Abstract
Objective
To examine the effect of reductions in hospital-based (HB) skilled nursing facility (SNF) bed supply on the rate of rehospitalization of patients discharged to any SNF from zip codes that lost HB beds.
Data Source
We used Medicare enrollment records, Medicare hospital and SNF claims, and nursing home Minimum Dataset assessments and characteristics (OSCAR) to examine nearly 10 million Medicare fee-for-service hospital discharges to SNFs between 1999 and 2006.
Study Design
We calculated the number of HB and freestanding (FS) SNF beds within a 22 km radius from the centroid of all zip codes in which Medicare beneficiaries reside in all years. We examined the relationship between HB and FS bed supply and the rehospitalization rates of the patients residing in corresponding zip codes in different years using zip code fixed effects and instrumental variable methods including extensive sensitivity analyses.
Principal Findings
Our estimated coefficients suggest that closure of 882 HB homes during our study period resulted in 12,000–18,000 extra rehospitalizations within 30 days of discharge. The effect was largely concentrated among the most acutely ill, high-need patients.
Conclusions
SNF patient-based prospective payment resulted in closure of higher cost HB facilities that had served most postacute patients. As other, less experienced SNFs replaced HB facilities, they were less able to manage high acuity patients without rehospitalizing them.
Keywords: Hospital-based skilled nursing facility, prospective payment policy, instrumental variables, rehospitalization
Faced with increasing medical care costs, policy makers introduced prospective payment systems (PPSs) for Medicare reimbursement of hospitals in 1983, skilled nursing facilities (SNFs) in 1998, and finally home health care agencies in 2000. In the years following the introduction of hospital PPS in 1983, many hospitals responded to incentives to reduce inpatient length of stay by purchasing skilled nursing facilities or establishing a skilled unit in an unused wing or on the grounds of the hospital (Bishop and Dubay 1991; Manton, Stallard, and Woodbury 1994). As these facilities were reimbursed on a cost basis, hospitals faced few financial constraints to owning a SNF, although they were substantially more costly than freestanding nursing homes (Schlenker, Shaughnessy, and Yslas 1983; Zimmerman et al. 2008). However, since the introduction of PPS for SNFs in 1998, SNFs are reimbursed based on the average cost of treating patients with certain needs and characteristics. As a result, hospitals lost their incentive to own SNFs and by 2008 only some 1,000 hospital-based facilities continued to operate, compared to around 2,500 a decade earlier (Kitchener, Bostrom, and Harrington 2004; Feng et al. 2011).
The goal of this study is to understand the impact of this market response to policy changes on the rate of rehospitalization of SNF patients over the period of SNF PPS implementation and its aftermath (1999–2006). Over 40 percent of all Medicare fee-for-service hospitalizations are discharged to a postacute care setting and about 20 percent of them are rehospitalized within 30 days (Jencks et al., 2009). Mor and colleagues (2010) found that the rate of rehospitalization from SNF has been growing over the last decade and is higher than the overall rate of rehospitalization of all Medicare patients. These hospitalizations are known to be frequent (Intrator et al. 2007), costly (Grabowski, O'Malley, and Barhydt 2007), and often preventable (Saliba et al. 2000; Intrator, Zinn, and Mor 2004). MedPAC has identified the rehospitalization of Medicare residents as a particularly salient measure of postacute nursing home quality (Donelan-McCall et al. 2006).
This study focuses on the local SNF market, seeking to determine how closure of hospital-based (HB) facilities in a given market affects the outcomes experienced by the population of SNF patients. More specifically, we used zip code as our unit of analysis and show how change in both types of SNF bed supply affects the rehospitalization of SNF patients within a zip code. Our analysis estimates the effect of exogenous changes in the supply of beds in a given area. The number of SNF facilities has been targeted by both federal policies (like BBA or Medicare and Medicaid certification) and state policies (like the requirement of Certification of Need [CON] to open up new facilities or increase the number of beds). Thus, this study not only estimates the aggregate effect of the closure of HB facilities but also informs policy makers about the possible impact of any policies that may affect the bed supply.
Conceptual Framework
The observed number of beds in a given market can be considered in an equilibrium state, endogenously determined by bed demand and supply. Demand side factors include average health and wealth of the potential nursing home population, whereas supply side factors include the cost of different inputs, technology, and policy shocks. Changes in supply will, on average, affect the aggregate nursing home quality experienced by residents, one measure of which is hospitalization (Grabowski et al. 2008; Konetzka, Spector, and Limcangco 2008). An exogenous change in the supply of HB SNF beds can affect the rehospitalization of SNF patients in several ways.
First, the equilibrium number and/or the average health of patients discharged to SNF may change. In the absence of HB SNF, patients with certain characteristics may go to inpatient rehabilitation facilities or long-term care hospitals for postacute care.
Second, HB and freestanding (FS) SNFs may not be perfect substitutes with respect to available clinical resources and quality of care, so a change in bed supply of one type of facility may not be met by the availability of beds in the other. HB facilities had more than a decade of experience serving patients intending to return home following a hospitalization and short recuperation in SNF, a market that most FS SNFs had not entered prior to 1998. However, the empirical findings regarding the substitutability of one type of facility for the other are mixed. Stearns et al. (2006) found that patients who were good candidates for quicker recovery were more likely to be admitted to HB facilities. Nevertheless, even after controlling for such selection using a propensity score matching approach, they found that being treated in a HB facility instead of an FS SNF had significant positive effects on health outcomes (e.g., quicker discharge to home and lower rehospitalization). On the other hand, White and Seagrave (2005) compared hospitals that closed their SNFs with those that kept SNFs operating between 1997 and 2001, using all discharges irrespective of their destination, or previous long-term care utilization history; they found no differences in the rehospitalization rates between such hospitals.
