Abstract
Background:
Data about the health-related quality of life (HR-QOL) of people living with HIV/AIDS (PLHA) after the implementation of free antiretroviral treatment in India are scarce.
Aim:
The study was to describe the HR-QOL and gender differences of PLHA in rural India.
Materials and Methods:
Cross sectional study of 120 PLHA who came to the outpatient department in a rural district hospital. Assessment of the HR-QOL was performed through interviews using a validated structured questionnaire from the Medical Outcome Study HIV Health Survey. Linear regression with robust standard errors was used for multivariable analysis.
Results:
Domains related to social and daily activities such as cognitive, role and social functioning had lower HR-QOL scores than domains related to physical health. Men had higher scores of HR-QOL in health transition, perceived HR-QOL, health distress, social functioning and role functioning. In multivariable analysis, factors associated with poorer HR-QOL were female sex, lower levels of education and being widowed or separated in women.
Conclusions:
HR-QOL of PLHA in rural India is poor, especially in widowed or separated women and people with lower levels of education. There is an urgent need of implementing programmes for improving the HR-QOL of HIV infected women in rural India.
Keywords: Domain, Education, Gender, HIV, Quality of life, Women
Introduction
The World Health Organization (WHO) defines health as a state of complete physical, mental, and social well-being and not merely the absence of disease. In general terms, quality of life extends beyond health. It may include satisfaction with one's geographic location, access to education, or level of income. Measurement of health must not only include estimates of the frequency and severity of diseases, but also well-being and health-related quality of life (HR-QOL).[1]
People living with HIV/AIDS (PLHA) need to cope with a range of HIV-related symptoms for extended periods. These symptoms may be related to the infection itself, co-morbid illnesses, or iatrogenic effects from HIV-related medication.[2] In addition, many of the patients struggle with numerous social problems such as stigma, poverty, depression, substance abuse, and cultural beliefs which can affect their HR-QOL, not only from the physical health aspect, but also from mental and social health point of view.
HR-QOL can be measured with a variety of multidimensional generic and disease specific instruments, some of which have been specifically developed for PLHA.[1] The assessment of the HR-QOL is useful for assessing patients’ perceived burden of chronic disease, tracking changes on health over time, assessing the effects of treatment and quantifying the return on health care investment.[2] Moreover, the assessment of HR-QOL is central for understanding how people's lives are affected by HIV infection and can help health care providers in planning of individual interventions for those areas and subgroups where HR-QOL is a significant problem.[3]
With the implementation of highly active antiretroviral therapy (ART) in developed and developing countries, HIV infection has become a chronic disease. The majority of the studies on HRQOL of PLHA in India have been performed before the complete implementation of free ART in the country, which happened approximately in 2007.[4–7] In some of these studies, important differences in HR-QOL between men and women were found, indicating that men had higher scores in domains related to psychological well being, positive feelings, sexual activity and financial resources.[4,8] However, many of the patients that were involved in these studies had severe physical problems related to opportunistic infection or other HIV-related diseases,[8] so the results of these studies may not be fully applicable to most PLHA living in India today. Moreover, these studies have been performed in urban settings by tertiary care centers, so information of HR-QOL of PLHA in rural areas is lacking. A better knowledge of the characteristics of HIV in rural area is important to understand the characteristics of the HIV epidemic in India, because two thirds of 2.4 million PLHA in India are rural residents.[9,10] The main objective of the present study was to describe the HR-QOL of men and women living with HIV/AIDS in a rural area of India.
Materials and Methods
The study was performed in the RDT Bathalapalli Hospital, Andhra Pradesh, India. The hospital belongs to a non-governmental organization called Rural Development Trust, and provides health care free of cost to PLHA. The study was approved by the Institutional Ethical Committee and all patients gave written informed consent.
