Abstract
Objective
To examine the trends in rates of endoscopic sinus surgery, open sinus procedures (open sinus surgery), and the prevalence of diagnosis of chronic rhinosinusitis in the Medicare population from 1998 to 2006.
Design
Retrospective cohort analysis.
Patients
Twenty-percent sample of Medicare beneficiaries aged 65 to 99 years for the years 1998 to 2006.
Main Outcome Measures
Change in per capita annual rates of endoscopic sinus surgery, open sinus surgery, and chronic rhinosinusitis diagnosis among Medicare beneficiaries.
Results
From 1998 to 2006, the rate of patients undergoing endoscopic sinus surgery per 1000 Medicare beneficiaries increased by 20%, from 0.72 (95% confidence interval [CI], 0.70-0.74) to 0.92 (95% CI, 0.89-0.95). Over the same period, the rate of open sinus surgery declined 40%, from 0.20 (95% CI, 0.19-0.21) to 0.11 (95% CI, 0.10-0.12). However, the per capita rate of beneficiaries diagnosed as having chronic rhinosinusitis declined by 1.4% over the study period. Further analysis by age cohort revealed significantly higher rates of surgery and diagnosis rates in the 65- to 69-year-old beneficiaries relative to older age groups. Over the study period, the per capita rate of diagnosis of chronic rhinosinusitis declined or remained stable across age groups. Despite this, all age groups showed increases in endoscopic sinus surgery rates.
Conclusions
Our findings indicate that endoscopic sinus surgery is increasingly becoming the mainstay of chronic rhinosinusitis management in the Medicare population. Because of the uncertainty regarding the outcomes of surgical vs medical management, the root causes of the observed increase in endoscopic sinus surgery rates need to be investigated. Given that sinusitis is a common diagnosis necessitating physician visits, comparative effectiveness studies examining medical vs surgical management would be warranted.
Chronic Rhinosinusitis is a medical disorder characterized by infection and inflammation of the paranasal sinus cavities and the nose. Patients with chronic rhinosinusitis often have symptoms of congestion, rhinorrhea, headache, facial pressure, and anosmia. Chronic rhinosinusitis is differentiated from acute sinusitis by duration of symptoms longer than 3 months.1 Both conditions—acute and chronic sinusitis— are leading reasons for physician visits. Mainstays of medical management for sinusitis include antibiotic therapy, systemic and topical intranasal steroids, and nasal saline irrigations.2 A subset of patients with chronic rhinosinusitis in whom medical management fails undergo surgery, sometimes repeatedly, for treatment of their disease. Since its introduction in 1985 in the United States, a minimally invasive endonasal technique (endoscopic sinus surgery) has reduced the impact of this procedure and has essentially supplanted open approaches (open sinus surgery).3
While endoscopic sinus surgery has emerged as a viable option in the management of chronic rhinosinusitis, evidence directly comparing its effectiveness with medical management suggests that surgery and long-term medical management may lead to comparable outcomes.4 Furthermore, in other clinical settings where clinical benefits are uncertain and minimally invasive surgical approaches have replaced open operations, total procedural volumes have invariably increased.5 The purpose of this study was to determine whether a similar phenomenon exists in the context of sinus surgery.
We undertook a retrospective study to determine national trends in the rates of endoscopic and open sinus surgery in the Medicare population between the years 1998 and 2006. In addition, we determined trends in the diagnosis of chronic rhinosinusitis to assess whether changes in surgery rates paralleled changes in diagnosis rates.
Methods
This study is a retrospective cohort study designed to assess trends in rates of chronic rhinosinusitis diagnoses and rates of sinus surgery procedures performed to treat chronic rhinosinusitis. We used a 20% sample of non-HMO Medicare beneficiaries aged 65 to 99 years from January 1, 1998, to December 31, 2006, to identify patients diagnosed as having chronic sinusitis and patients undergoing endoscopic or open sinus surgery. The data are provided by the Centers for Medicare and Medicaid Services to The Dartmouth Institute for Health Policy and Clinical Practice. A truly random 20% sample was generated by choosing beneficiaries whose last digit of their social security number ended in a 0 or 5. Clinician claims with Current Procedural Terminology (CPT) and International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes, date of procedure, and the race and ethnicity of the beneficiary were identified from the physician and supplier file. The denominator file provided information about age, sex, race and ethnicity, and eligibility by year for the Medicare Part B program.
