Abstract
This study evaluated the effectiveness of 3 approaches to transferring cognitive behavioral therapy (CBT) to addiction clinicians in the Republic of South Africa (RSA). Clinicians (N = 143) were assigned to 3 training conditions: (1) An in vivo (IV) approach in which clinicians received in-person training and coaching; (2) A distance learning (DL) approach providing training via video conference and coaching through teleconferencing; and (3) A control condition (C) providing a manual and 2-hour orientation. Frequency of use of CBT skills increased significantly with the IV and DL approaches compared to the C approach, and the IV approach facilitated greater use of CBT skills than the DL approach. During the active phase of the study, skill quality declined significantly for clinicians trained in the C condition, whereas those in the DL approach maintained skill quality and those in the IV approach improved skill quality. After coaching was discontinued, clinicians in the IV and DL approaches declined in skill quality. However, those in the IV approach maintained a higher level of skill quality compared to the other approaches. Cost of the IV condition was double that of the DL condition and 10 times greater than the C condition.
Keywords: Dissemination, Implementation, Addiction, Cognitive Behavioral Therapy, South Africa
Introduction
Cognitive behavioral therapy (CBT) has been empirically established as an efficacious treatment method for stimulant use disorders in controlled research trials [1-4]. However, it is not yet clear how to disseminate and implement CBT or other EBPs in routine practice settings in ways that ensure application fidelity. Further, if dissemination/implementation methodologies are costly, the use of CBT and other EBPs will be limited, especially in geographic areas with limited resources.
Fixsen et al. [5] cite a crucial need to improve the effectiveness of dissemination and implementation efforts to and among addiction specialists. Among the “core elements” of effective dissemination and implementation of EBPs is the training and coaching of treatment providers. As noted by Fixsen and colleagues [6]:
“Training and coaching are the principal ways in which behavior change is brought about for carefully selected staff in the beginning stages of implementation and throughout the life of evidence-based practices and programs.”
The past decade has seen increased efforts to successfully disseminate EBPs for treating substance use disorders, including work on the dissemination of such EBPs as CBT [7-9], Motivational Enhancement Therapy [10], Motivational Interviewing [11,12], and Multi-Systemic Therapy [13]. Much of the research on the dissemination and implementation of evidence-based addiction treatments has been conducted in the United States, whereas dissemination and implementation of evidence-based treatment approaches to professionals in other countries remains largely unstudied.
In the present report, we describe the evaluation of three methods for transferring CBT to clinicians in the Republic of South Africa (RSA), which has the world’s highest prevalence of people living with HIV (5.7 million) [14]. Research [15,16] has documented that stimulant use plays a role in HIV transmission by increasing risky behaviors, such as sex with multiple partners and unprotected sex. We chose South Africa as the site for this study because the sound implementation of CBT can potentially provide RSA clinicians with an effective approach for treating the large population of stimulant users (cocaine and methamphetamine), as well as making a potential contribution to national HIV prevention efforts [4,17].
The purpose of the present study was to implement and evaluate the efficacy of three dissemination and implementation approaches for a specific CBT protocol for the treatment of drug dependence to community treatment providers in the RSA. Distance education approaches have the potential to reduce costs by bringing the training (via the Internet or video conferencing) to the clinicians in an inexpensive manner rather than incurring the travel and related costs of bringing clinicians to a central training location or dispersing trainers to scattered clinics [18,19]. In the present study, we randomly assigned 24 substance abuse treatment clinics and their associated clinicians to receive one of three CBT dissemination/implementation conditions: (1) an In Vivo (IV) condition; (2) a Distance Learning (DL) condition; or (3) a Control (C) condition. The hypotheses were that the two active conditions would provide better dissemination and implementation of CBT techniques and that the DL condition would cost less than the IV training.
Method
Study Design
The 5-year study compared the efficacy and efficiency of three methods of disseminating and implementing a 12-session CBT protocol for the treatment of drug dependence to RSA clinician/counselors in selected community treatment centers. Training conditions included: (1) An In-Vivo (IV) approach consisting of a 3-day, in-person dissemination conference in which clinicians from the randomly selected RSA treatment centers travelled to a central training site for didactic training and role-playing of CBT methods, followed by six biweekly, in-person 90-minute coaching (implementation) sessions, in which a clinical supervisor traveled to the selected clinics; (2) A Distance Learning (DL) approach, in which clinicians received the same 3-day dissemination session over a televised, interactive instructional platform and received the same six biweekly 90-minute coaching sessions via telephone conference call; and (3) A Control (C) condition, in which no dissemination or coaching activities were provided, but a CBT manual was provided to clinicians along with a 2-hour orientation to the manual and guidelines for its use. The primary dependent measure was the extent to which the three approaches affected clinicians’ CBT practices by assessing selected audiotaped clinical sessions. All study activities were conducted under the approval and review of the Human Subjects committees of Friends Research Institute, Inc., and the University of Limpopo Medical University of South Africa (MEDUNSA).
