Abstract
Objective
Adolescent weight and depressive symptoms are serious population health concerns in their own right and as they relate to each other. This study asks whether relationships between weight and depressive symptoms vary by sex and race/ethnicity because both shape experiences of weight and psychological distress.
Methods
Results are based on multivariate analyses of National Longitudinal Study of Adolescent Health (Add Health) data.
Results
There are no associations between adolescent girls’ weight and depressive symptoms, but these associations vary considerably among boys. Underweight is associated with depressive symptoms among all boys and subpopulations of White and Hispanic boys. Among Hispanic boys, those who are overweight (versus normal weight) have a lower probability of reporting depressive symptoms. Finally, among normal weight boys, Hispanics and Blacks are more likely to report depressive symptoms than Whites.
Conclusions
Findings are a reminder that understanding population health issues sometimes requires a focus on subpopulations, not simply the population as a whole.
Keywords: underweight, overweight, obese, CES-D, depressive symptoms, health disparities
Normal weight adolescents are now a minority in the United States (US), which makes weight one of the most important population health issues that young people face today. More than half of all 12-19 year olds are currently overweight and 17% of this group is obese (Ogden et al. 2006). A small proportion of US adolescents also struggle with being underweight.
Weight clearly influences adolescents’ short- and long-term physical health (Daniels 2006) but evidence about its impact on psychological health is less clear. For example, few studies find widespread consequences for adolescent depressive symptoms (see Wardle and Cooke 2005 for a review) despite the powerful stigma of weight (Puhl, Andreyeva, and Brownell 2008). The majority of this research focuses on the consequences of body mass index (BMI) (e.g., Needham and Crosnoe 2005) or obesity (e.g., Mustillo et al. 2003), while some studies focus exclusively on samples of overweight and obese adolescents (e.g., Britz et al. 2000).
This study posits that limited evidence of associations between weight and depressive symptoms may arise if the relationship is nonlinear or not evident for all adolescents. We hypothesize that adolescents at the top and bottom of the weight continuum are at risk of depressive symptoms. We also posit that relationships between weight and adolescent depressive symptoms vary by gender and race/ethnicity given gender and race/ethnic differences in both weight and depressive symptoms. We analyze data from the National Longitudinal Study of Adolescent Health (Add Health) to test these hypotheses. To our knowledge, this is the first nationally representative study that considers whether the intersection of adolescents’ weight, gender and race/ethnicity is associated with depressive symptoms. Findings provide new information about US adolescent subpopulations that are at risk of depressive symptoms and in need of intervention to cope with these symptoms.
Background
Adolescence is a life course stage marked by many physiological and psychological transitions. For example, the onset of puberty occurs and brings about rapid physical development and increased sexual and gender differentiation between boys and girls. During this time, weight takes on new meaning and weight concerns increase (Field et al. 2001). The risk of the onset of depressive symptoms also increases during adolescence, with girls more likely than boys to report them (Wade, Cairney, and Pevalin 2002).
Theory on weight stigma suggests that weight and adolescent depressive symptoms should be related given the poor treatment that overweight individuals face. Weight is a physical characteristic and marker of health status that is easily observed by others, making it easy to label and stigmatize individuals who are “too heavy” or “too thin.” Experiments demonstrate that individuals stereotype and avoid overweight persons (Dejong 1980; Puhl and Brownell 2006); that children and adults are unlikely to befriend an obese person relative to persons with other stigmatizing physical characteristics (Latner, Stunkard, and Wilson 2005); and that young people rate overweight individuals as being unhealthy, ugly, lazy, dirty and stupid (Allon 1982; Crandall and Schiffhauer 1998). Recent research suggests that weight stigma is not decreasing even as the prevalence of overweight and obesity increases (Puhl, Andreyeva, and Brownell 2008).
However, now that more than one half of US adolescents are overweight or obese (Ogden et al. 2006), young people may have more social support available to help them cope with weight stigma. This could dampen or eliminate relationships between weight and depressive symptoms in recent youth cohorts, which could explain why most recent studies estimating associations between adolescents’ weight and depressive symptoms find few links, especially among community and prospective (versus clinical) samples (see Wardle and Cooke 2005 for a review).
Recent research suggests that weight predicts depressive symptoms only among certain adolescent subgroups. Age and sex have been used to define these subgroups. For example, obesity is associated with depressive symptoms among younger, but not older adolescents, regardless of whether weight is operationalized using self-reported (Needham and Crosnoe 2005) or interviewer assessed (Swallen et al. 2005) measures.
Studies have also examined sex differences in the relationship between weight and depressive symptoms. Evidence is mixed. Chronic obesity predicts depressive symptoms among rural White boys but not girls (Mustillo et al. 2003), while self-reported BMI is associated with depressive symptoms among a national sample of female but not male adolescents (when models do not account for dieting) (Needham and Crosnoe 2005). A third study contradicts both studies’ findings. Swallen and colleagues (2005) find no associations between weight and depressive symptoms regardless of respondents’ sex among a nationally representative sample of adolescents. The discrepant results of these three studies may reflect differences in samples, the operationalization of weight, and the assessment of weight (e.g., self-report versus measured).
The inconclusive evidence about sex differences in the association between weight and depressive symptoms leads us to estimate separate models predicting this relationship for girls and boys. We expect to find few relationships between girls’ weight and depressive symptoms because there is very limited evidence that this link exists (Wardle and Cooke 2005). In addition, body image scholars suggest that girls are dissatisfied with their weight regardless of actual weight (Kostanski, Fisher, and Gullone 2004). If all adolescent girls are displeased with their weight (a phenomenon known as normative discontent), then overweight and underweight girls may be no more likely than normal weight girls to report depressive symptoms.
We expect to find that boys’ weight and depressive symptoms are related, with boys at the bottom rather than at the top of the weight continuum having the greatest risk of depressive symptoms. To date, underweight boys have been largely ignored by research due to their low numbers in most samples; greater public health, policy and research attention on overweight and obesity; and a greater concern about the consequences of weight for girls.
Underweight may be stigmatizing for boys because boys and men value a large, muscular frame (see Cohane 2001 for a review). A small body of research supports the notion that underweight boys confront weight stigma. More than 20 years ago, Harmatz and colleagues (1985) found that underweight college men suffered from body image and social adjustment issues due to their failure to live up to masculine ideals of weight. Similar findings emerge in more recent studies of Australian and US boys (Falkner et al. 2001; Kostanski, Fisher, and Gullone 2004). Underweight is also negatively associated with self-esteem among British boys (Pierce and Wardle 1993) and both self-esteem and anxiety among male Japanese college students (Kajita et al. 2002). No study has examined underweight boys’ risk of depressive symptoms. This is a primary contribution of our study. Additionally, because we analyze nationally representative data, our findings are relevant to US population health issues and solutions.
