Abstract
In total hip arthroplasty (THA), combined anteversion (CA), the sum of cup anteversion (AV) and stem antetorsion (AT) are used as parameters to assess the appropriateness of overall prosthetic alignment. In this study, we evaluated the CA value based on the post-operative computed tomography (CT) measurements in our patient population who underwent THA using the OrthoPilot™ image-free navigation system (B/BRAUN-Aesculap, Tuttlingen, Germany). During surgery, cup alignment was adjusted with the use of the navigation system while the positioning of the femoral stem was arbitrarily adjusted by the surgeon. Seventy-nine THAs were included in the study. Post-operative CT assessment for the prosthetic alignment showed the average cup inclination and AV values to be 40.5°±4.1° and 20.6°±4.6°, respectively, demonstrating the effectiveness of the navigation system by small values of standard deviation. By contrast, the AT value measured for the stem showed wide variability (mean 23.6°±11.2°). Consequently, the resulting CA was also inconsistent (mean 44.4°±11.2°) and only 61 of the 79 THAs (77.2%) were defined as satisfactory.
Key words: combined anteversion, THA, image free navigation.
Introduction
Implant positioning is one of the critical factors influencing the post-operative outcome in total hip arthroplasty (THA). Malpositioning of the implant may lead to an increased risk of post-operative complications such as dislocation, restricted range of motion, polyethylene wear, and loosening. Impingement of the prosthetic femoral neck on the polyethylene cup liner occurring in hip motion can be a causative factor leading to those complications. Therefore, accurate and consistent prosthetic positioning is critical for preventing impingement phenomenon and achievement of implant longevity.
As far as the target of implant positioning to be aimed for during THA procedure is concerned, there have been a number of studies proposing optimal alignment of the acetabular cup. Lewinnek defined the safe zone of the cup alignment as 40°±10° of inclination and 15°±10° of anteversion (AV).1 He showed that the placement of the cup outside of this zone resulted in more than a 4-fold increase in the post-operative dislocation rate. Biedermann reported that AV of 15° and inclinations of 45° were associated with the lowest risk for dislocation.2 Wixson proposed a strict target zone of the cup positioning with inclination of 40–45° and AV of 17–23° in navigated THA performed through the posterior approach.3
By contrast, only a few studies have dealt with optimization of the prosthetic alignment on the femoral side. Recently, the concept of combined anteversion (CA), the sum of acetabular AV and femoral antetorsion (AT), have been proposed as parameters to assess the appropriateness of the overall prosthetic alignment. McKibbin first introduced this concept based on the results of anatomical studies of infant cadavers,4 and showed that the physiological CA ranged from 30–40°. In THA, CA is utilized as an indicator of overall rotational positioning of the implants. Yoshimine and Widmer attempted to determine the optimal CA using computer simulations. 5,6 They proposed formulas to identify the new safe zone value to achieve essential range of motion while avoiding prosthetic impingement.
In our clinical practice, we have been using an image-free THA navigation system (Orthopilot™; B/BRAUN-Aesculap, Germany) to ensure accurate and reproducible acetabular cup alignment. The effectiveness of this system in our clinical experience has been confirmed and reported in previous clinical studies.7–9 However, this system is not equipped with a tool to evaluate and control torsion of the stem. Consequently, the stem AT was determined arbitrarily by the surgeon and, therefore, the resultant CA value in our navigated THA can vary.
The purpose of this study was to evaluate the CA in our initial series of image-free navigated THA and examine the validity of the hypothesis that the CA value may not be consistent without the systemic control of stem AV.
Materials and Methods
Patients
From January 2006 to December 2010, 207 THAs were performed with the OrthoPilot™ image-free navigation system (B/Braun-Aesculap, Germany). In the initial case series, we performed post-operative computed tomography (CT) examination for the acetabular side alone, and thus stem AT was not evaluated. Among the total of 207 cases, 93 patients during the latter study period underwent CT evaluation from the level of the pelvis to the posterior femoral condyles for additional evaluation of femoral stem antetorsion. These 93 patients made up the basis of the study population; 14 patients with the prosthetic alignment intentionally set outside the optimal range were excluded from the study. The reasons for this adjustment were: 9 patients with severe posterior pelvic tilt requiring intentionally decreased cup anteversion and 5 patients with femoral neck or proximal femoral canal deformity combined with excessive femoral AT. The remaining 79 navigated THAs were included and evaluated in this study.
