Abstract
Purpose
To describe the results of endothelial keratoplasty (EK) in the management of irido-corneal endothelial (ICE) syndrome.
Design
Retrospective, consecutive, interventional case series.
Methods
Eight eyes of seven patients underwent EK for corneal edema owing to ICE syndrome. Simultaneous cataract surgery was performed in five eyes. The charts were reviewed for demographics, clinical findings, and outcomes after EK.
Results
Mean age was 50.4 years (range 35–59 years). Mean follow-up was 12.5 months (range 6–24 months). Corneal clarity was restored in all eyes and was maintained till the last follow-up. Four patients had acute rise in the intraocular pressure in the post-operative period, which was well controlled on medical treatment. One patient who was non-compliant with medications and regular follow-up advice had progression of glaucomatous disc changes and visual field loss. The best-corrected visual acuity ranged from 20/50–20/30.
Conclusions
EK is a viable option in ICE syndrome. Adequate control of glaucoma is the paramount factor in maintaining good visual acuity in these eyes.
Keywords: endothelial keratoplasty, ICE syndrome, glaucoma
Introduction
Irido-corneal endothelial (ICE) syndrome includes a spectrum of clinical manifestations characterized by abnormal proliferation of corneal endothelium leading to corneal edema.1, 2 Until recently, penetrating keratoplasty was performed for visual rehabilitation in these eyes.3, 4, 5 In this series, we report the clinical outcomes in eight eyes of seven patients who underwent endothelial keratoplasty (EK) in the management of this syndrome.
Materials and methods
From January 2009 to December 2011, eight eyes of seven patients were identified and the charts were reviewed for demographics, clinical findings, and outcomes after EK. One case (Patient 4) has been included in another published case series.6 Table 1 summarizes the demographics, clinical features, and the outcomes in the patients who underwent EK for ICE syndrome. Mean follow-up was 12.5 months (range 6–24 months).
Table 1. Clinical information.
| Pt. no. | Age/gender | Eye | Clinical findings | Pre-op CDR | Procedure | Post-op BCVA | Post-op CDR (after cleared graft) | Post-op events | Follow-up (mths) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 59/M | OD | Corneal edema, bullae, superficial scar, iris atrophy, cataract | No view (disc cupping on B scan) | DSAEK+Phaco/PCIOL | 20/40 | 0.8 | (1) Acute IOP rise at 6 months (controlled medically), (2) raised IOP at 10 months with profound vision loss: PL+, PR inaccurate | 21 |
| 2 | 51/M | OS | Corneal edema, hammered silver appearance, cataract | 0.3 | DSAEK+Phaco/PCIOL | 20/30 | 0.3 | — | 12 |
| OD | Corneal edema, hammered silver appearance, superficial haze, PAS (6 clock hours), corectopia, cataract | 0.3 | DSAEK+Phaco/PCIOL | 20/40 | 0.3 | — | 6 | ||
| 3 | 50/M | OS | corneal edema, bullae, PAS at 7 and 11 o'clock, corectopia, ectropion uvae, iris humps, cataract | No view, (disc cupping on B scan) | DSAEK +Phaco/PCIOL | 20/40 | 0.8, Bipolar notch | (1) Acute IOP rise at 3 monts (controlled medically) | 24 |
| 4 | 35/F | OS | Bleb superiorly, corneal edema, superficial haze, PAS 4 clock hours | 0.9, bipolar notch | N-DSAEK, synechiolysis | 20/40 | 0.9:1 | — | 12 |
| 5 | 55/M | OS | Corneal edema, bullae, PAS, cataract | 0.3 | DSAEK+ Phaco/PCIOL | 20/30 | 0.3 | — | 15 |
| 6 | 50/F | OS | Silver-beaten appearance, (CCT-518) iris pigments on endothelial surface, cataract | 0.6, IR thinning | DSAEK+Phaco+PCIOL | 20/50 | (1) Exaggerated early post-op inflammation with raised IOP, (2) acute rise in IOP at 1 and 3 months | 12 | |
| 7 | 53/F | OD | Corneal edema, PAS (3 clock hours) | 0.7:1 | DSAEK, synechiolysis | 20/40 | 0.7:1 | (1) Acute rise in IOP at 1 mth (controlled medically) | 8 |
Abbreviations: BCVA, best-corrected visual acuity; CCT, central corneal thickness; CDR, cup disc ratio; DSAEK, descemet stripping automated endothelial keratoplasty; IOP, intraocular pressure; IR,inferior rim; N-DSAEK, non-Descemet stripping automated endothelial keratoplasty; PAS, peripheral anterior synechaie; PCIOL, posterior chamber intraocular lens;.