We measured the incidence of CPT codes for the various endoscopic and open sinus surgery procedures (Table 1). To capture patients diagnosed as having chronic rhinosinusitis, we identified beneficiaries with an ICD-9 code for chronic rhinosinusitis during the year. We excluded patients with ICD-9 codes for nasal tumors (benign or malignant) to ensure that the surgical procedures were performed for chronic rhinosinusitis and not for endonasal tumors.
Table 1. Inclusion Diagnostic ICD-9 Codes for Chronic Rhinosinusitis and CPT Codes for Endoscopic and Open Sinus Surgery.
| Diagnostic Code | Description |
|---|---|
| ICD-9 | |
| 471 | Polyp nasal cavity |
| 471.1 | Polypoid sinus degeneration |
| 471.8 | Other polyp of sinus |
| 472 | Chronic rhinitis |
| 473 | Chronic maxillary sinusitis |
| 473.1 | Chronic frontal sinusitis |
| 473.2 | Chronic ethmoid sinusitis |
| 473.3 | Chronic sphenoid sinusitis |
| 473.8 | Pansinusitis |
| 473.9 | Unspecified chronic sinusitis |
| CPT–endoscopic surgery | |
| 31237 | Endoscopic polypectomy and biopsy |
| 31240 | Endoscopic concha bullosa resection |
| 31254 | Endoscopic partial ethmoidectomy |
| 31255 | Endoscopic total ethmoidectomy |
| 31256 | Endoscopic maxillary antrostomy |
| 31267 | Endoscopic maxillary antrostomy with tissue removal |
| 31276 | Endoscopic frontal sinusotomy |
| 31287 | Endoscopic sphenoidotomy |
| 31288 | Endoscopic sphenoidotomy with tissue removal |
| CPT–open surgery | |
| 31000 | Lavage and cannulation of maxillary sinus |
| 31002 | Lavage and cannulation of sphenoid sinus |
| 31020 | Sinusotomy maxillary; intranasal |
| 31084 | Sinusotomy frontal; obliteration with brow flap |
| 31085 | Sinusotomy frontal; obliteration with coronal flap |
| 31086 | Sinusotomy frontal; nonobliteration with brow flap |
| 31087 | Sinusotomy frontal; nonobliteration with coronal flap |
| 31090 | Sinusotomy unilateral, 3 or more |
| 31200 | Ethmoidectomy; intranasal, anterior |
| 31201 | Ethmoidectomy; intranasal, total |
| 31205 | Ethmoidectomy; extranasal, total |
Abbreviations: CPT, Current Procedural Terminology; ICD-9, International Classification of Diseases, Ninth Revision.
Per capita rates of chronic rhinosinusitis diagnosis were calculated by using the number of beneficiaries diagnosed as having chronic rhinosinusitis as the numerator and the number of beneficiaries as the denominator. We determined both the number of procedures per beneficiary as well as the number of beneficiaries undergoing sinus procedures. Per capita rates of surgical procedures (endoscopic sinus surgery and open sinus surgery) were analyzed by using procedure and patient counts and the denominator patient identification files. Statistical analyses were performed using commercially available software (STATA; StataCorp, College Station, Texas).
