Abstract
Background
Acute respiratory distress syndrome is characterized by damage to the lung caused by various insults, including ventilation itself, and tidal hyperinflation can lead to ventilator induced lung injury (VILI). We investigated the effects of a low tidal volume (V T) strategy (V T ≈ 3 ml/kg/predicted body weight [PBW]) using pumpless extracorporeal lung assist in established ARDS.
Methods
Seventy-nine patients were enrolled after a ‘stabilization period’ (24 h with optimized therapy and high PEEP). They were randomly assigned to receive a low V T ventilation (≈3 ml/kg) combined with extracorporeal CO2 elimination, or to a ARDSNet strategy (≈6 ml/kg) without the extracorporeal device. The primary outcome was the 28-days and 60-days ventilator-free days (VFD). Secondary outcome parameters were respiratory mechanics, gas exchange, analgesic/sedation use, complications and hospital mortality.
Results
Ventilation with very low V T’s was easy to implement with extracorporeal CO2-removal. VFD’s within 60 days were not different between the study group (33.2 ± 20) and the control group (29.2 ± 21, p = 0.469), but in more hypoxemic patients (PaO2/FIO2 ≤150) a post hoc analysis demonstrated significant improved VFD-60 in study patients (40.9 ± 12.8) compared to control (28.2 ± 16.4, p = 0.033). The mortality rate was low (16.5 %) and did not differ between groups.
Conclusions
The use of very low V T combined with extracorporeal CO2 removal has the potential to further reduce VILI compared with a ‘normal’ lung protective management. Whether this strategy will improve survival in ARDS patients remains to be determined (Clinical trials NCT 00538928).
Electronic supplementary material
The online version of this article (doi:10.1007/s00134-012-2787-6) contains supplementary material, which is available to authorized users.
Keywords: Lung protective ventilation, Pumpless extracorporeal lung support, Carbon dioxide removal, Acute respiratory distress syndrome, Ultraprotective ventilation
Introduction
Acute respiratory distress syndrome (ARDS) is characterized by damage to the lung parenchyma, caused by either indirect or direct insults, including ventilation itself [1]. Tidal hyperinflation and cyclic alveolar recruitment/derecruitment during mechanical ventilation can lead to an entity called ventilator induced lung injury (VILI) [2, 3]. A multi-centered clinical trial demonstrated that a lung protective strategy with tidal volumes (V T’s) of 6 ml/kg predicted body weight (PBW), and plateau pressures ≤30 cmH2O decreased mortality by a relative 22 % compared to control [4]. A post hoc analysis of this study [5] found that the lower the plateau pressure (P plat), the better the patient’s chances of survival, even for P plat substantially <30 cmH2O, and these data suggested that even lower tidal volumes might further improve survival. Grasso and colleagues [6] demonstrated that many ARDS patients ventilated using the ARDSNet strategy with table-based PEEP have a stress index indicating alveolar hyperinflation.
These data would suggest the use of even lower tidal volumes, but in severe ARDS the implementation of such a strategy may be limited by a therapeutic dilemma due to the increased likelihood of more severe hypercapnia and acidosis. The impact of hypercapnia on lung injury or on systemic effects including remote organ damage (myocardial insufficiency, renal failure, and hepatic/intestinal ischemia) is somewhat controversial [7, 8], delaying or preventing the implementation of adequate lung-protective strategies [9].
In the last few years, extracorporeal, pumpless arterio-venous approaches to CO2 removal using an artificial membrane lung have been developed and tested for clinical use retrospectively in 90 patients [10] demonstrating marked carbon dioxide removal and moderate oxygenation improvement. Additionally, in a prospective cohort study Terragni and coworkers [11] used a CO2 removal device to reduce tidal volume lower than 6 ml/kg and observed an improvement of morphological markers of lung protection. However, their study was not a randomized clinical trial and there was no concurrent control group. We set out to investigate the effects of combining a very low V T (3 ml/kg PBW) with arterio-venous extracorporeal CO2-elimination (avECCO2-R) in patients suffering from established ARDS.
We hypothesized mechanical ventilation using lower tidal volumes (3 ml/kg) assisted by avECCO2-R would enhance lung protection and hence increase 28-day and 60-day ventilator-free days, compared with mechanical ventilation using conventional tidal volumes (6 ml/kg).
Methods
Patients
The study was approved by the ethics committee of the Regensburg University Hospital (reference 07/012), and the ethics committees of all involved study centers. Before enrolment, written informed consent was obtained from the legal proxy of each patient. Patients were enrolled from September 2007 through December 2010 at eight intensive care units (ICU) in Germany and two ICU’s in Austria.
Entry criteria were: (1) presence of ARDS according to the American-European Consensus Conference [12] defined by bilateral infiltrates on chest X-ray, and a PaO2/FIO2 <200 present for at least 2 h. At the time of screening patients could not have any evidence of left ventricular failure; (2) age ≥18 years; (3) history of mechanical ventilation <7 days); (4) plateau pressure >25 cmH2O at defined ventilator settings (PEEP/FIO2-table + V T = 6 ml/kg); (5) absence of severe hemodynamic instability with high demand for vasopressors (mean arterial pressure ≥70 mmHg with continuous norepinephrine infusion ≤0.4 μg/kg/min). Exclusion criteria were: decompensated heart insufficiency, acute coronary syndrome, severe chronic obstructive pulmonary disease, advanced malignancy with life expectancy <6 months, chronic dialysis treatment, lung transplant patients, proven heparin-induced thrombocytopenia (HIT), morbid obesity (body mass index >40 kg/m2), cirrhosis of the liver Child Class ≥B (Child–Pugh scores ≥7), or acute fulminant hepatic failure, severe peripheral arterial occlusive disease, absence of limb doppler pulse, and acute brain injury (Glasgow Coma Scale ≤9).