Third, change in HB bed supply may affect the quality of care in both types of SNFs through change in competition in the market and spillover effects. Competition was found to be positively associated with quality measure scores (Castle, Engberg, and Liu 2007); expenditures on clinical, hotel, and administrative activities (Mukamel, Spector, and Bajorska 2005); reduced staffing (Zinn 1994); and average expenditures per patient (Nyman 1988). There is also limited evidence of intersegment spillover effects, for example, nonprofit SNFs have been shown to have a positive external effect on quality of for-profit SNFs in the market (Hirth 1999; Grabowski and Hirth 2003).
While this study seeks to estimate the aggregate effect of a change in HB bed supply, we do not attempt to distinguish between the mechanisms by which this change occurs. However, we control for the change in characteristics of the patients discharged to SNF and for the share of fee-for-service Medicare beneficiaries discharged to any SNF from a given zip code in different years and estimate the net effect of substitutability, competition, and spillover effects on quality as measured by rehospitalization. The exogenous policy shock to SNF supply that prompted the exit of HB facilities from the market in many areas allows us to test the causal relationship between bed supply and quality of care by specifically examining an aspect of quality sensitive to facilities' experience with postacute patients' needs. From this perspective, we hypothesize that the loss of HB facilities in a given area results in higher rehospitalization rates of nursing home residents.
Methods
Data
This study relies upon two types of individual-level data: Medicare claims and enrollment records and the nursing home minimum dataset (MDS) resident assessments completed around the time of admission to SNF. Nursing home characteristics were obtained from the On-line Survey & Certification Automated Record (OSCAR) and facility addresses were geo coded. We also use zip code tabulation area (ZCTA) and census population estimates of zip codes for the year 2000.
As our main explanatory variable, bed supply, is measured at the zip code level, our unit of analysis is the zip code. The Medicare enrollment record, which is updated annually, includes Medicare beneficiaries' mailing address zip code, which we treat as patients' home address. We assume that this home address is exogenous, that is, not affected by the choice of type of care or facility. Most beneficiaries' address does not change following postacute SNF use unless they become long stay residents, and we know when this occurs based upon the presence of repeated MDS assessment records.
The patient population includes all fee-for-service Medicare beneficiaries (MB) who entered a skilled nursing facility following a hospitalization event between 1999 and 2006 and who did not reside in a NH within 120 days before that hospitalization. We are able to identify prior nursing home residence using the Residential History File methodology (Intrator et al., 2011), which tracks Medicare beneficiaries' daily location by concatenating dates associated with Medicare claims and MDS records. Our working sample is composed of approximately 10 million acute hospital discharges, originating from approximately 26,000 zip codes in 48 contiguous states, excluding Washington, DC.
Each hospital discharge is linked to the beneficiary's home zip code and demographic characteristics from enrollment records, characteristics of the hospital stay (e.g., length of stay, ICU use, comorbidities, and primary diagnoses), characteristics of the postacute stay in a SNF, including the outcome of rehospitalization and various MDS-based clinical characteristics (e.g., the CHESS comorbidity index) (Hirdes, Frijters, and Teare 2003), activity of daily living (ADL) score (Morris, Fries, and Morris 1999), and case mix index (CMI) using resource utilization groups (RUGs) 5.12 (Fries et al. 1994).
We aggregated discharge-level records to the level of the zip code to create the number of discharges, the fraction of patients rehospitalized, average acuity, and selected demographic characteristics. From the Medicare enrollment records, we also calculated the total number of MB and the fraction enrolled in managed care, and the fraction dying in the year. We merged these data with bed supply variables, which we computed by aggregating OSCAR (1999–2006) data and merging with ZCTA (2000) data.
Outcome Variable
The outcome we are examining is rehospitalization, defined as returning to any acute general hospital within 30 days of the date of discharge from an acute general hospital to an SNF, although not necessarily to the same discharging hospital. To explore the effects of HB facility loss on particular types of rehospitalizations, we split the 30-day period into three mutually exclusive periods: 1–3 days, indicative of either premature discharge or inappropriate placement; 4–7 days, a sign of poor communication of clinical information between the hospital and SNF; and x 8–30 days, an indicator of SNF resources and quality.
Bed Supply
The bed supply, by type of SNF, in a given zip code in a particular year is defined by the total number of beds in that year across all facilities located within a 22 km radius from the centroid of that zip code. Several alternative definitions of market have been used in the SNF literature based on geographical area, that is, standard metropolitan statistical area, zip code (Feng et al. 2011), county (Zinn 1994) (Banaszak-Holl, Zinn, and Mor 1996), and physician referral regions (Garnick et al. 1987). Although county and zip codes may be a poor proxy for market because of heterogeneity in size and population density (Zwanziger, Mukamel, and Indridason 2002), all these definitions assume that markets do not overlap. We do not need to apply this restrictive assumption and use a distance-based definition following the argument of Garnick et al. (1987). We chose 22 km which is the 80th percentile of the distance of the destination SNF from the origin zip code of the patients in our sample.
To calculate bed supply we used the zip code centroids obtained from ZCTA for the year 2000. We matched each zip code with all the nursing homes available in a given year and calculated the distance of each zip code centroid from a given nursing home using the Haversine formula of distance. We calculated the total number of beds of both types of SNFs for each year. Change in the bed supply of a certain type in a zip code not only reflects closures but also new facility entrants as well as bed size changes among existing facilities.
