Abstract
Chronic traumatic encephalopathy is a progressive tauopathy that occurs as a consequence of repetitive mild traumatic brain injury. We analysed post-mortem brains obtained from a cohort of 85 subjects with histories of repetitive mild traumatic brain injury and found evidence of chronic traumatic encephalopathy in 68 subjects: all males, ranging in age from 17 to 98 years (mean 59.5 years), including 64 athletes, 21 military veterans (86% of whom were also athletes) and one individual who engaged in self-injurious head banging behaviour. Eighteen age- and gender-matched individuals without a history of repetitive mild traumatic brain injury served as control subjects. In chronic traumatic encephalopathy, the spectrum of hyperphosphorylated tau pathology ranged in severity from focal perivascular epicentres of neurofibrillary tangles in the frontal neocortex to severe tauopathy affecting widespread brain regions, including the medial temporal lobe, thereby allowing a progressive staging of pathology from stages I–IV. Multifocal axonal varicosities and axonal loss were found in deep cortex and subcortical white matter at all stages of chronic traumatic encephalopathy. TAR DNA-binding protein 43 immunoreactive inclusions and neurites were also found in 85% of cases, ranging from focal pathology in stages I–III to widespread inclusions and neurites in stage IV. Symptoms in stage I chronic traumatic encephalopathy included headache and loss of attention and concentration. Additional symptoms in stage II included depression, explosivity and short-term memory loss. In stage III, executive dysfunction and cognitive impairment were found, and in stage IV, dementia, word-finding difficulty and aggression were characteristic. Data on athletic exposure were available for 34 American football players; the stage of chronic traumatic encephalopathy correlated with increased duration of football play, survival after football and age at death. Chronic traumatic encephalopathy was the sole diagnosis in 43 cases (63%); eight were also diagnosed with motor neuron disease (12%), seven with Alzheimer’s disease (11%), 11 with Lewy body disease (16%) and four with frontotemporal lobar degeneration (6%). There is an ordered and predictable progression of hyperphosphorylated tau abnormalities through the nervous system in chronic traumatic encephalopathy that occurs in conjunction with widespread axonal disruption and loss. The frequent association of chronic traumatic encephalopathy with other neurodegenerative disorders suggests that repetitive brain trauma and hyperphosphorylated tau protein deposition promote the accumulation of other abnormally aggregated proteins including TAR DNA-binding protein 43, amyloid beta protein and alpha-synuclein.
Keywords: axonal injury, brain trauma, frontotemporal lobar degeneration, neurodegenerative disorders, traumatic brain injury
Introduction
Repetitive mild traumatic brain injury can trigger the development of chronic traumatic encephalopathy (CTE), a progressive neurodegeneration characterized by the widespread deposition of hyperphosphorylated tau (p-tau) as neurofibrillary tangles (Corsellis and Brierley, 1959; Corsellis et al., 1973, Hof et al., 1991; Geddes et al., 1999; Omalu et al., 2005, 2006, 2010; McKee et al., 2009, 2010; Gavett et al., 2010, 2011; Daneshvar et al., 2011a, b; Costanza et al., 2011; Stern et al., 2011; Goldstein et al., 2012; Saing et al., 2012). CTE was originally reported in 1928 by Harrison Martland, a New Jersey pathologist, who described the clinical aspects of a progressive neurological deterioration (‘punch drunk’) that occurred after repetitive brain trauma in boxers (Martland, 1928). Although originally termed ‘dementia pugilistica’ (Millspaugh, 1937), the recognition that activities other than boxing were associated with its development lead to the preferred use of terms such as progressive traumatic encephalopathy and later, CTE (Critchley, 1949; 1957).
CTE is clinically associated with symptoms of irritability, impulsivity, aggression, depression, short-term memory loss and heightened suicidality that usually begin 8–10 years after experiencing repetitive mild traumatic brain injury (McKee et al., 2009). With advancing disease, more severe neurological changes develop that include dementia, gait and speech abnormalities and parkinsonism. In late stages, CTE may be clinically mistaken for Alzheimer’s disease or frontotemporal dementia (Gavett et al., 2010, 2011). A subset of cases with CTE is associated with motor neuron disease (MND) (McKee et al., 2010).
The neuropathological changes of CTE are distinctive and easily distinguished from other tauopathies, including Alzheimer’s disease. The neuropathological features of CTE include generalized atrophy of the cerebral cortex, medial temporal lobe, diencephalon and mammillary bodies with enlarged ventricles; cavum septum pellucidum, often with fenestrations; extensive p-tau-immunoreactive neurofibrillary tangles and astrocytic tangles in the frontal and temporal cortices, particularly around small cerebral vessels and at the depths of cerebral sulci; extensive p-tau-immunoreactive neurofibrillary tangles in limbic regions, diencephalon and brainstem nuclei; extensive degeneration of axons and white matter fibre bundles; TAR DNA-binding protein 43 (TDP-43) immunoreactive intraneuronal and intraglial inclusions and neurites in most cases and a relative absence of amyloid-β peptide deposits (Corsellis and Brierley, 1959; Corsellis et al., 1973; Hof et al., 1991; Geddes et al., 1999; Omalu et al., 2005, 2006, 2010; McKee et al., 2009, 2010; Gavett et al., 2010, 2011; Daneshvar et al., 2011a, b; Costanza et al., 2011; Stern et al., 2011; Goldstein et al., 2012; Saing et al., 2012).
In 2008, the Center for the Study of Traumatic Encephalopathy (CSTE) at Boston University School of Medicine established the CSTE brain bank at the Bedford VA Hospital to analyse the brain and spinal cords after death of athletes, military veterans and civilians who experienced repetitive mild traumatic brain injury. Through this effort, we comprehensively analysed the brain and spinal cord of 85 donors for evidence of CTE, as well as for all other neurodegenerative diseases, including Alzheimer’s disease, frontotemporal lobar degeneration (FTLD), Parkinson’s disease, Lewy body disease and multiple system atrophy. We report the spectrum of CTE and neurodegenerative pathology found in the brain and spinal cord of these donors, compare the pathological findings with 18 cognitively normal age- and gender-matched control subjects without known history of mild traumatic brain injury, and correlate the clinical findings to the neuroanatomical regions of p-tau pathology. Although a brain donation study and autopsy directed case series will never establish the incidence or prevalence of a disorder such as CTE owing to ascertainment biases, systematic clinicopathological analysis allows insight into the spectrum of clinical and neuropathological alterations associated with the disorder and lays the foundation for future prospective longitudinal studies.
Materials and methods
Subjects
A total of 85 brains from former athletes, military veterans or civilians with a history of repetitive mild traumatic brain injury were comprehensively evaluated. Eighteen additional brains from cognitively intact individuals without history of mild traumatic brain injury were obtained from the Boston University Alzheimer’s Disease Center Brain Bank that included some subjects from the Framingham Heart Study. Next of kin provided written consent for participation and brain donation. Institutional review board approval for brain donation was obtained through the Boston University Alzheimer’s Disease Center, CSTE and the Bedford VA Hospital. Institutional review board approval for post-mortem clinical record review, interviews with family members and neuropathological evaluation was obtained through Boston University School of Medicine.
Clinical assessment
Concussion and mild traumatic brain injury history, history of cognitive and behavioural changes and clinical status leading up to death were determined through post-mortem interviews with next of kin performed by a neuropsychologist (R.A.S.) who was blind to the results of the neuropathological examination at the time of interview. Informants were interviewed before receiving the results of the neuropathological examination. The interview was semi-structured and conducted by telephone. Areas queried included demographics, athletic history, military service, concussion and brain trauma history, medical history (including neurological, psychiatric and substance use), family history, social/occupational history, and reported/observed changes in mood, behaviour, motor functions, cognition and activities of daily living. To semi-quantify cognitive, mood and functional changes, modifications of standard measures/interviews were administered to the informant to assess their perception of the subject in the months or years before death (Pfeffer et al., 1982; McNair et al., 1984; Brown and Schinka, 2005; Galvin et al., 2005). Medical record review was also performed (R.A.S. and A.C.M.).
In analysis of the clinical symptoms associated with CTE, case selection was restricted to those cases with post-mortem semi-structured family interviews and pathological diagnosis of CTE or CTE plus MND (CTE-MND), without other co-morbidities.
Duration of exposure to American football and position played
To examine the relationship between exposure and stage of CTE, analyses were performed on the subset of athletes who played American football. Only football played at the high school level or higher was considered for these analyses. Of the 85 brain donors, 58 played American football as their primary sport. Of those, 16 subjects were excluded owing to comorbid disease (Alzheimer’s disease, Parkinson’s disease, Lewy body disease, FTLD and multiple system atrophy), and seven were excluded owing to incomplete athletic information. Football players were also grouped by primary position played: offensive and defensive linemen, quarterbacks, wide receivers, all other offensive backs, defensive linebackers and defensive backs.
Neuropathological examination
The neuropathological processing followed the procedures previously established for the Boston University Alzheimer’s Disease Center Brain Bank (Vonsattel et al., 1995). Paraffin-embedded sections were stained with Luxol fast blue, haematoxylin and eosin, Bielschowsky’s silver, AT8, alpha-synuclein, amyloid-ß, TDP-43, phosphorylated TDP-43 (pTDP-43), SMI-31 and SMI-34 using methods described previously (McKee et al., 2009). In addition, multiple large coronal slabs of the cerebral hemispheres were cut at 50 µm on a sledge microtome and stained as free-floating sections using AT8, amyloid-ß, TDP-43, pTDP-43, CP13 and PHF-1 (McKee et al., 2009, 2010) (Supplementary Table 1). Neuropathological diagnoses were made without any knowledge of the subjects’ clinical histories (A.C.M.) and confirmed by two other neuropathologists (T.D.S. and V.E.A.).
Neuropathological diagnoses
Definition of chronic traumatic encephalopathy
Based on our previous studies and review of the literature on CTE (Corsellis et al., 1973; Hof et al., 1991; Geddes et al., 1999; Omalu et al., 2005, 2006, 2010; McKee et al., 2009, 2010; Goldstein et al., 2012; Saing et al., 2012), the diagnosis of CTE was defined by the presence of the following criteria (Table 1 and Figs. 1 and 2): (i) perivascular foci of p-tau immunoreactive astrocytic tangles and neurofibrillary tangles; (ii) irregular cortical distribution of p-tau immunoreactive neurofibrillary tangles and astrocytic tangles with a predilection for the depth of cerebral sulci; (iii) clusters of subpial and periventricular astrocytic tangles in the cerebral cortex, diencephalon, basal ganglia and brainstem; and (iv) neurofibrillary tangles in the cerebral cortex located preferentially in the superficial layers.
Table 1.
Distinctions in hyperphosphorylated tau pathology between Alzheimer’s disease and CTE
| Pathological features | Alzheimer’s disease | CTE |
|---|---|---|
| Tau protein | ||
| Six isoforms | All six isoforms present | All six isoforms presenta |
| 3 or 4 repeat tau | 3 repeat and 4 repeat tau present | 3 repeat and 4 repeat tau present |
| Cell origin | ||
| Neuronal | NFTs and pre-tangles | NFTs and pre-tangles |
| Astrocytic | Not presentb | Prominent astrocytic tangles |
| Neuronal domain | ||
| Cell body | Prominent | Prominent |
| Dendrite | Prominent | Prominent |
| Axon | Sparse | Prominent |
| Cell Pattern | ||
| Perivascular | Not present | Prominent NFTs and astrocytic tangles |
| Foci at depths of cerebral sulci | Not present | Prominent NFTs and astrocytic tangles |
| Irregular, patchy cortical distribution | Not present | Prominent |
| Cortical laminae | NFTs predominantly in laminae III and V | NFTs predominantly in laminae II–III |
| Subpial astrocytic tangles | Not present | Prominent |
| Periventricular astrocytic tangles | Not present | Present |
| Distribution | ||
| Mild pathology | Braak stages I–III: | CTE stages I–II: |
| NFTs in entorhinal cortex, amygdala and hippocampus | NFTs in focal epicentres in cerebral cortex, usually frontal lobe | |
| Advanced pathology | Braak stages IV–VI: | CTE stages III–IV: |
| High density of NFTs in widespread cortical areas and medial temporal lobe, uniform distribution | High density of NFTs in widespread cortical areas and medial temporal lobe, patchy irregular distribution | |
| Low densities of NFTs in basal ganglia and brainstem; none in mammillary bodies. White matter tracts relatively uninvolved. | High densities of NFTs in thalamus, hypothalamus, mammillary bodies, brainstem. Moderate densities of NFTs in basal ganglia, especially nucleus accumbens. Prominent p-tau pathology in white matter tracts. |
b Low densities of 4R immunoreactive ‘thorn-shaped astrocytes’ are found in the temporal lobe of some older subjects and older subjects with Alzheimer’s disease (Lace et al., 2012; López-González et al., 2012).
NFT = neurofibrillary tangles.
