Abstract
BACKGROUND
Obesity is associated with a higher systolic blood pressure (BP) and pulse pressure (PP) in African-American youths, increasing their risk for developing hypertension. However, it is unknown whether arterial stiffness and wave reflection are associated with a higher systolic BP and PP or with smaller PP amplification in overweight/obese (OW/OB) African-American adolescents.
METHODS
We measured carotid–femoral pulse wave velocity (CF-PWV), carotid–radial PWV (CR-PWV), the augmentation index (AIx) adjusted to a heart rate of 75 bpm (AI75), the augmentation pressure (AugP), PP amplification, and body composition in 227 healthy African-American adolescents (age, 16.9±0.2 years; 54% male).
RESULTS
Adolescents who were OW/OB (n = 86, body mass index (BMI) ≥ 85th percentile) demonstrated 5%–6%, 13%–16%, and 2.5% higher aortic and brachial systolic BP, brachial and aortic PP, and mean arterial pressure (MAP), respectively (all P < 0.05), than adolescents of normal-weight (NW, n = 141, BMI < 85th percentile). The OW/OB adolescents had a 7% higher CF-PWV, 5% lower CR-PWV, and 3.5% lower PP amplification than the NW group (all P < 0.05), but no differences in AI75 or AugP. In the entire cohort after adjustment for age, sex, heart rate, height, and MAP, CF-PWV was positively correlated, and CR-PWV and PP amplification were negatively correlated, with total and abdominal/hip adiposity. Additionally, CF-PWV, AI75, and AugP were positively correlated with MAP and negatively correlated with PP amplification. CR-PWV, AI75, and AugP were negatively correlated with brachial and aortic PP.
CONCLUSIONS
Higher aortic stiffness is associated with smaller PP amplification with increasing adiposity in African-American adolescents. Whether a reduction in PP amplification predicts increased CVD risk in obese African-American adolescents requires further study.
Keywords: augmentation index, wave reflection, aortic stiffness, pulse wave velocity, pediatric hypertension, obesity, blood pressure, hypertension.
Childhood obesity has increased dramatically in recent years in the US, with approximately one third of children and adolescents being overweight and approximately 17% being obese.1 The rates of overweight and obesity are even higher among ethnic minorities, including African-Americans, in whom these rates approach 40% and 24%, respectively.1 Paralleling this has been an increase in the rates of obesity-related prehypertension and hypertension in adolescents and young adults.2,3 Importantly, adolescents and young adults with prehypertension exhibit preclinical evidence of cardiovascular target-organ damage, such as increased left ventricular (LV) mass and carotid intimal–medial thickening.4,5 Given this, it is important to identify the early genesis of elevated BP in young persons to prevent the progression of increased BP to overt pre-hypertension and hypertension.
The BP phenotype typically observed in overweight/obese (OW/OB) adolescents is that of a higher systolic BP and PP, with smaller or no differences in diastolic BP than in their age- and sex-matched peers of normal weight (NW).6–8 Interestingly, this BP phenotype in obese children and adolescents resembles that of older adults with “isolated systolic hypertension” (ISH). In adults, ISH is attributed in large part to age-related stiffening of the large elastic arteries9 and the subsequent increase of the magnitude and early arrival of the reflected pressure wave at the ascending aorta.10–12 Indeed, carotid femoral pulse wave velocity (CF-PWV), the “gold standard” measurement of aortic stiffness, is higher in older adults with ISH and is associated with a larger and earlier wave reflection manifested as a higher augmentation index (AIx).9,13,14 Similarly, several recent studies confirm that OW/OB adolescents and young adults also demonstrate a higher CF-PWV than their age-matched NW peers,15,16 and that CF-PWV correlates positively with measures of adiposity. Moreover, elevated CF-PWV is the strongest determinant of a higher LV mass index in adolescents and young adults, independent of traditional risk factors for cardiovascular disease (CVD),17 suggesting a role for aortic stiffness in modulating LV thickening independent of BP. However, the precise hemodynamic mechanisms by which aortic stiffening contributes to premature LV remodeling in youth is unknown.