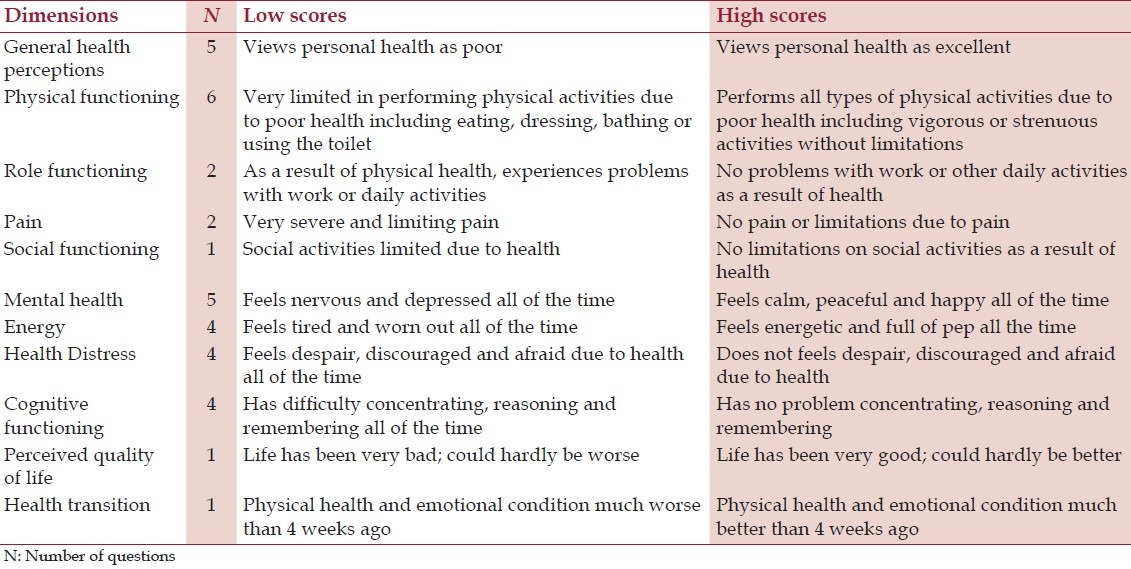
We carried out a descriptive cross sectional study on a stratified random sample of 60 men and 60 women who attended the outpatient section of the Department of Infectious Diseases during the second half of the year 2011. Only patients aged above 18 years were included in our study. After explaining the purpose of study, inform consent was taken to all patients before the interview. Interviews were done using a validated structured questionnaire of Medical Outcome Study (MOS) HIV health survey.[11] The MOS-HIV health survey was created for assessing the functional status and well-being of PLHA in multiple settings. The MOS-HIV Health Survey consists of 35 questions which assess 11 dimensions of HR-QOL including general health perceptions, physical functioning, role functioning, pain, social functioning, mental health, energy, health distress, cognitive functioning, perceived quality of life and health transition [Table 1].[12] Scores for dimensions range from 0 to 100, where higher scores indicate better health.
Table 1.
Description of domains in the HIV-MOS health survey
Statistical analysis
Statistical analysis was performed using Stata Statistical Software (Stata Corporation. Release 11, College Station, Texas, USA). Univariable analysis was performed with Student's t-test for continuous variables and Chi-square test for categorical variables. Linear regression with robust standard errors was used for the multivariable analysis of socio demographic factors associated with HR-QOL scores, so positive coefficients indicate positive linear relationship, negative coefficients indicate negative linear relationship and 0 indicates no linear relationship.[13] Internal consistency was calculated using scale reliability coefficients (Cronbach's alpha) with standardized items.
Results
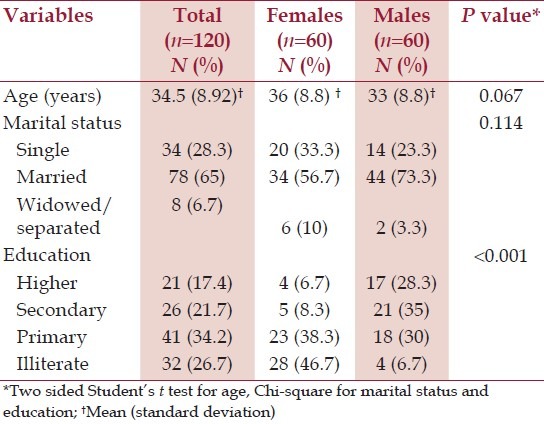
The characteristics of the patients are described in Table 2. The mean age of the patients was 34 years, almost two thirds were married and 27% were illiterate. Women had lower levels of education than men.
Table 2.