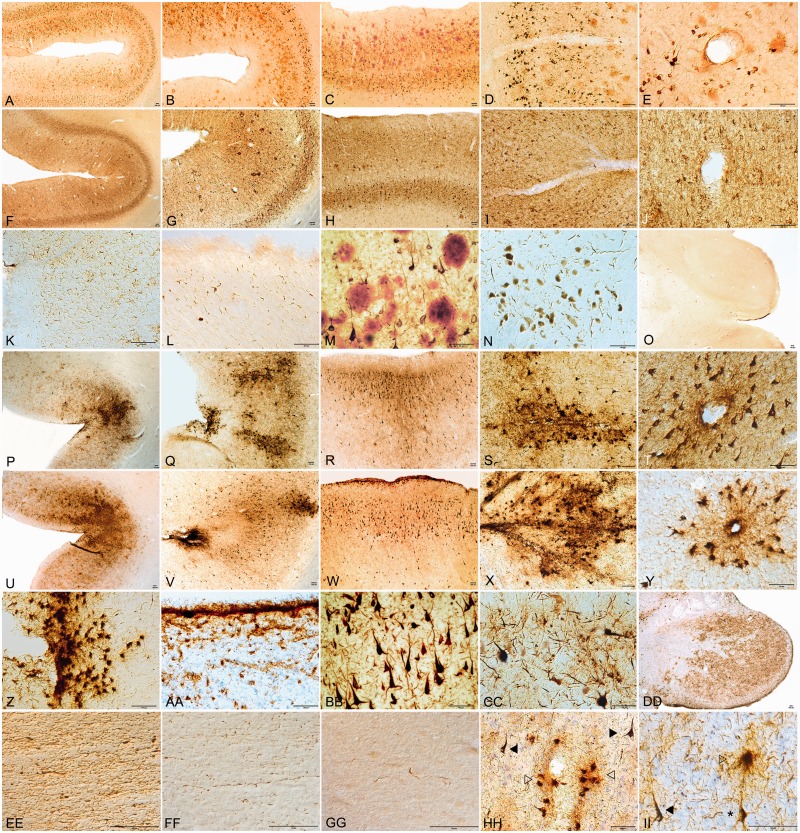
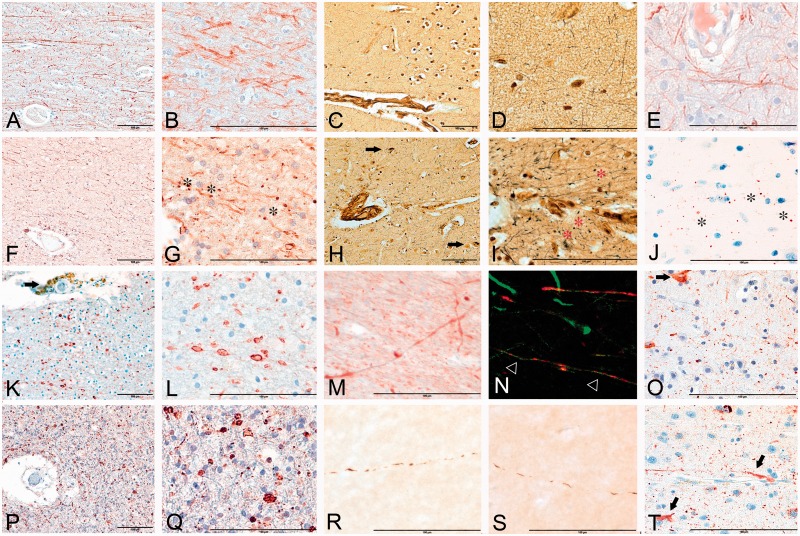
Figure 1.
Distinctive p-tau pathology of CTE compared with Alzheimer’s disease. (A–O) Alzheimer’s disease. (A–C) Double immunostained sections for amyloid-ß (red) and PHF-1 (brown) show diffuse cortical distribution of neurofibrillary tangles preferentially involving laminae III and V and without accentuation at depths of sulci. (D and E) Small blood vessels at sulcal depths show no clustering of neurofibrillary pathology perivascularly. (F and G) Sections immunostained for AT8 demonstrate diffuse cortical distribution of p-tau pathology without accumulations at sulcal depths. (H) Neurofibrillary tangles are preferentially distributed in laminae III and V. (I and J) Small blood vessels at bottom of cortical sulcus show no clustering of neurofibrillary pathology around vasculature (AT8 immunostain). (K) Subpial region at depth of sulcus shows no p-tau positive astrocytic tangles (AT8 immunostain). (L) Periventricular region of third ventricle shows no ependymal immunostaining for p-tau and low densities of p-tau neurites (AT8 immunostain). (M) Double immunostained section showing abundant amyloid-ß plaques (red) and interspersed PHF-1 neurofibrillary tangles (brown). (N) Moderate neurofibrillary change in substantia nigra pars compacta typical of severe Alzheimer’s disease (AT8 immunostain). (O) Absence of astrocytic tangles or neurofibrillary tangles in mammillary body in Alzheimer’s disease (AT8 immunostain). (P–FF) CTE. (P–R and U–W) Sections immunostained for AT8 showing irregular cortical distribution of p-tau pathology with prominent subpial clusters of p-tau astrocytic tangles, focal accentuation at depths of sulci and distribution of neurofibrillary tangles in superficial cortical laminae II–III. (S, T, X and Y) Small blood vessels at bottom of cortical sulcus prominent perivascular distribution of astrocytic tangles and neurofibrillary tangles (AT8). (Z) Subpial region at depth of sulcus shows prominent cluster of AT8 positive astrocytic tangles. (AA) Periventricular region of third ventricle shows intense ependymal immunostaining for AT8 and abundant pericapillary neurites. (BB) Double immunostained section for amyloid-ß (red) and PHF-1 (brown) shows dense neurofibrillary tangles without amyloid-ß deposition. (CC) Dense AT8 immunostained astrocytic tangles and neurofibrillary tangles in substantia nigra pars compacta of severe CTE (AT8). (DD) Dense AT8 immunostained astrocytic tangles and neurofibrillary tangles in mammillary body typical of CTE. (EE) Dense CP-13 immunostained axonal varicosities and neuropil threads in the anterior commissure in CTE. (FF) AT8 immunostained axonal varicosities and neuropil threads in the external capsule in CTE. (GG) Alzheimer’s disease: low densities of AT8 immunostained neuropil threads in subcortical white matter. (HH and II) CTE: AT8 immunostained astrocytic tangles (open arrowheads), neurofibrillary tangles (arrowheads) and pre-tangles (asterisk) characteristic of CTE. Some sections counter-stained with cresyl violet; all scale bars = 100 µm.
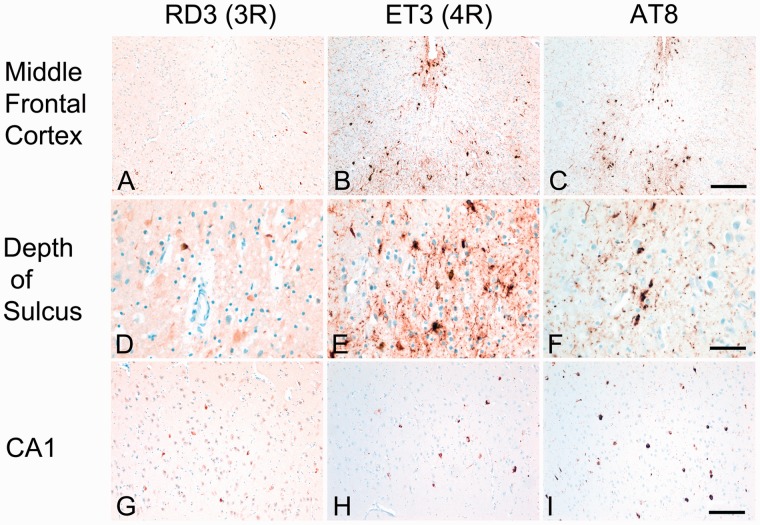
Figure 2.
Patterns of 3R and 4R Tau in CTE. (A, D and G) 3R immunostaining shows scattered RD3 immunoreactive neurons in middle frontal cortex and CA1 hippocampus. (B and E) 4R immunostaining shows many ET3 immunoreactive neurons and astrocytic tangles in the subpial region of the middle frontal cortex and at the depth of the sulcus. (H) 4R immunostaining shows many ET3 immunoreactive neurons in CA1 hippocampus. (C, F and I) AT8 immunostaining shows 3R and 4R immunopositive neurons and astrocytic tangles in middle frontal cortex and CA1 hippocampus. All are 10 -µm paraffin-embedded sections, scale bars = 50 µm.
Definition of chronic traumatic encephalopathy–motor neuron disease
The diagnosis of CTE-MND required a clinical diagnosis of definite amyotrophic lateral sclerosis using the revised El Escorial criteria for the diagnosis of amyotrophic lateral sclerosis (Brook et al., 1994, 2000), and the pathological diagnosis of CTE, as defined above, in addition to the following criteria (McKee et al., 2010): (i) degeneration of lateral and ventral corticospinal tracts of the spinal cord; (ii) marked loss of anterior horn cells from cervical, thoracic and lumbar spinal cord with gliosis; and (iii) TDP-43 or pTDP-43 positive neuronal, glial, neuritic or intranuclear inclusions in anterior horn cells and white matter tracts of the spinal cord.
Criteria for Alzheimer’s disease
The criteria for Alzheimer’s disease were based on the presence of amyloid-ß neuritic plaques and p-tau neurofibrillary tangles according to the NIA–Reagan criteria for intermediate and high likelihood Alzheimer’s disease and the recent NIA Alzheimer Association’s guidelines (Newell et al., 1999; Montine et al., 2012). The NIA–Reagan criteria take into account both the Braak and Braak staging of neurofibrillary tangles (Braak and Braak, 1991, 1993, 1994) and the overall density of neuritic plaques based on CERAD criteria (Mirra et al., 1991). The nature, pattern and distribution of p-tau neurofibrillary degeneration in CTE are distinctive from Alzheimer’s disease (Table 1 and Fig. 1; McKee et al., 2011).
Criteria for Parkinson’s disease and Lewy body disease
The diagnosis of Parkinson’s disease or Lewy body disease was based on the presence and distribution of alpha-synuclein-positive Lewy bodies and was considered brainstem-predominant (Parkinson’s disease), limbic or transitional Lewy body disease, and neocortical or diffuse Lewy body disease as defined by McKeith criteria (McKeith et al., 1996) and Braak staging (Del Tredici et al., 2002; Braak and Del Tredici, 2008).
Criteria for frontotemporal lobar degeneration
Neuropathological diagnosis of FTLD was based on predominant involvement of the frontal and temporal lobes and characteristic immunohistochemistry for p-tau, TDP-43 and p-TDP-43 using established criteria for FTLD (Cairns et al., 2007; Bigio, 2008; Mackenzie et al., 2010). The most common FTLD, FTLD with TDP-43-positive inclusions, FTLD-TDP, was defined by TDP-43-positive neuronal cytoplasmic and intranuclear inclusions, dystrophic neurites and glial cytoplasmic inclusions in the superficial layers of cerebral cortex and dentate gyrus. The diagnosis of FTLD-tau, which includes progressive supranuclear palsy, corticobasal degeneration and Pick’s disease, was defined by the specific patterns of p-tau glial and neuronal pathology and neuroanatomical areas of involvement according to consensus criteria (Litvan et al., 1996; Cairns et al., 2007; Dickson, 2009).
If criteria for more than one neurodegenerative disease were present, the case was considered to be mixed disease. Diagnosis of multiple system atrophy was based on published criteria (Dickson et al., 2009).
Semi-quantitative assessment of neuropathological features
The density of neurofibrillary tangles, astrocytic tangles, diffuse and neuritic amyloid–β plaques and vascular amyloid was rated semi-quantitatively using AT8 or amyloid-ß immunostained paraffin-embedded 10 µm sections according to methods previously reported (McKee et al., 2006).
Apolipoprotein E genotyping
Apolipoprotein E (ApoE) genotyping was conducted using restriction isotyping for determining ApoE isoforms based on brain tissue samples.
Statistical analysis
Stage of CTE was treated as an inexact ordinal variable; Spearman’s rank order correlation was used to determine the statistical dependence between CTE stage and all linear variables of interest (e.g. age, years of education, total number of reported concussions, total number of years of American football played and number of years between retirement and death). For non-linear independent variables, the Wilcoxon–Mann–Whitney two-sample rank-sum test was used for independent variables with only two groups (e.g. lifetime history of steroid use, presence of at least one ApoE e4 allele), whereas the Kruskall–Wallis test was used for variables with more than two groupings (e.g. position played).
Additionally, to determine whether the proportion of individuals with at least one ApoE e4 allele was higher in individuals diagnosed with CTE, a Chi-square goodness of fit test was performed comparing all CTE cases (n = 65) with the expected proportion in the US population (Corder et al., 1993).
Results
The 85 brain donors with a history of mild traumatic brain injury included 80 athletes (22 of whom were also military veterans), three military veterans with no history of contact sports, one civilian who had experienced multiple falls and one individual who engaged in self-injurious repetitive head-banging behaviour (84 males, one female, age range 14–98 years, mean 54.1 ± 23.3 years) (Table 2). We also analysed the brains of 18 cognitively intact subjects without known history of repetitive mild traumatic brain injury (17 males: one female, age range 18–88 years, mean 62.0 ± 17.4 years), seven of whom were military veterans and three of whom were athletes (skiing, sailing, golf and trap shooting) with no known history of mild traumatic brain injury.
Table 2.