This study also asks whether relationships between adolescent weight and depressive symptoms vary by race/ethnicity. A recent literature review laments the lack of research on this topic (Wardle and Cooke 2005) and this analysis is overdue given differences in adolescent weight by sex and race/ethnicity (Ogden et al. 2006), and disparities in depressive symptoms by sex (Wade, Cairney, and Pevalin 2002) and race/ethnicity (Bratter and Eschbach 2005; Brown, Meadows, and Elder 2007). Only one study exists on this topic. A British study using data from a South London sample of secondary students examines links between race/ethnicity, weight and depressive symptoms (Wardle et al. 2006). Among this sample of White, Black, Asian, mixed race and other race respondents, no race/ethnic differences in associations between weight and depressive symptoms emerged.
Our study builds on this research in important ways. First, it examines relationships between race/ethnicity, weight, and depressive symptoms in the US. Ethnic diversity in the US and Great Britain is quite different. This study also analyzes nationally representative data (rather than data from a single urban sample) that includes Hispanics, an ethnic group largely absent in Great Britain, which is rapidly growing in the US (Bratton 2006) especially in the Southwest and Southeast (Bullock and Hood 2006). Finally, this is the first study to consider how weight and depressive symptoms are differentially related across subgroups defined by both sex and race/ethnicity.
In summary, this study has two primary goals. It examines whether associations between weight and depressive symptoms are consequential for adolescents who are underweight and overweight. It also investigates whether associations between weight and depressive symptoms are dependent on an adolescent’s sex and race/ethnicity. By using data from a nationally representative sample, the study identifies which US adolescent subgroups defined by their weight, sex and race/ethnicity are at greatest risk of depressive symptoms.
Methods
Data and Sample
Add Health is a school-based, longitudinal, nationally representative survey of 20,745 adolescents in grades 7 through 12 from 134 public, private, and parochial schools (Bearman, Jones, and Udry 1997). Respondents were selected from a stratified random sample of students in schools. Three waves of in-home survey data were collected in 1995, 1996 and 2000-2001 and provide researchers with a wealth of information about adolescents’ health, well-being and backgrounds.
We use data from the first two survey waves because of our interest in relationships between weight and depressive symptoms during adolescence; Wave III contains data about respondents once most have reached early adulthood. We construct primary variables of interest from Wave II data, but control variables are constructed from Wave I data due to data availability issues.1 The Wave II sample includes 14,738 adolescents, 71% of the original Wave I sample (roughly 45% of attrition is due to the planned non-follow-up of Wave I twelfth graders). We restrict our sample to Add Health participants in Waves I and II who were 20 years old or younger at the time of the Wave II interview and had a valid sampling weight. We also exclude 712 pregnant female respondents from our sample due to concerns about calculating a measure of weight that does not accurately capture body fatness. Restrictions lead to a final analytic sample of 12,921 respondents (6,611 boys and 6,310 girls).2
Missing data on all analytic variables are replaced using multiple imputation.3 This procedure entails replacing missing values with predictions based on information observed in the sample (Rubin 1987). Prediction models are based on the rich set of social and economic variables obtained during Wave I and II Add Health data collection efforts. Data are imputed using a multiple imputation by chained equations (MICE) program called “ICE” created for Stata 9.0 (Royston 2005). ICE allows researchers to apply appropriate estimation equations for linear and non-linear variables with missing data. For example, logistic and ordinal logistic regression can be selected for imputation models for dichotomous and ordinal variables, respectively. In addition, ICE performs well when interactions are required to produce the best fitting predictive model (Acock 2005; Royston 2005). We follow standard protocols for accounting for the uncertainty in the imputation predictions by averaging results obtained across five multiple imputation samples and adjusting the standard errors (Acock 2005; Royston 2005). When we restrict analysis to cases with no missing data, results are not significantly different either substantively or statistically from results presented here.
Measures
Depressive Symptoms
Wave II of Add Health includes a modified version of Radloff’s (1977) original Center for Epidemiologic Studies Depression Scale (CES-D). It includes 19 items that ask respondents how often they: felt depressed, sad, lonely, fearful, disliked, that they could not shake blues or that others are unfriendly to them; felt that life was a failure or that life was not worth living; did not feel hopeful, happy, or as good as others; did not enjoy life; had a poor appetite; were too tired to do things; talked less than usual; are bothered by things; and had trouble focusing or trouble starting new things. Responses to all items range from 0 (never or rarely) to 3 (most or all of the time). Responses are summed so that higher scores indicate more depressive symptoms (in our sample α = .88)
In this study, CES-D scores are dichotomized to reflect scoring at least one standard deviation above the sample mean (1 = yes).4 This represents a score of 19 or higher on the overall CES-D scale. Our operationalization reflects our substantive goal of identifying especially troubled adolescents. It also accounts for the highly skewed distribution of the CES-D scale. Prior studies using Add Health, including an analysis of adolescent weight and depressive symptoms, also construct a dichotomous measure from CES-D scale data using the same approach (Langenkamp and Frisco 2008; Swallen et al. 2005).
Adolescent Weight
Waves I and II include height and weight data, but Wave I only includes self-reported measures. Wave II also includes indicators of height and weight that were measured by the interviewer. Self-reported weight is more subjective than measured weight, is confounded with weight perceptions (Brener, Eaton, Lowry, and McManus 2004), and is prone to misreports by respondents dissatisfied with their weight (Elgar, Roberts, Tudor-Smith, and Moore 2005). Girls are also likely to underreport their weight (Ge et al. 2001). Using self-reported data to construct BMI scores introduces unnecessary error into a study and may lead to less precise estimates of gender differences in predicted effects of weight.
We computed BMI scores from Add Health interviewer-measured Wave II height and weight data. We then use the Centers for Disease Control and Prevention (CDC) (2000) guidelines for constructing age-and sex-specific BMI scores for children and teens to classify BMI scores into categories for underweight (BMI < 5th percentile), normal weight (BMI ≥ 5th and < 85th percentile), overweight (BMI ≥ 85th and < 95th percentile), and obese (BMI ≥ 95th percentile).5 For brevity, we refer to these weight categories as a group as “weight.”