Statistical Model
Equation (1) describes the baseline statistical model that we estimated in this study.
| (1) |
Here, RHzt is the average rehospitalization of patients who were admitted to a SNF from zip code z in year t; B_HBzt is the supply of HB SNF beds within 22 km radius of zip code z in year t; B_FSzt is the supply of FS SNF beds within 22 km radius of zip code z in year t; Xztρ z is a vector of zip code fixed effects; and θt is a vector of time fixed effects; Xzt is a vector of control variables: total number of MB, share of MB enrolled in managed care, share of MB who died in the same year, share of FFS MB who are in our sample, demographic variables from Medicare enrollment records, and acuity indexes, that is, average hospital length of stay, reimbursement, ICU usage rate, Deyo and Elixhauser comorbidity scores from hospital claims; and uzt is the error term.
We estimated this equation using OLS and 2SLS methods and the total number of discharges in the corresponding zip code year as an analytical weight. The zip code-specific fixed effects assume that the demand factors in a zip code are time invariant and also capture the effects of neighborhoods as argued by Chandra and Skinner (2003).
Instrumental Variable
We estimated the effect of HB bed supply using an instrumental variable (IV) defined as the interaction of time and zip code population density (PD). Our measure of PD, that is, the population 65+ per square mile for each zip code, is derived from 2000 census data and therefore is time invariant. Time is a count variable, which is zero for year 1999, increasing by one for each subsequent year. We used a linear trend here because of its simplicity and the absence of any theoretical reason for nonlinearity. Our IV emerges because HB SNF closures after PPS were not uniformly distributed across zip codes. As hospitals are located in densely populated zip codes, the decline in HB beds is much higher in those zip codes. Given that the first-stage relationship holds, our exclusionary restriction assumption is that changes in rehospitalization over time do not vary systematically across zip codes with different population density, except through changes in HB bed supply.
We undertook a variety of modified versions of our baseline mode to test its robustness. The second alternate model includes aggregated MDS assessment acuity measures, which are not included in the baseline model because of nonrandom missing values in the MDS. Some 8.9 percent of SNF admissions do not have a MDS assessment, generally because they had very short stays. As the MDS acuity measures are constructed from many data items, missing values in any of these items further increased the missing data; roughly 21 percent of study patients were missing the CHESS score, 9 percent the ADL score, and 14 percent the case mix measure.
Our third model examines the exclusionary restriction assumption. Zip codes with high population density are likely to be in urban areas that may have different trends in average acuity of SNF patients and availability of substitutes of SNF care. Indeed, Dalton and Howard (2002) showed that increases in the number of HB SNFs in urban areas after hospital PPS was higher than in rural areas, meaning that decline in HB beds following SNF PPS will also be much greater in urban areas. In the presence of a differential trend in unobserved acuity in rural and urban areas, both of our estimation approaches will produce biased estimates. So our third model includes several differential trends with respect to different zip code characteristics: distance of the nearest hospital (DNH), percentage of rural population (PRP), and per capita income (PCY). All three variables are time invariant and included in the model interacted with time, like the instrumental variable. These interactions should identify the effects of unobserved, time variant severity of the admitted SNF patients and the availability of different postacute services.
The fourth version of the model estimates our baseline model but without weights. The fifth and sixth versions estimate the baseline model separately for the years 1999–2002 and 2003–2006 on the assumption that early response to the introduction of SNF PPS might differ from later response.
The seventh model alters the form of the dependent variable by deflating bed supply variables by the number of beneficiaries in the corresponding zip code year. We did not use the number of discharged individuals because they might be determined by bed supply, and, as such, endogenous. As an alternative to model 7, we estimated the effect of change in bed supply on the number of rehospitalization events, after controlling for total number of discharges. In this case we did not use any weights as the number of discharges is used as a control variable.
One may expect that HB SNFs have comparative advantage in treating high acuity. To test this, we divided our observations with nonmissing MDS-based SNF CMI into two groups based on the median (1.06) of that variable; that is, high versus low acuity cases. We then recalculated zip code year level aggregates and reestimated our baseline model separately for both the groups. We hypothesized that effect of HB bed supply will be larger on high acuity patients as they are at higher risk of rehospitalization.
Finally, we tried to separate out the effect of substitutability between HB and FS SNFs and the effect of reduced competition due to loss of HB beds. We calculated the Herfindahl–Hirschman Index (HHI) using number of beds by the different types of facilities within a 22 km radius of all zip codes for different years. We substituted two bed supply variables in the baseline model with share of HB beds among all bed supply and HHI. In this case, only share of HB beds has been instrumented.
Our multivariate analysis is based on a balanced panel of zip codes obtained by dropping the zip codes for which we do not have at least one patient in each study year. All the t-statistics reported are robust, obtained from clustering the error term by state. Clustering is expected to correct for autocorrelation of error terms, which might result from state-level policy shocks. We used STATA procedures developed by Schaffer (2010) designed for panel data fixed-effect instrumental variable regression.
Results
Trends in the Structure of the Nursing Home Industry
Table 1 presents the raw data over all study years regarding bed supply, patient characteristics, and the hospitalization rate outcome variables. As can be seen, the number of fee-for-service hospital discharges to SNF increased from about 1.1 million in 1999 to 1.4 million in 2006. In 1999, some 40 percent of community hospitalizations discharged to SNF went to an HB SNF, but by 2006, this figure was only about 19 percent. Over the 8-year study period, about 40 percent of HB facilities exited the industry, whereas the total number of FS SNFs remained relatively constant. The average number of beds located within a 22 km radius of zip code centroids declined by almost a third among HB facilities, but remained relatively constant among FS facilities.
Table 1.
