Abstract
Background
Children today are exposed to cell phones early in life, and may be the most vulnerable if exposure is harmful to health. We investigated the association between cell phone use and hearing loss in children.
Methods
The Danish National Birth Cohort (DNBC) enrolled pregnant women between 1996 and 2002. Detailed interviews were conducted during gestation, and when the children were 6 months, 18 months, and 7 years of age. We used multivariable-adjusted logistic regression, marginal structural models (MSM) with inverse-probability weighting, and doubly-robust estimation (DRE) to relate hearing loss at age 18 months to cell phone use at age seven years, and to investigate cell phone use reported at age seven in relation to hearing loss at age seven.
Results
Our analyses included data from 52,680 children. We observed weak associations between cell phone use and hearing loss at age seven, with odds ratios and 95% confidence intervals from the traditional logistic regression, MSM, and DRE models being 1.21 [0.99–1.46], 1.23 [1.01–1.49], and 1.22 [1.00–1.49], respectively.
Conclusions
Our findings could have been affected by various biases and are not sufficient to conclude that cell phone exposures have an effect on hearing. This is the first large-scale epidemiologic study to investigate this potentially important association among children, and replication of these findings is needed.
Cell phone use has increased rapidly in recent years, with over 5.2 billion cell phone subscribers at the end of 2010.1–4 This has led to concern about the potential health effects of exposure to radio frequency (RF) radiation from cell phones used at close proximity to the head. Today’s children are exposed to cell phones beginning at a very early age and continuing throughout life. They will have a higher and much longer lifetime exposure than today’s adults. Children may be more susceptible to potential effects of RF due to their developing organ and tissue systems, and differences in size, shape, water content, and tissue distribution of the head.5,6 Should RF exposure from cell phones have a harmful effect on human health, children may be at the highest risk and should be given high priority in research.7
The International Agency for Research on Cancer (IARC) recently classified RF radiation as possibly carcinogenic.8 Laboratory and provocation studies have reported a range of findings across various non-cancer outcomes as well, including changes in glucose metabolism and electrical activity in the brain, effects on visual and somatosensory evoked-potentials, and reports of subjective symptoms such as fatigue and skin sensations in relation to RF exposure.9,10 Epidemiologic studies have investigated changes in behavior and cognition11–13 and headaches14 with some observing positive associations, and numerous relevant outcomes are still to be examined. While no mechanism for an effect of RF exposure from cell phones on human health has been established, these findings along with widespread exposure call for further research into potential health effects of cell phone use, particularly among young children.
As cell phones are typically positioned close to the head during use, particularly the ear, their effect on the occurrence of auditory function is of interest. While several causes of hearing loss have been identified, including genetics, otitis media, certain prenatal and early-life infections, injuries, and prolonged exposure to loud noises, a recent review suggests that, for approximately 56% of hearing impaired children in the United States, the cause is unknown.15 To date, experimental and non-experimental studies have not provided solid evidence of effects of cell phones on auditory function.16–24 The only prospective study completed on this subject was of adults and found that cell phone users had a significant increase in average auditory threshold (evidence of hearing damage) at the end of three years of follow-up compared to non-users.24 While this study may have encountered problems of bias due to loss-to-follow-up, the results point to the need for additional research in this area.
In the present study we investigated the associations between mothers’ reports of cell phone use by children and hearing loss at age seven years using data from a large birth cohort. We also examined whether hearing loss at age 18 months affects cell phone use at age seven.
METHODS
We used data from the Danish National Birth Cohort (DNBC), which enrolled 91,661 pregnant women in Denmark between 1996 and 2002. Approximately 50% of all pregnant women in Denmark at the time were invited to participate in the DNBC, and about 60% of those invited accepted the invitation. The women and the children born from their pregnancies have been followed since enrollment, and follow-up will continue for decades into the children’s lifetimes. For each pregnancy, the DNBC collected detailed information on lifestyle and environmental exposures from interviews with the mothers at gestational weeks 12 and 30 and again when the children were six and 18 months of age.25
When the children reached seven years of age, mothers were invited to complete a new questionnaire that focused on the child’s exposures, lifestyle, and health problems. Letters were sent to participants’ homes instructing them how to respond to the Internet version of the age-seven questionnaire. Women that did not respond within four weeks were sent a reminder by mail. Paper questionnaires were sent to women who still had not responded four weeks after the reminders were sent. The format and questions of the Internet and paper questionnaires were identical.12
This study was approved by the Danish Data Protection Agency, regional science ethics committees in Denmark, and the Office for the Protection of Research Subjects at the University of California, Los Angeles. All women who participated in the DNBC gave their informed consent prior to inclusion in the cohort.
Exposure
Mothers were asked in the age-seven questionnaire, “Does your child use a mobile phone? (text messages do not count)”. Response options were “No, never”, “Yes, but less than one hour/week”, and “Yes, more than one hour per week”. This question was used to generate our main exposure variable of interest, “postnatal exposure”.
Outcome
Our main outcome of interest was permanent hearing loss at age seven years, which was reported by mothers in the age-seven questionnaire in response to the question, “Does your child have permanent hearing loss?” Diagnosis of reduced hearing was reported by mothers during the age-18-months interview.
Covariates
With data collected during various time points in the lives of the DNBC children, we included a number of covariates in our analysis. Information on social-occupational status and whether the mother smoked, used alcohol, or had a fever during pregnancy was collected during the prenatal interviews. Prior occurrence of ear infection in the child and breast feeding were reported by mothers in the age-six-months and age-18-months interviews. The age-seven questionnaire included questions about mothers’ cell phone use behaviors during pregnancy (prenatal exposure) and whether or not the child ever had inner ear inflammation up to age seven years.
With Denmark’s extensive population registration system, we linked each mother and child to the Danish Medical Birth Registry, from which we obtained the mother’s age and birth data for the children, including gestational age at birth and sex.
