Abstract
Objective
To understand what motivates primary care practices to engage in practice improvement, identify external and internal facilitators and barriers, and refine a conceptual framework.
Data Sources
In-depth interviews and structured telephone surveys with clinicians and practice staff (n = 51), observations, and document reviews.
Study Design
Comparative case study of primary care practices (n = 8) to examine aspects of the practice and environment that influence engagement in improvement activities.
Data Collection Methods
Three on-site visits, telephone interviews, and two surveys.
Principal Findings
Pressures from multiple sources create conflicting forces on primary care practices' improvement efforts. Pressures include incentives and requirements, organizational relationships, and access to resources. Culture, leadership priorities, values set by the physician(s), and other factors influence whether primary care practices engage in improvement efforts.
Conclusions
Most primary care practices are caught in a cross fire between two groups of pressures: a set of forces that push practices to remain with the status quo, the “15-minute per patient” approach, and another set of forces that press for major transformations. Our study illuminates the elements involved in the decision to stay with the status quo or to engage in practice improvement efforts needed for transformation.
Keywords: Primary care, practice transformation, quality improvement, qualitative research
Why do some primary care practices manage to transform themselves into new models of health care delivery whereas others do not? This is the central question of our research because the quality of care received by many Americans is often suboptimal (Schoen et al. 2007; Anderson and Marcovich 2010). Quality issues plaguing primary care include patients' lack of access to services (Huynh et al. 2006), inconsistencies in providing evidence-based medicine (Grol and Grimshaw 2003; McGynn et al. 2003), poor coordination of care across health system components (MacKinney, Ullrich, and Mueller 2011), and complexity involved in caring for individuals with chronic illnesses (Von Korff et al. 1997). Recognizing this problem, the Affordable Care Act emphasizes patient-centered care that is reliable, accessible, and safe; improves the health of the population; and reduces costs to deliver care. Primary care transformation is seen as a key element in meeting these goals. Knowing which practices have adopted new primary care approaches, like the patient-centered medical home (PCMH) model, and contrasting them with those that have not is an important step toward knowing which policies to select to remedy the overall capabilities of primary care delivery. Thus, in this study we differentiate between primary care practices that are and are not transforming to deliver evidence-based medicine, implementing new models of care delivery such as the PCMH, improving transparency through performance measurement and reporting, and creating strategic alliances for advanced integrated care models like accountable care organizations (ACOs).
Pressures external to the organization that favor these transformations come via pay-for-performance (P4P) compensation methods, public reporting of performance, government requirements for adoption and meaningful use of electronic health records (EHRs), board recertification processes, and increased expectations from patients and other stakeholder groups. However, primary care practices also experience pressures not to change. For example, payment systems encourage high volume and episodic care, which runs counter to key features of the PCMH and ACO models. Primary care practices are therefore caught in a cross fire of contradictory forces.
Recent literature has identified various internal and external factors that may influence practices' ability to transform (Milstein and Gilbertson 2009). Adoption of PCMH components was greatest for large medical groups and for those owned by large health systems—all more likely to have greater resources (Rittenhouse et al. 2008; Goldberg and Mick 2010). The National Demonstration Project identified access to resources as a facilitator of practice transformation, as well as having a supportive infrastructure and management model, facilitative leadership, and an empowering and responsive culture (Nutting et al. 2010). Wise et al. (2011) found that transformation to PCMHs correlated with perceived value of the change, understanding PCMH requirements, leadership and staff commitment, and financial incentives. Reid et al. (2011) reported lack of financial incentives as the primary reason why residency practices discontinued transformation efforts. Fernald et al. (2011) found that embedded culture from historical events, such as previous failed attempts at transformation, a lack of meeting structure, and lack of participation by key practice members influenced practices' ability to transform. They also identified barriers to practice transformation, including a lack of support by leadership and affiliated organizations, and nonsupportive organizational structures and processes. Although these studies present various influences on practice transformation, they do not provide an exploration of both pressures and internal practice characteristics affecting change. The present study begins to fill this gap.
