Abstract
Purpose/Background:
Female athletes have high rates of lower extremity (LE) injuries. Core strength (CS) and hip external rotator (HER) strength have been suggested to be factors that influence LE injury risk. Better balance has also been shown to decrease LE injury risk. Still, little research has examined whether core strength and hip muscle strength can influence LE balance. Therefore the purpose of the current study was to examine the relationships between core strength, hip ER strength and lower extremity balance as measured by the Star Excursion Balance Test (SEBT).
Methods:
CS was examined via the bent knee lowering test (BKLT) (grades 1‐5). Hip external rotator (HER) strength was measured singularly (HERL and HERR and combined (HERCOM) assessed via hand held dynamometry (reported in Newtons), and balance assessed via the SEBT expressed as % leg length, bilaterally in the postero‐medial, postero‐lateral, anterior directions and as a combined score (SEBTCOM). All outcomes were assessed in 45 female lacrosse players (16.0 ± 5.9 yrs, 65.1 ± 2.4 cm, 57.3 ± 7.4 kgs, experience=5.9 ± 2.9 yrs). Pearson product‐moment correlations examined relationships between the BKLT, HER and SEBT. Linear regression analyses examined possible influences of CS and HER on balance (p ≤ .05).
Results:
SEBTCOM was not correlated with BKLT [r(45)=–.20, p=.18] or HERCOM [r(45)=.20, p=.18]. There was no correlation between HER strength and CS (BKLT) [r(45)=.20, p=.20]. Overall scores on the BKLT were not correlated with any of the three balance SEBT scores. HERL [r(45)=.36, p=.02] and HERR [r(45)=.30, p=.05] were moderately positively correlated with left posteromedial SEBT direction. HERCOM and BKLT did not predict overall SEBTCOM balance scores (r2=.068, p=.23).
Conclusions:
BKLT scores and combined HER strength did not correlate with LE balance, as measured by the SEBT, in female lacrosse players. However, HER strength of both the left and right LE's (singularly) was moderately correlated with scores on one reach direction (left posteromedial) but not with combined SEBT scores. Researchers should continue to examine whether core and hip muscles influence LE balance.
Level of Evidence:
2b
Keywords: Balance, bent knee lowering test, hand held dynamometry, transversus abdominis
INTRODUCTION
Anterior cruciate ligament (ACL) and patellofemoral pain syndrome (PFPS) are among the most common lower extremity (LE) injuries in female athletes.1‐4 Females sustain ACL injuries 4‐6 times more frequently than males, leading to nearly $2 billion dollars in health care costs in the United States.1‐4 Patellofemoral pain syndrome (PFPS) in female athletes accounts for up to 20% of knee injuries seen in orthopedic centers.5‐7 Prior researchers have identified several risk factors for the increased incidence of ACL and PFPS injuries in female athletes including the lack of core strength, proximal hip muscle weakness, and lower extremity proprioception/balance deficits.1,4‐14
Equilibrium between strength and stability in the lower body kinetic chain is vital for prevention of injuries in the female athlete. Furthermore, core stability is necessary in order to provide a stable base for lower kinetic chain motion.15‐18 Core stability is defined as the foundation of trunk dynamic control that allows the production, transfer, and control of force and motion to the terminal segments of the lower body kinetic chain.9,18‐19 The transversus abdominis (TA) is the first muscle activated during lower extremity movements, indicating that it is the primary muscle linked to core stability during lower limb movements.4 Core strength (CS) is considered important because it provides proximal stability for distal mobility during athletic tasks.18 CS has been measured in prior research using the Bent Knee Lowering Test (BKLT) in conjunction with abdominal hollowing in order to actively contract and isolate the TA.20‐26
The relationship between CS and the lower extremity has been identified as a potential cause of overall lower extremity functional instability in females.4‐7,9‐12,19,27‐30 Zazulak et al9,19 demonstrated that decreased core proprioception and neuromuscular control was a predictor of knee injury risk in female athletes. However, the term “core” is often used interchangeably with hip strength. Several authors have examined the relationship of muscle weakness in the hip rather than the true abdominal musculature with lower extremity injury risk.5‐7,9‐12,19,27‐30 Overall prior researchers note that hip musculature provides a key element of stability to the knee complex, with the ability to reduce ACL and patellofemoral injuries.5‐7,14,28‐29,31‐32
Hip abductor and external rotator muscle strength are important in reducing knee adduction and internal rotation (IR) torque.31 Specifically, hip abductor and external rotator (ER) muscle strength deficits are associated with the femoral position of adduction and IR at the knee (dynamic knee valgus).5‐7,10‐12,19,28 This dynamic knee valgus position can lead to increased lateral retro‐patellar contact pressure and associated patellofemoral pain.6,27 Abdominal musculature can influence anterior pelvic tilt, which in turn increases gluteus muscle activity 33 and affects femoral internal rotation and adduction moments15,19,32‐33 Researchers examining gender differences in CS have found females to have lower side bridging endurance, hip abduction and ER isometric strength than males.8 Overall, prior authors have indicated that females may be predisposed to abnormal hip and trunk positions that may subsequently increase knee injury risk.