Descriptive Statistics by Year and Type of Skilled Nursing Facility
| 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | ||
|---|---|---|---|---|---|---|---|---|---|
| No. of discharges to SNF in 1,000 | 1,088 | 1,107 | 1,181 | 1,198 | 1,214 | 1,264 | 1,356 | 1,383 | |
| % of the discharged patients among FFS MB | 3.79 | 3.67 | 3.70 | 3.71 | 3.71 | 3.74 | 3.88 | 3.91 | |
| % of discharges went to HB SNF | 40.01 | 36.74 | 33.27 | 29.34 | 25.82 | 23.24 | 21.13 | 19.30 | |
| Avg. no. of SNFs to which hospitals discharge | 15.9 | 16.1 | 16.2 | 16.9 | 17.3 | 17.5 | 18.0 | 18.6 | |
| Bed supply variables | |||||||||
| Total no. of NH | FS | 14,941 | 14,922 | 14,866 | 14,832 | 14,764 | 14,697 | 14,637 | 14,584 |
| HB | 2,262 | 2,092 | 1,946 | 1,758 | 1,627 | 1,523 | 1,432 | 1,380 | |
| Supply of NH beds (‘100) | FS | 21.99 | 21.96 | 21.87 | 21.82 | 21.78 | 21.70 | 21.68 | 21.56 |
| HB | 1.55 | 1.45 | 1.36 | 1.28 | 1.19 | 1.11 | 1.05 | 1.03 | |
| Outcome variables | |||||||||
| % rehospitalized in 1–30 days | FS | 17.74 | 18.11 | 18.98 | 19.61 | 20.15 | 20.33 | 20.42 | 20.42 |
| HB | 18.72 | 18.80 | 19.18 | 19.16 | 18.89 | 18.72 | 18.13 | 17.82 | |
| % rehospitalized in 1–3 days | FS | 1.89 | 1.98 | 2.10 | 2.25 | 2.34 | 2.44 | 2.43 | 2.50 |
| HB | 1.18 | 1.21 | 1.25 | 1.39 | 1.43 | 1.48 | 1.46 | 1.46 | |
| % rehospitalized in 4–7 days | FS | 3.28 | 3.35 | 3.58 | 3.77 | 3.89 | 3.94 | 3.95 | 4.02 |
| HB | 3.18 | 3.13 | 3.25 | 3.19 | 3.19 | 3.22 | 3.11 | 3.03 | |
| % rehospitalized in 8–30 days | FS | 12.57 | 12.78 | 13.31 | 13.59 | 13.91 | 13.95 | 14.04 | 13.89 |
| HB | 14.36 | 14.46 | 14.67 | 14.58 | 14.27 | 14.02 | 13.56 | 13.33 | |
| Selected patient's characteristics | |||||||||
| Age | FS | 80.96 | 80.85 | 80.74 | 80.67 | 80.55 | 80.34 | 80.25 | 80.21 |
| HB | 78.77 | 78.82 | 78.85 | 78.79 | 78.75 | 78.74 | 78.78 | 78.89 | |
| Hospital Elixhauser comorbidity index | FS | 2.25 | 2.30 | 2.34 | 2.40 | 2.45 | 2.49 | 2.54 | 2.60 |
| HB | 2.20 | 2.26 | 2.31 | 2.37 | 2.41 | 2.46 | 2.51 | 2.58 | |
| Length of hospital stay | FS | 10.84 | 10.81 | 10.56 | 10.35 | 10.19 | 10.10 | 9.74 | 9.50 |
| HB | 8.08 | 8.21 | 8.20 | 8.15 | 7.99 | 7.89 | 7.64 | 7.53 | |
| Percent with an ICU stay in the hospital | FS | 26.60 | 27.53 | 28.26 | 29.35 | 30.36 | 31.33 | 31.97 | 32.55 |
| HB | 31.17 | 31.47 | 31.54 | 31.83 | 32.05 | 32.33 | 31.84 | 32.06 | |
The 30-day rehospitalization rate of HB SNF patients declined by one percentage point, whereas among freestanding (FS) facilities, the rehospitalization rate climbed by several percentage points. Rapid “bounce-back” (1–3 days) rehospitalizations increased for both types of facilities but more for FS. Other rehospitalizations decreased for HB facilities and increased for the FS ones.
Table 1 also presents the trends in acuity measures of patients admitted to different types of SNFs. Although these findings are not definitive evidence that hospitals have tended to discharge patients with more severe conditions to FS SNFs, the average acuity of patients admitted to FS SNFs has increased over time. The proportion of discharges that had spent time in the hospital ICU increased overall during the study period, but substantially more for patients entering FS facilities. Similarly, the average length of hospital stay and the average age of discharges to SNF declined more sharply for FS in comparison with HB facilities.
The First Stage
To show the relationship between our instrument and SNF closures, we plotted the change in both types of beds between 1999 and 2006 against zip code population density using a local linear regression smoother in Figure 1. It is obvious that zip codes with high population density lost more HB beds (and not FS beds) during our study period. Table 2 quantifies this observed relationship in the first stage of 2SLS estimation of the baseline model. We find that the interaction of time and population density is very highly correlated with the supply of HB beds with a t-statistic of 13.3, whereas there is no such statistically significant relationship with respect to the number of FS beds in the area. In addition, the acuity indices as well as the share of FFS MBs discharged to SNF are not correlated with HB bed supply, suggesting that changes in bed supply do not affect the observed acuity of the patients discharged to SNF significantly (see Appendix; Table 1).
Figure 1.
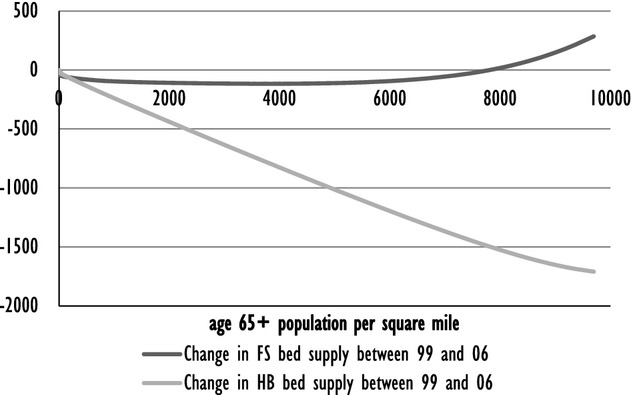
Local Linear Regression Plotting of Change in Bed Supply of HB and FS SNFs between 1999 and 2006 onto Zip Code Population Density
Table 2.