There are three critical aspects of current practice transformation efforts (Hoff 2010). First, is added payment for care coordination or case management to break the cycle of “15-minute medicine” caused by volume-driven fee-for-service reimbursement. Second is a “minimum level” of health information technology (HIT) capacity in every practice. And, third, is the transformation of existing patient care and administrative work into team-based care models, in which physicians become team leaders and nurses have increased roles and responsibilities for patient care. The problem is that:
It cannot nor should it be expected that after a decade or more of forcing PCPs [primary care physicians] to practice in an assembly-line-like manner provides an immediately favorable environment for practices to innovate…. PCP mindsets are attuned to the demands of high-volume medicine. (Hoff 2010, p. 181)
Given forces arrayed against practice transformation efforts, our basic question was what enables a practice to transform itself. Building on previous research was another goal of our study. Our aim was to gain additional knowledge from in-depth case studies to develop a framework explaining the mechanisms of influence and contextual modifiers on performance improvement in physician practices. We studied physician practices in their natural environment to understand performance improvement efforts or their lack and real-life complications, issues, and solutions.
Methods
We used a grounded theory approach in this research (Glaser and Strauss 1967), which involved theoretical sampling, in-depth data collection, identification of recurring themes and concepts, and development of a conceptual framework. The resulting framework was based on study themes and their interrelationships that were linked to previous studies and relevant theories.
Study Design and Sample
This research was a comparative case study of small primary care practices in Virginia. We conducted an in-depth examination of performance improvement activities, internal and external factors that influence practices, physician and staff desired improvement efforts, and facilitators and barriers of engaging in these efforts. We identified eight practices for study participation based on a previous survey of family medicine practices (Goldberg and Kuzel 2009). A purposeful sampling approach was used to select practices based on a maximum variation in the following characteristics: performance improvement activities (e.g., team-based care, performance measurement), location (rural/nonrural), and ownership form (independent vs. owned and operated by a larger system). A comparative case study approach (Stake 2006) enabled us to identify practice characteristics, environmental elements, and other attributes that distinguish practices that have aligned themselves with current transformation efforts and those that have not.
Table 1 displays sample characteristics. Practice sites were in various stages of improvement efforts, with several advanced practices aligned to PCMH and integrated care models, several practices that displayed no major improvement efforts, and others that had implemented one or more changes such as EHRs or open access scheduling systems. All practice sites had between 1 and 9 physicians.
Table 1.
Characteristics of Primary Care Practice Sample
| Characteristics of Practice Sample | N (%) | |
|---|---|---|
| Size (number of physicians) | Solo | 1 (12.5) |
| 2–3 | 3 (37.5) | |
| 4–9 | 4 (50) | |
| Ownership | Independent | 5 (62.5) |
| Not independent | 3 (37.5) | |
| Location | Rural | 3 (37.5) |
| Nonrural | 5 (62.5) | |
| PCMH characteristics | Team-based care | 3 (37.5) |
| Health information technology | ||
| EHR | 6 (75) | |
| Patient access to EHR | 1 (12.5) | |
| E-Prescribing | 5 (62.5) | |
| Decision support | 2 (25) | |
| Performance measurement/Quality improvement activities | 4 (50) | |
| ACO type integrated delivery system | Consumer engagement | 1 (12.5) 2 (25) |
Data Collection
Data collection included on-site visits involving interviews, observation of meetings and individual interactions, document reviews of policies and performance reports, and telephone interviews, including administration of the National Survey of Physician Organizations (NSPO) (Rittenhouse et al. 2008). We conducted more than 90 key informant interviews during three on-site visits to participating practices over a 16-month period. Examples of questions are listed in Table 2. We interviewed 51 physicians, nurses, medical assistants, practice administrators, mental health specialists, and quality improvement staff. Interviews were audio taped and transcribed for data analysis.
Table 2.
Examples of Interview Questions
| Topic | Question Examples |
|---|---|
| Practice goals and objectives | What do you see as the most important purpose of this practice? |
| How confident are you that you have the knowledge and skills needed to achieve the goals you have set? | |
| Culture | Describe what it is like to work in this practice—the general atmosphere, how people communicate and get along, how they deal with conflict |
| Environment | Describe the other primary care practices and clinics in your community |
| Describe your practice's relationship with these practices and clinics | |
| Improvement efforts | Describe current or recent improvement efforts at the practice |
| Are there improvements you would like to make but have not? If so, can you describe? | |
| Overall, how would you sum up how you approached quality improvement for yourself and your practice? | |
| Reaching goals | What issues, problems, or concerns regarding [the specific improvement activity under discussion] have you encountered? |
| Explain what would make it easier for your organization to implement [specific improvement activity] | |
| Successes and strategies | What strategies have you used to overcome these problems? |
| Describe the results of improvement efforts, i.e., performance measurement, patient feedback |
Data Analysis
The practice, not the medical group, was used as the unit of analysis. Data analysis involved coding transcriptions of interviews using NVivo software and identifying themes within and across cases. We used three phases of coding. The first involved examining the transcript text and developing themes of information. This involved a constant comparative method of identifying instances that represented the theme. In the second phase our team connected the themes, and in the third phase we developed a story from themes that resulted in a set of theoretical propositions (Creswell 2007).
