Abstract
This meta-analysis (N = 110,092) assessed the efficacy of HIV-prevention interventions across samples with higher and lower concentrations of Latinos/Latin Americans. Findings indicated that groups with higher percents of Latinos increased condom and HIV-related knowledge to a lesser extent than groups with lower percents of Latinos/ Latin Americans. Moreover, groups with greater percents of Latinos/Latin Americans only benefited from intervention strategies that included threat-inducing arguments, whereas groups with lower percents of Latinos/Latin Americans benefited from numerous strategies. In addition, groups with greater percents of Latinos/Latin Americans increased condom use when interventions were conducted by a lay community member, whereas groups with lower percents of these groups increased condom use the most in response to experts. Not surprisingly, there were important differences among Latinos/Latin Americans with different education levels, different genders, and US/Latin American nationality.
Keywords: HIV prevention, Knowledge, Behavior, Intervention, Ethnicity, Culture
Introduction
Although during recent years Hispanics or Latinos accounted for 13% of the total population living in the United States (United States Census Bureau, 2003), they currently represent 19% of the total number of new AIDS (Acquired Immunodeficiency Syndrome) cases (CDC Division of HIV/AIDS Prevention, 2002). Further, several countries of Latin America show increases in infection that place Latinos in those places at risk (University of California at San Francisco, 2005). The rapid progression of AIDS among Latinos (Latino Commission on AIDS, 2004; National Alliance of State and Territorial AIDS Directors, n.d.) combined with their unique socio-demographic characteristics (poverty, low literacy and language skills, and limited access to health care) demand knowledge about preventive strategies appropriate for this population. Therefore, the objective of the present meta-analysis was to systematically asses the efficacy of HIV/AIDS prevention interventions for the Latino1 and Latin American population. This objective was achieved by comparing interventions with greater and smaller percents of Latinos/Latin Americans.
In the past, several meta-analyses estimated the outcomes of HIV-prevention programs, particularly condom use (Albarracín, Gillette, Glasman, Durantini, & Ho, 2005; Johnson, Carey, Marsh, Levin, & Scott-Sheldon, 2003; Weinhardt, Carey, & Johnson, 1999). For example, Albarracín et al. (2005) revealed that HIV-prevention strategies produce small to moderate behavioral effects across the board, whereas Albarracín et al. (2003) reported no significant impacts across populations and strategies. Importantly, however, to the best of our knowledge, no prior meta-analysis has concentrated on the efficacy of programs among Latino/Latin Americans vs. non-Latino/Latin American audiences. In fact, there has been a single systematic review of the literature of these interventions for Latino audiences (Darbes, Kennedy, Peersman, & Zohrabyan, 2002). This study found that successful interventions were theory based, culturally sensitive, gender specific, of longer duration, and provided participants with skills training. Although this review was a valuable first step, it did not entail a calculation of the impact of the different programs (i.e., effect sizes). It also failed to consider a number of factors that we were interested in investigating, including the efficacy of interventions using attitude, normative, behavioral or threat inducing arguments, or the type of setting where interventions were conducted, like health clinics or community centers. Moreover, understanding what is unique about a certain population (e.g., Latinos) requires precise comparisons with other groups. These comparisons demand introducing percent of Latinos//Latin Americans as a moderator, which we attempted to do in this meta-analysis.
Our review included studies that specified the percent of Latinos even when that percent equaled zero. Thus, we were able to divide samples into two groups, depending on whether samples had an average percent of Latinos/Latin Americans that was below or above 50%. Our analyses then assessed the effects of different prevention characteristics on behavioral and knowledge change across these two groups. These analyses were conducted by also taking into account education, gender, and US vs. Latin-American nationality.
To test the effects of intervention contents, our meta-analysis classified the different intervention strategies as including (a) attitudinal arguments designed to increase the perceived desirability of the behavior (Ajzen & Madden, 1986; Fishbein & Ajzen, 1975), (b) normative arguments describing other people’s support of condom use (Ajzen & Madden, 1986; Fishbein & Ajzen, 1975), (c) behavioral skills arguments designed to verbally teach skills and increase perceptions that the behavior is easy and up to the individual (Bandura, 1986), (d) fear- or threat-inducing arguments designed to increase sensitivity to HIV risk (Rosenstock, Strecher, & Becker, 1994), (e) information about the transmission and prevention of the disease, and (Fishbein et al., 1992), (f) actual training in behavioral skills, including interpersonal skills (e.g., condom negotiation), condom use skills (condom application), and self-management skills like dealing with condom use in difficult situations (Fishbein et al., 1992).
Scholars working on HIV prevention for Latinos have criticized the above-described models for their failure to consider the cultural and social context of sexual behavior (Marín, Gomez, Tschann,&Gregorich, 1997). For example, gender roles differ between Latino men and women, partly because the machismo culture stresses virility, independence, physical strength, and sexual prowess. Thus, machismo creates a great cultural divide between men and women, which entails power distance but also a tendency for men to believe that they should cherish and protect women. Given these differential gender roles, Latinos/Latin Americans may present many gender differences in response to HIV-prevention interventions (Gómez & Marín, 1996; Ortiz-Torres, Serrano-Garcia, & Torres-Burgos, 2000). In this regard, we examined how gender moderates the effects of the different prevention strategies, sources, and settings.
Importantly, Hortensia Amaro (1998) cautions that propositions about Latino culture have not always taken into account important socioeconomic factors, such as education, socioeconomic status, participation in the labor force, and residence in rural versus urban areas. Although our meta-analysis did not have information about all these variables, it did assess the effect of education on HIV prevention efficacy. Further, nationality was considered because the living conditions and epidemic context of Latinos in the US and Latin-American countries (studies included in our meta-analysis were from Brazil, Ecuador, Honduras, Mexico, Nicaragua, Peru, and Puerto Rico) differ.
Our study also explored the effect of intervention sources on behavioral and knowledge change for groups with different rates of Latinos/Latin Americans. In particular, researchers and practitioners have debated if experts or lay community members (or peers) should conduct HIV-prevention interventions. The use of lay community members as sources in HIV prevention has become popular in recent years (Turner & Shepherd, 1999) and has been recommended for HIV prevention among Latinos (Amaro, 1995; Center for AIDS Prevention Studies, 2002; Ortiz-Torres et al., 2000). Nonetheless, a prior meta-analysis of this issue found that experts are more successful than peers (Durantini, Albarracín, Earl, & Mitchell, 2006; Schaalma, Abraham, Gillmore, & Kok, 2004) but that similarty in ethnicity, gender, and/or age matters for some groups. Given that these issues have not been examined for Latinos/Latin Americans, we considered them in our meta-analysis.
Finally, the context and type of presentation used in prevention programs may also have an impact on HIV prevention interventions for Latinos/Latin Americans. It was therefore important to determine the kind of setting (clinics, community settings) that is most appropriate, as well as whether presentations directed to groups or individuals are more or less efficacious in increasing Latinos’ condom use and HIV-related knowledge.
Method
Review and Inclusion Criteria
We conducted a review of reports that were available by June of 2005. First, we conducted a computerized search of Medline, PsycINFO, ERIC, Social Science Citation Index, and Dissertation Abstracts International using a number of keywords, including “HIV (AIDS) messages,” “HIV (AIDS) communications,” “HIV (AIDS) interventions,” “HIV (AIDS) prevention,” and “health education and HIV (AIDS).” Second, we manually searched all available issues appearing during or after 1985 of the journals, AIDS, AIDS Education and Prevention, AIDS Research, American Behavioral Scientist, American Journal of Community Psychology, American Journal of Nursing, American Journal of Public Health, Basic and Applied Social Psychology, Communication Research, Communications, Health Communication, Health Education Quarterly, Health Education Research, Health Psychology, Journal of the American Medical Association, Journal of Applied Communication Research, Journal of Applied Social Psychology, Journal of Consulting and Clinical Psychology, Journal of Personality and Social Psychology, Journal of Sex Research, Medical Anthropology, Morbidity and Mortality Weekly Report, Qualitative Health Research, and Social Science and Medicine. We also checked cross-references in the obtained reports, sent requests for information to researchers funded by National Institutes of Health (NIH), and contacted selected experts and agencies who could provide relevant materials.
We used several eligibility criteria to gather an optimal, relatively homogenous sample of studies that could serve our objectives well, and met our four-fold inclusion criteria. First, studies were included if they described the outcomes of an intervention to promote the use of condoms. We excluded interventions designed exclusively to promote safer intravenous-drug-related behaviors or abstinence from sex. Second, for inclusion, studies had to report outcomes of various types of interventions. Therefore, we included simple communications, as well as interventions in which recipients engaged in behaviors as part of the intervention (i.e., role-playing, practicing condom-use related skills, and HIV counseling and testing). Third, we only included studies that provided information to calculate the effect of interventions over time and excluded reports without a pretest. Most of the reports obtained pre and posttest measures on the same sample, but others used independent samples at each time (for an explanation of the advantages of the use of independent samples for longitudinal studies, see Cook & Campbell, 1979). Finally, we selected all available Latin American studies as well as studies that reported the proportion of Latinos in the sample (e.g., 0% and 70%). Forty-eight studies, comprising 78 intervention groups and 27 control groups were excluded for not reporting the proportion of Latinos in the sample.
Coding of Study Characteristics
Two independent raters coded characteristics relevant to the report and the methods used in the studies. Inter-coder agreement for all categories included in the coding sheet was 85%, and intercoder-reliability coefficients were above .70 in all cases. Disagreements were resolved by discussion and further examination of the studies.
We recorded the percent of people from Latin background, and people from other backgrounds (European, Asian, and Native Americans). In addition, we recorded the percent of people in each sample who completed high school, and the percent of males in each sample. The percents of Latinos/Latin Americans and males were dichotomized for the main analyses in this paper. We also recorded the percent of males, the percent of participants who completed at least high school, and whether the study was conducted in the US or abroad.
We recorded the type of intervention and strategy used in each case. Passive strategies included (a) attitudinal arguments, such as discussions of the positive implications of using condoms for the health of the partners and for the romantic relationship, (b) normative arguments about support of condom use provided by friends, family members, or partners, (c) factual information (i.e., mechanisms of HIV, HIV transmission, HIV prevention), (d) arguments designed to model behavioral skills (what to do when partners do not want to use a condom, when recipients or their partners are sexually excited, and when alcohol or drugs are involved), and (e) threat-inducing arguments, such as discussions about the recipients’ personal risk of contracting HIV or other Sexually Transmitted Infections (STIs). We also recorded the use of active interventions, namely behavioral strategies to train audiences in condom-use promoting skills, and the administration of HIV counseling and testing. Strategies to induce behavioral skills comprised (f) condom-use skills (e.g., practice with unwrapping and applying condoms), (g) interpersonal skills (e.g., role playing of interpersonal conflict over condom use and initiation of discussions about protection), and (h) self-management skills (e.g., practice in decision making while intoxicated, avoidance of risky situations), whereas (i) HIV counseling and testing involved the administration of a seropositivity test as well as the counseling in place. When the counseling was described as involving specific arguments or training aspects, we coded for those in addition to noting the presence of counseling and testing. Finally, we kept a record of whether, prior to the posttest, the researchers provided research participants with condoms.
Based on the above-described coding, control groups were those to whom no passive or active intervention was applied, although some control participants received condoms as part of the study. These codes allowed us to establish the likely effects of each type of strategy and of mere condom provision.
We also coded studies for characteristics of the report, including the (a) publication year and (b) geographic area. We also recorded characteristics of the participants, including demographics of the target group as well as specific characteristics and behaviors of the target group that are associated with HIV-infection risk. To describe the target population, we retrieved the: (a) sample size, (c) percent of participants of African, Asian, and American-Indian descent; and (e) population of the city or village at the time the intervention was conducted.
Finally, we coded for methodological characteristics that related to intervention setup. Thus, we classified each intervention group according to (a) the setting of the intervention (i.e., whether the intervention was delivered in clinics or community settings. We also recorded (b) whether exposure to the communication was individual or in groups. Other features were also coded and are available upon request.
Retrieval of Effect Sizes
Two raters calculated effect sizes independently. Disagreements were checked with a third researcher and resolved by discussion. Raters were instructed to calculate effect sizes representing change from the pretest to the most immediate posttest. Efforts were made to calculate effect sizes for all available measures of the constructs of interest. When there was more than one measure of a construct in one particular study, we first calculated effect sizes for each one and then obtained the average, which was used as the effect size for that particular variable.
To represent change from pretest to posttest measures, we used Becker’s (1988) g, which is calculated by subtracting the mean at the posttest from the mean at the pretest and dividing the difference by the standard deviation of the pretest measure. This measure controls for the inflation in the standard deviation following treatment. Effect sizes were also derived from exact reports of t-tests, F-ratios, proportions, P-values, and confidence intervals. To derive effect sizes for within-subject studies, it is ideal to know the correlation between posttest and pretest measures to calculate effect sizes. Because some reports did not offer this information, we adopted procedures recommended by Becker (1988) as well as by Dunlap, Cortina, Vaslow, and Burke (1996). We explain these procedures when they become relevant.
We also estimated effect sizes when a report contained inexactly described P-values—such as when the authors indicated that a given finding was not significant at .05—using the appropriate within- or between-subjects procedures. Thus, a reported non-significant finding was estimated to have a probability of .99, whereas a significant finding was estimated to have a probability at the level of the cutoff value used in the study (e.g., .05 or .01). However, because the use of such reports may lead to incorrect estimations, we conducted separate analyses on the set of exactly reported effect sizes, as well as on all the effect sizes, including the ones estimated on the basis of inexactly reported p values. Because both sets of analyses yielded similar results, we only report the results that included all effect sizes.
We calculated effect sizes representing change in knowledge and condom use. For the sake of space, we excluded change in norms, control perceptions, intentions, behavioral skills, perceived severity, and perceived susceptibility. These additional measures can be made available upon request.