Race/Ethnicity
Respondents are stratified into five race/ethnic groups using the Add Health guidelines for constructing mutually exclusive groups. Dummy variables then indicate whether respondents are White (reference), Black, Hispanic, Asian American, or Native American. Only 66 male and 38 female respondents are classified as Native American. We include these cases in our analyses and include interaction terms that estimate different effects of weight for Native American boys and girls in statistical models so that our racial/ethnic reference group includes only White respondents. We do not show main effects or interaction terms for Native Americans because estimates draw from so few cases, making them unreliable. Analyses excluding these respondents produce findings that are similar to results shown here (available upon request).
Control Variables
Multivariate models include Wave I sociodemographic and family-level variables that may confound estimates of adolescent weight and depressive symptoms. They include nativity (1 = US-born), age, family structure (reference = two parent household, other categories = living in a single parent, stepparent or other type of household), and parents’ obesity status (1 = at least 1 parent is obese). Models also control for continuous variables representing the highest education level obtained by an adolescent’s parents and six income percentile categories based on parents’ reports of 1994-95 yearly family income in thousands of US dollars. Parent’s highest education level ranges from 1 (no schooling) to 8 (post-college education). Its mean value (5.2) indicates postsecondary attendance by at least one parent. Family Income percentile categories range from 1 to 6. Its mean value (2.4) represents a family income in the 50th percentile of the distribution.
Our final two control variables indicate whether respondents report poor/fair self-assessed health (1= yes) and whether they are physically active on a regular basis (1 = yes, which is based on adolescent’s responses to three questions asking (1) whether they participate in school athletics, (2) the number of days they exercise, and (3) if they play an active sport. If adolescents responded “yes” to the first question or “5 or more times per week’ to the latter two questions, then the physical activity variable = 1). The latter two control variables help guard against the possibility that weight is confounded with muscle mass or poor health for some respondents. There are limitations with our physical activity measure, but it is the best measure we can construct with the Add Health data. Table 1 presents weighted descriptive statistics for all variables by gender.
Table 1.
Weighted Descriptive Statistics by Gender (Source: The National Longitudinal Study of Adolescent Health)a
| Boys | Girls | |||
|---|---|---|---|---|
| Mean or Proportion |
SD | Mean or Proportion |
SD | |
| Depressive Symptoms (1 = yes) | .111a | .179a | ||
| Weight Categories (Ref. = Normal Weight) | .658a | .701a | ||
| Underweight | .042a | .030a | ||
| Overweight | .152 | .150 | ||
| Obese | .148a | .119a | ||
| Race/Ethnicity (Ref. = White) | .673 | .690 | ||
| Black | .152 | .147 | ||
| Hispanic | .125 | .120 | ||
| Asian/Pacific Islander | .040 | .037 | ||
| Native American | .010a | .006a | ||
| Sociodemographic Control Variables | ||||
| Younger Adolescent (1 = Age 12-14) | .201 | .248 | ||
| Income percentile group | 2.125 | .066 | 2.165 | .064 |
| Parent’s Highest Education Level | 5.285 | .073 | 5.297 | .072 |
| Family Structure (Ref. = lives w/both parents) | .555 | .572 | ||
| Lives with Parent and Stepparent | .167 | .156 | ||
| Lives with Single Parent | .232 | .236 | ||
| Other | .046a | .036a | ||
| Nativity (1 = US Born) | .941 | .933 | ||
| Other Control Variables | ||||
| At Least 1 Parent is Obese (1 = yes) | .230 | .228 | ||
| Physically Active at Least 5 Days/Week (1 = yes) | .722 | .665 | ||
| Fair or Poor Self-Assessed Health | .059 | .068 | ||
|
| ||||
| N | 6,611 | 6,310 | ||
Indicates a statistically significant difference between estimates for boys and girls
Analytic Strategy
We estimate a series of models that are weighted and corrected for design effects using the Stata 9.0 “svy” procedure to estimate associations between weight and depressive symptoms. All analyses are stratified by gender so we use the Stata 9.0 “subpop” option to correctly calculate estimates of standard errors (Chantala 2001). Model 1 only includes weight and race/ethnicity. Model 2 adds control variables that may confound associations between weight, race/ethnicity and depressive symptoms. Model 3 then adds interaction terms that estimate how associations between weight and depressive symptoms vary by race/ethnicity.
Results
Table 2 shows results from models estimating associations between weight, race/ethnicity and depressive symptoms. The left panel presents results for adolescent boys. The right panel presents results for adolescent girls. The first column of results (Model 1a) for boys indicates that overweight and obesity are not associated with depressive symptoms among boys, but underweight is. Underweight boys’ odds of reporting depressive symptoms are almost two and a half times higher than their normal weight counterparts (Odds Ratio (OR) = exp(.881) = 2.413; Confidence Interval (CI) = 1.616, 3.606). Among girls, the first column of results (Model 1b) suggests that weight is not related to depressive symptoms. Ancillary models (available upon request) that exclude race/ethnicity from Models 1a and 1b show substantively similar associations between weight and depressive symptoms for adolescent boys and girls.
Table 2.