AIx, a composite measure of the amplitude and timing of pulse wave reflection at the ascending aorta which contributes to an augmented LV afterload, increases with advancing age and hypertension in adults. In contrast, AIx has been reported to be either elevated18 or reduced19 in obese adults. Similarly, although AIx is typically negative in children and adolescents, data are mixed on whether it is higher15 or unchanged20,21 with increased adiposity. Therefore, the contribution (if any) of AIx to increased systolic BP and PP in OW/OB adolescents is unclear. In contrast to CF-PWV and AIx, CR-PWV, an index of peripheral upper-limb artery stiffness, does not increase with aging in adults15,21 and may actually decrease with obesity or metabolic syndrome.18,22 Interestingly, we recently reported that CR-PWV was lower in obese African-American but not in obese white young persons in comparison with their NW peers,23 suggesting potential racial differences in the effects of obesity on upper-limb arterial stiffness.15 In addition, in children and adolescents there is typically a large amplification of the pulse pressure from the central to peripheral arteries (i.e., PP amplification). This widening of central-to-peripheral PP decreases with aging24 and obesity in adults,25 and has recently gained appreciation as a potential novel hemodynamic marker of CVD risk in adults.24,26 It is therefore conceivable that in the setting of increased aortic stiffness and decreased peripheral artery stiffness with obesity in children and adolescents, PP amplification would be reduced in OW/OB adolescents. However, it is currently unknown whether PP amplification is smaller in OW/OB compared with NW African-American adolescents and whether it is associated with aortic stiffness and measures of adiposity.
We therefore conducted the current study to test the primary hypothesis that CF-PWV, but not CR-PWV and AIx, is higher in OW/OB compared with NW African-American adolescents and is positively associated with obesity-related increases in brachial and aortic systolic BP and PP. We further hypothesized that PP amplification would be lower in OW/OB adolescents, partly because of concomitantly higher aortic stiffness and lower peripheral artery stiffness.
METHODS
Study subjects
A total of 227 healthy African-American adolescents (age, 15–19 years) were recruited from the community by advertising in local schools with permission of the principals at each school in Augusta, GA. All of the subjects were healthy on the basis of a parent’s (for subjects < 18 years of age) or the subject’s (for subjects ≥ 18–19 years of age) report of the subject’s health history and freedom from any diseases being treated by a physician or use of medications for cardiovascular, pulmonary, or metabolic disease. Parents of subjects < 18 years of age provided written informed consent for these subjects’ participation in the study, and subjects <18 read and signed a child assent document. Subjects > 18 years of age provided written informed consent. All procedures used in the study were in accordance with the ethical standards of the Helsinki Declaration, and all procedures and informed-consent documents were approved by the Human Assurance Committee of Georgia Health Sciences University. For the procedures used in determining anthropometrics, body composition, and BP, and those used in the measurement of pulse wave analysis and PWV see the section entitled “On-Line Supplementary Information” following the “References” section of this paper.
Statistical analysis
Differences in all variables in NW (body mass index, BMI < 85th percentile; mean BMI percentile, 50±2) and OW/OB (BMI ≥85th percentile; mean BMI percentile 94±1) adolescents were determined with two-tailed independent “t”-tests. Partial correlation analyses of variables for BP and arterial stiffness with those for anthropometrics and body composition were adjusted for age, sex, heart rate, height, and mean arterial pressure (MAP). Partial correlation analyses of brachial and aortic BP components with CF-PWV, CR-PWV, AIx adjusted to a heart rate of 75 bpm (AI75), and unadjusted augmentation pressure (AugP) were adjusted for age, sex, heart rate, and height. An alpha level of P < 0.05 was required for statistical significance. All data are reported as mean ± standard error (SE).
RESULTS
Subject characteristics and blood pressure components in normal-weight and overweight/obese adolescents
OW/OB adolescents did not differ in age from NW subjects, but as expected had a higher weight, body-fat percentage and greater waist and hip circumference (all P < 0.01; Table 1). OW/OB adolescents also had a higher brachial systolic BP (+ 5.6%), aortic systolic BP (+ 5%), brachial PP (+13%), and aortic PP (+16%) (all P < 0.01) than their NW peers (Table 1). The MAP of the OW/OB adolescents was slightly higher (+ 2.5%) than that of the NW group (P = 0.047), but brachial and aortic diastolic BP were not different in the two groups (P > 0.05).