The use of multiple cases strengthen our results by replicating the data matching, thus increasing confidence in the robustness of the theory (Stake 2006). Validity and reproducibility of findings were aided by primary review of transcripts followed by secondary review by an external qualitative researcher, triangulation of data from different sources, semistructured interview guides, and maintenance of an audit trail of theme development and analytic decisions.
Results
Our analysis revealed several broad themes that influence practice engagement in transformation efforts as well as a detailed understanding of these influences. First, study participants revealed four key pressures that influenced practices either to adopt or not adopt improvement efforts such as those exhibited by PCMH or integrated care models. They include incentives and requirements; organizational relationships; availability of financial, knowledge, and time resources; and competing work demands. Second, we identified two important practice characteristics that moderated the force of these pressures: leadership priorities and support, as well as an organizational culture based on innovation and improvement. The third influence on the decision making process involved characteristics of the innovation and included physician and staff knowledge of the transformation strategy and their perception of the ease of implementation and use, and costs and time. Table 3 provides characteristics of transformed and not transformed practices.
Table 3.
Characteristics of Transformed and Not Transformed Practices
| Pace of Transformation | Organizational Ownership | Resource Availability | Leadership Support | Culture of Innovation | Culture of Improvement | |
|---|---|---|---|---|---|---|
| Not transformed | None | System | No | No | No | No |
| None | Independent | No | No | No | No | |
| None | Independent | No | No | No | No | |
| Slow | Independent | Moderate | Moderate | Moderate | Moderate | |
| Transformed | Moderate | Independent | No | Yes | Yes | Yes |
| Moderate | Independent | No | Yes | Yes | Yes | |
| Fast | System | Yes | Yes | Yes | Yes | |
| Fast | System | Yes | Yes | Yes | Yes |
Pressures on Practices to Transform and/or Not Transform
Incentives and Requirements
Practices responded to mandatory requirements of quality improvement activities that benefit the physician or practice in some way, such as those required for medical specialty recertification. Many physicians described their coordination of a short-term quality improvement project required for the American Board of Family Medicine recertification. They reported difficulty in determining what to study and how to collect and analyze quality data for their recertification. One practice contracted with an Independent Practice Association (IPA) that required performance measurement and reporting activities for IPA membership. This physician described participation as straightforward and undemanding because IPA staff pulled and analyzed data, which did not take the physician's time away from patient care. Another practice reported previous participation in required quality improvement activities during its time as a university affiliated residency site. These activities included ongoing chart reviews by attending physicians and regular meetings to discuss quality improvement activities. Another practice previously tried to incorporate consumers into its improvement activities through committee participation. At the time, practice staff did not find consumer involvement helpful to improvement efforts and discontinued the program. Now that the National Committee for Quality Assurance (NCQA) has required consumer involvement in the 2011 PCMH standards, the practice has reconsidered and is planning to involve consumers in multiple improvement projects.
Much variation exists regarding voluntary quality incentives programs. Practice response is stronger if participation is easy to understand and simple. At the start of the study most practices claimed they were not participating in government quality incentive programs, such as the Center for Medicare and Medicaid Services (CMS) Physician Quality Reporting System (PQRS) P4P program, because incentives were too small, physicians/administrators heard negative experiences from other practices, and the program was difficult to understand and participate in. For instance, one practice administrator stated:
The CMS program (P4P) is, well…you think you're putting in all the right data and you wait for your check, and then find out, oh, no, that was wrong… that's disincentive to…participate. (Practice administrator, non-transformed practice)
During the 16-month study period, several practices decided to participate in PQRS only after CMS released more relaxed criteria and easier procedures for participation. Most practices (7 of 8) planned to participate in the EHR meaningful use incentive program because of the substantial financial incentive. Physicians from all practices in the study expressed a negative attitude toward P4P programs and performance reports from insurance companies. We heard several stories similar to the one presented below:
If I get some feedback from the insurance company, it goes into [the] trash because I'm sorry to say but, over the years, I've decided I do what I think is appropriate clinically. (Physician, non-transformed practice)
Organizational Relationships
Practices owned and operated by larger health care systems had access to needed financial and knowledge resources to focus on improvement efforts. Resources obtained from the larger organization for improvement activities include the following: EHR technical support and training; performance measurement and reporting; patient experience surveys; and expert advisors for HIT, quality improvement, and other aspects of the practice. These practices were also bound to comply with demands from the larger organization, including productivity standards and participation in specific programs or activities.