Decreased balance and proprioception are known risk factors for lower extremity injuries in females.34‐38 Enhanced balance could reduce knee injury risk by not allowing the knee to IR and adduct and reach a dynamic valgus position during activity. The Star Excursion Balance Test (SEBT) is a commonly used test to examine lower extremity balance/stability. Previous researchers have established that the SEBT has acceptable reliability,38‐40 and predictive validity as it can identify individuals at risk for lower extremity pathology.41 While the SEBT has 8 possible reach directions, Hertel et al40 and Plisky et al38 suggest the anterior (A), posteromedial (PM) and posterolateral (PL) directions are appropriate to assess balance. Filipa et al34 noted significant improvements on the SEBT composite scores with neuromuscular training of the lower extremity, which could possibly decrease the risk of knee injuries. Despite the research on CS, HER muscle strength and lower body balance, it is still unclear whether CS and hip ER strength actually influence lower body balance. Therefore the purpose of the current study was to examine the relationships between core strength, hip ER strength and lower extremity balance as measured by the SEBT.
METHODS
Participants
Forty‐five healthy female lacrosse players (age = 16.0 ± 5.9 yrs., height = 65.1 + 2.4 cm, mass = 57.3 ± 7.4 kg, years of experience = 5.9 ± 2.9 yrs.) participated in the study. Participants were recruited from several private high schools and private lacrosse leagues. To ensure participant homogeneity, all participants were required to be an active member of their high school or league lacrosse team. Participants had to be free from lower back and lower extremity injury in the past 3 months to participate in the study. The Physiotherapy Associates and Andrews University Institutional Review Boards approved all study procedures.
Procedures
Prior to participation, all participants and their parents/guardians received and signed an informed consent form and assent form as appropriate. Participants then performed the BKLT, had their bilateral HER strength measured using a hand‐held dynamometer, and completed the modified SEBT in a randomized order. A single examiner administered each test to all participants, and was blinded to the results of the other tests.
The Bent Knee Lowering Test (BKLT)
Participants were positioned supine with the knees and hips flexed to 90 degrees, as measured by a goniometer (Figure 1a).20 A pressure biofeedback cuff (i.e. the stabilizer pressure biofeedback unit, Chattanooga Group, Chattanooga, TN), was inflated to 40 mm Hg, and the center of the device was placed under the (Lumbar) L4–L5 segment.20,22‐25 Participants performed an abdominal hollowing maneuver while maintaining consistent 40 mm Hg pressure. To perform abdominal hollowing portion of the test, participants were positioned supine with knees bent to 45 degrees (Figure 1b). The center of the pressure cuff was placed under the lumbar lordosis at the L 4/5 segment and inflated to 40 mm Hg. Participants were instructed to draw the lower abdomen towards the spine, so as to hollow the abdomen.20,24‐26 If performed correctly, the pressure stayed at 40 mm Hg.21 Participants were not permitted to move the head or upper trunk, flex forward, push through their feet, or tilt their pelvis. If done properly, the same examiner felt tension at a point 2 cm medial and inferior to the anterior superior iliac spine (ASIS). If bulging was palpated, then the internal oblique muscle was contracting rather than the transversus abdominis muscle.20,26 Participants were then recued on how to properly perform the hallowing technique. Once participants were able to perform the abdominal hollowing maneuver, they were then instructed in the bent knee‐lowering portion of the test.