Table 1.
Subject characteristics
| Normal weight | Overweight/Obese | P value | |
|---|---|---|---|
| (n = 141) | (n = 86) | ||
| Age, years | 16.8 ± 0.1 | 16.9 ± 0.1 | 0.28 |
| Male/female, % | 55/45 | 51/49 | --- |
| Weight, kg | 61 ± 1 | 84 ± 2b | <0.01 |
| Height, m | 1.70 ± 0.01 | 1.68 ± 0.01 | 0.06 |
| Body mass index, kg/m2 | 21 ± 0.2 | 30 ± 0.5b | <0.01 |
| Total body fat, % | 18 ± 1 | 30 ± 1b | <0.01 |
| Waist circumference, cm | 72 ± 1 | 86 ± 2b | <0.01 |
| Hip circumference, cm | 95 ± 1 | 106 ± 2b | <0.01 |
| Brachial systolic BP, mm Hg | 125 ± 2 | 132 ± 2b | <0.01 |
| Brachial diastolic BP, mm Hg | 63 ± 1 | 62 ± 1 | 0.74 |
| Brachial pulse pressure, mm Hg | 62 ± 2 | 70 ± 2b | <0.01 |
| Brachial mean arterial pressure, mm Hg | 81 ± 1 | 83 ± 1 | 0.05 |
| Aortic systolic BP, mm Hg | 101 ± 1 | 106 ± 1b | <0.01 |
| Aortic diastolic BP, mm Hg | 64 ± 1 | 64 ± 1 | 0.87 |
| Aortic pulse pressure, mm Hg | 37 ± 1 | 43 ± 1b | <0.01 |
| Heart rate, bpm | 66 ± 1 | 68 ± 1.3 | 0.23 |
| Pulse pressure amplification | 1.7 ± 0.01 | 1.6 ± 0.02a | 0.04 |
Data are mean ± SE.
a P < 0.05; b P < 0.01 vs. normal-weight.
Abbreviations: BP, blood pressure; PP, pulse pressure.
Arterial stiffness, wave reflection, and PP amplification in NW and OW/OB adolescents.
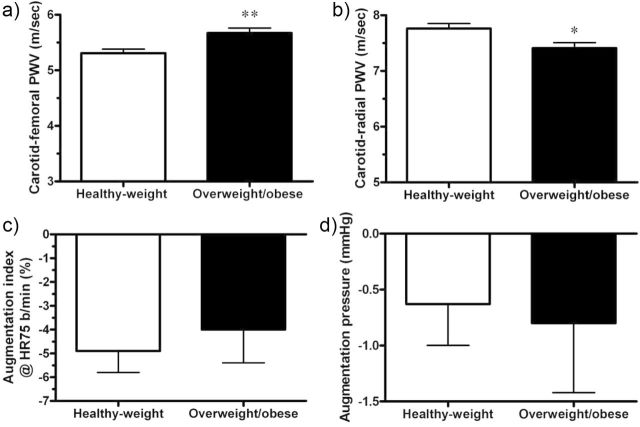
CF-PWV was 7% higher in OW/OB than in NW adolescents (P < 0.01) (Figure 1a), but AI75 and AugP were no different (P > 0.05) between the two groups (Figure 1b, d). Post hoc power calculations for AI75 and Aug BP, assuming an alpha of 0.05 and with a two-tailed test, showed a 99% and 90% power, respectively, to detect any differences in AI75 and AugP in the OW/OB and NW groups. The CR-PWV was 5% lower in the OW/OB subjects than in the NW subjects (P < 0.05; Figure 1d), indicating less upper-limb artery stiffness with higher adiposity. Additionally, PP amplification was significantly lower (P = 0.04) in the OW/OB compared with the NW subjects (Table 1).
Figure 1.
Carotid-femoral pulse wave velocity (PWV) (a), carotid- radial PWV (b), aortic augmentation index normalized to heart rate of 75 bpm (c), and augmentation pressure (d) in overweight/obese (n=141) vs. normal-weight (n=86) African-American adolescents. Data are mean ± standard error. **P < 0.01 vs. normal-weight. *P < 0.05 vs. normal-weight.