Results
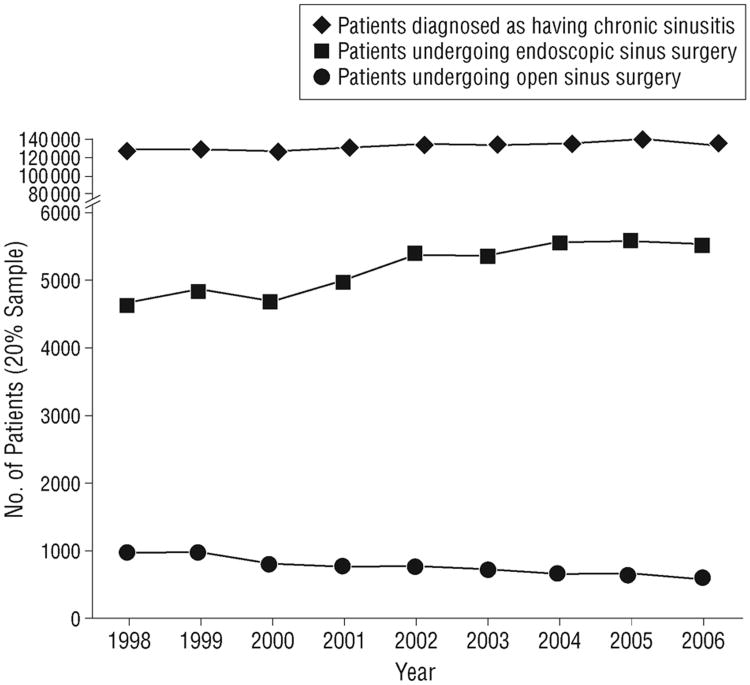
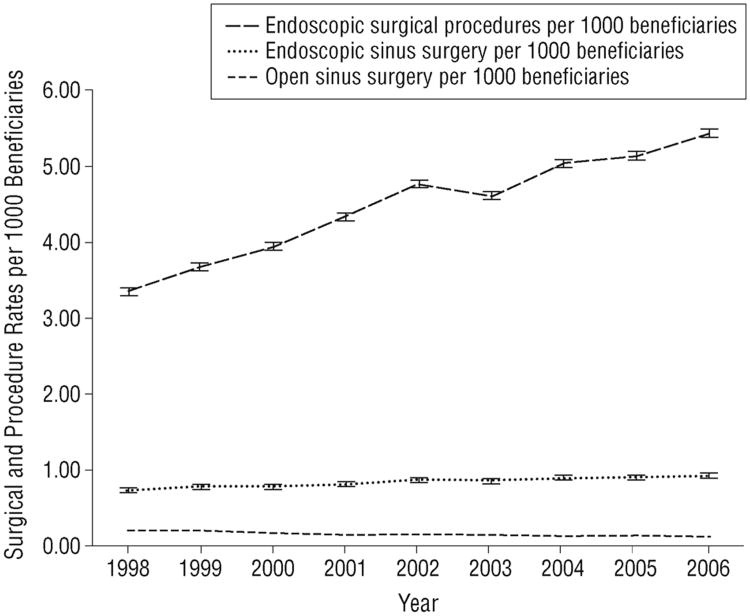
In the Medicare 20% sample during the period 1998 to 2006, the number of patients undergoing endoscopic sinus surgery increased 34.4%, from 3670 to 4932 per year, and the number of patients undergoing open sinus surgery declined 40.5%, from 992 to 590 per year. The number of patients diagnosed as having chronic sinusitis increased from 128 771 to 134 023—an increase of 4.1% (Figure 1). The per capita rate (per 1000 beneficiaries) of endoscopic surgery increased 19%, from 0.72 (95% confidence interval [CI], 0.70-0.74) to 0.92 (95% CI, 0.89-0.95), and the per capita rates of open surgery declined by 40%, from 0.20 (95% CI, 0.19-0.21) to 0.11 (95% CI, 0.10-0.12). The per capita rates of endoscopic surgical procedures (numbers of surgical CPTs) increased by 63%, from 3.34 (95% CI, 3.29-3.39) to 5.43 (95% CI, 5.38-5.48) per 1000 beneficiaries, indicating an unbundling effect: not only did the number of patients undergoing endoscopic sinus surgery increase, each patient underwent more procedures on average (Figure 2). As a percentage, the rate of decline in open sinus surgery was greater; however, the base per capita rate of endoscopic sinus surgery was higher, thereby increasing the total number of patients undergoing sinus surgery by 18.5%. This suggests that the increase in endoscopic sinus surgery was not merely a replacement for open surgery.
Figure 1.
Numbers of patients diagnosed as having chronic rhinosinusitis and undergoing endoscopic and open sinus surgery from a 20% sample of Medicare beneficiaries.
Figure 2.
Per capita rates of endoscopic surgical procedures, endoscopic sinus surgery, and open sinus surgery in the Medicare population. Error bars represent 95% confidence intervals.