Surgical procedure
Surgeries were performed using the same techniques for all patients by either of the 2 senior authors (SF and TF). We used a modified Hardinge (MIS) approach with a skin incision of 8 cm or less with the patient in a lateral position. All hips were implanted with a cementless cup (Plasma cup B™, B/Braun-Aesculap, Germany) and a cementless stem (Bicontact™, B/Braun-Aesculap, Germany). This stem is designed to have a flat, square crosssection enabling some allowance for rotational adjustment. For the cup positioning, inclination and AV angles were targeted at 40–45° and 15–20°, respectively, using navigation. The stem AT was arbitrarily adjusted under manual control.
Post-operative evaluation
All included patients underwent post-operative CT (Somatom; Siemens, Munich, Germany) scan from the level of the pelvis to the posterior femoral condyles, and the cup and stem position and alignment were assessed on the CT images. The CT data were transferred as DICOM files to a desktop computer. The software used was developed for the pre-operative 3D-Template system (3D-Template Ver.3.2, Japan Medical Materials Corporation, Japan) for specifying 3-dimensional coordinates and assessing the post-operative cup and stem orientation. During the calculation of the angles for prosthetic alignment, anatomical angles obtained from CT measurement were converted to the angle of radiological definition.10 Parameters adopted for the analysis were: X-ray cup inclination (RI), X-ray cup AV, and stem AT. AT was defined as the angle formed between the proximal femoral stem axis and the line connecting the bilateral posterior femoral condyler margin on the axial plane. The CA value was calculated by summing the AV and AT angles. Furthermore, we applied these parameters to the mathematical formula of Widmer (Widmer's CA = cup AV + 0.7 stem AT) and compared the resulting values with the target value of their formula (37.3°).6 In the assessment of the appropriateness of the overall alignment, the calculated Widmer's CA values of 37°±10° was regarded as satisfactory.6
Study design was approved by the Institutional Review Board and informed consent was obtained from each participant.
Statistical analysis
For comparison between the intra- and postoperative values, Wilcoxon's signed rank test was used to assess any difference. P<0.05 was considered significant.
Results
During the post-operative course, no dislocation or major complications were encountered in this series.
In the intra-operative evaluation using navigation, the mean RI and AV were 38.8±3.1° (range 34.0–46.1°) and 17.0±3.4° (range 8.3–24.6°), respectively, after the final implantation. Corresponding values determined by post-operative CT evaluation were 40.5°±4.1° (range 30.4–49.2°) and 20.6°±4.6° (range 8.7–32°), respectively. Consequently, the values obtained from both intra- and post-operative assessments, in general, agreed well. When the comparison between the two measurements was made for each patient, however, both RI and AV calculated from post-operative CT data were significantly higher than the intra-operative navigation values (P<0.05). Additionally, in the assessment of the cup positioning based on the Lewinnek's safe zone criteria,1 72 cases (91.1%) fell within this range (Figure 1).
Figure 1.
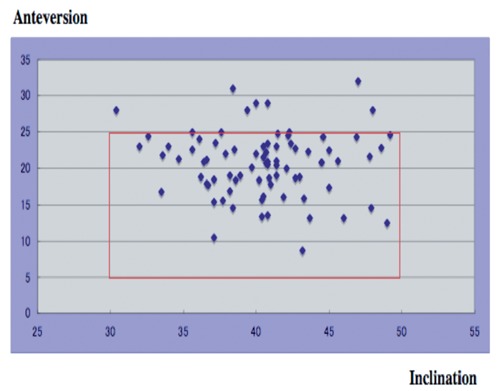
Scatter plots showing anteversion and X-ray inclination of the cup. Post-operative cup anteversion and inclination in each patient are presented by a dot. Range of Lewineck's safe zone is shown by the solid square. Cup alignment in 72 cases (91.1%) fell within Lewinnek's safe zone.
By contrast, distribution of the AT and CA values were scattered, as shown by large SD values. The measured AT and CA values averaged 23.6°±11.2° (range 2–45°) (Figure 2) and 44.4°±11.2° (range 23.0–65°), respectively (Figure 3). In addition, the average Widmer's CA value was 37.2°±8.2° (range 21.6–55.1°).6 In the assessment of the appropriateness of overall alignment, the Widmer's CA of 61 THAs (77.2%) was within the satisfactory range (37°±10°) in their definition,6 while the remaining 18 THAs (23.8%) fell into the less optimal category (Figure 4).
Figure 2.