Demographics, pathological diagnoses and immunoreactivity of the controls and mild traumatic brain injury cohort
| Case | MTBI exposure (sport /military) | Age (decade) | Race | Sex | ApoE | Cause of death | CTE | Amyloid-ß |
αSYN | TDP-43 | Other diagnoses | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DP | NP | CAA | |||||||||||
| 1 | No athletics | 10–19 | H | M | n/a | Cerebral aneurysm | 0 | ||||||
| 2 | No athletics | 20–29 | C | M | 34 | Suicide | 0 | ||||||
| 3 | No athletics, Vet | 50–59 | C | M | n/a | Kidney failure | 0 | ||||||
| 4 | No athletics, Vet | 60–69 | C | M | 33 | Malignancy | 0 | ||||||
| 5 | No athletics | 50–59 | C | M | 23 | Malignancy | 0 | ||||||
| 6 | No athletics | 60–69 | C | F | n/a | Malignancy | 0 | ||||||
| 7 | No athletics | 60–69 | C | M | 33 | Malignancy | 0 | ||||||
| 8 | Sailing, skiing | 60–69 | C | M | 23 | Malignancy | 0 | ||||||
| 9 | Trapshooting, Vet | 60–69 | C | M | 33 | MVA | 0 | ||||||
| 10 | Skiing, hiking, golfing, Vet | 60–69 | C | M | 33 | Malignancy | 0 | ||||||
| 11 | No athletics | 60–69 | C | M | 24 | ICH | 0 | +++ | + | + | |||
| 12 | No athletics, Vet | 60–69 | C | M | 34 | Cardiac | 0 | ++ | + | ||||
| 13 | No athletics, Vet | 70–79 | C | M | 23 | Malignancy | 0 | ||||||
| 14 | No athletics | 70–79 | C | M | 23 | Malignancy | 0 | ||||||
| 15 | No athletics, Vet | 70–79 | C | M | 33 | ICH | 0 | ++ | ++ | + | |||
| 16 | No athletics, Vet | 70–79 | C | M | 33 | Cardiac | 0 | ||||||
| 17 | No athletics | 70–79 | C | M | 33 | Respiratory failure | 0 | + | |||||
| 18 | No athletics | 80–89 | C | M | 23 | Cardiac | 0 | ||||||
| 19 | MS soccer | 10–19 | C | M | 33 | Cerebral oedema | 0 | ||||||
| 20 | HS AFB | 10–19 | C | M | 33 | Overdose | 0 | ||||||
| 21 | HS AFB | 10–19 | C | M | 33 | Overdose | 0 | ||||||
| 22 | HS AFB | 10–19 | C | M | 34 | Suicide | 0 | ||||||
| 23 | College hockey | 10–19 | C | M | 33 | Overdose | 0 | ||||||
| 24 | HS AFB | 10–19 | C | M | 33 | Cardiac | 0 | ||||||
| 25 | Pro ice hockey | 20–29 | C | M | n/a | Metabolic encephalopathy | 0 | ||||||
| 26 | HS AFB | 20–29 | C | M | n/a | GSW | 0 | ||||||
| 27 | Pro AFB | 20–29 | C | M | 33 | GSW | 0 | ||||||
| 28 | HS AFB | 20–29 | C | M | 33 | Suicide | 0 | ||||||
| 29 | MMA | 20–29 | C | M | 33 | Suicide | 0 | ||||||
| 30 | Pro wrestling | 30–39 | C | M | 33 | Suicide | 0 | ||||||
| 31 | Comp skiing | 30–39 | C | F | 34 | Suicide | 0 | ||||||
| 32 | HS AFB | 40–49 | C | M | n/a | Suicide | 0 | MSA | |||||
| 33 | HS baseball, hockey, Vet | 60–69 | C | M | n/a | Malignancy | 0 | ||||||
| 34 | Youth box | 70–79 | C | M | 23 | Cardiac | 0 | ||||||
| 35 | Firefighter | 80–89 | C | M | 34 | Respiratory failure | 0 | ||||||
| 36 | HS AFB, HS basketball | 10–19 | C | M | SIS | I | + | ||||||
| 37 | HS AFB, rugby | 10–19 | C | M | 33 | Cerebral oedema | I | + | |||||
| 38 | IED/explosives, HS AFB, Vet | 20–29 | H | M | 33 | ICH | I | ||||||
| 39 | Pro AFB | 20–29 | AA | M | 33 | Suicide | I | + | |||||
| 40 | HS AFB, Vet | 20–29 | C | M | 34 | Suicide | I | ||||||
| 41 | Pro AFB | 30–39 | C | M | 33 | Cardiac | I | + | |||||
| 42 | Pro AFB | 50–59 | C | M | 34 | Malignancy | I | ||||||
| 43 | College AFB | 20–29 | C | M | 34 | Suicide | II | + | |||||
| 44 | Pro wrestling | 20–29 | C | M | 33 | Overdose | II | ||||||
| 45 | Pro ice hockey | 20–29 | C | M | 33 | Overdose | II | + | |||||
| 46 | College AFB, HS wrestling | 30–39 | C | M | 33 | Respiratory failure | II | ++++ | CTE-MND | ||||
| 47 | IED, HS AFB, Prison guard, Vet | 30–39 | C | M | 33 | Overdose | II | + | |||||
| 48 | College AFB | 40–49 | AA | M | 33 | Respiratory failure | II | ++++ | CTE-MND | ||||
| 49 | IED, MVA, Vet | 40–49 | C | M | 33 | Cerebral aneurysm | II | 0 | |||||
| 50 | Pro ice hockey | 40–49 | C | M | 33 | Cardiac | II | + | |||||
| 51 | Pro AFB | 40–49 | C | M | 33 | Cardiac | II | 0 | |||||
| 52 | HS AFB | 40–49 | C | M | 33 | Suicide | II | + | |||||
| 53 | Pro AFB | 40–49 | AA | M | 34 | Respiratory failure | II | ++++ | CTE-MND | ||||
| 54 | College AFB | 50–59 | C | M | 33 | Malignancy | II | ++ | + | ||||
| 55 | Pro ice hockey | 50–59 | C | M | 34 | Cardiac | II | + | |||||
| 56 | Pro AFB, Vet | 80–89 | C | M | 33 | Cardiac | II | ++++ | + | + | |||
| 57 | Pro AFB | 30–39 | C | M | 33 | Suicide | III | 0 | |||||
| 58 | Pro box | 40–49 | C | M | 33 | Suicide | III | + | |||||
| 59 | HS basketball, college AFB, amateur box, Vet | 40–49 | C | M | 33 | Respiratory failure | III | +++ | CTE-MND | ||||
| 60 | College AFB | 40–49 | C | M | 33 | Overdose | III | + | |||||
| 61 | Pro AFB | 40–49 | C | M | 44 | GSW | III | 0 | |||||
| 62 | Pro AFB | 40–49 | C | M | 44 | Overdose | III | + | 0 | ||||
| 63 | Pro AFB | 50–59 | AA | M | 34 | Suicide | III | + | |||||
| 64 | Pro AFB | 50–59 | C | M | 34 | Cardiac | III | + | |||||
| 65 | Self-injury | 50–59 | C | M | n/a | Respiratory failure | III | 0 | |||||
| 66 | Pro AFB | 60–69 | C | M | 23 | Respiratory failure | III | ++++ | CTE-MND | ||||
| 67 | Pro AFB | 60–69 | AA | M | 33 | Overdose | III | + | |||||
| 68 | Pro AFB | 60–69 | C | M | 33 | Cardiac | III | + | |||||
| 69 | Pro AFB | 60–69 | C | M | 33 | Respiratory failure | III | +++ | CTE-MND | ||||
| 70 | TBI, PT epilepsy, Vet | 70–79 | C | M | 33 | Pneumonia | III | ++ | ++ | +++ | + | ||
| 71 | MVA, altercation, Vet | 80–89 | C | M | 33 | Pneumonia | III | + | + | ||||
| 72 | Pro box | 50–59 | AA | M | 33 | Respiratory failure | IV | + | |||||
| 73 | Pro box | 60–69 | C | M | 34 | Respiratory failure | IV | + | + | +++ | CTE-MND | ||
| 74 | Pro box | 60–69 | C | M | 33 | Cardiac | IV | ++ | + | +++ | CTE-MND | ||
| 75 | Pro box, Vet | 70–79 | C | M | 33 | FTT | IV | +++ | |||||
| 76 | Pro AFB | 70–79 | AA | M | 34 | Malignancy | IV | +++ | |||||
| 77 | Pro AFB | 70–79 | C | M | 23 | Cardiac | IV | ++ | |||||
| 78 | Pro AFB, Vet | 80–89 | AA | M | 44 | Respiratory failure | IV | + | ++++ | +++ | |||
| 79 | Pro box, Vet | 70–79 | AA | M | 33 | FTT | IV | + | + | + | +++ | ||
| 80 | Pro AFB, Vet | 70–79 | C | M | 33 | Respiratory failure | IV | ++ | + | + | +++ | ||
| 81 | Pro box | 80–89 | AA | M | 34 | Sepsis | IV | + | ++ | + | +++ | ||
| 82 | Pro AFB | 80–89 | C | M | 33 | FTT | IV | + | |||||
| 83 | Pro AFB, Vet | 80–89 | AA | M | 33 | FTT | IV | + | + | ++++ | |||
| 84 | Semi Pro AFB, Vet | 80–89 | C | M | 33 | FTT | IV | ++++ | + | + | +++ | ||
| 85 | Amateur box, Vet | 90–99 | C | M | n/a | FTT | IV | ++ | ++ | ++ | ++++ | ||
| 86 | Pro AFB, Vet | 90–99 | C | M | 33 | FTT | IV | + | ++++ | ||||
| 87 | College AFB | 60–69 | C | M | 44 | FTT | IV | ++++ | ++++ | ++ | + | + | Alzheimer’s disease |
| 88 | Pro AFB, Vet | 60–69 | C | M | 23 | FTT | IV | ++++ | +++ | ++ | + | Alzheimer’s disease | |
| 89 | College AFB | 60–69 | C | M | 33 | FTT | IV | ++++ | ++++ | +++ | + | + | Alzheimer’s disease |
| 90 | Pro AFB, Vet | 70–79 | C | M | 34 | FTT | IV | +++ | ++ | ++ | +++ | Alzheimer’s disease | |
| 91 | Pro AFB | 60–69 | C | M | 33 | FTT | IV | +++ | ++ | ++ | +++ | + | Alzheimer’s disease, Parkinson’s disease |
| 92 | Pro AFB | 70–79 | C | M | 34 | FTT | IV | +++ | ++ | ++++ | ++ | Alzheimer’s disease, Lewy Body disease | |
| 93 | Amateur ice hockey, Vet | 80–89 | C | M | 33 | FTT | IV | +++ | +++ | ++ | +++ | + | Alzheimer’s disease, Parkinson’s disease |
| 94 | College AFB, college rugby, Vet | 60–69 | C | M | 33 | FTT | IV | + | + | +++ | ++++ | Parkinson’s disease | |
| 95 | Pro AFB | 60–69 | C | M | 24 | Respiratory failure | II | + | + | + | ++++ | + | Lewy Body disease |
| 96 | Pro AFB | 70–79 | C | M | 33 | Cardiac | III | +++ | + | + | ++++ | + | Lewy Body disease |
| 97 | Pro ice hockey | 70–79 | C | M | 34 | FTT | III | ++ | ++ | ++++ | + | Lewy Body disease | |
| 98 | Pro AFB, Vet | 70–79 | C | M | 44 | Cardiac | IV | + | + | +++ | + | Parkinson’s disease | |
| 99 | Pro AFB, Vet | 80–89 | C | M | 33 | Malignancy | III | +++ | + | ++++ | + | Lewy Body disease | |
| 100 | Pro AFB | 70–79 | C | M | 33 | Cardiac | III | + | + | +++ | ++++ | Parkinson’s disease, FTLD-TDP | |
| 101 | Canadian AFB | 70–79 | C | M | 23 | Respiratory failure | II | + | + | Parkinson’s disease, PSP | |||
| 102 | Pro AFB | 60–69 | AA | M | 33 | FTT | I | + | + | Pick’s | |||
| 103 | Pro AFB | 80–89 | AA | M | 34 | FTT | IV | +++ | + | ++ | ++++ | FTLD-TDP | |
AFB = American football; αSYN = alpha-synuclein; AA = African American; Box = Boxing; C = Caucasian; CAA = cerebral amyloid angiopathy; Comp = competitive; DP = diffuse amyloid ß plaques; F = female; FB = football; FTT = failure to thrive associated with dementia; GSW = gunshot wound; H = Hispanic; HS = high school; ICH = intracerebral haemorrhage; IED = improvised explosive device blast exposure; LBD = Lewy body disease; M = male; MS = middle school; MTBI = mild traumatic brain injury; MVA = motor vehicle accident; MSA = multiple system atrophy; n/a = not available; NP = neuritic amyloid ß plaques; Pick’s = Pick’s disease; PT = post-traumatic; PSP = progressive supranuclear palsy; Pro = professional; SIS = second impact syndrome; TBI = traumatic brain injury; TDP43 = TAR DNA-binding protein; Vet = military veteran. Scoring scale: + = mild, ++ = moderate, +++ = severe, ++++ = very severe.
Pathological findings
Seven of the 18 control brains were completely negative for p-tau neurofibrillary tangles (mean age 48.1 ± 19.8 years), 11 control brains showed Alzheimer’s-type neurofibrillary pathology limited to the hippocampus and entorhinal cortex consistent with Braak neurofibrillary stages I and II (mean age 70.8 ± 7.8 years). Three control subjects showed small amounts of amyloid-ß deposition as diffuse, neuritic plaques or vascular amyloid (mean 69.7 ± 8.1 years). No control case showed evidence of perivascular clusters of neurofibrillary tangles or astrocytic tangles, neurofibrillary tangles localized to the depths of the cerebral sulci or neurofibrillary tangles primarily localized to the superficial cortical laminae (Table 2, Cases 1–18).
Brains from 17 of the 85 individuals with a history of repetitive mild traumatic brain injury (16 males: one female; mean age 32.6 ± 22.4 years, 20% of the mild traumatic brain injury sample) did not show any changes of CTE (Table 2, Cases 19–35). One individual who played high school football (Case 32) was diagnosed with multiple system atrophy. The brains of 68 of the 85 subjects showed p-tau immunoreactive neurofibrillary tangles and astrocytic tangles in a pattern and neuroanatomical distribution diagnostic of CTE (68 males, 0 females; mean age 59.5 ± 20.4 years, 80% of the mild traumatic brain injury sample). The 68 included 50 football players [34 of whom played professionally including 33 National Football League players (two athletes also played in the Canadian Football League and one also played in the United Football League) and one Canadian Football League player], one semi-professional football player, nine college football players, six high school football players, five hockey players (four National Hockey League players and one amateur hockey player), seven professional boxers, one amateur boxer and one professional wrestler. Four individuals without a history of contact sports also developed CTE including three veterans and one individual who displayed self-injurious head banging behaviour. CTE or CTE-MND was diagnosed in 51 cases (51 males, 0 females, mean age 55.3 ± 21.8 years; 60% of the mild traumatic brain injury sample, 75% of all CTE cases). CTE-MND was diagnosed in eight cases (including three cases previously reported, McKee et al., 2010; 9.4% of mild traumatic brain injury sample, 11.8% of CTE cases) (Table 2). The brains of seven subjects fulfilled criteria for CTE plus Alzheimer’s disease (mean age 69.9 ± 6.5 years, 8.2% of mild traumatic brain injury sample, 10.3% CTE cases); 11 were diagnosed with CTE plus Lewy body disease (mean age 73.4 ± 6.2 years; 12.9% of the mild traumatic brain injury sample, 16.2% of CTE cases), either as Parkinson’s disease, transitional or diffuse Lewy body disease; and four (mean age 75.5 ± 5.0 years; 4.7% of the mild traumatic brain injury sample, 5.9% of CTE cases) were diagnosed with CTE plus FTLD [FTLD-TDP in two, FTLD-tau in two (progressive supranuclear palsy and Pick’s disease in one each)] (Table 2).
Amyloid-β and Lewy bodies
Amyloid-ß deposition, either as diffuse plaques, neuritic plaques or vascular amyloid, was found in 30 brains (35.3% of the mild traumatic brain injury sample, 44.1% of CTE cases) and 14 (27.4%) pure CTE cases. Subjects with CTE and pure CTE whose brains showed amyloid-ß deposits were significantly older than those without amyloid-ß (P < 0.0001; P < 0.0001). Alpha-synuclein-positive Lewy bodies were found in 15 of the CTE cases (22.0%). In two cases with CTE, Lewy bodies were restricted to the olfactory bulb and medulla, and in two cases with CTE plus Alzheimer’s disease, Lewy bodies were restricted to the amygdala. Subjects with Lewy bodies were significantly older than those without (P = 0.03).