Knowledge
A large number of studies assessed the participant’s knowledge about HIV or AIDS, and typically comprised a series of statements that the participant evaluated as true or false (e.g., “The AIDS virus can be caught through ordinary close social contact, such as sitting next to an infected person,” Rigby, Brown, Anagnostou, Ross, & Rosser, 1989, p. 149). Knowledge scores in most cases were calculated by computing the percent of questions a participant answered correctly. When researchers reported statistics for individual items, we calculated effect sizes for each question and then averaged those effects into a global measure of change in knowledge.
Condom Use
Condom use measures included assessments on subjective frequency scales, as well as reports of the percent and number of times participants use condoms over a period of time. For example, the Community Demonstration Projects Research Group (CDC, 1993) asked participants “When you have vaginal sex with your main partner, how often do you use a condom?” (p. 11), and participants provided their response on a scale from 1 (every time) to 5 (never). To obtain a more precise report of condom use, Ploem and Byers (1997) asked participants to report the frequency of sexual intercourse over the previous four weeks, as well as the number of occasions of sexual intercourse for which condoms were used. The researchers then derived the percent of condom use for each participant. Similarly, Belcher et al. (1998) asked participants to list the first name of all of their sex partners in the previous 90 days. For each name listed, participants were then asked to identify the partner’s gender, the partner type (regular, casual, or new), the total frequency of vaginal sex, the frequency of condom-protected vaginal sex, the total frequency of anal sex, and the frequency of condom-protected anal sex. Percents were again derived based on relative frequencies.
Analytic Strategy
We calculated weighted mean effect sizes to examine change over time in intervention and control groups, and performed corrections for sample-size bias to estimate d. We used Hedges and Olkin’s (1985) procedures to correct the effects for sample-size bias, calculate weighted mean effect sizes, d., confidence intervals, and homogeneity statistics, Q, which test the hypothesis that the observed variance in effect sizes is no greater than that expected by sampling error alone. Calculations of the between-subject variance followed procedures developed by Hedges and Olkin (1985). For within-subjects designs, we calculated the variance of effect sizes using Morris’s (2000) procedures. Specifically, we performed calculations for the variance of within-subject effect sizes using three alternate correlations between pre- and posttest measures (see also, Albarracín et al., 2003, 2005). Thus, we assumed r = 0 and r = .99 as the most extreme values, and also imputed correlations from Project RESPECT (see Kamb et al., 1998), which provided moderate values of this association. Because results were similar regardless of the correlation we used, we present only the ones with the imputed correlations (see also Albarracín et al., 2003, 2005).
Computations of effect sizes were performed using fixed- and random-effects procedures. In the first case, one assumes a fixed population effect and estimates its sampling variance, which is an inverse function of the sample size of each group. The inverse of the effect size’s variance is used to weigh effect sizes prior to obtaining average values. Thus, effect sizes from studies with larger Ns are considered more precise and carry more weight than effect sizes obtained from studies with smaller sample sizes. These procedures are powerful and produce narrow confidence intervals (Wang & Bushman, 1999). In contrast, random-effects procedures are based on the assumption that the effect sizes are sampled from a population of effect sizes. Thus, the effect size from a given study results from sampling an effect size at random, but also contains measurement error, which is again an inverse function of the sample size in that particular study.
Because random-effects procedures use the variance of a sample of effect sizes as well as the variance in each study to estimate the variance in the population of effect sizes, the error term is larger and the procedure may overestimate Type I error (Hedges & Olkin, 1985; Hedges & Vevea, 1998; Hunter & Schmidt, 2000). Presumably, fixed-effects models are reasonable when one assumes that effect sizes vary as a result of a few, identifiable study characteristics, whereas random-effects models are appropriate when variation derives from multiple, unidentifiable sources (Raudenbush, 1994). Importantly, both sets of models yielded converging results. However, given that many of the random-effects models were non-significant, we restricted report to fixed-effects analyses.
The main analyses were weighted analyses of variance comparing treatments and controls across samples with higher and lower percents of Latinos. Other analyses looked at specific strategies, characteristics of the intervention facilitator, and intervention delivery. Further, many supplementary analyses were conducted. First, we crossed analyses of the Latin-background samples with gender, education, and nationality (US vs. Latin America). Second, our use of multiple conditions per study may imply greater statistical dependence within those conditions. Thus, we replicated all analyses with a sample of conditions with only one treatment per study. These analyses replicated most of the times and in no case altered our conclusions about associations between efficacy and percent of participants from Latin back-grounds. For the sake of space, we do not report these analyses.
Results
Description
Sample of Interventions
Our eligibility criteria yielded 142 studies, which provided 277 independent intervention groups and 73 independent control groups representing a total of 110,092 participants.2 These studies were conducted (see Table 1) in the US (282), Latin America (13), Europe (9), Africa (29), Asia (15), and Australia (2). Based on a split of the intervention groups into those with less and more than 50% Latinos/Latin Americans, 317 conditions were classified as under the mean and 33 as above the mean. The mean percent of Latinos/Latin Americans was 14.27. The means for the percent of Latinos/Latin Americans were 91.94 for samples with higher percents of Latinos/Latin Americans and 6.55 for samples with lower percents of Latinos/Latin Americans. In turn, the median was 100 and .70, respectively. Twenty-three studies had 100% participants from Latin backgrounds (10 from the US and 13 from Latin America).
Table 1.
Descriptive statistics (general characteristics of studies and demographic characteristics population)
| Variable | Intervention groups (k = 277) |
Control groups (k = 73) |
|---|---|---|
| General characteristics of the reports | ||
| Publication year | ||
| M | 1996.04 | 1995.86 |
| SD | 4.20 | 3.84 |
| Area where study was conducted | ||
| Africa | 6.9(19) | 13.7(10) |
| Asia | 4.7(13) | 2.7(2) |
| Australia | 2.7(2) | 2.7(2) |
| Europe | 1.8(5) | 5.5(4) |
| Latin America | 3.2(9) | 5.5(4) |
| US | 82.7(229) | 72.6(53) |
| Not identified | 9(32) | 10.1(10) |
| Latinos in sample | ||
| Less than 50% | 253 | 64 |
| M | 6.71 | 5.93 |
| SD | 10.54 | 10.49 |
| More than 50% | 24 | 9 |
| M | 94.06 | 86.29 |
| SD | 13.53 | 20.73 |
| Demographic characteristics of participants | ||
| Age | ||
| M | 25.59 | 24.45 |
| SD | 9.07 | 8.96 |
| % Male | 41.53 | 40.62 |
| Gender not indicated | .02 | .04 |
| % Completed high school | 29.20 | 32.20 |
| High school not indicated | 58.38 | 39.72 |
| % White | ||
| M | 31.50 | 32.45 |
| SD | 35.00 | 36.76 |
| % Black | ||
| M | 45.32 | 41.64 |
| SD | 38.90 | 39.67 |
| % Native American | ||
| M | .36 | .46 |
| SD | 1.36 | 1.21 |
| % Asian | ||
| M | 6.27 | 8.42 |
| SD | 20.57 | 23.38 |
| % Hispanic | ||
| M | 14.28 | 14.66 |
| SD | 26.88 | 29.19 |
| Other | ||
| M | 3.54 | 2.07 |
| SD | 13.46 | 3.99 |
We compared the characteristics of intervention and control groups summarized in Table 1 to detect systematic biases that may confound the reported differences in effect sizes across intervention and control groups. For that purpose, we used independent-sample t- and χ2 tests (Albarracín et al., 2003, 2005). Although intervention and control samples were highly comparable across most dimensions, high school completion was greater in control than intervention groups, t (157) = 5.18, P < .05. Thus, these findings are consistent with prior reports of comparability between studies with and without controls (Albarracin et al., 2003, 2005). This is important to analyze the effects of interventions in the absence of controls (Albarracin et al., 2003, 2005).
Relations Among Latino Ethnicity, Gender, Education, and Nationality
Many of our analyses had the objective of exploring the effects of gender, education, and nationality among samples with high percents of people from Latin backgrounds. Prior to this, however, we correlated percent of Latinos/Latin Americans in a sample with percent of males, percent of high school completion in a sample, and nationality. The only association was that studies in Latin American had more participants from Latin backgrounds than studies in the US (r = .16, P < .002). No other significant correlations emerged.
Efficacy
General Effects of Interventions Across Groups With Higher and Lower Percents of Latinos/Latin Americans, Genders, and Educational Levels
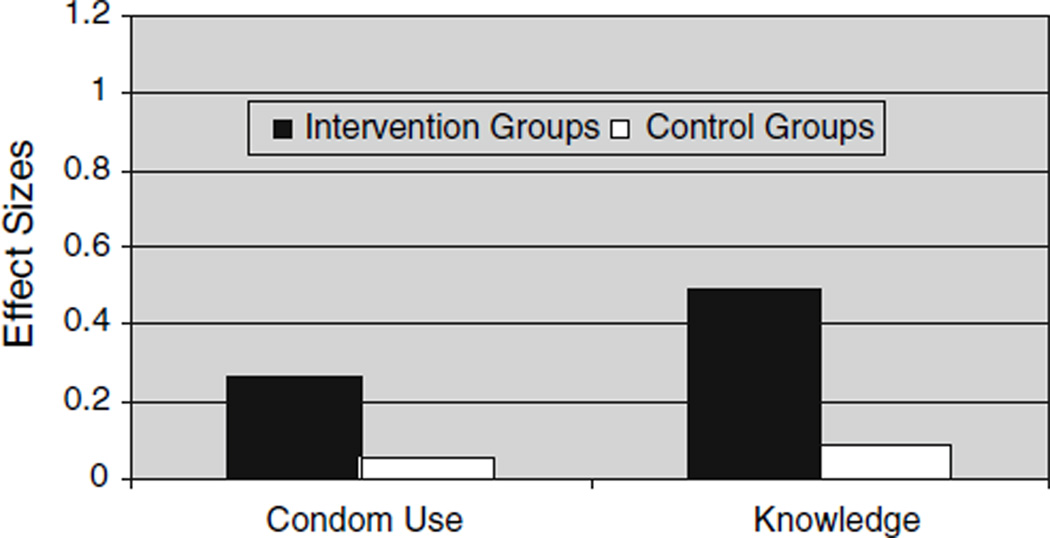
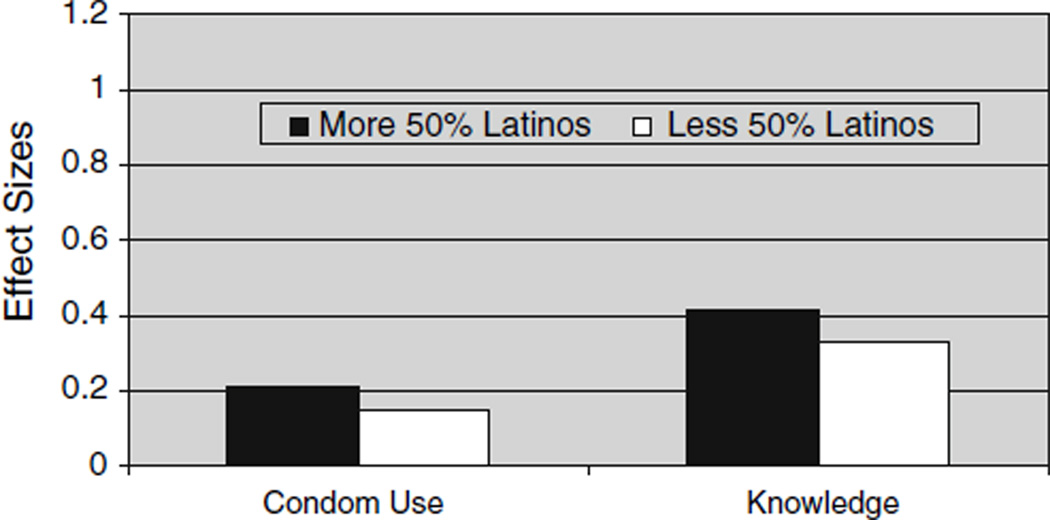
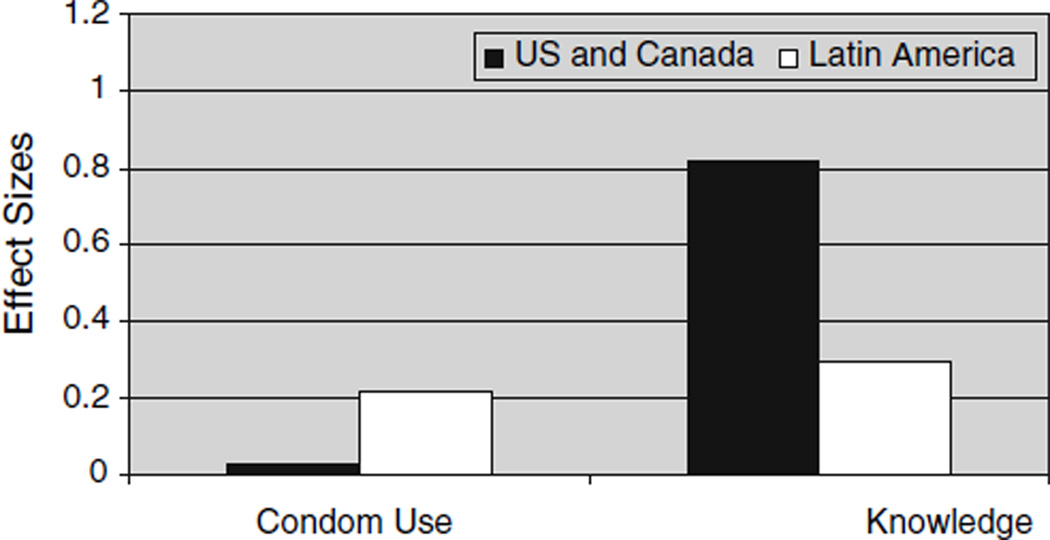
We first analyzed change as a function of group (intervention vs. control) and as a function of the percent of Latinos/Latin Americans in the sample. As Fig. 1 shows, intervention groups increased both their condom use (QB1 = 256.42) and their knowledge regarding HIV/AIDS related issues (QB1 = 832.19) to a greater extent than control groups. Figure 2 illustrates that intervention groups with a higher percent of Latinos/Latin Americans increased condom use less than those with a lower percent of Latinos/Latin Americans (d = .15 vs. .21, k = 207, QB1 = 9.10, P < .01). Intervention groups with more Latinos/Latin Americans also gained less HIV-related knowledge (Fig. 2) than those with fewer Latinos/Latin Americans (d = .33 vs. .41, k = 211, QB1 = 19.99, P < .001). So, in general the interventions perpetuated the gaps observed in the epidemic.