Partial correlates of body composition and anthropometric measures with blood pressure components, arterial stiffness, wave reflection, and pulse-pressure amplification
MAP was positively correlated with BMI (r = 0.14, P < 0.01), waist circumference (r = 0.19, P < 0.05), and hip circumference (r = 0.24, P < 0.01), but not with total body fat (P > 0.05). After adjustment for age, sex, height, heart rate and MAP, CF-PWV remained positively correlated with BMI, waist circumference, and hip circumference (all P < 0.01), but not with percent total body fat (Table 2). In contrast, CR-PWV was negatively correlated with BMI (P < 0.05) but not with any other body composition component. Neither AI75 nor AugP were related to any body-composition or anthropometric measures (all P > 0.05), suggesting that there was no association between increased adiposity and wave reflection in this cohort. Interestingly, PP amplification was inversely associated with BMI, total body fat, and waist and hip circumference (all P < 0.05), showing that smaller amplification was associated with increasing adiposity in these adolescents. Additionally, after the same adjustments as named above, brachial systolic BP and PP were related to BMI, total body fat, and waist circumference (all P <0.05; Table 2). These data suggest that select components of brachial and aortic pulsatile BP are associated with higher total and abdominal adiposity in African-American adolescents even after controlling for MAP and other confounders.
Table 2.
Partial correlations between anthropometrics and body composition with pulse wave velocity, augmentation index, augmentation pressure, and blood pressure components after adjustment for age, sex, height, heart rate, and mean blood pressure
| Body Mass Index (kg/m2) | Total Body Fat (%) | Waist Circumference (cm) | Hip Circumference (cm) | |
|---|---|---|---|---|
| Carotid-femoral PWV, m/s | 0.26b | 0.12 | 0.24b | 0.21b |
| Carotid-radial PWV, m/s | –0.16a | –0.13 | –0.11 | –0.10 |
| cAugmentation index@HR75, % | 0.01 | 0.07 | 0.06 | 0.11 |
| Augmentation pressure, mm Hg | –0.01 | 0.03 | 0.05 | 0.10 |
| Pulse pressure amplification | –0.16a | –0.18a | –0.15a | –0.19a |
| Brachial systolic BP, mm Hg | 0.17a | 0.13 | 0.11 | 0.06 |
| Brachial pulse pressure, mm Hg | 0.18b | 0.13 | 0.12 | 0.07 |
| Brachial diastolic BP, mm Hg | –0.20b | –0.16a | –0.12 | –0.10 |
| Aortic systolic BP, mm Hg | 0.23b | 0.18b | 0.17b | 0.14a |
| Aortic pulse pressure, mm Hg | 0.23b | 0.18b | 0.16a | 0.13 |
Values are partial r coefficients.
a P < 0.05; b P < 0.01.
Abbreviations: PWV, pulse wave velocity; BP, blood pressure; augmentation index@HR75, augmentation index adjusted to a heart rate of 75 bpm for each subject.
cNote: because augmentation index@HR75bpm is already corrected for heart rate, heart rate was not entered as a covariate in the partial regression for this variable only.
Partial correlates of blood pressure components with arterial stiffness, augmentation index, and pulse pressure amplification
After adjustment for age, sex, height, and heart rate, CF-PWV was positively related to MAP and inversely related to PP amplification (P < 0.05), but not to any other BP components (Table 3). Interestingly, AI75 and AugP were positively correlated with diastolic BP and MAP (P < 0.05) and negatively correlated with brachial and aortic systolic BP and PP (Table 3). These data suggest that smaller (not larger) pressure-wave reflection was associated with the higher systolic BP and PP in our cohort (all P < 0.01).
Table 3.
