the disease progression appeared to be slightly delayed compared to i.m. challenge with MARV or EBOV. They also stated that despite the route of infection, the lung seemed to be minimally involved with regard to disease progression compared to other organs, such as the liver and spleen. These findings are supported by recent efforts of Pratt et al. in which the authors evaluated the efficacy of an adenovirus 5 (Ad5) bivalent vaccine vector expressing EBOV and SUDV GPs against aerosolized ebolaviruses in NHPs. As with the previous report, this group demonstrated that a single vaccination could protect against aerosolized EBOV and that lung lesions in the control animal were unremarkable compared to i.m. challenge. This was not the case, however, for aerosol exposure to SUDV. Control NHPs challenged with aerosolized SUDV developed significant lesions in their lungs and mediastinal lymph nodes that were not seen in animals challenged by an i.m. route of administration. Furthermore, a single vaccination with the bivalent Ad5 ebolavirus vaccine was unable to fully protect NHPs against aerosol exposure to SUDV. Of more concern, the vaccinated NHP that succumbed to aerosolized SUDV infection presented with more severe lung lesions than those presented in the control animals. These lesions were characterized by necrotizing pneumonia and fibrinous pleuritis. The results of our studies support the findings reported by Pratt et al. in that aerosol exposure to SUDV caused significant respiratory disease in control animals and that a single vaccination with the VRP-SUDV GP vaccine was unable to protect NHPs against aerosolized SUDV. Consistent with the previous study, we also noted severe viral pneumonia and fibrinous pleural adhesions in control and vaccinated NHPs that succumbed to SUDV aerosol infection. As with the Ad5 vaccine, a second booster vaccination with VRP-SUDV GP was able to elicit protective immunity against aerosolized SUDV. However, with both the Ad5 and the VRP vaccines, foci of chronic inflammation were found in the respiratory tracts of twice-vaccinated animals that had displayed clinical signs but survived challenge. Thus, unlike EBOV or MARV aerosol exposure, NHPs exposed to aerosolized SUDV seem to experience enhanced viral pathogenesis characterized by complicating viral pneumonia in addition to classic filovirus associated liver, spleen, and kidney failure. All indications thus far imply that protection against aerosolized SUDV may be more difficult to achieve compared to aerosolized EBOV or MARV, suggesting that the SUDV aerosol model may represent the most stringent standard for vaccine efficacy studies going forward.
Although the results presented here are encouraging for the overall development of an effective ebolavirus vaccine, it is important to keep in mind that critical questions remain unanswered. We have yet to evaluate the duration of protective immunity associated with any of the ebolavirus VRP vaccines, and little has been reported in the way of other ebolavirus vaccine candidates regarding duration. Duration studies will be critical in understanding the practical utility of various vaccine candidates, and these studies may provide critical information needed to help select the best ebolavirus vaccine platform to move forward to licensure. As with any vector-based vaccine platform, preexisting immunity to the vector can have deleterious effects on vaccine efficacy. The prevalence of immunity to VEEV is difficult to predict in populations of the Americas where VEEV is endemic and results in sporadic human outbreaks (48, 49). The ebolavirus VRP vaccine candidate, as well as any other vector-based vaccine, may be required to demonstrate protective efficacy in the face of preexisting anti-vector immunity in order to advance to licensure. Finally, the mechanism by which the ebolavirus VRP vaccine induces protective immunity must be understood to gain U.S. Food and Drug Administration licensure. The antibody titers reported here clearly indicate that humoral immune responses are elicited following VRP vaccination and provide a useful determinant of seroconversion; however, these studies lack a comprehensive evaluation of both humoral and cellular immunity needed to define correlates of immunity. As with other ebolavirus vaccine candidates, clear correlates of immunity need to be defined and appropriate parallels to human immune responses must be drawn. Ongoing efforts are aimed at addressing these unanswered questions as we move toward advanced development and ultimately licensure of ebolavirus vaccines.