Currently practicing addiction clinicians were recruited into the study via an outreach campaign to licensed treatment centers in the RSA by the South African co-principal investigator (S. R.). Licensed clinicians (i.e., mental health nurse professionals, social workers, psychologists; N = 143) who worked in 24 addiction treatment centers in the RSA were the study participants. The clinicians were randomly assigned to one of the three training conditions by treatment center (i.e., all clinicians in a treatment center with a minimum of 3 clinicians per center were randomized to the same training condition [8 treatment centers per condition]). Data were collected at baseline on clinician knowledge and attitudes about CBT and an audiotaped session for each clinician was scored to determine the quantity and quality of CBT skills applied. Patients whose clinical sessions were audiotaped signed consent for taping, although no identifying information was obtained from patients.
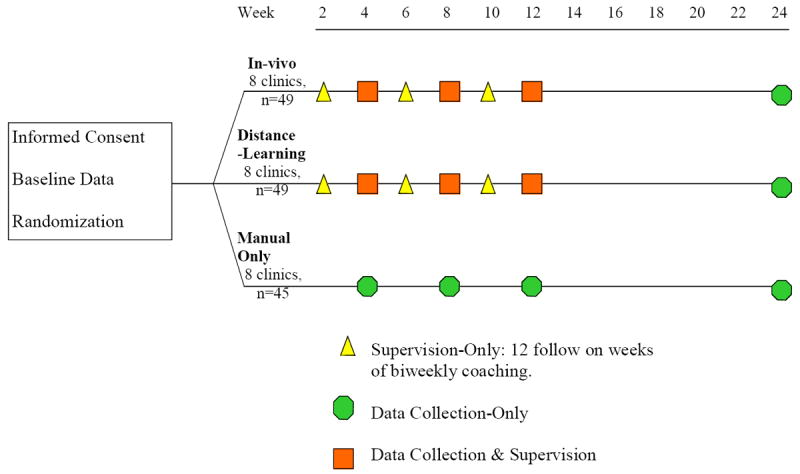
The study had two phases: dissemination-implementation and sustainability. We defined the dissemination-implementation phase of the study as from baseline through week 12 of the study, including the 3-day training period (dissemination) and the subsequent 12 weeks of biweekly coaching (implementation). During the 12-week period, each clinician treated a minimum of 3 stimulant-using clients employing the 12-session CBT protocol. Audiotaped sessions were collected from clinicians at weeks 0 (pre-dissemination session), and 4, 8, and 12 (implementation phase). We defined the sustainability phase as the period from week 13 to week 24. Data (including an audiotaped session) were collected at 24 weeks after baseline to assess sustained use of CBT techniques after discontinuation of the supervision/coaching activity. The study design is illustrated in Figure 1.
Figure 1. Study Design.
The three study conditions were compared with regard to the relative changes in CBT-related knowledge and skills (quantity and quality of CBT techniques employed, as rated by audiotaped sessions with clients). To compare the relative costs of the three study conditions, the cost of each approach was calculated over the course of the project.
Dissemination/Implementation Procedures
The 3-day IV training sessions were conducted at a conference center or community training facility located in a community central to the clinical staff cohort being trained. All IV group participants attended the 3-day session, with many requiring hotel accommodations. The DL condition broadcasts were from a hired video-conference facility or from Department of Health video conference facilities. Participants viewed and participated in the sessions at a local video conference center. It was not possible to deliver the videoconference sessions to the treatment centers due to bandwidth limitations. The technology for all DL group sessions allowed for live audio/video presentations by the master trainer and interactive audio/video feedback with the trainees.
After the initial 3-day training, clinicians began the 12-week period of implementation and coaching. During this 12-week period, clinicians practiced newly learned CBT skills during clinical sessions with three of their patients, guided by the 12-session CBT manual.
Clinicians assigned to the IV approach received six biweekly, 90-minute group coaching sessions conducted at each of the IV treatment center sites. During the sessions, the master trainer reviewed the CBT skills used during the previous 2 weeks of clinical sessions and the skills that were planned for use during the subsequent 2 weeks. Participants were asked to demonstrate how skills had been and would be implemented and were given feedback on skill development. Role plays were used and all coaching sessions were conducted by the Master trainer. Sessions employed a positive reinforcement approach, in which participants received praise for accomplishment and non-judgmental suggestions for ways to improve skill delivery.
Participants in the DL condition also received six biweekly, 90-minute group coaching sessions delivered via a telephone conference call. The master trainer called each DL site for the six scheduled conference calls. The same material was discussed as in the IV condition and the same type of coaching approach was used. However, because there was no video capability for these coaching sessions, the master trainer was not able to see the participants as they demonstrated their CBT skills. The original protocol included providing DL coaching via video conferencing in each of the DL sites. However, there was inadequate bandwidth at the time (2005) in many sites to accommodate video conferencing requirements. This is an important issue that may have affected outcomes and will be discussed below.