Neuropathology of chronic traumatic encephalopathy
In individuals with CTE or CTE-MND, 13 had diffuse plaques (25.5%), 10 had modest numbers of neuritic plaques (19.6%) and seven had small amounts of vascular amyloid (13.7%). These 51 brains showed a predictable range of unique p-tau pathology that could be divided into four distinct stages of disease (Figs 1–3). CTE disease severity ranged from very mild (stage I/IV, n = 7, age range 17–56 years, mean 28.3 years ± 13.5), mild (stage II/IV, n = 14, age range 21–87 years, mean 44.3 years ± 16.7), moderate (stage III/IV, n = 15, age range 38–82 years, mean 56.0 years ± 14.2) to severe (stage IV/IV, n = 15, age range 51–98 years, mean 77.4 years ± 11.7) (Table 2 and Supplementary Tables 3 and 4). The p-tau neurofibrillary tangles at all stages were immunoreactive for both 3 R and 4 R tau, and astrocytic tangles were predominantly immunoreactive for 4 R tau (Fig. 2).
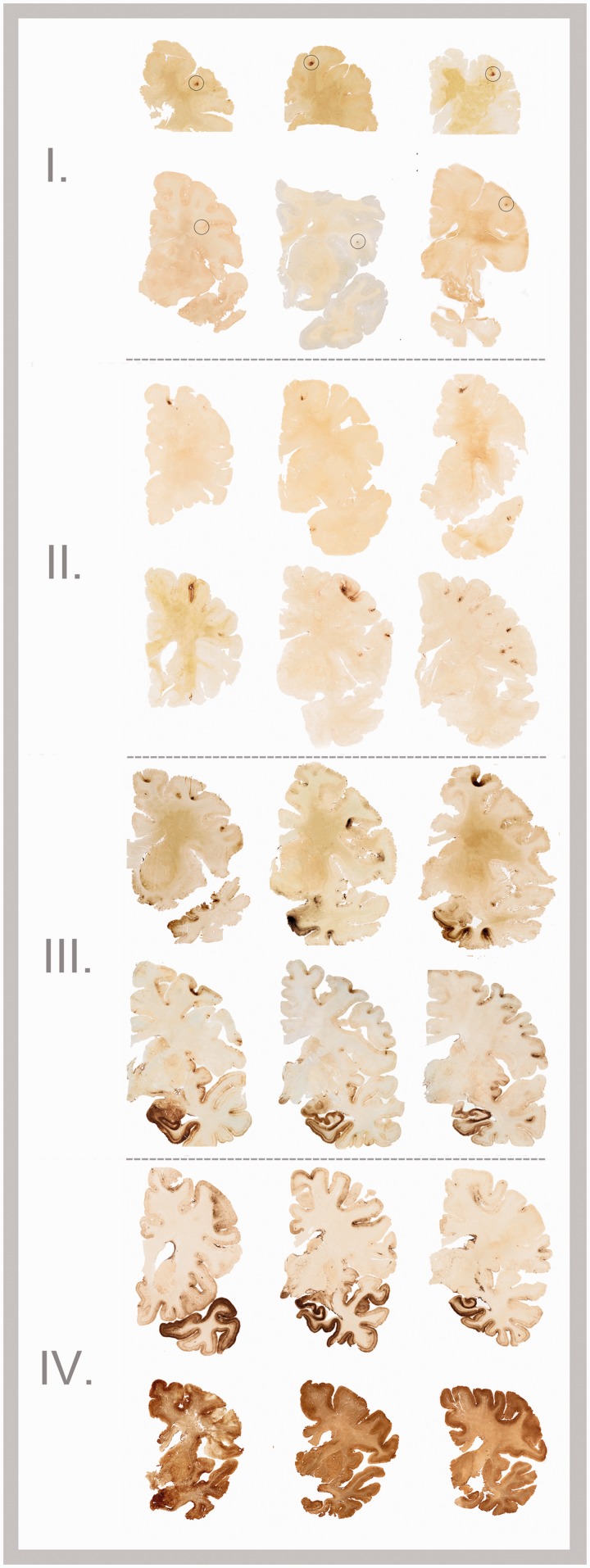
Figure 3.
The four stages of CTE. In stage I CTE, p-tau pathology is restricted to discrete foci in the cerebral cortex, most commonly in the superior, dorsolateral or lateral frontal cortices, and typically around small vessels at the depths of sulci (black circles). In stage II CTE, there are multiple epicentres at the depths of the cerebral sulci and localized spread of neurofibrillary pathology from these epicentres to the superficial layers of adjacent cortex. The medial temporal lobe is spared neurofibrillary p-tau pathology in stage II CTE. In stage III, p-tau pathology is widespread; the frontal, insular, temporal and parietal cortices show neurofibrillary degeneration with greatest severity in the frontal and temporal lobe, concentrated at the depths of the sulci. Also in stage III CTE, the amygdala, hippocampus and entorhinal cortex show neurofibrillary pathology. In stage IV CTE, there is severe p-tau pathology affecting most regions of the cerebral cortex and the medial temporal lobe, sparing calcarine cortex in all but the most severe cases. All images, CP-13 immunostained 50-µm tissue sections.
Stage I chronic traumatic encephalopathy
Seven brains showed stage I CTE (Table 2, Cases 36–42, Figs. 3 and 4, Supplementary Tables 2 and 3). Mild lateral ventricular enlargement was found in three of the five intact brain specimens. The gross neuropathological features and brain weights were otherwise unremarkable (mean brain weight 1463.3 ± 179.0 g). Microscopically, stage I was characterized by focal epicentres of perivascular p-tau neurofibrillary and astrocytic tangles, most prominent in the sulcal depths and typically affecting superior and dorsolateral frontal cortices (Figs 1–3). The cortex surrounding the epicentres was unremarkable except for rare isolated neurofibrillary tangles in superficial laminae. Low densities of neurofibrillary tangles were found in the locus coeruleus in two cases. One case showed sparse neurofibrillary tangles in the hippocampus, entorhinal cortex and substantia nigra; another case displayed p-tau neurofibrillary tangles and distorted axonal profiles in the medulla (Case 37). Phosphorylated neurofilament immunohistochemistry showed scattered distorted axonal varicosities in frontal cortex, subcortical white matter and deep white matter tracts of the diencephalon, which were also occasionally immunoreactive for p-tau (Fig. 4). TDP-43 immunopositive neurites were found in four of the seven cases (57%) in the frontal subcortical white matter and fornix.
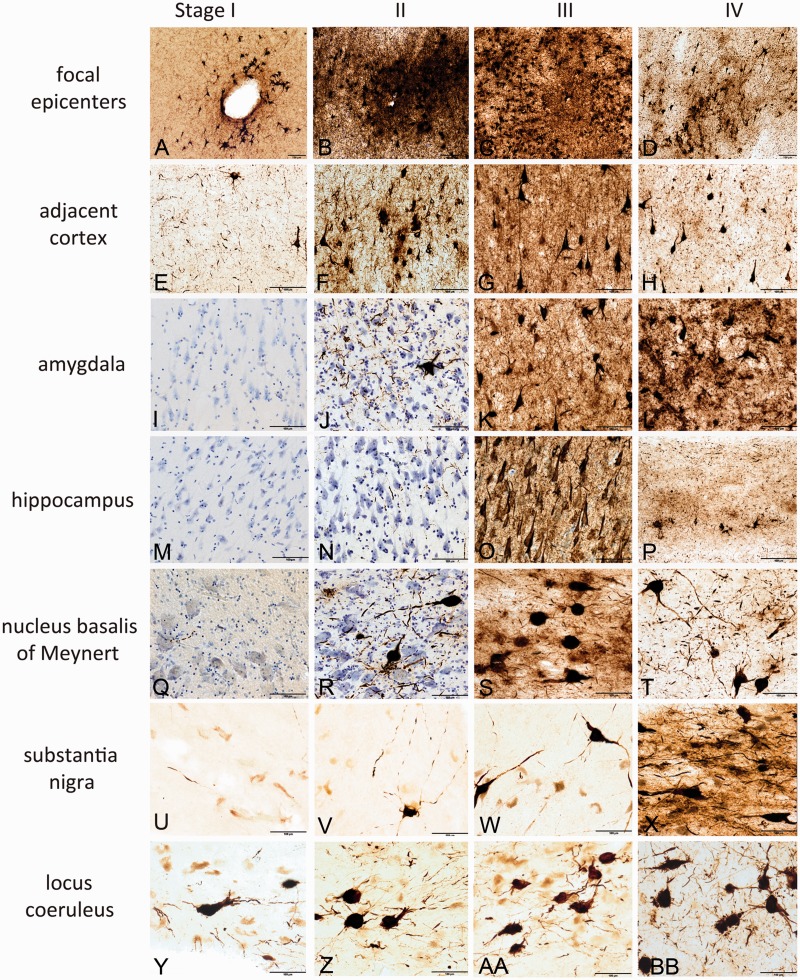
Figure 4.
Hyperphosphorylated tau pathology in the four stages of CTE. In stage I CTE (first column), p-tau pathology is found in limited discrete perivascular foci (A), typically at the depths of sulci or around small vessels. There is mild p-tau pathology in cerebral cortices neighbouring the epicentres (E). There is no or minimal p-tau pathology in the amygdala (I) or CA1 of hippocampus (M). Occasional p-tau neurites are found in the nucleus basalis of Meynert (Q) and substantia nigra (U); isolated neurofibrillary tangles are present in the locus coeruleus (Y) in stage I. In stage II CTE (second column), there is spread of pathology from focal epicentres (B) to the superficial layers of adjacent cortex (F). The medial temporal lobe shows only mild neurofibrillary pathology, including amygdala (J) and CA1 hippocampus (N). Nucleus basalis of Meynert (R) and locus coeruleus (Z) demonstrate moderate p-tau pathology as neurofibrillary tangles and neurites; the substantia nigra (V) shows only modest pathology. In stage III, p-tau pathology is severe and widespread throughout the frontal, insular, temporal and parietal cortices. The cortical epicentres and depths of the sulci often consist of confluent masses of neurofibrillary tangles and astrocytic tangles (C). The intervening cortices show advanced neurofibrillary degeneration (G). The amygdala (K), hippocampus (O) and entorhinal cortex demonstrate marked neurofibrillary pathology. The nucleus basalis of Meynert shows dense neurofibrillary tangles (S); the locus coeruleus (AA) shows advanced neurofibrillary pathology, and the substantia nigra is moderately affected (W) in stage III CTE. In stage IV CTE, there is widespread p-tau pathology affecting most regions of the cerebral cortex and medial temporal lobe with relative sparing of the calcarine cortex. Astrocytic tangles are prominent, and there is marked neuronal loss in the cortex, amygdala and hippocampus. Phosphorylated-tau neurofibrillary tangles are reduced in size and density. The cortical epicentres show severe neuronal loss and prominent astrocytic tangles (D); similar changes are found throughout the frontal, temporal and parietal cortices (H). The amygdala demonstrates intense gliosis and p-tau neuronal and glial degeneration (L). The hippocampus is sclerotic with marked neuronal loss, gliosis, ghost neurofibrillary tangles and astrocytic tangles (P). The nucleus basalis of Meynert shows marked neurofibrillary pathology and gliosis (T); the substantia nigra (X) and locus coeruleus (BB) show advanced neurofibrillary pathology. All images: CP-13 immunostained 50 -µm tissue sections, some counterstained with cresyl violet, all scale bars = 100 µm.
Clinical symptoms
Family interview and medical record review were available in six of the seven subjects with stage I CTE. One subject was asymptomatic. Four of the six reported headache and loss of attention and concentration, three reported short-term memory difficulties, aggressive tendencies and depression and two reported executive dysfunction and explosivity. Two subjects were diagnosed with post-traumatic stress disorder (Tables 3 and 4).
Table 3.
Clinical symptoms associated with stages of CTE
| Case | Years of education | Family history of neurological disease | Age of symptom onset | Presenting symptoms | Headache | Depression | Impulsivity | Explosivity | Aggression | |
|---|---|---|---|---|---|---|---|---|---|---|
| Stage I CTE | ||||||||||
| 36 | 11 | None | 17 | HA | ++ | |||||
| 37 | 12 | None | 18 | HA | ++ | |||||
| 38 | 12 | None | 20 | HA | ++ | ++ | ++ | ++ | ||
| 39 | 14 | None | 26 | ATT, STM, LANG | + | + | + | |||
| 41 | 16 | None | 30 | HA, STM | ++ | ++ | ++ | + | ||
| 42 | 16 | Mother: Alzheimer’s disease | n/a | None | ||||||
| Stage II CTE | ||||||||||
| 43 | 15 | None | n/a | None | + | |||||
| 44 | 11 | None | 26 | HA, STM | ++ | ++ | ++ | ++ | ||
| 45 | 11 | None | 26 | HA, STM, MS | ++ | ++ | ++ | ++ | ++ | |
| 46 | 16 | None | 30 | MND | ++ | + | ++ | ++ | ||
| 47 | 13 | None | 31 | STM, DEP, PTSD | ++ | ++ | ||||
| 48 | 17 | None | 40 | MND | + | ++ | + | ++ | ||
| 49 | 16 | None | 42 | HA, DEP, ATT | ++ | ++ | ||||
| 50 | 11 | None | 41 | STM, ATT, EXP, EXEC | + | + | ++ | ++ | ||
| 51 | 20 | None | 46 | HA | ++ | + | ||||
| 52 | 16 | Father: possible Alzheimer’s disease, bipolar disease | 47 | STM, ATT, EXEC, DEP | ++ | + | + | |||
| 53 | 12 | Father: possible undiagnosed dementia | 48 | MND | ++ | + | + | |||
| 54 | 14 | None | 52 | HA, STM | ++ | ++ | ++ | ++ | ++ | |
| 55 | 13 | None | n/a | None | + | + | ||||
| 56 | 18 | None | n/a | None | + | |||||
| Stage III CTE | ||||||||||
| 57 | 14.5 | None | 34 | HA, MS, PAR | ++ | + | ++ | + | ++ | |
| 58 | 15 | None | 37 | HA, psychosis, STM | ++ | ++ | ++ | ++ | ++ | |
| 59 | 16 | None | 27 | MND | + | |||||
| 60 | 16 | None | 38 | STM, DEP, EXP | ++ | ++ | ++ | ++ | ||
| 61 | 14 | None | 40 | STM, ATT, EXEC, EXP | ++ | |||||
| 62 | 16 | Father: bipolar disease | 42 | ATT, EXEC | + | |||||
| 63 | 18 | Father: Alzheimer’s disease | 45 | HA, EXP | ++ | ++ | + | ++ | ++ | |
| 64 | 16 | None | 53 | STM, ATT, EXEC | + | + | ++ | |||
| 66 | 16 | None | 56 | STM, apathy | ++ | ++ | ||||
| 67 | 16 | Brother: mental illness | 63 | STM, EXEC, ATT | + | |||||
| 68 | 15 | None | n/a | None | + | + | + | |||
| 69 | 18 | Father: depression | 52 | HA, STM, DEP, IMP | ++ | ++ | ++ | |||
| Stage IV CTE | ||||||||||
| 72 | 12 | None | 42 | AGG, DEP, PAR | ++ | + | ++ | |||
| 73 | 15 | None | 46 | EXEC, IMP, PAR, AGG | ++ | ++ | ++ | ++ | ||
| 74 | 12 | Sibling: ALS | 64 | STM, EXEC, PAR | ++ | ++ | ++ | |||
| 75 | 12 | None | 56 | STM, DEP, AGG, EXP | ++ | + | ++ | ++ | ||
| 76 | 12 | None | 35 | PAR, IMP, BIZ | ++ | ++ | ++ | ++ | ||
| 77 | 16 | Mother: bipolar disease | 58 | DEP, AGG | ++ | ++ | ++ | ++ | ||
| 78 | 18 | None | 60 | STM, EXEC, BIZ | ||||||
| 80 | 16 | None | 76 | STM, EXEC, LANG | ++ | + | + | |||
| 81 | 12 | Brother: Alzheimer’s disease | 35 | STM, ATT, Falls | ++ | ++ | ++ | |||
| 82 | 18 | None | 49 | ATT, AGG, EXP | ++ | ++ | ++ | ++ | ||
| 83 | 10 | None | 65 | AP, EXEC, EXP | ++ | ++ | ||||
| 84 | 16 | None | 74 | PAR | ++ | + | + | |||
| 86 | 16 | None | 83 | STM, EXEC | ||||||
AGG = aggression; ALS = amyotrophic lateral sclerosis; ATT = attention loss; BIZ = bizarre behaviours; DEP = Depression; EXEC = executive dysfunction; EXP = explosivity; HA = headaches; IMP = impulsivity; LANG = language disturbance; MS = mood swings; n/a = not applicable; PAR = paranoia; PTSD = post-traumatic stress disorder; STM = short-term memory loss.