Fig. 1.
Condom use and knowledge increase: intervention groups vs. control groups
Fig. 2.
Condom use and knowledge increase: samples with more than 50%
Even when the comparisons across treatments and controls (see Table 1) were reassuring, contrasting all interventions with all control groups is insufficient to rule out two important rival hypotheses. First, considering interventions without controls allows for the possibility that spontaneous maturation might be responsible for the observed increases in condom use (see Cook & Campbell, 1979). Secondly, comparing interventions and controls that did not employ random assignment cannot control for selection biases, and particularly the possibility that the group assigned to the intervention was easier to change than the group assigned to the control. In light of these alternative hypotheses, an additional analysis was conducted in which we calculated scores representing controlled change. For this purpose, we selected only studies that employed random assignment as well as a control group, and subtracted the d representing change in the control group from the d representing change in the treatment group. The variance of the resulting Δ (Becker, 1988) equals the inverse of the sum of the variances of the ds that entered the calculation of Δ, and was used to derive a confidence interval for the overall efficacy of HIV prevention intervention when one selects only controlled randomized trials that had true control (k = 33). These analyses provided the same results.
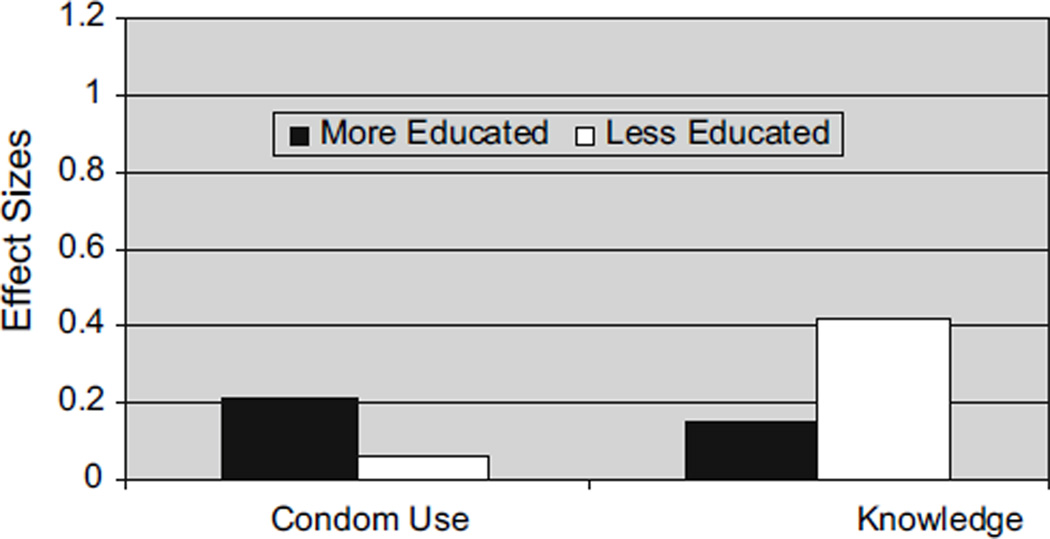
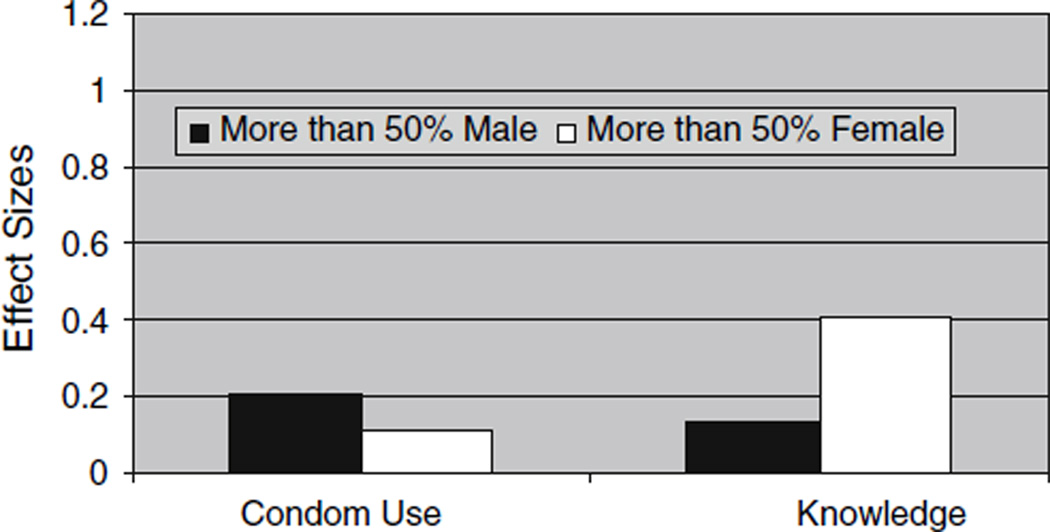
Some analyses were conducted to explore the impact of education and gender on HIV-prevention efficacy for groups with higher concentrations of Latinos/Latin Americans. For this purpose, we built two dichotomous variables reflecting education (complete/incomplete high school) and gender (male/female) of the majority of the participants (more than 50%). In two separate analyses, we used these variables to predict behavior and knowledge change in the samples with higher percents of Latinos/Latin Americans. These analyses were conducted with intervention groups. As Fig. 3 shows, intervention groups with greater education increased their use of condoms (d = .21 vs. .06, k = 8, QB1 = 4.13, P < .05) but gained less knowledge (d = .15 vs. .42, k = 9, QB1 = 18.71, P < .001) than groups with less educated ones. With regards to gender (see Fig. 4), for the groups with higher proportion of Latinos/Latin Americans, those with a higher proportion of males increased the desired behavior more (d = .21 vs. .11, k = 19, QB1 = 6.50, P < .001) but gained less HIV-related knowledge than groups with more females (d = .13 vs. .41, k = 25, QB1 = 67.23, P < .001). With respect to nationality (see Fig. 5), intervention groups in Latin America showed more condom use but acquired less knowledge than studies in the US; QB1 = 4.69. P < .05, and 8.68, P < .01.
Fig. 3.
Condom use and knowledge increase in samples with more than 50% Latinos/Latin Americans: more vs. less educated
Fig. 4.
Condom use and knowledge increase in samples with more than 50% Latinos/Latin Americans: males vs. females
Fig. 5.
Condom use and knowledge increase: US vs. Latin America
Effects of Various Characteristics of the Interventions, the Interventionists, and the Settings
Our remaining analyses examined condom use and knowledge change in all intervention groups as a function of whether interventions (a) included various strategies like attitudinal arguments and behavioral skills training, (b) had expert or lay sources and had sources that were demographically similar or dissimilar, and (c) were presented in community settings or clinics and directed to groups or to individuals. The mean analyses conducted to describe these effects are summarized in Table 2. Tables 3 and 4 present the same analyses except that they consider education and gender as additional moderators using only the groups with higher percents of Latinos/Latin Americans.
Table 2.
Effects of characteristics of the interventions, the interventionists, and the settings as a function of percent of Latinos/Latin Americans
| Moderator | Higher percent of Latinos/Latin Americans (50–100%) |
Lower percent of Latinos/Latin Americans (0–49.99%) |
Overall | ||||
|---|---|---|---|---|---|---|---|
|
d. |
QB1 for simple effect |
d. |
QB1 for simple effect |
QB1 for interaction |
|||
| Strategy include |
Strategy not included |
Strategy included |
Strategy not included |
||||
| Behavior: Condom use | |||||||
| Intervention strategies (k = 162) | |||||||
| Attitudinal arguments | .31 | .48 | 11.89*** | .46 | .41 | 6.96** | 127.37*** |
| Normative arguments | −.22 | .57 | 185.21*** | .41 | .50 | 17.42*** | 138.16*** |
| Behavioral-skills arguments | .13 | .38 | 19.51*** | .61 | .31 | 117.67*** | 93.81*** |
| Threat-inducing arguments | .45 | .35 | 5.29* | .31 | .55 | 240.57*** | 49.04*** |
| Any kind of information | .41 | – | – | .47 | .38 | 8.62** | – |
| Interpersonal skills training | .08 | .52 | 66.586*** | .43 | .46 | 1.02 | 58.57*** |
| Condom use skills training | .17 | .46 | 32.51*** | .47 | .43 | 4.06* | 44.24*** |
| Self-management training | –.16 | .20 | 3.85* | .61 | .25 | 152.81*** | 15.43*** |
| HIV counseling and testing | –.13 | .34 | 53.17*** | .68 | .25 | 627.10*** | 176.26*** |
| Condom provision | .30 | .47 | 11.31*** | .44 | .42 | 1.08 | 12.83*** |
| Intervention sources | |||||||
| Expert (k = 115) | .19 | .31 | 3.13 | .42 | .14 | 376.95*** | 102.50*** |
| Lay community member (k = 106) | .03 | .20 | 12.71*** | .27 | .29 | .94 | 9.31** |
| Ethnic similarity (k = 66) | .11 | .14 | .09 | .28 | .07 | 109.45*** | 5.74* |
| Gender similarity (k = 89) | .11 | .14 | .09 | .40 | .07 | 393.28*** | 13.24*** |
| Age similarity (k = 52) | .03 | .09 | .53 | .19 | .07 | 8.22** | 3.49 |
| Intervention settings (k = 162) | |||||||
| Clinic | .08 | .20 | 5.54* | .54 | .12 | 880.57*** | 103.18*** |
| Community settings | .14 | .20 | 1.57 | .16 | .34 | 188.44*** | 8.84** |
| Type of presentation (k = 162) | |||||||
| Group | .17 | .13 | .07 | .33 | .19 | 104.35*** | .32 |
| Individual | .14 | .19 | 1.23 | .19 | .34 | 117.52*** | 4.82* |
| HIV related knowledge | |||||||
| Intervention strategies (k = 168) | |||||||
| Attitudinal arguments | .32 | .81 | 68.56*** | .41 | .44 | 1.76 | 57.93*** |
| Normative arguments | .52 | .42 | 2.44 | .38 | .43 | 4.67* | 4.75* |
| Behavioral-skills arguments | .38 | .48 | 2.50 | .41 | .46 | 2.71 | .54 |
| Threat-inducing arguments | .54 | .38 | 9.92** | .47 | .39 | 19.98*** | 2.49 |
| Any kind of information | .65 | – | – | .64 | .21 | 164.42*** | – |
| Intervention sources | |||||||
| Expert (k = 139) | .44 | .52 | 2.90 | .66 | .36 | 363.42*** | 65.30*** |
| Lay community member (k = 132) | .72 | .39 | 54.98*** | .41 | .56 | 95.47*** | 104.48*** |
| Ethnic similarity (k = 86) | .49 | .69 | 8.63** | .43 | .55 | 30.34*** | 1.41 |
| Gender similarity (k = 112) | .51 | .69 | 6.66** | .41 | .57 | 83.15*** | .08 |
| Age similarity (k = 94) | .84 | .65 | 7.53** | .65 | .52 | 30.69*** | .62 |
| Intervention settings (k = 168) | |||||||
| Clinic | .62 | .40 | 18.59*** | .38 | .52 | 44.13*** | 42.06*** |
| Community settings | .23 | .56 | 62.79*** | .67 | .44 | 203.47*** | 157.04*** |
| Type of presentation (k = 2168) | |||||||
| Group | .45 | – | – | .54 | .15 | 313.20*** | – |
| Individual | .35 | .59 | 33.60*** | .29 | .52 | 102.41*** | .02 |
Note: All factors were dummy coded (strategy [e.g., experts or normative arguments] included = 1; strategy not included = 0). d. = fixed-effects weighted model means adjusted for all other effects. Control means for higher and lower percents of Hispanics were .05 in both cases. QB for simple and main effect = homogeneity coefficient for the difference across levels of a factor, distributed as a χ2 with number of factor levels −1 degrees of freedom. QB for interaction = homogeneity coefficient for the interaction between factors, distributed as a χ2 with (number of levels of factor A − 1) × (number of levels of factor B − 1) degrees of freedom. Significant QBs indicate significant effects of the involved factors. k = number of conditions in analysis. –: could not be calculated due to incomplete cells
P < .05;
P < .01.
P < .001
Table 3.
Effects of characteristics of the interventions, the interventionists, and the settings as a function of education (samples with at least 50% of Latinos/Latin Americans): condom use
| Intervention Characteristics |
Majority completed high school |
Majority incomplete high school |
Overall | ||||
|---|---|---|---|---|---|---|---|
|
d. |
QB1 for simple effect |
d. |
QB1 for simple effect |
QB1 for interaction |
|||
| Strategy include |
Strategy not included |
Strategy included |
Strategy not included |
||||
| Intervention strategies (k = 69) | |||||||
| Attitudinal arguments | .71 | .52 | 4.81* | .16 | .68 | 10.87** | 63.07*** |
| Normative arguments | – | .55 | – | .39 | .38 | .00 | 15.67*** |
| Behavioral-skills arguments | .70 | .30 | 16.20*** | −.08 | .24 | 2.34 | 36.41*** |
| Threat-inducing arguments | .41 | .87 | 22.06*** | .48 | −.34 | 16.41*** | 27.14*** |
| Any kind of information | .53 | – | – | .12 | – | – | 35.23*** |
| Interpersonal skills training | .48 | .60 | 1.21 | .05 | .72 | 18.16*** | 1.29 |
| Condom use skills training | .53 | .64 | 1.26 | −.48 | .61 | 28.54*** | 98.06*** |
| Self-management training | – | .55 | – | −.37 | .53 | 19.30*** | 10.68*** |
| HIV counseling and testing | – | .28 | – | – | .09 | – | 68.90*** |
| Condom provision | .55 | .61 | .50 | – | .47 | – | 123.46*** |
| Intervention source | |||||||
| Expert (k = 47) | .44 | .44 | .00 | .14 | .00 | .84 | 9.16** |
| Lay community member (k = 45) | .04 | – | – | – | .09 | – | – |
| Ethnic similarity (k = 21) | .04 | – | – | – | .14 | – | – |
| Gender similarity (k = 35) | .04 | – | – | – | .14 | – | – |
| Age similarity(k = 23) | – | – | – | – | .09 | – | – |
| Intervention settings (k = 69) | |||||||
| Clinic | – | .21 | – | – | .09 | – | – |
| Community settings | .04 | .44 | 30.98*** | .14 | .03 | .84 | .37 |
| Type of presentation (k = 69) | |||||||
| Group | .20 | – | – | .09 | – | – | – |
| Individual | – | .21 | – | – | .09 | – | – |
Note: All factors were dummy coded (strategy [e.g., experts or normative arguments] included = 1; strategy not included = 0). d. = fixed-effects weighted model means adjusted for all other effects. Control means for higher and lower education were .13 and .21, respectively. QB for simple and main effect = homogeneity coefficient for the difference across levels of a factor, distributed as a χ2 with number of factor levels −1 degrees of freedom. QB for interaction = homogeneity coefficient for the interaction between factors, distributed as a χ2 with (number of levels of factor A − 1) × (number of levels of factor B −1) degrees of freedom. Significant QBs indicate significant effects of the involved factors. k = number of conditions in analysis. –: could not be calculated due to incomplete cells
Table 4.