Statistical analysis
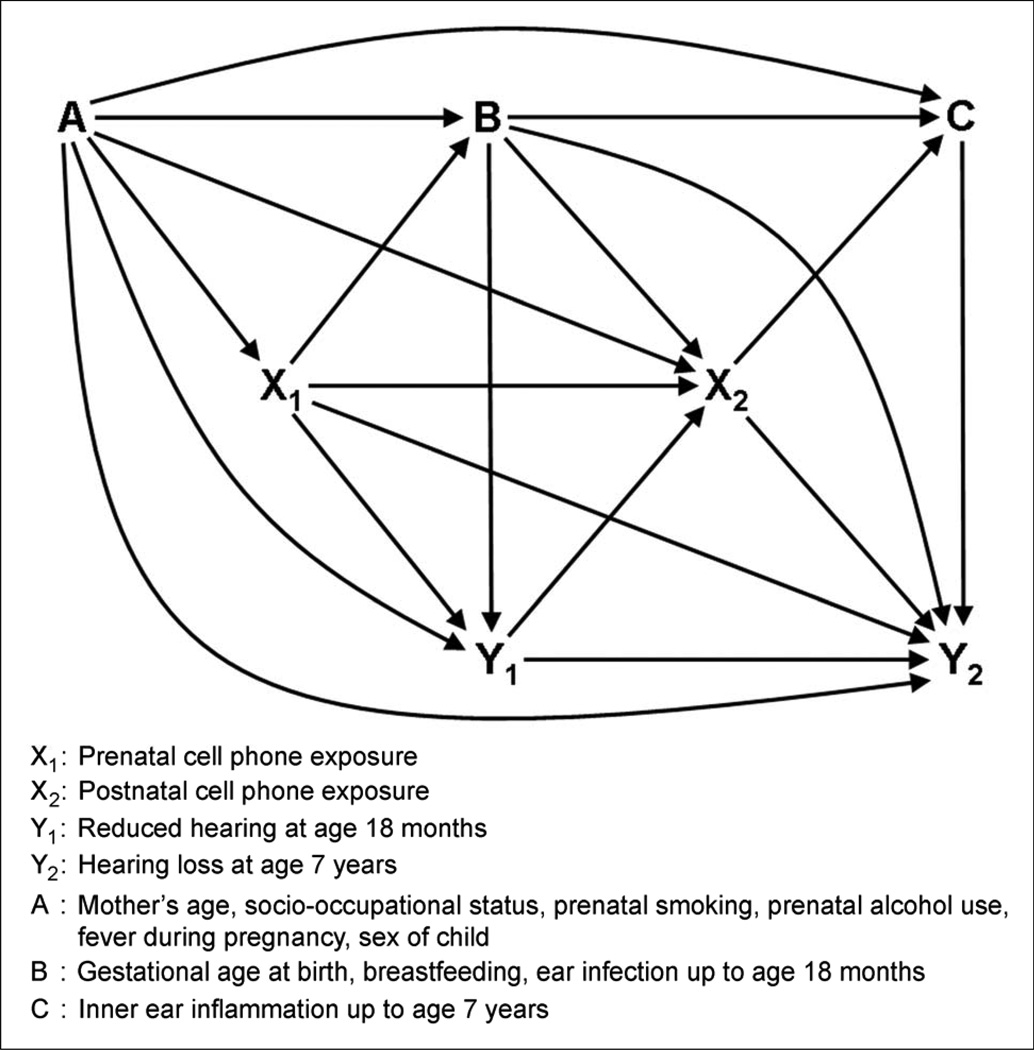
Our analyses were guided by the directed acyclic graph (DAG) shown in Figure 1. We investigated (i) whether diagnosis of reduced hearing at age 18 months (Y1) affects later cell phone use at age seven years (X2) and (ii) the association between postnatal exposure (X2) and permanent hearing loss at age seven years (Y2). We expected that both of these relationships could be affected by prenatal exposure (X1) and prenatal and postnatal variables A and B, but not by ear inflammation at age seven years.
Figure 1.
Directed Acyclic Graph for Associations between Cell Phone Exposure and Hearing Loss
For each of the two relationships, we employed three types of estimation in our analysis, partly to address possible time-varying confounding and residual confounding due to potential model misspecification.
First, we adjusted for the variables in A, B, and X1 using traditional logistic regression.
Second, we used marginal structural models (MSM), fit with inverse probability weighting (IPW).26 In our analysis of the effect of diagnosis of reduced hearing on postnatal cell phone exposure, we used logistic regression to generate a stabilized IPW: P(Y1 = y1)/P(Y1 = y1| X1 = x1, A = a, B = b). Those records with diagnosed reduced hearing Y1 = 1 were subsequently weighted by P(Y1 = 1)/P(Y1 = 1|X1 = x1, A = a, B = b), while those without reduced hearing, namely Y1 = 0, were weighted by P(Y1 = 0)/P(Y1 = 0|X1 = x1, A = a, B = b) in a second-stage logistic regression relating diagnosis of reduced hearing Y1 to postnatal exposure X2. For the association between postnatal cell phone exposure and permanent hearing loss at age seven years, we generated a stabilized IPW: P(X2 = x2)/P(X2 = x2| X1 = x1, Y1 = y1, A = a, B = b). Those records with exposure X2 = 1 were subsequently weighted by P(X2 = 1)/P(X2 = 1 | X1 = x1, Y1 = y1, A = a, B = b) while the unexposed, namely X2 = 0, were weighted by P(X2 = 0)/P(X2 = 0 | X1 = x1, Y1 = y1, A = a, B = b) in a second-stage logistic regression relating postnatal exposure X2 to outcome Y2.
Third, we combined the traditional regression model with the MSM in a so-called doubly robust estimation (DRE), aimed at hedging a bet against model misspecification provided either the traditional outcome regression or MSM model is correctly specified.27,28
The point estimates and their 95% confidence intervals (95% CI) are reported as odds ratios (OR). For the MSM and DRE, robust standard errors were used to compute the 95% CI. To estimate the possible effect of time-trends in cell phone use, results for the association of hearing loss at age seven years are presented for all children combined as well as stratified by birth year of the child. All statistical analyses were conducted in SAS version 9.2 (SAS Institute Inc., Cary, North Carolina, USA).