Figure 1.
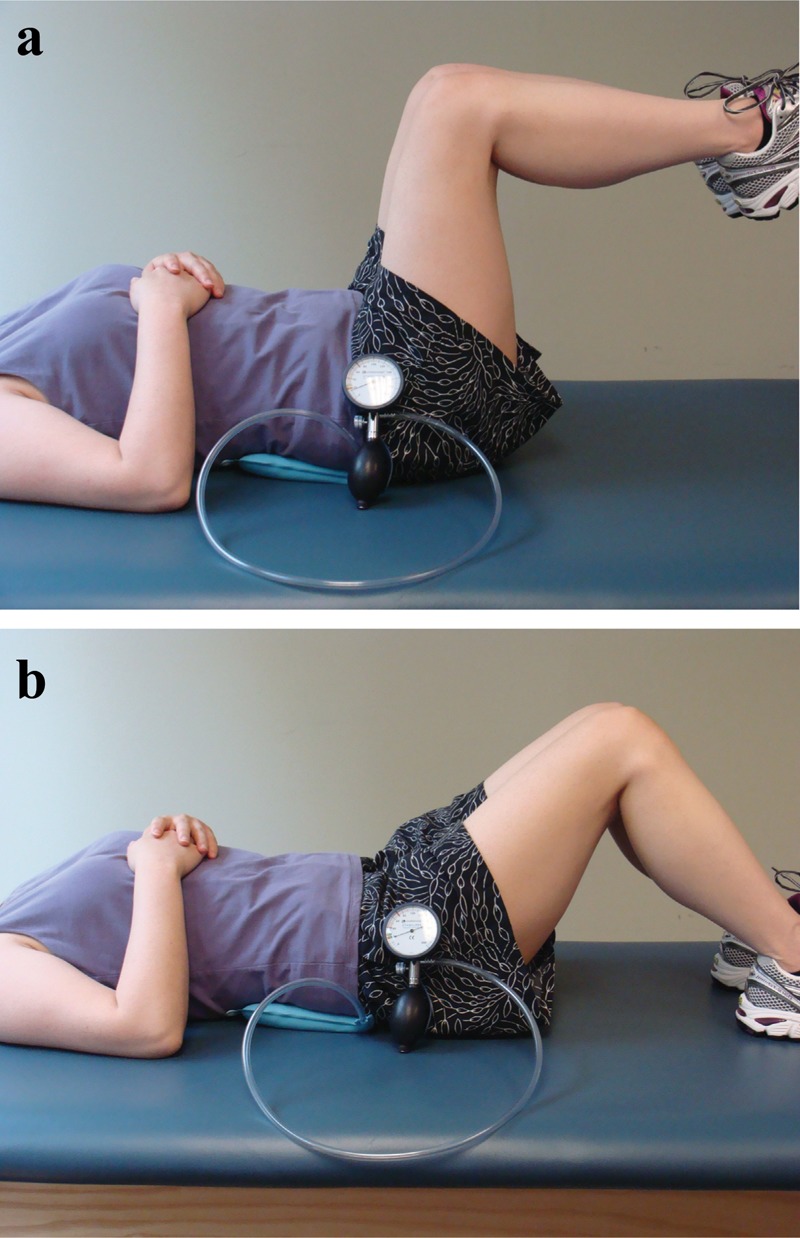
(a) Initial Position of the Bent Knee Lowering Test (BKLT). (b) Abdominal Hollowing Position of the Bent Knee Lowering Test (BKLT).