Logistic Regression Coefficients and Standard Errors (in parentheses) from Models Estimating Associations between Adolescent Weight and Depressive Symptoms, by Gender (Source: The National Longitudinal Study of Adolescent Health) ab
| Boys | Girls | |||||
|---|---|---|---|---|---|---|
| Model 1a | Model 2ab | Model 3ab | Model 1b | Model 2bb | Model 3bb | |
| Weight (Reference = Normal) | ||||||
| Underweight | .881 ***a (.202) |
.843 ***a (.222) |
1.016 ***a (.259) |
−.176 a (.245) |
−.202 a (.236) |
−.192 a (.339) |
| Overweight | −.083 (.131) |
−.034 (.137) |
.104 (.208) |
−.068 (.148) |
−.102 (.146) |
−.041 (.196) |
| Obese | .200 (.159) |
.053 (.172) |
.097 (.238) |
.099 (.136) |
−.086 (.150) |
−.057 (.208) |
| Race/Ethnicity (Reference = White) | ||||||
| Black | .568 *** (.131) |
.290 * (.150) |
.356 * (.180) |
.375 *** (.112) |
.043 (.113) |
.154 (.142) |
| Hispanic | .705 *** (.149) |
.495 ** (.171) |
.690 *** (.204) |
.598 *** (.146) |
.352 * (.164) |
.278 (.184) |
| Asian/Pacific Islander | .414 (.256) |
.567 * (.244) |
.413 (.282) |
.541 ** (.193) |
.397 (.217) |
.461 (.256) |
| Interaction Terms: Weight × Race/Ethnicity | ||||||
| Underweight × Black |
−1.210 * (.584) |
−.252 (.955) |
||||
| Hispanic | −.215 (.553) |
390 (.645) |
||||
| Asian/Pacific Islander | .341 (1.088) |
−.566 (.778) |
||||
| Overweight × Black |
−.071 (.331) |
−.279 (.329) |
||||
| Hispanic | −.762 * (.362) |
.149 (.365) |
||||
| Asian/Pacific Islander | .193 (.585) |
−.554 (.914) |
||||
| Obese × Black |
−.073 (.410) |
−.320 (.281) |
||||
| Hispanic | −.487 (.428) |
.191 (.456) |
||||
| Asian/Pacific Islander | .568 (.447) |
.415 (.602) |
||||
| Constant | −2.376 ***a (.092) |
−1.884 *** (.324) |
−1.921 *** (.340) |
−1.691 ***a (.072) |
−1.221 *** (.264) |
−1.234 (.273) |
|
| ||||||
| N | 6,611 | 6,310 | ||||
p<=.001
p<=.010
p<=.050
Indicates a statistically significant difference between estimates for boys and girls
Models also include control variables representing family income percentile, parents’ highest education level, family structure, nativity, parents’ obesity status, physical activity at least 5 days/week, poor/fair self-assessed health, Native American race/ethnicity, and (model 3 only) interaction terms between Native American race/ethnicity and weight
Models 1a and 1b also indicate that when weight is controlled, male and female racial/ethnic minorities are more likely than Whites to report depressive symptoms. Compared to White peers, the odds of reporting depressive symptoms are 77% (OR = exp(.568) = 1.765; CI = 1.363, 2.285) higher and twice as high (OR = exp(.705) = 2.023; CI = 1.505, 2.720) for Black and Hispanic boys, respectively. Among female respondents, Black, Hispanic and Asian/Pacific Islanders all have higher odds of reporting depressive symptoms than Whites. Ancillary models (available upon request) that exclude weight from Models 1a and 1b show substantively similar associations between race/ethnicity and depressive symptoms for adolescent boys and girls.
Model 2a presents estimated associations between weight, race/ethnicity and depressive symptoms when control variables are included in statistical models. Compared to normal weight boys, underweight boys’ estimated odds of reporting depressive symptoms are still higher. Black and Hispanic boys are also still significantly more likely to report depressive symptoms than White boys, but effect sizes are reduced substantially. Conversely, Asian/Pacific Islanders’ odds of depressive symptoms increase and are now significantly higher than White boys.
When control variables are included in models estimating girls’ odds of depressive symptoms (Model 2b), weight is still not significantly associated with our outcome and associations between girls’ race/ethnicity and depressive symptoms are substantially reduced. Black girls are no more likely than White girls to report depressive symptoms; the coefficient is almost reduced to zero. Asian/Pacific Islanders are also not significantly more likely than Whites to report depressive symptoms. Only Hispanic girls have higher odds than Whites of reporting depressive symptoms (OR = exp(.352) = 1.422; CI = 1.027, 1.969).
The final columns of results (Models 3a and 3b) in Table 2 for boys and girls indicate that associations between weight and depressive symptoms vary by race/ethnicity for boys only. Among boys, being either underweight or Black is associated with higher odds of reporting depressive symptoms (see Model 2a), but the interaction of the two provides a protective effect when the reference group is normal weight White boys (in Model 3a). This finding is better demonstrated when calculated predicted probabilities of reporting depressive symptoms for underweight, Black boys (.09) and normal weight, White boys (.08) are compared.6 Underweight White boys also have higher odds of reporting depressive symptoms than normal weight White boys (in Model 3a, the coefficient for underweight represents the estimated effect of being White and underweight). Results additionally suggest that among boys, being Hispanic and overweight may provide a protective effect. Hispanics’ odds of reporting depressive symptoms are higher than Whites (see Model 2a), but overweight Hispanic boys’ odds of reporting depressive symptoms are actually similar to those of normal weight White boys. These findings are again better depicted when the predicted probability of reporting depressive symptoms among overweight, Hispanic boys (.10) and normal weight, White boys (.08) are compared.
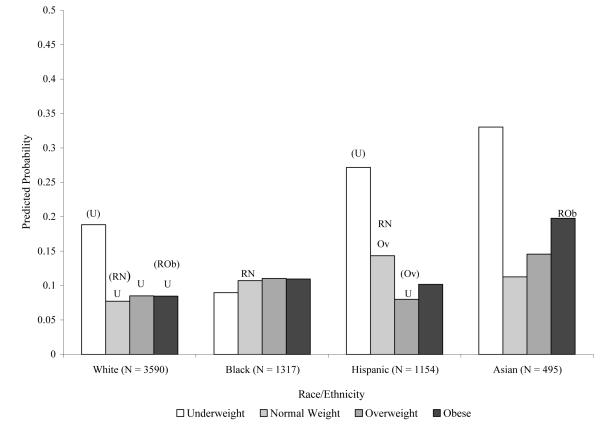
To provide more insight into the way that race/ethnicity and weight intersect and are associated with depressive symptoms for boys7, we present Figure 1. It depicts all significant within- and between-race differences in relationships between boys’ weight and depressive symptoms using predicted probabilities.8
Figure 1.
Within- and Between Group Racial/Ethnic Differences in Adolescent Boys’ Predicted Probability of Reporting Depressive Symptoms by Weight when Confounders are Held Constant (Source: National Longitudinal Study of Adolescent Health)
Notes
a U denotes a significant within race/ethnic group difference between underweight boys and boys in other weight categories: Ref = (U)
b Ov denotes a significant within race/ethnic group difference between overweight boys and boys in other weight categories: Ref = (Ov)
c RN denotes a significant between-race group difference between normal weight boys in different race/ethnic groups: Ref = (RN)
d ROb denotes a significant between-race group difference between obese boys in different race/ethnic groups: Ref = (ROb)
We first discuss differences in the estimated probability of reporting depressive symptoms by weight among boys of the same race/ethnicity. Among Whites, there is statistically no difference in the predicted probability of reporting depressive symptoms across normal weight, overweight and obese boys. However, underweight White boys’ predicted probability of reporting depressive symptoms is roughly twice as high as boys in the other three weight categories. Among Black boys, there are no significant differences in the predicted probability of reporting depressive symptoms by weight. Their estimated probability of reporting depressive symptoms is about .10 regardless of weight. Among Hispanics boys, there are significant differences in the predicted probability of reporting depressive symptoms by weight. Underweight Hispanic boys have a significantly higher probability of reporting depressive symptoms than their overweight counterparts, who have the lowest estimated probability of reporting depressive symptoms. In fact, overweight Hispanic boys are less likely to report depressive symptoms than normal weight Hispanic boys. Among male Asian/Pacific Islanders, the predicted probability of reporting depressive symptoms varies by weight, but differences are not statistically significant. This finding may stem from the small number of underweight (N = 33) and obese (N = 16) male Asian/Pacific Islanders.