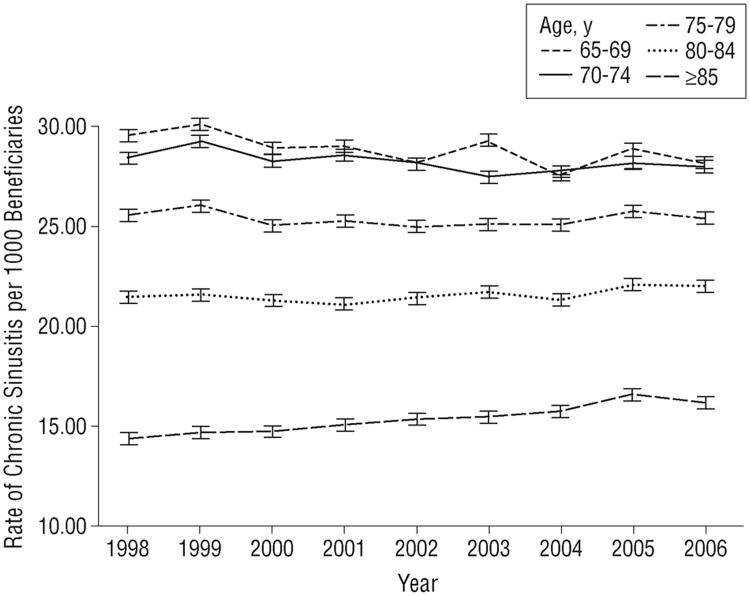
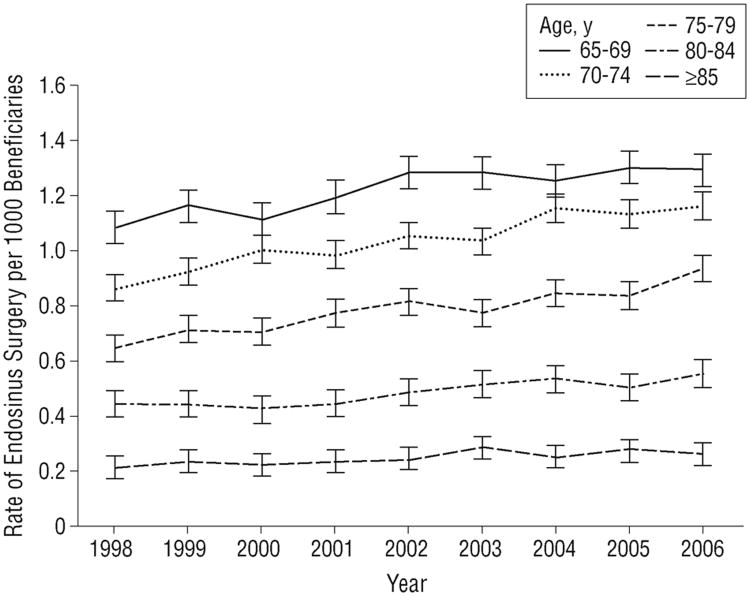
We compared trends in rates of chronic rhinosinusitis diagnosis and endoscopic sinus surgery across age categories. The per capita rate of chronic rhinosinusitis diagnosis was highest in the 65- to 69-year age group (Figure 3). The trend in diagnosis rates in all age cohorts was stable between 1998 and 2006. Despite the overall decline in rates of diagnosis, there were increases in the endoscopic sinus surgery rates in all age groups (Figure 4). Similar to chronic rhinosinusitis diagnosis trends, per capita rates of endoscopic sinus surgery were much higher in the 65- to 69-year age cohort relative to the older age groups: 1.08 (95% CI, 1.02-1.14) vs 0.21 (95% CI, 0.17-0.25) in 1998, our index year.
Figure 3.
Per capita rates of chronic rhinosinusitis diagnosis by age cohort in the Medicare population. Error bars represent 95% confidence intervals.
Figure 4.
Per capita rates of endoscopic sinus surgery by age cohort in the Medicare population. Error bars represent 95% confidence intervals.