In the C condition, the project director visited each treatment center and spent 2 hours per site with the staff participants and the director and/or clinical supervisor in a group orientation session to review the CBT manual. The clinician was instructed to conduct sessions as directed in the manual and to work with the site director/clinical supervisor to deliver the 12 sessions of treatment to clients. After the study was completed, clinicians randomized to the C condition were offered further in-person CBT training.
Sites and Staff Participants
One hundred forty-three clinicians were recruited from 24 treatment centers (8 per condition) in five provinces of the RSA. Centers were selected for inclusion based on voluntary participation by the director and staff and if they had a minimum of three clinician volunteers. Randomization was done by treatment center, so that all clinicians in a selected site were assigned to the same condition and received the same training. The inclusion criteria were that clinicians had to be willing to be randomly assigned to either the IV, DL, or C conditions, participate in 3-day training sessions and six biweekly coaching sessions (for the IV and DL conditions), and have their sessions audiotaped with three patients for review over the duration of the protocol. Randomization of sites occurred in five waves, or cohorts, during the course of the study. An urn randomization procedure was used by the UCLA Data Management Center to assign sites to conditions, balancing assignment in terms of size of the facility (large vs. small) and ethnic make-up of the clinician population (White vs. non-White ratio).
Study Assessments
Domains assessed for all clinicians at baseline included:
Clinician Assessment
We examined clinician characteristics likely to be associated with the acquisition of skills under the various conditions. Domains assessed before protocol initiation included demographics (clinician gender, age, race) and history of training and experience (years of experience in substance abuse, years at current site, education/degree, certification status, and primary therapeutic orientation).
CBT Knowledge Questionnaire
Knowledge of CBT was assessed with a 28-item multiple-choice questionnaire, developed by the CBT manual/YACS adaptation team, at baseline and at the end of the 12-week intervention. Domains assessed for all clinicians at weeks 0, 4, 8, and 12 included:
Retention
Retention was measured by the number of time points that the staff participants submitted their audiotape.
CBT Skills
Skill of CBT implementation was measured by assessment of audiotapes of therapy sessions at each time point (weeks 0, 4, 8, and 12), using the Yale Adherence and Competence Scale (YACS). All domains were also assessed at 24 weeks to measure CBT skill retention. Costs for delivering the three study conditions were also calculated and compared as described in the Results.
Primary Dependent Measure: The Yale Adherence and Competence Scale
The Yale Adherence and Competence Scale (YACS) [7,20] is a 55-item scale that assesses general (clinician interventions or behaviors common to most therapies) and unique (interventions specific to a given therapy such as CBT) elements of behavioral treatments for drug use disorders.
The YACS focuses exclusively on the clinicians’, not the patient’s, behavior. All YACS items used a common 7-point Likert scale format (ranging from 1 to 7). For each item, there were two rating dimensions: The first dimension is an extensiveness/adherence rating that assessed the degree to which the intervention was present in the session (e.g., whether it occurred and with what frequency). The second is a competence/skillfulness rating that indicates the skill level of the clinician in delivering the intervention (and is rated only if the intervention occurred within the session rated).
Data Collection Procedures
The project director collected all questionnaire data from the participants at weeks 0, 4, 8, 12, and 24. Data were sent via a commercial courier (i.e., FedEx) to the UCLA ISAP Data Management Center. At weeks 0, 4, 8, 12, and 24, participants audiotaped one clinical session with each of three stimulant-abusing clients (with written client consent). One of the audiotaped sessions was randomly selected by the project director, identified with a staff participant code number, and mailed to the Friends Research Institute in California, where they were scored using the YACS by raters blind to participant training condition. Raters were trained in a didactic seminar that included detailed review of the YACS rating manual as well as several group practice ratings using taped examples. Rater trainees rated practice tapes, which were compared to consensus ratings of these tapes by three clinical experts on CBT. Raters were certified only after their ratings achieved acceptable reliability, which was defined as achieving an intraclass correlation coefficient of .70 or greater for the CBT items compared to expert consensus ratings.
General Data Analysis Strategy
Power Analysis
A power analysis was used to determine adequate sample size for the trial. For primary outcomes, clinicians were the intended unit of analysis, corresponding to a sample size of n = 150 (n = 50 per condition). For 5 period repeated measures, n = 50 was determined an adequate sample size per condition to allow detection of medium effects when testing for group differences over time (i.e., main effects of group), with or without attrition, assuming a correlation of approximately .2 over time, with power = .80 and alpha = .05.
Randomization
The urn randomization procedure [21] was employed, a procedure that distributes variables that may affect outcomes equally across conditions and sites. Primary analyses were based on an intent-to-treat design, i.e., they included the entire sample of clinician participants who provided signed informed consent and received randomization to training condition, whether or not they dropped out.
Retention
Mean weeks retained in the study were compared across groups using an ANOVA. Efforts were made to retain participants until the completion of all of their audiotaped sessions at week 24. Participants who terminated early were not replaced.
CBT Knowledge Assessment
This assessment was designed by the US and RSA CBT experts to measure the extent to which individuals could identify key constructs in CBT. Differential group changes in CBT knowledge scores from baseline to post implementation were compared using a one-way ANOVA. In our study sample, Cronbach’s alpha for this knowledge assessment was .56, indicating adequate reliability.