The two practices that were most aligned to the PCMH model [both NCQA-recognized as a PCMH] were practices owned by large health care systems. Another recently NCQA-recognized practice, owned by a solo practitioner, belonged to an IPA that provided support for improvement efforts such as performance data collection and analysis. A separate practice, not aligned with the PCMH model, was more involved in improvement activities when it was a university residency site, in part because these activities were required and came with financial support.
Resources
Practices more closely aligned to the PCMH model indicated that time, money, information systems, and knowledge and expertise were not barriers to engaging in practice improvement activities. The two practices most aligned to the PCMH model received considerable technical support and financial resources from the parent organization on HIT, performance measurement, and improvement initiatives. A quality improvement specialist, at a health system-owned PCMH practice, working toward PCMH recognition for other practices in their medical group organization, asserted:
The [larger organization] made a commitment to … help with [the] Medical Home project and to do the quality improvement piece… [We] meet all the time, constantly, and we go to practice sites and we do practice assessments… I go in and show people all kind of things … (Quality improvement specialist, transformed practice)
Practices least aligned with the PCMH model reported having less time and money than practices closer to the PCMH model. Several independent practices lacked the necessary infrastructure and support staff for quality improvement activities. Others were struggling to stay financially afloat and found it difficult to secure resources to invest in improvement efforts. A staff nurse at one non-PCMH practice described their situation:
We're on almost a paycheck to paycheck kind of situation. And so most of us don't really want to ask for anything that we even think is going to improve stuff because we're always told we have no money. (Nurse, non-transformed practice)
Many small practices also faced difficulty with a lack of knowledge of not only improvement efforts but also change management strategies and process redesign needed for major transformations like the move toward a PCMH or ACO type model. Practices that were either moderately or unaligned to the PCMH model lacked the knowledge to utilize EHR functions for data collection and monitoring performance. Many practices did not understand how to participate in government-sponsored quality incentive programs.
Another issue described repeatedly by practices was having insufficient time to devote to improvement efforts. The quote below, expressed by one of the physicians at a PCMH practice, shows the conflict between the need to meet productivity requirements and to deliver quality care.
On my busier days… there's danger of going back into your old mindset of volume driven medicine versus quality driven medicine. (Physician, transformed practice)
Competing Work Demands
While practices furthest from the PCMH model experienced more problems with workload and financial resources, they also seemed to be burdened by inertia—an inability or unwillingness to engage in quality improvement activities. These practices, overwhelmed by financial constraints and day-to-day activities, found it difficult to understand how and what changes to make to their practice and were unable or unwilling to devote time for improvement efforts. The physician leader and others at one practice expressed a desire to make improvements; however, they were overwhelmed with day-to-day tasks, contracts with insurance companies, and coding and billing problems. Below are quotes from two individuals at this practice:
We were looking for some progress and I don't think we really knew exactly how to achieve that. We knew the concept, but we probably fell short on implementing and doing it properly. (Managing physician, non-transformed practice)
I do think that business wise we are probably weak… there are business things that we can do more business like. I don't know what [that] would do to the relationship [with] the patients, and to the culture, and to what we established being here for 30 years. (Office manager, non-transformed practice)
Personal and Professional Modifiers
Leadership Priorities
Leadership priorities stood out as a critical influence on whether practices engaged in improvement efforts. The lead physician at one practice, extremely dissatisfied with the “15-minute care model,” described why he transformed his practice into a patient-centered, team-based care model.