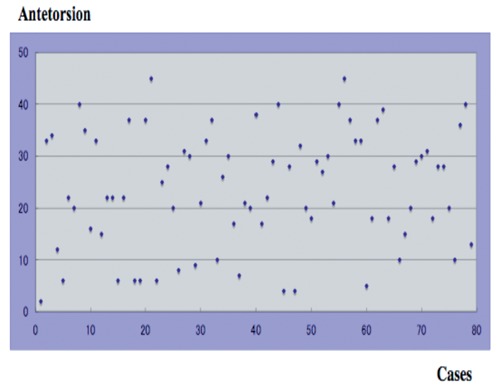
Scatter plots showing stem antetorsion. Distribution of antetorsion values were scattered as shown by large standard deviation values (range 2–45°).
Figure 3.
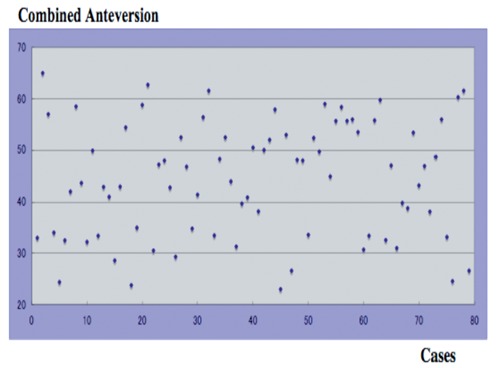
Scatter plots showing combined anteversion. Distribution of combined anteversion values were scattered as shown by large standard deviation values (range 23.0–65°).
Figure 4.
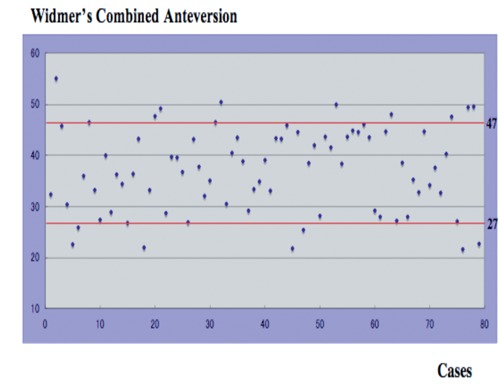
Scatter plots showing Widmer's combined anteversion. The two solid lines indicate the satisfactory range: 37°±10° (27° and 37°). The combined anteversion values in 61 cases (77.2%) were within this satisfactory range, while the corresponding values in the remaining 18 total hip arthroplasties (23.8%) fell into the less optimal category.
Discussion
Implant-on-implant impingement and dislocation are among the major complications following THA that may lead to clinical failure and the need for revision surgery. Achievement of optimal implant positioning is critical for prevention of these complications. When optimizing prosthetic alignment, the rotational alignment of both acetabular and femoral implants should be taken into consideration.
In the majority of previous clinical studies dealing with this subject, however, only cup positioning was discussed without referring to the stem AT. The accuracy of the image-free THA cup navigation system has been assessed and reported in several clinical studies and satisfactory agreement between the intra-operative navigation results and the post-operative values obtained from X-rays have been reported.11–15 In our previous studies,7,8 we also reported satisfactory results with cup setting angle with the use of the image-free navigated THA. However, we did not look into stem AT and CA in our initial reports. Ranawat et al.16 addressed the significance of CA and proposed that CA values should be within the range of 25° to 35° in men, and 25° to 45° in women to avoid problems caused by inappropriate prosthetic alignment. Jolles raised multiple predisposing factors for dislocation after THA procedure,17 and showed that the dislocation rate increased 6.9 times when the CA value was outside the range of 40° and 60°. Regarding the theoretical analysis, there have been several computer simulation studies investigating the appropriate CA range to avoid implant-on-implant impingement.5,6,18,19 Based on the results of the computerized 3-D model analysis, Widmer et al.6 claimed that an optimal combination for positioning of both components was 20–28° of AV and 40–45° of inclination. In addition, they proposed the formula (cup AV + 0.7 stem AT) to calculate the CA value and defined the ideal value to be 37.3°. Yoshimine et al.5 conducted similar computerized simulation studies using more critical criteria. They proposed that the formula that the sum of the cup AV, plus 0.8 times the stem AT, plus the cup inclination should be 90.8° (AV + 0.8AT + RI = 90.8). More recently, Hisatome et al.18 proposed another formula indicating that the sum of the cup AV plus 0.7 times the stem AT should be 42° (AV + 0.7AT = 42°) with a cup inclination of 45° and a head diameter of more than 32 mm. These authors also recommended the optimal value for each angle to be RI 45°, cup AV 25° and stem AT 25°.