Estimated Effect of Instrumental Variable (Population Density Interacted with Time) on Different Types of NH Bed Supply
| (1) | (2) | |
|---|---|---|
| 100 HB Beds within 22 km | 100 FS Beds within 22 km | |
| Time × Population density | −0.0293** | 0.0062 |
| [−13.26] | [0.41] | |
| Control variables | Yes | Yes |
| Year fixed effects | Yes | Yes |
| Zip code fixed effects | Yes | Yes |
| Observations | 201,360 | 201,360 |
| R-squared | 0.985 | 0.999 |
Notes. Each observation is weighted by the number of patients discharged to NH from that zip code in that year. Control variables include average age, fraction of black, fraction of female, average length of stay at the hospital before discharge, fraction of patients treated in ICU, average Medicare reimbursement, mean Deyo and Elixhauser indexes among the patients in our sample, number of Medicare beneficiaries (MB), fraction of MB enrolled in Managed care, fraction of MB died in corresponding year, and fraction of MB who are in our sample of corresponding zip code year. Robust t-statistics calculated by clustering the errors at state level are in the square brackets. Detailed results of regression presented in column (1) are presented in column (1) of Appendix Table 1.
p < .01.
The Multivariate Model
The results of the baseline two-stage least-squares model are shown in Table 3 along with the results of the ordinary least-squares analysis. The coefficients of the effect of HB bed supply on SNF rehospitalizations using the 2SLS model are larger than the ones obtained from OLS for all four measures of rehospitalization. We tested the endogeneity of HB bed supply using Durbin-Wu-Hausman chi-square test and rejected the null hypothesis of exogeneity at .1 percent level of significance.
Table 3.
Estimated Effect of Different Types of Bed Supply on Rehospitalization Rate
| Estimation Method | Explanatory Variables | 1–30 Days | 1–3 Days | 4–7 Days | 8–30 Days |
|---|---|---|---|---|---|
| OLS with zip code and year fixed effects | 100 FS beds within 22 km | −0.0414* [−1.811] | −0.00139 [−0.954] | −0.0162** [−2.630] | −0.0229 [−1.267] |
| 100 HB beds within 22 km | −0.112*** [−4.525] | −0.008*** [−2.689] | −0.048*** [−3.748] | −0.055*** [−3.830] | |
| 2SLS with zip code and year fixed effects† | 100 FS beds within 22 km | −0.0499** [−2.546] | −0.00213 [−1.557] | −0.0185*** [−3.075] | −0.0278* [−1.776] |
| 100 HB beds within 22 km | −0.194*** [−5.253] | −0.015*** [−4.188] | −0.0688*** [−3.109] | −0.103*** [−3.926] |
Notes. The sample size is 201,360 and each observation is weighted by the number of patients discharged to NH from that zip code in that year. Control variables include zip code and year fixed effects, average age, fraction of black, fraction of female, average length of stay at the hospital before discharge, fraction of patients treated in ICU, average Medicare reimbursement, mean Deyo and Elixhauser indexes among the patients in our sample, number of Medicare beneficiaries (MB), fraction of MB enrolled in Managed care, fraction of MB died in corresponding year, and fraction of MB who are in our sample of corresponding zip code year. Robust t-statistics calculated by clustering the errors at state level are in the square brackets.
Here only HB bed supply is instrumented and the IV is population density interacted with time. Corresponding first stage is reported in column (1) of Table 2 and Appendix Table 1.
***p < .01, **p < .05, *p < .1.
We undertook a variety of sensitivity tests of our basic model to test it under alternative assumptions. Each row in Table 4 presents the result of an alternative specification of the baseline model. Inclusion of MDS assessment case mix acuity measures reduces the number of zip codes in the model, resulting in a slightly diminished estimated effect of HB bed supply (row 2 of Table 4).
Table 4.
Estimated Effect of HB Bed Supply on 30-Day Rehospitalization under Different Model Specifications
| Model Specification | N | OLS | 2SLS |
|---|---|---|---|
| (2) Including MDS variables as zip code aggregates | 199,861 | −0.104*** | −0.166*** |
| (3) Including zip code variables interacted with time | 201,280 | −0.0770*** | −0.125*** |
| (4) Unweighted by discharge volume | 201,360 | −0.106*** | −0.238*** |
| (5) For years 1999–2002 | 100,680 | −0.167*** | −0.352*** |
| (6) For years 2003–2006 | 100,680 | −0.0509 | −0.109** |
| (7) Bed supply per 1,000 MB as explanatory variable | 201,360 | −0.00731 | −0.124*** |
| (8) No. of patients rehospitalized as dependent variable | 201,360 | −0.333 | −0.701*** |
| (9) RUGs CMI less than median | 192,297 | −0.0489** | −0.0402 |
| (10) RUGs CMI more than or equal to median | 190,905 | −0.164*** | −0.224*** |
| (11) % of HB beds among all bed supply and HHI as explanatory variable | 183,212 | −.005 | −.924*** |
Note. All the regressions are estimated using zip code fixed effects. All the regressions except rows 4 and 8 are weighted by the number of patients discharged to any NH from a given zip code in a given year. T-statistics and the *s are robust obtained clustering by state. Different row represent different specification and corresponding first stages are reported in same numbered columns in Appendix Table 1. Row 2 presents the result with three patient average acuity variables calculated using CHESS, ADL, and NCMI indexes from MDS. Third row includes interaction of time with distance of the nearest hospital, percentage of rural population, and per capita income, which are time-invariant zip code level variables calculated from census 2000. Row 4 is the estimation of the baseline with our weights. Rows 5 and 6 show the result using observations between 1999 and 2002 and 2003 and 2006, respectively. Row 7 represents model where the bed-supply variables are deflated with number of Medicare beneficiaries in corresponding zip code year. Row 8 represents the model where the dependent variable is total number of rehospitalization event in a given zip code year. Rows 9 and 10 are based on 50% of the individuals divided using RUGs CMI. Row 11 presents the coefficient of share of HB beds among all supplied beds and obtained using a model where HB and FS bed supply variables in baseline are substituted with share of HB beds and HHI.