Few between-race differences in the probability of reporting depressive symptoms by weight emerge. Among normal weight boys, both Black and Hispanic boys have higher predicted probabilities of depressive symptoms than White boys. Among obese boys, the predicted probability of reporting depressive symptoms is more than twice as high for Asian/Pacific Islanders versus Whites.
Discussion
The goal of this study was to examine whether weight is associated with depressive symptoms for some but not all adolescent subgroups defined by their weight, sex and race/ethnicity. Unlike prior research, our analysis acknowledges that weighing more or less than what is considered normal for one’s height may be associated with depressive symptoms. It is also the first study to examine whether the relationship between weight and depressive symptoms varies by race/ethnicity among subgroups of US adolescent girls and boys.
Study results make several contributions to the literature. Generally, they show the importance of considering subpopulations when studying population health issues and interventions that target them. In this study, if we only estimated relationships between weight and depressive symptoms for all adolescents, our analyses would not reveal the risk of depressive symptoms for underweight boys or variations in the relationship between boys’ weight and depressive symptoms by race/ethnicity.
The consistent association between underweight and depressive symptoms for boys supports the premise that underweight is a stigmatizing physical and social status for them. The finding is also consistent with literature suggesting the importance of a large, muscular frame for adolescent boys (Falkner et al. 2001; Jones 2004) and that underweight boys face a range of negative social and psychological outcomes (Harmatz, Gronendyke, and Thomas 1985; Jones and Crawford 2006).
Unlike the small number of prior studies elucidating consequences of underweight for boys, this is the first study to focus on depressive symptoms and to analyze nationally representative data. Findings are thus generalizable to the US population of adolescent boys. The proportion of underweight boys in the US is small, but our findings suggest that they are at an exceptionally high risk of depressive symptoms. Results also serve as a reminder that obesity is not the only weight classification with negative consequences for adolescents.
As such, parents and clinicians should be encouraged to talk to underweight boys about their social and psychological experiences. These adults should also be prepared to offer underweight boys strategies to cope with their stigmatized status. This recommendation is especially relevant to parents and clinicians who interact with underweight White and Hispanic boys. Both of these groups have at least double the risk of depressive symptoms as other boys in their racial/ethnic group.
Given the projected growth of the US Hispanic population (Bratton 2006) and lack of knowledge about Hispanic adolescents’ risk factors for psychological distress (Flores et al. 2002), our ability to analyze associations between Hispanic adolescents’ weight and depressive symptoms is an important study contribution. Relative to normal weight Hispanic boys, underweight Hispanic boys are at risk of depressive symptoms, while overweight Hispanic boys appear to be protected. The latter group’s probability of reporting depressive symptoms is similar to that of normal weight White boys, who have the lowest risk of depressive symptoms.
Future research is needed to explain these findings, but we speculate about their meaning here. They may reflect the fact that Hispanic boys are heavier than every other US racial/ethnic and gender adolescent subpopulation (Flores et al. 2002; Ogden et al. 2006). In a peer context where Hispanic boys are exposed to other, relatively heavy adolescents, underweight Hispanic boys may face incredible weight stigma and overweight boys may be more socially accepted.
Like Hispanic boys, the prevalence of overweight and obesity is also high among Black adolescent boys, but unlike their Hispanic peers, we found no significant associations between weight and depressive symptoms among Black boys. These findings are consistent with evidence that the range of weights Blacks see as acceptable is quite wide (Cash and Henry 1995).
When we compare how weight and depressive symptoms vary across racial/ethnic groups, differences in the estimated effects of underweight, overweight and obesity are largely absent.9 Instead, the estimated effects of being in the normal weight range vary by race/ethnicity. Normal weight Blacks and Hispanics (versus Whites) are more likely to report depressive symptoms. These findings may shed light on results from previous studies indicating that racial and ethnic minorities are more likely to report depressive symptoms (e.g., Brown et al. 2007). This greater risk, however, may not apply to all adolescents. Instead, prior research may reflect the experiences of normal weight adolescents. The fact that we find that overweight Hispanic, underweight Black, and normal weight White boys have a similar risk of depressive symptoms suggests that accounting for weight is important when estimating relationships between race/ethnicity and depressive symptoms. Moreover, clinicians should recognize that normal weight minority boys may be on track for good physical health, but at risk of poor mental health.
Our study’s final contribution is to add further evidence that weight and depressive symptoms are not linked among female adolescents. This result is consistent with girls’ normative discontent about their weight (Kostanski, Fisher, and Gullone 2004) and evidence that girls’ weight perceptions (rather than actual weight) influences depressive symptoms (Pesa, Syre, and Jones 2000). Girls’ weight could, however, affect other mental health outcomes.
Findings for boys versus girls are a reminder to those interested in population health issues that hypotheses about health and well-being are not always as straightforward as one would expect. Because of girls’ weight concerns and their greater risk of depression (versus boys), it is often assumed that overweight and obese female adolescents are especially at risk of depressive symptoms, but this relationship is not borne out in the bulk of the literature on this topic among nationally representative samples. Instead, weight is a risk factor for boys’ depressive symptoms, but as noted previously, underweight, not overweight places them at risk.
Our findings are robust, but this study is not without limitations. Our analysis is cross-sectional because we use Wave II Add Health data to operationalize weight categories and depressive symptoms. Models only speak to relationships between adolescents’ current weight and depressive symptoms and cannot be used to fully discern causality.10 Theory about weight stigma offers reason to believe that adolescent weight predicts depressive symptoms, but we acknowledge research predicting the reverse causal direction (Goodman and Whitaker 2002). A second limitation is our inability to disaggregate Hispanics by ethnicity to better understand how weight and psychological distress are linked among Hispanic subgroups. Doing so results in cell sizes too small for multivariate analyses that include interaction terms between weight and race/ethnicity. On a related note, the small sample of Native Americans limited our ability to make meaningful comparisons between them and adolescent boys and girls in other racial/ethnic groups. Attrition may also limit the generalizability of our findings, but supplementary analyses suggest few differences between our sample and the Wave I Add Health sample. Weighting and correcting statistical models for design effects also helps to reduce attrition bias. Finally, as is the case with most studies that involve secondary data analysis, data availability limits our ability to operationalize key variables of interest. For example, weight categories could be more precise if other indicators of body fatness such as results from DXA (Dual energy X-ray absorptiometry) scans or waist-to-hip ratios were available in Add Health. Our variable measuring parental obesity is also crudely measured (it relies on a parent’s report of whether (s)he is obese, not a BMI score) and we previously noted the limitations of our physical activity measure.