Table 4.
Clinical symptoms associated with stages of CTE
| Case | Attention | Paranoia | Executive function | Suicidal | Memory | Language | Visuospatial | Apathy | Dementia | Gait | Dysarthria | Parkinsonian | PTSD |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Stage I CTE | |||||||||||||
| 36 | + | ||||||||||||
| 37 | |||||||||||||
| 38 | ++ | + | + | PTSD | |||||||||
| 39 | ++ | + | ++ | ++ | + | PTSD | |||||||
| 41 | + | + | + | ||||||||||
| 42 | |||||||||||||
| Stage II CTE | |||||||||||||
| 43 | ++ | ||||||||||||
| 44 | ++ | + | |||||||||||
| 45 | ++ | ++ | ++ | ++ | ++ | + | |||||||
| 46 | + | + | + | + | + | a | a | ||||||
| 47 | ++ | + | ++ | ++ | + | + | PTSD | ||||||
| 48 | + | + | a | a | |||||||||
| 49 | ++ | ||||||||||||
| 50 | ++ | ++ | ++ | ++ | ++ | ||||||||
| 51 | |||||||||||||
| 52 | ++ | ++ | ++ | ++ | + | ||||||||
| 53 | a | a | |||||||||||
| 54 | + | ++ | + | + | + | + | |||||||
| 55 | |||||||||||||
| 56 | |||||||||||||
| Stage III CTE | |||||||||||||
| 57 | + | ++ | ++ | ++ | + | + | + | ||||||
| 58 | ++ | ++ | ++ | ++ | ++ | ++ | ++ | + | + | + | |||
| 59 | ++ | a | a | ||||||||||
| 60 | + | + | + | + | |||||||||
| 61 | ++ | ++ | ++ | + | + | + | |||||||
| 62 | ++ | ++ | + | + | + | ||||||||
| 63 | ++ | ++ | ++ | ++ | + | + | + | + | |||||
| 64 | + | + | + | + | + | + | |||||||
| 66 | ++ | ++ | + | + | ++ | + | a | a | |||||
| 67 | ++ | ++ | ++ | ++ | + | ||||||||
| 68 | + | ||||||||||||
| 69 | + | + | ++ | + | + | + | a | a | |||||
| Stage IV CTE | |||||||||||||
| 72 | ++ | ++ | ++ | ++ | + | ++ | + | ++ | + | + | |||
| 73 | ++ | ++ | ++ | ++ | ++ | ++ | ++ | a | a | ||||
| 74 | ++ | ++ | ++ | ++ | + | ++ | ++ | a | a | + | |||
| 75 | ++ | ++ | ++ | ++ | ++ | ++ | ++ | ++ | ++ | + | |||
| 76 | + | ++ | ++ | ++ | ++ | ||||||||
| 77 | ++ | ++ | + | ++ | +++ | ++ | + | ||||||
| 78 | ++ | ++ | ++ | ++ | ++ | +++ | ++ | ++ | ++ | + | |||
| 80 | ++ | ++ | ++ | ++ | |||||||||
| 81 | ++ | ++ | ++ | ++ | ++ | ++ | ++ | + | + | + | |||
| 82 | ++ | ++ | + | ++ | ++ | ++ | + | ++ | + | ||||
| 83 | ++ | ++ | ++ | ++ | ++ | ++ | ++ | ++ | |||||
| 84 | ++ | ++ | ++ | ++ | ++ | + | ++ | + | |||||
| 86 | ++ | ++ | ++ | ++ | ++ | ++ | |||||||
a Gait and speech difficulties associated with MND.
PTSD = post-traumatic stress disorder.
Stage II chronic traumatic encephalopathy
Fourteen brains showed stage II pathology (Table 2, Cases 43–56). Grossly, there was no evidence of cerebral atrophy with a mean brain weight of 1463.3 ± 100.1 g. There was mild enlargement of the frontal horn of the lateral ventricles or third ventricle in 6 of the 11 intact specimens, and a small cavum septum (0.2–0.7 cm) was found in four; the third ventricle was enlarged and sharply concave in three. Three cases showed pallor of the locus coeruleus and substantia nigra. There was severe gliosis and atrophy of one mammillary body in one case (Case 45). P-tau pathology was found in multiple discrete foci of the cortex, most commonly superior, dorsolateral, lateral, inferior and subcallosal frontal, anterior, inferior and lateral temporal, inferior parietal, insular and septal cortices. Neurofibrillary tangles were also found in the superficial layers of cortex (Figs. 1 and 3). Moderate densities of neurofibrillary tangles were also found in the locus coeruleus, nucleus basalis of Meynert and amygdala even in the younger individuals (Fig. 4 and Supplementary Table 3). Low densities of p-tau neurofibrillary tangles and pretangles were present in the hypothalamus, CA1 of hippocampus, entorhinal cortex, thalamus, substantia nigra and dorsal and median raphe nuclei of the midbrain. Distorted axonal varicosities, some p-tau immunoreactive, were found in frontal and temporal cortices as well as white matter tracts (Figs. 1 and 5). Eleven of the 14 subjects with stage II CTE also showed TDP-43 immunopositivity (79%). TDP-43 immunopositivity consisted of rare neurites or inclusions in the cerebral subcortical white matter, brainstem or medial temporal lobe in eight cases, often in a subpial, periventricular or perivascular distribution (Fig. 6). Three subjects showed severe TDP-43 abnormalities as neuronal and glial inclusions and neurites in widespread regions of the CNS, including the cerebral hemispheres, basal ganglia, diencephalon, brainstem, anterior horn cells and white matter tracts of the spinal cord (Fig. 6). These cases also demonstrated degeneration of lateral and ventral corticospinal tracts of the spinal cord and marked loss of anterior horn cells from the spinal cord; features that support the diagnosis of CTE-MND.
Figure 5.
The axonal pathology of CTE. (A and B) Phosphorylated neurofilament immunostaining for SMI-34 (red) in control subcortical white matter shows regular alignment and linear morphology of most axonal profiles. (C and D) Axons in control cerebral cortex stained with Bielschowsky’s silver method show a fine linear pattern and regularity. (E) Phosphorylated neurofilament immunostaining (SMI-34) in control cerebral cortex also shows regular alignment and linear morphology of axons even around small vessels. (F and G) Phosphorylated neurofilament immunostaining in cerebral cortex of stage II CTE demonstrates alterations in alignment and numerous rounded axonal varicosities around small vessels (asterisks). (H and I) Bielschowsky silver method in stage I CTE shows neurofibrillary tangles (arrows) and silver positive axonal varicosities (asterisks) around small arteriole. (J) SMI-34 immunostaining of same cortical focus as in H and I also shows axonal varicosities (asterisks) around cortical arteriole. (K and L) SMI-34 immunostaining in cerebral cortex of stage III CTE shows marked reduction in axonal staining and numerous large, irregular axonal varicosities. A small arteriole shows marked infiltration with haemosiderin-laden macrophages (arrow). (M) Axonal varicosities and irregularities are also found in stage I CTE. (N) CTE stage II double immunostained for phosphorylated tau (PHF-1, brown) and phosphorylated neurofilament (SMI-34, red) shows axonal swellings in continuity with phosphorylated tau neuritic abnormalities. (O) Double immunofluorescence staining for phosphorylated neurofilament, SMI-34 (red) and PHF-1 (green) in the subcortical white matter of CTE stage III demonstrates contiguous axonal varicosities (red) as well as p-tau (green) (arrowheads) in the axon. (P and Q) SMI-34 immunostaining in subcortical white matter of stage IV CTE shows severe axonal loss and multiple large, irregular axonal varicosities. (R and S) Phosphorylated tau (AT8, brown) immunoreactive irregular axonal profiles found in deep white matter tracts CTE stage I. (T) Dense axonal varicosities, distorted axonal profiles and neurofibrillary tangles (arrows) characterize the cerebral cortex of CTE stage IV immunostained with phosphorylated neurofilament (SMI-34). Images from 10 µm tissue sections, scale bars = 100 µm, except O = 10 µm.
Figure 6.
The phosphorylated TDP43 pathology of CTE and CTE-MND. (A) pTDP-43 immunostained neurites found in periventricular region of the third ventricle in CTE II. (B) CTE stage II demonstrating pTDP-43 immunostained neurites in a perivascular distribution. (C) pTDP-43 immunoreactive inclusion in locus coeruleus in CTE stage II. (D) Clusters of pTDP-43 immunoreactive neurites in the subpial region of the brainstem in stage III CTE. (E) Perivascular pTDP-43 neurites in stage III CTE. (F) Subpial pTDP-43 neurites in the corpus callosum of stage IV CTE. (G) Dense pTDP-43 abnormalities in the temporal cortex of stage IV CTE-MND. (H) Dense pTDP-43 pathology of CA1 hippocampus in stage IV CTE. (I–O) (I) perivascular focus at sulcal depth pTDP-43 abnormalities are widespread throughout the CNS in CTE associated with MND (CTE-MND) (J, corpus callosum; K, cerebral peduncle; L, fornix; M, subpial region of frontal cortex; N, perivascular region frontal cortex; O, Rolandic cortex). All images: 50-µm tissue sections, all scale bars = 100 µm.
Clinical symptoms
Eleven of the 14 individuals with stage II CTE were symptomatic; common presenting symptoms were depression or mood swings, headaches and short-term memory loss. Three subjects presented with symptoms of MND. Symptoms in stage II subjects included depression or mood lability, explosivity, loss of attention and concentration, short-term memory loss and headache. Less common symptoms included executive dysfunction, impulsivity, suicidality and language difficulties (Tables 3 and 4).
Stage III chronic traumatic encephalopathy
Fifteen brains showed stage III pathology (Table 2, Cases 57–71). Grossly, most brains showed mild cerebral atrophy with dilation of the lateral and third ventricles; mean brain weight was 1394 ± 106.7 g. Septal abnormalities were found in 5 of the 12 intact brain specimens (42%) ranging from cavum septum, septal perforations or complete absence of the septum. Seven brains showed moderate depigmentation of the locus coeruleus (58%); six showed mild depigmentation of the substantia nigra (42%). Other common gross pathological features were atrophy of the mammillary bodies and thalamus, sharply convex contour of the medial thalamus, thinning of the hypothalamic floor and thinning of the corpus callosum. Microscopically, neurofibrillary tangles were widespread throughout superior frontal, dorsolateral frontal, inferior orbital, septal, insular, temporal pole, superior middle and inferior temporal and inferior parietal cortices. There were also extensive neurofibrillary tangles in the hippocampus, entorhinal cortex, amygdala, nucleus basalis of Meynert and locus coeruleus (Supplementary Table 3). Neurofibrillary tangles were frequent in olfactory bulbs, hypothalamus, mammillary bodies, substantia nigra and dorsal and median raphe nuclei. Sparse neurofibrillary tangles were found in Rolandic, cingulate cortices, thalamus, nucleus accumbens, dorsal motor nucleus of the vagus, dentate nucleus of the cerebellum and spinal cord. Severe axonal loss and distorted axonal profiles were found in the subcortical white matter, particularly affecting the frontal and temporal cortices (Fig. 5). TDP-43 immunoreactive neurites were evident in the cerebral cortex, medial temporal lobe or brainstem of most cases. Widespread, more severe TDP-43 neuronal and glial inclusions and neurites were found in three cases with stage III CTE diagnosed with CTE-MND.
Clinical symptoms
Family interview and medical record review were available for 12 subjects with stage III CTE; one individual was asymptomatic (Case 68). The most common presenting symptoms were memory loss, executive dysfunction, explosivity and difficulty with attention and concentration. Other symptoms frequently found in stage III subjects were depression or mood swings, visuospatial difficulties and aggression. Less common symptoms included impulsivity, apathy, headaches and suicidality. Seventy-five per cent of subjects were considered cognitively impaired. Two subjects developed symptoms of MND after the onset of cognitive or behavioural abnormalities, another developed cognitive changes after the onset of MND (Tables 3 and 4).