Sensitivity analysis
As a number of factors that were not measured by the DNBC (e.g., use of headphones or other sound-delivery devices) could have confounded the relationship between cell phone use and hearing loss, we performed sensitivity analyses to estimate the extent to which bias due to unmeasured, hence uncontrolled, confounding may have over- or under-estimated the true effect. These analyses were conducted using the methods described in the literature.29 We varied the prevalence of the unmeasured confounder among exposed and unexposed children as well as the strength of the association between the unmeasured confounder and hearing loss to reflect various plausible scenarios.
We also performed sensitivity analyses for the effect of misclassification of hearing loss at age seven years on the association of interest, again using recently published methods.29 As many cases of mild hearing loss go unnoticed and undiagnosed, and identification of hearing loss may be affected by cell phone use, misclassification of the outcome could have affected our results. The “naive” odds ratios (OR) and 95% confidence intervals (CI) calculated using the observed frequencies for postnatal cell phone use and reported hearing loss at age seven years only account for random error. To account for misclassification error, we developed eight different scenarios with varying distributions of the sensitivity and specificity of hearing loss classification. We randomly sampled values for sensitivity and specificity from these distributions, and used the sampled values to correct the numbers of exposed and unexposed migraine cases and non-cases. These corrected cell values were used to calculate adjusted ORs that accounted for systematic (here, misclassification) error as well as random error. We ran this simulation 1,000 times to obtain each misclassification adjusted OR and 95% simulation interval.
RESULTS
Of the 91,256 mothers that were invited to participate in the age-seven interview, 59,975 completed and submitted the questionnaire (66% participation rate). This study is based on data from 52,680 children from singleton births who were included in the age-seven DNBC questionnaire. Permanent hearing loss at age seven years was reported in 1.6% (n=836) of children. (Table 1) While 1,405 (2.7%) of children reportedly had a diagnosis of reduced hearing at age 18 months, only 6% (n=82) of them also had permanent hearing loss at age seven years according to mothers’ reports. (not shown)
Table 1.
Hearing Loss in Children by Postnatal Cell Phone Exposure
| Postnatal Exposure (n=18,935) |
No Postnatal Exposurea (n=33,466) |
Unknown Exposureb (n=279) |
Total (n=52,680) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | OR [95% CI] | n | % | n | % | |
| Diagnosed reduced hearing at age 18 months |
|||||||||
| Yes | 483 | 2.6 | 917 | 2.7 | 0.97 [0.87–1.09] | 5 | 1.8 | 1,405 | 2.7 |
| Noa | 14,096 | 74.4 | 25,979 | 77.6 | 198 | 71.0 | 40,273 | 76.4 | |
| Permanent hearing loss at age 7 years |
|||||||||
| Yes | 338 | 1.8 | 490 | 1.5 | 1.23 [1.07–1.41] | 8 | 2.9 | 836 | 1.6 |
| Noa | 17,984 | 95.0 | 32,024 | 95.7 | 195 | 69.9 | 50,203 | 95.3 | |
Percentages do not sum to 100% due to missing responses
Reference
Unknown exposure refers to children whose mothers did not report their child’s cell phone exposure
Approximately 36% (n=18,935) of children used a cell phone at age seven years, (Table 2) but less than 1% used it more than one hour per week (not shown). Thirty-nine percent of mothers used a cell phone during pregnancy, and mothers who used a cell phone prenatally were more likely to have children who used a cell phone at age seven years. Boys were less likely than girls to use a cell phone at age seven, and being breast-fed was also negatively associated with postnatal cell phone use. While about one-third of children had an ear infection by the age of 18 months, 61% had experienced inner ear inflammation by the time they reached seven years of age according to mothers’ reports.
Table 2.
Distribution of Covariates by Postnatal Cell Phone Exposure
| Postnatal Exposure (n=18,935) |
No Postnatal Exposurea (n=33,466) |
Unknown Exposureb (n=279) |
Total (n=52,680) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | OR [95% CI] | n | % | n | % | |
| Prenatal cell phone use | |||||||||
| Yes | 9,781 | 51.7 | 10,690 | 31.9 | 2.40 [2.31–2.49] | 11 | 3.9 | 20,482 | 38.9 |
| Noa | 8,213 | 43.4 | 21,507 | 64.3 | 74 | 26.5 | 29,794 | 56.6 | |
| Prenatal smoking | |||||||||
| Yes | 5,380 | 28.4 | 7,047 | 21.1 | 1.51 [1.45–1.58] | 87 | 31.2 | 12,514 | 23.8 |
| Noa | 12,113 | 64.0 | 24,017 | 71.8 | 162 | 58.1 | 36,292 | 68.9 | |
| Prenatal alcohol use | |||||||||
| Yes | 6,254 | 33.0 | 11,386 | 34.0 | 0.97 [0.93–1.01] | 91 | 32.6 | 17,731 | 33.7 |
| Noa | 10,615 | 56.1 | 18,762 | 56.1 | 145 | 52.0 | 29,522 | 56.0 | |
| Fever during pregnancy | |||||||||
| Yes | 4,678 | 24.7 | 8,115 | 24.2 | 1.05 [1.01–1.09] | 73 | 26.2 | 12,866 | 24.4 |
| Noa | 12,352 | 65.2 | 22,477 | 67.2 | 167 | 59.9 | 34,996 | 66.4 | |
| Child ever had ear infection up to age 18 months |
|||||||||
