Dear Editor,
Anaphylactic shock following wasp sting is an emergency, often treated with intravenous antihistaminics, steroids and epinephrine. The administration of epinephrine in these situations remains controversial, as it worsens the coronary vasospasm and may precipitate a myocardial infarction.
A 30-year-old male patient, presented to the emergency department 3 hours after being stung by multiple wasps [Figure 1a]. The patient gave history of precordial chest pain, diaphoresis, palpitations, and syncope following the stings. He did not smoke and did not have any significant medical illnesses in the past. At admission, the patient was drowsy with cold and clammy extremities. Peripheral pulses were not palpable and blood pressure was not recordable. Bradycardia with a heart rate of 40/min was recorded. Heart sounds were muffled.
Figure 1.
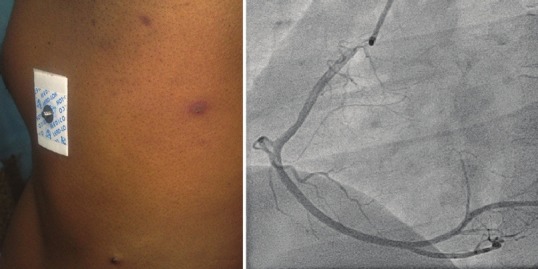
(a) Two wasp sting lesions on the left side of chest and axilla of the patient, (b) Angiogram showing normal coronaries of the patient
In the emergency room, patient was started on resuscitative measures; intravenous (IV) normal saline-2 liters, intramuscular adrenaline 0.5 mg (1:1000), hydrocortisone 100 mg IV and chlorpheniramine maleate 10 mg IV were administered. There was no immediate improvement in blood pressure or heart rate. Electrocardiogram showed ST segment elevation in leads II, III, aVF with reciprocal ST depression in I, aVL, V2, V3 and sinus bradycardia with first degree heart block [Figure 2a, b]. Cardiac biomarkers were elevated (Creatine Kinase Total {CK}-533IU/L, CK-MB isoform-41 IU/L), troponin T was negative. Echocardiography revealed hypokinesia of inferior and posterior walls. A diagnosis of inferior wall and posterior wall myocardial infarction with right ventricular wall extension, first degree heart block and anaphylactic or cardiogenic shock following wasp stings, was made. Heart rate normalized and blood pressure stabilized at 94/70 mmHg with vasopressors. Thrombolysis with intravenous streptokinase 1.5 million units was started. No adverse reactions to streptokinase were noted. Sensorium improved and patient was planned for angiography. Coronary arteries were normal on angiography [Figure 1b]. Work up for hyperlipidemia and hyperhomocysteinemia were normal except for low HDL (28 mg/dl). Serum tryptase levels could not be done due to lack of this facility at our institute. Patient's echocardiographic evaluation at the end of one week of hospital stay was normal. The patient is asymptomatic on follow-up.
Figure 2.
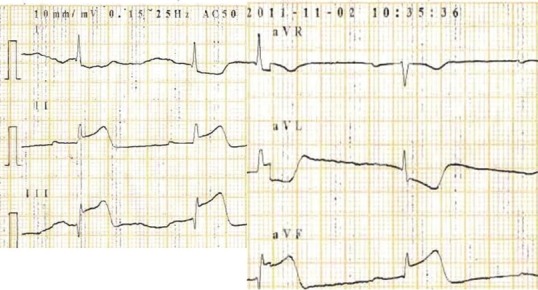
ECG showing ST elevation in leads II, III, aVF and ST depression in aVR and aVL leads
Wasp belongs to the Hymenoptera genus and its sting initiates IgE mediated Type I hypersensitivity reaction, mast cell and basophil degranulation, leading to anaphylaxis. Large amount of venom is released by these insects in cases of mass stinging incidents. The wasp venom is toxic and contains active amines (serotonin, histamine, tyramine, catecholamines), kinins (like bradykinin) and mastoparan (histamine releasing peptides), phospholipases and hyaluronidases.[1] Mass stinging by hundreds of wasps can also precipitate coronary spasm due to direct toxicity of the venom.
Cardiac involvement in anaphylaxis is due to release of basophil and mast cell derived mediators into the circulation during an IgE mediated hypersensitivity reaction. Heart itself has mast cells which are located near small intramural coronary arteries, as well as in the wall of large epicardial vessels. Activated mast cells release the renin, chymase, histamine, leukotriene C4, platelet activating factor (PAF) etc., Renin and chymase-released from activated cardiac mast cells initiate activation of the local (cardiac) renin-angiotensin system (RAS) and causes vasoconstriction. Leukotrienes also cause a marked constriction of the small intramural coronary vessels. PAF released within systemic circulation induces peripheral vasodilation with relative hypovolemia and severe hypotension. Histamine induced stimulation of the H1 receptor leads to a reduction of coronary blood flow either from vasodilation of small coronary resistance vessels or from stimulation of vasoconstricting H1 receptors of large epicardial coronary arteries. Histamine may also be involved in arrhythmias during anaphylaxis.[2,3] Intravenous epinephrine, used to treat anaphylactic shock can also cause coronary vasoconstriction.
Allergic angina is called as Kounis syndrome. It is the concurrence of an allergic episode causing release of inflammatory mediators and precipitating anginal chest pain.[3] Allergic angina may evolve to allergic myocardial infarction (MI). Type 1 Kounis syndrome refers to chest pain, normal or raised cardiac enzymes and ECG abnormality secondary to coronary spasm, accompanying an allergic reaction, in a patient with normal coronaries. Type 2 Kounis syndrome refers to allergic angina or MI, due to coronary spasm, plaque erosion or rupture, in patients with atherosclerosed coronaries.[3] Right coronary artery is commonly involved and regional wall motion abnormality resolves by 1-4 weeks in patients with Type 1 Kounis syndrome.[4] Kounis syndrome has been reported in patients with allergic reaction to drugs, drug eluting stents, asthma, exercise, food and serum sickness apart from environmental triggers.[4] Intramuscular or subcutaneous epinephrine (1:1000) is useful for anaphylactic shock, however, in view of exacerbation of coronary vasoconstriction, its use in Kounis syndrome remains controversial.
Our patient had allergic MI, following wasp sting, with ST elevation in ECG, raised cardiac biomarkers, transient regional wall motion abnormalities and angiographically normal coronaries, fitting into Type 1 Kounis syndrome. This case is being reported due to its rarity and to emphasize the importance of early recognition of Kounis syndrome.
References
- 1.Vetter RS, Visscher PK, Camazine S. Mass envenomations by honey bees and wasps. West J Med. 1999;170:223–7. [PMC free article] [PubMed] [Google Scholar]
- 2.Triggiani M, Patella V, Staiano RI, Granata F, Marone G. Allergy and the cardiovascular system. Clin Exp Immunol. 2008;153:7–11. doi: 10.1111/j.1365-2249.2008.03714.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kounis NG, Mazarakis A, Tsigkas G, Giannopoulos S, Goudevenos J. Kounis syndrome: A new twist on an old disease. Future Cardiol. 2011;7:805–24. doi: 10.2217/fca.11.63. [DOI] [PubMed] [Google Scholar]
- 4.Biteker M. Current understanding of Kounis syndrome. Expert Rev Clin Immunol. 2010;6:777–88. doi: 10.1586/eci.10.47. [DOI] [PubMed] [Google Scholar]