Partial correlations between brachial and central blood pressure components with carotid-femoral pulse-wave velocity, augmentation index, augmentation pressure, and carotid-radial pulse-wave velocity after adjustment for age, sex, height, and heart rate
| Brachial systolic BP | Brachial PP | Brachial diastolic BP | Central systolic BP | Central PP | Mean arterial pressure | PP amplification | |
|---|---|---|---|---|---|---|---|
| Carotid-femoral PWV | 0.07 | 0.02 | 0.13 | 0.14 | 0.06 | 0.17a | –0.16a |
| Augmentation index@HR75c | –0.28b | –0.35a | 0.24b | –0.04 | –0.22b | 0.22b | –0.56b |
| Augmentation pressure | –0.38b | –0.43b | 0.21b | –0.14a | –0.27b | 0.16a | –0.64b |
| Carotid-radial PWV | –0.13 | –0.19b | 0.20b | –0.09 | –0.20b | 0.06 | 0.06 |
Values are partial r coefficients.
Abbreviations: PWV, pulse wave velocity; PP, pulse pressure; BP, blood pressure; augmentation index@HR75, augmentation index adjusted to a heart rate of 75 bpm for each subject.a P < 0.05; b P < 0.01.
cNote: because augmentation index@HR75 is already corrected for heart rate, heart rate was not entered as a covariate in the partial regression for this variable only.
Both AI75 and AugP were also negatively correlated with PP amplification, indicating that larger wave reflection was related to smaller amplification of the aortic-brachial pulse pressure. Moreover, CR-PWV was positively correlated with diastolic BP but was negatively correlated with brachial and aortic PP (all P < 0.01), suggesting the possibility that lower (not higher) peripheral upper-limb artery stiffness is associated with augmented aortic and peripheral PP in African-American adolescents (Table 3).
DISCUSSION
The primary finding in the current study is that African-American adolescents who are OW/OB demonstrate higher aortic stiffness (CF-PWV), in the absence of any differences in pressure wave reflection (AI75 or Aug BP) compared with their age-matched NW peers. Although the observed higher brachial and aortic systolic BPs in the OW/OB adolescents were expected, the magnitude of the elevation in systolic BP and PP as compared with MAP, and lack of increase in diastolic BP, underscores the novel observation that higher pulsatile pressure, rather than MAP, is the major hemodynamic abnormality associated with obesity in adolescents. Interestingly, CF-PWV was positively associated with MAP but not with brachial or central systolic BP or PP. This suggests the possibility that the increase in CF-PWV is not related to the higher systolic BP and PP observed in our OW/OB cohort. However, we are unable to determine whether higher CF-PWV is the cause of or a consequence of elevated MAP. Nevertheless, CF-PWV was positively correlated with most measures of total and abdominal adiposity (Table 2) even after adjustment for MAP, confirming that the association between higher CF-PWV and greater adiposity is not simply mediated by the augmented distending pressure.
The second novel finding in our study was that AI75 and AugP did not differ between OW/OB and NW adolescents, and that both were inversely associated with brachial and central systolic BP and PP. Although it was not surprising that AI75 and AugP are negative in healthy adolescents,20 the inverse relation with BP implies that the higher systolic BP and PP in the central and peripheral arteries are paradoxically associated with reduced wave reflection rather than with augmented wave reflection. This finding is not just a result of the use of PP in the mathematical calculation of AI75, because these findings were similar for AugP.
Third, in accord with the findings in our previous study23 and some studies of adults,18,22 CR-PWV was lower in OW/OB adolescents compared with their lean peers, and was negatively associated with brachial and central systolic BP. Additionally, we report for the first time that PP amplification, an index of the magnitude of amplification of the PP from the aorta to the brachial arteries, was lower in the OW/OB compared with the NW African-American adolescents in our study (Table 1). Consistent with this finding was the negative relation of PP amplification to BMI, total body fat, and hip circumference (Table 2) after adjustment for confounders, confirming the findings in a recent study of adults that smaller PP amplification was associated with higher adiposity.25 Furthermore, PP amplification was inversely correlated with CF-PWV, suggesting the possibility that increased aortic stiffness contributes in part to the reduced amplification of PP with increasing adiposity in teenagers.