ACKNOWLEDGMENTS
We thank Jennifer Brannan (USAMRIID) and Jens Kuhn (NIAID) for reviewing the manuscript; Alan Schmaljohn (University of Maryland) and Michael Parker (USAMRIID) for helpful discussions on experimental design; the Veterinary Medicine Division (USAMRIID) for assisting with animal treatments; the Center for Aerobiological Sciences (USAMRIID) for technical assistance with aerosol challenge; and the Pathology Division (USAMRIID) for technical assistance with animal necropsies, histology, and immunohistochemistry.
This study was kindly supported by the Defense Threat Reduction Agency (project CBM.VAXPLAT.05.10.RD.005).
The opinions, conclusions, interpretations, and recommendations included here are those of the authors and are not necessarily endorsed by the U.S. Army. The mention of trade names or commercial products does not constitute endorsement or recommendation for use by the Department of the Army or the Department of Defense.
A.S.H., G.G.O., W.D.P., J.F.S., M.K.H., and J.M.D. conceived and designed the experiments. A.S.H., A.I.K., J.F.B., R.A.O., D.K.N., S.E.Z., S.W.S., M.A.M., R.R.B., L.I.P., J.L.G., J.S.L., W.D.P., M.C., K.I.K., and J.M.D. performed the experiments. A.S.H., A.I.K., J.F.B., D.K.N., S.W.S., and J.M.D. analyzed the data. A.S.H., D.K.N., and J.M.D. wrote the paper.
Footnotes
Published ahead of print 13 February 2013
REFERENCES
- 1. Hoenen T, Groseth A, Falzarano D, Feldmann H. 2006. Ebola virus: unraveling pathogenesis to combat a deadly disease. Trends Mol. Med. 12:206–215 [DOI] [PubMed] [Google Scholar]
- 2. Kuhn JH, Becker S, Ebihara H, Geisbert TW, Johnson KM, Kawaoka Y, Lipkin WI, Negredo AI, Netesov SV, Nichol ST, Palacios G, Peters CJ, Tenorio A, Volchkov VE, Jahrling PB. 2010. Proposal for a revised taxonomy of the family Filoviridae: classification, names of taxa and viruses, and virus abbreviations. Arch. Virol. 155:2083–2103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ascenzi P, Bocedi A, Heptonstall J, Capobianchi MR, Di Caro A, Mastrangelo E, Bolognesi M, Ippolito G. 2008. Ebolavirus and Marburgvirus: insight the Filoviridae family. Mol. Aspects Med. 29:151–185 [DOI] [PubMed] [Google Scholar]
- 4. Sanchez A, Feldmann GTWH. 2007. Filoviridae: Marburg and Ebola viruses, p 1409–1448 In Knipe DM, Griffin DE, Lamb RA, Martin MA, Roizman B, Straus SE. (ed), Fields virology, 5th ed, vol 1 Lippincott/Williams & Wilkins Co, Philadelphia, PA [Google Scholar]
- 5. Leroy EM, Kumulungui B, Pourrut X, Rouquet P, Hassanin A, Yaba P, Delicat A, Paweska JT, Gonzalez JP, Swanepoel R. 2005. Fruit bats as reservoirs of Ebola virus. Nature 438:575–576 [DOI] [PubMed] [Google Scholar]
- 6. Swanepoel R, Leman PA, Burt FJ, Zachariades NA, Braack LE, Ksiazek TG, Rollin PE, Zaki SR, Peters CJ. 1996. Experimental inoculation of plants and animals with Ebola virus. Emerg. Infect. Dis. 2:321–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Swanepoel R, Smit SB, Rollin PE, Formenty P, Leman PA, Kemp A, Burt FJ, Grobbelaar AA, Croft J, Bausch DG, Zeller H, Leirs H, Braack LE, Libande ML, Zaki S, Nichol ST, Ksiazek TG, Paweska JT. 2007. Studies of reservoir hosts for Marburg virus. Emerg. Infect. Dis. 13:1847–1851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Towner JS, Amman BR, Sealy TK, Carroll SA, Comer JA, Kemp A, Swanepoel R, Paddock CD, Balinandi S, Khristova ML, Formenty PB, Albarino CG, Miller DM, Reed ZD, Kayiwa JT, Mills JN, Cannon DL, Greer PW, Byaruhanga E, Farnon EC, Atimnedi P, Okware S, Katongole-Mbidde E, Downing R, Tappero JW, Zaki SR, Ksiazek TG, Nichol ST, Rollin PE. 2009. Isolation of genetically diverse Marburg viruses from Egyptian fruit bats. PLoS Pathog. 5:e1000536 doi:10.1371/journal.ppat.1000536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Leroy EM, Epelboin A, Mondonge V, Pourrut X, Gonzalez JP, Muyembe-Tamfum JJ, Formenty P. 2009. Human Ebola outbreak resulting from direct exposure to fruit bats in Luebo, Democratic Republic of Congo, 2007. Vector Borne Zoonotic Dis. 9:723–728 [DOI] [PubMed] [Google Scholar]