Despite limitations, this study makes important contributions to literature on adolescent weight and depressive symptoms. There is currently well-founded attention given to the problem of adolescent obesity, but this study’s findings are a reminder that weighing less than what is considered to be normal can also be problematic, especially for adolescent boys. In addition, this study highlights the need to consider how adolescents’ physical and psychosocial well-being are related among subpopulations, not just in the adolescent population at large. More detailed comparisons of adolescents in different social positions offer new insight into how to best address population health issues during adolescence.
Endnotes
Some control variable can only be constructed using Wave I data (e.g., family income, parent’s obesity status). For consistency, we thus construct all control variables using Wave I data. When Waves I and II data were available to construct a control variable, we tested whether replacing the Wave I variable with the Wave II variable in statistical models significantly changed primary results of interest or regression coefficients for that control variable. It did not.
Supplementary analyses suggest that attrition from Waves I to II does not significantly influence the generalizability of our findings. Our sample’s characteristics are not significantly different than the original sample with respect to most study variables. There is one exception: physical activity. Those not followed up were less likely to report physical activity.
Few variables required substantial imputation. Weight was missing for .96% of the sample (n=124). Depressive symptoms were imputed for .33% of the sample (n=43). Race/Ethnicity was imputed for .33% of the sample (n=43). No data were missing on age, family structure, gender, or physical activity. The rage of missing data on other control variables is .02% to 8.20%. Parental obesity (8.2%, n=1059) and family income (5.83%, n = 754) have the most missing data.
There is controversy over how to operationalize depressive symptoms using the CES-D scale. Some scholars argue for our approach (e.g., Wheaton 2001). Others argue for use of a continuous or a log-transformed scale variable (e.g., Mirowsky and Ross 2002; Mirowsky 1999). Both approaches tap important aspects of mental health (Kessler 2002; Schwartz 2002; Wheaton 2001), but dichotomous measures capture persons who are likely distressed to the point of impairment (Schwartz 2002; Wheaton 2001). Most Add Health studies that dichotomize the scale use one of two cut-points: ours or a cut-point of 22 for boys and 24 for girls (e.g., Goodman 1999). One other study uses a cut-point of 16 (Needham and Crosnoe 2005). To test findings for sensitivity to different depressive symptoms operationalizations, we estimated alternative models that predicted depressive symptoms using all 4 alternative operationalizations observed in prior studies. Results from these models are substantively and statistically similar to results presented here but findings presented here are more conservative than findings obtained when we use the CES-D scale as a continuous variable (regardless of whether it is transformed) or a dichotomous variable with a cut-point of 16 for determining depressive symptoms. Results using 22 and 24 point cutoffs are largely the same as findings presented here.
The CDC recommends using the terms “at risk of overweight” and “overweight” to describe adolescents with BMI scores in the 85th through 94th percentiles and at or above the 95th percentiles. The Institute of Medicine (IOM) and pediatricians recommend use of “overweight” and “obese,” respectively, to describe these adolescents (see Krebs et al 2007). The IOM and Krebs et al. (2007) argue that “overweight” and “obese” better reflect the problematic nature of BMI scores at or above the 85th and 95th percentiles. We agree with their assessment and use this terminology here.
Predicted probabilities are based on findings in Model 3a in Table 2 when control variables are held at mean or modal values.
No comparable findings for girls are shown because weight and depressive symptoms are not related regardless of girls’ race/ethnicity (results available upon request).
Predicted probabilities are based on findings in Model 3a in Table 2 when control variables are held constant at mean or modal values. To estimate all relevant comparisons, we switched out reference groups for interaction terms in supplementary analyses (available upon request).
The one exception is that obese male Asian/Pacific Islanders have a higher probability of depressive symptoms than obese White boys. We do not interpret this finding because few obese Asian/Pacific Islanders also report depressive symptoms (N = 3) and this finding could be a data artifact. We do not interpret the lack of associations between weight and depressive symptoms among male Asian/Pacific Islanders for similar reasons. These findings may reflect small cell sizes.
Supplementary analyses checked whether controlling for Wave I depressive symptoms substantially changed associations between weight and Wave II symptoms. It did not. We do not include the Wave I indicator of depressive symptoms in final models because doing so produces a lagged dependent variable model and results would be interpreted in terms of change over time. Weight categories are Time 2 measures, so this approach would violate causal order assumptions by estimating the effect of Time 2 weight on changes in depressive symptoms between Time 1 and 2.
Dr. Frisco will share all data and coding information with readers who wish to replicate the study. Note, though, that this study uses data from The National Longitudinal Study of Adolescent Health, a research program designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, and funded by grant P01-HD31921 from the National Institute of Child Health and Human Development, with cooperative funding from 17 other agencies. Anyone wishing to use the Add Health data must obtain proper approval from Add Health administrators. The authors acknowledge support from the Penn State University Population Research Institute, a grant from the National Institute of Child Health and Human Development (R01 HD40428-02, PI: Gary Sandefur), and the Career Development Program in Women’s Health Research at Penn State (K 12HD055882, principal investigator Carol Weisman), a program sponsored by NICHD. We would like to thank Kristin Burnett, Ashleigh May, Tamar Mendelson, Kristi Williams, Penn State Population Research Institute browbag attendees, and Rutgers University Institute for Health, Health Care Policy and Aging Research seminar series attendees for their helpful comments on this manuscript.