Overweight/obesity, carotid-femoral pulse-wave velocity and augmentation index/pressure
Previous studies have found higher aortic stiffness and systolic BP in OW/OB young persons,15,20 but data are mixed on whether AI75 is altered in obese youth. Urbina et al. 15 reported a higher CF-PWV and AI75 in OW/OB adolescents and young adults but no difference in AI75 between NW and obese adolescents and young adults in another study.20 Interestingly, in the latter study, Urbina et al. reported that AI75, but not CF-PWV, was higher only in obese adolescents/young adults with a higher homeostasis model assessment of insulin resistance (HOMA) score, indicating that the presence of insulin resistance in obese young persons may adversely modulate wave reflection. However, the HOMA score did not remain as a significant predictor in multivariate models with age, sex, BMI, and BP. The differences between our study and Urbina and colleagues’ study may be explained by the wider age range (10–24 years) of subjects in their study than in our cohort (age 14–19 years), differences in racial/ethnic makeup, and their inclusion of subjects with hypertension and antihypertensive medications.
In accord with our findings, Lurbe et al. 21 reported that a higher Alx was not associated with obesity in a comparative study with children, but that rather a low birth weight was the best predictor of a higher AIx in the children their study. Our study extends these findings to African-American adolescents and demonstrates that despite higher aortic stiffness and BP, AI75 is not increased with higher adiposity and is not associated with any measure of body fatness. Taken together, our data suggest that AI75 probably does not contribute positively to the obesity-related increases in systolic pressure and PP observed in African-American adolescents in our study, and indicate that other central hemodynamic mechanisms are likely involved.
Overweight/obesity and carotid-radial pulse wave velocity
The finding in our study that CR-PWV was lower in the OW/OB subjects and inversely related to adiposity was surprising but not without precedent. Urbina et al. 15 reported no difference in CR-PWV but a lower brachial artery distensibility in obese than in NW adolescents/young adults. We previously reported a lower CR-PWV in a cohort of obese as compared with NW African-American adolescents/young adults despite the lack of any differences in the two groups’ 24-hour systolic BP.23 Interestingly, that same study found no difference in CR-PWV in a white, age-matched obese cohort, suggesting that a racial difference may exist in peripheral upper-limb artery stiffness with obesity in adolescents/young adults. Furthermore, our data showed that CR-PWV was also inversely related to brachial and aortic PP, suggesting that upper-limb artery stiffness does not positively contribute to augmented systolic BP and PP in OW/OB African-American adolescents.
Overweight/obesity and pulse pressure amplification
Our study is the first to report that OW/OB adolescents demonstrate a small but significant reduction in PP amplification as compared with their NW peers, and that PP amplification was negatively associated with adiposity. In addition, PP amplification was negatively related to CF-PWV in our cohort, indicating the possibility that aortic stiffness contributes in part to the reduced amplification of PP with increased adiposity in African-American teenagers. Given that upper-limb artery stiffness was lower in OW/OB youth in the setting of higher aortic stiffness, it is conceivable that an exaggerated reduction in impedance mismatching between the elastic aorta and the upper-limb muscular arteries explains this observation. These findings have significant clinical implications because PP amplification was recently identified as a novel hemodynamic biomarker of CVD risk in adults.24 Therefore, future studies need to determine whether a reduction in PP amplification is an important early predictor of increased CVD risk in obese African-American adolescents.
Our results should be interpreted in the context of several limitations. First, the estimated aortic BP and related hemodynamics (AI75, AugP, and PP amplification) were obtained from an aortic pressure waveform derived from a radial pressure waveform using a transfer function that has not been validated in children. However, most of the subjects were peri- or postpubertal, and transfer function-derived aortic BP and AIx have been reported previously in this age group15,17,20,21 making the transfer function likely to be as accurate, but with the same limitations as in adults.28 Second, our results were obtained from African-American adolescents and may therefore not be generalized to other ethnic minorities or Caucasian teenagers. Lastly, our data are cross-sectional and are limited to associations, therefore the causal relation between variables cannot be determined from our study.
In summary, aortic stiffness is greater and PP amplification is smaller in OW/OB African-American adolescents compared with a group of NW adolescents, and both are associated with select measures of increased total and abdominal adiposity. In contrast, wave-reflection does not differ between the two group and peripheral artery stiffness is lower with increasing adiposity in African-American adolescents. Moreover, increased wave reflection and decreased peripheral artery stiffness are associated with lower (not higher) systolic BP or PP. Future investigations are required to determine whether a small reduction in PP amplification is a novel indicator of increased CVD risk in African-American adolescents who are overweight or obese, and whether additional central pulsatile hemodynamic characteristics contribute to the increase in systolic BP and PP in this group.