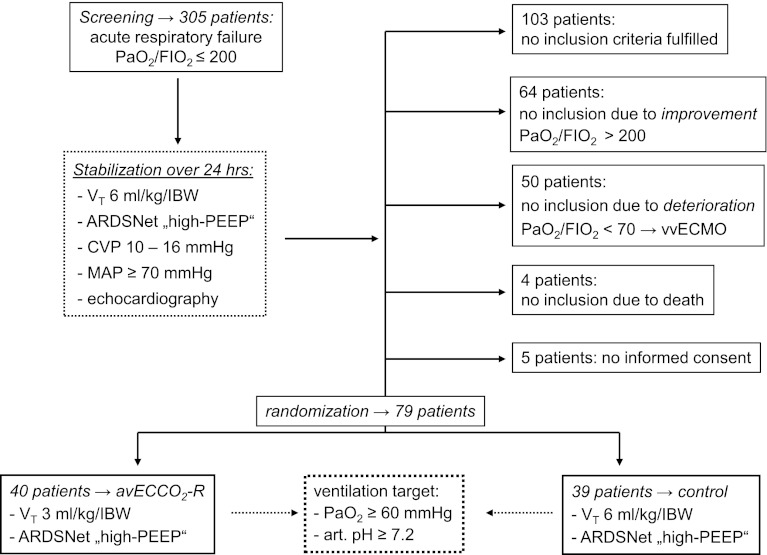
To identify patients presenting with established ARDS and to help further rule out patients with acute cardiogenic pulmonary edema, the screening was followed by a stabilization period for 24 h, characterized by lung protective mechanical ventilation with high PEEP (≥12 cmH2O), the use of supportive measures, and hemodynamic evaluation (echocardiography). Patients who had ARDS criteria (PaO2/FIO2 <200) after 24 h despite optimal supportive treatment were identified as those with established ARDS [13], and were randomized through phone hot line by a random number table generated by the involved statistician with respect to the stratum pulmonary/non-pulmonary ARDS (Fig. 1). The principal investigator (TB) performed visits aimed at information and supervision of the study protocol in the participating centers. An independent Data Safety Monitoring Board monitored the study.
Fig. 1.
Screening, randomization and follow-up according to study protocol. V T tidal volume, CVP central venous pressure, MAP mean arterial pressure, vvECMO veno-venous ECMO
Treatment of the study group
The intensive care management in both groups followed the ‘best clinical evidence’ recommended by the European Society of Intensive Care Medicine [14]. The daily monitoring included the assessment of awakeness/sedation (Richmond Agitation Sedation Scale [RASS]) and the daily evaluation of the Sequential Organ Failure Assessment (SOFA) and the Simplified Acute Physiology Score (SAPS-II).
After randomization to the treatment group, percutaneous cannulation and initiation of pumpless extracorporeal lung assist (iLA AV, Novalung, Heilbronn, Germany) was performed. Unlike “classic” pump-driven extracorporeal carbon dioxide removal, iLA does not require a blood pump, because the extremely low resistance of this circuit allows flows of about 1–2 l/min with normal arterial pressures (for more detailed description: [10, 15]). Evaluation, cannulation and clinical monitoring for avECCO2-R can be found in electronic supplementary material (ESM).
After initiation of avECCO2-R, adaptation of the ventilation strategy according to study protocol was performed as follows: a rapid titration down to V T 3 ml/kg/PBW, PEEP following ARDSNet “high-PEEP/FIO2” table [16], respiratory rate 10–25/min with an inspiratory/expiratory ratio of 1:1. Termination of the avECCO2-R therapy and decannulation was performed according to a defined algorithm (see ESM).
Treatment of the control group
The ventilatory management followed the algorithm of the study group except for the use of a V T = 6 ml/kg/PBW. The target blood gases for both groups were: PaO2 ≥60 mmHg and arterial pH ≥7.2. The use of buffering (tris-(hydroxymethyl) aminomethane [TRIS]) was permitted if the patient had hypercapnia and respiratory acidosis (pH <7.2).
Weaning and extubation procedures
In both groups daily screening was performed as a precondition for carrying out a spontaneous breathing trial (SBT): ability to breathe spontaneously (FIO2 ≤0.4, SaO2 ≥90 %, PEEP ≤8 cmH2O, hemodynamic stability, RASS score ≥−1, body temperature <38.5°).
SBT was carried out over 1 h with augmented spontaneous breathing (ASB) 5 cmH2O with an active humidifier or, 10 cmH2O with HME filter (PEEP ≤8 cmH2O, flow trigger <3 l/min). Patients were extubated when no deterioration was observed over a 1 h period.
Data collection
At the time of screening (24 h prior to randomization) physiologic data were recorded and relevant laboratory, radiographic and clinical findings were collected. Throughout the complete study period, data on ventilator settings, laboratory, physiologic, radiographic and interventional data were recorded. Relevant data of the ventilation management (V T, PEEP, P plat, minute ventilation, proportion of spontaneous ventilation on minute ventilation, arterial oxygen saturation) as well as results of the blood gas analyses (PaO2, PaCO2, pH) were recorded three times daily (8 a.m., 2 p.m., 10 p.m.) and the mean values of repeated measures were used for further analysis. SOFA score, SAPS-II and RASS scores were calculated daily (8 a.m.).