***p < .01, **p < .05, *p < .1.
Row 3 of Table 4 shows the results after including the differential trend with respect to different zip code characteristics. Changes in HB bed supply over time within zip codes vary significantly with the fraction of the rural population in zip codes but not with per capita income or distance to the nearest hospital (column 3 of Appendix Table 1). Inclusion of interactions (especially with the fraction of rural population) as additional control variables reduces the magnitude of the effect of HB bed supply obtained.
Row 4 presents the baseline model without weighting by the number of hospital discharges to SNF. When the baseline model is estimated without weights, the effect of HB bed supply becomes larger (−.238 vs −.194), likely due to the heterogeneous effect of bed supply, that is, an increase of 100 HB beds in an area with a large number of hospital discharges to SNF will have a much smaller effect compared with similar increases in areas with fewer discharges.
Rows 5 and 6 present our baseline model separately for 1999–2002 and for 2003–2006 to determine whether the strength of the HB bed loss effect is stronger when temporally closer to the BBA. The effect is much larger in the first 4 years after the introduction of PPS for SNF than is the case for subsequent years (row 5 vs 6 of Table 4).
Models 7 and 8 show that similar effects of HB bed supply are observed when we use per capita bed supply instead of the absolute number of beds or absolute number of rehospitalizations instead of the rehospitalization rate. The estimated coefficients in these two models are not directly comparable with the baseline model as we calculated the effect size in terms of extra rehospitalizations due to closure and this figure is slightly larger than the benchmark model. As shown in rows 9 and 10 of Table 4, the effect of HB bed supply has a statistically insignificant effect on rehospitalization of patients with low CMI acuity but a large effect on the patients with high CMI acuity. Finally, model 11 shows that FS facilities are not perfect substitutes for HB SNFs and increases in the share of HB beds in total bed supply reduce the rehospitalization rate. The estimated coefficient suggests that if the percentage of HB beds among the total bed supply in that area increases by 1, the percentage of patients rehospitalized within 30 days of admission to SNF declines by 1. We did not find any significant relationship between competition and rehospitalization, which is most likely due to the fact that HHI in this case is endogenous.
The negative effect of HB SNF closures on SNF patient rehospitalization in a given area is a relationship that is robust across most specifications. The most conservative estimate (IV estimate of model 4) suggests that a decrease of 100 HB nursing home beds within a 22 km radius of a zip code increases the 30-day rehospitalization rate by 0.13 percent. Thus, had the number of HB beds remained constant over the study period, about 12,000 rehospitalizations could have been avoided. Alternatively, if rehospitalization had remained at the 1999 rate throughout the study period, we would have observed about 100,000 fewer 30-day rehospitalizations, with about 12 percent of these extra hospitalizations due to closure of HB homes. Similarly, about 20 percent of 1–3 days, 13 percent of 4–7 days, and 9 percent of 8–30 days extra rehospitalizations over the study period could have been avoided if there had been no reduction in HB beds. Using the baseline model, the estimated number of rehospitalizations that could have been avoided is 18,000.
Discussion
PPS for Medicare nursing home reimbursement was introduced to limit the growing cost of postacute care. One consequence of this policy was that many HB facilities were closed or sold by their parent hospital corporations due to lower reimbursements under PPS relative to their operating costs. Before SNF PPS, 40 percent of all hospital discharges to postacute SNF care were sent to HB SNF facilities. As these facilities closed, FS facilities filled the breach. Our study finds that a consequence of this policy change was increased rehospitalization from SNF, a phenomenon that contributed to the general increase experienced by Medicare beneficiaries over the past decade (Jencks et al., 2009; Mor et al. 2010).
The increasing acuity of patients discharged from hospital to SNF over the course of our study clearly reveals a faster increase for those entering FS facilities, apparently in direct response to closure of HB facilities. Our results indicate that after the implementation of BBA, hospitals discharged their patients to a wider array of SNFs in the area rather than concentrating them in a small number of partners. As this group of SNFs began to fill the gap left by closing HB facilities, hospitals were increasingly discharging less medically stable patients to SNF. As FS SNFs historically had fewer nurses and a less-skilled complement of staff, they may have had more difficulty serving these complex patients, particularly given the limited role of physicians in FS SNFs (Angelelli et al. 2002; Katz et al. 2000). The fact that we see a much stronger effect of HB bed loss shortly after BBA than later is consistent with this interpretation. This suggests that over time FS SNFs may have become more capable of handling more acute patients.
Although the proportion of rapid bounce back (i.e., within 72 hours) rehospitalizations increased much faster than the other two types of rehospitalization over the course of the study, our results reveal that HB facilities were more effective in restraining growth of such bounce backs. This implies that HB facilities may be more effective at avoiding early rehospitalizations, perhaps due to the proximity of physicians and higher levels of nurse staffing. Consistent with these findings, our results reveal that closure of HB SNFs has a much larger adverse effect on patients with higher case mix. As the case mix acuity of hospital discharges to SNFs has continued to increase, we might expect rehospitalizations to increase without significant improvements in the levels of clinical care available in FS SNFs.