Effects of characteristics of the interventions, the interventionists, and the settings as a function of gender (samples with at least 13.3% of Latinos/Latin Americans): condom use
| Intervention Characteristics |
Predominantly male |
Predominantly female |
Overall | ||||
|---|---|---|---|---|---|---|---|
|
d. |
QB1 for simple effect |
d. |
QB1 for simple effect |
QB1 for interaction |
|||
| Strategy include |
Strategy not included |
Strategy included |
Strategy not included |
||||
| Intervention strategies | |||||||
| Attitudinal arguments | .61 | .53 | 1.33 | .18 | .60 | 31.31*** | 106.79*** |
| Normative arguments | – | .63 | .00 | −.27 | .53 | 146.68*** | 72.54*** |
| Behavioral-skills arguments | .87 | .49 | 18.19*** | −.14 | .48 | 78.15*** | 57.67*** |
| Threat-inducing arguments | .49 | .62 | 4.38* | .64 | .53 | 19.48*** | 12.41*** |
| Any kind of information | .57 | – | – | .28 | – | – | 105.83*** |
| Interpersonal skills training | .70 | .63 | .63 | −.09 | .60 | 100.31*** | 34.91*** |
| Condom use skills training | .75 | .61 | 4.66* | −.31 | .62 | 161.06*** | 181.60*** |
| Self-management training | – | .39 | – | −.11 | .11 | 1.49 | 89.79*** |
| HIV counseling and testing | – | .37 | – | −.10 | .32 | 34.65*** | 193.70*** |
| Condom provision | .55 | .48 | .97 | .17 | .51 | 22.03*** | 267.68*** |
| Intervention sources | |||||||
| Expert (k = 112) | .30 | .44 | 2.29 | .13 | .00 | 1.13 | 2.04 |
| Lay community member (k = 104) | .04 | .23 | 6.20* | .02 | .19 | 6.74** | 3.06 |
| Ethnic similarity (k = 64) | .11 | – | – | .11 | .14 | .07 | – |
| Gender similarity (k = 89) | .11 | – | – | .11 | .14 | .07 | – |
| Age similarity (k = 52) | – | – | – | .02 | .09 | .53 | – |
| Intervention settings (k = 159) | |||||||
| Clinic | – | .21 | – | .08 | .17 | 2.30 | – |
| Community settings | .11 | .44 | 24.85*** | .20 | .07 | 4.13* | 24.95*** |
| Type of presentation (k = 159) | |||||||
| Group | .21 | – | – | .13 | .13 | .00 | – |
| Individual | .23 | .21 | .07 | .11 | .15 | .34 | 5.89* |
Note: All factors were dummy coded (strategy [e.g., experts or normative arguments] included = 1; strategy not included = 0). d. = fixed-effects weighted model means adjusted for all other effects. Control means for predominantly male and female samples were .21 and .04, respectively. QB for simple and main effect = homogeneity coefficient for the difference across levels of a factor, distributed as a χ2 with number of factor levels –1 degrees of freedom. QB for interaction = homogeneity coefficient for the interaction between factors, distributed as a χ2 with (number of levels of factor A −1) × (number of levels of factor B −1) degrees of freedom. Significant QBs indicate significant effects of the involved factors. k = number of conditions in analysis. –: could not be calculated due to incomplete cells
Effects of Different Intervention Strategies
This study also sought to determine whether different types of strategies commonly used in HIV prevention were more or less successful at increasing condom use and knowledge in groups with higher (vs. lower) percent of Latinos/Latin Americans. For this purpose, we analyzed change as a function of all the coded strategies entered simultaneously, including also the dichotomous percent of Latin background as well as interactions between Latin background and each strategy at a time. Thus, the analyses of each strategy represent its effect independently of (covarying out) the effects of other strategies. All possible strategies were analyzed for condom use; only passive strategies were analyzed for knowledge.
As Table 2 shows, fewer strategies were efficacious for groups with higher percent of Latino/Latin Americans s as compared with groups with lower percent of Latinos/Latin Americans. That is, in samples with fewer Latinos/Latin Americans, attitudinal and behavioral skills arguments, information provision, condom-use skills training, self-management training, and HIV counseling and testing were associated with increased condom use. In contrast, only threat inducing strategies were associated with increased condom use in samples with a higher percent of Latinos/Latin Americans. Further, three strategies decreased condom use in samples with a higher proportion Latinos/Latin Americans (i.e., normative arguments, self-management skills training, and HIV counseling and testing), whereas no strategy did so in samples with fewer Latinos/Latin Americans. Threat-inducing strategies were associated with greater knowledge change in both samples.
Education may impact the way in which Latinos/Latin Americans behave and react to different intervention strategies. Thus, we repeated the analyses in Table 2 by only taking samples with higher percents of Latinos/Latin Americans and adding education alone and in interaction with each intervention strategy at the time while controlling for all other strategies. Interestingly, education analyses (see Table 3) showed that groups with more Latinos/Latin Americans and higher educational levels increased condom use when intervention strategies used attitudinal and behavioral-skills arguments. In turn, lower educated groups with high percents of Latinos/Latin Americans increased condom use in response to threat-inducing strategies, but decreased condom use when interventions included behavioral skills arguments, and condom-use and self-management-skills training.
The analyses to establish if gender moderated the impact of intervention content in samples with higher percents of Latinos/Latin Americans were very similar. That is, we repeated the analyses in Table 2 by only taking samples with higher percents of Latinos/Latin Americans and adding gender alone and in interaction with each intervention strategy at the time while controlling for all other strategies. These procedures (see Table 4) revealed 10 significant interactions. Three of these analyses suggested that male dominated samples increased condom use when interventions included behavioral skills arguments and condom use training but had no change when interventions included threat-inducing arguments. In contrast, females responded favorably only to threat inducing arguments and decreased condom use interventions included normative and behavioral skills arguments, interpersonal and condom-use-skills training, and HIV counseling and testing. In addition, the predominantly female group showed no change in response to attitudinal arguments.
A last set of analyses of intervention strategies, crossed samples with higher percents of Latinos with US and Latin-American nationality. The only significant interaction was for fear inducing arguments, and condom-skills training (See Table 5).3 Fear-inducing arguments had a positive effect in the US but a negative effect in Latin-American countries (See Table 5). In contrast, condom-use skills training had a negative effect in the US, but a positive effect in other countries.
Table 5.
Effects of characteristics of the interventions, the interventionists, and the settings for studies conducted in the US vs. Latin America (samples with at least 50% of Latinos/Latin Americans): condom use
| Intervention Characteristics |
Study conducted in the US |
Study conducted in Latin America |
Overall | ||||
|---|---|---|---|---|---|---|---|
|
d. |
QB1 for simple effect |
d. |
QB1 for simple effect |
QB1 for interaction |
|||
| Strategy include |
Strategy not included |
Strategy included |
Strategy not included |
||||
| Intervention strategies (k = 162) | |||||||
| Attitudinal arguments | −.24 | .53 | 34.40*** | .60 | .60 | .02 | 154.08*** |
| Normative arguments | –.22 | .27 | 19.80*** | – | .62 | – | 1.62 |
| Behavioral-skills arguments | –.19 | .43 | 36.33*** | .86 | .45 | .83*** | 3.59 |
| Threat-inducing arguments | .53 | −.16 | 36.52*** | .48 | .72 | 19.80*** | 37.14*** |
| Any kind of information | −.04 | – | – | .66 | – | – | 57.70*** |
| Interpersonal skills training | −.12 | .39 | 8.68** | .62 | .59 | .77 | .32 |
| Condom use skills training | –.36 | .58 | 83.05*** | .74 | .58 | 5.87** | 354.29*** |
| Self-management training | −.20 | −.25 | .63 | – | .42 | – | 53.34*** |
| HIV counseling and testing | −.18 | .20 | 15.00*** | – | .41 | – | 149.63*** |
| Condom provision | −.38 | .40 | 64.59*** | .61 | .61 | – | 326.81*** |
| Intervention source | |||||||
| Expert (k = 113) | .02 | .00 | .03 | .26 | .44 | 4.71* | .31 |
| Lay community member (k = 106) | .02 | .00 | .04 | .04 | .22 | 10.10** | .63 |
| Ethnic similarity (k = 66) | .02 | .00 | .02 | .14 | .20 | .21 | .60 |
| Gender similarity (k = 89) | .02 | .00 | .02 | .14 | .20 | .21 | .07 |
| Age similarity (k = 52) | .02 | .00 | .04 | – | .20 | – | – |
| Intervention settings (k = 162) | |||||||
| Clinic | .02 | .05 | .11 | .28 | .21 | .44 | 1.36 |
| Community settings | .00 | .03 | .04 | .15 | .40 | 20.57*** | 3.37 |
| Type of presentation (k = 69) | |||||||
| Group | .03 | .13 | .34 | .22 | – | – | – |
| Individual | .03 | .03 | – | .22 | .21 | .01 | .14 |
Note: All factors were dummy coded (strategy [e.g., experts or normative arguments] included = 1; strategy not included = 0). d. = fixed-effects weighted model means adjusted for all other effects. Control means for higher and lower education were .13 and .21, respectively. QB for simple and main effect = homogeneity coefficient for the difference across levels of a factor, distributed as a χ2 with number of factor levels −1 degrees of freedom. QB for interaction = homogeneity coefficient for the interaction between factors, distributed as a χ2 with (number of levels of factor A −1) × (number of levels of factor B −1) degrees of freedom. Significant QBs indicate significant effects of the involved factors. k = number of conditions in analysis. –: could not be calculated due to incomplete cells
Effects of Agent Characteristics
As mentioned above, the use of peer sources for interventions has become popular, in particular for Latino/Latin Americans populations. Our study examined how the presence of experts or lay community members among the intervention sources affected behavioral and knowledge change. In addition, similar analyses explored these effects with regards to the source’s demographic similarity to the recipients. These findings are summarized in Table 2 and were conducted by introducing one source variable at a time as well as the dichotomous Latin-ethnicity predictor and the interaction between the two. There were significant interactions for inclusion of experts and community members on both behavior and knowledge change. Specifically, the inclusion of lay community members decreased condom use but increased HIV related knowledge in the groups with high proportions of Latinos/Latin Americans. Correspondingly, samples with lower proportion of Latinos/Latin Americans increased condom use and knowledge when interventions used experts as sources. No significant moderation of these findings was found when education, gender, or nationality were considered.
Further, our study was also intended to assess the impact of the source’s similarity to recipient (in terms of race, gender, and age) on behavior and knowledge change. For behavior change, there were significant interactions with percent of Latinos/Latin Americans in all cases but age. These analyses indicated that none of the similarities had significant effects on behavior for samples with higher proportion of Latinos/Latin Americans. In contrast, samples with lower percents of Latinos/Latin Americans increased condom use when sources were similar in ethnicity, gender, and age. For knowledge change, there were no interactions between proportion of Latinos/Latin Americans and demographic similarities. Across the board, groups increased HIV knowledge more when sources were age similar, but less when the source were gender and ethnic similar. Unfortunately, the interactions with education, gender, and nationality could not be tested due to incomplete cells.
Setting/Groups Versus Individual Presentations
A final analysis considered change as a function of the setting and formats variables, each introduced separately. A large portion of the interventions took place in health centers (or clinics) and community settings like neighborhood organizations. This setting interacted with Latin ethnicity for both behavior and knowledge change. For samples with higher proportion of Latinos/Latin Americans, interventions at clinics were successful at increasing knowledge but less successful at increasing condom use. Interventions taking place at community settings had a negative impact on knowledge but no significant impact on behavior (see Table 2). In contrast, groups with lower percents of Latinos/Latin Americans increased condom use when interventions were conducted in health centers but not in community contexts. Education analyses revealed that community settings proved unsuccessful in increasing condom use in lower educated samples with high percents of Latinos/Latin Americans (see Table 3). Unfortunately, we did not have enough cases to asses the effect of education for clinics. In turn, gender analyses showed that unlike samples with higher percents of males and Latinos/Latin Americans, samples with higher percents of Latinos/Latin Americans and females increased condom use when interventions took place in community settings (see Table 4). Finally, there were no interactions between settings and nationality (Table 5).
With respect to whether interventions were more efficacious when directed to groups or individuals, our study revealed that the group format produced more important increases in both condom use and knowledge in samples with lower numbers of Latinos/Latin Americans (see Table 2). Results for samples with more Latinos/Latin Americans were not significant. Supplementary analyses of education, gender, and nationality showed no significant differences either (see Tables 2 and 3).