In addition, in a subgroup of study patients of the Regensburg University Hospital, depending on ‘in-the-daytime’-availability of requested lab values, the levels of proinflammatory cytokines (tumour necrosis factor [TNF], interleukin 6 [IL-6] and interleukin 8 [IL-8]) were assessed from serum probes of avECCO2-R-patients (n = 20) and control patients (n = 15) at various time points during the study, since the measurement of these parameters is part of the routine laboratory program in this hospital. Furthermore, in all participating centers the daily cumulative doses of vasopressors (norepinephrine, adrenaline, dobutamine), sedative and analgesic agents (sufentanil, propofol, midazolam) and net fluid balances were calculated in each patient and recorded.
Primary outcome
The primary outcome parameter was the proportion of days without assisted ventilation in a 28-day period (“ventilator-free” days within 28 days [28-VFD]) and in a 60 days period (“ventilator-free” days within 60 days [60-VFD]) [17].
Secondary outcomes
Secondary outcomes were: inspiratory plateau pressure levels (P plat), the proportion of spontaneous breathing as a percentage of the minute ventilation (automatically calculated by the ventilator’s software), the RASS score, hemodynamic changes, the incidence of complications or adverse reactions, the frequency and duration of other adjunctive therapeutic measures, transfusion requirements [packed red blood cell transfusions (units), fresh frozen plasma units, platelet transfusion], the daily cumulative doses of analgesic and sedative agents, cumulative catecholamine requirements/24 h throughout the study period, frequency and duration of renal replacement therapy, the number of failing organs, the “organ-failure-free days” within 28 days after randomisation, and “in-hospital” mortality.
Statistical analysis
Assuming an increase in 28-VFD from 6.0 ± 10 (control group) to 11.0 ± 8 (study group [13]), we estimated that 53 patients would be needed per group for a power of 0.8 and an alpha of 0.05 (calculation by Charitè Centrum für Therapieforschung, Berlin, Germany). We assumed a “drop-out-rate” of 10 % and we calculated that 120 patients would need to be enrolled. However, after an interim analysis with 56 patients by the Data Safety Monitoring Board, it was decided to limit the study period to 3 years, since a statistical significant difference was not expected in a longer study period.
We used a Student’s t-test, the Wilcoxon test, the chi-square test or Fisher’s exact test to assess differences between the groups, as appropriate. A Kaplan–Meier curve was calculated and plotted to assess the days until successful weaning from the ventilator. Furthermore, a nonparametric analysis of longitudinal data in factorial experiments was performed. Changes in interesting clinical outcomes with respect to time were analyzed using multivariate nonparametric analysis of longitudinal data in a two-factorial design (1st [independent] factor: groups, 2nd [dependent] factor: repetitions in time). Therefore, all the time points were simultaneously compared on the corresponding response curves (analysis according to Brunner [Brunner-analysis 18]). Additionally, a post hoc analysis was performed in patients with greater hypoxemia (PaO2/FIO2 ≤150) regarding primary outcome parameters. The reported P values are two-sided and significance was set at P < 0.05.
Results
Between September 2007 and December 2010, 40 patients were randomized to avECCO2-R and 39 patients to control. Baseline data are given in Table 1. Patients did not differ with respect to age and body mass index, but in the avECCO2-R-group there were more patients with secondary ARDS. Ventilatory and gas exchange data are shown in Table 2.
Table 1.
Baseline characteristics of the patients
| avECCO2-R (n = 40) | Control (n = 39) | |
|---|---|---|
| Age (years) | 49.8 ± 12 | 48.7 ± 17 |
| Gender (male/female) | 38/2 | 30/9 |
| Lung Injury Score (Murray) | 2.8 ± 0.7 | 2.7 ± 0.8 |
| Body mass index (kg/m2) | 28.6 ± 5 | 28.8 ± 5 |
| Source of ARDS | ||
| Pulmonary/non-pulmonary ARDS | 31/9 | 37/2 |
| Non-pulmonary | ||
| SIRS/Sepsis | 5 | 1 |
| Massive transfusion | 1 | 0 |
| Trauma | 3 | 1 |
| Pulmonary | ||
| Pneumonia | 24 (58 % bacterial) | 21 (62 % bacterial) |
| Aspiration | 1 | 6 |
| Lung contusion | 6 | 9 |
| Inhalation | 1 | 0 |
| Comorbidities | ||
| Diabetes mellitus | 2 | 3 |
| COPD | 5 | 3 |
| Arterial hypertension | 10 | 7 |
| Coronary artery disease | 1 | 1 |
| Chronic renal impairment | 2 | 0 |
| Other | 19 | 15 |
| Atrial fibrillation | 3 | 2 |
| Alcohol use disorder | 2 | 3 |
| Obesity | 2 | 3 |
The data are presented as mean ± standard deviation or absolute numbers
Table 2.
Ventilation parameters and gas exchange after 24-h stabilization period at randomization
| avECCO2-R (n = 40) | Control (n = 39) | p | |
|---|---|---|---|
| PaO2/FIO2 | 152 ± 37 | 168 ± 37 | 0.044 |
| PaCO2 (mmHg) | 57.3 ± 12 | 54.3 ± 9 | 0.352 |
| Arterial pH | 7.34 ± 0.07 | 7.36 ± 0.07 | 0.317 |
| V T (ml/kg, PBW) | 5.9 ± 1.2 | 6.0 ± 0.6 | 0.495 |
| Minute ventilation (l/min) | 9.9 ± 1.6 | 9.8 ± 2.4 | 0.745 |
| Frequency/min | 22.4 ± 3 | 22.7 ± 3.5 | 0.854 |
| PEEP (cmH2O) | 16.1 ± 3 | 16.0 ± 3 | 0.898 |
| Plateau pressure (cmH2O) | 29.0 ± 5 | 28.0 ± 7 | 0.384 |
| Delta (PEEP-Plateau) (cmH2O) | 12.9 ± 4 | 12.4 ± 4 | 0.475 |
| FIO2 | 0.62 ± 0.2 | 0.53 ± 0.1 | 0.028 |
The data are presented as mean ± standard deviation
Initially all patients were ventilated with high PEEP and low tidal volume according to the ARDSNet protocol, and had moderate hypercapnia. At randomization there were no significant differences regarding mean arterial pressure, heart rate or demand vasopressor uses (data not shown). However, there was a significantly lower PaO2/FIO2-ratio in the intervention arm. The mean duration of iLA-treatment was 7.4 ± 4 days with a mean blood flow of 1.3 ± 0.2 l/min throughout the treatment period.
