Abstract
Background
Investing in mental well-being is considered a supplement to current mental health service delivery in which the treatment and prevention of mental disorders are core components. It may be possible for people to enhance their well-being by boosting their “mental fitness.”
Objective
Psyfit, an online, multi-component, fully automated self-help intervention, was developed with the aim of improving well-being and reducing depressive symptoms. The efficacy and cost-effectiveness of this intervention will be examined in a randomized controlled trial.
Methods
In this two-armed randomized controlled trial, a total of 290 participants will be assigned to use Psyfit (experimental condition) or to a 6-month waiting list (control condition). Adults with mild to moderate depressive symptoms interested in improving their mental fitness will be recruited from the general population through advertisements on the Internet and in newspapers. Online measurements by self-assessment will be made prior to randomization (pre-test), 2 months after baseline (post-test), and 6 months after baseline (follow-up).
Results
The primary outcome is well-being. Secondary outcomes are depressive symptoms, general health, vitality, and economic costs. Analysis will be conducted in accordance with the intention-to-treat principle.
Conclusions
This study will examine the efficacy and cost-effectiveness of an online intervention that aims to promote well-being in people with elevated levels of depressive symptoms. If shown to be effective, the intervention could prove to be an affordable and widely accessible intervention to improve well-being in the general population.
Trial Registration
The study is registered with the Netherlands Trial Register, part of the Dutch Cochrane Centre (NTR2126).
Keywords: Mental health; public health; preventive medicine; depression, well-being; happiness
Introduction
Depression, anxiety disorders, and alcohol dependency are highly prevalent mental disorders [1,2] and among the 10 disorders with the greatest disease burden [3]. These disorders are associated with reduced quality of life [4] and high economic costs due to productivity losses and high levels of health service uptake [5]. In addition, many more people suffer from poor well-being [6], subclinical depression [7], and stress at work [8] putting them at greater risk of developing a mental disorder later on. In the current dynamic and innovative knowledge- and service-driven economy, more people are faced with mentally demanding jobs. This places unique demands on people’s emotional, social, and cognitive capacities [9,10]. Countries are challenged by the adverse consequences stemming from these demanding circumstances, such as burnout, absenteeism, and subsequent economic costs. Therefore, it is important is to reach people at an early stage when the development of a full-blown mental disorder might still be prevented. So far, preventive interventions developed for this reason focus mainly on the prevention of mental health problems and disorders, and less on the improvement of well-being [11].
The World Health Organization (WHO) defines mental health as “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively, and is able to make a contribution to his or her community.” This definition of mental health represents a paradigm shift from focusing on the narrow medical constructs of illness and disease only, to embracing well-being as well [12].
The WHO definition also underscores the notion that mental health is not merely the absence of mental illness. Well-being and mental illness, although correlated, are independent concepts and not just opposites on a single continuum. People presenting with low levels of well-being have similarly poor psychosocial outcomes as people suffering from mental illness [13]. Likewise, people with mental disorders are capable of experiencing well-being, to some degree [14]. In general, people with high levels of well-being are physically healthier, live longer, are more productive at work, and use less health care [15,16]. Longitudinal and experimental evidence suggests that positive affect and well-being may generate these desirable outcomes [17]. The available evidence suggests that the enhancement of well-being might be a valuable public health strategy in mental health promotion.
With this positive approach to mental health in mind, we developed an Internet-based self-help intervention (“Psyfit”) aimed at the promotion of well-being. Below, we elaborate on the public health rationale for this type of intervention, including the definition of well-being, the relevance of the Internet as an implementation vehicle, and the use of positive psychology interventions as a starting point.
Definition of Well-being
There are three different types, or concepts, of well-being. The first is subjective well-being, which is a cognitive and/or affective appraisal of one’s own life as a whole and seeking a balance between positive and negative emotions [18]. The second is the concept of psychological well-being. This concept builds on the work of Carol Ryff who was dissatisfied with the emphasis on subjective well-being and focused more on the optimal functioning of the individual [19]. In Ryff’s view, psychological well-being contains six elements: self-acceptance, autonomy, environmental mastery, personal growth, purpose in life, and personal relations with others. According to this view, the attainment of personal happiness is not the goal in life, but rather self-actualization and meaning. The third concept arose from the work of Corey Keyes who called for a broader and less self-centered orientation towards well-being and for the expansion of subjective and psychological well-being to include social well-being; in other words, a complete state model of mental health [6]. Social well-being refers to the extent to which a person feels at home in society, trusts other people, and makes sense out of the world. The WHO’s definition is clearly rooted in this perspective.
Using the Internet: eHealth
The promotion of well-being requires the delivery of effective and accessible interventions aimed at sustainable behavioral change. The Internet might offer the opportunity to reach this goal. Using persuasive technology techniques, programs designed to change attitudes and behaviors can be made for computers, game systems, and mobile devices [20] so that they are highly engaging and enjoyable at the same time. Internet interventions are defined as highly structured; self- or semi self-guided; founded on evidence-based, face-to-face interventions; tailored to provide follow-up and feedback; personalized to the user; interactive; and enhanced by animation, audio, or video technology (if possible) [21].
eMental Health interventions can vary from plain information, tailored advice, single exercises, and interactive self-help programs to structured online therapies with or without guidance from a therapist. The major advantages of eMental Health are that Internet interventions can be offered on a broad scale, they are able to engage hard-to-reach people, and they can reduce therapists’ time (ie, reduce costs) [22].
In the field of Internet interventions, the efficacy of interventions aimed at the reduction of depressive symptoms or anxiety has been demonstrated meta-analytically [23]. The majority of these programs are based on cognitive behavioral therapy [24] and problem-solving therapy [25,26].
Positive Psychology Interventions
The positive psychology movement has developed many interventions that focus on flourishing and positive functioning. These include counting one’s blessings [27-29], practicing kindness [30,31], setting personal goals [32-34], expressing gratitude [28,29], and using personal strengths [28]. A comprehensive meta-analysis of 51 positive psychology interventions has demonstrated moderate effect sizes for enhancing well-being and reducing depressive symptoms [35].