We would turn away patients that I had been seeing for 20 years … what kind of quality is that? I can't see you on the day you need to be seen. I wanted to be able to see my patients on their schedule… [Regarding] quality of the medical care, we weren't giving them enough; I didn't have time to ask all the right questions. I didn't have time to have an accurate chart…
I now [after transformation] have time to focus on all the patients' medical needs… [the nurses] ask all the questions. I can walk in a room and focus… on [the patients'] medical needs… and not five or six other things. I can really deal with their medical issues, that is huge, that's the biggest reason. The nurses asking all the right questions and having an accurate chart…
We made our changes to improve finances, to maintain quality… Because of the nurse's availability that physicians don't have, our quality went to a level that I've never seen. (Physician, transformed practice)
Organizational-level leaders of PCMH practices also exhibited a desire to transform and improve performance and provided support and dedicated resources for transformation efforts. A quality improvement nurse at one PCMH practice described her organization CEO in the following way:
I would say that —–, is very visionary as the CEO… he really feels like patient care, if you put patients first… if you put safety first, the other things will follow, so I feel like he really wants to have patient centeredness first. (Nurse practitioner, transformed practice)
The leaders of this PCMH practice and its larger organization emphasized quality and performance, which was reflected in articulated goals, clinical performance measurement and reporting, individual performance assessments, and physician compensation methods.
Organizational Culture
Practices with the closest alignment to the PCMH model exhibited an emphasis on innovation, teamwork and communication, formal structure, written policies and procedures, employee support, financial attentiveness, and performance improvement. Practices furthest from the PCMH model exhibited few of these characteristics with one exception—all practices in the study were dedicated to providing good patient care. Another theme is that the culture of the larger organization influenced the supporting structure and resource availability for quality improvement activities. Physician values and goals had a tremendous influence on whether the practice engaged in quality improvement activities. For instance, one physician from a PCMH practice stated:
Through the years we've always had this “can do” mentality, if we thought it was going to improve patient care, we went for it. (Physician, transformed practice)
This particular practice displayed a focus on performance as well as an innovative spirit. It emphasized performance throughout the organization, embedded in everything from staff and physician performance appraisals, multiple ongoing efforts to capture patient experience information, and performance measurement at the individual and practice level.
Characteristics of the Innovation
Our findings also indicate that leaders' perception of the transformation initiative was a key influence on a practice's decision to adopt or not adopt. Practices that adopted new technologies and models of care delivery and those that had not adopted considered the value of the transformation, knowledge and complexity of the transformation and implementation strategies, ease of use, and the costs and time associated with implementation. For example, all three practices that had not adopted an EHR at the time of the study cited limited knowledge of EHR systems, lack of technical support, costs, and time as reasons for not implementing an EHR. Two practices that adopted formal team-based care models considered various types of team care models as well as quality of care, financial outcomes, and efficiency of patient care as part of their decision making process. Practices moving toward a PCMH model described their process of acquiring information on PCMH components and implementation, appraising value, and evaluating costs and time associated with the transformation.
Study Limitations
Comparative case studies of practices are an appropriate method to conduct an in-depth examination of practices engaging in improvement efforts and those that are not. This methodology limited the number of practices in our sample, which were drawn from small family medicine practices in Virginia. Also, self-reported data from interviews may present biases, and data analysis was subject to interpretation by the team. To address these concerns, we purposefully sampled practices to ensure diversity in location, organizational structure, and performance improvement efforts. We also assembled a multidisciplinary team that interviewed key informants numerous times over a 16-month period. Key informants included both clinical and nonclinical staff. Multiple members of our team coded and analyzed data, which were later reviewed by an external qualitative researcher. Differing interpretations were resolved through consensus and/or additional data collection.
Discussion And Conceptual Framework
Based on our grounded observations and our understanding of organization theory, we were able to construct a preliminary framework for examining the central question that our study addresses: Why have some practices elected to engage in practice improvement efforts whereas others have not?
Structural contingency theory (SCT) suggests that organizations perform better if they strategically align their structures and processes with major internal and external pressures (Donaldson 2001). With this in mind, the underlying issue is to what extent primary care practices were or were not aligned with the environmental pressures that bear on them. As our data show, pressures that practices face consist of stark contrasts and contradictory choices. The major pressures we identified are consistent with forces posited by macro-level organizational theories on the influence of the environment on organizations. We also identified specific aspects of leadership, organizational culture, and the actual improvement activity as influences on the ability of practices to transform.
Our findings support and build upon previous research that linked adoption of PCMH components to the existence of financial incentives, access to resources, supportive leadership, and organizational culture (Goldberg and Mick 2010; Nutting et al. 2010; Fernald et al. 2011; Reid et al. 2011; Rittenhouse et al. 2011; Wise et al. 2011). Our case study research suggests that knowledge and expertise, implementation assistance, and finances are important resources that enable practice transformation. Our research highlights how organizational relationships provide resources to assist practices with improvement efforts. Larger organizations often provide necessary resources such as financial support and technical assistance to aid practices in their transformation.