To address the possibility that this was a population effect based on the increasing number of beneficiaries, we determined the changes in the Medicare beneficiary population. The number of Medicare beneficiaries increased by 5%; in our sample, the number of patients diagnosed as having chronic rhinosinusitis increased by 4.1% (Table 2), leading to a decline of 1.4% in the rate of chronic rhinosinusitis diagnosis. We assessed the rate of endoscopic sinus surgery and open sinus surgery per beneficiary diagnosed as having chronic rhinosinusitis. Between 1998 and 2006, endoscopic sinus surgery rates per thousand beneficiaries diagnosed as having chronic rhinosinusitis increased from 28.5 (95% CI, 27.57-29.39) to 36.8 (95% CI, 35.83-37.85) and open sinus surgery rates per thousand declined from 7.7 (95% CI, 7.26-8.22) to 4.4 (95% CI, 4.03-4.73) (Table 2). Given the divergent rates of diagnosis and surgery rates, our findings imply that endoscopic sinus surgery was increasingly performed in patients with chronic rhinosinusitis among Medicare beneficiaries.
Table 2. Changes in the Per Capita Rates of Endoscopic Sinus Surgery and Open Sinus Surgery Among Beneficiaries Diagnosed as Having Chronic Rhinosinusitis.
| Year | Patients With Chronic Rhinosinusitis (20% Sample) | Chronic Rhinosinusitis Diagnosis per 1000 Beneficiaries (95% CI) | Patients Undergoing Endoscopic Sinus Surgery per 1000 Beneficiaries Diagnosed as Having Chronic Rhinosinusitis (95% CI) | Patients Undergoing Open Sinus Surgery per 1000 Beneficiaries Diagnosed as Having Chronic Rhinosinusitis (95% CI) |
|---|---|---|---|---|
| 1998 | 128778 | 25.2 (25.04-25.32) | 28.5 (27.57-29.39) | 7.7 (7.26-8.22) |
| 2006 | 134023 | 24.8 (24.69-24.95) | 36.8 (35.83-37.85) | 4.4 (4.03-4.73) |
| Change, % | 4.1 | −0.14 | 29.1 | −42.8 |
Abbreviation: CI, confidence interval.
Comment
During the period 1998 to 2006, the rates of endoscopic sinus surgery increased considerably in Medicare beneficiaries. Despite the increase in the number of patients undergoing endoscopic sinus surgery, the per capita rate of patients diagnosed as having chronic rhinosinusitis among Medicare beneficiaries overall was essentially unchanged during our study period. As minimally invasive techniques are introduced, rates of use of these procedures typically increase as patients and surgeons choose treatments that cause less morbidity and appear to be safer. A recent example of this trend is the use of percutaneous coronary intervention to treat coronary artery disease as a replacement for conventional cardiac bypass surgery. Studies by other members of our group have indicated similar phenomena in laparoscopic antireflux surgery5,6 and carotid endovascular procedures.7 When comparing open with endovascular techniques in carotid surgery, the authors found an overall stable rate of surgical procedures but increasing numbers of endovascular approaches, indicating a substitution phenomenon. This was not the case with our study, in which the increase in overall surgical rates was caused primarily by significant increases in endoscopic sinus surgery rates, while the rates of chronic rhinosinusitis diagnosis were stable. Unlike endoscopic sinus surgery, carotid surgery has clear, established guidelines for surgical intervention, based on large randomized studies. When clear evidence is lacking regarding benefits of one therapeutic intervention vs another, there is inherent variation as people choose the less invasive procedural “cure.”
Detection biases and the preference sensitive nature of chronic rhinosinusitis management likely contribute to the apparent increase in endoscopic sinus surgery rates. Our technical ability to detect minimal amounts of sinus disease with computed tomographic scanning, which correlate very poorly with symptoms,8,9 leads to a detection bias.10 Advances in radiologic diagnosis have outpaced our knowledge of the clinical effectiveness of surgical intervention vs continued medical management and our understanding of the natural history of the disease. In addition, chronic rhinosinusitis and sinus surgery in particular is an exemplar of preference sensitive care, in which surgical decision making is driven by patient or physician preferences rather than clearly defined, evidence-based indications. Unfortunately, the medical management of chronic rhinosinusitis is very inconsistent. For example, types of antibiotics, use of systemic steroids, and duration of therapy are highly variable.11-13 Consultation with an otolaryngologist is likely to bias the management decision toward surgical intervention. With advances in optics, intraoperative image guidance, and use of powered instrumentation, endoscopic sinus surgery is now routinely performed safely in an outpatient setting with minimal postoperative pain, in contrast to open approaches, which involve significantly greater pain, blood loss, and often inpatient stays. This may make the decision for surgery a more palatable option for both surgeons and patients and lower the threshold for surgical intervention. Nonetheless, greater evidence of the effectiveness of these procedures, as well as its intersection with patient preferences, is warranted.