However, experimental research on well-being interventions offered over the Internet is still scarce and the results are mixed. A randomized controlled trial with 2 separate interventions (working with your strengths and problem solving) and a placebo control group showed mixed results [36]. Well-being was improved, but there was not a significant impact on mental illness. In another trial [28], the Internet was used for the recruitment of participants and the collection of data. The single exercises (using signature strengths in a new way and recapitulating three good things) enhanced well-being and reduced depressive symptoms for up to 6 months. Also, “writing and reading a gratitude letter” was effective, but only in the short term. However, a more critical look at the interventions reveals that these exercises were not truly Internet-based interventions as described in the previously cited definition by Ritterband [21] because the interventions were neither interactive nor personalized. Another two randomized controlled trials examined the effects of multi-component interventions [37, 38]. In a workplace setting, an intervention called “Resilience Online” did not demonstrate any significant effects [37]. In another study using an online version of positive psychotherapy, depressive symptoms were significantly reduced, but there was no improvement in subjective well-being [38].
The Current Study
The aim of this study is to evaluate the efficacy and cost-effectiveness of Psyfit, an online well-being program [39]. The study will add to the existing literature by testing a multi-component and flexible Internet-based intervention to promote well-being. To date, the research in this area is limited to either single interventions focusing on one well-being exercise at a time [28, 36] or to multiple protocol-based interventions [37,38]. In these studies, participants in the intervention groups are allocated to an inflexible intervention, although most people would prefer to choose what they need and feel up to doing [30,40,41]. For this reason, Psyfit offers a choice of different interventions that participants can tailor themselves.
The primary objective of this study is to evaluate the effectiveness of the Psyfit intervention in comparison to a waiting list control group. We hypothesize that the intervention group will demonstrate a significant increase in well-being and a reduction in depressive symptoms at post-test and follow-up compared to the control group. Secondary study objectives are to conduct an economic evaluation and to examine if particular subgroups benefit differently (ie, more or less) than others from the intervention.
Methods
Study Design
This study is designed as a randomized trial with two parallel groups. In the experimental condition, participants will receive 2 months free access to Psyfit. In the control condition, participants will be put on a waiting list for 6 months before they are offered access to Psyfit. The study is designed to compare the efficacy and cost-effectiveness of Psyfit relative to the waiting list control condition. A secondary objective is to examine whether certain groups (eg, based on depressive symptoms, gender, and education level) benefit differently from the intervention. Participants in both conditions will have unrestricted access to professional help, if needed. The study protocol, interventions, participant information, and informed consent procedure have been approved by the Dutch Medical Ethics Committee for Mental Health Care (METIGG), under registration number 9218.
Inclusion and Exclusion Criteria
The participant group is defined as everyone willing to improve their “mental fitness.”
Participants will be included if they: (1) are 21 years or older; (2) present with very mild to moderate depressive symptoms with a score between 10-24 on the Center for Epidemiological Studies Depression Scale (CES-D); (3) have moderate or low levels of well-being as measured with the Mental Health Continuum-Short Form (MHC-SF); (4) have access to a computer and the Internet; and (5) have sufficient knowledge of the Dutch language. The CES-D [42] and MHC-SF [43,44] inclusion and exclusion scores are based on established cut-off points.
People with serious depressive symptoms (CES-D score =>25) or active suicidal thoughts or plans (determined from the Web Screening Questionnaire [45]) will be excluded from this study. Those who fail to meet these selection criteria will be notified by email and will be advised to contact their general practitioner if their depressive symptoms exceed the threshold limit. In cases of suicidal ideation, people will be urgently referred to the national online suicide-prevention platform for help.
Recruitment
Participants will be recruited through banners on Internet websites related to mental health and well-being. In addition, advertisements will be placed in newspapers and monthly magazines on health-related topics.
The recruitment message for the study is formulated positively (ie, not with a focus on symptoms and problems): “Would you like to increase your mental fitness? Would you like to feel better? Improve your mental fitness and participate in our study of an online self-help program, Psyfit.” The analogy is made with physical fitness: “There are certain lifestyle behaviors you could adopt that can make you feel mentally fit.” Preliminary focus group research has shown that people with minor mental health problems, those experiencing stress, or those who just “don’t feel good” are attracted by the “mental fitness” message [46].
The advertisements will include the website address where people can register for Psyfit (www.psyfit.nl). This website contains complete information about the study and a demonstration video of the intervention. Those interested in participating can leave their name and email address. The email and Internet Protocol (IP) addresses will be checked for multiple registrations. Following this, prospective participants will receive an email with additional information about the study and a link to the online informed consent form and online questionnaire.
Randomization
The online randomization procedure will be carried out at the individual level. After returning the informed consent form and completing the baseline questionnaire, people who meet the inclusion criteria will be randomly allocated to the experimental group (Psyfit) or to the waiting list and they will be notified by email. Randomization will be stratified by gender, education, and severity of symptoms based on CES-D scores (scores between 10-15 and 16-24). A computer program will allocate participants using a generated randomization list. Block randomization in blocks of two will be performed to ensure equal distribution of participants across conditions.