References
- Acock Alan C. Working with Missing Values. Journal of Marriage and Family. 2005;67:1012–1028. [Google Scholar]
- Allon Natalie. The Stigma of Overweight in Everyday Life. In: Wolman B, editor. Psychological Aspects of Obesity: A Handbook. Van Nostrand; New York: 1982. pp. 130–174. [Google Scholar]
- Bearman Peter S, Jones Jo, Udry J. Richard. The National Longitudinal Study of Adolescent Health: Research Design. Carolina Population Center; Chapel Hill, NC: 1997. [Google Scholar]
- Bratter Jenifer, Eschbach Karl. Race/Ethnic Differences in Nonspecific Psychological Distress: Evidence from the National Health Interview Survey. Social Science Quarterly. 2005;86:620–645. [Google Scholar]
- Bratton Kathleen A. The Behavior and Success of Latino Legislators: Evidence from the States. Social Science Quarterly. 2006;87:1136–1157. [Google Scholar]
- Brener Nancy D., Eaton Danice K., Lowry Richard, McManus Tim. The association between weight perception and BMI among high school students. Obesity Research. 2004;12:1866–1874. doi: 10.1038/oby.2004.232. [DOI] [PubMed] [Google Scholar]
- Britz B, Siegfried W, Ziegler A, Lamertz C, Herpertz-Dahlmann BM, Remschmidt H, Wittchen HU, Hebebrand J. Rates of Psychiatric Disorders in a Clinical Study Group of Adolescents with Extreme Obesity and in Obese Adolescents Ascertained via a Population-Based Study. International Journal of Obesity and Related Metabolic Disorders. 2000;24:1707–1714. doi: 10.1038/sj.ijo.0801449. [DOI] [PubMed] [Google Scholar]
- Brown J. Scott, Meadows Sarah O, Elder Glen H. Race-Ethnic Inequality and Psychological Distress: Depressive Symptoms from Adolescence to Young Adulthood. Developmental Psychology. 2007;43:1295–1311. doi: 10.1037/0012-1649.43.6.1295. [DOI] [PubMed] [Google Scholar]
- Bullock Charles S., III, Hood MV., III A Mile-Wide Gap: The Evolution of Hispanic Political Emergence in the Deep South. Social Science Quarterly. 2006;87:1117–1135. [Google Scholar]
- Cash Thomas F., Henry Patricia E. Women’s Body Images: The Results of a National Survey in the U.S.A. Sex Roles. 1995;33:19–28. [Google Scholar]
- Center for Disease Control and Prevention . Healthy Weight, Physical Activity, and Nutrition: Focus Group Research with African American, Mexican American, and White Youth: Executive Summary. Centers for Disease Control; Atlanta, GA: 2000. [Google Scholar]
- Chantala Kim. Using STATA to Analyze Data from a Sample Survey. Carolina Population Center, University of North Carolina, Chapel Hill; Chapel Hill, NC: 2001. [Google Scholar]
- Cohane Geoffrey H., Pope Harrison G., Jr. Body Image in Boys: A Review of the Literature. International Journal of Eating Disorders. 2001;29:373–379. doi: 10.1002/eat.1033. [DOI] [PubMed] [Google Scholar]
- Crandall Christian, Schiffhauer Kristin. Anti-fat Prejudice: Beliefs, Values, and American Culture. Obesity Research. 1998;6:458–460. doi: 10.1002/j.1550-8528.1998.tb00378.x. [DOI] [PubMed] [Google Scholar]
- Daniels Stephen R. The Consequences of Childhood Overweight and Obesity. The Future of Children. 2006;16:47–67. doi: 10.1353/foc.2006.0004. [DOI] [PubMed] [Google Scholar]
- Dejong William. The Stigma of Obesity: The Consequences of Naïve Assumptions Concerning the Causes of Physical Deviance. Journal of Health and Social Behavior. 1980;21:75–87. [PubMed] [Google Scholar]
- Elgar Frank, Roberts Chris, Tudor-Smith Chris, Moore Laurence. Validity of Self-Reported Height and Weight as Predictors of Bias in Adolescents. Journal of Adolescent Health. 2005;37:371–375. doi: 10.1016/j.jadohealth.2004.07.014. [DOI] [PubMed] [Google Scholar]
- Falkner Nicole H., Neumark-Sztainer Diane, Story Mary, Jeffery Robert W., Beuhring Trish, Resnick Michael D. Social, Educational, and Psychological Correlates of Weight Status in Adolescents. Obesity Research. 2001;9:32–42. doi: 10.1038/oby.2001.5. [DOI] [PubMed] [Google Scholar]
- Field Alison E, Camargo Carlos A., Jr., Barr Taylor C, Berkey Catherine S, Roberts Susan B, Colditz Graham A. Peer, Parent, and Media Influences on the Development of Weight Concerns and Frequent Dieting among Preadolesecent and Adolescent Girls and Boys. Pediatrics. 2001;107:54–60. doi: 10.1542/peds.107.1.54. [DOI] [PubMed] [Google Scholar]
- Flores Glenn, Fuentes-Afflick Elena, Barbot Oxiris, Carter-Pokras Olivia, Claudio Luz, Marielena Lara, McLaurin Jennie A, Pachter Lee, Gomez Francisco Ramos, Mendoza Fernando, Valdez R. Burciaga, Villarrueal Antonia M, Zambrana Ruthe E, Greenberg Robert, Weitzman Michael. The Health of Latino Children: Urgent Priorities, Unanswered Questions and a Research Agenda. Journal of the American Medical Association. 2002;288:82–92. doi: 10.1001/jama.288.1.82. [DOI] [PubMed] [Google Scholar]
- Ge Xiaojia, Elder Glen H., Jr., Regnerus Mark, Cox Christine. Pubertal Transitions, Perceptions of Being Overweight, and Adolescents’ Psychological Maladjustment: Gender and Ethnic Differences. Social Psychology Quarterly. 2001;64:363–375. [Google Scholar]
- Goodman Elizabeth. The Role of Socioeconomic Status Gradients in Explaining Differences in US Adolescents’ Health. American Journal of Public Health. 1999;89:1522–1528. doi: 10.2105/ajph.89.10.1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman Elizabeth, Whitaker Robert C. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110:497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- Harmatz Morton G., Gronendyke James, Thomas Todd. The Underweight Male: The Unrecognized Problem Group of Body Image Research. The Journal of Obesity and Weight Regulation. 1985;4:258–267. [Google Scholar]
- Horwitz Allan V. Outcomes in the Sociology of Mental Health and Illness: Where Have We Been and Where are We Going? Journal of Health and Social Behavior. 2002;43:143–151. [PubMed] [Google Scholar]