Discussion
Overall, participants in the 277 intervention groups summarized in this meta-analysis increased condom use and HIV-related knowledge. However, groups with higher proportions of Latinos/Latin Americans increased condom use less and acquired less knowledge than groups with lower proportion of Latinos/Latin Americans. This finding is worrisome in suggesting that interventions are less efficacious at increasing protective behavior in one of the populations that is disproportionately affected by HIV/AIDS.
Also, it was surprising that only threat inducing strategies proved efficacious in increasing condom use and knowledge in samples with higher proportion of Latinos in the US. Furthermore, the use of this strategy was also efficacious with samples of lower education and greater proportion of women. According to this finding, HIV prevention models concentrating on the role of the perceived threat posed by a health problem (for example, Rosenstock et al., 1994) may have greater application among Latino populations than any other group. In contrast, a number of different strategies were effective in increasing condom use among populations with lower percents of Latinos (i.e., attitudinal and behavioral skills arguments, information provision, condom use skills and self-management training, and HIV counseling and testing). We believe that this difference gives support to the contention that HIV prevention campaigns for the Latino population need to attend to culture (Marín et al., 1997; Ortiz-Torres et al., 2000). However, more research needs to be conducted to determine why threat-inducing arguments may be more effective among persons of Latino origin relative to other backgrounds.
Consistent with the need of separating culture from education, in this paper we found that education had an important moderating role in the efficacy of HIV prevention campaigns. In this regard, our study showed for samples with higher proportion of Latinos/Latin Americans, more educated populations increased condom use to a greater extent than less educated ones. However, they also gained less knowledge. One possible explanation for the latter result is that more educated populations may have more previous knowledge about HIV/AIDS. Our study also showed that the strategies that were effective among more and less educated populations for samples with high percents of Latinos/Latin Americans were different. Attitudinal and behavioral skills arguments worked better among more educated populations, whereas only threat inducing arguments worked among less educated ones. Although further research may be required, we believe that education should be carefully considered when designing HIV prevention strategies for Latinos/Latin Americans.
Another important finding of this review is that predominately Latino/Latin Americans samples with higher proportions of males showed greater improvement in condom use than samples with higher proportion of females. This difference offers support for the contention that gender roles should receive great attention in designing HIV prevention interventions for Latin/Latin Americans populations (Gomez & Marin, 1996; Marin & Marin, 1992; Marin, Gomez, Tschann & Gregorich, 1997). The reasons for the more limited positive change in females are presently unclear. However, it may be that the prevalent Machismo4 among Latinos/Latin Americans limits women’s involvement in condom use decisions, resulting in less increase in both condom use and knowledge about these issues. At the same time, Latino/Latin American women are considered pure beings, and are not expected to discuss sexual issues with their sex partners (Gómez & Marín, 1996). Thus, it seems imperative to find methods to effectively empower women from Latin backgrounds so that they can be proactive regarding condom use.
Our study also showed some differences with regards to the prevention strategies more effective among samples with more Latino/Latin American men and women. Latino/Latin American men increased condom use when intervention strategies included behavioral skills arguments and condom skills training. Although condom-use training may work for men for the obvious reason that these men may be in charge of condom-use decisions, the efficacy of behavioral skills arguments for Latino/Latin American males may require further research. Social cognitive theory (Bandura, 1986) states that that people will engage in the protective behavior when they have the necessary skills (behavioral skills) that yield successful performance of the behavior (and also the knowledge about the transmission and prevention of the disease). In turn, the literature on Latino gender roles tells us that Latino males consider themselves as sexual beings, and believe that their sexual impulses are beyond their control (Marín & Marín, 1992). Thus, intervention strategies that give Latino/Latin American men control-enhancing tools may be effective.
Our findings with regards to the strategies that were effective among Latino/Latin American women may also require further research. As mentioned above, Latino/Latin American women responded well to strategies that emphasized the perceived threat of HIV. But there were several strategies that reduced condom use among Latino/Latin American women (normative and behavioral skills arguments, interpersonal skills, condom use, and self-management training, and HIV counseling and testing). Because Latino/Latin American women had less increase in condom use than Latino/Latin American men, the failure of these specific strategies may be the reflection of the general difficulty of Latino/Latin American women in changing their behavior. In turn, this difficulty may be related to the above mentioned machismo culture prevalent among populations from Latin backgrounds.
Our results with regards to the source of the intervention (expert vs. lay community member, source similarity (ethnic, gender, or age), the type of setting (clinic vs. community center), and the format of the intervention (group vs. individual) are less conclusive. With regards to the source of the intervention, we found that the use of lay community members did not increase condom use for groups with higher percents of Latinos/Latin Americans (even when gender was considered) and that groups with lower percents of Latinos/Latin Americans responded well to experts. This finding with regards to Latinos is worrisome considering the use of lay community members has been recommended for HIV prevention among Latinos (Center for AIDS Prevention Studies, University of California at San Francisco, 2002; Ortiz-Torres et al., 2000). However, the use of lay community members proved effective in increasing HIV related knowledge in groups with high percents of Latinos/Latin Americans.
Source similarity did not yield any significant results for groups with more Latinos/Latin Americans but all types of source similarity were effective to change behavior in samples with fewer Latinos/Latin Americans. Ideally, more research should be conducted in this area. Interventions in clinics proved ineffective to increase condom use among groups with more Latinos/Latin Americans but were successful among samples with less Latinos/Latin Americans. Also, interventions in clinics were effective in increasing HIV related knowledge among groups with more Latinos/Latin Americans. In turn, interventions taking place in community settings increased condom use among female participants. This latter finding is important considering that very few strategies were effective among samples with higher percents of Latinas/Latin Americans. Finally, the format of the intervention (group vs. individual) made no difference for samples with more Latinos/Latin Americans, but group presentations worked better among samples with lower percents of Latinos/Latin Americans.
With regards to the differences between samples with higher proportion of Latinos in the US versus Latin Americans, we found that the first group increased condom use less but acquired knowledge. More research should be conducted to explain this finding. In supplementary analyses, we explored the composition of the samples with regards to education and gender and the only difference was that Latin American countries included more studies that were predominantly female (and females increased condom use less than males). Because this difference does not explain the cross-national differences, we believe that Latin American countries may be better than the US at designing/implementing prevention strategies that are sensitive to the needs of their population.
We also identified the types of intervention strategies that were successful among samples with higher proportions of Latinos in the United States versus Latin Americans. In this regard, we found that strategies that included attitudinal, and fear arguments were successful for samples with more Latinos in the US but not for Latin Americans. However, interventions that comprised condom use skills training and condom distribution were successful in Latin America but not in the US. We believe that these findings may be a good point of departure for further research about the differences between Latin Americans of different origins.
In closing, this meta-analysis is an important step in clarifying the HIV prevention programs that work better for populations with greater and smaller Latino/Latin Americans percents. As such, it is the first to statistically analyze the efficacy of different HIV-prevention strategies for these populations. Nonetheless, it suggests that more work is warranted for HIV prevention among Latinos. Only 23 samples had 100% Latinos, 13 of which were from Latin America. This fact is perplexing considering the incidence of the HIV/AIDS epidemic in the Latino community in the US. More empirical research must be conducted to design interventions with proven behavior-change efficacy for the Latino community.
Appendix
Papers Included in Meta-Analysis
- Allen S, Tice J, Van de Perre P, Serufilira A, Hudes E, Nsengumuremyi F, Bogaerts J, Lindan C, Hulley S. Effect of serotesting with counseling on condom use and seroconversion among HIV discordant couples in Africa. British Medical Journal. 1992;304:1605–1609. doi: 10.1136/bmj.304.6842.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asamoah-Adu A, Weir S, Pappoe M, Kanlisi N, Neequaye A, Lamptey P. Evaluation of a targeted AIDS prevention intervention to increase condom use among prostitutes in Ghana. AIDS. 1994;8:239–246. doi: 10.1097/00002030-199402000-00012. [DOI] [PubMed] [Google Scholar]
- Baldwin JI, Whiteley S, Baldwin JD. Changing AIDS-and fertility-related behavior: The effectiveness of sexual education. The Journal of Sex esearch. 1990;2:245–262. [Google Scholar]
- Barros T, Barreto D, Pérez F, Santander R, Yépez E, Abad-Franch F, Aguilar M. Un modelo de prevención primaria de las enfermedades de transmisión sexual y del VIH/SIDA en adolescentes. Revista Panameña de Salud Pública. 2001;10:86–94. doi: 10.1590/s1020-49892001000800003. [DOI] [PubMed] [Google Scholar]
- Belcher L, Kalichman S, Topping M, Smith S, Emshoff J, Norris F, Nurss J. A randomised trial of a brief HIV risk reduction counseling intervention for women. Journal of Consulting and Clinical Psychology. 1998;66:856–861. doi: 10.1037//0022-006x.66.5.856. [DOI] [PubMed] [Google Scholar]
- Bell RA, Grissom S, Stephenson JJ, Fricrson R, Hunt L, Lacefield P, Teller D. Evaluating the outcomes of AIDS education. AIDS Education and Prevention. 1990;2:71–84. [PubMed] [Google Scholar]
- Bentley ME, Spratt K, Shepherd ME, Gangakhedkar RR, Thilikavathi S, Bollinger RC, Mehendale SM. HIV testing and counseling among men attending sexually transmitted disease clinics in Pune, India: Changes in condom use and sexual behavior over time. AIDS. 1998;1:1869–1877. doi: 10.1097/00002030-199814000-00019. [DOI] [PubMed] [Google Scholar]
- Berrier J, Sperling R, Preisinger J, Evans V, Maso J, Walther V. HIV/AIDS education in a prenatal clinic: An assessment. AIDS Education and Prevention. 1991;3:100–117. [PubMed] [Google Scholar]
- Bhave G, Lindan CP, Hudes ES, Desai S, Wagle U, Tripathi SP, Mandel JS. Impact of an intervention on HIV, sexually transmitted diseases, and condom use among sex workers in Bombay, India. AIDS. 1995;9:521–530. [PubMed] [Google Scholar]
- Boekeloo BO, Schamus LA, Simmens SJ, Cheng TL, O’Connor K, D’Angelo LJ. A STD/HIV prevention trial among adolescents in managed care. Pediatrics. 1999;103:107–115. doi: 10.1542/peds.103.1.107. [DOI] [PubMed] [Google Scholar]
- Booth-Kewley S, Shaffer RA, Minagawa RY, Brodine SK. Effectiveness of two versions of a sexually transmitted diseases/human immunodeficiency virus prevention program. Military Medicine. 2002;167:254–259. [PubMed] [Google Scholar]
- Borgia P, Spadea T, Perucci CA, de Pascali V, Fano V, Schifano P, Abeni DDC. Limited effectiveness of a school-based HIV prevention campaign in Italy. European Journal of Public Health. 1997;7:411–417. [Google Scholar]
- Boyer C, Barrett DC, Peterman TA, Bolan G. Sexually transmitted disease (STD) and HIV risk in heterosexual adults attending a public STD clinic: Evaluation of a randomized controlled behavioral risk-reduction intervention trial. AIDS. 1997;11:359–367. doi: 10.1097/00002030-199703110-00014. [DOI] [PubMed] [Google Scholar]
- Branson BM, Peterman TA, Cannon RO, Ransom R, Zaidi AA. Group counselling to prevent sexually transmitted disease and HIV: A randomized trial. Sexually Transmitted Disease. 1998;25:553–560. doi: 10.1097/00007435-199811000-00011. [DOI] [PubMed] [Google Scholar]
- Brown WJ. An AIDS prevention campaign. American Behavioral Scientist. 1991;34:666–678. [Google Scholar]
- Brown LK, Barone VJ, Fritz GK, Nassau JH. AIDS education: The Rhode Island experience. Health Education Quarterly. 1991;18:195–206. doi: 10.1177/109019819101800205. [DOI] [PubMed] [Google Scholar]