Previous research found no significant relationship between regulatory forces and the adoption of PCMH elements, such as EHRs and performance measurement (Goldberg and Mick 2010). Our case study research suggests that practices will engage in incentive programs if the incentive is strong enough and easy to participate in. Physicians also respond to mandatory requirements for engaging in quality improvement projects when required by their certification authority. Earlier research also established that an organizational culture that emphasizes quality is related to the existence of practice improvement activities (Dugan et al. 2011). Our case study research supports this finding and provides additional evidence that leadership priorities and support greatly influenced practice improvement efforts. We also found that teamwork and strong communication systems existed in practices that were more aligned with PCMH and/or ACO models and that these practices exhibited a culture of innovation, financial attentiveness, formal organizational structure, and written policies and procedures.
In the conceptual framework of practice engagement in improvement efforts (Figure 1), we integrate structural contingency theory with a strategic action approach. Shortell and Rundall (2003) described strategic intent as the behavioral actions purposefully taken by organizations to shape their response to environmental pressure and to reshape their environment. This view is consistent with a structural contingency perspective of an organization's management actively examining the “alignment” between pressures on the organization and its structures and processes. The role of management is to diagnose lack of “alignment” and find structures and processes that improve performance (Donaldson 2001). If further resources are required to secure “alignment,” management may strive to find ways to secure these resources, leading to a variety of potential actions such as practices joining an IPA or becoming part of a health system.
Figure 1.
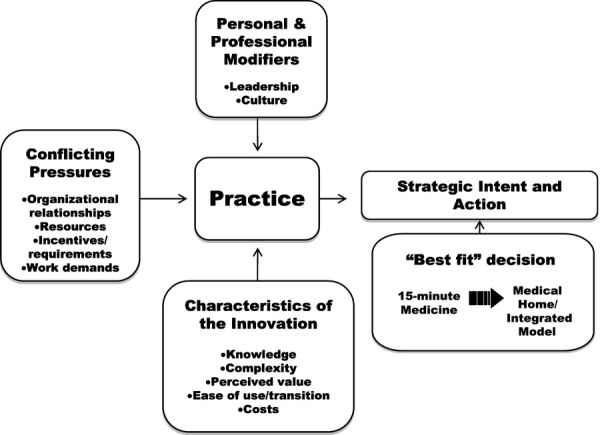
Conceptual Framework for Primary Care Practice Engagement in Improvement Efforts
We argue that primary care practices are caught in a cross fire of conflicting pressures that push practices away from and toward transformation. It is not surprising that among just eight in-depth case studies we find a continuum of improvement activities. Our results illustrate a set of forces that produce pressures on practices in which the “best fit” would be to institute major changes to improve quality of care, access, patient experience, and/or business functionality. Professional pressure exists to redesign medical practices to improve care by employing evidence-based medicine, new technologies, and structures and processes of the PCMH. We also identified pressures from public and private payers to engage in these improved approaches via performance measurement and reporting requirements. An example of a practice embracing transformation in our study is one that achieved level three PCMH recognition by NCQA, created an innovative care coordination model, and is moving toward an ACO type integrated care model. This practice, owned by a large health care system, receives encouragement and support from health system leadership, has defined organizational structure and processes and effective communication systems, and has an embedded culture of improvement and innovation. In this case, the health system's strategy for its primary care network is to be competitive in the market by providing high-quality, accessible, and efficient services.
At the other extreme, we found practices that followed the “15-minute per patient” practice form (Bodenheimer 2008; Hoff 2010). Here, the wider pressures are regulatory, scarcity of resources, payer requirements, and an inability to change or to change quickly enough to respond positively to environmental pressures. Taken together, these forces provide an incentive to structure practices into assembly line-like production systems, screening, and referring out difficult cases immediately to specialists, relying on as much standardization of procedures as possible, all aiming to get a patient in and out of the exam room in about 15 minutes. This can be hypothesized to provide the “best fit” to comply with these pressures. An example of a practice in our study responding to these pressures is one that has not engaged in major changes to their care delivery model or business functions. The physicians and staff at this independent practice were overwhelmed with day-to-day tasks, compliance with payer requirements, and other financial issues. They did not perceive value in investing resources in major transformation initiatives and were strapped with a lack of financial resources and knowledge of how to make improvements to their practice.