- 10. Bermejo M, Rodriguez-Teijeiro JD, Illera G, Barroso A, Vila C, Walsh PD. 2006. Ebola outbreak killed 5000 gorillas. Science 314:1564. [DOI] [PubMed] [Google Scholar]
- 11. Walsh PD, Breuer T, Sanz C, Morgan D, Doran-Sheehy D. 2007. Potential for Ebola transmission between gorilla and chimpanzee social groups. Am. Nat. 169:684–689 [DOI] [PubMed] [Google Scholar]
- 12. Johnson E, Jaax N, White J, Jahrling P. 1995. Lethal experimental infections of rhesus monkeys by aerosolized Ebola virus. Int. J. Exp. Pathol. 76:227–236 [PMC free article] [PubMed] [Google Scholar]
- 13. Lub M, Sergeev AN, P'Iankov VO, P'Iankova GO, Petrishchenko VA, Kotliarov LA. 1995. Certain pathogenetic characteristics of a disease in monkeys in infected with the Marburg virus by an airborne route. Vopr. Virusol. 40:158–161 (In Russian.) [PubMed] [Google Scholar]
- 14. Borio L, Inglesby T, Peters CJ, Schmaljohn AL, Hughes JM, Jahrling PB, Ksiazek T, Johnson KM, Meyerhoff A, O'Toole T, Ascher MS, Bartlett J, Breman JG, Eitzen EM, Jr, Hamburg M, Hauer J, Henderson DA, Johnson RT, Kwik G, Layton M, Lillibridge S, Nabel GJ, Osterholm MT, Perl TM, Russell P, Tonat K. 2002. Hemorrhagic fever viruses as biological weapons: medical and public health management. JAMA 287:2391–2405 [DOI] [PubMed] [Google Scholar]
- 15. Reed DS, Mohamadzadeh M. 2007. Status and challenges of filovirus vaccines. Vaccine 25:1923–1934 [DOI] [PubMed] [Google Scholar]
- 16. Carette JE, Raaben M, Wong AC, Herbert AS, Obernosterer G, Mulherkar N, Kuehne AI, Kranzusch PJ, Griffin AM, Ruthel G, Dal Cin P, Dye JM, Whelan SP, Chandran K, Brummelkamp TR. 2011. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature 477:340–343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chandran K, Sullivan NJ, Felbor U, Whelan SP, Cunningham JM. 2005. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science 308:1643–1645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Geisbert TW, Geisbert JB, Leung A, Daddario-DiCaprio KM, Hensley LE, Grolla A, Feldmann H. 2009. Single-injection vaccine protects nonhuman primates against infection with Marburg virus and three species of Ebola virus. J. Virol. 83:7296–7304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pratt WD, Wang D, Nichols DK, Luo M, Woraratanadharm J, Dye JM, Holman DH, Dong JY. 2010. Protection of nonhuman primates against two species of Ebola virus infection with a single complex adenovirus vector. Clin. Vaccine Immunol. 17:572–581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Geisbert TW, Daddario-Dicaprio KM, Geisbert JB, Reed DS, Feldmann F, Grolla A, Stroher U, Fritz EA, Hensley LE, Jones SM, Feldmann H. 2008. Vesicular stomatitis virus-based vaccines protect nonhuman primates against aerosol challenge with Ebola and Marburg viruses. Vaccine 26:6894–6900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Falzarano D, Geisbert TW, Feldmann H. 2011. Progress in filovirus vaccine development: evaluating the potential for clinical use. Expert Rev. Vaccines 10:63–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pushko P, Parker M, Ludwig GV, Davis NL, Johnston RE, Smith JF. 1997. Replicon-helper systems from attenuated Venezuelan equine encephalitis virus: expression of heterologous genes in vitro and immunization against heterologous pathogens in vivo. Virology 239:389–401 [DOI] [PubMed] [Google Scholar]