- Butler RB, Schultz JR, Forsberg AD, Brown LK, Parsons JT, King G, Kocik SM, Jarvis D, Schultz SL, Manco-Johnson M the CDC Adolescent HBIEP Study Group. Promoting safer sex among HIV-positive youth with haemophilia: Theory, intervention, and outcome. Haemophilia. 2003;9:214–222. doi: 10.1046/j.1365-2516.2003.00722.x. [DOI] [PubMed] [Google Scholar]
- Butts JB, Hartman S. Project BART: Effectiveness of a behavioral intervention to reduce HIV risk in adolescents. The American Journal of Maternal/Child Nursing. 2002;27:163–169. [PubMed] [Google Scholar]
- Caceres CF, Rosasco AM, Mandel JS, Hearst N. Evaluating a School-based Intervention for STD/AIDS Prevention in Peru. Journal of Adolescent Health. 1994;15:582–591. doi: 10.1016/1054-139x(94)90143-q. [DOI] [PubMed] [Google Scholar]
- Calsyn DA, Saxon AJ, Freeman G, Jr, Whittaker S. Ineffectiveness of AIDS education and HIV antibody testing in reducing high-risk behaviors among injection drug users. American Journal of Public Health. 1992;82:573–575. doi: 10.2105/ajph.82.4.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Maisto SA, Kalichman SC, Forsyth AD, Wright EM, Johnson BT. Enhancing motivation to reduce the risk of HIV infection for economically disadvantaged urban women. Journal of Consulting and Clinical Psychology. 1997;65:531–541. doi: 10.1037//0022-006x.65.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi KH, Lew S, Vittinghoff E, Catania JA, Barrett D, Coates TJ. The efficacy of brief group counseling in HIV risk reduction among homosexual Asian and Pacific Islander men. AIDS. 1996;10:81–87. doi: 10.1097/00002030-199601000-00012. [DOI] [PubMed] [Google Scholar]
- Clark LR, Brasseux C, Richmond D, Getson P, D’Angelo LJ. Effect of HIV counseling and testing on sexually transmitted diseases and condom use in an urban adolescent population. Archive of Pediatrics and Adolescence Medicine. 1998;152:269–273. doi: 10.1001/archpedi.152.3.269. [DOI] [PubMed] [Google Scholar]
- Collins C, Kohler C, DiClemente R, Wang MQ. Evaluation of the exposure effects of a theory-based street outreach HIV intervention on African-American drug users. Evaluation and Program Planning. 1999;22:279–293. doi: 10.1016/s0149-7189(99)00018-x. [DOI] [PubMed] [Google Scholar]
- Deren S, Davis WR, Beardsley M, Tortu S, Clatts M. Outcomes of a risk-reduction intervention with HIV-risk populations: The Harlem AIDS project. AIDS Education and Prevention. 1995;7:379–390. [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Harrington KF, et al. Efficacy of an HIV prevention intervention for African American adolescent girls: a randomized controlled trial. Journal of American Medical Association. 2004;292:171–179. doi: 10.1001/jama.292.2.171. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Pies CA, Stoller EJ, Straits C, Olivia GE, Haskin J, Rutherford GW. Evaluation of school-based AIDS education curricula in San Francisco. The Journal of Sex Research. 1989;26:188–198. [Google Scholar]
- Diers JA. Efficacy of a stage-based counseling intervention to reduce the risk of HIV in women. Unpublished dissertation. New Jersey: Princeton University; 1999. [Google Scholar]
- Dilley JW, Woods WJ, Sabatino J, Lihatsh T, Adler B, Casey S, Rinaldi J, Brand R, McFarland W. Changing sexual behavior among gay male repeat testers for HIV. Journal of Acquire Immune Deficiency Syndrome. 2002;30:177–186. doi: 10.1097/00042560-200206010-00006. [DOI] [PubMed] [Google Scholar]
- Dommeyer CJ, Marquardt JL, Gibson JE, Taylor RL. The effectiveness of an AIDS education campaign on a college campus. College Health. 1989;38:131–135. doi: 10.1080/07448481.1989.9938431. [DOI] [PubMed] [Google Scholar]
- Eldridge GD, St. Lawrence JS, Little CE, Shelby MC, Brasfield TL, Service JW, Sly K. Evaluation of an HIV risk reduction intervention for women entering inpatient substance abuse treatment. AIDS Education and Prevention. 1997;9:62–76. [PubMed] [Google Scholar]
- Elkins D, Maticka-Tyndale E, Kuyyakanond T, Miller P, Haswell-Elkins M. Toward reducing the spread of HIV in northeastern Thai villages: Evaluation of a village-based intervention. AIDS Education and Prevention. 1997;9:49–67. [PubMed] [Google Scholar]
- Farley TA, Pompitius PF, Sabella W, Helgerson SD, Hadler JL. Evaluation of the effect of school-based education on adolescents’ AIDS knowledge and attitudes. Connecticut Medicine. 1991;55:15–18. [PubMed] [Google Scholar]
- Fawole JO, Asuzu MC, Oduntan SO, Brieger WR. A school-based AIDS education programme for secondary school students in Nigeria: A review of effectiveness. Health Education Research. 1999;14:675–683. doi: 10.1093/her/14.5.675. [DOI] [PubMed] [Google Scholar]
- Ferreira-Pinto JB, Ramos R. HIV/ AIDS prevention among female sexual partners of injection drug users in Ciudad Juarez, Mexico. AIDS Care. 1995;7:477–488. doi: 10.1080/09540129550126425. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychology. 2002;21:177–186. [PubMed] [Google Scholar]
- Fitzgerald AM, Stanton BF, Terreri N, Shipena H, Li W, Kahihuata J, Ricardo I, Galbraith J, de Jaeger AM. Use of westernbased HIV risk-reduction interventions targeting adolescents in an African setting. Journal of Adolescent Health. 1999;25:52–61. doi: 10.1016/s1054-139x(98)00120-7. [DOI] [PubMed] [Google Scholar]
- Flaskerud JH, Nyamathi AM. Effects of an AIDS education program on the knowledge, attitudes and practices of low income Black and Latina women. Journal of Community Health. 1990;15:343–355. doi: 10.1007/BF01324297. [DOI] [PubMed] [Google Scholar]
- Flaskerud JH, Nyamathi AM, Uman GC. Longitudinal effects of an HIV testing and counseling programme for low-income Latina women. Ethnicity and Health. 1997;2:89–103. doi: 10.1080/13557858.1997.9961818. [DOI] [PubMed] [Google Scholar]
- Ford N, Koetsawang S. A pragmatic intervention to promote condom use by female sex workers in Thailand. Bulletin of the World Health Organization. 1999;77:888–894. [PMC free article] [PubMed] [Google Scholar]
- Fox LJ, Bailey PE, Clarke-Martínez KL, Coello M, Ordoñ ez FN, Barahona F. Condom use among high-risk women in Honduras: Evaluation of an AIDS prevention program. AIDS Education and Prevention. 1993;5:1–10. [PubMed] [Google Scholar]
- Gerrard M, Rheis TJ. Retention of contraceptive and AIDS information in the classroom. The Journal of Sex Research. 1989;26:315–323. [Google Scholar]
- Goertzel TG, Bluebond-Langner M. What is the impact of a campus AIDS education course? College Health. 1991;40:87–92. doi: 10.1080/07448481.1991.9936261. [DOI] [PubMed] [Google Scholar]
- Hämäläinen S, Keinähen-Kiukaanniemi S. A controlled study of the effect of one lesson on the knowledge and attitudes of school children concerning HIV and AIDS. Health Educational Journal. 1992;51:135–138. [Google Scholar]
- Harris RM, Barker Bausell R, Scott DE, Hetherington SE, Kavanagh KH. An intervention for changing high-risk HIV behaviors of African-American drug-dependent women. Research in Nursing & Health. 1998;21:239–250. doi: 10.1002/(sici)1098-240x(199806)21:3<239::aid-nur7>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Harvey B, Stuart J, Suan T. Evaluation of a drama-in-education programme to increase AIDS awareness in South African high schools: A randomized community intervention trial. International Journal of STD and AIDS. 2000;11:105–111. doi: 10.1177/095646240001100207. [DOI] [PubMed] [Google Scholar]
- Hillman E, Hovell MF, Williams L, Hofstetter R, Burdyshaw C, Rugg D, Atkins C, Elder J, Blumbberg E. Pregnancy, STDs, and AIDS prevention: Evaluation of new image teen theatre. AIDS Education and Prevention. 1991;3:328–340. [PubMed] [Google Scholar]
- Hobfoll SE, Jackson AP. Effects of generalizability of communally oriented HIV-AIDS prevention versus general health promotion groups for single, inner-city women in urban clinics. Journal of Consulting and Clinical Psychology. 2002;70:950–960. doi: 10.1037//0022-006x.70.4.950. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE, Jackson AP, Lavin J, Britton P, Shepherd JB. Reducing inner-city women’s AIDS risk activities: A study of single, pregnant women. Health Psychology. 1994;13:397–403. doi: 10.1037//0278-6133.13.5.397. [DOI] [PubMed] [Google Scholar]
- Hoffman HJA, Klein H, Crosby H, Clark DC. Project Neighborhoods in action: An HIV related intervention project targeting drug abusers in Washington, DC. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 1999;76:419–434. doi: 10.1007/BF02351500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovell MF, Blumberg EJ, Liles S, Powell L, Morrison TC, Duran G, Sipan CL, Burkham S, Kelley N. Training AIDS and anger prevention social skills in at-risk adolescents. Journal of Counseling and Development. 2001;79:347–355. [Google Scholar]
- Huszti HC, Clopton JR, Mason PJ. Acquired immunodeficiency syndrome educational program: effects on adolescents’ knowledge and attitudes. Pediatrics. 1989;84:986–994. [PubMed] [Google Scholar]
- Jackson DJ, Rakwar JP, Richardson BA, Mandaliya K, Chohan B, Bwayo JJ, Ndinya-Achola JO, Martin HL, Jr, Moses S, Kreiss JK. Decreased incidence of sexually transmitted diseases among trucking company workers in Kenya: Results of a behavioural risk-reduction programme. AIDS. 1997;11:903–909. doi: 10.1097/00002030-199707000-00010. [DOI] [PubMed] [Google Scholar]
- Jemmott LS, Jemmott JB., III Increasing condom-use intentions among sexually active black adolescent women. Nursing Research. 1992;41:273–279. [PubMed] [Google Scholar]
- Johnson JA, Sellew JF, Campbell AE, Haskell EG, Gay AA, Bell BJ. A program using medical students to teach high school students about AIDS. Journal of Medical Education. 1988;63:522–530. doi: 10.1097/00001888-198807000-00003. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Cherry C, Browne-Sperling F. Effectiveness of a video-based motivational skills-building HIV risk-reduction intervention for inner-city African American men. Journal of Consulting and Clinical Psychology. 1999;67:956–966. doi: 10.1037//0022-006x.67.6.959. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Kelly JA, Hunter TL, Murphy DA, Tyler R. Culturally tailored HIV-AIDS risk-reduction messages targeted to African-American urban women. Journal of Consulting and Clinical Psychology. 1993;61:291–295. doi: 10.1037//0022-006x.61.2.291. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D, Coley B. Experimental component analysis of a behavioral HIV-AIDS prevention intervention for inner-city women. Journal of Consulting and Clinical Psychology. 1996;4:687–693. doi: 10.1037//0022-006x.64.4.687. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D, Coley B. Lack of positive outcomes from a cognitive-behavioral HIV and AIDS prevention intervention for inner-city men: Lessons from a controlled pilot study. AIDS Education and Prevention. 1997;9:299–313. [PubMed] [Google Scholar]
- Kegeles SM, Hays RB, Coates TJ. The Mpowerment project: A community-level HIV prevention intervention for young gay men. American Journal of Public Health. 1996;86:1129–1136. doi: 10.2105/ajph.86.8_pt_1.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JA, McAuliffe TL, Sikkema KJ, Murphy DA, Somlai AM, Mahy GM, Miller JG, Stevenson LY, Fernandez MI. Reduction in risk behavior among adults with severe mental illness who learned to advocate for HIV prevention. Psychiatric Services. 1997a;18:1283–1288. doi: 10.1176/ps.48.10.1283. [DOI] [PubMed] [Google Scholar]
- Kelly JA, Murphy DA, Sikkema KJ, McAuliffe TL, Roffman RA, Solomon LJ, Winett RA, Kalichman SC the Community HIV Prevention Research Collaborative. Randomized, controlled, community-level HIV-prevention Intervention for sexual-risk behavior among homosexual men in US cities. The Lancet. 1997b;350:1500–1505. doi: 10.1016/s0140-6736(97)07439-4. [DOI] [PubMed] [Google Scholar]
- Kelly JA, Murphy DA, Washington CD, Wilson TS, Koob JJ, Davis DR, Ledezma G, Davantes B. The effect of HIV/AIDS intervention groups for high-risk women in urban clinics. American Journal of Public Health. 1994;84:1918–1922. doi: 10.2105/ajph.84.12.1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JA, St. Lawrence JS, Diaz YE, Stevenson LY, Hauth AC, Brasfield TL, Kalichman SC, Smith JE, Andrew ME. HIV risk behavior reduction following intervention with key opinion leaders of population: An experimental analysis. American Journal of Public Health. 1991;81:168–171. doi: 10.2105/ajph.81.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kipke MD, Boyer C, Hein K. An evaluation of an AIDS risk reduction education and skills training (arrest) program. Journal of Adolescent Health. 1993;14:533–539. doi: 10.1016/1054-139x(93)90136-d. [DOI] [PubMed] [Google Scholar]
- Kirby D, Korpi M, Adivi C, Weissman J. An impact evaluation of project SNAPP: And AIDS and pregnancy prevention middle school program. AIDS Education and Prevention. 1997;9:44–61. [PubMed] [Google Scholar]
- Klepp KI, Ndeki SS, Leshabari MT, Hannan PJ, Lyimo BA. AIDS education in Tanzania: Promoting risk reduction among primary school children. American Journal of Public Health. 1997;87:1931–1936. doi: 10.2105/ajph.87.12.1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazebnik R, Grey SF, Ferguson C. Integrating substance abuse content into an HIV riskreduction intervention: A pilot study with middle school-aged Hispanic students. Substance Abuse. 2001;22:105–117. doi: 10.1080/08897070109511450. [DOI] [PubMed] [Google Scholar]
- Li X, Stanton B, Feigelman S, Galbraith J. Unprotected sex among African-American adolescents: A three year study. Journal of the National Medical Association. 2002;94:789–796. [PMC free article] [PubMed] [Google Scholar]
- Lindenberg CS, Solorzano RM, Bear D, Strickland O, Galvis C, Pittman K. Reducing substance use and risky sexual behavior among young, low-income, Mexican-American women: Comparison of two interventions. Applied Nursing Research. 2002;16:137–148. doi: 10.1053/apnr.2002.34141. [DOI] [PubMed] [Google Scholar]