Primary outcome results
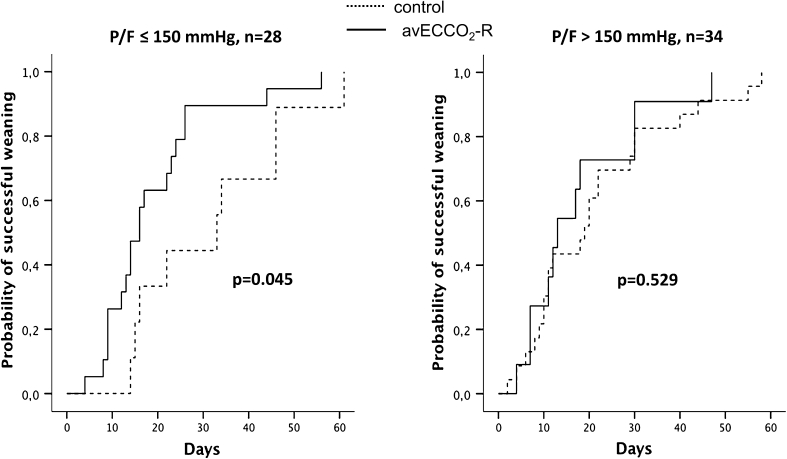
We found no statistical differences in VFD-28 or VFD-60 between groups, (Table 3), but a post hoc analysis demonstrated that surviving patients with greater hypoxemia (PaO2/FIO2 ≤150 at randomization) treated with avECCO2-R had a significantly shorter period of ventilation (VFD-60 = 40.9 ± 12.8) compared to control (28.2 ± 16.4, p = 0.033) Fig. 2). Non-pulmonary organ failure free days within 60 days, intensive care and hospital days were not statistically different between groups.
Table 3.
Outcome parameters of the study
| All patients | Subgroup: PaO2/FIO2 <150 | |||||
|---|---|---|---|---|---|---|
| avECCO2-R | Control | p | avECCO2-R | Control | p | |
| Ventilator-free-days-28 | 10.0 ± 8 | 9.3 ± 9 | 0.779 | 11.3 ± 7.5 | 5.0 ± 6.3 | 0.033 |
| Ventilator-free-days-60 | 33.2 ± 20 | 29.2 ± 21 | 0.469 | 40.9 ± 12.8 | 28.2 ± 16.4 | 0.033 |
| Non-pulmonary organ failure free days-60 | 21.0 ± 14 | 23.9 ± 15 | 0.447 | 24.1 ± 7.5 | 29.0 ± 17.7 | 0.428 |
| Lung injury score on day 10 | 2.2 ± 0.6 | 2.1 ± 0.5 | 0.854 | 2.3 ± 0.8 | 2.2 ± 0.5 | 0.601 |
| Length of stay in hospital (days) | 46.7 ± 33 | 35.1 ± 17 | 0.113 | 42.0 ± 16.6 | 40.3 ± 15.7 | 0.815 |
| Length of stay in ICU (days) | 31.3 ± 23 | 22.9 ± 11 | 0.144 | 25.9 ± 13.1 | 31.0 ± 12.7 | 0.258 |
| In-hospital mortality | 7/40 (17.5 %) | 6/39 (15.4 %) | 1.000 | 1/21 (4.8 %) | 1/10 (10 %) | 0.563 |
Fig. 2.
Post-hoc analysis: probability of successful weaning in patients presenting with PaO2/FIO2 ≤150 versus >150 (only surviving patients)
Secondary outcome results
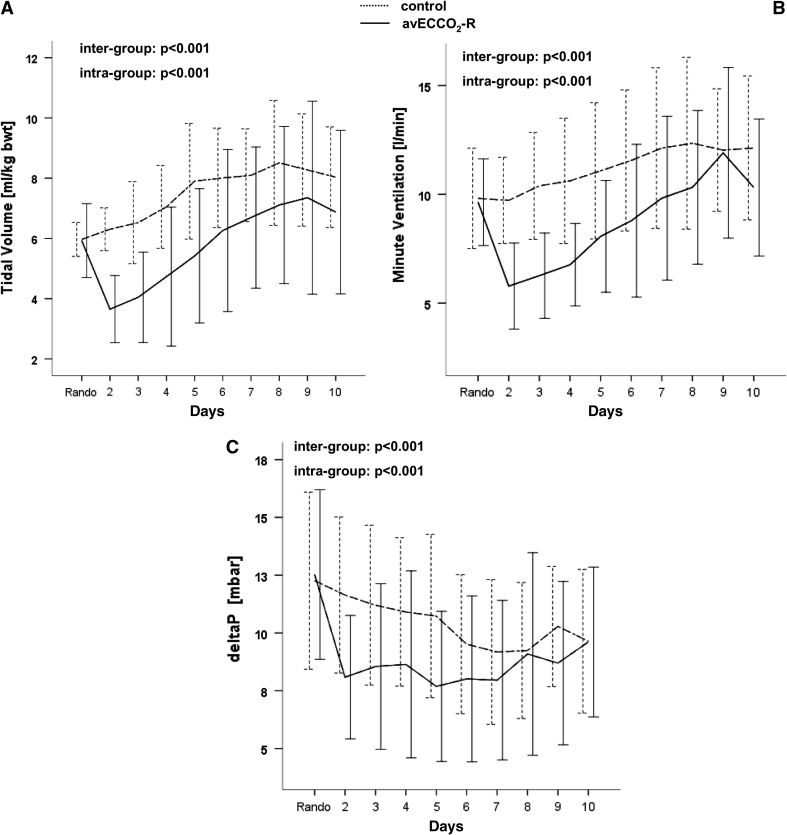
After insertion of pumpless extracorporeal lung assist, a V T of 3 ml/kg PBW was achieved in most patients which increased moderately (as spontaneous breathing increased) to day 6 after randomization (Fig. 3), while in control patients V T increased from 6 ml to 8 ml/kg/PBW (p < 0.001 between groups). Minute ventilation was significantly decreased, and the difference between plateau pressure and PEEP (P plat − PEEP) was significantly reduced in study patients compared to control.