| Yes | 6,082 | 32.1 | 10,767 | 32.2 | 1.05 [1.01–1.10] | 80 | 28.7 | 16,929 | 32.1 |
| Noa | 7,298 | 38.5 | 13,564 | 40.5 | 106 | 38.0 | 20,968 | 39.8 | |
| Child ever had inner ear inflammation up age 7 years |
|||||||||
| Yes | 11,889 | 62.8 | 20,177 | 60.3 | 1.11 [1.07–1.15] | 176 | 63.1 | 32,242 | 61.2 |
| Noa | 7,018 | 37.1 | 13,218 | 39.5 | 98 | 35.1 | 20,334 | 38.6 | |
| Social-occupational Status | |||||||||
| High | 11,782 | 62.2 | 22,891 | 68.4 | 0.56 [0.51–0.62] | 157 | 56.3 | 34,830 | 66.1 |
| Medium | 5,436 | 28.7 | 8,294 | 24.8 | 0.71 [0.64–0.79] | 85 | 30.5 | 13,815 | 26.2 |
| Lowa | 797 | 4.2 | 866 | 2.6 | 16 | 5.7 | 1,679 | 3.2 | |
| Mother's age at birth of child | |||||||||
| Older than 35 years | 2,235 | 11.8 | 4,614 | 13.8 | 0.52 [0.49–0.56] | 39 | 14.0 | 6,888 | 13.1 |
| 31 to 35 years | 6,198 | 32.7 | 12,478 | 37.3 | 0.54 [0.50–0.57] | 103 | 36.9 | 18,779 | 35.6 |
| 26 to 30 years | 7,865 | 41.5 | 13,527 | 40.4 | 0.63 [0.59–0.67] | 106 | 38.0 | 21,498 | 40.8 |
| 25 years or youngera | 2,637 | 13.9 | 2,847 | 8.5 | 31 | 11.1 | 5,515 | 10.5 | |
| Mean (SD) | 30.1 (4.4) | 30.9 (4.1) | 30.8 (4.6) | ||||||
| Gestational age at birth | |||||||||
| Post-term (>42 weeks) | 304 | 1.6 | 602 | 1.8 | 0.80 [0.67–0.94] | 3 | 1.1 | 909 | 1.7 |
| Normal (37–42 weeks) | 17,919 | 94.6 | 31,730 | 94.8 | 0.89 [0.81–0.98] | 264 | 94.6 | 49,913 | 94.7 |
| Pre-term (< 37 weeks)a | 667 | 3.5 | 1,051 | 3.1 | 10 | 3.6 | 1,728 | 3.3 | |
| Mean (SD) | 40.0 (1.8) | 40.0 (1.7) | 39.9 (2.0) | ||||||
| Sex of child | |||||||||
| Boy | 8,876 | 46.9 | 17,968 | 53.7 | 0.76 [0.73–0.79] | 144 | 51.6 | 26,988 | 51.2 |
| Girla | 10,059 | 53.1 | 15,498 | 46.3 | 135 | 48.4 | 25,692 | 48.8 | |
| Child was breast fed | |||||||||
| Yes | 11,091 | 58.6 | 21,379 | 63.9 | 0.82 [0.78–0.86] | 148 | 53.0 | 32,618 | 61.9 |
| Noa | 4,270 | 22.6 | 6,745 | 20.2 | 68 | 24.4 | 11,083 | 21.0 | |
Percentages do not sum to 100% due to missing responses
Reference
Unknown exposure refers to children whose mothers did not report their child’s cell phone exposure
We did not observe an association between reduced hearing at age 18 months and postnatal cell phone exposure. None of the analytic approaches we used, namely, traditional logistic regression, MSM with IPW, and DRE, produced ORs suggesting an effect. (Table 3)
Table 3.
Odds Ratios for the Association Between Hearing Loss at Age 18 months and Postnatal Cell Phone Exposure (According to Mothers' Reports)
| OR [95% CI] | |
|---|---|
| Unadjusted | 0.97 [0.87–1.09] |
| Adjusted, traditional outcome regression modela | 0.98 [0.85–1.12] |
| Adjusted, marginal structural model with IPWa | 0.94 [0.80–1.10] |
| Adjusted, doubly robust estimation modelb | 0.93 [0.79–1.10] |
Adjustment model or IPW included mother's cell phone use during pregnancy, alcohol use during pregnancy, smoking during pregnancy, fever during pregnancy, mother's age, social-occupational status, breast feeding, ear infection by age 18 months, sex of child, and gestational age at birth.
Doubly robust estimation combining covariate adjustment in the traditional outcome regression with IPW application in a marginal structural model using adjustment scheme.
Overall, we observed weak associations between postnatal exposure and hearing loss at age seven years for all birth years combined. The ORs and 95% CIs for the traditional, MSM, and DRE models are 1.21 [0.99–1.46], 1.23 [1.01–1.49], and 1.22 [1.00–1.49], respectively. (Table 4) Stratification by the child’s birth year did not reveal any clear time-trend effects, although these results were imprecise.
Table 4.
Odds Ratios for the Association Between Postnatal Cell Phone Exposure and Hearing Loss in Children at Age 7 Years (According to Mothers' Reports)
| Year of Child’s Birth | Unadjusted | Adjusted, traditional outcome regression modela |
Adjusted, marginal structural model with IPWa |
Adjusted, doubly robust estimation modelb |
|---|---|---|---|---|
| 1997 (n=24) | --c | --c | --c | --c |
| 1998 (n=6,779) | 1.12 [0.75–1.68] | 1.18 [0.61–2.26] | 1.34 [0.70–2.54] | 1.32 [0.68–2.55] |
| 1999 (n=11,298) | 1.29 [0.96–1.74] | 1.18 [0.78–1.77] | 1.17 [0.78–1.77] | 1.17 [0.78–1.77] |
| 2000 (n=13,131) | 1.33 [1.00–1.76] | 1.46 [1.01–2.11] | 1.48 [1.02–2.15] | 1.48 [1.02–2.15] |
| 2001 (n=11,319) | 1.08 [0.79–1.48] | 0.79 [0.49–1.28] | 0.80 [0.49–1.30] | 0.79 [0.48–1.29] |
| 2002 (n=9,136) | 1.39 [1.00–1.92] | 1.32 [0.86–2.00] | 1.34 [0.88–2.03] | 1.33 [0.87–2.03] |
| 2003 (n=993) | 0.85 [0.27–2.70] | 5.17 [0.52–51.41] | 3.43 [0.37–32.20] | --c |
| Combined (n=52,680) | 1.23 [1.07–1.41] | 1.21 [0.99–1.46] | 1.23 [1.01–1.49] | 1.22 [1.00–1.49] |
Adjustment model or IPW included mother's cell phone use during pregnancy, alcohol use during pregnancy, smoking during pregnancy, fever during pregnancy, mother's age, social-occupational status, breast feeding, ear infection by age 18 months, sex of child, and gestational age at birth, and reduced hearing at age 18 months.
Doubly robust estimation combining covariate adjustment in the traditional outcome regression with IPW application in a marginal structural model using adjustment scheme.