SUPPLEMENTARY MATERIAL
Supplementary materials are available at the American Journal of Hypertension online (http://www.oxfordjournals.org/our_journals/ajh/). Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author.
DISCLOSURE
The authors have no conflicts of interest in the information presented in this paper.
ACKNOWLEDGMENTS
The authors thank the subjects who participated in this study. This study was supported by a GHSU Child Health Discovery Institute grant to G.L.P. and National Institutes of Health grant R01 HL077230-02 to Y.D.
REFERENCES
- 1. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012; 307: 483–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McNiece KL, Poffenbarger TS, Turner JL, Franco KD, Sorof JM, Portman RJ. Prevalence of hypertension and pre-hypertension among adolescents. J Pediatr 2007; 150: 640–644 644 e1 [DOI] [PubMed] [Google Scholar]
- 3. Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation 2007; 116: 1488–1496 [DOI] [PubMed] [Google Scholar]
- 4. Urbina EM, Khoury PR, McCoy C, Daniels SR, Kimball TR, Dolan LM. Cardiac and vascular consequences of pre-hypertension in youth. J Clin Hypertens (Greenwich) 2011; 13: 332–342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhu H, Yan W, Ge D, Treiber FA, Harshfield GA, Kapuku G, Sneider H, Dong Y. Cardiovascular characteristics in American youth with prehypertension. Am J Hypertens 2007; 20: 1051–1057 [DOI] [PubMed] [Google Scholar]
- 6. Sorof J, Daniels S. Obesity hypertension in children: a problem of epidemic proportions. Hypertension 2002; 40: 441–447 [DOI] [PubMed] [Google Scholar]
- 7. Sorof JM, Poffenbarger T, Franco K, Bernard L, Portman RJ. Isolated systolic hypertension, obesity, and hyperkinetic hemodynamic states in children. J Pediatr 2002; 140: 660–666 [DOI] [PubMed] [Google Scholar]
- 8. Tu W, Eckert GJ, DiMeglio LA, Yu Z, Jung J, Pratt JH. Intensified effect of adiposity on blood pressure in overweight and obese children. Hypertension 2011; 58: 818–824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wallace SM, Yasmin, McEniery CM, Maki-Petaja KM, Booth AD, Cockcroft JR, Wilkinson IB. Isolated systolic hypertension is characterized by increased aortic stiffness and endothelial dysfunction. Hypertension 2007; 50: 228–233 [DOI] [PubMed] [Google Scholar]
- 10. Mitchell GF, Wang N, Palmisano JN, Larson MG, Hamburg NM, Vita JA, Levy D, Benjamin EJ, Vasan RS. Hemodynamic correlates of blood pressure across the adult age spectrum: noninvasive evaluation in the framingham heart study. Circulation 2010; 122: 1379–1386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mitchell GF, Parise H, Benjamin EJ, Larson MG, Keyes MJ, Vita JA, Vasan RS, Levy D. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women: the Framingham Heart Study. Hypertension 2004; 43: 1239–1245 [DOI] [PubMed] [Google Scholar]
- 12. McEniery CM, Yasmin, Hall IR, Qasem A, Wilkinson IB, Cockcroft JR. Normal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo-Cardiff Collaborative Trial (ACCT). J Am Coll Cardiol 2005; 46: 1753–1760 [DOI] [PubMed] [Google Scholar]
- 13. McEniery CM, Yasmin, Wallace S, Maki-Petaja K, McDonnell B, Sharman JE, Retallick C, Franklin SS, Brown MJ, Lloyd RC, Cockcroft JR, Wilkinson IB. Increased stroke volume and aortic stiffness contribute to isolated systolic hypertension in young adults. Hypertension 2005; 46: 221–226 [DOI] [PubMed] [Google Scholar]
- 14. Mitchell GF, Conlin PR, Dunlap ME, Lacourciere Y, Arnold JM, Ogilvie RI, Neutel J, Izzo JL, Jr, Pfeffer MA. Aortic diameter, wall stiffness, and wave reflection in systolic hypertension. Hypertension 2008; 51: 105–111 [DOI] [PubMed] [Google Scholar]