- 23. Schlesinger S. 2001. Alphavirus vectors: development and potential therapeutic applications. Expert Opin. Biol. Ther. 1:177–191 [DOI] [PubMed] [Google Scholar]
- 24. Davis NL, Brown KW, Johnston RE. 1996. A viral vaccine vector that expresses foreign genes in lymph nodes and protects against mucosal challenge. J. Virol. 70:3781–3787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Frolov I, Frolova E, Schlesinger S. 1997. Sindbis virus replicons and Sindbis virus: assembly of chimeras and of particles deficient in virus RNA. J. Virol. 71:2819–2829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Smerdou C, Liljestrom P. 1999. Two-helper RNA system for production of recombinant Semliki Forest virus particles. J. Virol. 73:1092–1098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rayner JO, Dryga SA, Kamrud KI. 2002. Alphavirus vectors and vaccination. Rev. Med. Virol. 12:279–296 [DOI] [PubMed] [Google Scholar]
- 28. Pushko P, Bray M, Ludwig GV, Parker M, Schmaljohn A, Sanchez A, Jahrling PB, Smith JF. 2000. Recombinant RNA replicons derived from attenuated Venezuelan equine encephalitis virus protect guinea pigs and mice from Ebola hemorrhagic fever virus. Vaccine 19:142–153 [DOI] [PubMed] [Google Scholar]
- 29. Wilson JA, Bray M, Bakken R, Hart MK. 2001. Vaccine potential of Ebola virus VP24, VP30, VP35, and VP40 proteins. Virology 286:384–390 [DOI] [PubMed] [Google Scholar]
- 30. Hevey M, Negley D, Pushko P, Smith J, Schmaljohn A. 1998. Marburg virus vaccines based upon alphavirus replicons protect guinea pigs and nonhuman primates. Virology 251:28–37 [DOI] [PubMed] [Google Scholar]
- 31. Geisbert TW, Pushko P, Anderson K, Smith J, Davis KJ, Jahrling PB. 2002. Evaluation in nonhuman primates of vaccines against Ebola virus. Emerg. Infect. Dis. 8:503–507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kamrud KI, Alterson KD, Andrews C, Copp LO, Lewis WC, Hubby B, Patel D, Rayner JO, Talarico T, Smith JF. 2008. Analysis of Venezuelan equine encephalitis replicon particles packaged in different coats. PLoS One 3:e2709 doi:10.1371/journal.pone.0002709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kamrud KI, Custer M, Dudek JM, Owens G, Alterson KD, Lee JS, Groebner JL, Smith JF. 2007. Alphavirus replicon approach to promoterless analysis of IRES elements. Virology 360:376–387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Montgomery SA, Berglund P, Beard CW, Johnston RE. 2006. Ribosomal protein S6 associates with alphavirus nonstructural protein 2 and mediates expression from alphavirus messages. J. Virol. 80:7729–7739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Reap EA, Morris J, Dryga SA, Maughan M, Talarico T, Esch RE, Negri S, Burnett B, Graham A, Olmsted RA, Chulay JD. 2007. Development and preclinical evaluation of an alphavirus replicon particle vaccine for cytomegalovirus. Vaccine 25:7441–7449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hartings JM, Roy CJ. 2004. The automated bioaerosol exposure system: preclinical platform development and a respiratory dosimetry application with nonhuman primates. J. Pharmacol. Toxicol. Methods 49:39–55 [DOI] [PubMed] [Google Scholar]