In the bent knee lowering portion of the test, participants lowered their legs toward the bed until the investigator noted a visual change on the pressure cuff monitor indicating a change in pelvic position.21 The hip angle (in degrees) was measured at this point. The strength scoring scale for the BKLT is presented in Table 1. Participants were given two practice trials prior to the three test trials. The best score from the three test trials was recorded for data analyses. A single examiner gave all participants verbal and visual instruction on the BKLT prior to testing.
Table 1.
Strength Scoring Scale for the Bent Knee Lowering Test.20
| Grade | Description |
|---|---|
| Normal (5) | Able to reach 0‐15 degrees from the table before pelvis tilts |
| Good (4) | Able to reach 16‐45 degrees from the table before the pelvis tilts |
| Fair (3) | Able to reach 46‐75 degrees from the table before the pelvis tilts |
| Poor (2) | Able to reach 76‐90 degrees from the table before the pelvis tilts |
| Trace (1) | Unable to hold the pelvis in neutral |
Hip External Rotation (HER) strength
HER isometric strength was recorded bilaterally using a hand held dynamometer (PowerTrack II commander, J‐Tech Medical, Salt Lake City, UT). The intra‐rater reliability of HER isometric strength testing has been established in prior literature.42 HER was tested in a position similar to traditional manual muscle testing procedures.43 Participants were positioned on a chair with their hips and knees flexed to 90 degrees. Then a strap was placed over their thigh and a towel roll between their knees to prevent substitution of the hip adductors.7 The dynamometer was placed five centimeters proximal to the medial malleolus. The dynamometer was zeroed prior to testing. Participants had two practice trials and three test trials. The peak value (N=Newton) from the three test trials was recorded for data analyses (HERL = Left side, HERR = Right side, HERCOM = Average HER of both HERL and HERR). The same examiner performed the HER for all participants.
Star Excursion Balance Test (SEBT)
The SEBT is a functional screening tool to assess lower extremity dynamic stability.34 The SEBT incorporates a single leg stance on one leg and requires participant to perform a maximal reach of the opposite leg along a grid in multiple directions. A modified SEBT was used in this study where 3 reach directions were measured (Anterior (A), Posteromedial (PM), Posterolateral (PL).34,13 The SEBT has been shown to have acceptable intra‐tester reliability (Intra‐class Coefficients(2,1) = 0.67 to 0.87).39 A single examiner demonstrated and completed all SEBT measurements. Participants stood on one lower extremity (stance foot), with the distal aspect of their great toe in the center of the grid. Next, they reached in an anterior, then posteromedial, and finally posterolateral direction using the other leg (reach leg), while maintaining a single leg stance (SLS). Participants performed two practice and three test trials with each leg.
The trial was not counted and was repeated if:
The participant was unable to maintain SLS
The heel of the stance foot did not remain in contact with the floor
Weight was shifted onto reach foot
The reach foot did not touch the line
The participant did not maintain start and return positions for one full second.
The farthest reach distance in each direction was recorded (cm). Reach distances were normalized to leg length (% leg length). The average of all directions was defined as SEBTCOM. Leg length was measured from the ASIS to the most distal aspect of the medial malleolus in supine, after the pelvis was leveled by lifting the hips up and lowering them to the start position.34,38
Data Analysis
Pearson product‐moment correlations were used to examine the relationships between the BKLT, HER, and SEBT. A linear regression analysis (with HERCOM and BKLT used as predictor variables entered simultaneously) examined possible influences of these variables on SEBTCOM scores. All statistical analyses were conducted using SPSS v18.0 (Statistical Package for Social Sciences, Chicago, IL) at an a priori alpha level of .05.
RESULTS
All BKLT, HER, and SEBT scores are presented in Table 2. SEBTCOM normalized scores were not correlated with BKLT [r (45) = –.20, p=.18] or HERCOM combined [r (45) =.20, p=.18]. Overall BKLT was not correlated with either SEBTCOM or other SEBT scores. HERL [r (45) = .36, p=.02] and HERR [r (45)=.30, p=.05] were moderately positively correlated with SEBTPM‐L). There was no correlation between HERCOM and CS (BKLT) [r (45)= .20, p=.20). HERCOM average and BKLTCOM did not predict overall SEBTCOM scores (r2=.068, p=.23).