Demographic characteristics of patients by gender
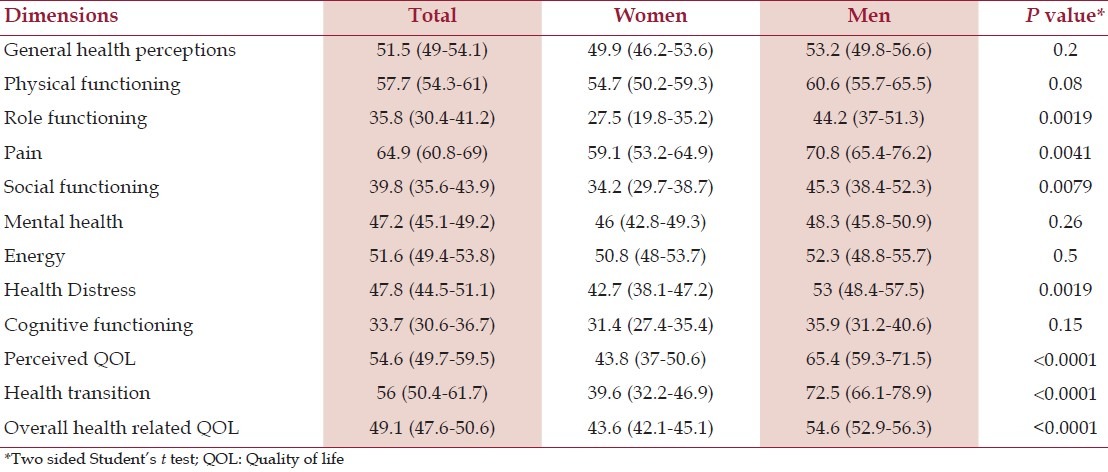
Scores of HR-QOL stratified by gender are presented in Table 3. Lowest mean scores were observed for cognitive, role and social functioning. Mean scores of HR-QOL were higher in men than in women in all HR-QOL domains. Men had significantly higher scores of HR-QOL in health transition, perceived quality of life, health distress, social functioning and role functioning. The overall scale reliability coefficient was 0.53. By gender, the scale reliability coefficient was 0.54 for females and 0.58 for males.
Table 3.
Mean and 95% confidence interval for each domain score in the HIV-medical outcome study health survey
Multivariable regression analysis of socio-demographic factors associated with higher HR-QOL scores are presented in Table 4. Factors associated with better HR-QOL were being married, not being illiterate and male sex. We found important differences between men and women. Single or widowed/separated women had lower scores of HR-QOL than married women, but marital status was not an important factor for determining HR-QOL in men. In both men and women, having higher education was associated with better HR-QOL. Compared to women who finished primary or secondary education, illiterate women had worse HR-QOL, but this was not observed in men.
Table 4.
Linear regression multivariable analysis with robust standard errors of overall health related quality of life scores stratified by gender
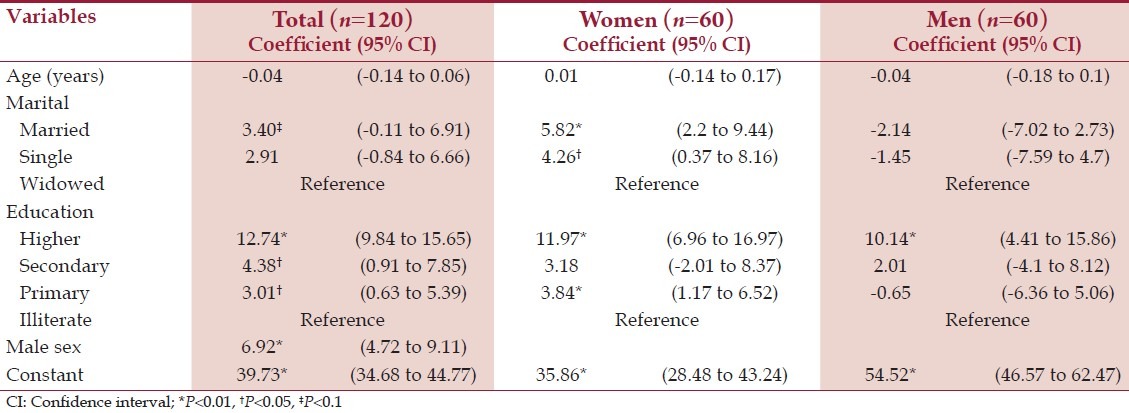
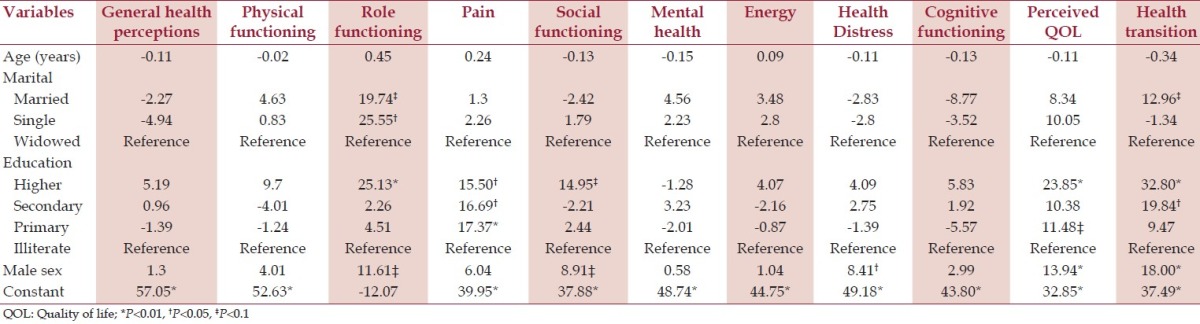
Coefficients of linear regression analysis for each domain of the HIV-MOS health survey are presented in Table 5. Being widowed or separated was associated with worse role functioning. Being illiterate was associated with lower scores in pain and perceived quality of life, whereas having higher education was associated with having higher scores in role and social functioning.