Surgical technique
The donor cornea dissection was done using Moria ALTK microkeratome system (Moria/Microtek Inc., Doylestown, PA, USA) equipped with 350 μm microkeratome head. Descemet's membrane stripping was done in all eyes except one (Case 4). Sheets IOL glide (BD Medical-Ophthalmic Systems, Waltham, MA, USA) was used and donor lenticle was inserted using the push-in technique protecting the endothelium with sodium hyaluronate 1% (Healon, Abbott Medical Optics Inc., Abbott Park, IL, USA). The graft was positioned using air tamponade. Additional procedures such as synechiolysis and cataract surgery were performed when needed.
Post-operative evaluation was performed at regular intervals and included assessment of best-corrected visual acuity, slit lamp examination, tonometry, and confocal microscopy (Confoscan 4, Nidek, Gamagori, Japan) whenever possible. The patients were treated with anti-glaucoma medications based on the intraocular pressure (IOP) and the disc findings after consultation with the glaucoma specialists.
Case reports
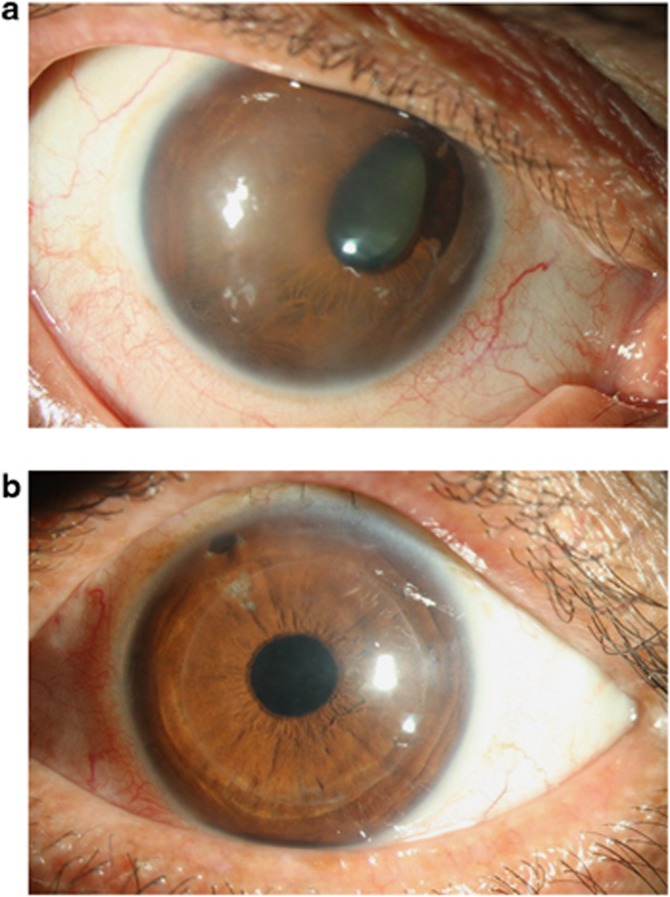
Six patients had unilateral and one (Case 2) had bilateral presentation (Figure 1a and b). One patient (Case 4) developed progressive corneal decompensation following trabeculectomy surgery. Five eyes had glaucomatous disc changes before surgery; in two the disc changes were evident on B scan ultrasonographaphy as the fundus view was obscured owing to corneal edema. The disc changes were confirmed after the restoration of corneal clarity following EK. The IOP was normal in all eyes at the time of surgical intervention. All eyes were phakic at the time of surgery, but six eyes had significant cataract. All patients had visual acuity <20/200 at the time of surgery.
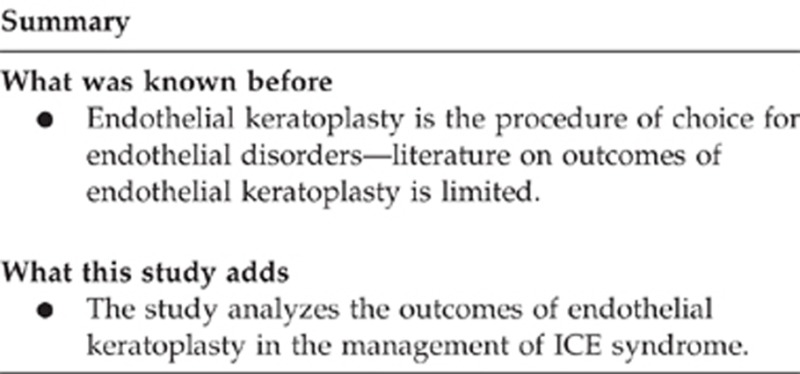
Figure 1.
(a) Pre-operative slit lamp photograph of the right eye of Patient 2. (b)Post-operative photograph of the left eye of the Patient 2.
Corneal clarity was restored and grafts remained clear till the last visit in all eyes. Post-operative visual acuity ranged from 20/50–20/30. No intra-operative and immediate post-operative complications were encountered in any patient except one patient, who had an exaggerated anterior segment inflammation, which was controlled with steroid treatment. In one patient (Case 4), anterior chamber was very shallow despite performing synechiolysis. Descemet stripping was deferred in this patient to avoid inadvertent trauma to the clear lens. The interface was clear throughout the post-operative period.