Table 2.
Mean and Standard Deviations for all Tested Outcome Variables.
| Test | Variable | Mean | Standard Deviation |
|---|---|---|---|
| BKLT (degrees) | |||
| BKLT | 77.1 | 5.4 | |
| HER (Newtons) | |||
| HERL | 93.2 | 16.7 | |
| HERR | 105 | 14.7 | |
| HERCOM | 99.1 | 14.7 | |
| SEBT (% leg length) | |||
| SEBTL.A | 96.8% | 6.2% | |
| SEBTL‐PM | 87.8% | 8.5% | |
| SEBTL‐PL | 102.5% | 15.3% | |
| SEBTL‐COM | 90.1% | 6.7% | |
| SEBTR‐A | 96.3% | 7.0% | |
| SEBTR‐PM | 87.0% | 9.4% | |
| SEBTR‐PL | 82.6% | 9.3% | |
| SEBTR‐COM | 88.6% | 7.5% | |
| SEBTOVER‐COM | 89.4% | 6.9% | |
Table Legend
BKLT = Bent Knee Lowering Test, HER = Hip External Rotator Strength (N), L = Left, R = Right. COM = Combined, SEBT = Star Excursion Balance Test, A = Anterior Direction, PM = Postero‐Medial Direction, PL = Postero‐Lateral Direction, OVER = Overall, SEBT = Star Excursion Balance Test
DISCUSSION
The purpose of this study was to examine the relationships between core strength, HER strength and LE balance. We also investigated whether CS and HER muscle strength had an influence on LE balance. The primary results showed no relationships between CS, HER and SEBT scores. Hip ER strength and CS were not predictive of overall SEBT scores. However, there was an observed positive correlation between HER muscle strength bilaterally (HERL and HERR) and the left posteromedial SEBT reach direction.
Core and SEBT performance
As shown in previous research, CS is an important component of LE movement and kinematics. However, to the authors knowledge, little research exists describing the exact relationships between CS and balance. In this study, no significant correlations between CS and balance were found. One possible explanation is the actual role and contribution of TA as part of the CS. In an investigation of the effects of voluntary activation of the core musculature on frontal plane hip and knee kinematics, Shirley et al noted that participants who voluntarily activated their core musculature had improved frontal plane hip and knee kinematics as measured by the single leg squat than participants who did not activate their core.45 The BKLT20 incorporates the abdominal hollowing maneuver in order to measure core strength using the lower abdominal musculature. Specifically, and as utilized during the BKLT, the abdominal hollowing maneuver is the most typical maneuver used to activate the TA muscle.22,33 Alternatively, abdominal bracing and pelvic tilt activates the rectus abdominis and external oblique muscles in conjunction with the TA.21 Further, abdominal hollowing has been shown to demonstrate the least amount of global muscle involvement, as compared to bracing and pelvic tilt.21 The average BKLT score of this study's participants was 77.1 degrees, (classified as poor or grade 2/5 MMT of the lower abdominals).20 Despite isolating the TA by using the BKLT in the current study, it is possible that the BKLT is not as specific to TA activation as suggested in prior research. Involvement of other core muscles (external oblique, internal oblique, rectus abdominis muscles) may have influences on BKLT scores. Muscle activation of all the core musculature was not measured. Researchers can use electromyography and dynamic ultrasound in the future to help clarify the roles of these muscles with regards to balance and core stability. It is possible that other core muscles also contribute to maintenance of core stability during the BKLT. Overall it appears that future research is needed to specifically delineate the roles of TA and its contribution to core strength and lower extremity mechanics.