Insufficient sample size
Our sensitivity analyses for unmeasured confounding suggest that the weak associations we observed between postnatal cell phone exposure and hearing loss at age 7 are unlikely to have been due to confounding only. (Table 5) It is only after adjustment for a very strong confounder (e.g., one that produces a 2–3 fold increase in risk of both hearing loss and cell phone exposure) that we see a complete attenuation of the association between cell phone exposure and hearing loss. Adjustment for more moderate confounders produced little change in the results.
Table 5.
Sensitivity of Odds Ratios for Association Between Postnatal Cell Phone Exposure and Hearing Loss in Children at Age 7 Adjusted for Unmeasured Confounding
| Prevalence of unmeasured confounder |
ORCD |
|||||
|---|---|---|---|---|---|---|
| 1.10 | 1.25 | 1.50 | 2.00 | 3.00 | ORCX | |
| p1=0.65, p0=0.38 | 1.20 | 1.16 | 1.10 | 1.03 | 0.94 | 3.03 |
| p1=0.60, p0=0.40 | 1.21 | 1.17 | 1.13 | 1.07 | 1.00 | 2.25 |
| p1=0.50, p0=0.40 | 1.22 | 1.20 | 1.18 | 1.15 | 1.11 | 1.50 |
| p1=0.40, p0=0.35 | 1.22 | 1.21 | 1.20 | 1.18 | 1.16 | 1.24 |
| p1=0.25, p0=0.23 | 1.23 | 1.22 | 1.22 | 1.21 | 1.20 | 1.12 |
| p1=0.23, p0=0.25 | 1.23 | 1.23 | 1.24 | 1.25 | 1.26 | 0.90 |
| p1=0.35, p0=0.40 | 1.23 | 1.24 | 1.25 | 1.27 | 1.30 | 0.81 |
| p1=0.40, p0=0.50 | 1.24 | 1.26 | 1.28 | 1.32 | 1.36 | 0.67 |
| p1=0.40, p0=0.60 | 1.25 | 1.28 | 1.33 | 1.40 | 1.50 | 0.44 |
| p1=0.38, p0=0.65 | 1.26 | 1.30 | 1.37 | 1.47 | 1.61 | 0.33 |
ORCD = Odds ratio for association between unmeasured confounder and hearing loss
ORCX = Odds ratio for association between unmeasured confounder and postnatal cell phone exposure
p1 = prevalence of unmeasured confounder among exposed children
p0 = prevalence of unmeasured confounder among unexposed children
Unadjusted OR = 1.23
Table 6 summarizes the results of our sensitivity analysis for misclassification of hearing loss at age seven years. In all scenarios after accounting for both systematic and random error, the odds ratios for the association between postnatal cell phone exposure and hearing loss increased to approximately 1.8. This suggests that if misclassification of hearing loss affected our results, it would have most likely biased our estimates of association toward the null under plausible or our assumed priors and models.
Table 6.
Results of Probabilistic Bias Analysis of Hearing Loss Misclassification (n = 1,000 simulations)
| Sensitivity of Hearing Classification |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Postnatal Cell Phone Use | No postnatal cell phone use | Simulation OR (95% Simulation Interval) | ||||||||
| min | m1 | m2 | max | min | m1 | m2 | max | Naive Error | Systematic Error | Total Error |
| 0.10 | 0.25 | 0.35 | 0.50 | 0.10 | 0.25 | 0.35 | 0.50 | 1.23 [1.07–1.41] | 1.81 [1.29–14.93] | 1.83 [1.22–15.23] |
| 0.20 | 0.35 | 0.45 | 0.60 | 0.10 | 0.25 | 0.35 | 0.50 | 1.23 [1.07–1.41] | 1.79 [1.28–25.30] | 1.79 [1.21–26.55] |
| 0.10 | 0.25 | 0.50 | 0.75 | 0.10 | 0.25 | 0.50 | 0.75 | 1.23 [1.07–1.41] | 1.75 [1.28–19.23] | 1.76 [1.22–20.46] |
| 0.20 | 0.35 | 0.60 | 0.85 | 0.10 | 0.25 | 0.50 | 0.75 | 1.23 [1.07–1.41] | 1.82 [1.27–22.01] | 1.81 [1.22–22.38] |
| 0.20 | 0.35 | 0.60 | 0.85 | 0.20 | 0.35 | 0.60 | 0.85 | 1.23 [1.07–1.41] | 1.76 [1.28–14.56] | 1.76 [1.22–13.86] |
| 0.35 | 0.45 | 0.70 | 0.95 | 0.20 | 0.35 | 0.60 | 0.85 | 1.23 [1.07–1.41] | 1.80 [1.27–19.84] | 1.80 [1.22–19.10] |
| 0.50 | 0.65 | 0.75 | 0.95 | 0.50 | 0.65 | 0.75 | 0.95 | 1.23 [1.07–1.41] | 1.77 [1.27–18.33] | 1.77 [1.23–17.70] |
| 0.60 | 0.75 | 0.85 | 0.99 | 0.50 | 0.65 | 0.75 | 0.95 | 1.23 [1.07–1.41] | 1.78 [1.27–20.86] | 1.77 [1.19–20.72] |
Assumes trapezoidal distributions for specificity and sensitivity of hearing loss classification where min = minimum, m1 = mode 1, m2 = mode 2, max = maximum
Distribution of specificity of hearing classification is the same for all scenarios: min = 0.95, m1 = 0.97, m2 = 0.97, max = 1.00
COMMENTS
In this study, we observed a weak association between cell phone use and hearing loss in children at age seven years. This is the first large-scale study in children to examine this association, and it has the advantage of a large sample size and allows for adjustment of a number of potential confounding factors. However, our results should be interpreted with caution, and do not mean that cell phone use has an effect on the development of hearing loss in children, as biases may have contributed to the observed findings.
The primary association of interest in this study – between postnatal cell phone exposure and hearing loss at age seven years – was estimated using a cross-sectional analysis. Since both the exposure and outcome were assessed from mothers’ reports in the age-seven questionnaire of the DNBC, we cannot account for the temporality of the association, and therefore our results cannot be used to assess the direction of causation. However, the present study serves as a primary investigation into this association using the DNBC data. As the age-11 data collection in the DNBC is currently underway, we may revisit this association in future investigations using a prospective analysis once the latest dataset is available.