Our study describes conflicting forces that practices can respond to, which originate from organizational relationships, acquisition of resources such as financial reimbursement for services, incentives and requirements, and competing work demands. Many would argue that primary care practices would be better aligned to certain forces, such as incentive programs, by adopting elements of these new models in their structures and processes. However, by not changing, some practices are well aligned with other external forces such as traditional fee-for-service payment methods. In the long run, the latter approach may lead to gradual misalignment as one by one the forces favoring status quo are removed from the environment.
The conceptual framework illustrates that transformed practices were able to access needed financial resources and technical expertise; have supportive leadership and organizational structure; possess a culture focused on improvement, teamwork, and innovation; and have the ability to manage multiple work demands. All these factors must be considered to understand whether a practice can transform versus remain with the status quo of “15 minute medicine.” Practices that desire to adopt more idealized models of primary care practice must be mindful of these factors and recognize that they will find both incentives and disincentives to transform. Small, unaffiliated practices may choose to become part of a larger health system to acquire additional resources of expertise and money needed for transformation, which is a better fit for the current environment of forces.
Implications for policy makers and payer organizations are evident. Incentives need to be clearly aligned to desired improvement strategies and strong enough to motivate and sustain change. As current payment systems were designed for acute care medicine, there should be continued efforts to find innovative ways to pay for preventive service delivery, chronic disease care, and population management—all critical for improving quality of care. In the current payment “environment,” small and unaffiliated primary care practices have a more difficult time transforming than larger, system-owned practices. Programs aimed at improving primary care delivery should consider contextual information such as practice size, ownership status, resource availability, and competing demands on practices. Given that small independent practices are a critical component of the health care system, it seems appropriate to create programs that can help some unaffiliated practices stay independent and yet have adequate training, finances, and coaching to improve capacity and quality in primary care.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This research was funded by the U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality under grant number R01HS018422. We gratefully acknowledge the secondary review of qualitative findings by Rita H. Pickler, Ph.D., R.N., P.N.P.-B.C., F.A.A.N.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Anderson G, Marcovich S. New York: The Commonwealth Fund; 2010. “Multinational Comparisons of Health Systems Data 2008”. [accessed on December 1, 2011]. Available at: http://www.commonwealthfund.org/Publications/Chartbooks/2010/Apr/Multinational-Comparisonsof-Health-Systems-Data-2008.aspx. [Google Scholar]
- Bodenheimer T. “The Future of Primary Care: Transforming Practice”. The New England Journal of Medicine. 2008;359(20):2086–9. doi: 10.1056/NEJMp0805631. [DOI] [PubMed] [Google Scholar]
- Creswell JW. Qualitative Inquiry and Research Design: Choosing among Five Traditions. 2nd Edition. Thousand Oaks, CA: Sage Publications; 2007. [Google Scholar]
- Donaldson L. The Contingency Theory of Organizations. Thousand Oaks, CA: Sage Publications; 2001. [Google Scholar]
- Dugan D, Scholle S, Mick SS, Steidle E, Goldberg DG. “The Relationship between Organizational Culture and Practice Systems in Primary Care”. Journal of Ambulatory Care Management. 2011;34(1):47–56. doi: 10.1097/JAC.0b013e3181ff6ef2. [DOI] [PubMed] [Google Scholar]
- Fernald DH, Deaner N, O'Neill C, Jortberg BT, deGruy FV, Dickinson WP. “Overcoming Early Barriers to PCMH Practice Improvement in Family Medicine Residencies”. Family Medicine. 2011;43(7):503–9. [PubMed] [Google Scholar]