Hip Muscle Strength and SEBT performance
The average hip ER strength scores in the current study (HERR=105 N and HERL=93.2 N) are similar to those reported in previous literature (93.25 N).7 Most of the participants in the current study identified the right lower extremity as their dominant LE. Thus it is understandable that HERR would be stronger, allowing participants to reach further in the SEBTPM‐L direction. However, HERL was not associated with the SEBTPM‐R reach direction (standing on left reaching with right). A possible explanation for this finding may be that participants' left leg (the non‐dominant leg) may be less stable than the right leg, consequently resulting in lower reach distance on the HERL. However, the authors still are uncertain as to why HERL had a positive correlation with SEBTPM‐L reach direction, and further investigation is warranted to examine this observation.
The current findings also indicate that only HER may not influence SEBT scores. Researchers have noted that different lower extremity muscles are activated at different levels during LE balance in the SEBT.44 Prior research has identified hip extensors and abductors in combination influence lower extremity balance.7,11,34 So, it is possible that other muscles (e.g. hip extensors, abductors) individually or in combination may play a greater role in altering lower extremity balance. Future researchers should investigate the specific roles that the hip musculature may have in relation to lower extremity balance and injury risk.
Limitations and Recommendations
The authors acknowledge several study limitations. The current findings are limited to our participant group and sample. Still, to our knowledge, ours is the first combined examination of core strength, hip muscle strength, and a functional balance test in female lacrosse players. These results indicated that there are some but not necessarily consistent relationships between the two different types of measurements, an open‐chain muscle strength test of the external rotators and a functional closed‐chain test, the SEBT. Additional research is needed to examine how these open‐chain measurements relate to each other in other functional tasks (e.g. agility, speed). Maturation levels were not confirmed in our study population. Whether puberty affects all the variables examined in the current study should be further investigated. Another limitation may have been the test for core strength – the BKLT. While this test was chosen based upon prior research, it is possible that there may be another more sensitive test that may isolate the TA and better measure core strength. Finally, the hip external rotator muscles may not be the most influential or only muscles that affect balance and core strength. Additional research is necessary to determine whether other hip musculature strength e.g. hip abductors, flexors, and extensors or other factors (e.g. flexibility) may influence performance on the SEBT. Researchers should also examine how these factors influence actual lower extremity injury risk in future work.
CONCLUSIONS
The findings suggest that a TA specific core strength measure and HER do not relate to performance on the SEBT in female lacrosse players. Subjects demonstrated positive correlations between hip external rotator strength, in either the left or the right leg, and SEBT performance in the postero‐medial direction. Additional research is needed examine the roles of multiple core and hip muscles on lower extremity balance. These investigations will help elucidate the interactions between core strength, hip muscle strength, and lower extremity balance, as well as their potential combined effects on lower extremity injury risk.
References
- 1.Garrett WE, Bing Y. Mechanisms of non contact ACL injuries. Br J Sports Med. 2007;41:i47–i51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Myer GD, Ford KR, McLean SG, et al. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34(3):445–455 [DOI] [PubMed] [Google Scholar]