In the present series, the measured cup RI and AV averaged 40.5°±4.1° and 20.6°±4.6°, respectively. As shown by the small SD values, the cup positioning could be well controlled. By contrast, the stem AT was arbitrarily adjusted according to the surgeon's judgement and, therefore, the stem AT averaged 23.6°±11.2° (range 2–45°) indicating a large SD. Consequently, the resultant CA (cup AV + stem AT) was also variable, and CA values in 44 hips (43%) were classified into the risky range (<40° or >60°) for dislocation as proposed by Jolles et al.17 Therefore, we could not achieve consistent results of CA when implanted with image-free cup navigation system that was not equipped with stem navigation. The inconsistent AT in the current THA procedure has also been shown in several previous follow-up studies. Wassilew et al.20 reported that post-operative AT measurement for the femoral stem inserted without navigation showed a wide range (−5° to 39°), while Sendter et al.21 and Wine et al.22 evaluated the AT on post-operative CT images and similarly reported wide variability in the measured values (−19° to 33° and −15° to 45°, respectively). The AT cannot be well controlled only on the basis of the anatomy of the proximal femur because of the individual differences to be found between patients. This is especially true when the anatomical fit and fill type stem in cementless THA is adopted.23 With regards to the individual differences in the native femoral AT, Husmann et al.24 measured the femoral AT in 300 patients with primary osteoarthritis before THA, and reported that the native femoral AT in this patient population ranged from 0.29° to 44.5° (SD 8.7°). Sugano et al.25 also reported wide variation in these values ranging from 0° to 50° based on measurements on 3-D CT images. In order to achieve better adjustment for CA values, Amuwa et al.26 and Dorr et al.27 proposed a combined anteversion technique. They recommended preparing the femur and estimating the stem AT with the trial implant prior to the acetabular preparation. The cup AV can then be determined based on the estimated stem AT value. In our navigated THA procedure, the femoral implant design is a Bicontact stem that possesses a flat, square crosssection configuration allowing some rotational adjustment. This adjustability can be further enhanced with adoption of cemented stem fixation. Based on our clinical experiences with the image-free navigated THA, we have designed a novel AT guide to enable intra-operative stem AT assessment. Currently, we are using this AT guide along with the new-version navigation system that can measure stem AT. Consequently, improved accuracy in adjustment of the stem AT and the resultant CA value can be achieved in our current procedure. In this second series of THA, we have not experienced dislocation or early implant failure. However, a long-term follow-up study for this cohort of patients and a comparison of outcomes between the initial and subsequent series will be required in order to validate our modified procedure.
Conclusions
We evaluated the CA value based on the postoperative CT measurement in our patient population who underwent THA using the OrthoPilot™ image-free cup navigation system without stem navigation. Post-operative CT assessment for the prosthetic alignment showed the average cup inclination and AV values to be 40.5°±4.1° and 20.6°±4.6°, respectively, demonstrating effectiveness of the navigation system by small SD values. By contrast, the AT values measured for the stems showed wide variability (mean 23.6°±11.2°). Consequently, the resultant CA was also inconsistent (mean 44.4°±11.2°) and only 61 of the 79 THAs (77.2%) were defined as satisfactory. It is thought that accuracy and consistency in CA adjustment cannot be accomplished with the use of the navigation system for acetabular side alone.