Our outcome variables were based on mothers’ reports of hearing loss in children, and while we expect mothers to be able to report this information accurately, we cannot rule out the possibility of misclassification. We expect most diagnoses of hearing loss in children at age seven years to be made by physicians or during school hearing screening exams and that mothers are most likely aware of their children’s hearing diagnoses. The data collection instrument included many questions on a wide range of outcomes and exposures, and questions about hearing loss were asked separately from questions about cell phone use. Further, at the time of the age-seven data collection, no studies had been published to cause mothers to believe that cell phone exposure was associated with hearing loss. It is therefore unlikely that our data suffered from a differential reporting error that biased our results.
While only a small percentage of the children who were reportedly diagnosed with reduced hearing at age 18 months had permanent hearing loss at age seven years, this change in prevalence is not surprising. Most cases of reduced hearing in very young children are temporary and often due to infections.30 In some cases, these conditions can lead to permanent damage to auditory function and children with recurrent ear infections are at higher risk for hearing loss, but the underlying causes of permanent hearing loss at age seven years in our study may be different from most cases of reduced hearing at age 18 months. This reasoning is consistent with our results relating reduced hearing at age 18 months to cell phone use at age seven years. If hearing loss in early childhood were to persist up to age seven years, we would have expected reduced hearing at age 18 months to be negatively associated with cell phone use. However, we found no association, which likely reflects the temporary nature of reduced hearing in early life. Further, it is possible that the few children who did suffer permanent hearing loss in early life were undeterred from using a cell phone in later childhood with the help of hearing treatment, which now is compatible with cell phone use.
Many cases of mild hearing loss are likely to have gone unnoticed. The prevalence of hearing loss in children and adolescents in the United States is estimated at approximately 3% based on clinical data, but the prevalence based on parent/self-reported data is considerably lower at 1.9%.15 This discrepancy is in line with our data in the DNBC, and suggests that some children in our study with mild hearing loss may have been misclassified because the condition went unnoticed. Should cell phone exposure have an effect on auditory functioning in children, we would expect the effect to be mild. Rather than producing severe hearing loss, it is more likely that cell phone exposure could have a weak effect on hearing, thus increasing the hearing threshold only slightly upon prolonged exposure. Even a weak effect of this highly prevalent exposure can have a profound impact on public health and childhood school performance.31,32
We did not include hearing diagnoses from the Danish National Hospital Register in our analyses. As the hospital register includes only those diagnoses made during hospital admissions, visits to emergency rooms, and visits to specialty outpatient clinics, it is likely to include only the most serious cases of hearing loss or those related to another hearing-related condition. Since any effect of cell phone exposure on the development of hearing loss, should it exist, is likely to be small, the cases in the hospital register are unlikely to be caused by cell phone exposure alone. Future investigations into this association among the DNBC children may allow us to use data from the school screening tests.
Exposure assessment in this study was limited to mothers’ reports of their children’s cell phone use at age seven years. Although actual RF exposure was not measured, mothers reported that most children were not using cell phones at age seven years, and those who were did so for short periods of time. Therefore, children’s overall exposure to RF from cell phones was most likely low. While no mechanism for harmful effects of RF from cell phones has been demonstrated, and we did not observe strong associations between cell phone exposure and hearing loss in children, we cannot rule out the possibility that RF from cell phone exposure could have an effect. Future studies using prospective data on exposure and additional outcome information are needed to better document the possible relationship.
We do not expect high levels of exposure misclassification to have affected our results. Although objective measures of cell phone use and RF exposure with more detailed information would have been ideal, obtaining such measurements was not feasible in this large sample of children. Regardless, assessment of the child’s cell phone use was very general (whether the child uses a cell phone more or less than one hour per week or not at all), and mothers should be able to answer the question accurately.
Selection bias is unlikely to account for the results we observed, as both the exposure and outcome of interest occurred after enrollment into the cohort. Therefore, women who chose not to participate in the DNBC are unlikely to be different from participants on factors that could introduce bias into our results.
A large proportion of the original study participants were not included in our analysis due to non-response during age-seven data collection. A recent study estimating loss-to-follow-up bias in the DNBC found that mothers who were lost-to-follow-up were more likely to be in the low social-occupational status category than women who continued participation.33 Several studies have reported that cell phone use among children and adolescents is inversely associated with social-occupational status.34–38 Therefore, it is possible that children (and possibly mothers) who are heavier cell phone users may have been less likely to continue follow-up in the DNBC, and therefore are under-represented in our data. Denmark has a relatively homogenous population in terms of healthcare access and utilization, and therefore diagnoses of hearing loss are unlikely to be related to social-occupational status in Denmark. Therefore, loss-to-follow-up bias in relation to SES is not likely to account for our results.
It is possible that our results reflect detection bias. Children with hearing loss may notice that they have difficulty communicating by voice calls on a cell phone, and may therefore be more likely to get a hearing examination and diagnosis than children who do not use a cell phone. On the other hand, the opposite may also be possible since increasing the volume on the cell phone speaker may compensate for poor hearing for some children. Due to the nature of the exposure and outcome in this case, questionnaire-based epidemiologic investigations of this relationship may be prone to detection bias. However, investigations using data from school hearing screening tests, where all children are screened for hearing loss, can bypass the issue of detection bias.
As an additional check, we performed sensitivity analyses to estimate the impact of possible unmeasured confounding and outcome misclassification on our results. Our sensitivity analyses suggested that our results are unlikely to be due to unmeasured confounding or misclassification of hearing loss alone. Only a very strong risk factor for both hearing loss and cell phone exposure could have produced the results we observed, and we do not expect such a risk factor to be highly prevalent among children. Nonetheless, since uncontrolled confounding is untestable and pervasive in observational epidemiology, we cannot rule it out a possible explanation for our findings. The sensitivity analyses also suggested that misclassification of hearing loss across a number of plausible scenarios is more likely to have attenuated our results than to have produced spurious associations in the positive direction.