- 3.Hewett TE, Myer GD. Anterior Cruciate Ligament Injuries in female athletes: part 2, a meta analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006;34(3):490–498 [DOI] [PubMed] [Google Scholar]
- 4.Zazulak BT, Ponce PL, Staub SJ, et al. Gender Comparison of Hip Muscle Activity during Single Leg Landing. J Orthop Sports Phys Ther. 2005;35(5):292–299 [DOI] [PubMed] [Google Scholar]
- 5.Magalhaes E, Fukuda TY, Sacramento SN, et al. A comparison of hip strength between sedentary females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2010;40(10): 641–647 [DOI] [PubMed] [Google Scholar]
- 6.McKenzie K, Galea V, Wessel J, et al. Lower extremity kinematics of females with patellofemoral pain syndrome while stair stepping. J Orthop and Sports Phys Ther. 2010;40(10):625–632 [DOI] [PubMed] [Google Scholar]
- 7.Ireland ML, Willson JD, Ballantyne BT, et al. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33(11):671–676 [DOI] [PubMed] [Google Scholar]
- 8.Leetun DT, Ireland ML, Willson JD, et al. Core stability measures as risk factors for lower extremity injury in athletes. Medi. Sci. Sports Exerc. 2004;36(6):926–934 [DOI] [PubMed] [Google Scholar]
- 9.Zazulak BT, Hewett TE, Reeves NP, et al. The effects of core proprioception on knee injury: a prospective biomechanical-epidemiological study. Am J Sports Med. 2007;35:368–373 [DOI] [PubMed] [Google Scholar]
- 10.Souza RB, Powers CM. Predictors of hip internal rotation during running: an evaluation of hip strength and femoral structure in women with and without patellofemoral pain. Am J Sports Med. 2009;37:579–587 [DOI] [PubMed] [Google Scholar]
- 11.Earl JE, Hoch AZ. A proximal strengthening program improves pain function and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med. 2010:1–10 [DOI] [PubMed] [Google Scholar]
- 12.Boling MC, Padua DA, Marshall SW, et al. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: The joint undertaking to monitor and prevent ACL injury cohort. Am J Sports Med. 2009;37:2108–2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star excursion balance test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911–919 [DOI] [PubMed] [Google Scholar]
- 14.Ireland ML. The female ACL: why is it more prone to injury. Orthop Clin N Am. 2002;33:637–651 [DOI] [PubMed] [Google Scholar]
- 15.Hodges PW, Richardson CA. Contraction of the abdominal muscles associated with movement of the lower limb. Phys Ther. 1997;77(2):132–141 [DOI] [PubMed] [Google Scholar]
- 16.Okada T, Huxel KC, Nesser TW. Relationship between core stability, functional movement, and performance. J Strength Cond Res. 2011;25(1): 252–261 [DOI] [PubMed] [Google Scholar]
- 17.Comfort P, Pearson SJ, Mather D. An electromyographical comparison of trunk muscle activity during isometric trunk and dynamic strengthening exercises. J Strength Cond Res. 2011;25(1):149–154 [DOI] [PubMed] [Google Scholar]
- 18.Kibler WB, Press J, Sciascia A. The role of core stability in athletic function. Sports Med. 2006;36(3):189–198 [DOI] [PubMed] [Google Scholar]
- 19.Zazulak BT, Hewett TE, Reeves NP, et al. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35: 1123–1130 [DOI] [PubMed] [Google Scholar]
- 20.Dutton M. Orthopaedic Examination, Evaluation, and Intervention. McGraw Hill; 2008. [Google Scholar]
- 21.Drysdale CL, Earl JE, Hertel J. Surface electromyographic activity of the abdominal muscles during pelvic-tilt and abdominal hollowing exercises. J Athl Train. 2004;39(1):32–36 [PMC free article] [PubMed] [Google Scholar]
- 22.Hodges P, Richardson C, Jull G. Evaluation of the relationship between laboratory and clinical tests of transversus abdominis function. Physiother Res Int. 1996;1(1):30–40 [DOI] [PubMed] [Google Scholar]
- 23.Ashmen KJ, Swanik CB, Lephart SM. Strength and flexibility characteristics of athletes with chronic low back pain. J Sports Rehab. 1996;5:275–286 [Google Scholar]
- 24.Richardson C, Jull G, Toppenberg R, Comerford M. Techniques for active lumbar stabilization for spinal protection: a pilot study. Aust J Physiother. 1992;38:105–112 [DOI] [PubMed] [Google Scholar]