Analysis of CBT Skills
A generalized linear model was used for evaluating differences across conditions in skill changes over time. The overall model included condition (IV, DL, and C) as a between-group factor, five observations over time (weeks 0, 4, 8, 12, and 24) as a within-subjects factor, and ethnicity as a covariate. Models were estimated separately for extensiveness/adherence scores and competence/skillfulness scores. This approach maximized the use of available data, since some cases were missing one or more observations across the study time period. During the dissemination-implementation phase, we tested contrasts to examine specific differences between the control (group C) condition and the combined experimental conditions (IV plus DL) and also the difference between the two experimental training conditions (IV vs. DL). We first examined an early acquisition measure (week 0 vs. week 4), and then an implementation measure (week-8 and week-12 measures), and a sustainability measure (week 12 vs. week 24).
Results
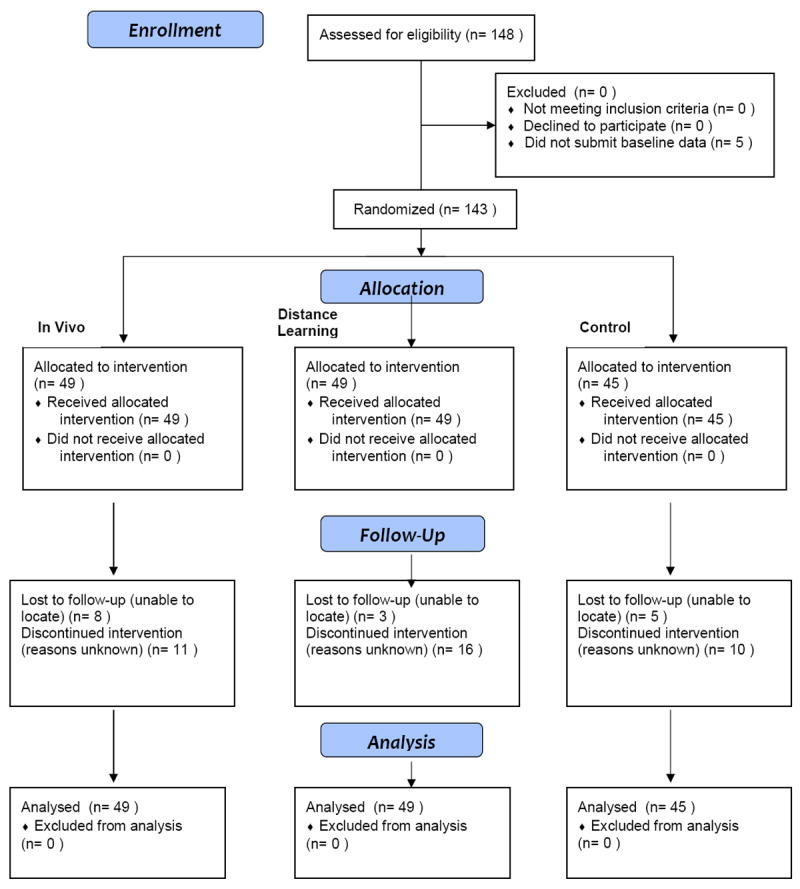
A total of 148 individuals from 24 clinics initially consented to participate in the study, but 5 failed to provide baseline data and subsequently did not participate in the training protocol, resulting in a final study sample of 143 clinicians (97%; In-Vivo = 49, Distance Learning = 49, Control = 45), of which 62.9% completed the entire 24 weeks. Figure 2 displays a CONSORT Flow Diagram that shows the number of individuals at recruitment, allocation to condition, follow-up, and analysis.
Figure 2. CONSORT Flow Diagram.
Participant Characteristics
Seventy-five percent of the RSA clinicians were female, with an average age of 38.1 years (SD = 11.8). They were ethnically diverse, with 36.4% identifying themselves as White, 30.8% as Black, 18.9% as Colored (mixed race), 12.6% as Indian or Asian, and 1.4% as Cape Malay. Participants’ average number of years of education was 16.5 (SD = 3.1), and their average number of years’ experience as a clinician was 7.3 (SD = 7.8). The majority (62.3%) held at least an equivalent of a bachelor’s degree, and just under half (49%) were registered social workers.
No statistically significant training condition differences were found for demographic variables of age, F (2,140) = 1.19, p = .31, or gender, χ2(2, N = 142) = 3.27, p = .20. Further, there were no significant group differences in baseline measures of competence, F (2,118) = 1.51, p = .23, adherence, F (2,80) = .88, p = .42, or CBT knowledge, F (2,90) = 1.30, p = .28.