- 37. Roy CJ, Pitt LM. 2006. Infectious disease aerobiology: aerosol challenge methods, p 61–76 In Swearengen JR. (ed), Biodefense: research methodology and animal models. Taylor & Francis Group, Boca Raton, FL [Google Scholar]
- 38. Moe JB, Lambert RD, Lupton HW. 1981. Plaque assay for Ebola virus. J. Clin. Microbiol. 13:791–793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dye JM, Herbert AS, Kuehne AI, Barth JF, Muhammad MA, Zak SE, Ortiz RA, Prugar LI, Pratt WD. 2012. Post-exposure antibody prophylaxis protects nonhuman primates from filovirus disease. Proc. Natl. Acad. Sci. U. S. A. 109:5034–5039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Trombley AR, Wachter L, Garrison J, Buckley-Beason VA, Jahrling J, Hensley LE, Schoepp RJ, Norwood DA, Goba A, Fair JN, Kulesh DA. Comprehensive panel of real-time TaqMan polymerase chain reaction assays for detection and absolute quantification of filoviruses, arenaviruses, and New World hantaviruses. Am. J. Trop. Med. Hyg. 82:954–960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Jones SM, Feldmann H, Stroher U, Geisbert JB, Fernando L, Grolla A, Klenk HD, Sullivan NJ, Volchkov VE, Fritz EA, Daddario KM, Hensley LE, Jahrling PB, Geisbert TW. 2005. Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat. Med. 11:786–790 [DOI] [PubMed] [Google Scholar]
- 42. Sullivan NJ, Geisbert TW, Geisbert JB, Xu L, Yang ZY, Roederer M, Koup RA, Jahrling PB, Nabel GJ. 2003. Accelerated vaccination for Ebola virus haemorrhagic fever in non-human primates. Nature 424:681–684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Nishimoto KP, Laust AK, Wang K, Kamrud KI, Hubby B, Smith JF, Nelson EL. 2007. Restricted and selective tropism of a Venezuelan equine encephalitis virus-derived replicon vector for human dendritic cells. Viral Immunol. 20:88–104 [DOI] [PubMed] [Google Scholar]
- 44. Thompson JM, Whitmore AC, Staats HF, Johnston RE. 2008. Alphavirus replicon particles acting as adjuvants promote CD8+ T cell responses to co-delivered antigen. Vaccine 26:4267–4275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sanchez A, Trappier SG, Mahy BW, Peters CJ, Nichol ST. 1996. The virion glycoproteins of Ebola viruses are encoded in two reading frames and are expressed through transcriptional editing. Proc. Natl. Acad. Sci. U. S. A. 93:3602–3607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hensley LE, Mulangu S, Asiedu C, Johnson J, Honko AN, Stanley D, Fabozzi G, Nichol ST, Ksiazek TG, Rollin PE, Wahl-Jensen V, Bailey M, Jahrling PB, Roederer M, Koup RA, Sullivan NJ. 2010. Demonstration of cross-protective vaccine immunity against an emerging pathogenic Ebolavirus species. PLoS Pathog. 6:e1000904 doi:10.1371/journal.ppat.1000904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Falzarano D, Feldmann F, Grolla A, Leung A, Ebihara H, Strong JE, Marzi A, Takada A, Jones S, Gren J, Geisbert J, Jones SM, Geisbert TW, Feldmann H. 2011. Single immunization with a monovalent vesicular stomatitis virus-based vaccine protects nonhuman primates against heterologous challenge with Bundibugyo ebolavirus. J. Infect. Dis. 204(Suppl 3):S1082–S1089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Weaver SC. 2005. Host range, amplification, and arboviral disease emergence. Arch. Virol. 2005(Suppl):33–44 [DOI] [PubMed] [Google Scholar]
- 49. Weaver SC, Ferro C, Barrera R, Boshell J, Navarro JC. 2004. Venezuelan equine encephalitis. Annu. Rev. Entomol. 49:141–174 [DOI] [PubMed] [Google Scholar]