Intervention Group: Psyfit
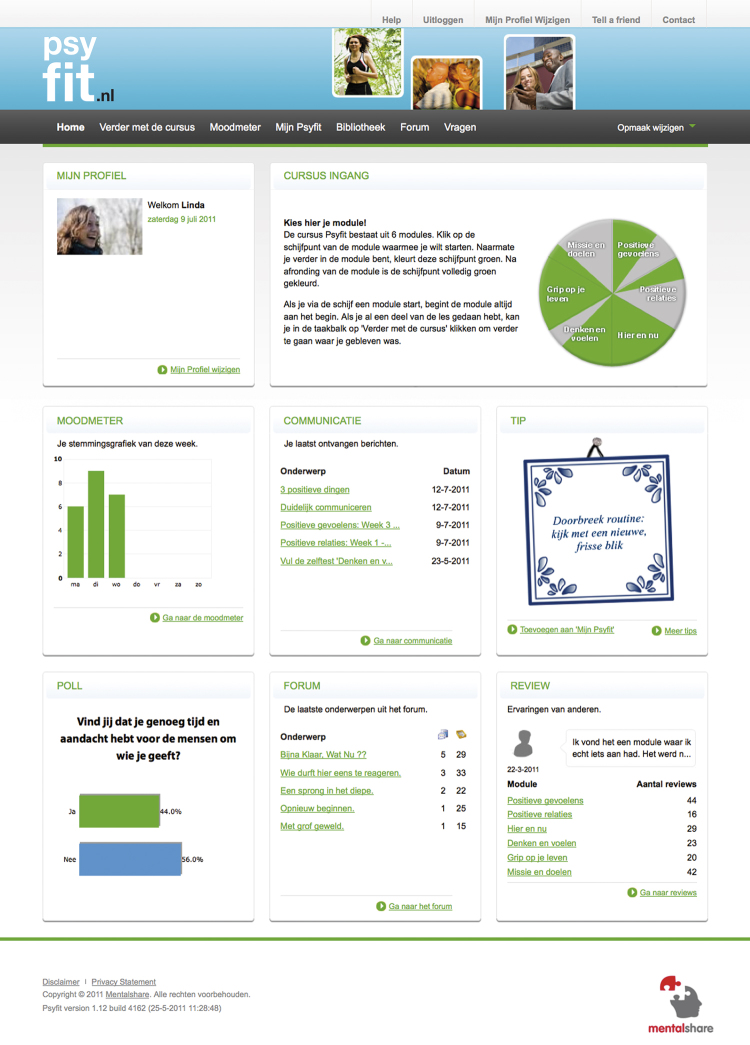
Psyfit is offered as an online and fully automated self-help intervention without active support from a therapist (see Figure 1 for a screenshot of the intervention). Participants tailor their own intervention program to their personal needs and measure their progress by several self-tests. In addition, they can discuss their experiences in an online community accessed via Psyfit.
Figure 1.
Screenshot of the Psyfit portal.
The content of the well-being program, Psyfit, is based on an extensive literature review [10]. Elements in the intervention originate from positive psychology [28,35], mindfulness [47], cognitive behavioral therapy [48], and problem-solving therapy [49].
Psyfit consists of six modules, each containing a 4-week program:
1. Mission and goals (living from a deeply felt mission and personal values);
2. Positive feelings (positive thinking and working on your positive affect);
3. Positive relations (connection with other people and your environment);
4. Living in the moment (consciously living and enjoying);
5. Thinking and feeling (change negative thinking patterns, optimistic thinking); and
6. Master your life (managing personal energy, stress, and problems).
In theory, each module is likely to have impact on well-being. During the study, the Psyfit website is accessible only to the participants in the experimental group. An email will be sent to each participant assigned to Psyfit with a personal username and password. From the moment the participant logs on, a 2-month free access to the intervention is activated. If a participant doesn’t log on, a reminder email with the log-on codes will be sent after one week and, if necessary, after two weeks and again after three weeks. Participants are allowed to use the program at any time they want during the trial period. Participants are advised to choose and finish at least one module during the intervention period. During each 4-week module, participants receive background information on the specific subject, view short films, and receive a weekly assignment that they are expected to complete during that week. On average, this takes 20 to 30 minutes each day.
Participants are free to use all other functionalities offered in Psyfit and can always choose to start a new module. For an overview of functionalities, see Textbox 1.
Functionalities in Psyfit.
General self-test to assess individual well-being level beforehand and after 2 months.
A personal plan in which the participant can reflect on his or her goals, motives, and pitfalls.
A “mood meter” for monitoring changes in the mood of the participant. The outcomes are presented in a graph.
Automatic email service twice a week with reminders, tips, and advice.
Online community for sharing experiences and peer-to-peer support.
Contact form: participants can ask questions and receive feedback from a psychologist via email. If required, the participant is referred to professional care. Technical assistance is also provided.
“My Psyfit”: the participant can download and print out a personal PDF blueprint of the intervention with all the modules, exercises, and progress measurements completed.
Videos: each module starts with a video showing a Dutch expert explaining the relevance of this particular module.
Module self-tests: each module starts and ends with a short self-test to see if the particular skill has improved.
The participant can work through the intervention independently (self-help) but can fill in a contact form with a question if necessary. Psyfit could be likened to a toolbox from which people can “pick and mix” whatever they like and need. The web statistics module will systematically track and trace the actions of each participant, such as the number of log-on times, the time spent on the website, and the modules chosen. This enables adherence to the intervention to be examined.
Control Group
Participants in the control condition are placed on a waiting list for 6 months. After a 6-month follow-up assessment, they will receive their personal user name and password for Psyfit.
Assessments
The primary outcome measure is well-being. Secondary outcome measures include depressive symptoms, general health and vitality, and economic costs (as measured by health care use, days of absence, inefficient job performance, and work productivity). For an overview of outcomes and instruments, see Table 1.
Table 1.
Questionnaires and assessment times.
| T0 | T1 | T2 | ||
| Questionnairea | Measurement | Pre-test | Post-testb | Follow-upc |
| MHC-SF | Well-being/positive mental health | X | X | X |
| WHO-5 | Well-being | X | X | X |
| CES-D | Symptoms of depression | X | X | X |
| MOS SF-36 subscales | Vitality and general health | X | X | X |
| TIC-P and PRODISQ | Health service uptake and production losses | X | X | X |
| CSQ-8 | Client satisfaction | X | ||
| Demographics | Age, gender, education, marital status, job status | X |
a all questionnaires are discussed within Instruments section
b 2 months after T0
c 6 months after T0
Measurements will be taken at baseline (pre-test), directly after the intervention (post-test, 2 months after baseline), and 6 months later (follow-up). All measurements are self-report measures and will be administered via email with a link to the questionnaire on the Internet.