- 15. Urbina EM, Kimball TR, Khoury PR, Daniels SR, Dolan LM. Increased arterial stiffness is found in adolescents with obesity or obesity-related type 2 diabetes mellitus. J Hypertens 2010; 28: 1692–1698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sakuragi S, Abhayaratna K, Gravenmaker KJ, O'Reilly C, Srikusalanukul W, Budge MM, Telford RD, Abhayaratna WP. Influence of adiposity and physical activity on arterial stiffness in healthy children: the lifestyle of our kids study. Hypertension 2009; 53: 611–616 [DOI] [PubMed] [Google Scholar]
- 17. Urbina EM, Dolan LM, McCoy CE, Khoury PR, Daniels SR, Kimball TR. Relationship between Elevated Arterial Stiffness and Increased Left Ventricular Mass in Adolescents and Young Adults. J Pediatr 2011; 158: 715–721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ounis-Skali N, Bentley-Lewis R, Mitchell GF, Solomon S, Seely EW. Central aortic pulsatile hemodynamics in obese premenopausal women. J Am Soc Hypertens 2007; 1: 341–346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Maple-Brown LJ, Piers LS, O'Rourke MF, Celermajer DS, O'Dea K. Central obesity is associated with reduced peripheral wave reflection in Indigenous Australians irrespective of diabetes status. J Hypertens 2005; 23: 1403–1407 [DOI] [PubMed] [Google Scholar]
- 20. Urbina EM, Gao Z, Khoury PR, Martin LJ, Dolan LM. Insulin resistance and arterial stiffness in healthy adolescents and young adults. Diabetologia 2012; 55: 625–631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lurbe E, Carvajal E, Torro I, Aguilar F, Alvarez J, Redon J. Influence of concurrent obesity and low birth weight on blood pressure phenotype in youth. Hypertension 2009; 53: 912–917 [DOI] [PubMed] [Google Scholar]
- 22. Fantin F, Di Francesco V, Rossi A, Giuliano K, Marino F, Cazzadori M, Gozzoli MP, Vivian ME, Bosello O, Rajkumar C, Zamboni M. Abdominal obesity and subclinical vascular damage in the elderly. J Hypertens 2010; 28: 333–339 [DOI] [PubMed] [Google Scholar]
- 23. Zhu H, Yan W, Ge D, Treiber FA, Harshfield GA, Kapuku G, Sneider H, Dong Y. Relationships of cardiovascular phenotypes with healthy weight, at risk of overweight, and overweight in US youths.. Pediatrics 2008; 121: 115–122 [DOI] [PubMed] [Google Scholar]
- 24. Benetos A, Thomas F, Joly L, Blacher J, Pannier B, Labat C, Salvi P, Smulyan H, Safar ME. Pulse pressure amplification a mechanical biomarker of cardiovascular risk.. J Am Coll Cardiol 2010; 55: 1032–1037 [DOI] [PubMed] [Google Scholar]
- 25. Wykretowicz A, Rutkowska A, Krauze T, Przymuszala D, Guzik P, Marciniak R, Wysocki H. Pulse pressure amplification in relation to body fatness.. Br J Clin Pharmacol 2012; 73: 546–552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Regnault V, Thomas F, Safar ME, Osborne-Pellegrin M, Khalil RA, Pannier B, Locolley P. Sex difference in cardiovascular risk: role of pulse pressure amplification.. J Am Coll Cardiol 2012; 59: 1771–1777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sugawara J, Hayashi K, Tanaka H. Distal shift of arterial pressure wave reflection sites with aging.. Hypertension 2010; 56: 920–925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Verbeke F, Segers P, Heireman S, Vanholder R, Verdonck P, Van Bortel LM. Noninvasive assessment of local pulse pressure: importance of brachial-to-radial pressure amplification.. Hypertension 2005; 46: 244–248 [DOI] [PubMed] [Google Scholar]