- MacLachlan M, Chimombo M, Mpeba N. AIDS Education for youth through active learning: A school-based approach from Malawi. International Journal of Educational Development. 1997;17:41–50. [Google Scholar]
- MacNair RR, Elliott TR, Yoder B. AIDS prevention groups as persuasive appeals: Effects on attitudes about precautionary behaviors among persons in substance abuse treatment. Small Group Research. 1991;22:301–319. [Google Scholar]
- MacNair-Semands RR, Cody WK, Simono RB. Sexual behavior change associated with a college HIV course. AIDS Care. 1997;9:727–738. doi: 10.1080/713613222. [DOI] [PubMed] [Google Scholar]
- Malow RM, West JA, Corrigan SA, Pena JM, Cunningham SC. Outcome of psychoeducation for HIV risk reduction. AIDS Education and Prevention. 1994;6:113–125. [PubMed] [Google Scholar]
- Mansfield CJ, Conroy ME, Emans SJ, Woods ER. A Pilot study of AIDS education and counseling of high-risk adolescents in an office setting. Journal of Adolescent Health. 1993;14:115–119. doi: 10.1016/1054-139x(93)90095-7. [DOI] [PubMed] [Google Scholar]
- McCusker J, Stoddard AM, Hindin RN, Garfield FB, Frost R. Changes in HIV risk behavior following alternative residential programs of drug abuse treatment and AIDS education. Annals of Epidemiology. 1996;6:119–125. doi: 10.1016/1047-2797(95)00128-x. [DOI] [PubMed] [Google Scholar]
- McCusker J, Stoddard AM, Zapka JG, Lewis BF. Behavioral outcomes of AIDS education interventions for drug users in short term treatment. American Journal of Public Health. 1993;83:1463–1466. doi: 10.2105/ajph.83.10.1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuinness T, Mason M, Tolbert G, DeFontaine C. Becoming responsible teens: Promoting the health of adolescents in foster care. Journal of the American Psychiatric Nurse Association. 2002;8:92–98. [Google Scholar]
- McMahon RC, Malow RM, Jennings TE, Gómez CJ. Effects of a cognitive-behavioral HIV prevention intervention among HIV negative male substance abusers in VA residential treatment. AIDS Education and Prevention. 2001;13:91–107. doi: 10.1521/aeap.13.1.91.18921. [DOI] [PubMed] [Google Scholar]
- Mercer MA, Gates N, Holley M, Malunga L, Arnold R. Rapid KABP survey for evaluation of NGO HIV/AIDS prevention projects. AIDS. Education and Prevention. 1996;8:143–154. [PubMed] [Google Scholar]
- Miller RL. Assisting gay men to maintain safer sex: An evaluation of an AIDS service organization’s safer sex maintenance program. AIDS Education and Prevention. 1995;7:48–63. [PubMed] [Google Scholar]
- Miller RL, Klotz D, Eckholdt HM. HIV prevention with male prostitutes and patrons of hustler bars: Replication of an HIV preventive intervention. American Journal of Community Psychology. 1998;26:97–131. doi: 10.1023/a:1021886208524. [DOI] [PubMed] [Google Scholar]
- Miller TE, Booraem C, Flowers JV, Iversen AE. Changes in knowledge, attitudes, and behavior as a result of a community-based AIDS prevention program. AIDS Education and Prevention. 1990;2:12–23. [PubMed] [Google Scholar]
- Neaigus A, Sufian M, Friedman SR, Goldsmith DS, Stepherson B, Mota P, Pascal J, Des Jarlais DC. Effect of outreach intervention on risk reduction among intravenous drug users. AIDS Education and Prevention. 1990;2:253–271. [PubMed] [Google Scholar]
- Newman C, Durant RH, Seymore Ashworth C, Gaillard G. An evaluation of a school-based AIDS/HIV education program for young adolescents. AIDS. Education and Prevention. 1993;5:327–339. [PubMed] [Google Scholar]
- Ngugi EN, Plummer FA, Simonsen JN, Cameron DW, Bosire M, Waiyaki P, Ronald AR, Ndinya-Achola JO. Prevention of transmission of human immunodeficiency virus in Africa: Effectiveness of condom promotion and health education among prostitutes. The Lancet. 1988;15:887–890. doi: 10.1016/s0140-6736(88)92480-4. [DOI] [PubMed] [Google Scholar]
- NIMH Multisite HIV Prevention Trial Group. Social-cognitive theory mediators of behavior change in the National Institute of Mental Health Multisite HIV Prevention Trial. Health Psychology. 1998;20:369–376. [PubMed] [Google Scholar]
- Nyamathi AM, Stein JA. Assessing the impact of HIV risk reduction counseling in impoverished African American women: A structural equations approach. AIDS Education and Prevention. 1997;9:253–273. [PubMed] [Google Scholar]
- Nyamathi AM, Flaskerud J, Bennett C, Leake B, Lewis C. Evaluation of two AIDS education programs for impoverished Latina women. AIDS Education and Prevention. 1994;6:296–309. [PubMed] [Google Scholar]
- Nyamathi AM, Flaskerud JH, Leake B, Dixon EL, Lu A. Evaluating the impact of peer, nurse case-managed, and standard HIV risk-reduction programs on psychosocial and health-promoting behavioral outcomes among homeless women. Research in Nursing and Health. 2001;24:410–422. doi: 10.1002/nur.1041. [DOI] [PubMed] [Google Scholar]
- O’Hara P, Messick B, Fichtner RR, Parris D. A peer-led AIDS prevention program for students in an alternative school. Journal of School Health. 1996;66:176–182. doi: 10.1111/j.1746-1561.1996.tb06271.x. [DOI] [PubMed] [Google Scholar]
- O’Leary A, Ambrose TK, Raffaelli M, Mailbach E, Jemmott LS, Jemmott JB, III, Labouvie E, Celentano D. Effects of an HIV risk reduction project on sexual risk behavior of lowincome STD patients. AIDS Education and Prevention. 1998;10:483–492. [PubMed] [Google Scholar]
- O’Leary A, Jemmott LS, Goodhart F, Gebelt J. Effects of an institutional AIDS prevention intervention: Moderation by gender. AIDS Education and Prevention. 1996;8:516–528. [PubMed] [Google Scholar]
- Otto-Salaj LL, Kelly JA, Stevenson LY, Hoffmann R, Kalichman SC. Outcomes of a randomized small-group HIV prevention intervention trial for people with serious mental illness. Community Mental Health Journal. 2001;37:123–144. doi: 10.1023/a:1002709715201. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Weinstein RS, Maslack C. Adolescent AIDS prevention in context: Impact of peer educator qualities and classroom environments on interventions efficacy. American Journal of Community Psychology. 1997;25:289–323. doi: 10.1023/a:1024624610117. [DOI] [PubMed] [Google Scholar]
- Papaevangelou G, Roumeliotou A, Kallinikos G, Papoutsakis G, Trichopoulou E, Stefanou T. Education in preventing HIV infection in Greek registered prostitutes. Journal of Acquired Immune Deficiency Syndromes. 1988;1:386–389. [PubMed] [Google Scholar]
- Pauw J, Ferrie J, Rivera Villegas R, Medrano Martínez J, Gorter A, Egger M. A controlled HIV/AIDS-related health education programme in Managua, Nicaragua. AIDS. 1996;10:537–544. doi: 10.1097/00002030-199605000-00014. [DOI] [PubMed] [Google Scholar]
- Peterson JL, Coates TJ, Catania J, Hauck WW, Acree M, Daigle D, Hillard B, Middleton L, Hearst N. Education of an HIV risk reduction intervention among African-American homosexual and bisexual men. AIDS. 1996;10:319–325. doi: 10.1097/00002030-199603000-00011. [DOI] [PubMed] [Google Scholar]
- Picciano JF, Roffman RA, Kalichman SC, Rutledge SE, Berghuis JP. A telephone based brief intervention using motivational enhancement to facilitate HIV risk reduction among MSM: A pilot study. AIDS and Behavior. 2001;5:251–262. [Google Scholar]
- Ploem C, Byers S. The effects of two AIDS risk-reduction interventions on heterosexual college women’s AIDS-related knowledge, attitudes and condom use. Journal of Psychology and Human Sexuality. 1997;9:1–23. doi: 10.1300/j056v09n01_01. [DOI] [PubMed] [Google Scholar]
- Ponton LE, DiClemente RJ, McKenna S. AIDS education and prevention program for hospitalized adolescents. Journal of American Academy of Child and Adolescent Psychiatry. 1991;30:729–734. [PubMed] [Google Scholar]
- Quirk ME, Godkin MA, Schwenzfeier E. Evaluation of two AIDS prevention interventions for inner-city adolescent and young adult women. American Journal of Preventive Medicine. 1993;9:21–26. [PubMed] [Google Scholar]
- Rao AV, Swaminathan R, Baskaran S, Belinda C, Andla G, Saleem K. Behaviour change in HIV infected subjects following health education. Indian Journal of Medical Research. 1991;93:345–349. [PubMed] [Google Scholar]
- Reeder GD, Pryor JB, Harsh L. Activity and similarity in safer sex workshops led by peer educators. AIDS Education and Prevention. 1997;9:77–89. [PubMed] [Google Scholar]
- Rhodes F, Wolitski R. Affect of instructional videotapes on AIDS knowledge and attitudes. College Health. 1989;37:266–271. doi: 10.1080/07448481.1989.9937493. [DOI] [PubMed] [Google Scholar]
- Rigby K, Brown M, Anagnostou P, Ross MW, Rosser BRS. Shock tactics to counter AIDS: The Australian experience. Psychology and Health. 1989;3:145–159. [Google Scholar]
- Rosser BRS, Bockting WO, Rugg DL, Robinson BBE, Ross MW, Bauer GR, Coleman E. A randomized controlled intervention trial of a sexual health approach to long term HIV risk reduction for men who have sex with men: Effects of the intervention on unsafe sexual behavior. AIDS Education and Prevention. 2002;14:59–71. doi: 10.1521/aeap.14.4.59.23885. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Koopman C, Haignere C, Davies M. Reducing HIV sexual risk behaviors among runaway adolescents. Journal of the American Medical Association. 1991;266:1237–1242. [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Lee MB, Murphy DA, Futterman D, Duan N, Birnbaum JM, Lightfoot M the Teens Linked to Care Consortium. Efficacy of a preventive intervention for youth living with HIV. American Journal of Public Health. 2001;91:400–405. doi: 10.2105/ajph.91.3.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Murphy DA, Fernández MI, Srinivasan S. A brief HIV intervention for adolescents and young adults. American Journal of Orthopsychiatry. 1998;68:553–563. doi: 10.1037/h0080364. [DOI] [PubMed] [Google Scholar]
- Ruder AM, Flam R, Flatto D, Curran AS. AIDS education: Evaluation of school and worksite based presentations. New York State Journal of Medicine. 1990;90:129–133. [PubMed] [Google Scholar]
- Sampaio M, Brites C, Stall R, Hudes ES, Hearst N. Reducing AIDS risk among men who have sex with men in Salvador, Brazil. AIDS and Behavior. 2002;6:173–181. [Google Scholar]
- Schinke SP, Gordon AN. Self-Instruction to prevent HIV infections among African-American and Hispanic-American adolescents. Journal of Consulting and Clinical Psychology. 1990;58:432–436. doi: 10.1037//0022-006x.58.4.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scollay PA, Doucett M, Perry M, Winterbottom B. AIDS education of college students: the effect of an HIV-positive lecturer. AIDS Education and Prevention. 1992;4:160–171. [PubMed] [Google Scholar]
- Shrier LA, Ancheta R, Goodman E, Chiou VM, Lyden MR, Emans SJ. Randomized controlled trial of a safer sex intervention for high-risk adolescent girls. Archive of Pediatrics and Adolescent Medicine. 2001;155:73–79. doi: 10.1001/archpedi.155.1.73. [DOI] [PubMed] [Google Scholar]
- Shulkin JJ, Mayer JA, Wessel LG, de Moor C, Elder JP, Franzini LR. Effects of a peer-led AIDS intervention with university students. College Health. 1991;40:75–79. doi: 10.1080/07448481.1991.9936259. [DOI] [PubMed] [Google Scholar]
- Siegel DM, Aten MJ, Roghmann KJ, Enaharo M. Early effects of a school-based human immunodeficiency virus infection and sexual risk prevention intervention. Archive of Pediatrics and Adolescent Medicine. 1998;152:961–970. doi: 10.1001/archpedi.152.10.961. [DOI] [PubMed] [Google Scholar]
- Siegel DM, DiClemente R, Durbin M, Krasnorsky F, Saliba P. Change in junior high school students aid-related knowledge, misconceptions, attitudes, and HIV-preventive behaviors: Effects of a school-based intervention. AIDS Education and Prevention. 1995;7:534–543. [PubMed] [Google Scholar]
- Sikkema KJ, Kelly JA, Winett RA, Solomon LJ, Cargill VA, Roffman RA, McAuliffe TL, Heckman TG, Anderson EA, Wagstaff DA, Norman AD, Perry MJ, Crumble DA, Mercer MB. Outcomes of a randomized community-level HIV prevention intervention for women living in 18 low-income housing developments. American Journal of Public Health. 2000;90:57–63. doi: 10.2105/ajph.90.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikkema KJ, Winett RA, Lombard DN. Development and Evaluation of an HIV-Risk Reduction Program for Female College Students. AIDS Education and Prevention. 1995;7:145–159. [PubMed] [Google Scholar]
- Singh YN, Malaviya AN. Experience of HIV prevention interventions among female sex workers in Delhi, India. International Journal of STD and AIDS. 1994;5:56–57. doi: 10.1177/095646249400500113. [DOI] [PubMed] [Google Scholar]
- Slap GB, Plotkin SL, Najma K, Michelman DF, Forke C. A human immunodeficiency virus peer education program for adolescent females. Journal of Adolescent Health. 1992;12:434–441. doi: 10.1016/1054-139x(91)90020-x. [DOI] [PubMed] [Google Scholar]
- Smith MU, Katner HP. Quasiexperimental evaluation of three AIDS prevention activities for maintaining knowledge, improving attitudes, and changing risk behaviors of high risk school seniors. AIDS Education and Prevention. 1995;7:391–402. [PubMed] [Google Scholar]
- Smith MU, Dane FC, Archer ME, Devereux RS, Katner HP. Students together against negative decisions (STAND): Evaluation of a schoolbased sexual risk-reduction intervention in the rural south. AIDS Education and Prevention. 2000;12:49–70. [PubMed] [Google Scholar]
- St. Lawrence JS, Crosby RA, Basfield T, O’Bannon RE., III Reducing STD and HIV risk behavior of substance-dependent adolescents: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2002;70:1010–1021. [PubMed] [Google Scholar]
- St. Lawrence JS, Jefferson KW, Alleyne E, Brasfield TL. Comparison of education versus behavioral skills training interventions in lowering sexual HIV-risk of substance-dependent adolescents. Journal of Consulting and Clinical Psychology. 1995;63:154–157. doi: 10.1037//0022-006x.63.1.154. [DOI] [PubMed] [Google Scholar]