Table 5.
Coefficients of linear regression analysis with robust standard errors for each domain of the medical outcome study-HIV health survey
Discussion
To our knowledge, this is the first published study describing the HR-QOL of PLHA living in rural areas of India. Unlike other studies performed before the implementation of free ART in India,[7] domains related to physical health such as pain or physical functioning had higher scores than other domains. In a study performed on 60 patients taking ART in an urban setting in Chennai, South India, the lowest HR-QOL scores were seen in social domains.[14] Similarly, in our study the lowest scores were seen as well in domains related to social and daily activities such as role, social and cognitive functioning, probably due to the stigma and discrimination associated with HIV infection in India.[15]
Gender differences are important for explaining the HIV epidemic in rural India.[9,16] We found that women have poorer HR-QOL than men. Although there was no significant difference in cognitive functioning, women had poorer perception of their health and their quality of life, and consequently, women had more problems in their daily and social activities than men. Our results are in accordance with other two urban studies performed in South India, indicating that HIV infected women have poorer HR-QOL than men both in urban and rural areas of India.[5,8]
The poorest HR-QOL scores were seen in illiterate persons and widowed/separated women. The negative impact of low educational levels in the HR-QOL of PLHA in India has been previously described.[14,17] Stigma, discrimination and lack of support, even from relatives and friends, are common in widowed or separated women living with HIV in rural areas of India.[18,19] These data indicate that there is a need to implement specific programmes for improving the HR-QOL of women infected by HIV in India, especially illiterate or widowed/separated women.[20] These programmes should aim to improve the social and economical status of HIV infected women with the objective of achieving economic independence and building a social network, sometimes outside of their families, where they can feel safe.
The study has some limitations. We did not collect clinical information such as CD4 + lymphocyte count, concomitant diseases or treatment of patients. Therefore, our linear regression models performed poorer in domains related to physical health such as physical and cognitive functioning, general health perceptions, and energy and health distress. Including clinical data related to HIV infection would have improved the predictive power of these models. While scale reliability coefficients improved somewhat after stratification by gender, the scale reliability coefficient was lower than in previous studies,[12] indicating poor inter-domain consistency of the MOS-HIV health survey in our setting. Moreover, we did not include other important factors that could affect the HR-QOL of the patients such as the mode of transmission or the time since HIV diagnosis.
Conclusion
The results of this study demonstrate that PLHA in rural India have poor HR-QOL. Compared to previous studies performed before the implementation of free ART in India, we have observed an improvement in domains related to physical health, but not in domains related to social and daily activities. We found that specific groups, widowed or separated women and people with lower levels of education, had the lowest HR-QOL scores and, therefore, they are more vulnerable than others. These results can be used to design target programmes for improving the HR-QOL of PLHA in rural areas of India.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Franchi D, Wenzel RP. Measuring health-related quality of life among patients infected with human immunodeficiency virus. Clin Infect Dis. 1998;26:20–6. doi: 10.1086/516262. [DOI] [PubMed] [Google Scholar]
- 2.Basavaraj KH, Navya MA, Rashmi R. Quality of life in HIV/AIDS. Indian J Sex Transm Dis. 2010;31:75–80. doi: 10.4103/2589-0557.74971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rüütel K, Uusküla A, Minossenko A, Loit HM. Quality of life of people living with HIV and AIDS in Estonia. Cent Eur J Public Health. 2008;16:111–5. doi: 10.21101/cejph.a3461. [DOI] [PubMed] [Google Scholar]