Four of the seven patients had increased IOP in the post-operative follow-up period. The IOP rise was controlled medically with short course of acetazolamide and addition of one or two topical anti-glaucoma medication. The patients who had post-operative increase in IOP and/or had clinical evidence of glaucomatous disc changes were continued on one or two topical anti-glaucoma medications based on the IOP control. In one patient (Case 1), there was a significant progression of disc and field changes in post-operative period due to non-compliance to the anti-glaucoma medications.
No apparent increase in anterior chamber angle abnormalities after keratoplasty was noted on clinical slit lamp examination during the follow-up visits.
Discussion
ICE syndrome includes progressive essential iris atrophy, Chandler's syndrome, and the Iris-nevus syndrome.1 It is typically considered as unilateral, although cases of bilateral involvement of the same or two different forms might occur.7 Price and Price8 first reported the management of these eyes with EK with good results in three patients with a follow-up range of 1–14 months.
In our series, 5/7 (71.4%) patients had pre-existing glaucomatous disc changes. Four of the five patients had episodes of rise in IOP in the post-operative period, which was managed medically. One patient was non-compliant with anti-glaucoma medications and progressed to advanced field loss. As EK effectively restores the corneal clarity, the paramount factor in maintaining good visual acuity in these eyes is adequate control of glaucoma, which is seen episodically in this syndrome and may not be associated with symptoms such as pain or headaches. Another reason for the rise in IOP could be attributed to a steroid response, although this is difficult to differentiate from the natural course of the disease in these eyes. Hence, patients undergoing EK for ICE syndrome should be followed up regularly and probably at more frequent intervals to closely monitor for IOP control. This is particularly important in eyes with pre-existing glaucomatous disc changes.
We did not observe any remarkable changes in iris and angle abnormalities following EK. A longer period of follow-up is needed for better understanding. In conclusion, surgical intervention in the form of EK along with good control of IOP is pertinent in the management of ICE syndrome.
Acknowledgments
Financial support was provided by the Hyderabad Eye Research Foundation, India.
Author contributions
Involved in design, conduct of study, and data collection: SCH; analysis and interpretation of results: SCH; preparation of manuscript and literature search: SCH and MR; and review of manuscript and final approval: SCH, MR, SIM, SIR, PG, and VSS). Institutional Review Board, LV Prasad Eye Institute, Hyderabad, approved the study.
The authors declare no conflict of interest.
References
- Yanoff M. Iridocorneal endothelial syndrome: unification of a disease spectrum. Surv Ophthalmol. 1979;24:1–2. doi: 10.1016/0039-6257(79)90142-5. [DOI] [PubMed] [Google Scholar]
- Shields MB. Progressive essential iris atrophy, Chandler's syndrome, and the iris nevus (Cogan-Reese) syndrome: a spectrum of disease. Surv Ophthalmol. 1979;24 (1:3–20. doi: 10.1016/0039-6257(79)90143-7. [DOI] [PubMed] [Google Scholar]
- Buxton JN, Lash RS. Results of penetrating keratoplasty in the iridocorneal endothelial syndrome. Am J Ophthalmol. 1984;98 (3:297–301. doi: 10.1016/0002-9394(84)90319-2. [DOI] [PubMed] [Google Scholar]
- Crawford GJ, Stulting RD, Cavnagh HD, Waring GO. III.Penetrating keratoplasty in the management of iridocorneal endothelial syndrome. Cornea. 1989;8 (1:34–40. [PubMed] [Google Scholar]
- Alvim PT, Cohen EJ, Rapuano CJ, Rapuano CJ, Chung CW, Pereira ML, et al. Penetrating keratoplasty in iridocorneal endothelial syndrome. Cornea. 2001;20 (2:134–140. doi: 10.1097/00003226-200103000-00003. [DOI] [PubMed] [Google Scholar]
- Chaurasia S, Ramappa M, Murthy SI, Garg P, Sangwan VS. Endothelial keratoplasty without stripping the Descemet's membrane. Br J Ophthalmol. 2011;95 (10:1473–1474. doi: 10.1136/bjo.2011.204008. [DOI] [PubMed] [Google Scholar]
- Huna R, Barak A, Melamed S. Bilateral iridocorneal endothelial syndrome presented as Cogan – Reese and Chandler's syndrome. J Glaucoma. 1996;5 (1:60–62. [PubMed] [Google Scholar]
- Price MO, Price FW. Descemet stripping with endothelial keratoplasty for treatment of iridocorneal endothelial syndrome. Cornea. 2007;26 (4:493–497. doi: 10.1097/ICO.0b013e318030d274. [DOI] [PubMed] [Google Scholar]