High dropout rates are a characteristic feature of online trials and can be as high as 50% [50]. Therefore, email reminders and rewards (eg, raffle of six iPods and vouchers) for filling in the questionnaires will be used. It is expected that this will lead to a lower attrition rate.
Instruments
Well-Being and Positive Mental Health
Well-being will be assessed with two questionnaires measuring different concepts. The Mental Health Continuum-Short Form (MHC-SF) [51] is a 14-item self-report questionnaire that categorizes measures of well-being as “languishing,” “moderate,” or “flourishing.” Participants rate the items on a 6-point scale from 0 (never) to 5 (every day). The MHC-SF measures subjective well-being as well as psychological and social well-being. These aspects are all addressed in Psyfit; therefore, this questionnaire was chosen. The MHC-SF has shown good internal consistency (> .80) and discriminant validity [44,52].
The WHO-Five Well-being Index (WHO-5) contains 5 positively formulated items on mental health [53]. Participants are asked to rate the items using a 6-point scale ranging from 0 (never) to 5 (all of the time). The WHO-5 has been validated in different populations [53] and is useful as a screening instrument for depression [54]. It was chosen as a measurement instrument because of its brevity and the concurrent validity with depression.
Depressive Symptoms
Depressive symptoms will be measured by the Dutch version of the Center for Epidemiological Studies Depression Scale, the CES-D [55]. The CES-D is a 20-item self-rating scale with item scores ranging from 0 to 3 (higher scores indicating more depression), and a total score from 0 to 60. The CES-D has acceptable reliability and validity with a cut-off score of 16 for mild depressive symptoms [42] and a cut-off score of 25 for severe depressive symptoms [56]. When applied via the Internet, the CES-D appears to be a reliable and valid instrument [45].
Vitality and General Health
Two quality of life related constructs, “vitality” and “general physical health” will be measured with two scales from the Medical Outcomes Study Short Form-36 (MOS SF-36) [57]. The vitality subscale contains 4 items which are rated on a 4-point scale ranging from 1 (all the time) to 6 (never). The “perception of general health” subscale consists of 5 items which are rated on a 5-point Likert scale (1 = “exactly right” to 5 = “exactly wrong”). The MOS SF-36 has demonstrated good reliability and validity [58].
Economic Costs
The economic evaluation will be conducted from a societal perspective. It includes utilization costs of any type of health care and medicines (direct medical costs), costs incurred by the participants for travel and parking (direct non-medical costs), and costs due to production losses (indirect non-medical costs) [59,60]. All costs will be expressed in Euro (€) on an annual per capita basis for the reference year 2010. Data on direct medical and non-medical costs are obtained by using the Dutch Cost Questionnaire for Psychiatry (TIC-P) [59]. Six items from the Productivity and Disease Questionnaire (PRODISQ) will be used to measure indirect non-medical costs [61] stemming from productivity losses due to days of absence and presenteeism/inefficient job performance.
Other Variables
Participant satisfaction with the intervention will be measured with an adapted Dutch version of the Client Satisfaction Questionnaire-short form (CSQ-8) [62,63]. The internal consistency of this scale in the Dutch population is very high (Cronbach alpha =.93). The 8-item self-report questionnaire has a scale ranging from 1 to 4 and a total score range from 8 to 32.
Furthermore, participants will be asked about important life events and whether they are currently receiving treatment from a mental health specialist.
Sample Size
Depressive symptoms and well-being are used as a starting point for the power calculation. We aim to be able to show differences between Psyfit and the waiting list control condition with a standardized effect size (Cohen’s d) of 0.33 or larger. A standardized effect of 0.33 can be considered as the lower limit of a moderate clinical effect [64] and is based on a meta-analysis of well-being intervention research [35] and a recent randomized controlled trial [36]. To demonstrate this effect, and assuming an alpha of 0.05 and a statistical power (1-Beta) of 80%, we need 145 participants in each condition; therefore, we need 290 participants in total for the trial.
Analysis
Results will be reported according to the Consolidated Standards of Reporting Trials (CONSORT) statement regarding eHealth [65,66]. We will adhere to the intention-to-treat (ITT) principle, which means all participants who have been randomized will be included in the analyses. Missing data at T1 and T2 will be imputed using the expectation-maximization (EM) method, as implemented in Statistical Package for the Social Sciences (SPSS) Missing Value Analysis. The program imputes missing values by maximum likelihood estimation using the observed data in an iterative process [67]. In online trials dropout is to be expected, and sometimes a large amount of missing data has to be estimated. Although ITT analysis is the approach of choice according to the CONSORT statement, there may also be pitfalls, such as when the missing-at-random assumption is not plausible and the results of the analysis are subsequently biased [68]. Therefore, a completers-only analysis and a per-protocol analysis will be conducted in addition (sensitivity analysis). Reasons for dropout in the study will be checked at random by telephone follow-up (dropout analysis).
To examine differences between the two conditions, we will use multiple regression analyses with the clinical outcomes on continuous measures (MHC-SF, WHO-5, CES-D, and the vitality and general health scales from MOS SF-36) as dependent variables and an intervention-control group dummy as predictor variable. We will compute standardized effect sizes (Cohen’s d). Cohen’s d is computed by subtracting the mean post-test intervention score from the mean post-test control group score and dividing the difference by the pooled standard deviation [69].
Moderator analyses will be conducted to examine which groups benefit more (or less) from the intervention by regressing the outcomes on independent variables such as gender, education, mild/moderate depressive symptoms, the treatment dummy, and the interaction with the treatment dummy and the selected independent variables.