Participant retention in the trial
A repeated-measures ANOVA was used to compare retention of clinicians over time. Time (weeks 0, 4, 8, 12, 24) served as the within-subjects factor, and group (IV, DL, and C conditions) as the between-subjects factor. There was no difference in retention rate by condition, Wilks’ Λ = .97, F (8, 274) = .62, p = .76, η2 = .02. Overall, retention of participants in the study fell from 98.6% at baseline (week 0) to 83.9% at week 4, 77.6% at week 8, 74.1% at week 12, and 62.9% at week 24. There was no replacement of participants who dropped out of the study. Reasons for study discontinuation were primarily due to employment changes or reassignment of therapists to different patient populations. There are no national data in South Africa on the rate of therapist employment turnover; thus, we cannot assess if this study cohort was more or less stable than therapists across the national substance use disorder treatment system. It has been documented in the United States that personnel in the U.S. treatment system have high rates of employment turnover (53% turnover in a 12-month period) [22].
CBT Knowledge
A one-way repeated measures ANOVA was used to compare gain in CBT knowledge from baseline to week 12 between groups. Possible knowledge scores ranged from 0 to 28, and change scores were created by subtracting the baseline score from the week-12 score. The average change in score for all staff clinicians was an increase of 3.8. A significant difference in change scores was found between groups, F (2,90) = 3.73, p = .028. Follow-up Sidak-corrected post-hoc analyses revealed that the IV condition, M = 5.38, SD = 4.31, had a greater gain in CBT knowledge over the course of the study (p = .03) compared to the C condition, M = 2.69, SD = 2.89. Although at an intermediate level, the DL condition, M = 3.29, SD = 4.17, did not significantly differ from either of the other conditions.
CBT Skills
Extensiveness/adherence
Figure 3 shows the scores for this domain (frequency of use of CBT skills) over the study. The overall condition-by-time interaction was significant, LR χ2 = 35.99, df = 8, p < .001, indicating differences among conditions in patterns of scores over the study period, with the DL and IV groups significantly differing from the C group. Participants in the C group exhibited poorer early acquisition of CBT skills (week 0–week 4) than did the combined training groups, LR χ2 = 16.43, df = 1, p < .001; the DL and IV groups did not differ significantly from each other.
Figure 3. Extensiveness/Adherence Scores by Condition.
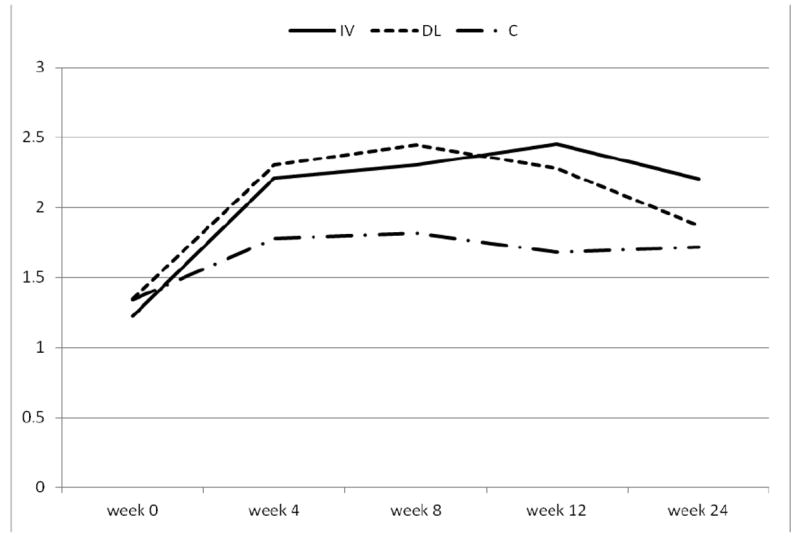
Extensiveness/Adherence ratings are on a 7-point Likert scale: 1=not at all, 2=a little(once), 3=infrequently(twice), 4=somewhat(3-4 times), 5=quite a bit(5-6 times), 6=considerably(>6 times/more in-depth), 7=extensively(high frequency/characterizes entire session).
*Please note, time point at week 24 is not equidistant with other time points and not accurately scaled in this figure.
From week 4 through 12, each of the three groups exhibited relatively flat patterns, with no significant linear or quadratic time trends over this period. However, the C group participants had significantly lower extensiveness/adherence scores than the combined IV and DL training groups, LR χ2 = 28.68, df = 1, p < .001, whereas these latter two groups did not differ significantly from each other during this study phase.
At week 24, there was a significant difference in the degree of decline in scores between the C group and the combined DL and IV groups, LR χ2 = 5.44, df = 1, p = .02. The DL and IV groups declined to a greater extent than the C group, but did not differ significantly from each other. However, the IV group participants demonstrated an absolute higher level of CBT extensiveness/adherence across the entire study period than did the DL group, LR χ2 = 5.47, df = 1, p = .02, and these two groups (DL+IV) combined maintained higher levels than the C group across the study period, LR χ2 = 21.06, df = 1, p < .001.
Competence/Skillfulness
Scores for the quality of the CBT skills are plotted over the five data collection time points in Figure 4.
Figure 4. Competence/Skill Scores by Group.