Stage IV chronic traumatic encephalopathy
Fifteen individuals were considered to have stage IV CTE (Table 2, Cases 72–86). Macroscopic brain changes included atrophy of the cerebral cortex and white matter and marked atrophy of the medial temporal lobe, thalamus, hypothalamus and mammillary body. Mean brain weight was significantly smaller than lower stage CTE (1208 ± 168.1 g; P < 0.001). Most brains showed ventricular enlargement, a sharply concave contour of the third ventricle, cavum septum pellucidum ranging in size from 0.5 to 1.0 cm, and septal perforations or septal absence. Pallor of the locus coeruleus and substantia nigra were found in all instances where it could be assessed. Microscopically, there was striking neuronal loss in the cortex, hippocampal sclerosis affecting CA1 and subiculum and astrocytic p-tau pathology. Severe p-tau abnormalities were found widely distributed throughout the cerebrum, diencephalon, basal ganglia, brainstem and spinal cord (Figs 1–4). Primary visual cortex was relatively spared. Subcortical white matter tracts showed marked axonal loss and distorted axonal profiles (Fig. 5). TDP-43 immunoreactivity was severe in most cases consisting of dense TDP-43 positive rounded and threadlike neurites, intraglial and intraneuronal inclusions in cerebral cortex, medial temporal lobe, diencephalon, basal ganglia, brainstem and, less frequently, spinal cord. Subpial, periventricular and perivascular TDP-43 immunoreactive neurites were also present (Fig. 6). In the most severely affected cases, there were dense cortical TDP-43 inclusions and neurites in all neocortical layers, particularly layer II, as well as occasional TDP-43-positive inclusions in the dentate fascia of the hippocampus.
Clinical symptoms
Family interview and medical record review were available on 13 subjects with stage IV CTE; all were symptomatic. Executive dysfunction and memory loss were the most common symptoms at onset, and all developed severe memory loss with dementia during their course. Most subjects also showed profound loss of attention and concentration, executive dysfunction, language difficulties, explosivity, aggressive tendencies, paranoia, depression, gait and visuospatial difficulties. Less common symptoms were impulsivity, dysarthria and parkinsonism; 31% were suicidal at some point in their course. Two of the 13 subjects developed symptoms of MND years after developing cognitive and behavioural abnormalities.
Professional American football players
Of the 35 former professional American football players (34 National Football League and one Canadian Football League), one showed no disease (Case 27, age 26 years), three had stage I/IV disease, three had stage II/IV, nine had stage III/IV disease, seven had stage IV/IV disease, two had CTE plus Alzheimer’s disease, four had CTE plus Lewy body disease, two had CTE plus Alzheimer’s disease and Lewy body disease, four had CTE plus FTLD and three had CTE-MND. One National Football League player had a primary diagnosis of Pick’s disease with only modest evidence of CTE (Case 102), one had a primary diagnosis of Lewy body disease with stage II CTE (Case 95) and another had a primary diagnosis of progressive supranuclear palsy with stage II CTE (Case 101). Thirty-one of the 34 former professional American football players had stage III–IV CTE or CTE plus co-morbid disease (89%). Sixteen former National Football League players had pure CTE stage III–IV (47%), 94% were symptomatic; the most common presenting symptoms were short-term memory loss, executive dysfunction and attention and concentration loss. Mean age at symptom onset was 54.1 ± 14.1 years (range 34–83 years). Positions played by National Football League players positive for CTE included offensive linemen (26%), running backs (20%), defensive linemen (14%), linebackers (14%), quarterbacks (6%), defensive backs (6%), tight ends (6%) and wide receivers (6%). Mean age at death for former National Football League players diagnosed with CTE was 67.1 ± 16.6 years (range 38–98 years).
Professional hockey players
Of the five former professional hockey players, the brain of one young player showed no signs of CTE (age 20 years). Three of the four former National Hockey League players had stage II CTE (75%), one had stage III CTE + Lewy body disease (25%) (mean age 51.3 years, range 28–73 years); only three of the four were symptomatic at the time of death.
Exposure to football, steroid use, position played and ApoE genotype
Of the 103 subjects, 58 played football as their primary sport. Of those, 42 subjects were diagnosed with CTE or CTE-MND; the families of 35 were available for structured interview regarding athletic exposure. These 35 brain donors (mean age 50.3 ± 23.3 years, range 17–98 years) played football for a mean of 11.9 ± 6.5 years (range 2–24 years). The number of years played (Spearman’s test, ρ = 0.805, P < 0.0001), years since retirement (Spearman’s test, ρ = 0.753, P < 0.0001) and age at death (Spearman’s test, ρ = 0.806, P < 0.0001) were significantly correlated with pathological stage of CTE. Family reported number of concussions (Spearman’s test, ρ = 0.259, P = 0.184); years of education (Spearman’s test, ρ = 0.258, P = 0.134), lifetime steroid use (Wilcoxon–Mann–Whitney test, P = 0.731) and position played (Kruskall–Wallis test, P = 0.407) were not significantly related to CTE stage. Furthermore, of the 68 individuals diagnosed with CTE, the proportion of the sample carrying at least one ApoE e4 allele was not significantly different than that observed in the general population (Chi-square goodness of fit, P = 0.334).
Military veterans
Sixteen of the 21 military veterans with CTE were also athletes, including eight National Football League players. Nine veterans saw combat: four in the Iraq and Afghanistan conflicts, one in the Gulf War, two in Vietnam and two in World War II. Three veterans with CTE experienced a moderate-to-severe traumatic brain injury while in service (one contusion, one intraparenchymal traumatic brain injury with persistent, poorly controlled post-traumatic epilepsy, one spinal cord injury). Three were exposed to blast from improvized explosive devices and explosive munitions; one athlete was also exposed to explosive munitions in Vietnam. Three veterans of the conflicts in Iraq and Afghanistan were diagnosed with post-traumatic stress disorder, two of whom were exposed to blast from improvized explosive devices and one who experienced repetitive concussive injuries during combat and in civilian life [four veterans of the Iraq and Afghanistan conflicts were also reported in Goldstein et al. (2012)].
Cause of death and suicide
Among the 51 subjects with CTE and CTE-MND, there were seven deaths from suicide; six others clearly expressed suicidal ideations at some point during their life (26% suicidal tendencies or completed suicide, 14% completed suicide). There were six deaths from drug or alcohol overdose (12%). The most common causes of death were respiratory failure (60% associated with CTE-MND), cardiac disease, suicide, overdose, failure to thrive associated with end-stage dementia and malignancy.
Discussion
CTE is a progressive tauopathy with distinctive clinical and pathological features that occurs after repetitive mild traumatic brain injury. Although historically, CTE has been primarily associated with boxing, CTE may also occur as a consequence of American football, hockey, wrestling, rugby and exposure to blast or concussive injury associated with military service (Corsellis and Brierley, 1959; Corsellis et al., 1973; Hof et al., 1991; McKenzie et al., 1996; Geddes et al., 1999; Omalu et al., 2005, 2006, 2010; McKee et al., 2009, 2010; Gavett et al., 2010, 2011; Costanza et al., 2011; Daneshvar et al., 2011a, b; Stern et al., 2011; Baugh et al., 2012; Goldstein et al., 2012; Saing et al., 2012). We analysed the brains of 85 individuals with a history of repetitive mild traumatic brain injury and found evidence of CTE in 80%; all males, ranging in age from 17 to 98 years (mean = 59.5 years), including 64 athletes, 21 military veterans (most of whom were also athletes) and one individual who engaged in self-injurious head-banging behaviour. The development of CTE in one individual in this series and two others in the literature in whom self-injurious head banging was the sole environmental exposure suggests that repetitive mild traumatic brain injury alone is sufficient to trigger CTE in some people (Hof et al., 1991; Geddes et al., 1999). Athletes with CTE included 50 football players (33 National Football League, one Canadian Football League, one semi-professional, nine college, six high school), four National Hockey League players, one amateur hockey player, seven professional boxers, one amateur boxer and one professional wrestler. Veterans with CTE included marines, soldiers and sailors from World War II, Vietnam, Gulf War, Iraq and Afghanistan.
Neuropathological staging of chronic traumatic encephalopathy
The evidence suggests that CTE begins focally, usually perivascularly, at the depths of the sulci in the cerebral cortex and spreads slowly over decades to involve widespread regions of neocortex, medial temporal lobe, diencephalon, basal ganglia, brainstem and spinal cord. The early, focal changes of CTE demonstrated here and by others (Hof et al.1991; Geddes et al., 1999) are distinctive from p-tau pathology of the Alzheimer type reported in some cognitively normal young adults (Braak and Del Tredici, 2011) and in association with other environmental exposures (Anthony et al., 2010). The tau isoform profile and phosphorylation state in CTE is similar to Alzheimer’s disease (Schmidt et al., 2001), and the neuronal tau pathology shows immunoreactivity to both 3R and 4R tau. The astrocytic p-tau pathology in CTE is predominantly 4R tau immunopositive; however, it is topographically distinct from the 4R tau immunoreactive thorn-shaped astrocytes that have been reported in the medial temporal lobe in ageing and Alzheimer’s disease (Lace et al. 2012; López-González et al., 2012).
We divided the topographically predictable pattern of p-tau pathology of CTE into four stages. Stage I was characterized by perivascular p-tau neurofibrillary tangles in focal epicentres at the depths of the sulci in the superior, superior lateral or inferior frontal cortex and was clinically associated with headache and loss of attention and concentration. In stage II CTE, neurofibrillary tangles were found in superficial cortical layers adjacent to the focal epicentres and in the nucleus basalis of Meynert and locus coeruleus. Individuals with stage II CTE experienced depression and mood swings, explosivity, loss of attention and concentration, headache and short-term memory loss. Stage III CTE showed macroscopic evidence of mild cerebral atrophy, septal abnormalities, ventricular dilation, a sharply concave contour of the third ventricle and depigmentation of the locus coeruleus and substantia nigra. There was dense p-tau pathology in medial temporal lobe structures (hippocampus, entorhinal cortex and amygdala) and widespread regions of the frontal, septal, temporal, parietal and insular cortices, diencephalon, brainstem and spinal cord. Most individuals with stage III CTE demonstrated cognitive impairment with memory loss, executive dysfunction, loss of attention and concentration, depression, explosivity and visuospatial abnormalities. Stage IV CTE was associated with further cerebral, medial temporal lobe, hypothalamic, thalamic and mammillary body atrophy, septal abnormalities, ventricular dilation and pallor of the substantia nigra and locus coeruleus. Microscopically, p-tau pathology involved widespread regions of the neuraxis including white matter, with prominent neuronal loss and gliosis of the cerebral cortex and hippocampal sclerosis. Subjects with stage IV CTE were uniformly demented with profound short-term memory loss, executive dysfunction, attention and concentration loss, explosivity and aggression. Most also showed paranoia, depression, impulsivity and visuospatial abnormalities. Advancing pathological stage was associated with a significant decrease in brain weight and increased severity of cognitive abnormalities supporting the validity of the pathological staging scheme. In addition, pathological stage correlated with duration of exposure to American football, survival after football and age at death in those who played football.
Spread of tau pathology
Under normal conditions in the mature human CNS, tau is primarily associated with microtubules in axons, where it is neither toxic nor associated with neurofibrillary pathology. Brain trauma causes some tau to become dissociated from microtubules in axons via mechanisms that most likely include intracellular calcium influx, glutamate receptor-mediated excitotoxicity and kinase activation mediating hyperphosphorylation of intracellular tau (Genis et al., 2000; Liang et al., 2009; Chen et al., 2010; Tran et al., 2011a, b; Schoch et al., 2012). Tau dissociated from microtubules may become abnormally phosphorylated, misfolded, aggregated and proteolytically cleaved by calpains and caspases, all of which are associated with neurotoxicity (Amadoro et al., 2006; Khlistunova et al., 2006; Zilka et al., 2006). Direct and indirect evidence for interneuronal tau transfer in animal models has recently suggested that interneuronal spreading of tau pathology may be due to transfer of toxic tau species between neurons (Clavaguera et al., 2009; Kim et al., 2010; DeCalignon et al., 2012; Liu et al., 2012). This might be mediated by either a prion-like templated misfolding of tau (Guo et al., 2011; DeCalignon et al., 2012; Liu et al., 2012; reviewed by Hall and Patuto, 2012) or by calcium dysregulatory effects of oligomeric or toxic N-terminal tau in the receiving neuron (Park and Ferreira, 2005; Frost et al., 2009). Although spreading of tau pathology is generally thought to occur in association with neuronal synapses, glial to glial spread, periventricular and diffuse extracellular tau migration patterns. CSF fluid enters the brain parenchyma along the Virchow–Robin spaces surrounding penetrating arteries, and brain interstitial fluid is cleared along paravenous drainage pathways suggesting a possible spread of tau pathology through this route, similar to the clearance of amyloid-ß peptide. Recent studies have demonstrated that amyloid-ß peptide (Iliff et al., 2012). Clearance through paravenous flow and the CSF might also regulate extracellular levels of p-tau and TDP-43 and explain the frequent perivascular, subpial and periventricular localization of these proteins.
Axonal injury and TDP-43
In addition to p-tau pathology, axonal injury was apparent in all stages of CTE, ranging from multifocal, often perivascular, axonal varicosities in the cortex and subcortical white matter in stages I–II to severe, diffuse axonal loss in the cortex and white matter in CTE stages III–IV. TDP-43 abnormalities were also found in the majority of CTE cases. In CTE stages I–III, sparse TDP-43 neurites were found in various regions of the cortex, medial temporal lobe and brainstem. In stage IV CTE, TDP-43 immunoreactivity was severe, with intraneuronal and intraglial inclusions, rounded and threadlike neurites in the cortex, white matter, diencephalon, basal ganglia and brainstem. Although it is well-established that p-tau pathology correlates with the severity of cognitive impairment in other tauopathies, such as Alzheimer’s disease (Wilcock and Esiri, 1982; McKee et al., 1991; Arriagada et al., 1992), the contribution of TDP-43 proteinopathy to symptoms of CTE cannot be overlooked, especially in late stage disease. As with frontotemporal dementia, CTE usually begins with behaviour and personality changes at mid-life (mean age of onset 44.3 years, range 17–83 ± 12.1 years). But, unlike Alzheimer’s disease or frontotemporal dementia, the clinical course of CTE is slow, progressing at a rate of 11–14 years between pathological stages. In addition, it is likely that axonal dysfunction and loss contribute to the production of clinical symptoms, especially in the early stages of CTE when tau pathology is focal and unlikely to account for the headache, attention and concentration loss, and memory difficulties experienced by subjects with stage I or II disease. Although the data suggest that CTE pathology is progressive, it remains to be determined whether some individuals are relatively resilient with static or even reversible pathology. Eleven per cent of individuals with CTE were asymptomatic, with a mean age at death of 59 years (range 26–87 years) and most with stage II disease, suggesting that CTE may not progress or may not progress at the same rate in all patients.