The economic evaluation will be conducted from a societal perspective, thus including the intervention costs (ie, Psyfit), the costs of health care uptake (TIC-P), the participants’ out-of-pocket costs for obtaining health care (TIC-P), and the economic costs due to productivity losses in paid work (PRODISQ). The incremental cost-effectiveness ratio (ICER) will be calculated. Uncertainty in the ICER will be captured using a bootstrap approach, producing a scatter of simulated ICERs over the ICER-plane and by drawing an ICER acceptability curve of the likelihood that Psyfit is more cost-effective for a range of willingness-to-pay (WTP) ceilings.
All analyses will be conducted using two-sided tests and alphas of .05. For this purpose, the most recent version of the SPSS software will be used.
Discussion
This online trial will examine whether an Internet-based self-help intervention for the enhancement of well-being is effective in terms of clinical outcomes and economic costs. A second objective is to examine whether certain groups benefit more or less from the intervention. The enhancement of well-being on a large scale may contribute to public mental health by resulting in better health, fewer mental disorders, and enhanced quality of life on a population level [11,70].
This study has several a priori limitations. First, dropout may occur in either of the two groups. To examine any selectiveness, we will conduct dropout analysis and a telephone survey for examining reasons for dropout. Moreover, we will conduct intention-to-treat analyses in which missing values are replaced by their most likely estimates. Second, we will only use self-report questionnaires, not formal diagnostic instruments, to establish diagnoses. Therefore, we will not know whether participants meet the criteria for a Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) diagnosis so results about prevention of mental disorders will not be available. We opted for self-rating because the intervention should be easily accessible and highly applicable because of its public nature. We don’t want to scare people off by intensive diagnostic procedures. A third limitation of this study concerns the use of questionnaires that are not (yet) validated for online purposes. Psychometric properties of online assessments may differ from their paper-and-pencil counterparts [71]. On the other hand, the CES-D [45] and the MHC-SF [52], which are used in this study, have been proven to be reliable and valid instruments even if used on the Internet. Finally, the open recruitment strategy may attract certain groups, for example, more higher-educated people or more spiritually engaged and higher-motivated people. Therefore, care must be taken in generalizing the results.
Our study also has several strengths. It is likely to add to the existing literature because it is—at least to our knowledge—the first evaluation of an online flexible and multiple-component intervention aimed at the improvement of well-being to include people with mild depressive symptoms. As such, we will be able to draw conclusions about the potential impact of such an intervention on mental health. Although the recruitment procedure could be a weakness as previously mentioned, at the same time it creates the opportunity to strengthen external validity (real world implementation potential) by analyzing which target groups are attracted by the “open access” and positively formulated recruitment strategy.
Online interactive programs may attract large numbers of people, therefore, even small or moderate effect sizes can have an impact on population health. If proven to be effective, Psyfit may be an affordable instrument that can be distributed on a large scale to enhance population well-being.
Acknowledgments
We are grateful to Jan Walburg, Jolanda Lourens, Jorne Grolleman, and Monique Hulsbergen for their help with the development of the Psyfit intervention. Also, we would like to thank Roisin de Jong for the English language edit. This study is funded by the Dutch Ministry of Health, Welfare, and Sport.
Abbreviations
- CES-D
Center for Epidemiological Studies Depression Scale
- CONSORT
Consolidated Standards for Reporting Trials
- CSQ-8
Client Satisfaction Questionnaire
- DSM-IV
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
- EM
expectation-maximization
- ICER
incremental cost-effectiveness ratio
- IP
Internet Protocol
- ITT
intention-to-treat
- METIGG
Medical Ethics Committee for Mental Health Care
- MHC-SF
Mental Health Continuum-Short Form
- MOS SF-36
Medical Outcomes Study Short Form (36 items)
- PRODISQ
Productivity and Disease Questionnaire
- SPSS
Statistical Package for the Social Sciences
- TIC-P
Trimbos Institute and Institute of Medical Technology questionnaire for Costs associated with Psychiatric illness
- WHO
World Health Organization
- WHO-5
WHO-Five Well-being Index
- WTP
willingness-to-pay
Multimedia Appendix 1
CONSORT-EHEALTH checklist (V1.6) [72].
Footnotes
Conflicts of Interest: Linda Bolier and Merel Haverman are the developers of Psyfit.nl.
Authors' Contributions: LB is the principal investigator and wrote the manuscript. MH is responsible for recruitment of participants and data collection. All authors contributed to the design of the study. EB, BB, JK, and FS are advisors in the project. HR obtained funding for the study. All authors provided comments and approved the final manuscript.