One major limitation of our analysis is that the exclusion restriction assumption of the IV might be too strong. Population density is correlated with variables like urban location, and a differential trend in patient characteristics or policies affecting the health outcome might be present with respect to such variables. We explicitly controlled for a few such differential trends by incorporating the share of the rural population, proximity to hospital, and per capita income that might be correlated with population density in zip codes. In addition, we did not observe differential trends in any of our observed acuity variables with respect to population density or share of rural population in the zip code.
Another limitation is that we only included patients using postacute care in an SNF. White and Seagrave (2005) found that if a hospital loses its HB SNF, patients are somewhat more likely to go to non-SNF-based postacute care such as an independent rehabilitation facility (IRF). However, in our data, we did not find any association between share of FFS patients discharged to SNF and supply of HB SNF beds.
The fact that we observe an increase in rehospitalization in those areas which lost HB facilities and beds, presumably because hospital discharges went to FS SNFs that were not prepared to care for such sick patients, has substantial implications for the future of hospital-SNF collaborations. It is critical that we better understand what it is about the relationship between a hospital and a SNF that facilitates smooth transfer of patients during the discharge process. Indeed, in light of the ACA-imposed policy changes governing rehospitalizations, it will be imperative for hospital and SNF administrators as well as clinicians in both settings to develop protocols to insure smooth transitions of patients from hospital to SNF.
Acknowledgments
Joint Acknowldgment/Disclosure Statement: This work was supported by the National Institute on Aging grant P01AG027296 (PI: Vincent Mor). Some preliminary results from this study have been presented at the Academy Health Annual Research Meeting, June 12–14, 2011, held in Seattle, WA. No conflicts of interest or financial disclosures are declared by any author of this study.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Table S1: Regression of Hospital-Based (HB) Bed Supply onto and Instrumental and Other Explanatory Variables (First-Stage Relationship) under Alternative Specification.
Table S2: Estimated Effect of Different Types of Bed Supply on Rehospitalization by Different Day Interval under Different Model Specifications.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Angelelli J, G D, Intrator O, Gozalo P, Laliberte L, Mor V. “Access to Postacute Nursing Home Care before and after the BBA. Balanced Budget Act”. Health Affairs (Millwood) 2002;21(5):254–64. doi: 10.1377/hlthaff.21.5.254. [DOI] [PubMed] [Google Scholar]
- Banaszak-Holl J, Zinn JS, Mor V. “The Impact of Market and Organizational Characteristics on Nursing Care Facility Service Innovation: A Resource Dependency Perspective”. Health Services Research. 1996;31(1):97–117. [PMC free article] [PubMed] [Google Scholar]
- Bishop CE, Dubay LC. “Medicare Patient Access to Post-Hospital Skilled Nursing Facility Care”. Inquiry. 1991;28(4):345–56. [PubMed] [Google Scholar]
- Castle NG, Engberg J, Liu D. “Have Nursing Home Compare Quality Measure Scores Changed over Time in Response to Competition?”. Quality and Safety in Health Care. 2007;16:185–91. doi: 10.1136/qshc.2005.016923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra A, Skinner J. Cambrige, MA: National Bureau of Economic Research; 2003. “Geography and Racial Health Disparities”. 9513: NBER working paper. [Google Scholar]
- Dalton K, Howard HA. “Market Entry and Exit in Long-Term Care: 1985–2000”. Health Care Financing Review. 2002;24(2):17–32. [PMC free article] [PubMed] [Google Scholar]
- Donelan-McCall N, Eilersen T, Fish R, Kramer A. Small Patient Population and Low Frequency Event Effects on the Stability of SNF Quality Measures. Washington, DC: Medicare Payment Advisory Commission; 2006. [Google Scholar]
- Feng Z, Lepore M, Clark MA, Tyler D, Smith DB, Mor V, et al. “Geographic Concentration and Correlates of Nursing Home Closures: 1999–2008”. Archives of Internal Medicine. 2011;171(9):806–13. doi: 10.1001/archinternmed.2010.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fries BE, Schneider DP, Foley WJ, Gavazzi M, Burke R, Cornelius E. Refining a Case-Mix Measure for Nursing Homes: Resource Utilization Groups (RUG-III) Medical Care. 1994;32(7):668–85. doi: 10.1097/00005650-199407000-00002. [DOI] [PubMed] [Google Scholar]
- Garnick D, Luft H, Robinson J, Maerki S, McPhee S. “Appropriate Measures of Hospital Market Areas”. Health Services Research. 1987;22:69–90. [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC, Hirth RA. “Competitive Spillovers across Non-Profit and For-Profit Nursing Homes”. Journal of Health Economics. 2003;22(1):1–22. doi: 10.1016/s0167-6296(02)00093-0. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, O'Malley AJ, Barhydt NR. “The Costs and Potential Savings Associated with Nursing Home Hospitalizations”. Health Affairs (Millwood) 2007;26(6):1753–61. doi: 10.1377/hlthaff.26.6.1753. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Stewart KA, Broderick SM, Coots LA. “Predictors of Nursing Home Hospitalization: A Review of the Literature”. Medical Care Research and Review. 2008;65(1):3–39. doi: 10.1177/1077558707308754. [DOI] [PubMed] [Google Scholar]