- Jones Diane Carlson. Body Image Among Adolescent Girls and Boys: A Longitudinal Study. Developmental Psychology. 2004;40:823–835. doi: 10.1037/0012-1649.40.5.823. [DOI] [PubMed] [Google Scholar]
- Jones Diane Carlson, Crawford Joy K. The peer appearance culture during adolescence: gender and body mass variations. Journal of Youth and Adolescence. 2006;35:257–269. [Google Scholar]
- Kajita Miwako, Takahashi Toshihiko, Hayashi Kimiko, Fukuharu Michitaro, Sato Juichi, Sato Yuzo. Self-Esteem and Mental Health Characteristics Especially Among Lean Students Surveyed by University Personality Inventory. Psychiatry and Clinical Neurosciences. 2002;56:123–129. doi: 10.1046/j.1440-1819.2002.00947.x. [DOI] [PubMed] [Google Scholar]
- Kessler Ronald C. The Categorical versus Dimensional Assessment Controversy in the Sociology of Mental Illness. Journal of Health and Social Behavior. 2002;43:171–188. [PubMed] [Google Scholar]
- Kostanski Marion, Fisher Adiran, Gullone Eleonora. Current Conceptualization of Body Image Dissatisfaction: Have We Got it Wrong? Journal of Child Psychology and Psychiatry. 2004;45:1317–1325. doi: 10.1111/j.1469-7610.2004.00315.x. [DOI] [PubMed] [Google Scholar]
- Krebs Nancy F, Himes John H, Jacobson Dawn, Nicklas Theresa A, Guilday Patricia, Styne Dennis. Assessment of Child and Adolescent Obesity. Pediatrics. 2007;120:S193–S228. doi: 10.1542/peds.2007-2329D. [DOI] [PubMed] [Google Scholar]
- Langenkamp Amy, Frisco Michelle L. Family Transitions and Adolescent Severe Emotional Distress: The Salience of Family Context. Social Problems. 2008;55:238–253. doi: 10.1525/sp.2008.55.2.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latner Janet, Stunkard Albert J., Wilson G.Terence. Stigmatized Students: Age, Sex, and Ethnicity Effects in the Stigmatization of Obesity. Obesity Research. 2005;13:1226–1231. doi: 10.1038/oby.2005.145. [DOI] [PubMed] [Google Scholar]
- Mirowsky John. Analyzing Associations between Mental Health and Social Circumstances. In: Aneshensel C, Phelan JC, editors. Handbook of the Sociology of Mental Health. Kluwer Academic/Plenum Publishers; New York: 1999. pp. 105–126. [Google Scholar]
- Mirowsky John, Ross Catherine E. Measurement for a Human Science. Journal of Health and Social Behavior. 2002;43:152–170. [PubMed] [Google Scholar]
- Mustillo Sarah, Worthman Carol, Erkanli Alattin, Keeler Gordon, Angold Adrian, Costello E. Jane. Obesity and Psychiatric Disorder: Developmental Trajectories. Pediatrics. 2003;111:851–859. doi: 10.1542/peds.111.4.851. [DOI] [PubMed] [Google Scholar]
- Needham Belinda L., Crosnoe Robert. Overweight Status and Depressive Symptoms During Adolescence. Journal of Adolescent Health. 2005;36:48–55. doi: 10.1016/j.jadohealth.2003.12.015. [DOI] [PubMed] [Google Scholar]
- Ogden Cynthia L, Carroll Margaret D, Curtin Lester R, McDowell Margaret A, Tabak Carolyn J, Flegal Katherine M. Prevalence of Overweight and Obesity in the United States, 1999-2004. Journal of the American Medical Association. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Pesa Jacqueline A, Syre Thomas R., Jones Elizabeth. Psychosocial Differences Associated with Body Weight Among Female Adolescents: The Importance of Body Image. Journal of Adolescent Health. 2000;26:330–337. doi: 10.1016/s1054-139x(99)00118-4. [DOI] [PubMed] [Google Scholar]
- Pierce Jeanne Walsh, Wardle Jane. Self Esteem, Parental Appraisal, and Body Size in Children. Journal of Child Psychology and Psychiatry. 1993;34:1125–1136. doi: 10.1111/j.1469-7610.1993.tb01778.x. [DOI] [PubMed] [Google Scholar]
- Puhl Rebecca M, Andreyeva Tatiana, Brownell Kelly D. Perceptions of Weight Discrimination: Prevalence and Comparison to Race and Gender Discrimination in America. International Journal of Obesity. 2008;295:1549–1557. doi: 10.1038/ijo.2008.22. [DOI] [PubMed] [Google Scholar]
- Puhl Rebecca M, Brownell Kelly D. Confronting and Coping with Weight Stigma: An Investigation of Overweight and Obese Adults. Obesity Research. 2006;14:1802–1815. doi: 10.1038/oby.2006.208. [DOI] [PubMed] [Google Scholar]
- Radloff Lenore Sawyer. The CES-D Scale: A self-report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Royston Patrick. Multiple Imputation of Missing Values: Update of Ice. Stata Journal; 2005;5:527–536. [Google Scholar]
- Rubin Donald. Multiple Imputation for Non-Response in Surveys. Wiley; New York: 1987. [Google Scholar]
- Schwartz Sharon. Outcomes for the Sociology of Mental Health. Journal of Health and Social Behavior. 2002;43:223–235. [PubMed] [Google Scholar]
- Swallen Karen, Reither Eric N., Haas Steven A., Meier Ann M. Overweight, Obesity, and Health-Related Quality of Life Among Adolescents: The National Longitudinal Study of Adolescent Health. Pediatrics. 2005;115:340–347. doi: 10.1542/peds.2004-0678. [DOI] [PubMed] [Google Scholar]
- Wade Terrance J, Cairney John, Pevalin David J. Emergence of Gender Differences in Depression During Adolescence: National Panel Results From Three Countries. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:190–198. doi: 10.1097/00004583-200202000-00013. [DOI] [PubMed] [Google Scholar]
- Wardle Jane, Williamson Sara, Johnson Fiona, Edwards C. Depression in Adolescent Obesity: Cultural Moderators of the Association Between Obesity and Depressive Symptoms. International Journal of Obesity. 2006;30:634–643. doi: 10.1038/sj.ijo.0803142. [DOI] [PubMed] [Google Scholar]
- Wardle Jane, Cooke Lucy. The impact of obesity on psychological well-being. Best Practice and Research. Clinical Endocrinology and Metabolism. 2005;19:421–40. doi: 10.1016/j.beem.2005.04.006. [DOI] [PubMed] [Google Scholar]
- Wheaton Blair. The Role of Sociology in the Study of Mental Health...and the Role of Mental Health in the Study of Sociology. Journal of Health and Social Behavior. 2001;42:221–234. [PubMed] [Google Scholar]