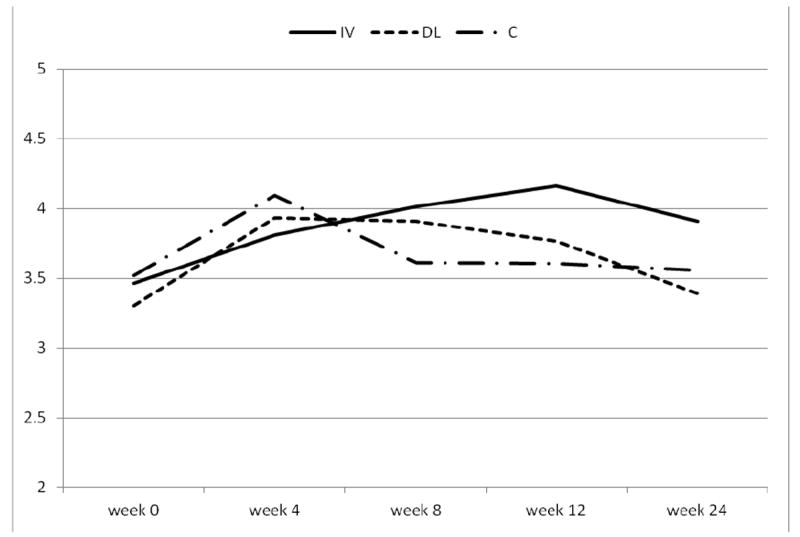
Competence/Skill ratings are on a 7-point Likert scale: 1=very poor, 2=poor, 3=acceptable, 4-adequate, 5=good, 6=very good, 7=excellent. Mean competence ratings are made only when an item occurs within a session.
*Please note, time point at week 24 is not equidistant with other time points and not accurately scaled in this figure.
The overall condition-by-time (5 observations) interaction was significant (likelihood ratio [LR] χ2 = 24.08, df = 8, p = .002), indicating differences among conditions in skills across the study period. No significant differences in the competence/skillfulness score changes from baseline to 4 weeks were detected between the C and the combined DL+IV groups or between the DL and IV groups. All groups improved significantly in this domain (effect of time on average score across three groups, LR χ2 = 25.79, df = 1, p < .001). However, during the week-4 to week-12 period, the C group showed a declining linear trend over time compared to the combined DL+IV groups (LR χ2 = 8.00, df = 1, p = .005). The linear trend also differed between the DL and IV groups (LR χ2 = 7.81, df = 1, p = .005); specifically, the DL group showed little change in competence/skillfulness scores over this period (linear trend was not significant for this group), whereas the IV group showed an increased skills score (LR χ2 = 8.84, df = 1, p = .003).
Results at week 24 showed an overall general decline in scores for all groups, (LR χ2 = 7.09, df = 1, p = .008) compared to week 12. The degree of decline from week 12 to week 24 did not differ significantly between the C and combined DL+IV groups or between the DL and IV groups. The IV group did have a higher skill level at week 24 than did the DL group, (LR χ2 = 12.23, df = 1, p < .001) and the C group (LR χ2 = 9.87, df = 1, p = .002).
Cost Comparison
The comparison of the costs of the three training/coaching approaches was conducted by recording all expenses that were specific to the delivery of each of the three CBT training conditions. These expenses included materials costs, travel costs (hotel and mileage/airfare) for the master trainer to visit the IV sites, personnel costs (portion of master trainer salary needed to deliver training/supervision for IV and DL conditions), and costs of the videoconferencing service. Because it was not possible to calculate these costs on each staff participant individually, we tabulated the total costs that were involved in the delivery of each condition across all the participants within a specific training condition. This approach precludes a statistical examination, since it results in a single aggregate total for each of the three conditions. However, the magnitude of the difference in cost between the three conditions allows meaningful inferences to be made about the relative costs of the three approaches. Using the financial records from the project to document costs, the costs of the combined dissemination/implementation activities of the three conditions are illustrated in Table 1. Based on these data, the cost of the IV condition was $1,485 per participant, the DL condition was $768 per participant, and the cost for the C condition was $145 per participant.
Table 1.
Total cost and cost per participant of the three study conditions: control, in vivo, and distance learning.
| Total Cost | Cost per Participant | |
|---|---|---|
| Control Condition | $6,522 | $145 |
| Distance Learning Condition | $37,648 | $768 |
| In Vivo Condition | $72,791 | $1,485 |
Discussion
Using a randomized clinical trial, this study assessed the relative effectiveness and cost of different approaches to disseminating and implementing cognitive behavioral therapy knowledge and skills to addiction treatment clinicians in the Republic of South Africa.
The two active conditions (IV and DL) appear to have produced very similar increases in the early acquisition of CBT skill delivery. However, the in-person coaching sessions resulted in continued increases in the frequency of use of CBT compared to the telephone conference-call coaching sessions used in the DL condition. Further, the IV condition resulted in an overall higher frequency of CBT application across the study period than was produced by the DL condition. However, as the combined IV-DL condition produced higher levels of CBT skill implementation than the C condition across the study period, it is clear that, overall, an active training-coaching approach is superior to the manual-only condition. The fact that the frequency of CBT tool application decreased over the last 12 weeks, when coaching was withdrawn, suggests that an ongoing program of supervision/coaching is required for CBT to be used at a high frequency.