- Glaser BG, Strauss A. Discovery of Grounded Theory: Strategies for Qualitative Research. London: Aldine Transaction; 1967. [Google Scholar]
- Goldberg DG, Kuzel AJ. “Elements of the Patient-Centered Medical Home in Family Practices in Virginia”. Annals of Family Medicine. 2009;7(4):301–8. doi: 10.1370/afm.1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg DG, Mick SS. “Medical Home Infrastructure: Effect of the Environment and Practice Characteristics on Adoption in Virginia”. Medical Care Research and Review. 2010;67(4):431–49. doi: 10.1177/1077558710367795. [DOI] [PubMed] [Google Scholar]
- Grol R, Grimshaw J. “From Best Evidence to Best Practice: Effective Implementation of Change”. Lancet. 2003;362(9391):1225–30. doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]
- Hoff T. Practice under Pressure: Primary Care Physicians and Their Medicine in the Twenty-first Century. Piscataway, NJ: Rutgers University Press; 2010. [Google Scholar]
- Huynh PT, Schoen C, Osborn R, Holmgren AL. New York: The Commonwealth Fund; 2006. “The U.S. Health Care Divide: Disparities in Primary Care Experiences by Income”. [accessed on December 1, 2011]. Available at: http://www.commonwealthfund.org/Publications/Fund-Reports/2006/Apr/The-U-S–Health-Care-Divide–Disparities-in-Primary-Care-Experiences-by-Income.aspx. [Google Scholar]
- MacKinney AC, Ullrich F, Mueller K. Iowa: RUPRI Center for Health Policy Analysis, University of Iowa; 2011. “Patient-Centered Medical Home Services in 29 Primary Care Practices: A Work in Progress”. Rural Policy Brief No. 2011-6. [PubMed] [Google Scholar]
- McGynn E, Asch S, Adams J, Keesey J. “The Quality of Health Care Delivered to Adults in the United States”. New England Journal of Medicine. 2003;348(26):2635–46. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- Milstein A, Gilbertson E. “American Medical Home Runs”. Health Affairs. 2009;28(5):1317–26. doi: 10.1377/hlthaff.28.5.1317. [DOI] [PubMed] [Google Scholar]
- Mueller KJ, Ullrich F, MacKinney AC. Iowa: RUPRI Center for Health Policy Analysis, University of Iowa; 2011. “Use of Health Information Technology in Support of Patient-Centered Medical Homes Is Low among Non-Metropolitan Family Medicine Practices,” Rural Policy Brief No. 2011-2. [Google Scholar]
- Nutting PA, Crabtree BF, Miller WL, Stewart EE, Stange KC, Jaén CR. “Journey to the Patient-Centered Medical Home: A Qualitative Analysis of the Experiences of Practices in the National Demonstration Project”. Annals of Family Medicine. 2010;8(Suppl 1):s45–56. doi: 10.1370/afm.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid A, Baxley E, Stanek M, Newton W. “Practice Transformation in Teaching Settings: Lessons from the I³ PCMH Collaborative”. Family Medicine. 2011;43(7):487–94. [PubMed] [Google Scholar]
- Rittenhouse DR, Casalino LP, Gillies RR, Shortell SM, Lau B. “Measuring the Medical Home Infrastructure in Large Medical Groups”. Health Affairs. 2008;27(5):1246–58. doi: 10.1377/hlthaff.27.5.1246. [DOI] [PubMed] [Google Scholar]
- Rittenhouse DR, Casalino LP, Shortell SM, McClellan SR, Gillies RR, Alexander JA, Drum ML. “Small and Medium-size Physician Practices Use Few Patient-centered Medical Home Processes”. Health Affairs. 2011;30(8):1575–84. doi: 10.1377/hlthaff.2010.1210. [DOI] [PubMed] [Google Scholar]
- Schoen C, Osborn R, Doty MM, Bishop M, Peugh J. “Toward Higher-performance Health Systems: Adults' Health Care Experiences in Seven Countries”. Health Affairs. 2007;26(6):w711–34. doi: 10.1377/hlthaff.26.6.w717. [DOI] [PubMed] [Google Scholar]
- Shortell SM, Rundall TG. “Physician-Organization Relationships: Social Networks and Strategic Intent”. In: Mick SS, Wyttenbach ME, editors. Advances in Health Care Organization Theory. San Francisco, CA: Jossey-Bass; 2003. pp. 141–73. [Google Scholar]
- Stake R. Multiple Case Study Analysis. New York: Gilford Press; 2006. [Google Scholar]
- Von Korff M, Gruman J, Schaefer J, Curry S, Wagner E. “Collaborative Management of Chronic Illness”. Annals of Internal Medicine. 1997;127(12):1097–102. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]
- Wise CG, Alexander JA, Green LA, Cohen GR, Koster CR. “Journey toward a Patient-Centered Medical Home: Readiness for Change in Primary Care Practices”. Milbank Quarterly. 2011;89(3):399–424. doi: 10.1111/j.1468-0009.2011.00634.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