Our study has the advantage of a large sample size with good exposure contrast and rich covariate data from a well-published prospective cohort. Given that cell phones were still gaining popularity and were not as frequently used by children as they are today, our study captured a large number of both exposed and unexposed children. Children born today are likely to start using cell phones earlier and to continue for longer periods of time. A study like this may be much more difficult to repeat today, as very few non-exposed children remain.39,40
Using data from the DNBC offers many additional advantages. With long-term follow-up of the children and linkage to population registers we were able to measure and control for a large number of variables in our analysis. Further, Denmark is a relatively homogenous population in terms of ethnic background, socio-economic status, and access to healthcare, resulting in less likelihood of confounding by these factors compared to studies conducted in many other countries.
The associations between cell phone use and hearing loss in children that we observed in this study are not sufficient to conclude that cell phone exposure has an effect on hearing, but they provide justification for continuing to study this association. As the DNBC is an ongoing study, follow-up of children and mothers is planned to continue for several years to come, allowing for longitudinal analysis of the association between cell phone use and hearing loss outcomes in the future. The latest wave of data collection is currently underway, with questionnaires to be completed by mothers and their children at the age of 11 years. The age-11 questionnaire includes more detailed exposure assessment questions. Additionally, all school children in Denmark undergo hearing examinations as part of a nation-wide screening. As the latest DNBC data become available, we hope to investigate this association further with a prospective analysis and linkage to school-based hearing examination results. Replication of this work in other cohorts, particularly of children, is needed.
ACKNOWLEDGEMENTS
This work was supported by the Lundbeck Foundation [grant number 195/04]; the Danish Medical Research Council [grant number SSVF 0646]; the National Institutes of Health/National Institute of Environmental Health Sciences [grant number R21ES016831]; and a Veni career grant from the Netherlands Organization for Scientific Research (NWO) to OAA [grant number 916.96.059].
The authors would like to thank the coordinator of data collection, Inge Kristine Meder, data analysts, Inge Eisensee and Lone Fredslund Møller, and the participating mothers.
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Geekzone. [Accessed January 2013];Number of mobile phone users worldwide to increase to 2 billion by 2007. 2003 http://www.geekzone.co.nz/content.asp?contentid=1245.
- 2.MyBroadband. [Accessed January 2013];Mobile broadband: do we need another technology war? 2008 http://mybroadband.co.za/news/Wireless/3498.html.
- 3.International Telecommunication Union. ITU sees 5 billion mobile subscriptions globally in 2010. [Accessed January 2013];Newsroom Press Release. 2010 http://www.itu.int/net/pressoffice/press_releases/2010/06.aspx.
- 4.International Telecommunication Union. Global mobile cellular subscriptions, total and per 100 inhabitants. 2000-20102011. [Google Scholar]
- 5.Kheifets L, Repacholi M, Saunders R, van Deventer E. The sensitivity of children to electromagnetic fields. Pediatrics. 2005;116(2):e303–e313. doi: 10.1542/peds.2004-2541. [DOI] [PubMed] [Google Scholar]
- 6.Wiart J, Hadjem A, Wong MF, Bloch I. Analysis of RF exposure in the head tissues of children and adults. Phys Med Biol. 2008;53(13):3681–3695. doi: 10.1088/0031-9155/53/13/019. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. [Accessed January 2013];WHO Research Agenda for Radiofrequency Fields. 2010 http://whqlibdoc.who.int/publications/2010/9789241599948_eng.pdf.
- 8.Baan R, Grosse Y, Lauby-Secretan B, El Ghissassi F, Bouvard V, Benbrahim-Tallaa L, et al. Carcinogenicity of radiofrequency electromagnetic fields. Lancet Oncol. 2011;12(7):624–626. doi: 10.1016/s1470-2045(11)70147-4. [DOI] [PubMed] [Google Scholar]
- 9.Volkow ND, Tomasi D, Wang GJ, Vaska P, Fowler JS, Telang F, et al. Effects of cell phone radiofrequency signal exposure on brain glucose metabolism. JAMA. 2011;305(8):808–813. doi: 10.1001/jama.2011.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Rongen E, Croft R, Juutilainen J, Lagroye I, Miyakoshi J, Saunders R, et al. Effects of radiofrequency electromagnetic fields on the human nervous system. J Toxicol Environ Health B Crit Rev. 2009;12(8):572–597. doi: 10.1080/10937400903458940. [DOI] [PubMed] [Google Scholar]
- 11.Thomas S, Heinrich S, von Kries R, Radon K. Exposure to radio-frequency electromagnetic fields and behavioural problems in Bavarian children and adolescents. Eur J Epidemiol. 2010;25(2):135–141. doi: 10.1007/s10654-009-9408-x. [DOI] [PubMed] [Google Scholar]
- 12.Divan HA, Kheifets L, Obel C, Olsen J. Prenatal and postnatal exposure to cell phone use and behavioral problems in children. Epidemiology. 2008;19(4):523–529. doi: 10.1097/EDE.0b013e318175dd47. [DOI] [PubMed] [Google Scholar]
- 13.Divan HA, Kheifets L, Obel C, Olsen J. Cell phone use and behavioural problems in young children. Journal of Epidemiology and Community Health. 2012;66(6):524–529. doi: 10.1136/jech.2010.115402. [DOI] [PubMed] [Google Scholar]