References
- 1.Bijl RV, Ravelli A, van Zessen G. Prevalence of psychiatric disorder in the general population: results of The Netherlands Mental Health Survey and Incidence Study (NEMESIS) Soc Psychiatry Psychiatr Epidemiol. 1998 Dec;33(12):587–95. doi: 10.1007/s001270050098. [DOI] [PubMed] [Google Scholar]
- 2.Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, de Girolamo G, Graaf R, Demyttenaere K, Gasquet I, Haro JM, Katz SJ, Kessler RC, Kovess V, Lépine JP, Ormel J, Polidori G, Russo LJ, Vilagut G, Almansa J, Arbabzadeh-Bouchez S, Autonell J, Bernal M, Buist-Bouwman MA, Codony M, Domingo-Salvany A, Ferrer M, Joo SS, Martínez-Alonso M, Matschinger H, Mazzi F, Morgan Z, Morosini P, Palacín C, Romera B, Taub N, Vollebergh WA, ESEMeD/MHEDEA 2000 Investigators, European Study of the Epidemiology of Mental Disorders (ESEMeD) Project Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;(420):21–7. doi: 10.1111/j.1600-0047.2004.00327.x. [DOI] [PubMed] [Google Scholar]
- 3.WHO . The global burden of disease: update 2004. Geneva: World Health Organization; 2004. [2011-02-04]. http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/index.html. [Google Scholar]
- 4.Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, de Girolamo G, Graaf R, Demyttenaere K, Gasquet I, Haro JM, Katz SJ, Kessler RC, Kovess V, Lépine JP, Ormel J, Polidori G, Russo LJ, Vilagut G, Almansa J, Arbabzadeh-Bouchez S, Autonell J, Bernal M, Buist-Bouwman MA, Codony M, Domingo-Salvany A, Ferrer M, Joo SS, Martínez-Alonso M, Matschinger H, Mazzi F, Morgan Z, Morosini P, Palacín C, Romera B, Taub N, Vollebergh WA, ESEMeD/MHEDEA 2000 Investigators, European Study of the Epidemiology of Mental Disorders (ESEMeD) Project Disability and quality of life impact of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;(420):38–46. doi: 10.1111/j.1600-0047.2004.00329.x. [DOI] [PubMed] [Google Scholar]
- 5.Smit F, Cuijpers P, Oostenbrink J, Batelaan N, de Graaf R, Beekman A. Costs of nine common mental disorders: implications for curative and preventive psychiatry. J Ment Health Policy Econ. 2006 Dec;9(4):193–200. [PubMed] [Google Scholar]
- 6.Keyes CL. Promoting and protecting mental health as flourishing: a complementary strategy for improving national mental health. Am Psychol. 2007;62(2):95–108. doi: 10.1037/0003-066X.62.2.95. [DOI] [PubMed] [Google Scholar]
- 7.Cuijpers P, Smit F. [Subclinical depression: a clinically relevant condition?] Tijdschr Psychiatr. 2008;50(8):519–28. http://www.tijdschriftvoorpsychiatrie.nl/en/tijdschrift/artikel/TVPart_1785. [PubMed] [Google Scholar]
- 8.Milczarek M, Schneider E, Eusebio RG. Stress at work - facts and figures. European Risk Observatory Report. Luxembourg: European Communities; 2009. [2011-02-04]. http://osha.europa.eu/en/publications/reports/TE-81-08-478-EN-C_OSH_in_figures_stress_at_work. [Google Scholar]
- 9.Weehuizen R. Mental Capital: The Economic Significance of Mental Health (dissertation) Maastricht: University of Maastricht; 2008. [2011-02-04]. http://www.merit.unu.edu/training/theses/Thesis_Weehuizen_final.pdf. [Google Scholar]
- 10.Walburg JA. Mentaal Vermogen -Investeren in geluk (Mental Capital - The investment in happiness) Amsterdam: Nieuw Amsterdam; 2008. [Google Scholar]
- 11.Beddington J, Cooper CL, Field J, Goswami U, Huppert FA, Jenkins R, Jones HS, Kirkwood TB, Sahakian BJ, Thomas SM. The mental wealth of nations. Nature. 2008 Oct 23;455(7216):1057–60. doi: 10.1038/4551057a. [DOI] [PubMed] [Google Scholar]
- 12.WHO . Promoting mental health: Concepts, emerging evidence, practice (summary report) Geneva: World Health Organization; 2004. [2011-02-04]. http://www.who.int/mental_health/evidence/en/promoting_mhh.pdf. [Google Scholar]
- 13.Keyes CL. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J Consult Clin Psychol. 2005 Jun;73(3):539–48. doi: 10.1037/0022-006X.73.3.539. [DOI] [PubMed] [Google Scholar]
- 14.Bergsma A, ten Have M, Veenhoven R, De Graaf R. Most people with mental disorders are happy: A 3-year follow-up in the Dutch general population. The Journal of Positive Psychology. 2011;6(4):253–59. doi: 10.1080/17439760.2011.577086. http://www.tandfonline.com/doi/abs/10.1080/17439760.2011.577086. [DOI] [Google Scholar]
- 15.Keyes CL, Grzywacz JG. Health as a complete state: the added value in work performance and healthcare costs. J Occup Environ Med. 2005 May;47(5):523–32. doi: 10.1097/01.jom.0000161737.21198.3a. [DOI] [PubMed] [Google Scholar]
- 16.Veenhoven R. Gezond geluk: Effecten van geluk op gezondheid en wat dat kan betekenen voor de preventieve gezondheidszorg (Healthy happiness: effect of happiness on health and what this could mean for preventive public health) Rotterdam: Erasmus Universiteit; 2006. [2011-02-04]. http://www2.eur.nl/fsw/research/veenhoven/Pub2000s/2005e-fulln.pdf. [Google Scholar]
- 17.Lyubomirsky S, King L, Diener E. The benefits of frequent positive affect: does happiness lead to success? Psychol Bull. 2005 Nov;131(6):803–55. doi: 10.1037/0033-2909.131.6.803. [DOI] [PubMed] [Google Scholar]
- 18.Diener E. Subjective well-being. Psychol Bull. 1984 May;95(3):542–75. [PubMed] [Google Scholar]
- 19.Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology. 1989;57:1069–1081. doi: 10.1037/0022-3514.57.6.1069. [DOI] [Google Scholar]
- 20.Fogg BJ. Persuasive Technology: Using Computers to Change What We Think and Do. San Francisco: Morgan Kaufmann; 2003. [Google Scholar]