Fig. 3.
Mean tidal volumes (ml per kg predicted body weight), minute ventilation and difference of plateau pressure and PEEP (P plat − PEEP), in the treatment and control groups during the study period
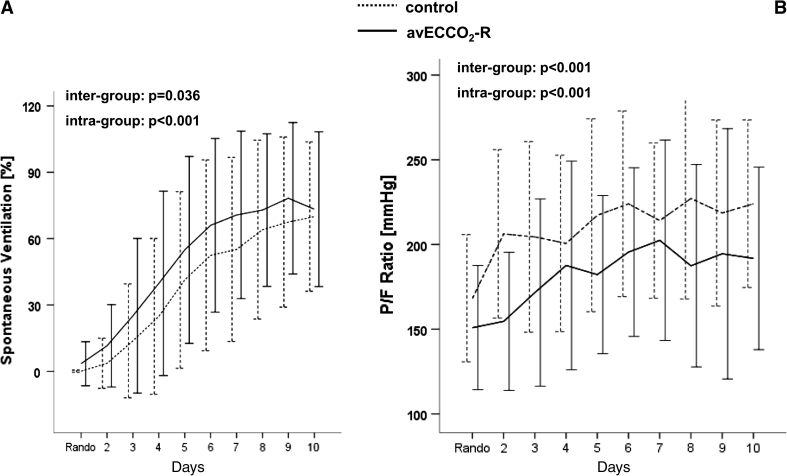
The fractional amount of augmented spontaneous breathing as a percent of total minute ventilation was significantly increased from day 3 in avECCO2-R compared to control (Fig. 4).
Fig. 4.
Percent of spontaneous ventilation on minute ventilation and oxygenation (PaO2/FIO2) in the treatment and control groups during the study period
In line with previous data, extracorporeal CO2 removal required higher FIO2 which is thought to be due to the lower partial pressure of alveolar oxygen (PAO2) secondary to a decreased lung respiratory quotient [19], and due to a reduction in functional residual capacity with a V T of 3 ml/kg compared to 6 ml/kg [20]. PaCO2-values, arterial pH, and mean respiratory rates/min were similar between groups, but mean PEEP levels tended to be elevated in the study group. During the study period, patients with avECCO2-R had a modest reduction in MAP without increased demand for continuous norepinephrine infusion.
The cumulative amount of opioid (sufentanil) and benzodiazepine infusion (midazolam) was significantly lower in the study group, but mean RASS-scores were not different between groups during the study period (Fig. 5, ESM).
The number of units of red blood cells transfused was significantly higher in the avECCO2-R -group in the period between randomization and day 10 (3.7 ± 2.4 units RBC) compared with control (1.5 ± 1.3, p < 0.05). The incidence of avECCO2-R -related adverse events was low (3 patients = 7.5 %): in one patient, transient ischemia of the lower limb was observed, while two patients developed a ‘false’ aneurysm as a result of arterial cannulation. The overall hospital mortality was low (16.5 %) and we found no significant difference between avECCO2-R-group (17.5 %) and control (15.4 %).
Results of the cytokine assessments
TNF-α, IL-6, and IL-8 levels are presented in Table 4. Serum TNF-α levels remained unchanged during the early study period in both groups, while IL-6 levels decreased significantly in the avECCO2-R-group, but not in the control group within 24 h after study initiation. IL-8 levels increased in the first few study days in the control group, but not in study patients.
Table 4.
The serum level of tumor necrosis factor (TNF), interleukin 6 (IL-6), and interleukin 8 (IL-8) in treatment and control patients (median values and 25/75 percentiles)
| TNF (pg/ml) | Before begin of the study | 24 h | 48 h | 72 h |
|---|---|---|---|---|
| avECCO2-R (n = 20) | 19.8 (13.8–23) | 20 (13.2–23.6) | 15.3 (13.7–21.4) | 22.5 (12.8–33.2) |
| Control (n = 15) | 20.5 (14.2–26.8) | 21 (13.9–48.6) | 15.9 (13.6–28) | 15.2 (12.7–25) |
| IL-6 (pg/ml) | ||||
| avECCO2-R (n = 20) | 163 (86–419) | 85 (50–193)$ | 53 (20–109)$$ | 60 (35–155)$ |
| Control (n = 15) | 97 (84–214) | 111 (52–171) | 102 (58–166) | 64 (18–90) |
| IL-8 (ng/l) | ||||
| avECCO2-R (n = 20) | 72 (23–98) | 65 (30–100) | 71 (28–94) | 81 (43–120) |
| Control (n = 15) | 34 (23–49) | 36 (24–126) | 45 (29–529) | 25 (17–191) |
$ p < 0.05 in comparison with before
$$ p < 0.01 in comparison with before
Discussion
Lung protective ventilation using V T’s of 6 ml/kg/PBW and limiting P plat to 30 cmH2O improves outcomes in patients with acute lung injury [4]. However, the concept that this approach may not be sufficiently lung protective in all patients has been suggested by a post hoc analysis of the ARDSNet data [5], by animal investigations [21], human physiological studies [3], and by a clinical study [11]. We extended these findings in patients with severe established ARDS by performing a prospective randomized trial using a strategy of very low tidal volume ventilation (3 ml/kg) and an extracorporeal lung assist system providing CO2-elimination.