One possible limitation of this analysis is whether Medicare beneficiaries are an appropriate population to study, given that chronic rhinosinusitis is more common in the young. As a comparison, we examined data from the Vital Health Statistics surveys done in 1997 and 2007.14,15 Office visits for sinusitis were significantly more common in the 65 year and younger population in both 1997 (27.1 million vs 4.6 million) and 2007 (21.4 million vs 4.5 million). This implies that our findings may underestimate overall national trends. Our study further suggests that growth in endoscopic sinus surgery reflects a shift from medical to surgical treatment. Second, although we did not include patients with diagnoses of benign or malignant nasal tumors, there may have been a small overlap in diagnoses. Therefore, patients with chronic rhinosinusitis could have been overrepresented in our sample. Despite this possibility, the overall rate of chronic rhinosinusitis diagnosis was essentially unchanged in our study period. Another limitation of our study is the difficulty in detecting disease recurrence and revision surgery, since CPT codes for primary and revision surgical procedures are the same. However, in either case the notable increases in endoscopic sinus surgery rates still raises questions regarding the appropriate role of surgery in the management of rhinosinusitis.
Endoscopic sinus surgery has been a revolutionary technology and has the potential to improve the poor quality of life of patients with rhinosinusitis16,17 with markedly less morbidity relative to open approaches. Despite these increases in rates of use, the possibility exists that sinus surgery was not offered as frequently as an option for management of chronic rhinosinusitis prior to introduction of endoscopic techniques leading to chronically poor quality of life for these patients. In the absence of longitudinal long-term outcome studies in this population, the appropriate rate of endoscopic sinus surgery remains unknown. As a next step, we are assessing regional variation nationwide in endoscopic sinus surgery rates, with the overall aim of estimating potential cost savings by comparing high-usage vs low-usage areas. We are also interested in the intersection of patient preferences and surgical decision making, and in this regard are investigating the cost-effectiveness of sinus surgery relative to medical management. As a first step, however, we would propose increasing shared decision making to educate patients about the complex nature of chronic rhinosinusitis, the potential benefits and adverse effects of the various treatment options, and persistent uncertainty regarding the role of surgery in the management of this common disease.
Acknowledgments
Funding/Support: Dr Venkatraman has received a Harmes Surgical Scholar Award, Dartmouth Hitchcock Medical Center (2007). David Goodman receives funding support from the Robert Wood Johnson Foundation and the National Institute on Aging (grant PO1 AG19783).
Footnotes
Author Contributions: Dr Venkatraman and Mr Zhou had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Venkatraman, Likosky, Finlayson, and Goodman. Acquisition of data: Zhou. Analysis and interpretation of data: Venkatraman, Likosky, Zhou, Finlayson, and Goodman. Drafting of the manuscript: Venkatraman and Likosky. Critical revision of the manuscript for important intellectual content: Venkatraman, Likosky, Zhou, Finlayson, and Goodman. Statistical analysis: Zhou and Goodman. Obtained funding: Venkatraman and Finlayson. Administrative, technical, and material support: Finlayson and Goodman. Study supervision: Finlayson.
Financial Disclosure: None reported.