After week 4, the CBT skills of the C group showed deterioration compared to the two active training conditions. Further, the IV condition appeared to result in a greater improvement in CBT skills than the DL approach. When the coaching was discontinued for the DL and IV group participants, their skill level declined. However, the IV condition continued to deliver the CBT in a more skillful way as compared to the DL and C groups.
The cost data are straightforward. Providing clinicians with a CBT treatment manual and a brief 2-hour orientation is a very inexpensive way to deliver information on the use of CBT for the treatment of stimulant dependence, costing approximately $145 per clinician being trained. The distance learning approach increased the cost fivefold, and the cost of the in vivo condition was 10 times greater than the C condition and double the DL condition.
Study Implications and Limitations
Implications
This study produced new information on the dissemination and implementation of research-supported drug treatment protocols. The study findings suggest that:
CBT knowledge can be somewhat increased by providing clinicians with a manual and brief orientation; however, participation in a program of training and coaching produces significantly better knowledge acquisition and more extensive use of skills.
The frequency with which CBT skills will be used in treatment sessions can be substantially increased by the manner in which coaching is provided. In vivo coaching appears to be a superior method of promoting increased frequency of CBT delivery compared to coaching over the telephone.
Had it been technically possible to deliver the coaching via videoconference as originally planned, the distance-learning coaching might have produced an effect far more comparable to the in vivo condition.
Quality of CBT skills can be improved by exposure to the CBT training materials in any of the three formats used for dissemination. However, for the quality of CBT skills to significantly improve, an effective method of coaching is critical.
To effectively transfer CBT into the repertoire of a clinician, a coaching period of more than 12 weeks is required, and it is likely that ongoing clinical supervision is an essential component in the effective implementation of CBT and other evidence-based psychosocial treatment approaches.
The costs of the in vivo method of CBT training could be prohibitive and preclude the widespread transfer of CBT. In contrast, providing a manual and a brief orientation, although inexpensive, did not appear to produce a substantial amount of CBT implementation. The distance learning approach appears to have substantial potential in terms of transferring CBT knowledge and skills at a reasonable cost, and with improved inexpensive videoconferencing capabilities, there appears to be great promise with this approach.
Limitations
The treatment centers and the clinicians involved in the study were not selected to be a representative sample of service providers in the Republic of South Africa, which limits the generalizability of the findings. There was a substantially high drop-out rate of therapists for the study. However, since there is evidence that the turnover rate among therapists/counselors (in the United States) is quite high [22], it is unclear if this rate of study drop-out is an aberration or if it is consistent with the normal employment turnover of this profession. There was no attempt to determine if the approaches changed patient treatment outcomes. The technologies used to deliver the distance learning approach employed strategies available in 2004–2008. It is likely that with current technology, the distance learning approach could be delivered at a lower cost and with coaching that includes video feedback.
Acknowledgments
The authors acknowledge Donnie W. Watson, Ph.D., for his leadership and many contributions to this project. We thank Shamim Garda of the SANCA treatment organization, Johannesburg, Republic of South Africa (RSA); Charles Parry, Ph.D., with the Medical Research Council, Cape Town, Western Cape, RSA; Steve Martino, Ph.D., with Yale University, New Haven, Connecticut; Felipe Castro, Ph.D., Arizona State University, Phoenix, Arizona; and Frank Vocci, Ph.D., Friends Research Institute, Inc., Baltimore, Maryland. We particularly express gratitude to and admiration for the clinicians who participated in the study. Their dedication and commitment to helping those with substance use disorders in the RSA is a major contribution to the public health of the citizens of the RSA.
The project was supported by NIDA Grant R01 DA019063 to Donnie Watson, PI, and Richard Rawson, Co-PI. Dr. Fox was supported by NIDA Training Grant 5T32 DA07272-18 to Richard Rawson (PI). Dr. Richard Rawson is a consultant for Catalyst Pharma.