The main findings of our study are: (1) Ventilation with ≈3 ml/kg PBW combined with avECCO2-R was safe and feasible, and did not result in physiologically relevant hypercapnia/acidosis. (2) The use of extracorporeal CO2-elimination was associated with a significant reduction in analgesic and sedative use, and resulted in an increased ratio of spontaneous breathing compared to control. (3) The serum levels of the pro-inflammatory cytokine IL-6 were significantly reduced in the early study period in patients treated with very low V T compared to control patients, and (4) Mechanical ventilation using lower tidal volumes (3 ml/kg) assisted by extracorporeal CO2-removal was not associated with a significant reduction of the period of mechanical ventilation within 28 or 60 days or the intensive care and hospital stay, but a post hoc analysis demonstrated that ARDS patients who were more hypoxemic (PaO2/FIO2 ≤150 at randomization) at baseline and who were treated with the low V T strategy had a significantly shorter ventilation period.
The strength of this study is the evaluation of patients with ‘established’ ARDS: We only accepted patients for randomization who passed a ‘stabilization period’ (24-h ventilation period with high PEEP) and other measures of optimization and who continued to have persistent impairment of oxygenation (PaO2/FIO2 ≤200). In a recent analysis [13] this patient group was identified as having a high mortality compared to patients with PaO2/FIO2 >200. However, our study has limitations. Due to a restriction of the enrolment period to 3 years and a ‘strict’ recruitment protocol we did not reach the pre-specified sample size. Another limitation is the fact that we only enrolled patients with stable hemodynamics, since severe cardiovascular instability was an exclusion criterion for the pumpless circuit. This exclusion criterion might explain the very low mortality rate in the overall study population.
Tidal hyperinflation [3, 4, 22], and cyclic recruitment/derecruitment [23, 24] are important mechanisms leading to ventilator-induced lung injury in patients with ARDS, but sufficient clinical data are lacking indicating that a reduction of these phenomena is beneficial. The inhomogeneously injured lung leads to heterogeneous distribution of airway pressure and V T, resulting in partial hyperinflation, cyclic opening and closing of moderate injured lung regions, and no ventilation in atelectatic regions, making it difficult to chose a single V T that completely limits ‘global’ stress/strain injury [25]. Since it is not possible to adopt ventilation to the protective ‘demands’ of different lung regions, we hypothesized that even a small V T of 6 ml/kg might aggravate VILI, and therefore we carried out the first reported randomized controlled study using a very low tidal volume lung strategy.
Our data demonstrate the integration of augmented spontaneous breathing in the ventilation management of severe ARDS patients [26, 27] without a consequent increase in tidal volume or in the demand for sedative agents. We hypothesize that avECCO2-R might allow an easy ‘switch’ from controlled low V T-ventilation to augmented spontaneous breathing with minimal patient-ventilator asynchrony. Although we did not formally assess ineffective breathing or other signs of asynchrony, we demonstrated that the respiratory rate was not different between the groups, whereas the demand for sedation was significantly lower in the avECCO2-R group. A reduction of the hypercapnia likely resulted in decreased respiratory drive as shown by Karagiannidis and coworkers [28] using neurally adjusted ventilatory assist (NAVA).
In the present study, avECCO2-R required higher fractional inspiratory oxygen concentration to maintain adequate oxygenation, while both patient groups were treated with the same high PEEP management. There are two possible mechanisms to explain this finding. The first is a decrease in alveolar ventilation due to the removal of CO2 by the extracorporeal circuit [19], and the second mechanism relates to potential de-recruitment of the lung as demonstrated by Dembinski et al. [29] in a lung lavage animal model (V T 3 ml/kg and avECCO2-R). However, in this study the authors used a relatively low PEEP level (5 cmH2O), where we used a ‘high PEEP strategy’. Such a finding is of clinical relevance when considering extracorporeal CO2-elimination as an adjunct measure for lung protective ventilation [30] with very low V T [31]. A ‘safe border’ of V T to derecruitment is not known.
On the other hand use of very small V T’s might reduce VILI. Using an experimental model, Frank et al. [21] demonstrated that a reduction in V T from 6 to 3 ml/kg led to a further reduction of epithelial and endothelial injury (extravascular lung water, alveolar epithelial type I cell antigen [RT 140]) in acid-injured rat lungs. In line with these experimental findings we found that ventilation with very low V T reduced serum levels of the proinflammatory cytokine IL-6 compared with ‘normal’ protective V T.
In recent years, techniques of extracorporeal lung support have become easier to use, with smaller devices and greater efficacy. There is evidence that this has led to a reduction in the rate of severe complications [32]. In the present study only moderate complications attributable to avECCO2-R occurred in three patients (7.5 %), and none led to permanent impairment. This complication rate is down from 24 and 12 % [10, 15], likely related to the use of a screening algorithm, careful evaluation, new material and a modified insertion technique [15].