References
- 1.Lewinnek GE, Lewis JL, Tarr R, et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–20. [PubMed] [Google Scholar]
- 2.Biedermann R, Tonin A, Krismer M, et al. Reducing the risk of dislocation after total hip arthroplasty. The effect of orientation of the acetabular component. J Bone Joint Surg Br. 2005;87B:762–9. doi: 10.1302/0301-620X.87B6.14745. [DOI] [PubMed] [Google Scholar]
- 3.Wixson RL, MacDonald MA. Total hip arthroplasty through a minimal posterior appro-ach using imageless computer–assisted hip navigation. J Arthroplasty. 2005;20:51–6. doi: 10.1016/j.arth.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 4.McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br. 1970;52:148–59. [PubMed] [Google Scholar]
- 5.Yoshimine F. The safe-zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements. J Biomech. 2006;39:1315–23. doi: 10.1016/j.jbiomech.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–21. doi: 10.1016/j.orthres.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 7.Fukunishi S, Fukui T, Imamura F, et al. Assessment of accuracy of acetabular cup orientation in CT-free navigated total hip arthroplasty. Orthopaedics. 2008;31:987–987. [PubMed] [Google Scholar]
- 8.Fukui T, Fukunishi S, Nishio S, et al. Use of image-free navigation in determination of acetabular cup orientation: analysis of factors affecting precision. Orthopedics. 2010;33:38–42. doi: 10.3928/01477447-20100510-61. [DOI] [PubMed] [Google Scholar]
- 9.Nishio S, Fukunishi S, Fukui T, et al. Adjustment of leg length using imageless navigation THA software without a femoral tracker. J Orthop Sci. 2011;16:171–6. doi: 10.1007/s00776-011-0038-2. [DOI] [PubMed] [Google Scholar]
- 10.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–32. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 11.Dorr LD, Hishiki Y, Wan Z, et al. Development of imageless computer navigation for acetabular component position in total hip replacement. Iowa Orthop J. 2005;25:1–9. [PMC free article] [PubMed] [Google Scholar]
- 12.Kiefer H. OrthoPilot cup navigation - how to optimise cup positioning? Int Orthop. 2003;27:37–42. [PubMed] [Google Scholar]
- 13.Kiefer H, Othman A. OrthoPilot total hip arthroplasty workflow and surgery. Orthopedics. 2005;28:1221–6. doi: 10.3928/0147-7447-20051002-04. [DOI] [PubMed] [Google Scholar]
- 14.Lazovic D, Kaib N. Results with navigated bicontact total hip arthroplasty. Orthopedics. 2005;28:1227–33. doi: 10.3928/0147-7447-20051002-05. [DOI] [PubMed] [Google Scholar]
- 15.Najarian BC, Kilgore JE, Markel DC. Evaluation of component positioning in primary total hip arthroplasty using an imageless navigation device compared with traditional methods. J Arthroplasty. 2009;24:15–21. doi: 10.1016/j.arth.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Ranawat CS, Maynard MJ. Modern techniques of cemented total hip arthroplasty. Tech Orthop. 1991;6:17–25. [Google Scholar]
- 17.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty. J Arthroplasty. 2007;17:282–8. doi: 10.1054/arth.2002.30286. [DOI] [PubMed] [Google Scholar]
- 18.Hisatome T, Doi H. theoretically optimum position of the prosthesis in total hip arthroplasty to fulfill the severe range of motion criteria due to neck impingement. J Orthop Sci. 2011;16:229–37. doi: 10.1007/s00776-011-0039-1. [DOI] [PubMed] [Google Scholar]
- 19.Barsoum WK, Patterson RW, Higuera C, et al. A computer model of the position of the combined component in the prevention of impingement in total hip replacement. J Bone Joint Surg Br. 2007;89B:839–45. doi: 10.1302/0301-620X.89B6.18644. [DOI] [PubMed] [Google Scholar]
- 20.Wasssilew GI, Perka C, Koenig K, et al. 3D CT analysis of combined cup and stem anteversion in case of cup navigation hip arthroplasty. Orthopedics. 2010;33:48–51. doi: 10.3928/01477447-20100510-53. [DOI] [PubMed] [Google Scholar]
- 21.Sendtner E, Tibor S, Winkler R, et al. Stem torsion in total hip replacement. CT measurements in 60 patients. Acta Ortopaedica. 2010;81:579–82. doi: 10.3109/17453674.2010.524596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wines AP, McNicol D. Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty. 2006;21:696–701. doi: 10.1016/j.arth.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 23.Bargar WL, Jamali AA, Najad AH. Femoral anteversion in THA and its lack of correction with native acetabular anteversion. Clini Ortop Relat Res. 2010;468:527–32. doi: 10.1007/s11999-009-1040-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Husmann O, Rubin PJ, Leyvraz PF, et al. Three-dimensional morphology of the proximal femur. J Arthroplasty. 1997;12:444–50. doi: 10.1016/s0883-5403(97)90201-1. [DOI] [PubMed] [Google Scholar]
- 25.Sugano N, Noble PC, Kamaric E. A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr. 1998;22:610–4. doi: 10.1097/00004728-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 26.Amuwa C, Dorr LD. The combined anteversion technique for acetabular component anteversion. J Arthroplasty. 2008;23:1068–70. doi: 10.1016/j.arth.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 27.Dorr LD, Malik A, Dastane M, Wan Z. Combined anteversion technique for total hip arthroplasty. Clini Ortop Relat Res. 2009;467:119–27. doi: 10.1007/s11999-008-0598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