References
- 1.Carroll KM. Therapy Manual for Drug Addiction Series. A Cognitive Behavioral Approach Treating Cocaine Addiction. Rockville, MD: National Institute on Drug Abuse; 1998. National Institutes of Health Publication No 98-4308. [Google Scholar]
- 2.Carroll KM, Rawson RA. Relapse prevention approaches for stimulant dependent individuals. In: Marlatt GA, Donovan D, editors. Relapse Prevention Approaches for the Treatment of Substance Use Disorders. New York: Guilford; 2005. pp. 130–150. [Google Scholar]
- 3.Rawson RA, Huber A, Brethen P, Obert J, Gulati V, Shoptaw S, et al. Status of methamphetamine users 2-5 years after outpatient treatment. J Addict Dis. 2002;21:107–19. doi: 10.1300/j069v21n01_09. [DOI] [PubMed] [Google Scholar]
- 4.Woody GE, Gallop R, Luborsky L, Blaine J, Frank A, Salloum IM, et al. HIV risk reduction in the National Institute on Drug Abuse Cocaine Collaborative Treatment Study. J Acquir Immune Defic Syndr. 2003;33:82–87. doi: 10.1097/00126334-200305010-00012. [DOI] [PubMed] [Google Scholar]
- 5.Fixsen DL, Naoom SF, Blasé KA, Friedman RM, Wallace F. Implementation Research: A Synthesis of the Literature. Tampa, FL: University of South Florida, Louis de la Parte Florida Mental Health Institute; 2005. The National Implementation Research Network (FMHI Publication #231) [Google Scholar]
- 6.Fixsen DL, Blasé KA, Naoom SF, Wallace F. Core implementation components. Res Soc Work Pract. 2009;19:531–40. [Google Scholar]
- 7.Carroll KM, Nich C, Sifry RL, Nuro KF, Frankforter TL, Ball SA, et al. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug Alcohol Depend. 2000;57:225–238. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- 8.Morgenstern J, Morgan TJ, McCrady BS, Keller DS, Carroll KM. Manual-guided cognitive-behavioral therapy training: a promising method for disseminating empirically supported substance abuse treatments to the practice community. Psychol Addict Behav. 2001;15:83–88. [PubMed] [Google Scholar]
- 9.Sholomskas DE, Syracuse-Siewert G, Rounsaville BJ, Ball SA, Nuro KF, Carroll KM. We don’t train in vain: a dissemination trial of three strategies of training clinicians in cognitive-behavioral therapy. J Consult Clin Psychol. 2005;73:106–115. doi: 10.1037/0022-006X.73.1.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martino S, Ball SA, Nich C, Frankforter TL, Carroll KM. Community program therapist adherence and competence in motivational enhancement therapy. Drug Alcohol Depend. 2008;96:37–48. doi: 10.1016/j.drugalcdep.2008.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller WR, Yahne CE, Moyers TB, Martinez J, Pirritano M. A randomized trial of methods to help clinicians learn motivational interviewing. J Consult Clin Psychol. 2004;72:1050–1062. doi: 10.1037/0022-006X.72.6.1050. [DOI] [PubMed] [Google Scholar]
- 12.Shafer MS, Rhode R, Chong J. Using distance education to promote the transfer of motivational interviewing skills among behavioral health professionals. J Subst Abuse Treat. 2004;26:141–148. doi: 10.1016/S0740-5472(03)00167-3. [DOI] [PubMed] [Google Scholar]
- 13.Schoenwald SK, Sheidow AJ, Chapman JE. Clinical supervision in treatment transport: effects on adherence and outcomes. J Consult Clin Psychol. 2009;77:410–421. doi: 10.1037/a0013788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.UNAIDS. 2008 Report on the Global AIDS Epidemic. Geneva: UNAIDS; 2008. [18 February 2011]. Available at http://www.unaids.org/en/dataanalysis/epidemiology/2008reportontheglobalaidsepidemic/, Archived by WebCite at http://www.webcitation.org/5wbKyBbDI. [Google Scholar]
- 15.Boone TL, Lefkowitz ES, Romo L, Corona R, Sigman M, Au TKF. Mothers’ and adolescents’ perceptions of AIDS vulnerability. J Behav Develop. 2003;27:347–354. [Google Scholar]
- 16.Morojele NK, Kachieng’a M, Nkoko M, Moshia KM, Mokoko E, Parry CDH. The Development of a Methodology to Study Factors Related to Risky Sexual Behaviour among Alcohol Users in Diverse Cultural Settings: Conceptual Framework and Instruments for Qualitative and Quantitative Research on Alcohol Use-related Sexual Risk Behaviour in South Africa. Pretoria, South Africa: Medical Research Council; 2003. [Google Scholar]
- 17.Rawson RA, Gonzales R, Pearce V, Ang A, Marinelli-Casey P, Brummer J. Methamphetamine dependence and human immunodeficiency virus risk behavior. J Subst Abuse Treat. 2008;35:279–284. doi: 10.1016/j.jsat.2007.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kennealley DA. comparison of on-campus and off-campus education by alcohol/drug counselors. J Teach Addict. 2002;1:33–51. [Google Scholar]
- 19.Willis B. Distance Education at a Glance. Guide #1: Distance Education: An Overview. College of Engineering; University of Idaho: [23 April 2010]. Available at: http://www.uiweb.uidaho.edu/eo/dist1.html, archived by WebCite at http://www.webcitation.org/5whLQXBsc. [Google Scholar]
- 20.Corvino J, Carroll KM, Nuro KF, Nich C, Sifry RL, Frankforter TL, et al. Yale Adherence and Competence Scale guidelines. West Haven, CT: Yale University Psychotherapy Development Center; 2000. [Google Scholar]
- 21.Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol. 1994;(Supplement 12):70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- 22.McLellan AT, Carise D, Kleber HD. Can the national addiction treatment infrastructure support the public’s demand for quality care? J Subst Abuse Treat. 2003;25(2):117–121. [PubMed] [Google Scholar]