- 14.Schuz J, Waldemar G, Olsen JH, Johansen C. Risks for central nervous system diseases among mobile phone subscribers: a Danish retrospective cohort study. PLoS One. 2009;4(2):e4389. doi: 10.1371/journal.pone.0004389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehra S, Eavey RD, Keamy DG., Jr The epidemiology of hearing impairment in the United States: newborns, children, and adolescents. Otolaryngol Head Neck Surg. 2009;140(4):461–472. doi: 10.1016/j.otohns.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 16.Ozturan O, Erdem T, Miman MC, Kalcioglu MT, Oncel S. Effects of the electromagnetic field of mobile telephones on hearing. Acta Otolaryngol. 2002;122(3):289–293. doi: 10.1080/000164802753648178. [DOI] [PubMed] [Google Scholar]
- 17.Uloziene I, Uloza V, Gradauskiene E, Saferis V. Assessment of potential effects of the electromagnetic fields of mobile phones on hearing. BMC Public Health. 2005;5:39. doi: 10.1186/1471-2458-5-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parazzini M, Brazzale AR, Paglialonga A, Tognola G, Collet L, Moulin A, et al. Effects of GSM cellular phones on human hearing: the European project "GUARD". Radiation Research. 2007;168(5):608–613. doi: 10.1667/RR1020.1. [DOI] [PubMed] [Google Scholar]
- 19.Parazzini M, Sibella F, Lutman ME, Mishra S, Moulin A, Sliwinska-Kowalska M, et al. Effects of UMTS cellular phones on human hearing: results of the European project EMFnEAR. Radiation Research. 2009;172(2):244–251. doi: 10.1667/RR1679.1. [DOI] [PubMed] [Google Scholar]
- 20.Parazzini M, Bell S, Thuroczy G, Molnar F, Tognola G, Lutman ME, et al. Influence on the mechanisms of generation of distortion product otoacoustic emissions of mobile phone exposure. Hear Res. 2005;208(1–2):68–78. doi: 10.1016/j.heares.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 21.Hutter HP, Moshammer H, Wallner P, Cartellieri M, Denk-Linnert DM, Katzinger M, et al. Tinnitus and mobile phone use. Occup Environ Med. 2010;67(12):804–808. doi: 10.1136/oem.2009.048116. [DOI] [PubMed] [Google Scholar]
- 22.Oktay MF, Dasdag S. Effects of intensive and moderate cellular phone use on hearing function. Electromagn Biol Med. 2006;25(1):13–21. doi: 10.1080/15368370600572938. [DOI] [PubMed] [Google Scholar]
- 23.Davidson HC, Lutman ME. Survey of mobile phone use and their chronic effects on the hearing of a student population. Int J Audiol. 2007;46(3):113–118. doi: 10.1080/14992020600690472. [DOI] [PubMed] [Google Scholar]
- 24.García Callejo FJ, García Callejo F, Peña Santamaría J, Alonso Castañeira I, Sebastián Gil E, Marco Algarra J. Hearing level and intensive use of mobile phones. Acta Otorrinolaringol Esp. 2005;56:187–191. doi: 10.1016/s0001-6519(05)78598-8. [DOI] [PubMed] [Google Scholar]
- 25.Olsen J, Melbye M, Olsen SF, Sorensen TI, Aaby P, Andersen AM, et al. The Danish National Birth Cohort--its background, structure and aim. Scand J Public Health. 2001;29(4):300–307. doi: 10.1177/14034948010290040201. [DOI] [PubMed] [Google Scholar]
- 26.Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550–560. doi: 10.1097/00001648-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Bang H, Robins JM. Doubly robust estimation in missing data and causal inference models. Biometrics. 2005;61(4):962–973. doi: 10.1111/j.1541-0420.2005.00377.x. [DOI] [PubMed] [Google Scholar]
- 28.van der Laan M, Robbins J. Unified Methods for Censored Longitudinal Data and Causality. New York: Springer Verlag; 2003. [Google Scholar]
- 29.Lash TL, Fox CS, Fink AK. Applying Quantitative Bias Analysis to Epidemiologic Data. New York: Springer; 2009. [Google Scholar]
- 30.American Speech-Language-Hearing Association. [Accessed January 2013];Causes of Hearing Loss in Children. http://www.asha.org/public/hearing/disorders/causes.htm#congenital.
- 31.Khairi Md Daud M, Noor RM, Rahman NA, Sidek DS, Mohamad A. The effect of mild hearing loss on academic performance in primary school children. Int J Pediatr Otorhinolaryngol. 2010;74(1):67–70. doi: 10.1016/j.ijporl.2009.10.013. [DOI] [PubMed] [Google Scholar]
- 32.Tharpe AM, Bess FH. Minimal, progressive, and fluctuating hearing losses in children. Characteristics, identification, and management. Pediatr Clin North Am. 1999;46(1):65–78. doi: 10.1016/s0031-3955(05)70081-x. [DOI] [PubMed] [Google Scholar]
- 33.Greene N, Greenland S, Olsen J, Nohr EA. Estimating bias from loss to follow-up in the Danish National Birth Cohort. Epidemiology. 2011;22(6):815–822. doi: 10.1097/EDE.0b013e31822939fd. [DOI] [PubMed] [Google Scholar]
- 34.Mezei G, Benyi M, Muller A. Mobile phone ownership and use among school children in three Hungarian cities. Bioelectromagnetics. 2007;28(4):309–315. doi: 10.1002/bem.20270. [DOI] [PubMed] [Google Scholar]
- 35.Koivusilta LK, Lintonen TP, Rimpela AH. Orientations in adolescent use of information and communication technology: a digital divide by sociodemographic background, educational career, and health. Scand J Public Health. 2007;35(1):95–103. doi: 10.1080/14034940600868721. [DOI] [PubMed] [Google Scholar]
- 36.Bohler E, Schuz J. Cellular telephone use among primary school children in Germany. Eur J Epidemiol. 2004;19(11):1043–1050. doi: 10.1007/s10654-004-2174-x. [DOI] [PubMed] [Google Scholar]
- 37.Soderqvist F, Hardell L, Carlberg M, Hansson Mild K. Ownership and use of wireless telephones: a population-based study of Swedish children aged 7–14 years. BMC Public Health. 2007;7:105. doi: 10.1186/1471-2458-7-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thomas S, Heinrich S, Kuhnlein A, Radon K. The association between socioeconomic status and exposure to mobile telecommunication networks in children and adolescents. Bioelectromagnetics. 2010;31(1):20–27. doi: 10.1002/bem.20522. [DOI] [PubMed] [Google Scholar]
- 39.Lenhart A. Teens, Cell Phones and Texting: Text Messaging Becomes Centerpiece Communication. Washington, DC: Pew Research Center; 2010. [Google Scholar]
- 40.Child Research Net. [Accessed January 2013];Children and Mobile Phone Use. 2005 http://www.childresearch.net/data/school/2005_05.html.