Chronic traumatic encephalopathy plus comorbid neurodegenerative disease
Of the 68 cases with CTE, 37% had co-morbid neurodegenerative disease, including MND, Parkinson’s disease or Lewy body disease, Alzheimer’s disease and FTLD. Repetitive traumatic brain injury and axonal injury might trigger molecular pathways that result in the overproduction and aggregation of other proteins prone to pathological accumulation in neurodegenerative disease including TDP-43, α-synuclein and amyloid-ß, thereby increasing the likelihood of MND, FTLD Lewy body disease or Alzheimer’s disease. Multiple epidemiological studies have shown that trauma is a risk factor for dementia, especially Alzheimer’s disease, as well as for amyotrophic lateral sclerosis and Parkinson’s disease (Plassman et al., 2000; Goldman et al., 2006; Schmidt et al., 2010; Pupillo et al., 2012). In addition, CTE and the accumulation of misfolded tau aggregates may promote the aggregation of pathological proteins through cross-seeding (Johan et al., 1998; Morales et al., 2009). Cross-seeding might explain the accumulation of TDP-43 in the large majority of CTE cases, its partial immunohistochemical co-location with tau and the particularly severe deposition of TDP-43 found in advanced CTE.
Chronic traumatic encephalopathy with motor neuron disease
Most subjects with CTE-MND (63%) presented with symptoms of MND, developing cognitive and behavioural symptoms several years after the onset of motor weakness, atrophy and fasciculations. The minority presented with apathy, depression, memory loss, cognitive decline, paranoia, impulsivity or executive dysfunction 1–8 years before the development of motor neuron symptoms. There was a tendency for subjects with CTE-MND to die from respiratory insufficiency at an earlier age (53.0 ± 14.3 years) than those without MND (55.8 ± 23.0 years), although the difference was not significant. Individuals with MND and CTE, independent of the stage of p-tau pathology, demonstrated severe TDP-43 pathology as neuronal, glial and neuritic inclusions involving widespread regions of the CNS including motor cortex and spinal cord.
Clinicopathological correlation
Neuroanatomical areas that are preferentially affected in CTE include superior, dorsolateral and lateral frontal cortices. Pathology in these regions may underlie the clinical features of disinhibition, lack of insight and poor executive function found in subjects even at early stages of CTE. Pathological involvement of the inferior temporal lobe and amygdala might contribute to the frontal symptoms and to the irritability, impulsivity, explosivity and outbursts of aggression so commonly experienced as early manifestations of CTE. Pathology of the nucleus basalis of Meynert and septal nuclei might contribute to the cognitive symptoms. Moreover, pathology in the subcallosal and inferior orbital frontal cortex and brainstem, especially the locus coeruleus and median raphe, might be related to the common symptoms of depression and mood lability. Mammillary body, anterior thalamic and hippocampal pathology most likely play a major role in producing memory loss, cognitive impairment and eventual dementia.
Even though the brain donors were not screened for cognitive impairments, an autopsy-based case series is limited by significant ascertainment bias, as families of individuals showing behavioural or cognitive symptoms are much more likely to initiate and participate in a brain donation programme than families of normally functioning individuals. Consequently, no generalizations regarding the incidence and prevalence of CTE in living athletes and veterans can be made. Furthermore, in several of the cases, the clinical symptoms were confounded by drug and alcohol abuse; therefore, the degree to which the extensive p-tau, TDP-43 and axonal pathology and neurodegeneration is responsible for the subject’s clinical presentation is unclear.
Inclusion of more rigorous control subjects, such as individuals who experienced repetitive mild traumatic brain injury and did not develop behavioural or cognitive abnormalities, will be extremely useful in future studies designed to delineate critical aspects of the traumatic exposure and susceptibility to trauma-induced neurodegeneration.
Future prospective longitudinal studies are planned to address these limitations. For instance, by studying a large number of retired National Football League athletes prospectively and conducting neuropathological analyses at death, a control group matched on age, education, athletic history, medical comorbidities and cause of death can be used to examine differences between individuals with and without clinical and neuropathological evidence of Similarly, current studies focused on a large cohort of Iraq and Afghanistan veterans with histories of blast and concussive traumatic brain injuries and post-traumatic stress disorder will shed light on the overlap between traumatic brain injury, CTE and post-traumatic stress disorder, as well as the role of combat-associated injury in producing CTE (Goldstein et al. 2012). Clinical criteria for the diagnosis of CTE need to be established and tested. Although ApoE does not appear to be a risk factor for the development of CTE or the severity of CTE pathology in this autopsy series, large prospective population-based studies need to be implemented to address this definitively (Gandy and DeKosky, 2012). The current results establish that a distinctive pattern of neuropathological changes, previously reported primarily in boxers, can also be found in other athletes and military veterans and provide a clear impetus for future studies.
CTE is a unique neurodegenerative condition that is associated with repetitive mild traumatic brain injury. Although there are many issues that require more thorough investigation, such as how much head trauma is causative, what type, and how frequent, the age when players are most susceptible and whether some individuals are genetically more prone than others, this study clearly shows that for some athletes and war fighters, there may be severe and devastating long-term consequences of repetitive brain trauma that has traditionally been considered only mild.
Funding
The Department of Veterans Affairs; Veterans Affairs Biorepository (CSP 501); Translational Research Center for Traumatic Brain Injury and Stress Disorders (TRACTS) Veterans Affairs Rehabilitation Research and Development Traumatic Brain Injury Center of Excellence (B6796-C to A.M.); National Institute of Aging Boston University Alzheimer’s Disease Center [P30 AG13846 to N.W.K.; supplement 0572063345-5 to A.C.M., R.A.S.]; National Institute of Aging Boston University Framingham Heart Study R01 [AG1649]; National Institute of Neurological Disorders and Stroke, National Institute of Aging, National Institute of Child Health and Human Development R01 [NS078337 to R.A.S.]; Sports Legacy Institute; National Operating Committee on Standards for Athletic Equipment, and the resources and use of facilities at the Edith Nourse Rogers Memorial Veterans Hospital in Bedford, MA. This work was also supported by an unrestricted gift from the National Football League. The funding sources were not involved in the preparation, review or approval of this manuscript.
Supplementary material
Supplementary material is available at Brain online.
Acknowledgements
The authors gratefully acknowledge the use of resources and facilities at the Edith Nourse Rogers Memorial Veterans Hospital (Bedford, MA), Lisa McHale and Dr. David Hemmy for their expert logistical assistance, Dr. Peter Davies (Albert Einstein College of Medicine) and Dr. Rohan de Silva (Queens Square, London) for antibodies. They also gratefully acknowledge the individuals and families whose participation and contributions made this work possible.
Glossary
Abbreviations
- CTE
chronic traumatic encephalopathy
- FTLD
frontotemporal lobar degeneration
- MND
motor neuron disease
References
- Amadoro G, Ciotti MT, Costanzi M, Cestari V, Calissano P, Canu N. NMDA receptor mediates tau-induced neurotoxicity by calpain and ERK/MAPK activation. Proc Natl Acad Sci USA. 2006;103:2892–7. doi: 10.1073/pnas.0511065103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anthony IC, Norrby KE, Dingwall T, Carnie FW, Millar T, Arango JC, et al. Predisposition to accelerated Alzheimer-related changes in the brains of human immunodeficiency virus negative opiate abusers. Brain. 2010;133:3685–98. doi: 10.1093/brain/awq263. [DOI] [PubMed] [Google Scholar]
- Arriagada PV, Growdon JH, Hedley-Whyte ET, Hyman BT. Neurofibrillary tangles but not senile plaques parallel duration and severity of Alzheimer’s disease. Neurology. 1992;42:631–9. doi: 10.1212/wnl.42.3.631. [DOI] [PubMed] [Google Scholar]
- Baugh CM, Stamm JM, Riley DO, Gavett BE, Shenton ME, Lin A, et al. Chronic traumatic encephalopathy: neurodegeneration following repetitive concussive and subconcussive brain trauma. Brain Imaging Behav. 2012;2:244–54. doi: 10.1007/s11682-012-9164-5. [DOI] [PubMed] [Google Scholar]
- Bigio EH. Update on recent molecular and genetic advances in FTLD. J Neuropathol Exp Neurol. 2008;67:635–48. doi: 10.1097/NEN.0b013e31817d751c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braak H, Braak E. Neuropathological staging of Alzheimer-related changes. Acta Neuropathol. 1991;82:239–59. doi: 10.1007/BF00308809. [DOI] [PubMed] [Google Scholar]
- Braak H, Braak E, Bohl J. Staging of Alzheimer-related cortical destruction. Eur Neurol. 1993;33:403–8. doi: 10.1159/000116984. [DOI] [PubMed] [Google Scholar]
- Braak H, Braak E. Morphological criteria for the recognition of Alzheimer’s disease and the distribution pattern of cortical changes related to this disorder. Neurobiol Aging. 1994;15:355–6. doi: 10.1016/0197-4580(94)90032-9. [DOI] [PubMed] [Google Scholar]
- Braak H, Del Tredici K. Nervous system pathology in sporadic Parkinson disease. Neurology. 2008;70:1916–25. doi: 10.1212/01.wnl.0000312279.49272.9f. [DOI] [PubMed] [Google Scholar]
- Braak H, Del Tredici K. The pathological process underlying Alzheimer's disease in individuals under thirty. Acta Neuropathol. 2011;121:171–81. doi: 10.1007/s00401-010-0789-4. [DOI] [PubMed] [Google Scholar]
- Brooks BR. El Escorial World Federation of Neurology criteria for the diagnosis of amyotrophic lateral sclerosis. Subcommittee on Motor Neuron Diseases/Amyotrophic Lateral Sclerosis of the World Federation of Neurology Research Group on Neuromuscular Diseases and the El Escorial ‘Clinical limits of amyotrophic lateral sclerosis’ workshop contributors. J Neurol Sci. 1994;124:96–107. doi: 10.1016/0022-510x(94)90191-0. [DOI] [PubMed] [Google Scholar]
- Brooks BR, Miller RG, Swash M, Munsat TL. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord. 2000;1:293–9. doi: 10.1080/146608200300079536. [DOI] [PubMed] [Google Scholar]
- Brown LM, Schinka JA. Development and initial validation of a 15-item informant version of the Geriatric Depression Scale. Int J Geriatr Psychiatry. 2005;20:911–8. doi: 10.1002/gps.1375. [DOI] [PubMed] [Google Scholar]
- Cairns NJ, Bigio EH, Mackenzie IR, Neumann M, Lee VM, Hatanpaa KJ, et al. Neuropathologic diagnostic and nosologic criteria for FTLD: consensus of the Consortium for Frontotemporal Lobar Degeneration. Acta Neuropathol. 2007;114:5–22. doi: 10.1007/s00401-007-0237-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen LJ, Wang YJ, Tseng GF. Compression alters kinase and phosphatase activity and tau and MAP2 phosphorylation transiently while inducing the fast adaptive dendritic remodeling of underlying cortical neurons. J Neurotrauma. 2010;27:1657–69. doi: 10.1089/neu.2010.1308. [DOI] [PubMed] [Google Scholar]
- Clavaguera F, Bolmont T, Crowther RA, Abramowski D, Frank S, Probst A, et al. Transmission and spreading of tauopathy in transgenic mouse brain. Nat Cell Biol. 2009;11:909–13. doi: 10.1038/ncb1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small GW, et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science. 1993;261:921–3. doi: 10.1126/science.8346443. [DOI] [PubMed] [Google Scholar]
- Costanza A, Weber K, Gandy S, Bouras C, Hof PR, Giannakopoulos G, et al. Review: Contact sport-related chronic traumatic encephalopathy in the elderly: clinical expression and structural substrates. Neuropathol Appli Neurobiol. 2011;37:570–84. doi: 10.1111/j.1365-2990.2011.01186.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corsellis JA, Brierley JB. Observations on the pathology of insidious dementia following head injury. J Ment Sci. 1959;105:714–20. doi: 10.1192/bjp.105.440.714. [DOI] [PubMed] [Google Scholar]
- Corsellis JA, Bruton CJ, Freeman-Browne D. The aftermath of boxing. Psychol Med. 1973;3:270–303. doi: 10.1017/s0033291700049588. [DOI] [PubMed] [Google Scholar]
- Critchley M. Punch-drunk syndromes: the chronic traumatic encephalopathy of boxers. In: Hommage à Clovis Vincent. Paris: Maloine, 1949. [Google Scholar]
- Critchley M. Medical Aspects of Boxing, Particularly from a Neurological Standpoint. Br Med J. 1957;1:357–62. doi: 10.1136/bmj.1.5015.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daneshvar DH, Baugh CM, Nowinski CJ, McKee AC, Stern RA, Cantu RC. Helmets and mouth guards: the role of personal equipment in preventing sport-related concussions. Clin Sports Med. 2011;30:145–63. doi: 10.1016/j.csm.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daneshvar DH, Nowinski CJ, McKee AC, Cantu RC. The epidemiology of sport-related concussion. Clin Sports Med. 2011;30:1–17. doi: 10.1016/j.csm.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Calignon A, Polydoro M, Suárez-Calvet M, William C, Adamowicz DH, Kopeikina KJ, et al. Propagation of tau pathology in a model of early Alzheimer’s disease. Neuron. 2012;73:685–97. doi: 10.1016/j.neuron.2011.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Tredici K, Rub U, De Vos RA, Bohl JR, Braak H. Where does parkinson disease pathology begin in the brain? J Neuropathol Exp Neurol. 2002;61:413–26. doi: 10.1093/jnen/61.5.413. [DOI] [PubMed] [Google Scholar]