- Hirdes JP, Frijters DH, Teare GF. “The MDS-CHESS Scale: A New Measure to Predict Mortality in Institutionalized Older People”. Journal of the American Geriatrics Society. 2003;51(1):96–100. doi: 10.1034/j.1601-5215.2002.51017.x. [DOI] [PubMed] [Google Scholar]
- Hirth RA. “Consumer Information and Competition between Nonprofit and For-Profit Nursing Homes”. Journal of Health Economics. 1999;18(2):219–40. doi: 10.1016/s0167-6296(98)00035-6. [DOI] [PubMed] [Google Scholar]
- Intrator O, Hiris J, Berg K, Miller SC, Mor V. “The Residential History File: Studying Nursing Home Residents’ Long-Term Care Histories(*)”. Health Services Research. 2011;46(Pt 1):120–37. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intrator O, Zinn J, Mor V. “Nursing Home Characteristics and Potentially Preventable Hospitalizations of Long-Stay Residents”. Journal of the American Geriatrics Society. 2004;52(10):1730–6. doi: 10.1111/j.1532-5415.2004.52469.x. [DOI] [PubMed] [Google Scholar]
- Intrator O, Grabowski DC, Zinn J, Schleinitz M, Feng Z, Miller S, et al. “Hospitalization of Nursing Home Residents: The Effects of States' Medicaid Payment and Bed-Hold Policies”. Health Services Research. 2007;42(4):1651–71. doi: 10.1111/j.1475-6773.2006.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jencks SF, Williams MV, Coleman EA. “Rehospitalizations among Patients in the Medicare Fee-for-Service Program”. New England Journal of Medicine. 2009;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Katz PR, Karuza J, Intrator O, Zinn J, Mor V, Caprio T, Caprio A, Dauenhauer J, Lima J. “Medical Staff Organization in Nursing Homes: Scale Development and Validation”. Journal of the American Medical Directors Association. 2000;10(7):498–504. doi: 10.1016/j.jamda.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitchener M, Bostrom A, Harrington C. “Smoke without Fire: Nursing Facility Closures in California, 1997–2001”. Inquiry. 2004;41(2):189–202. doi: 10.5034/inquiryjrnl_41.2.189. [DOI] [PubMed] [Google Scholar]
- Konetzka RT, Spector W, Limcangco MR. “Reducing Hospitalizations from Long-Term Care Settings”. Medical Care Research and Review. 2008;65(1):40–66. doi: 10.1177/1077558707307569. [DOI] [PubMed] [Google Scholar]
- Manton KG, Stallard E, Woodbury MA. “Home Health and Skilled Nursing Facility Use: 1982–90”. Health Care Financing Rev. 1994;16(1):155–86. [PMC free article] [PubMed] [Google Scholar]
- Mor V, Intrator O, Feng Z, Grabowski DC. “The Revolving Door of Rehospitalization from Skilled Nursing Facilities”. Health Affairs (Millwood) 2010;29(1):57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JN, Fries BE, Morris SA. “Scaling ADLs within the MDS”. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 1999;54(11):M546–53. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- Mukamel DB, Spector WD, Bajorska A. “Nursing Home Spending Patterns in the 1990s: The Role of Nursing Home Competition and Excess Demand”. Health Services Research. 2005;40(4):1040–55. doi: 10.1111/j.1475-6773.2005.00394.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyman JA. “The Effect of Competition on Nursing Home Expenditures under Prospective Reimbursement”. Health Services Research. 1988;23(4):555–74. [PMC free article] [PubMed] [Google Scholar]
- Saliba D, Kington R, Buchanan J, Bell R, Wang M, Lee M. “Appropriateness of the Decision to Transfer Nursing Facility Residents to the Hospital”. Journal of the American Geriatrics Society. 2000;48(2):54–163. doi: 10.1111/j.1532-5415.2000.tb03906.x. [DOI] [PubMed] [Google Scholar]
- Schaffer M. “xtivreg2: Stata Module to Perform Extended IV/2SLS, GMM and AC/HAC, LIML and K-class Regression for Panel Data Models”. 2010. Available at: http://ideas.repec.org/c/boc/bocode/s456501.html [accessed on September 25, 2012]
- Schlenker R, Shaughnessy P, Yslas I. “The Effect of Case Mix and Quality on Cost Differences between Hospital-Based and Freestanding Nursing Homes”. Inquiry. 1983;20(4):361–8. [PubMed] [Google Scholar]
- Stearns SC, Dalton K, Holmes GM, Seagrave SM. “Using Propensity Stratification to Compare Patient Outcomes in Hospital-Based versus Freestanding Skilled-Nursing Facilities”. Medical Care Research and Review. 2006;2006(63):599. doi: 10.1177/1077558706290944. [DOI] [PubMed] [Google Scholar]
- White C, Seagrave S. “What Happens When Hospital-Based Skilled Nursing Facilities Close? A Propensity Score Analysis”. Health Services Research. 2005;40(6):1883–97. doi: 10.1111/j.1475-6773.2005.00434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman S, Gruber-Baldini AL, Hebel JR, Burton L, Boockvar K, Taler G, Quinn CC, Magaziner J. “Nursing Home Characteristics Related to Medicare Costs for Residents with and without Dementia”. American Journal of Alzheimer's Disease & Other Dementias. 2008;23(1):57–65. doi: 10.1177/1533317507308778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinn JS. “Market Competition and the Quality of Nursing Home Care”. Journal of Health Politics, Policy and Law. 1994;19(3):555–82. doi: 10.1215/03616878-19-3-555. [DOI] [PubMed] [Google Scholar]
- Zinn JS, Mor V, Feng Z, Intrator O. “Determinants of Performance Failure in the Nursing Home Industry”. Social Science and Medicine. 2009;68:933–40. doi: 10.1016/j.socscimed.2008.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwanziger J, Mukamel DB, Indridason I. “Use of Resident-Origin Data to Define Nursing Home Market Boundaries”. Inquiry. 2002;39:56–66. doi: 10.5034/inquiryjrnl_39.1.56. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