- 21.Ritterband LM, Gonder-Frederick LA, Cox DJ, Clifton A, WEst RW, Borowitz SM. Internet interventions: In review, in use, and into the future. Professional Psychology: Research and Practice. 2003;34(5):527–534. doi: 10.1037/0735-7028.34.5.527. [DOI] [Google Scholar]
- 22.Smit F, Riper H. E-mental health: presence and future -factsheet. Utrecht: Trimbos-instituut; 2008. [2011-02-04]. http://www.icom.trimbos.nl/documents/downloads/factsheet%20e-mental%20health%20(I.COM).pdf. [Google Scholar]
- 23.Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med. 2007 Aug;37(3):319–28. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- 24.Spek V, Cuijpers P, Nyklicek I, Smiths N, Riper H, Keyzer J, Pop V One-year follow-up results of a randomized controlled clinical trial on Internet-based cognitive behavioural therapy for subthreshold depression in people over 50 years. Psychol Med. 2007 Mar;38(5):635–39. doi: 10.1017/S0033291707002590. [DOI] [PubMed] [Google Scholar]
- 25.Warmerdam L, van Straten A, Twisk J, Riper H, Cuijpers P. Internet-based treatment for adults with depressive symptoms: randomized controlled trial. J Med Internet Res. 2008;10(4):e44. doi: 10.2196/jmir.1094. http://www.jmir.org/2008/4/e44/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Straten A, Cuijpers P, Smits N. Effectiveness of a web-based self-help intervention for symptoms of depression, anxiety, and stress: randomized controlled trial. J Med Internet Res. 2008;10(1):e7. doi: 10.2196/jmir.954. http://www.jmir.org/2008/1/e7/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Emmons RA, McCullough ME. Counting blessings versus burdens: an experimental investigation of gratitude and subjective well-being in daily life. J Pers Soc Psychol. 2003 Feb;84(2):377–89. doi: 10.1037//0022-3514.84.2.377. [DOI] [PubMed] [Google Scholar]
- 28.Seligman ME, Steen TA, Park N, Peterson C. Positive psychology progress: empirical validation of interventions. Am Psychol. 2005;60(5):410–21. doi: 10.1037/0003-066X.60.5.410. [DOI] [PubMed] [Google Scholar]
- 29.Sheldon KM, Lyubomirsky S. How to increase and sustain positive emotion: The effects of expressing gratitude and visualizing best possible selves. The Journal of Positive Psychology. 2006;1:73–82. doi: 10.1080/17439760500510676. [DOI] [Google Scholar]
- 30.Lyubomirsky S, Sheldon KM, Schkade D. Pursuing Happiness: The Architecture of Sustainable Change. Review of General Psychology. 2005;9:111–131. doi: 10.1037/1089-2680.9.2.111. [DOI] [Google Scholar]
- 31.Otake K, Shimai S, Tanaka-Matsumi J, Otsui K, Fredrickson BL. Happy people become happier through kindness: A counting kindnesses intervention. J Happiness Stud. 2006 Sep;7(3):361–375. doi: 10.1007/s10902-005-3650-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sheldon KM, Kasser T, Smith K, Share T. Personal goals and psychological growth: testing an intervention to enhance goal attainment and personality integration. J Pers. 2002 Feb;70(1):5–31. doi: 10.1111/1467-6494.00176. [DOI] [PubMed] [Google Scholar]
- 33.Green LS, Oades LG, Grant AM. Cognitive-behavioral, solution-focused life coaching: Enhancing goal striving, well-being, and hope. The Journal of Positive Psychology. 2006;1:142–149. doi: 10.1080/17439760600619849. [DOI] [Google Scholar]
- 34.Spence GB, Grant AM. Professional and peer life coaching and the enhancement of goal striving and well-being: An exploratory study. The Journal of Positive Psychology. 2007;2:185–194. doi: 10.1080/17439760701228896. [DOI] [Google Scholar]
- 35.Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J Clin Psychol. 2009 May;65(5):467–87. doi: 10.1002/jclp.20593. [DOI] [PubMed] [Google Scholar]
- 36.Mitchell J, Stanimirovic R, Klein B, Vella-Brodrick D. A randomised controlled trial of a self-guided internet intervention promoting well-being. Computers in Human Behavior. 2009;25(3):749–760. doi: 10.1016/j.chb2009.02.03. http://dl.acm.org/citation.cfm?id=1534990. [DOI] [Google Scholar]
- 37.Abbott JA, Klein B, Hamilton C, Rosenthal A. The impact of online resilience training for sales managers on wellbeing and performance. E-Journal of Applied Psychology. 2009;5(1):89–95. http://ojs.lib.swin.edu.au/index.php/ejap/article/view/145. [Google Scholar]
- 38.Parks-Sheiner AC. Positive psychotherapy: Building a model of empirically supported self-help. Cambridge: ProQuest Dissertation Publishing; 2009. [Google Scholar]
- 39.psyfit.nl. [2012-01-27]. http://www.psyfit.nl/
- 40.Lyubomirsky S. The how of happiness: A practical approach to getting the life you want. New York: Penguin; 2008. [Google Scholar]
- 41.Bergsma A. Do self-help books help? Journal of Happiness Studies. 2007;9(3):341–360. doi: 10.1007/s10902-006-9041-2. [DOI] [Google Scholar]
- 42.Haringsma R, Engels GI, Beekman AT, Spinhoven P. The criterion validity of the Center for Epidemiological Studies Depression Scale (CES-D) in a sample of self-referred elders with depressive symptomatology. Int J Geriatr Psychiatry. 2004 Jun;19(6):558–63. doi: 10.1002/gps.1130. [DOI] [PubMed] [Google Scholar]
- 43.Keyes CL, Shmotkin D, Ryff CD. Optimizing well-being: the empirical encounter of two traditions. J Pers Soc Psychol. 2002 Jun;82(6):1007–22. [PubMed] [Google Scholar]
- 44.Westerhof GJ, Keyes CLM. Maandblad Geestelijke Gezondheid(63):808-820. 2008. [2012-04-21]. Geestelijke gezondheid is meer dan de afwezigheid van ziekte (Mental health is more then the absence of disease) http://mgv.boomtijdschriften.nl/artikelen/GV-63-10-808_Geestelijke%20gezondheid%20is%20meer%20dan%20de%20af.html.