- 25.Jull G, Richardson C, Toppenberg R, Comerford M, Bui B. Towards a measurement of active muscle control for lumbar Stabilization. Aust J Physiother. 1993;39:187–193 [DOI] [PubMed] [Google Scholar]
- 26.O'Sullivan PB, Twomey L, Allison GT. Altered abdominal muscle recruitment in patients with chronic back pain following a specific exercise intervention. J Orthop Sports Phys Ther. 1998;27(2):114–124 [DOI] [PubMed] [Google Scholar]
- 27.Willson JD, Macleod SB, Davis IS. Lower extremity jumping mechanics of female athletes with and without patellofemoral pain before and after exertion. Am J Sports Med. 2008;36:1587–1596 [DOI] [PubMed] [Google Scholar]
- 28.Nadler SF, Malanga GA, Bartoli LA, et al. Hip muscle imbalance and low back pain in athletes: influence of core strengthening. Med. Sci. Sports Exerc. 2002;34(1):9–16 [DOI] [PubMed] [Google Scholar]
- 29.Nadler SF, Malanga GA, De Prince ML, et al. The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. Clin J Sport Med. 2000;10:89–97 [DOI] [PubMed] [Google Scholar]
- 30.Nadler SF, MaLanga GA, Feinberg JH, et al. The relationship between hip muscle imbalance and occurrence of low back pain in collegiate athletes: a prospective study. Am J Phys Med Rehabil. 2001;80(8):572–577 [DOI] [PubMed] [Google Scholar]
- 31.Thijis Y, Tiggelen DV, Willems T, et al. Relationship between hip strength and frontal plane posture of the knee during a forward lunge. Br J Sports Med. 2007;41:723–727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anderson K, Sabrina M, Strickland SM, et al. Hip and groin injuries in athletes. Am J Sports Med. 2001;29:521–533 [DOI] [PubMed] [Google Scholar]
- 33.Oh JS, Cynn HS, Won JH, et al. Effects of performing an abdominal drawing-in maneuver during prone hip extension exercises on hip and back extensor muscle activity and amount of anterior pelvic tilt. J Orthop Sports Phys Ther. 2007;37(6):320–324 [DOI] [PubMed] [Google Scholar]
- 34.Filipa A, Byrnes R, Paterno MV, Myer GD, Hewett TE. Neuromuscular training improves performance on the star excursion balance test in young females athletes. J Orthop Sports Phys Ther. 2010; 40(9): 551–558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McGuine TA, Green JJ, Best T, et al. Balance as a predictor of ankle injuries in high school basketball players. Clin J Sport Med. 2000;10(4):239–244 [DOI] [PubMed] [Google Scholar]
- 36.Hewett TE, Paterno MV, Myer GD. Strategies for enhancing proprioception and neuromuscular control of the knee. Clin Orthop Relat Res. 2002;402:76–94 [DOI] [PubMed] [Google Scholar]
- 37.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Plisky PJ, Gorman PP, Butler RJ, et al. The reliability of an instrumented device for measuring components of the star excursion balance test. North Am J Sports Phys Ther. 2009;4(2):92–99 [PMC free article] [PubMed] [Google Scholar]
- 39.Kinzey SJ, Armstrong CW. The reliability of the star excursion test in assessing dynamic balance. J Orthop Sports Phys Ther. 1998;27(5):356–360 [DOI] [PubMed] [Google Scholar]
- 40.Hertel J, Miller SJ, Denegar CR. Intratester and intertester reliability during the star excursion balance tests. J Sport Rehabil. 2009;9:104–116 [Google Scholar]
- 41.Olmsted LC, Carcia CR, Hertel J, Shultz SJ. Efficacy of the star excursion balance tests in detecting reach deficits in subjects with chronic ankle instability. J Athl Train. 2002;37(4):501–06 [PMC free article] [PubMed] [Google Scholar]
- 42.Scott, BS David A., Bond, BS E. Quin, Sisto, PhD, PT Sue Ann, Nadler, DO Scott F. The Intra- and Interrater Reliability of Hip Muscle Strength Assessments Using a Handheld Versus a Portable Dynamometer Anchoring Station. Arch Phys Med Rehab. 2004;85:598–603 [DOI] [PubMed] [Google Scholar]
- 43.Kendal FP, Mc Creary EK, Provance PG. Muscles: Testing and function. 4th ed Baltimore, MD: William and Wilkins;1993 [Google Scholar]
- 44.Earl JE, Hertel J. Lower-extremity muscle activation during the star excursion balance tests. J Sport Rehabil. 2001;10:93–104 [Google Scholar]