References
- 1.Benninger MS, Ferguson BJ, Hadley JA, et al. Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol Head Neck Surg. 2003;129(3(suppl)):S1–S32. doi: 10.1016/s0194-5998(03)01397-4. [DOI] [PubMed] [Google Scholar]
- 2.Chan Y, Kuhn FA. An update on the classifications, diagnosis, and treatment of rhinosinusitis. Curr Opin Otolaryngol Head Neck Surg. 2009;17(3):204–208. doi: 10.1097/MOO.0b013e32832ac393. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy DW, Zinreich SJ, Rosenbaum AE, Johns ME. Functional endoscopic sinus surgery: theory and diagnostic evaluation. Arch Otolaryngol. 1985;111(9):576–582. doi: 10.1001/archotol.1985.00800110054002. [DOI] [PubMed] [Google Scholar]
- 4.Khalil HS, Nunez DA. Functional endoscopic sinus surgery for chronic rhinosinusitis. Cochrane Database Syst Rev. 2006;3:CD004458. doi: 10.1002/14651858.CD004458.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Finlayson SR, Birkmeyer JD, Laycock WS. Trends in surgery for gastroesophageal reflux disease: the effect of laparoscopic surgery on utilization. Surgery. 2003;133(2):147–153. doi: 10.1067/msy.2003.13. [DOI] [PubMed] [Google Scholar]
- 6.Finlayson SR, Laycock WS, Birkmeyer JD. National trends in utilization and outcomes of antireflux surgery. Surg Endosc. 2003;17(6):864–867. doi: 10.1007/s00464-002-8965-9. [DOI] [PubMed] [Google Scholar]
- 7.Goodney PP, Lucas FL, Likosky DS, Malenka DJ, Fisher ES. Changes in the use of carotid revascularization among the Medicare population. Arch Surg. 2008;143(2):170–173. doi: 10.1001/archsurg.2007.43. [DOI] [PubMed] [Google Scholar]
- 8.Stewart MG, Sicard MW, Piccirillo JF, Diaz-Marchan PJ. Severity staging in chronic sinusitis: are CT scan findings related to patient symptoms? Am J Rhinol. 1999;13(3):161–167. doi: 10.2500/105065899781389704. [DOI] [PubMed] [Google Scholar]
- 9.Bhattacharyya T, Piccirillo J, Wippold FJ., II Relationship between patient-based descriptions of sinusitis and paranasal sinus computed tomographic findings. Arch Otolaryngol Head Neck Surg. 1997;123(11):1189–1192. doi: 10.1001/archotol.1997.01900110039006. [DOI] [PubMed] [Google Scholar]
- 10.Black WC, Welch HG. Advances in diagnostic imaging and overestimations of disease prevalence and the benefits of therapy. N Engl J Med. 1993;328(17):1237–1243. doi: 10.1056/NEJM199304293281706. [DOI] [PubMed] [Google Scholar]
- 11.Dubin MG, Liu C, Lin SY, Senior BA. American rhinologic society member survey on “maximal medical therapy” for chronic rhinosinusitis. Am J Rhinol. 2007;21(4):483–488. doi: 10.2500/ajr.2007.21.3047. [DOI] [PubMed] [Google Scholar]
- 12.Dubin MG, Kuhn FA, Melroy CT. Radiographic resolution of chronic rhinosinusitis without polyposis after 6 weeks vs 3 weeks of oral antibiotics. Ann Allergy Asthma Immunol. 2007;98(1):32–35. doi: 10.1016/S1081-1206(10)60856-3. [DOI] [PubMed] [Google Scholar]
- 13.Subramanian HN, Schechtman KB, Hamilos DL. A retrospective analysis of treatment outcomes and time to relapse after intensive medical treatment for chronic sinusitis. Am J Rhinol. 2002;16(6):303–312. [PubMed] [Google Scholar]
- 14.Blackwell DL, Collins JG, Coles R. Summary health statistics for US adults: National health interview survey, 1997. Vital Health Stat 10. 2002;(205):1–109. [PubMed] [Google Scholar]
- 15.Pleis JR, Lethbridge-Cejku M. Summary health statistics for US adults: National Health Interview Survey, 2006. Vital Health Stat 10. 2007;(235):1–153. [PubMed] [Google Scholar]
- 16.Gliklich RE, Metson R. The health impact of chronic sinusitis in patients seeking otolaryngologic care. Otolaryngol Head Neck Surg. 1995;113(1):104–109. doi: 10.1016/S0194-59989570152-4. [DOI] [PubMed] [Google Scholar]
- 17.Gliklich RE, Metson R. Effect of sinus surgery on quality of life. Otolaryngol Head Neck Surg. 1997;117(1):12–17. doi: 10.1016/S0194-59989770199-2. [DOI] [PubMed] [Google Scholar]