- Dickson DW. Neuropathology of non-Alzheimer degenerative disorders. Int J Clin Exp Pathol. 2009;3:1–23. [PMC free article] [PubMed] [Google Scholar]
- Frost B, Jacks RL, Diamond MI. Propagation of tau misfolding from the outside to the inside of a cell. J Biol Chem. 2009;284:12845–52. doi: 10.1074/jbc.M808759200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvin JE, Roe CM, Powlishta KK, Coats MA, Muich SJ, Grant E, et al. The AD8: a brief informant interview to detect dementia. Neurology. 2005;65:559–64. doi: 10.1212/01.wnl.0000172958.95282.2a. [DOI] [PubMed] [Google Scholar]
- Gandy S, Dekosky ST. APOE ϵ4 status and traumatic brain injury on the gridiron or the battlefield. Sci Transl Med. 2012;4:134ed4. doi: 10.1126/scitranslmed.3004274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavett BE, Stern RA, Cantu RC, Nowinski CJ, McKee AC. Mild traumatic brain injury: a risk factor for neurodegeneration. Alzheimers Res Ther. 2010;2:18. doi: 10.1186/alzrt42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavett BE, Stern RA, McKee AC. Chronic traumatic encephalopathy: a potential late effect of sport-related concussive and subconcussive head trauma. Clin Sports Med. 2011;30:179–88. doi: 10.1016/j.csm.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geddes JF, Vowles GH, Nicoll JA, Revesz T. Neuronal cytoskeletal changes are an early consequence of repetitive head injury. Acta Neuropathol. 1999;98:171–8. doi: 10.1007/s004010051066. [DOI] [PubMed] [Google Scholar]
- Genis L, Chen Y, Shohami E, Michaelson DM. Tau hyperphosphorylation in apolipoprotein E-deficient and control mice after closed head injury. J Neurosci Res. 2000;60:559–64. doi: 10.1002/(SICI)1097-4547(20000515)60:4<559::AID-JNR15>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Goldman SM, Tanner CM, Oakes D, Bhudhikanok GS, Gupta A, Langston JW. Head injury and Parkinson’s disease risk in twins. Ann Neurol. 2006;60:65–72. doi: 10.1002/ana.20882. [DOI] [PubMed] [Google Scholar]
- Goldstein LE, Fisher AM, Tagge CA, Zhang XL, Velisek L, Sullivan JA, et al. Chronic traumatic encephalopathy in blast-exposed military veterans and a blast neurotrauma mouse model. Sci Transl Med. 2012;4:134ra60. doi: 10.1126/scitranslmed.3003716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo JL, Lee VM. Seeding of normal Tau by pathological Tau conformers drives pathogenesis of Alzheimer-like tangles. J. Biol Chem. 2011;286:15317–31. doi: 10.1074/jbc.M110.209296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall GF, Patuto BA. Is tau now ready for admission to the Prion club? Prion. 2012;6:223–233. doi: 10.4161/pri.19912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hof PR, Knabe R, Bovier P, Bouras C. Neuropathological observations in a case of autism presenting with self-injury behaviour. Acta Neuropathol. 1991;82:321–6. doi: 10.1007/BF00308819. [DOI] [PubMed] [Google Scholar]
- Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, et al. A paravascular pathway facilitates csf flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4:147 ra111. doi: 10.1126/scitranslmed.3003748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johan K, Westermark G, Engström U, Gustavsson A, Hultman P, Westermark P. Acceleration of amyloid protein A amyloidosis by amyloid-like synthetic fibrils. Proc Natl Acad Sci USA. 1998;95:2558–63. doi: 10.1073/pnas.95.5.2558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim WH, Lee S, Jung C, Ahmed A, Lee G, Hall GF. Interneuronal Transfer of Human Tau Between Lamprey Central Neurons in situ. J Alzheimer’s Dis. 2010;19:647–64. doi: 10.3233/JAD-2010-1273. [DOI] [PubMed] [Google Scholar]
- Khlistunova I, Biernat J, Wang Y, Pickhardt M, von Bergen M, Gazova Z, et al. Inducible expression of Tau repeat domain in cell models of tauopathy: aggregation is toxic to cells but can be reversed by inhibitor drugs. J BiolChem. 2006;281:1205–1214. doi: 10.1074/jbc.M507753200. [DOI] [PubMed] [Google Scholar]
- Lace G, Ince PG, Brayne C, Savva GM, Matthews FE, de Silva R, et al. Mesial temporal astrocyte tau pathology in the MRC-CFAS ageing brain cohort. Dement Geriatr Cogn Disord. 2012;3(34):15–24. doi: 10.1159/000341581. [DOI] [PubMed] [Google Scholar]
- Liang Z, Liu F, Iqbal K, Grundke-Iqbal I, Gong C-X. Dysregulation of tau phosphorylation in mouse brain during excitotoxic damage. J Alzheimers Dis. 2009;17:531–9. doi: 10.3233/JAD-2009-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litvan I, Hauw JJ, Bartko JJ, Lantos P, Daniel SE, Horoupian DS, et al. Validity and reliability of the preliminary NINDS neuropathologic criteria for progressive supranuclear palsy and related disorders. J Neuropathol Exp Neurol. 1996;55:97–105. doi: 10.1097/00005072-199601000-00010. [DOI] [PubMed] [Google Scholar]
- Liu L, Drouet V, Wu JW, Witter MP, Small SA, Clelland C, et al. Trans-synaptic spread of tau pathology in vivo. PLoS One. 2012;7:e31302. doi: 10.1371/journal.pone.0031302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-González I, Carmona M, Blanco R, Luna-Muñoz J, Martínez-Mandonado A, Mena R, et al. Characterization of thorn-shaped astrocytes in white matter of temporal lobe in Alzheimer disease brains. Brain Pathol. 2012 doi: 10.1111/j.1750-3639.2012.00627.x. doi: 10.1111/j.1750-3639.2012.00627.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenzie IR, Neumann M, Bigio EH, Cairns NJ, Alafuzoff I, Kril J, et al. Nomenclature and nosology for neuropathologic subtypes of FTLD: an update. Acta Neuropathol. 2010;119:1–4. doi: 10.1007/s00401-009-0612-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martland HS. Punch Drunk. JAMA. 1928;91:1103–7. [Google Scholar]
- McKee AC, Au R, Cabral HJ, Kowall NW, Seshadri S, Kubilus C, et al. Visual association pathology in preclinical Alzheimer’s disease. J Neuropath Exp Neurol. 2006;65:621–30. doi: 10.1097/00005072-200606000-00010. [DOI] [PubMed] [Google Scholar]
- McKee AC, Cantu RC, Nowinski CJ, Hedley-Whyte ET, Gavett BE, Budson AE, et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol. 2009;68:709–35. doi: 10.1097/NEN.0b013e3181a9d503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee AC, Gavett BE, Stern RA, Nowinski CJ, Cantu RC, Kowall NW, et al. TDP-43 proteinopathy and motor neuron disease in chronic traumatic encephalopathy. J Neuropathol Exp Neurol. 2010;69:918–29. doi: 10.1097/NEN.0b013e3181ee7d85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee AC, Kosik KS, Kowall NW. Neuritic pathology and dementia in Alzheimer's disease. Ann Neurol. 1991;30:156–65. doi: 10.1002/ana.410300206. [DOI] [PubMed] [Google Scholar]
- McKee A, Montine T, Alvarez V, Schantz A, Steinbart E, Bird T. Distinctive patterns of tau and tdp-43 in a former professional football player and marine as compared to 3 siblings. J Neuropathol Exp Neurol. 2011;70(6):517. [Google Scholar]
- McKeith IG, Galasko D, Kosaka K, Perry EK, Dickson DW, Hansen LA, et al. Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): Report of the consortium on DLB international workshop. Neurology. 1996;47:1113–24. doi: 10.1212/wnl.47.5.1113. [DOI] [PubMed] [Google Scholar]
- McKenzie JE, Roberts GW, Royston MC. Comparative investigation of neurofibrillary damage in the temporal lobe in Alzheimer’s disease, Down’s SYNDROME and dementia pugilistica. Neurodegeneration. 1996;5:259–64. doi: 10.1006/neur.1996.0034. [DOI] [PubMed] [Google Scholar]
- McNair DM, Kahn RJ, Frankenthaler LM, Faldetta LL. Amoxapine and amitriptyline. II. Specificity of cognitive effects during brief treatment of depression. Psychopharmacology (Berl) 1984;83:134–9. doi: 10.1007/BF00429721. [DOI] [PubMed] [Google Scholar]
- Millspaugh JA. Dementia pugilistica. US Naval Med Bulletin. 1937;35:297–61. [Google Scholar]
- Mirra SS, Heyman A, McKeel D, Sumi SM, Crain BJ, Brownlee LM, et al. The consortium to establish a registry for Alzheimer’s disease (CERAD): Part II standardization of the neuropathologic assessment of Alzheimer’s disease. Neurology. 1991;41:479–86. doi: 10.1212/wnl.41.4.479. [DOI] [PubMed] [Google Scholar]
- Montine TJ, Phelps CH, Beach TG, Bigio EH, Cairns NJ, Dickson DW, et al. National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease: a practical approach. Acta Neuropathol. 2012;123:1–11. doi: 10.1007/s00401-011-0910-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales R, Estrada LD, Diaz-Espinoza R, Morales-Scheihing D, Jara MC, Castilla J, et al. Molecular cross talk between misfolded proteins in animal models of Alzheimer’s and prion diseases. J Neurosci. 2010;30:4528–35. doi: 10.1523/JNEUROSCI.5924-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales R, Green KM, Soto C. Cross currents in protein misfolding disorders: interactions and therapy. CNS Neurol. Disord. Drug Targets. 2009;8:363–71. doi: 10.2174/187152709789541998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newell KL, Hyman BT, Growdon JH, Hedley-Whyte ET. Application of the National Institute on Aging (NIA)-Reagan Institute criteria for the neuropathological diagnosis of Alzheimer disease. J Neuropathol Exp Neurol. 1999;58:1147–55. doi: 10.1097/00005072-199911000-00004. [DOI] [PubMed] [Google Scholar]
- Omalu BI, DeKosky ST, Hamilton RL, Minster RL, Kamboh MI, Shakir AM, et al. Chronic traumatic encephalopathy in a national football league player: part II. Neurosurgery. 2006;59:1086–92. doi: 10.1227/01.NEU.0000245601.69451.27. discussion 92–3. [DOI] [PubMed] [Google Scholar]
- Omalu BI, DeKosky ST, Minster RL, Kamboh MI, Hamilton RL, Wecht CH. Chronic traumatic encephalopathy in a national football league player. Neurosurgery. 2005;57:128–34. doi: 10.1227/01.neu.0000163407.92769.ed. [DOI] [PubMed] [Google Scholar]
- Omalu BI, Bailes J, Hammers JL, Fitzsimmons RP. Chronic traumatic encephalopathy, suicides and parasuicides in professional American athletes: the role of the forensic pathologist. Am J Forensic Med Pathol. 2010;31:130–2. doi: 10.1097/PAF.0b013e3181ca7f35. [DOI] [PubMed] [Google Scholar]
- Park S-Y, Ferreira A. The Generation of a 17 kDa Neurotoxic Fragment: An Alternative Mechanism by which Tau Mediates ß-Amyloid-Induced Neurodegeneration. J Neurosci. 2005;25:5365–75. doi: 10.1523/JNEUROSCI.1125-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeffer RI, Kurosaki TT, Harrah CH, Chance JM, Filos S. Measurement of functional activities in older adults in the community. J Gerontol. 1982;37:323–9. doi: 10.1093/geronj/37.3.323. [DOI] [PubMed] [Google Scholar]
- Plassman BL, Havlik RJ, Steffens DC, Helms MJ, Newman TN, Drosdick D, et al. Documented head injury in early adulthood and risk of Alzheimer’s disease and other dementias. Neurology. 2000;55:1158–66. doi: 10.1212/wnl.55.8.1158. [DOI] [PubMed] [Google Scholar]
- Pupillo E, Messina P, Logroscino G, Zoccolella S, Chiò A, Calvo A, et al. EURamyotrophic lateral sclerosis Consortium. Trauma and amyotrophic lateral sclerosis: a case-control study from a population-based registry. Eur J Neurol. 2012 doi: 10.1111/j.1468-1331.2012.03723.x. doi: 10.1111/j.1468-1331.2012.03723.x. [DOI] [PubMed] [Google Scholar]
- Saing T, Dick M, Nelson PT, Kim RC, Cribbs DH, Head E. Frontal cortex neuropathology in dementia pugilistica. J Neurotrauma. 2012;29:1054–70. doi: 10.1089/neu.2011.1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt ML, Zhukareva V, Newell KL, et al. Tau isoform profile and phosphorylation state in dementia pugilistica recapitulate Alzheimer’s disease. Acta Neuropathol. 2001;101:518–24. doi: 10.1007/s004010000330. [DOI] [PubMed] [Google Scholar]
- Schmidt S, Kwee LC, Allen KD, Oddone EZ. Association of amyotrophic lateral sclerosis with head injury, cigarette smoking and APOE genotypes. J Neurol Sci. 2010;291:22–9. doi: 10.1016/j.jns.2010.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoch KM, Evans HN, Brelsfoard JM, Madathil SK, Takano J, Saido TC, et al. Calpastatin overexpression limits calpain-mediated proteolysis and behavioural deficits following traumatic brain injury. Exp Neurol. 2012;236:371–82. doi: 10.1016/j.expneurol.2012.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern RA, Riley DO, Daneshvar DH, Nowinski CJ, Cantu RC, McKee AC. Long-term consequences of repetitive brain trauma: chronic traumatic encephalopathy. PM R. 2011;3:S460–7. doi: 10.1016/j.pmrj.2011.08.008. [DOI] [PubMed] [Google Scholar]
- Tran HT, Sanchez L, Esparza TJ, Brody DL. Distinct temporal and anatomical distributions of amyloid-β and tau abnormalities following controlled cortical impact in transgenic mice. PLoS One. 2011a;6:e25475. doi: 10.1371/journal.pone.0025475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran HT, LaFerla FM, Holtzman DM, Brody DL. Controlled cortical impact traumatic brain injury in 3xTg-Alzheimer’s disease mice causes acute intra-axonal amyloid-β accumulation and independently accelerates the development of tau abnormalities. J Neurosci. 2011b;31:9513–25. doi: 10.1523/JNEUROSCI.0858-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vonsattel JPG, Aizawa H, Ge P, DiFiglia M, McKee AC, MacDonald M, et al. An improved approach to prepare human brains for research. J Neuropathol Exp Neurol. 1995;54:42–56. doi: 10.1097/00005072-199501000-00006. [DOI] [PubMed] [Google Scholar]
- Wilcock GK, Esiri MM. Plaques, tangles and dementia: a quantitative study. J Neurol Sci. 1982;56:343–56. doi: 10.1016/0022-510x(82)90155-1. [DOI] [PubMed] [Google Scholar]
- Zilka N, Filipcik P, Koson P, Fialova L, Skrabana R, Zilkova M, et al. Truncated tau from sporadic Alzheimer’s disease suffices to drive neurofibrillary degeneration in vivo. FEBS Lett. 2006;580:3582–8. doi: 10.1016/j.febslet.2006.05.029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.