In summary, we demonstrate that the use of very low tidal volume (≈3 ml/kg PBW) combined with extracorporeal elimination of carbon dioxide is feasible without major side effects and might be beneficial in the treatment of patients with severe ARDS. The integration of augmented spontaneous breathing might be easier and more comfortable with extracorporeal CO2-removal, and a reduced demand for sedative and analgesic medication could be advantageous. Future studies are required to determine whether ‘ultraprotective’ ventilation will improve survival in patients suffering from severe ARDS.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
We are grateful to the Members of the Data Safety Monitoring Board, Konrad Falke, Berlin, Germany, and Peter Suter, Geneva, Switzerland. This study was supported by a grant from Novalung, Heilbronn, Germany.
Conflicts of interest
T. Bein and A. Slutsky are consults for Novalung and received honoraria. A. Slutsky is also a consultant to Maquet Medical. The other authors declare no conflicts of interest.
Footnotes
T. Bein and S. Weber-Carstens contributed equally to the work.
This article is discussed in the editorial available at doi:10.1007/s00134-012-2805-8.
References
- 1.Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med. 2000;342:1334–1337. doi: 10.1056/NEJM200005043421806. [DOI] [PubMed] [Google Scholar]
- 2.Terragni PP, Rosboch G, Tealdi A, Corno E, Menaldo E, Davini O, Gandini G, Herrmann P, Mascia L, Quintel M, Slutsky AS, Gattinoni L, Ranieri VM. Tidal hyperinflation during low tidal volume ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2007;175:160–166. doi: 10.1164/rccm.200607-915OC. [DOI] [PubMed] [Google Scholar]
- 3.Grasso S, Stripoli T, Sacchi M, Sacchi M, Trerotoli P, Staffieri F, Franchini D, De Monte V, Valentini V, Pugliese P, Crovace A, Driessen B, Fiore T. Inhomogeneity of lung parenchyma during the open lung strategy: a computed tomography scan study. Am J Respir Crit Care Med. 2009;180:415–423. doi: 10.1164/rccm.200901-0156OC. [DOI] [PubMed] [Google Scholar]
- 4.The Acute Respiratory Distress Syndrome Network Ventilation with lower tidal volume as compared with traditional tidal volume for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 5.Hager DN, Krishnan JA, Hayden DL, Hayden DL, Brower RG, ARDS Clinical Trials Network Tidal volume reduction in patients with acute lung injury when plateau pressures are not high. Am J Respir Crit Care Med. 2005;172:1241–1245. doi: 10.1164/rccm.200501-048CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grasso S, Stripoli T, De Michele M, Bruno F, Moschetta M, Angelelli G, Munno I, Ruggiero V, Anaclerio R, Cafarelli A, Driessen B, Fiore T. ARDSNet ventilatory protocol and alveolar hyperinflation: role of positive end-expiratory pressure. Am J Respir Crit Care Med. 2007;176:761–767. doi: 10.1164/rccm.200702-193OC. [DOI] [PubMed] [Google Scholar]
- 7.Azzam ZS, Sharabi K, Guetta J, Bank EM, Gruenbaum Y. The physiological and molecular effects of elevated CO2 levels. Cell Cycle. 2010;15:1528–1532. doi: 10.4161/cc.9.8.11196. [DOI] [PubMed] [Google Scholar]
- 8.Peltekova V, Engelberts D, Otulakowski G, Otulakowski G, Uematsu S, Post M, Kavanagh BP. Hypercapnic acidosis in ventilator-induced lung injury. Intensive Care Med. 2010;36:869–878. doi: 10.1007/s00134-010-1787-7. [DOI] [PubMed] [Google Scholar]
- 9.Rubenfeld GD, Cooper C, Greg Carter RT, Thompson BT, Hudson LD. Barriers to providing lung-protective ventilation to patients with acute lung injury. Crit Care Med. 2004;32:1289–1293. doi: 10.1097/01.CCM.0000127266.39560.96. [DOI] [PubMed] [Google Scholar]
- 10.Bein Th, Weber F, Philipp A, Prasser C, Pfeifer M, Schmid FX, Butz B, Birnbaum D, Taeger K, Schlitt HJ. A new pumpless extracorporeal interventional lung assist in critical hypoxemia/hypercapnia. Crit Care Med. 2006;34:1372–1379. doi: 10.1097/01.CCM.0000215111.85483.BD. [DOI] [PubMed] [Google Scholar]
- 11.Terragni PP, Del Sorbo L, Mascia L, Urbino R, Martin EL, Birocco A, Faggiano C, Quintel M, Gattinoni L, Ranieri VM. Tidal volume lower than 6 ml/kg enhances lung protection: role of extracorporeal carbon dioxide removal. Anesthesiology. 2009;111:826–835. doi: 10.1097/ALN.0b013e3181b764d2. [DOI] [PubMed] [Google Scholar]
- 12.Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, LeGall JR, Morris A, Spragg R. American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- 13.Villar J, Pérez-Méndez L, López J, Belda J, Blanco J, Saralegui I, Suárez-Sipmann F, López J, Lubillo S, Kacmarek RM, HELP Network An early PEEP/FIO2 trial identifies different degrees of lung injury in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2007;176:795–804. doi: 10.1164/rccm.200610-1534OC. [DOI] [PubMed] [Google Scholar]
- 14.ESICM Systematic Review Group (Ed.) (2011) Clinical evidence in intensive care. Medizinisch Wissenschaftliche Verlagsgesellschaft, Berlin, Germany