- 4.Solomon S, Venkatesh KK, Brown L, Verma P, Cecelia AJ, Daly C, et al. Gender-related differences in quality of life domains of persons living with HIV/AIDS in South India in the era prior to greater access to antiretroviral therapy. AIDS Patient Care STDS. 2008;22:999–1005. doi: 10.1089/apc.2008.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahalakshmy T, Premarajan K, Hamide A. Quality of life and its determinants in people living with human immunodeficiency virus infection in puducherry, India. Indian J Community Med. 2011;36:203–7. doi: 10.4103/0970-0218.86521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kohli RM, Sane S, Kumar K, Paranjape RS, Mehendale SM. Modification of medical outcome study (MOS) instrument for quality of life assessment and its validation in HIV infected individuals in India. Indian J Med Res. 2005;122:297–304. [PubMed] [Google Scholar]
- 7.Kohli RM, Sane S, Kumar K, Paranjape RS, Mehendale SM. Assessment of quality of life among HIV-infected persons in Pune, India. Qual Life Res. 2005;14:1641–7. doi: 10.1007/s11136-004-7082-8. [DOI] [PubMed] [Google Scholar]
- 8.Chandra PS, Satyanarayana VA, Satishchandra P, Satish KS, Kumar M. Do Men and Women with HIV Differ in their Quality of Life? A study from South India. AIDS Behav. 2009;13:110–7. doi: 10.1007/s10461-008-9434-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alvarez-Uria G, Midde M, Pakam R, Naik PK. Gender differences, routes of transmission, socio-demographic characteristics and prevalence of HIV related infections of adults and children in an HIV cohort from a rural district of India. Infect Dis Rep. 2012;4:e19. doi: 10.4081/idr.2012.e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.USAID. INDIA. HIV/AIDS Health Profile. 2010. Dec, [Accessed September 27, 2012]. at http://www.usaid.gov/our_work/global_health/aids/Countries/asia/india_profile.pdf .
- 11.Grossman HA, Sullivan PS, Wu AW. Quality of life and HIV: Current assessment tools and future directions for clinical practice. AIDS Read. 2003;13:583–90. [PubMed] [Google Scholar]
- 12.Albert W Wu. MOS HIV Health Survey Manual. [Accessed August 3, 2012]. at http://www.jhsph.edu/research/affiliated.programs/medical.outcomes.study.HIV/User_manual/index.html .
- 13.Norris CM, Ghali WA, Saunders LD, Brant R, Galbraith D, Faris P, et al. Ordinal regression model and the linear regression model were superior to the logistic regression models. J Clin Epidemiol. 2006;59:448–56. doi: 10.1016/j.jclinepi.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 14.Nirmal B, Divya KR, Dorairaj VS, Venkateswaran K. Quality of life in HIV/AIDS patients: A cross-sectional study in south India. Indian J Sex Transm Dis. 2008;29:15. [Google Scholar]
- 15.Charles B, Jeyaseelan L, Pandian AK, Sam AE, Thenmozhi M, Jayaseelan V. Association between stigma, depression and quality of life of people living with HIV/AIDS (PLHA) in South India-A community based cross sectional study. BMC Public Health. 2012;12:463. doi: 10.1186/1471-2458-12-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alvarez-Uria G, Midde M, Pakam R, Kannan S, Bachu L, Naik PK. Factors Associated with late presentation of HIV and estimation of antiretroviral treatment need according to CD4 + lymphocyte count in a resource-limited setting: Data from an HIV cohort study in India. Interdiscip Perspect Infect Dis. 2012;2012:293795. doi: 10.1155/2012/293795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wig N, Lekshmi R, Pal H, Ahuja V, Mittal CM, Agarwal SK. The impact of HIV/AIDS on the quality of life: A cross sectional study in north India. Indian J Med Sci. 2006;60:3–12. [PubMed] [Google Scholar]
- 18.Alvarez-Uria G, Midde M, Naik PK. Socio-demographic risk factors associated with HIV infection in patients seeking medical advice in a rural hospital of India. J Public health Res. 2012;1:e14. doi: 10.4081/jphr.2012.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pallikadavath S, Garda L, Apte H, Freedman J, Stones RW. HIV/AIDS in rural India: Context and health care needs. J Biosoc Sci. 2005;37:641–55. doi: 10.1017/S0021932004006893. [DOI] [PubMed] [Google Scholar]
- 20.Crook J, Browne G, Roberts J, Gafni A. Impact of support services provided by a community-based AIDS service organization on persons living with HIV/AIDS. J Assoc Nurses AIDS Care. 2005;16:39–49. doi: 10.1016/j.jana.2005.05.003. [DOI] [PubMed] [Google Scholar]