- St. Lawrence JS, Wilson TE, Eldridge GD, Brasfield TL, O’Bannon RE., III Community-based interventions to reduce low income, African American women’s risk of sexually transmitted diseases: A randomized controlled trial of three theoretical models. American Journal of Community Psychology. 2001;29:937–964. doi: 10.1023/A:1012919700096. [DOI] [PubMed] [Google Scholar]
- Stall RD, Paul JP, Barrett DC, Crosby GM, Bein E. An outcome evaluation to measure changes in sexual risk-taking among gay men undergoing substance use disorder treatment. Journal of Studies on Alcohol. 1999;60:837–844. doi: 10.15288/jsa.1999.60.837. [DOI] [PubMed] [Google Scholar]
- Stanton BF, Li X, Kahihuala J, Fitzgerald AM, Neumbo S, Kanduuombe G, Ricardo IB, Galbraith JS, Terreri N, Guevara I, Shipena H, Strijdom J, Clemens R, Zimba RF. Increased protected sex and abstinence among Namibian youth following a HIV risk-reduction intervention: A randomized longitudinal study. AIDS. 1998;12:2473–2380. doi: 10.1097/00002030-199818000-00017. [DOI] [PubMed] [Google Scholar]
- Stanton BF, Li X, Ricardo I, Galbraith J, Feigelman S, Kaljee L. A randomized, controlled effectiveness trial of an AIDS prevention program for low-income African-American youths. Archives of Pediatrics and Adolescent Medicine. 1996;150:363–372. doi: 10.1001/archpedi.1996.02170290029004. [DOI] [PubMed] [Google Scholar]
- Sterk CE, Theall KP, Elifson KW. Effectiveness of a risk reduction intervention among African American women who use crack cocaine. AIDS Education and Prevention. 2003;15:15–32. doi: 10.1521/aeap.15.1.15.23843. [DOI] [PubMed] [Google Scholar]
- The Centers for Disease Control AIDS Community Demonstration Projects Research Group. Community-level HIV intervention in 5 cities: Final outcome data from the CDC AIDS Community Demonstration Projects. American Journal of Public Health. 1999;89:336–345. doi: 10.2105/ajph.89.3.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toro-Alfonso J, Varas-Díaz N, Andújar-Bello I. Evaluation of an HIV/AIDS prevention intervention targeting Latino gay men and men who have sex with men in Puerto Rico. AIDS Education and Prevention. 2002;14:445–456. doi: 10.1521/aeap.14.8.445.24110. [DOI] [PubMed] [Google Scholar]
- Valdiserri RO, Lyter DW, Kingsley LA, Leviton LC, Schofield JW, Huggins J, Ho M, Rinaldo CR. The effect of group education on improving attitudes about AIDS risk reduction. New York State Journal of Medicine. 1987;87:272–278. [PubMed] [Google Scholar]
- Valente T, Bharath U. An evaluation of the use of drama to communicate HIV/AIDS information. AIDS Education and Prevention. 1999;11:203–211. [PubMed] [Google Scholar]
- Van Griensven GJP, Limanonda B, Ngaokeow S, Ayuthaya SIN, Poshyachinda V. Evaluation of a targeted HIV prevention programme among female commercial sex workers in the south of Thailand. Sexually Transmitted Infections. 1998;74:54–58. doi: 10.1136/sti.74.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaz RG, Gloyd S, Trindade R. The effect of peer education on STD and AIDS knowledge among prisoners in Mozambique. International Journal of STD and AIDS. 1996;7:51–54. doi: 10.1258/0956462961917069. [DOI] [PubMed] [Google Scholar]
- Walden VM, Mwangulube K, Makhumula-Nkhoma P. Measuring the impact of a behaviour change intervention for commercial sex workers and their potential clients in Malawi. Health Education Research. 1999;14:545–554. doi: 10.1093/her/14.4.545. [DOI] [PubMed] [Google Scholar]
- Walter HJ, Vaughan RP. AIDS risk reduction among a multiethnic sample of urban high school students. Journal of the American Medical Association. 1993;270:725–730. [PubMed] [Google Scholar]
- Waters JA, Morgen K, Kuttner P, Schmitt B. The ‘‘Guiding Adolescents to Prevention’’ program: Reducing HIV transmission and drug use in youth in a detention center. Crisis intervention. 1996;3:85–96. [Google Scholar]
- Week K, Levy SR, Zhu C, Perhats C, Handler A, Flay BR. Impact of a school-based AIDS prevention program on young adolescents’ selfefficacy skills. Health Education Research. 1995;10(3):329–344. [Google Scholar]
- Winett RA, Anderson ES, Moore JF, Taylor CD, Hook RJ, Webster DA, Neubauer TE, Harden MC, Mundy LL. Efficacy of a home-based human immunodeficiency virus prevention video program for teens and parents. Health Education Quarterly. 1993;20:555–567. doi: 10.1177/109019819302000413. [DOI] [PubMed] [Google Scholar]
- Xiaoming S, Yong W, Choi KH, Lurie P, Mandel J. Integrating HIV prevention education into existing family planning services: Results of a controlled trial of a community-level intervention for young adults. AIDS and Behavior. 2000;4:103–110. [Google Scholar]
Footnotes
The US Census Bureau (2003) defines Latino or Hispanic as those persons living in the US who indicate that their origin is Mexican, Puerto Rican, Cuban, Central or South American, or some other Hispanic origin. In this paper, “Latin background, origin, or ethnicity” includes Latin Americans and Latinos. Latin Americans are those living in Latin America.
For other general characteristics of the studies see Table 1.
There were other significant interactions that showed no significant simple effects for either one of or both groups (See Table 5).
The traditional gender role of Machismo can have positive aspects as well like protection of the women and family. Thus, further research should explore the potential of this trait of Machismo for HIV/AIDS prevention.
Contributor Information
Julia Albarracin, Western Illinois University, Macomb, IL, USA.
Dolores Albarracin, Email: dalbarra@ufl.edu, Psychology Department, University of Florida, Gaineville, FL 32608, USA.
Marta Durantini, Psychology Department, University of Florida, Gaineville, FL 32608, USA.
References
- Ajzen I, Madden TJ. Prediction of goal-directed behavior: Attitudes, intentions, and perceived behavioralc-Control. Journal of Experimental Social Psychology. 1986;22:453–474. [Google Scholar]
- Albarracín D, McNatt PS, Klein C, Ho R, Mitchell A, Kumkale GT. Persuasive communications to change actions: An analysis of behavioral and cognitive impact in HIV prevention. Health Psychology. 2003;22:166–177. doi: 10.1037//0278-6133.22.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, Gillette J, Earl A, Glasman LR, Durantini MR, Ho MH. A test of major assumptions about behavior change: A comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychological Bulletin. 2005;131:856–897. doi: 10.1037/0033-2909.131.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amaro H. Considerations for prevention of HIV infection among Hispanic women. Psychology of Women Quarterly. 1998;12:429–443. [Google Scholar]
- Amaro H. Love, sex, power: Considering women’s realities in HIV prevention. American Psychologist. 1995;50:437–447. doi: 10.1037//0003-066x.50.6.437. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- Becker BJ. Synthesizing standardized mean-change measures. British Journal of Mathematical & Statistical Psychology. 1988;41:257–278. [Google Scholar]
- Belcher L, Kalichman S, Topping M, Smith S, Emshoff J, Norris F, Nurss J. A randomised trial of a brief HIV risk reduction counseling intervention for women. Journal of Consulting and Clinical Psychology. 1998;66:856–861. doi: 10.1037//0022-006x.66.5.856. [DOI] [PubMed] [Google Scholar]
- Center for AIDS Prevention Studies, University of California at San Francisco. What are US Latinos’ HIV prevention needs? 2002 Retrieved May 19, 2005, from http://www.caps.ucsf.edu/latinotext.html.
- CDC. Documentation for the brief street intercept and coffee shop interview questionnaires. Atlanta, GA: Community Demonstration Projects Research Group; 1993. [Google Scholar]
- CDC Division of HIV/AIDS Prevention. The state of Latinos in HIV prevention community planning. 2002 Retrieved April 27, 2005, from http://www.cdc.gov/hiv/pubs/SLCP/epidemic.htm.
- Cook TD, Campbell DT. Quasi-experimentation: Design and analysis issues for field settings. Boston: Houghton Mifflin Company; 1979. [Google Scholar]
- Darbes L, Kennedy GE, Peersman G, Zohrabyan L, Rutherford GW. Systematic review of HIV behavioral prevention research in Latinos. 2002 Retrieved November 10, 2004, from http://hivinsite.ucsf.edu/In-Site.jsp?page=kb-07-04-11.
- Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1:170–177. [Google Scholar]
- Durantini MR, Albarracín D, Earl A, Mitchell AL. Conceptualizing the influence of social agents of change: A meta-analysis of HIV prevention interventions for different groups. Psychological Bulletin. 2006;132:212–248. doi: 10.1037/0033-2909.132.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbein M, Ajzen I. Belief, attitude, intention and behavior: An introduction to theory and research. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- Fishbein M, Bandura A, Triandis HC, Kanfer FH, Becker MH, Middlestadt SE, Eichler A. Report prepared for the National Institute of Mental Health (NIMH) Bethesda, MD: NIMH; 1992. Factors influencing behavior and behavior change. [Google Scholar]
- Gómez CA, Marín BV. Gender, culture, and power: Barriers for HIV-prevention strategies for women. Journal of Sex Research. 1996;33:355–362. [Google Scholar]
- Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychological Methods. 1998;3:486–504. [Google Scholar]
- Hedges LV, Olkin I. Statistical methods for meta-analysis. Orlando, FL: Academic Press; 1985. [Google Scholar]
- Hunter JE, Schmidt FL. Fixed effects vs. random effects meta-analysis models: Implications for cumulative research knowledge. International Journal of Selection and Assessment. 2000;8:275–292. [Google Scholar]
- Johnson BT, Carey MP, Marsh KL, Levin KD, Scott-Sheldon LA. Interventions to reduce sexual risk for the Human Immunodeficiency Virus in adolescents, 1985–2000: A research synthesis. Archives of Pediatrics and Adolescent Medicine. 2003;157:381–388. doi: 10.1001/archpedi.157.4.381. [DOI] [PubMed] [Google Scholar]
- Kamb ML, Fishbein M, Douglas JM, Jr, Rhodes F, Rogers J, Bolan G, Zenilman, Hoxworth T, Malotte CK, Iatesta M, Kent C, Lentz A, Graziano S, Byers, Peterman TA. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: A randomized controlled trial. Project RESPECT Study Group. Journal of the American Medical Association. 1998;280:1161–1167. doi: 10.1001/jama.280.13.1161. [DOI] [PubMed] [Google Scholar]
- Latino Commission on AIDS. Latinos & HIV/AIDS. 2004 Retrieved April 26, 2005, from http://www.latinoaids.org/nlaad/2004/latihiv_latinos.asp.
- Marín BV, Gomez CA, Tschann JM, Gregorich SE. Condom use in unmarried Latino men: A test of cultural constructs. Health Psychology. 1997;16:458–467. doi: 10.1037//0278-6133.16.5.458. [DOI] [PubMed] [Google Scholar]
- Marín BV, Marín G. Predictors of condom accessibility among Hispanic Americans in San Francisco. American Journal of Public Health. 1992;82:592–595. doi: 10.2105/ajph.82.4.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris SB. Distribution of the standardized mean change effect size for meta-analysis on repeated measures. British Journal of Mathematical & Statistical Psychology. 2000;53:17–29. doi: 10.1348/000711000159150. [DOI] [PubMed] [Google Scholar]
- National Alliance of State and Territorial AIDS Directors (NASTAD) Addressing HIV/AIDS: Latino perspectives and policy recommendations. (n.d.) Retrieved April 26, 2005, from http://www.nastad.org/pdf/latinodoc.pdf.
- Ortiz-Torres B, Serrano-García I, Torres-Burgos N. Subverting culture: Promoting HIV/AIDS prevention among Puerto Rican and Dominican women. American Journal of Community Psychology. 2000;28 doi: 10.1023/A:1005167917916. Retrieved May 20, 2005, from http://www.ingentaconnect.com/content/klu/ajcp/2000/00000028/00000006/00227133;jsessionid=566054shmi60r.henrietta. [DOI] [PubMed] [Google Scholar]
- Ploem C, Byers S. The effects of two AIDS risk-reduction interventions on heterosexual college women’s AIDS-related knowledge, attitudes and condom use. Journal of Psychology and Human Sexuality. 1997;9:1–23. doi: 10.1300/j056v09n01_01. [DOI] [PubMed] [Google Scholar]
- Rigby K, Brown M, Anagnostou P, Ross MW, Rosser BRS. Shock tactics to counter AIDS: The Australian experience. Psychology and Health. 1989;3:145–159. [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. The health belief model and HIV risk behavior change. In: DiClemente R, Peterson JL, editors. Preventing AIDS: Theories and methods of behavioral interventions. AIDS prevention and mental health. New York, NY: Plenum Press; 1994. pp. 5–24. [Google Scholar]
- Raudenbush SW. Random effects models. In: Cooper H, Hedges LV, editors. The handbook of research synthesis. New York: Russell Sage Foundation; 1994. pp. 301–321. [Google Scholar]
- Schaalma HP, Abraham C, Gillmore MR, Kok G. Sex education as health promotion: What does it take? Archives of Sexual Behavior. 2004;33:259–269. doi: 10.1023/B:ASEB.0000026625.65171.1d. [DOI] [PubMed] [Google Scholar]
- Turner G, Shepherd J. A method in search of a theory: Peer education and health promotion. Health Education Research. 1999;14:235–247. doi: 10.1093/her/14.2.235. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. The Hispanic population in the United States: March 2002. 2003 Retrieved April 26, 2005, from http://www.census.gov/prod/2003pubs/p20-545.pdf.
- University of California at San Francisco HIV Insite. HIV/AIDS in Latin America. 2005 Retrieved May 23, 2006, from http://hivinsite.ucsf.edu/global?page=cr05-00-00.
- Wang MC, Bushman BJ. Integrating results through meta-analytic review using SAS software. Cary, NC: SAS Institute Inc; 1999. [Google Scholar]
- Weinhardt LS, Carey MP, Johnson BT. Effects of HIV counseling and testing on sexual risk behavior: A meta-analytic review of published research, 1985–1997. American Journal of Public Health. 1999;89:1397–1405. doi: 10.2105/ajph.89.9.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]