- 45.Donker T, van Straten A, Marks I, Cuijpers P. Brief self-rated screening for depression on the Internet. J Affect Disord. 2010 May;122(3):253–9. doi: 10.1016/j.jad.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 46.Notenboom M, Van Male J. Positive mental health - Resultaten naar aanleiding van een verkennend onderzoek, intern rapport (Positive mental health - results of a exploratory focus group study - internal report) Amsterdam: Markt- en communicatieonderzoek Ferro; 2008. [Google Scholar]
- 47.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res. 2004 Jul;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 48.Riper H, Kramer J. Kleur je leven - internettherapie preventie van depressie (Color Your life - internettherapie for the prevention of depression) Utrecht: Trimbos-instituut; 2007. [2011-02-04]. https://www.kleurjeleven.nl/ [Google Scholar]
- 49.CuijpersP . Everything under control - problem solving therapy at the internet. Amsterdam: VU University Amsterdam; 2005. [2011-02-04]. Everything under control - problem solving therapy at the internet https://www.allesondercontrole.nu/portal/ [Google Scholar]
- 50.Christensen H, Griffiths KM, Farrer L. Adherence in internet interventions for anxiety and depression. J Med Internet Res. 2009;11(2):e13. doi: 10.2196/jmir.1194. http://www.jmir.org/2009/2/e13/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Keyes CL. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. 2002 Jun;43(2):207–22. [PubMed] [Google Scholar]
- 52.Lamers SM, Westerhof GJ, Bohlmeijer ET, ten Klooster PM, Keyes CL. Evaluating the psychometric properties of the Mental Health Continuum-Short Form (MHC-SF) J Clin Psychol. 2011 Jan;67(1):99–110. doi: 10.1002/jclp.20741. [DOI] [PubMed] [Google Scholar]
- 53.Bech P. Measuring the dimension of psychological general well-being by the WHO-5. Quality of Life Newsletter. 2004;32:15–16. [Google Scholar]
- 54.Henkel V, Mergl R, Kohnen R, Maier W, Möller HJ, Hegerl U. Identifying depression in primary care: a comparison of different methods in a prospective cohort study. BMJ. 2003 Jan 25;326(7382):200–1. doi: 10.1136/bmj.326.7382.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 56.Beekman AT, Deeg DJ, Van Limbeek J, Braam AW, De Vries MZ, Van Tilburg W. Criterion validity of the Center for Epidemiologic Studies Depression scale (CES-D): results from a community-based sample of older subjects in The Netherlands. Psychol Med. 1997 Jan;27(1):231–5. doi: 10.1017/s0033291796003510. [DOI] [PubMed] [Google Scholar]
- 57.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992 Jun;30(6):473–83. [PubMed] [Google Scholar]
- 58.Brazier JE, Harper R, Jones NM, O'Cathain A, Thomas KJ, Usherwood T, Westlake L. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992 Jul 18;305(6846):160–4. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hakkaart-van Roijen L, van Straten A, Donker M. Trimbos/iMTA questionnaire for costs associated with psychiatric illness (TIC-P) Rotterdam: iMTA; 2002. [2011-02-04]. http://publishing.eur.nl/ir/repub/asset/1337/bmgimt20020711143439.pdf. [Google Scholar]
- 60.Hakkaart-van Roijen L, Tan SS, Bouwmans CAM. Handleiding voor kostenonderzoek - methoden en standaard kostprijzen voor economische evaluaties in de gezondheidszorg (Manual for costing research - in Dutch, actualized version 2010) Rotterdam: Institute for Medical Technology Assessment, Erasmus University; 2010. [2011-02-11]. http://www.cvz.nl/binaries/content/documents/cvzinternet/nl/documenten/rubriek+zorgpakket/cfh/handleiding-kostenonderzoek-2010.pdf. [Google Scholar]
- 61.Koopmanschap MA. PRODISQ: a modular questionnaire on productivity and disease for economic evaluation studies. Expert Rev Pharmacoecon Outcomes Res. 2005 Feb;5(1):23–8. doi: 10.1586/14737167.5.1.23. [DOI] [PubMed] [Google Scholar]
- 62.de Brey H. A cross-national validation of the client satisfaction questionnaire: the Dutch experience. Eval Program Plann. 1983;6(3-4):395–400. doi: 10.1016/0149-7189(83)90018-6. [DOI] [PubMed] [Google Scholar]
- 63.Nguyen TD, Attkisson CC, Stegner BL. Assessment of patient satisfaction: development and refinement of a service evaluation questionnaire. Eval Program Plann. 1983;6(3-4):299–313. doi: 10.1016/0149-7189(83)90010-1. [DOI] [PubMed] [Google Scholar]
- 64.Lipsey MW. Design sensitivity: statistical power for experimental research. Newbury Park, Calif.: Sage Publications; 1990. [Google Scholar]
- 65.Altman DG. Better reporting of randomised controlled trials: the CONSORT statement. BMJ. 1996 Sep 7;313(7057):570–1. doi: 10.1136/bmj.313.7057.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Eysenbach G, CONSORT-EHEALTH Group CONSORT-EHEALTH: improving and standardizing evaluation reports of Web-based and mobile health interventions. J Med Internet Res. 2011;13(4):e126. doi: 10.2196/jmir.1923. http://www.jmir.org/2011/4/e126/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dempster AP, Laird NM. Rubin DB: Maximum Likelihood from Incomplete Data via the EM Algorithm. Journal of the Royal Statistical Society Series B (Methodological) 1977;39(Suppl 1):1–38. doi: 10.2307/2984875. [DOI] [Google Scholar]
- 68.Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, N.J.: L. Erlbaum Associates; 1988. [Google Scholar]
- 70.Veenhoven R. Positive psychology in practice. Hoboken, N.J.: Wiley; 2004. Happiness as an aim in public policy: The greatest happiness principle. [Google Scholar]
- 71.Buchanan T. Online assessment: Desirable or dangerous? Professional Psychology: Research and Practice. 2002;33(2):148–154. doi: 10.1037/0735-7028.33.2.148. [DOI] [Google Scholar]
- 72.Eysenbach G, CONSORT-EHEALTH Group CONSORT-EHEALTH: improving and standardizing evaluation reports of Web-based and mobile health interventions. J Med Internet Res. 2011;13(4):e126. doi: 10.2196/jmir.1923. http://www.jmir.org/2011/4/e126/ [DOI] [PMC free article] [PubMed] [Google Scholar]