- 15.Zimmermann M, Bein T, Arlt M, Philipp A, Rupprecht L, Mueller T, Lubnow M, Graf BM, Schlitt HJ. Pumpless extracorporeal interventional lung assist in patients with acute respiratory distress syndrome: a prospective pilot study. Crit Care. 2009;13:R10. doi: 10.1186/cc7703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brower RG, Lanken PN, Macintyre N, Matthay MA, Morris A, Ancukiewicz M, Schoenfeld D, Thompson BT, National Heart, Lung, and Blood Institute ARDS Clinical Trials Network Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351:327–336. doi: 10.1056/NEJMoa032193. [DOI] [PubMed] [Google Scholar]
- 17.Schoenfeld DA, Bernard GR, ARDS Network Statistical evaluation of ventilator-free days as an efficacy measure in clinical trials of treatments for acute respiratory distress syndrome. Crit Care Med. 2002;30:1772–1777. doi: 10.1097/00003246-200208000-00016. [DOI] [PubMed] [Google Scholar]
- 18.Brunner E, Domhof S, Langer F, editors. Nonparametric analysis of longitudinal data in factorial experiments. New York: Wiley; 2002. [Google Scholar]
- 19.Aurigemma NM, Feldman NT, Gottlieb M, Ingram RH, Jr, Lazarus JM, Lowrie EG. Arterial oxygenation during hemodialysis. N Engl J Med. 1977;297:871–873. doi: 10.1056/NEJM197710202971607. [DOI] [PubMed] [Google Scholar]
- 20.Gattinoni L, Kolobow T, Tomlinson T, Iapichino G, Samaja M, White D, Pierce J. Low-frequency positive pressure ventilation with extracorporeal carbon dioxide removal (LFPPV-ECCO2R): an experimental study. Anesth Analg. 1978;57:470–477. doi: 10.1213/00000539-197807000-00018. [DOI] [PubMed] [Google Scholar]
- 21.Frank JA, Gutierrez JA, Jones KD, Allen L, Dobbs L, Matthay MA. Low tidal volume reduces epithelial and endothelial injury in acid-injured rat lungs. Am J Respir Crit Care Med. 2002;165:242–249. doi: 10.1164/ajrccm.165.2.2108087. [DOI] [PubMed] [Google Scholar]
- 22.Chiumello D, Carlesso E, Cadringher P, Caironi P, Valenza F, Polli F, Tallarini F, Cozzi P, Cressoni M, Colombo A, Marini JJ, Gattinoni L. Lung stress and strain during mechanical ventilation for acute respiratory distress syndrome. Am J Respir Crit Care Med. 2008;178:346–355. doi: 10.1164/rccm.200710-1589OC. [DOI] [PubMed] [Google Scholar]
- 23.Bruhn A, Bugedo D, Riquelme F, Varas J, Retamal J, Besa C, Cabrera C, Bugedo G. Tidal volume is a major determinant of cyclic recruitment-derecruitment in acute respiratory distress syndrome. Minerva Anestesiol. 2011;77:418–426. [PubMed] [Google Scholar]
- 24.Caironi P, Cressoni M, Chiumello D, Ranieri M, Quintel M, Russo SG, Cornejo R, Bugedo G, Carlesso E, Russo R, Caspani L, Gattinoni L. Lung opening and closing during ventilation of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2010;181:578–586. doi: 10.1164/rccm.200905-0787OC. [DOI] [PubMed] [Google Scholar]
- 25.Plataki M, Hubmayr RD. The physical basis of ventilator-induced lung injury. Expert Rev Respir Med. 2010;4:373–385. doi: 10.1586/ers.10.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Putensen C, Muders T, Kreyer S, Wrigge H. Lung protective ventilation—protective effect of adequate supported spontaneous breathing [article in German] Anaesthesiol Intensivmed Notfallmed Schmerzther. 2008;43:456–462. doi: 10.1055/s-2008-1081393. [DOI] [PubMed] [Google Scholar]
- 27.Weber-Carstens S, Bercker S, Hommel M, Deja M, MacGuill M, Dreykluft C, Kaisers U. Hypercapnia in late-phase ALI/ADS: providing spontaneous breathing using pumpless extracorporeal lung assist. Intensive Care Med. 2009;35:1100–1105. doi: 10.1007/s00134-009-1426-3. [DOI] [PubMed] [Google Scholar]
- 28.Karagiannidis C, Lubnow M, Philipp A, Riegger GA, Schmid C, Pfeifer M, Mueller T. Autoregulation of ventilation with neurally adjusted ventilatory assist on extracorporeal lung support. Intensive Care Med. 2010;36:2038–2044. doi: 10.1007/s00134-010-1982-6. [DOI] [PubMed] [Google Scholar]
- 29.Dembinski R, Hochhausen N, Terbeck S, Uhlig S, Dassow C, Schneider M, Schachtrupp A, Henzler D, Rossaint R, Kuhlen R. Pumpless extracorporeal lung assist for protective mechanical ventilation in experimental lung injury. Crit Care Med. 2007;35:2359–2366. doi: 10.1097/01.CCM.0000281857.87354.A5. [DOI] [PubMed] [Google Scholar]
- 30.Nierhaus A, Frings DP, Braune S, Baumann HJ, Schneider C, Wittenburg B, Kluge S. Interventional lung assist enables lung protective mechanical ventilation in acute respiratory distress syndrome. Minerva Anestesiol. 2011;77:797–801. [PubMed] [Google Scholar]
- 31.Gattinoni L, Carlesso E, Langer T. Towards ultraprotective mechanical ventilation. Curr Opin Anesthesiol. 2012;25:141–147. doi: 10.1097/ACO.0b013e3283503125. [DOI] [PubMed] [Google Scholar]
- 32.Müller T, Philipp A, Luchner A, Karagiannidis C, Bein T, Hilker M, Rupprecht L, Langgartner J, Zimmermann M, Arlt M, Wenger J, Schmid C, Riegger GA, Pfeifer M, Lubnow M. A new miniaturized system for extracorporeal membrane oxygenation in adult respiratory failure. Crit Care. 2009;13:R205. doi: 10.1186/cc8213. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.